Ovarian cancer the silent killer
THE OVARIES are the primary female reproductive organs. These glands have three important functions: they secrete hormones, they protect the eggs a female is born with, and they release eggs for possible fertilisation. Women are typically born...
THE OVARIES are the primary female reproductive organs. These glands have three important functions: they secrete hormones, they protect the eggs a female is born with, and they release eggs for possible fertilisation. Women are typically born...
1 year 4 months ago
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Evening Exercise May Offer Higher Health Benefits for Obese Adults: Study
A recent research published in the recent issue of Diabetes Care journal found that the timing of exercise plays a crucial role in reducing the risk of death and cardiovascular diseases in adults with obesity by including those with type 2 diabetes (T2D).
The study utilized accelerometry data to monitor physical activity, suggests that performing aerobic moderate to vigorous physical activity (MVPA) in the evening could be particularly beneficial.
The study utilized data from the UK biobank and encompassed a large group of a total of 29,836 adults who were classified as obese with a body mass index (BMI) of 30 kg/m2 or higher. The participants were monitored over an average period of nearly eight years. During this time, the study recorded 1,425 deaths, 3,980 cardiovascular disease (CVD) events and 2,162 microvascular disease (MVD) events among the group.
The participants were divided into categories based on the timing of their exercise routines which were at morning, afternoon and evening. The reference group consisted of the individuals who averaged less than one bout of aerobic MVPA per day. The data revealed that engaging in exercise during the evening was associated with the lowest risk of all-cause mortality with a hazard ratio (HR) of 0.39. Morning and afternoon activities also showed beneficial effects but were less pronounced when compared to evening exercises.
The risk of developing cardiovascular and microvascular diseases were significantly lower among the evening exercisers. The findings showed that evening activity was associated with a 36% lower risk of CVD and a 24% reduction in MVD risk. The benefits extended to the individuals with obesity and T2D that suggests a potentially vital strategy for managing both conditions.
The study adjusted for a variety of potential confounders by ensuring that the results robustly support the conclusion that not just the quantity, but the timing of physical activity is critical for health outcomes in obese adults. These findings could be transformative for the management strategies of obesity and type 2 diabetes that emphasizes the importance of regular physical activity and also its timing. Further research may explore the physiological mechanisms that support why evening exercise offers these health benefits.
Reference:
Sabag, A., Ahmadi, M. N., Francois, M. E., Postnova, S., Cistulli, P. A., Fontana, L., & Stamatakis, E. (2024). Timing of Moderate to Vigorous Physical Activity, Mortality, Cardiovascular Disease, and Microvascular Disease in Adults With Obesity. In Diabetes Care (Vol. 47, Issue 5, pp. 890–897). American Diabetes Association. https://doi.org/10.2337/dc23-2448
1 year 4 months ago
Diabetes and Endocrinology,Diabetes and Endocrinology News,Top Medical News
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Inhaling Fentanyl may cause irreversible brain damage, finds study
According to a report in the journal BMJ Case Reports, Inhaling the synthetic opioid fentanyl may cause potentially irreversible brain damage (toxic leukoencephalopathy). The doctors warned after treating a middle-aged man found unresponsive in his hotel room after snorting the drug.
Leukoencephalopathy refers to inflammation and damage to the brain’s white matter—the network of nerve fibres that enable the exchange of information and communication between different areas of the brain’s grey matter. Toxic leukoencephalopathy is a sudden or longstanding neurological syndrome, which has been reported after heroin inhalation. The condition manifests in various signs and symptoms, the most obvious of which are neurological and behavioural changes, ranging from mild confusion to stupor, coma, and death.In this case, a previously healthy man was discovered unconscious in his hotel room with unidentified crushed pills nearby. Upon admission to the hospital, he exhibited neurological deficits, including an inability to respond to questions or commands, and only responding to pain stimuli in his legs. Brain imaging revealed inflammation and swelling in the white matter and cerebellar injury, affecting his gait and balance. Despite testing negative for epilepsy, a urine test indicated exceptionally high levels of fentanyl, leading to a diagnosis of toxic leukoencephalopathy induced by fentanyl inhalation. Over the following weeks, he remained bedbound and required various medical interventions for urinary incontinence, kidney injury, cognitive impairment, suspected opioid withdrawal, pain, agitation, and pneumonia. After 26 days, he was discharged to a rehabilitation facility and later returned home with outpatient physiotherapy and occupational therapy support. Remarkably, within a year of his hospitalization, he fully recovered and resumed full-time work.“This is the first reported case associated with fentanyl. This case illustrates the need for the inclusion of fentanyl in routine urine drug screens for earlier identification and appropriate management,” said the report authors.Reference: Eden CO, Alkhalaileh DS, Pettersson DR, et alClinical and neuroradiographic features of fentanyl inhalation-induced leukoencephalopathyBMJ Case Reports CP 2024;17:e258395.
1 year 4 months ago
Neurology and Neurosurgery,Neurology & Neurosurgery News,Top Medical News,Neurology and Neurosurgery Videos,MDTV,Neurology and Neurosurgery MDTV,MD shorts MDTV,Neurology & Neurosurgery Shorts,Channels - Medical Dialogues,Latest Videos MDTV,MD Shorts
The benefits of eating pumpkin
“Different parts of the pumpkin can be used to secure different vitamins and phytonutrients the body needs”
View the full post The benefits of eating pumpkin on NOW Grenada.
“Different parts of the pumpkin can be used to secure different vitamins and phytonutrients the body needs”
View the full post The benefits of eating pumpkin on NOW Grenada.
1 year 4 months ago
Agriculture/Fisheries, Health, PRESS RELEASE, gfnc, grenada food and nutrition council, pumpkin
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
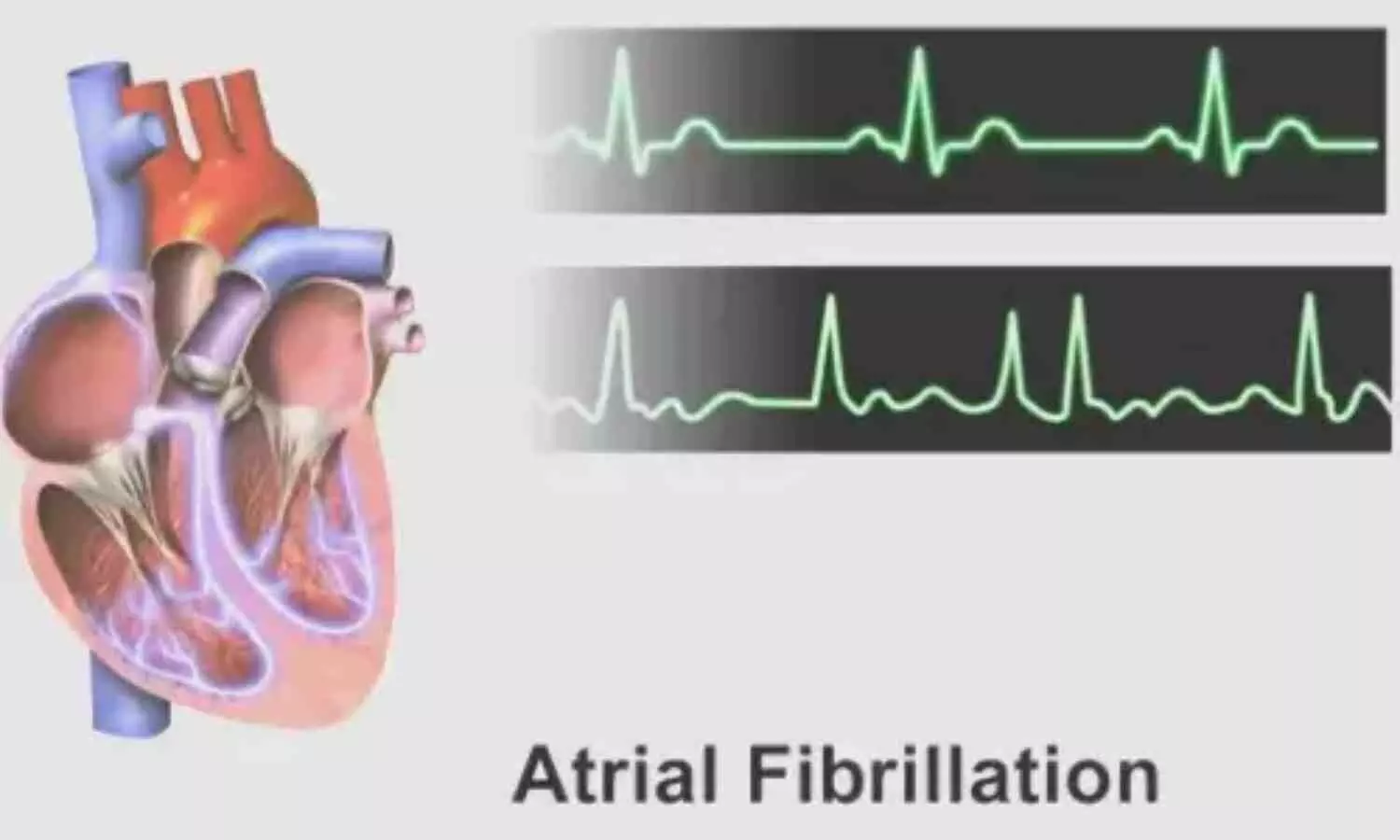
Afib more common and dangerous in younger people than previously thought, claims study
Atrial fibrillation (Afib), a common type of arrhythmia that is on the rise in people under the age of 65, is more dangerous in this increasingly younger population than previously thought, according to a new study published today in Circulation Arrhythmia and Electrophysiology and authored by physician-scientists at the UPMC Heart and Vascular Institute.
The study, which is among the first to examine a large group of Afib patients younger than 65 in the U.S., found that these younger patients were more likely to be hospitalized for heart failure, stroke or heart attack and had significantly higher rates of comorbidity and mortality, compared to similarly aged and gender-matched people who do not have Afib.
“Common knowledge among cardiologists is that, in people under 65, Afib is extremely uncommon and not detrimental. But there really hasn’t been any data to back that up,” said lead author Dr. Aditya Bhonsale, M.D., M.H.S, a UPMC cardiac electrophysiologist in HVI’s Division of Cardiology who is also an assistant professor of medicine at the University of Pittsburgh.
“At UPMC, we've been seeing a lot more young patients with Afib in recent years and have been interested in understanding the real-world clinical course of these individuals. As a payer-provider with patient records across more than 40 hospitals, UPMC was uniquely positioned to ask this question, which no one has been able to ask before,” Bhonsale added.
Drawing from the electronic health records of 67,221 UPMC patients seeking care for Afib from 2010 through 2019, the researchers found that more than a quarter of them (17,335) were under the age of 65, a stark contrast to the 2% prevalence commonly estimated. The high proportion likely reflects an increasing burden of cardiovascular risk factors in younger Americans, said Bhonsale.
The UPMC team found that over the course of a decade, survival rates for those with the arrythmia were 1.3 to 1.5 times worse for men with Afib, and 1.82 to 3.16 times worse for women, compared to similarly aged patients who did not have Afib. The patients studied also had high rates of cardiovascular disease risk factors, including smoking, obesity, hypertension and sleep apnea, which contribute to damaging structural and electrical changes in the heart over time.
“We are optimistic that data from this study will foster future investigation to evaluate optimal therapies for patients with Afib,” said senior author Sandeep Jain, M.D., director of cardiac electrophysiology in HVI’s Division of Cardiology who is also a professor of medicine at the University of Pittsburgh.
Reference:
Aditya Bhonsale, Jianhui Zhu, Floyd Thoma, Steve Koscumb, Krishna Kancharla, Andrew Voigt, Jared Magnani, N.A. Estes, Samir Saba, Oscar Marroquin, Suresh Mulukutla and Sandeep Jain, Mortality, Hospitalization, and Cardiac Interventions in Patients With Atrial Fibrillation Aged <65 Years, Circulation: Arrhythmia and Electrophysiology, https://doi.org/10.1161/CIRCEP.123.012143.
1 year 4 months ago
Cardiology-CTVS,Cardiology & CTVS News,Latest Medical News
SeNaSa hires more than 1,500 doctors
Santo Domingo.- The director of SeNaSa emphasized that during his tenure alone, 1,549 codes have been granted to healthcare professionals. Additionally, he mentioned that he continued processing the 132 cases inherited upon assuming office, ensuring compliance with regulations set by the Superintendency of Health and Occupational Risks (Sisalril).
Santo Domingo.- The director of SeNaSa emphasized that during his tenure alone, 1,549 codes have been granted to healthcare professionals. Additionally, he mentioned that he continued processing the 132 cases inherited upon assuming office, ensuring compliance with regulations set by the Superintendency of Health and Occupational Risks (Sisalril).
The executive director of SeNaSa stated that the Dominican ARS is currently handling 28 applications, with completion imminent, and only fourteen are awaiting evaluation. “Upon completion of this process, a total of 1,591 professionals from various healthcare fields will have their codes under our administration.”
He specified that these health professionals meeting supervisory body requirements are spread across the country and represent various specialties including family medicine, urology, cardiology, pediatrics, anesthesiology, psychology, proctology, perinatology, rheumatology, neurology, internal medicine, nephrology, hematology, and obstetrics-gynecology, among others.
“We are dedicated to fostering dialogue and collaborating on solutions that benefit our members the most. Our commitment remains ensuring access to quality services that comply with current standards,” stated Dr. Hazim.
He recalled the agreement reached last year with the Dominican Medical College and Sislaril, establishing the requirements for obtaining these codes through various meetings.
Dr. Hazim concluded by affirming SeNaSa’s ongoing commitment to open dialogue in pursuit of continual enhancements in member services.
1 year 4 months ago
Health
STAT+: Former MIT biologist David Sabatini, forced out after sexual harassment accusations, to lead new Boston team
Former MIT and Whitehead Institute star biologist David Sabatini, who lost his lofty positions after being accused of violating sexual harassment policies in 2021, is rejoining the Boston scientific community as head of a research group at a new laboratory under the umbrella of a Czech-based scientific institute.
Sabatini, who has denied harassing anyone and filed litigation over the claims, has been working since last October in a senior research position at the Institute of Organic Chemistry and Biochemistry, in the Czech Republic capital of Prague, investigating scientific questions in the areas of cell growth and metabolism, similar to his past research at Whitehead.
The Czech institute, known as IOCB Prague, is realizing a long-held ambition to expand into the Boston biotech hub, confirmed the institute’s director, Jan Konvalinka.
1 year 4 months ago
In the Lab, ethics, Research, scientists, STAT+
PAHO/WHO | Pan American Health Organization
PAHO Director statement on the External Evaluation of PAHO’s Results-Based Management Framework Implementation
PAHO Director statement on the External Evaluation of PAHO’s Results-Based Management Framework Implementation
Cristina Mitchell
30 Apr 2024
PAHO Director statement on the External Evaluation of PAHO’s Results-Based Management Framework Implementation
Cristina Mitchell
30 Apr 2024
1 year 4 months ago
An Arm and a Leg: The Hack
When Change Healthcare, a subsidiary of UnitedHealth Group, got hit by a cyberattack this winter, a big chunk of the nation’s doctors, pharmacists, hospitals, and therapists stopped getting paid.
When Change Healthcare, a subsidiary of UnitedHealth Group, got hit by a cyberattack this winter, a big chunk of the nation’s doctors, pharmacists, hospitals, and therapists stopped getting paid. The hack also limited health providers’ ability to share medical records and other information critical to patient care.
The cyberattack revealed an often overlooked part of how health care is paid for in the United States and raised concerns for antitrust advocates about how large UnitedHealth has grown.
Host Dan Weissmann speaks with reporters Brittany Trang of Stat News and Maureen Tkacik of The American Prospect about their reporting on the hack and what it says about antitrust enforcement of health care companies.
Dan Weissmann
Host and producer of "An Arm and a Leg." Previously, Dan was a staff reporter for Marketplace and Chicago's WBEZ. His work also appears on All Things Considered, Marketplace, the BBC, 99 Percent Invisible, and Reveal, from the Center for Investigative Reporting.
Credits
Emily Pisacreta
Producer
Adam Raymonda
Audio wizard
Ellen Weiss
Editor
Click to open the Transcript
Transcript: The Hack
Note: “An Arm and a Leg” uses speech-recognition software to generate transcripts, which may contain errors. Please use the transcript as a tool but check the corresponding audio before quoting the podcast.
Dan: Hey there.
Brittany Trang is a reporter at STAT News– that’s a health care news outlet. We talked with Brittany’s colleague Bob Herman in our last episode. Like Bob, she’s been covering the business of health care.
And for Brittany, this story starts with Bob flagging a story to their team. He…
Brittany Trang: Dropped a link in the chat that said like, hey guys, I think we should write about this, question mark, and nobody replied,
Dan: The story was about a cyber-attack against a company called Change Healthcare.
Brittany Trang: I was like that sounds like a startup and I was like who cares about some sort of health tech startup
Dan: But Bob kept bringing it up.
Brittany Trang: And I finally clicked on the link, and I was like, oh no, this is a big deal. This touches most of the American healthcare system.
Dan: Yeah, and it’s no joke. Change Healthcare is what’s called a data clearinghouse. And it’s a big one. It’s an important part of health care’s financial plumbing. Someone had gone in and basically hijacked their computer system and said, Unless we get $22 million dollars, we’re not giving it back. So Change went offline, and a huge chunk of the country’s Pharmacists, doctors, therapists, hospitals just stopped getting paid. And Change Healthcare stayed offline for weeks and weeks. As we record this, seven weeks in, big parts of it remain offline. And here’s this other thing: Change Healthcare is not a startup. It’s been around for like 20 years. And in late 2022, Change got purchased by another company– a company that’s starting to become a real recurring character on this show: UnitedHealth Group.
You may remember: They’re the country’s biggest insurance company AND they’ve got their hands in just about every other part of health care, in a big way. For instance, they’re the very biggest employer of physicians in the country, by a huge margin. They’ve got their own bank, which– among other things– offers payday loans to doctors. And they have a huge collection of companies that do back-end services. In our last episode we heard about Navi Health— and how, under United’s ownership, insurance companies have been using NaviHealth’s algorithm to cut off care for people in nursing homes. [Boy, yeah– that was a fun story…] And as we’ve been learning: When one company like this gets so big, their problems– like this cyber-attack– become everybody’s problem. And in this case, everybody’s problem seems to create an opportunity for United. We’ll break down how THAT could possibly work, but obviously it doesn’t seem like the way a lot of us would WANT things to work.. And we’ll end up talking about what we can maybe do about it. Not “we” as in a bunch of individuals trying to tackle an opponent this big. Good luck with that. But “we” as in the “We the people” of the United States Constitution. We may already be on the case.
This is An Arm and a Leg– a show about why health care costs so freaking much, and what we can maybe do about it. I’m Dan Weissmann. I’m a reporter, and I like a challenge. So our job on this show is to take one of the most enraging, terrifying, depressing parts of American life, and bring you a show that’s entertaining, empowering, and useful.
We’ll start with an attempt to answer what you’d think would be a simple question: What does Change Healthcare do?
Here’s Brittany Trang from STAT News again.
Brittany Trang: It’s kind of like Visa or Mastercard or something. Like, when you go to the grocery store and you pay with a credit card, you are not putting your money directly into the pockets of the grocery store. There’s a middleman in there and change is that middleman, but for a ton of different things.
Dan: Like insurance claims. Brittany says hospitals and doctors offices often don’t submit claims directly to insurance companies. They send the claim to a middleman like Change. And then Change figures out where that claim needs to go next. Like: I’m sending a bunch of mail– I put it all in one mailbox, and the post office figures out how to get it where it goes. Except of course, there’s no paper here, no envelopes, no physical packages: All those claims are basically data. Which is why a company like Change is called a data clearinghouse. And even if a given provider uses some other clearinghouse– and of course there are others– Change may still be involved. Because INSURANCE companies like Aetna also use Change as a place to COLLECT claims from providers. On that side, Change is kind of like a post-office box. But claims are just one of the types of data that Change handles. For instance…
Brittany Trang: when you went to the pharmacy counter or when you would check in at the doctor’s office and they take your insurance information and figure out like what you’re going to pay for this visit. Both of those processes were messed up.
Dan: Yeah, and there’s more! Prior authorizations– like when your doctor checks in advance to make sure your insurance company is OK with paying for whatever. Those all go through companies like Change. So, if change is offline, do they do your MRI, or your surgery– and just hope it doesn’t get denied when Change comes back? And once claims get approved, data for payments goes through Change too. So payments– a lot of payments– just stopped going out. Here’s Brittany Trang.
Brittany Trang: it’s just kind of flabbergasting how big this is. This collapsed most of healthcare in some way or another.
Dan: Overall, the numbers are wild: Change reportedly processes 1.5 trillion dollars a year in claims. Maybe a third of everything that happens in healthcare. According to the American Hospital Association, 94 percent of hospitals said they were affected. Some more than others. Not all providers use Change as their primary clearinghouse. But lots do. And for them, everything just stopped.
Brittany Trang: I talked to one provider she’s like, Oh, I can, I can talk. I’m, here today and tomorrow before we close. And I was like, before we close for spring break. And she said, no, we have 3 and 13 cents left in our bank account. Brittany says that provider got a last minute reprieve– an emergency loan from United. There have been two or three rounds of these loans so far, plus some advance payments from Medicare. But as the outage has dragged on– it started in February, and we’re recording this seven weeks later– it’s hard to know if those are going to be enough. At the end of March, I talked with Emily Benson. She runs a therapy practice in a Minneapolis suburb. Eight clinicians, mostly treating kids. She says the practice does maybe 70 or 80 thousand dollars worth of business a month. But then in February… Emily Benson: essentially everything went dark for us.
Dan: United publicly acknowledged the Change hack on February 21st. But Emily Benson says she didn’t actually get a heads-up until almost a week later.
Emily Benson: a lot of alarm bells went off, that was the end of the month. And so a lot of payments came due
Dan: Her rent. Paychecks for her colleagues, and herself.
Emily Benson: I mean, I was in a panic. Y’know, I didn’t know where I was going to go.
Dan: She says she usually gets two payments a week from insurance, with everything passing through Change. But it’s not just the payments from insurance. Change also provides the documents that say how much an insurance company is GOING to pay for any given claim.
Emily Benson: That’s a critical document because that tells me what does the family owe us. And then the beneficiary is also going to get that information. So they’re not surprised by what we charge them. So now every week we’re stacking up and stacking up these amounts that the family’s going to owe us.
Dan: By the time we talked, Emily Benson had gotten two loans from United. About 40,000 each: maybe a month’s worth of billing for her, between the two loans.
Emily Benson: That first one was wiped out. Pretty quickly because now we’re on week five I’m working on the second, um, installment that I got from united. But, you know, that’s half gone now too. So I don’t know what the next step is. We’re nowhere near. Getting claims processing yet and so. I’m kind of panicking Yeah.
Emily Benson: it looks like the terms are within 45 days. You have to pay back that temporary loan. How am I going to do that if I don’t have claims coming?
Dan: God.
Emily Benson: I’m still panicking.
Dan: I’ll bet. Oh my God. You’re very, you’re very calm for somebody in this situation.
Emily Benson: Well, you know, I’ve had a lot of therapy of my own. That’s how you become a therapist. So panicking doesn’t help anyone.
Dan: I guess that’s, I’ll take that under advisement.
Dan: So, to pay back those loans– which are supposed to be repaid within 45 days– Emily Benson is gonna have to start getting paid again. As we spoke, she’d had been living without systems for filing claims and getting paid for five weeks. And even when those systems get moving again, she’s not gonna see all that money right away.
Emily Benson: Imagine the backlog and the clog. Five weeks worth of insurance claims I mean, we’re looking at a major traffic jam.
Dan: Oh myGod.Andif everybody were to work double time for the next five weeks, then it would be 10 weeks. But people can’t really work double time.
Emily Benson: When you say that out loud,
Dan: Sorry.
Emily Benson: I don’t feel as grounded,
Dan: I’m so sorry.
Emily Benson: but, but, but it’s probably realistic.
Dan: Other news outlets are talking to providers like Emily Benson all over the country. We’re recording this in mid-April. United hasn’t responded to our questions on this story, but their website says “We’re determined to make this right.” It says they’ve put out 4 point 7 billion dollars in emergency loans to providers so far. And it says that for the vast majority of Change Healthcare’s services, a restoration date is “still pending.” We have no idea what’s going to happen. What it’ll mean for our doctors, our therapists, our local hospitals. And look, there are elements of this story that go beyond health care. How many of us have personal health information– maybe financial information– that got seized by who the heck knows who in this? And yes, United’s getting some heat. They got a list of pointed questions from U.S. Representative Jamie Raskin. Their CEO is supposed to testify in a Senate hearing at the end of April. But as we’ll get into in a minute, this disaster– United’s disaster– could turn out to have a silver lining– for United: An opportunity to keep on growing. And that opportunity arises precisely because they’re so big, and doing so much business in so many parts of the medical-industrial complex. Which doesn’t sound great. It raises questions about the, uh, potential downsides for a lot of people, when individual companies get this freaking big. And it raises questions about what we can maybe do about it. And the answer is: Maybe more than we think. That’s all coming right up.
This episode of An Arm and a Leg is produced in partnership with KFF Health News. That’s a nonprofit newsroom covering health care in America. Their reporters do amazing work, and we’re honored to be in cahoots with them. So, as we’ve seen, a company like United is so big that their problems become everybody’s problem. And at least in one case that I’ve seen so far, everybody’s problem can become United’s opportunity. That’s what happened in Oregon, and a reporter from Washington, DC, was in a position to make it a national story.
Maureen Tkacik: My name is Maureen Tkacik, but you can call me Mo and I am the Investigations Editor at the American Prospect, and a Senior Fellow at the American Economic Liberties Project.
Dan: The Prospect is a politically-progressive news magazine, and the Economic Liberties Project is a non-profit that pushes an anti-monopoly agenda. A lot of Mo’s reporting looks at how financial behemoths are looking like monopolists– especially in health care. So…
Maureen Tkacik: have come to know United Healthcare, pretty well, over past, year or so,
Dan: Looking at, for instance, how they gobble up medical practices. And as we mentioned, that kind of gobbling has made United the biggest employer of physicians in the country– by huge margins– in just the last few years. About one doc in ten now works for them, as employees or “affiliates.” As we’ve reported before, big players– like United, like big hospital systems, and like private equity groups– have been gobbling up medical practices for years. And: that kind of consolidation often leads to us paying more– and often for lousier healthcare. Moe Tkacik has been reporting on that kind of gobbling– and recently, she’d been looking at how the state of Oregon had been trying to slow it down. Then, in January 2024, a good-size medical group in Corvallis, Oregon said they were ready for United to gobble them up. The group is called the Corvallis Clinic, and it’s got more than a hundred docs. But United and the Clinic would have to go through a whole process to get approval from state regulators. That process includes: regulators asking the public for comments on the transaction. And in this case…
Maureen Tkacik: they were. inundated with comments.
Dan: Like 378 of them in just a few weeks. And the comments were overwhelmingly AGAINST the sale. In February, the regulators sent United and Corvallis a 5-page list of conditions under which they might approve a deal. A source of Moe’s sent me the document, which he got through a public-records request. The conditions are like, to not reduce service levels in the community for at least 10 years. To keep accepting non-United insurance. And to submit to a lot of monitoring. Then, as negotiations were starting, Change Healthcare went offline. And in early March, Moe got a tip: The clinic and United were gonna make an end run around this process. She talked with an anonymous insider at the clinic. Who told her: It turns out that all of the clinic’s billing had been connected to Change.
Maureen Tkacik: So we’re talking about just a calamitous cash crunch. Their revenue came to a standstill
Dan: And by the time Moe’s insider source learned what was up– this had been going on for two weeks.
Maureen Tkacik: this source said that , Thursday, they all had a meeting and they were not sure they were going to be able to open their doors the following Monday.
Dan: That was Thursday March 7. The next day, March 8th, lawyers for Corvallis Clinic filed an application for an emergency exemption from the normal review process. A week later, they got that exemption. And this time regulators had not demanded any conditions. As Moe’s story laid out, United’s problem– the Change Healthcare hack– became everybody’s problem, including Corvallis. And their problem seemed to have become United’s opportunity. To gobble up the practice without having to agree to any conditions from pesky regulators. And a postscript to the Corvallis Clinic story: Shortly after regulators approved that deal, United sent notices to thousands of patients at another clinic it had taken over in nearby Eugene, saying basically: We don’t have a doctor for you anymore. Goodbye and good luck. News reports said that clinic had lost more than 30 doctors since United took over. And among the public comments urging regulators to kibosh the Corvallis clinic, a bunch of people cited lousy experiences at that Eugene clinic under United’s ownership. This is the kind of thing that Moe Tkacik and her colleagues at the American Economic Liberties Project– and what’s become a kind of anti-monopoly movement– want to change. And here’s where this episode becomes maybe just a little less of a horror story, and maybe a little more of an action movie. Because the anti-monopoly movement has gotten a big backer in the last three years: The Biden Administration. In 2017, a woman named Lina Khan made a name for herself in legal circles when she published a paper arguing that Amazon had become the kind of super-dominant company that antitrust laws were designed to constrain. Lina Khan was a law student when she published that paper. In 2021, Joe Biden appointed her to lead the Federal Trade Commission. The FTC and the Department of Justice split the job of antitrust enforcement, and they’ve both become super-aggressive. They’ve filed big lawsuits against Google, Amazon, and– in March of this year– Apple. And gotten a fair amount of attention. As we were writing up this episode, Jon Stewart interviewed Lina Khan on “The Daily Show.” And here’s how she described her approach in that conversation.
LK: We’ve really focused on how companies are behaving. Are they behaving in ways that suggest they can harm their customers, harm their suppliers, harm their workers, and get away with it? And that type of too big to care type approach is really what ends up signaling that a company has monopoly power because they can start mistreating you, but they know you’re stuck.
Dan: Earlier this year, the Wall Street Journal reported that Lina Khan’s allies– antitrust folks at the Department of Justice are investigating United. Neither the Justice Department nor United has commented on that report. Meaning: Nobody’s denied it. So far, some of the Biden administration’s antitrust lawsuits have pan out, and some haven’t. Actually, in 2021, the Justice Department sued to prevent UnitedHealth Group from buying Change Healthcare. That one, they lost. But when the sued to block Penguin Random House from buying another giant publisher, Simon and Schuster, they won. And as Lina Khan told Jon Stewart, she and her colleagues aren’t just suing to prevent mergers. They sued to get infamous Pharma Bro Martin Skhreli banned for life from the pharma trade. And they won. And they’re looking at other ways big companies, especially in health care, screw people.
LK: Just to give you one example, inhalers. They’ve been around for decades, but they still cost hundreds of dollars. So our staff took a close look and we’ve realized the, some of the patents that had been listed for these inhalers were improper. There were bogus. And so we sent hundreds of warning letters around these patents. And in the last few weeks, we’ve seen companies deal list these patents and three out of the four major manufacturers have now said, Within a couple of months, they’re going to cap how much Americans pay to just 35.
Dan: I think we should start paying a lot more attention to what Lina Khan and her colleagues are up to– and what their chances are. I’ve started reading up, and getting in touch with folks who are in this fight, and who are watching it closely. Because this is looking like the kind of action movie I kind of like. Meanwhile, I’m posting a link to Jon Stewart’s interview with Lina Khan wherever you’re listening to this. I’ll have a few other links for you in our newsletter– you can sign up for that at arm and a leg show dot com, slash, newsletter. And I’ll catch you in a few weeks. Till then, take care of yourself.
This episode of an arm and a leg was produced by me, Dan Weissmann, with help from Emily Pisacreta, and edited by Ellen Weiss. Big thanks this time to the novelist, journalist and activist Cory Doctorow, who has been writing about the antitrust revival for years, breaking down complex, technical stories in clear, accessible ways. Thanks to professor Spencer Waller from the Loyola University Chicago law school for talking about antitrust with me. And thanks to Dr. John Santa in Oregon– for sharing material he got via a public-records request to the state, and for his observations. Adam Raymonda is our audio wizard. Our music is by Dave Weiner and blue dot sessions. Extra music in this episode from Epidemic Sound. Gabrielle Healy is our managing editor for audience. She edits the first aid kit newsletter. Bea Bosco is our consulting director of operations. Sarah Ballama is our operations manager. And Armand a Leg is produced in partnership with KFF Health News. That’s a national newsroom producing in depth journalism about healthcare in America and a core program at KFF, an independent source of health policy research, polling and journalism. Zach Dyer is senior audio producer at KFF Health News. He’s editorial liaison to this show. And thanks to the Institute for Nonprofit News for serving as our fiscal sponsor, allowing us to accept tax exempt donations. You can learn more about INN at INN. org. Finally, thanks to everybody who supports this show financially– you can join in any time at arm and a leg show dot com, slash, support– and thanks for listening.
“An Arm and a Leg” is a co-production of KFF Health News and Public Road Productions.
To keep in touch with “An Arm and a Leg,” subscribe to the newsletter. You can also follow the show on Facebook and the social platform X. And if you’ve got stories to tell about the health care system, the producers would love to hear from you.
To hear all KFF Health News podcasts, click here.
And subscribe to “An Arm and a Leg” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 4 months ago
Health Care Costs, Health Industry, Multimedia, An Arm and a Leg, Podcasts
Toxic Gas Adds to a Long History of Pollution in Southwest Memphis
MEMPHIS, Tenn. — For many years, Rose Sims had no idea what was going on inside a nondescript brick building on Florida Street a couple of miles from her modest one-story home on the southwestern side of town.
Like other residents, she got an unwelcome surprise in October 2022 at a public forum held by the Environmental Protection Agency at the historic Monumental Baptist Church, known for its role in the civil rights movement. The EPA notified the predominantly Black community that Sterilization Services of Tennessee —which began operations in the brick building in the 1970s — had been emitting unacceptably high levels of ethylene oxide, a toxic gas commonly used to disinfect medical devices.
Airborne emissions of the colorless gas can increase the risk of certain medical conditions, including breast cancer. Sims, who is 59 and Black, said she developed breast cancer in 2019, despite having no family history of it, and she suspects ethylene oxide was a contributing factor.
“I used to be outside a lot. I was in good health. All of a sudden, I got breast cancer,” she said.
Local advocates say the emissions are part of a pattern of environmental racism. The term is often applied when areas populated primarily by racial and ethnic minorities and members of low-socioeconomic backgrounds, like southwest Memphis, are burdened with a disproportionate amount of health hazards.
The drivers of environmental racism include the promise of tax breaks for industry to locate a facility in a heavily minority community, said Malini Ranganathan, an urban geographer at American University in Washington, D.C. The cheaper cost of land also is a factor, as is the concept of NIMBY — or “not in my backyard” — in which power brokers steer possible polluters to poorer areas of cities.
A manager at Sterilization Services’ corporate office in Richmond, Virginia, declined to answer questions from KFF Health News. An attorney with Leitner, Williams, Dooley & Napolitan, a law firm that represents the company, also declined to comment. Sterilization Services, in a legal filing asking for an ethylene oxide-related lawsuit to be dismissed, said the use of the gas, which sterilizes about half the medical devices in the U.S., is highly regulated to ensure public safety.
Besides southwest Memphis, there are nearly two dozen locales, mostly small cities — from Athens, Texas, to Groveland, Florida, and Ardmore, Oklahoma — where the EPA said in 2022 that plants sterilizing medical devices emit the gas at unusually high levels, potentially increasing a person’s risk of developing cancer.
The pollution issue is so bad in southwest Memphis that even though Sterilization Services planned to close shop by April 30, local community leaders have been hesitant to celebrate. In a letter last year to a local Congress member, the company said it has always complied with federal, state, and local regulations. The reason for its closure, it said, was a problem with renewing the building lease.
But many residents see it as just one small win in a bigger battle over environmental safety in the neighborhood.
“It’s still a cesspool of pollution,’’ said Yolonda Spinks, of the environmental advocacy organization Memphis Community Against Pollution, about a host of hazards the community faces.
The air in this part of the city has long been considered dangerous. An oil refinery spews a steady plume of white smoke. A coal plant, which is now closed, leaked components of coal ash, such as arsenic, into the ground and groundwater, according to a corrective action report from the Tennessee Valley Authority. The TVA is proposing to gut an existing gas plant and replace turbines in the facility with new ones. A continual stream of heavy trucks chug along nearby highways and roads. Other transportation sources of air pollution include the Memphis International Airport and barge traffic on the nearby Mississippi River.
Lead contamination is also a concern, not just in drinking water but in the soil from now-closed lead smelters, said Chunrong Jia, a professor of environmental health at the University of Memphis. Almost all the heavy industry in Shelby County — and the associated pollutants — are located in southwest Memphis, Jia added.
Sources of pollution are often “clustered in particular communities,” said Darya Minovi, a senior analyst with the Union of Concerned Scientists, a nonprofit that advocates for environmental justice. When it comes to sterilizing facilities that emit ethylene oxide, areas inhabited largely by Black, Hispanic, low-income, and non-English-speaking people are disproportionately exposed, the group has found.
Four sites that the EPA labeled high-risk are in low-income areas of Puerto Rico. Seven sterilizer plants operate in that U.S. territory.
The EPA, responding to public concerns and to deepened scientific understanding of the hazards of ethylene oxide, recently released rules that the agency said would greatly reduce emissions of the toxic gas from sterilizing facilities.
KeShaun Pearson, who was born and raised in south Memphis and has been active in fighting environmental threats, said he is frustrated that companies with dangerous emissions are allowed to create “toxic soup” in minority communities.
In the area where the sterilization plant is located, 87% of the residents are people of color, and, according to the Southern Environmental Law Center, life expectancy there is about 10 years lower than the average for the county and state. The population within 5 miles of the sterilizer plant is mostly low-income, according to the Union of Concerned Scientists.
Pearson was part of Memphis Community Against the Pipeline, a group formed in 2020 to stop a crude oil pipeline that would have run through Boxtown, a neighborhood established by emancipated slaves and freedmen after the signing of the Emancipation Proclamation of 1863.
That campaign, which received public support from former Vice President Al Gore and actress-activist Jane Fonda, succeeded. After the ethylene oxide danger surfaced in 2022, the group changed the last word of its name from “pipeline” to “pollution.”
Besides breast and lymphoid cancers, animal studies have linked inhaling the gas to tumors of the brain, lungs, connective tissue, uterus, and mammary glands.
Last year, with the help of the Southern Environmental Law Center, the south Memphis community group urged the Shelby County Health Department to declare the ethylene oxide situation a public health emergency and shut down the sterilizing plant. But the health department said the company had complied with its existing air permit and with the EPA’s rules and regulations.
A health department spokesperson, Joan Carr, said Shelby County enforces EPA regulations to ensure that companies comply with the federal Clean Air Act and that the agency has five air monitoring stations around the county to detect levels of other pollutants.
When the county and the Tennessee Department of Health did a cancer cluster study in 2023, the agencies found no evidence of the clustering of high rates of leukemia, non-Hodgkin lymphoma, or breast or stomach cancer near the facility. There were “hot and cold spots” of breast cancer found, but the study said it could not conclude that the clusters were linked to the facility.
Scientists have criticized the study’s methodology, saying it did not follow the Centers for Disease Control and Prevention’s recommendations for designing a cancer cluster investigation.
Meanwhile, several people have sued the sterilizing company, claiming their health has been affected by the ethylene oxide emissions. In a lawsuit seeking class-action status, Reginaé Kendrick, 21, said she was diagnosed with a brain tumor at age 6. Chemotherapy and radiation have stunted her growth, destroyed her hair follicles, and prevented her from going through puberty, said her mother, Robbie Kendrick.
In response to proposed stricter EPA regulations, meanwhile, the Tennessee attorney general helped lead 19 other state AGs in urging the agency to “forgo or defer regulating the use of EtO by commercial sterilizers.”
Sims said she’s glad her neighborhood will have one less thing to worry about once Sterilization Services departs. But her feelings about the closure remain tempered.
“Hope they don’t go to another residential area,” she said.
[Clarification: This article was updated at 3:15 p.m. ET on May 1, 2024, to specify which substances leaked into the ground and groundwater and what changes will occur related to the Tennessee Valley Authority’s activities in Shelby County, Tennessee.]
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 4 months ago
Public Health, Race and Health, States, Disparities, Environmental Health, Florida, Oklahoma, Tennessee, texas, Virginia
Nearly half of patients with giant cell arteritis achieve remission with upadacitinib
Nearly half of patients with giant cell arteritis who received upadacitinib while tapering steroids achieved remission from weeks 12 through 52 in a phase 3 trial, according to a press release from AbbVie.“Based on these results, upadacitinib has the potential to be the first oral treatment option for patients with GCA, a disease with inflammation of the large arteries that primarily impacts ol
der people and has only one approved treatment to date commonly used with steroids,” lead investigator Daniel Blockmans, MD, PhD, of the department of general internal medicine at University
1 year 4 months ago
AbbVie’s Humira takes a hit in first-quarter 2024 financial results due to competition
AbbVie reported a worldwide net revenue of $12.31 billion in the first quarter of 2024 despite Humira sales dropping due to biosimilar competition, according to a company press release.AbbVie’s worldwide net revenue represented a 0.7% increase on a reported basis.
However, global net revenues from the company’s immunology portfolio, which totaled $5.371 billion, decreased 3.9% due to competition from Humira (adalimumab) biosimilars.Humira net revenues decreased by 35.9% globally, totaling $2.27 billion, and 39.9% in the U.S., totaling $1.771 billion. Internationally, Humira net
1 year 4 months ago
Ministry of Agriculture suspends issuance of burn permits
“By ceasing the issuance of burning licences, the Ministry of Agriculture and Lands, Forestry and Marine Resources is taking a proactive stance to protect public health and the environment”
View the full post Ministry of Agriculture suspends issuance of burn permits on NOW Grenada.
1 year 4 months ago
Agriculture/Fisheries, Environment, Health, PRESS RELEASE, burning licence, ministry of agriculture, rgpf, royal grenada police force
Health Archives - Barbados Today
Fogging schedule for May 2 – 3
The Vector Control Unit will conduct its fogging exercise for two days this week, due to the upcoming public holidays. The team will be in the parish of St Michael for both days.
On Thursday, May 2, the following districts will be sprayed: Chelston Cross Gap, Chelston Avenue and Garden, Tamarind Avenue, Chapel Place, Dalkeith Village, Seamen Village, Bullens Avenue, Paddock Road and avenues, Kings Village, Deighton Road, and Gooding Land and avenues.
The fogging exercise for the week will conclude on Friday, May 3, when the Unit visits Dayrells Road, Brathwaite Gap, Gooding Road, Plum Close, Overdene Drive, Ventor Gardens, and surrounding districts.
Fogging takes place from 4:30 to 8:30 p.m. daily. Householders are reminded to open their windows and doors to allow the spray to enter. Children should not be allowed to play in the fog.
Members of the public are advised that the completion of scheduled fogging activities may be affected by events beyond the Unit’s control. In such circumstances, the Unit will return to communities affected in the soonest possible time.
The post Fogging schedule for May 2 – 3 appeared first on Barbados Today.
1 year 4 months ago
Health, Local News
Health Archives - Barbados Today
24-hour mental health helpline with trained operators launches
If you or someone you know is struggling with a mental illness, experiencing emotional distress or harbouring thoughts of self-harm, a new 24-hour mental health hotline is officially here to help.
Lifeline Barbados – 536-4500 – was officially launched Friday by the government to offer support for mental health issues.
If you or someone you know is struggling with a mental illness, experiencing emotional distress or harbouring thoughts of self-harm, a new 24-hour mental health hotline is officially here to help.
Lifeline Barbados – 536-4500 – was officially launched Friday by the government to offer support for mental health issues.
Already, the helpline has received more than 300 calls since it began operating two months ago, revealing anxiety, depression, social issues, other personal matters, financial challenges, and thoughts of suicide among callers.
“The vast majority of the calls related to suicide ideation were categorised as low risk,” Minister of State in the Ministry of Health Davidson Ishmael told attendees at the helpline’s launch at the ministry’s Culloden Road offices. “What we found interesting and encouraging is that there were several calls from persons who simply wanted to speak to someone.”
Lifeline Barbados was established in collaboration with the Pan American Health Organisation/World Health Organisation (PAHO/WHO) with the goal of addressing the growing number of mental health challenges faced by Barbadians, particularly following the peak of the COVID pandemic, according to Ishmael.
In recent years, mental health has risen in importance for Barbadians, prompting the government to address the challenge, he said.
Ishmael said: “Barbadians would be acutely aware that we had a period of time in recent years where there was an unfortunate and undesirable spate of suicides which occurred within our island, and which captured the immediate attention of our government and varied stakeholders and partners within the mental health space. This captured attention quickly turned to robust planning, and that robust planning has led us to decisive action in the form of the creation of Lifeline Barbados.”
The hotline began operating “quietly” in February, operating from 2 p.m. to 6 p.m. daily on two shifts, including holidays. Now, with help from the ministry’s partners, training for the hotline operators has been carried out, said the minister.
“The hotline is currently staffed by 15 persons, comprising the hotline manager, four supervisors, and ten hotline operators,” Ishmael said. “The operators who man the phones and interface with the caller will be responsible for providing general mental health information, emotional support and crisis intervention services. Accordingly, I can confirm that the entire hotline staff have been trained to perform their critical functions. With the support of our strategic partner PAHO/WHO, the ministry was able to engage the services of an international consultant to develop the standard operating procedures and to train the staff in the hotline in helpline crisis intervention techniques.”
The minister stressed that although the island’s suicide rate was well below the global average, suicide and self-harm were “fully recognised” as health issues prompting the need for the helpline.
“Local health statistics show that on average, twice as many persons [have]sought out mental health services at our multiple polyclinics as compared to the pre-COVID years,” said Ishmael.
“Lifeline Barbados has been established based on international best practice guidelines, and it is anticipated that it will further enhance our national response to mental health challenges, allowing for immediate and appropriate interventions and follow-up. Ultimately, the ministry’s objective is to ensure that all citizens have improved access to quality mental health services that meet their needs, without exposing them to any financial hardships or duress.”
The minister also assured that a complete restructuring of the country’s mental health framework was on the horizon.
(SB)
The post 24-hour mental health helpline with trained operators launches appeared first on Barbados Today.
1 year 4 months ago
Health, Local News
VIDEO: Half of patients with obesity face nutritional deficiencies
DENVER — It is important for clinicians to check for nutritional deficiencies in patients with obesity, a speaker at the Obesity Medicine Association conference noted.Patients with obesity “can have a variety of different nutritional deficiencies ... [which] may not be obvious to us in the moment as we’re seeing them in our office,” Lydia C.
Alexander, MD, FOMA, DABOM, DABLM, incoming president of the Obesity Medicine Association and chief medical officer of Enara Health, explained.She pointed out that 50% of patients with obesity can have nutritional deficiencies.
1 year 4 months ago
STAT+: Up and down the ladder: The latest comings and goings
Hired someone new and exciting? Promoted a rising star? Finally solved that hard-to-fill spot? Share the news with us, and we’ll share it with others. That’s right. Send us your changes, and we’ll find a home for them. Don’t be shy. Everyone wants to know who is coming and going.
And here is our regular feature in which we highlight a different person each week. This time around, we note that Recludix Pharma hired Ajay Nirula as executive vice president and head of R&D. Previously, he worked at Eli Lilly, where he was senior vice president and the immunology therapeutic area head.
But all work and no play can make for a dull head of R&D.
1 year 4 months ago
Pharma, Pharmalot, biotechnology, Pharmaceuticals, STAT+
STAT+: Pharmalittle: We’re reading about Cigna biosimilar plans, a Vertex deal in South Africa, and more
And so, another working week will soon draw to a close. Not a moment too soon, yes? This is, you may recall, our treasured signal to daydream about weekend plans. Our agenda is likely to be low key. We plan to manicure the Pharmalot grounds, promenade with the official mascots, and catch up on our napping.
We may also hold a listening party, where the rotation may include this, this, this and this. And what about you? This is a lovely time of year to enjoy the great outdoors. Perhaps you can catch a view of some cherry blossom trees while there is still time. You could stroll city streets to take in the sights. Life is with people, as they say. Or you could hold your breath and spend time catching up on the news of the world. Well, whatever you do, have a grand time. But be safe. Enjoy, and see you soon. …
Cigna plans to make copies of AbbVie’s Humira arthritis drug available with no out-of-pocket payment to eligible patients in the U.S. using its Accredo specialty pharmacy beginning in June, Reuters writes. Cigna said it will stock high- and low-concentration versions from Boehringer Ingelheim, Teva Pharmaceutical, and Alvotech, which will be priced at about 85% lower than the $6,922.62 monthly list price of Humira. Deals were made with the manufacturers as well as its distributor Quallent to bring the out-of-pocket cost down to $0. Cigna said the move should save around $3,500 on average per year for some of the 100,000 Accredo patients using either Humira or biosimilar.
The World Health Organization says new evidence shows the extensive overuse of antibiotics during the Covid-19 pandemic worldwide, which may have exacerbated “silent” spread of antimicrobial resistance. While only 8% of hospitalized patients with Covid-19 had bacterial co-infections requiring antibiotics, some 75% of patients have been treated with antibiotics “just in case” they help. Overall, antibiotic use did not improve clinical outcomes for patients with Covid-19. The highest rate of antibiotic use was seen among patients with severe or critical Covid-19, with a global average of 81%. In mild or moderate cases, there was a considerable variation across regions.
1 year 4 months ago
Pharma, Pharmalot, pharmalittle, STAT+
Pro Consumidor clears rice brands of harmful metals
Santo Domingo.- The Executive Director of the National Institute for the Protection of Consumer Rights (Pro Consumidor), Eddy Alcántara, announced on Thursday that the initial laboratory studies conducted by the institution on a dozen rice brands sold in the country revealed no presence of harmful metals detrimental to people’s health.
Santo Domingo.- The Executive Director of the National Institute for the Protection of Consumer Rights (Pro Consumidor), Eddy Alcántara, announced on Thursday that the initial laboratory studies conducted by the institution on a dozen rice brands sold in the country revealed no presence of harmful metals detrimental to people’s health.
Speaking at a press conference held at the Pro Consumidor headquarters, Alcántara assured that these studies provide assurance that the rice consumed in the Dominican Republic poses no health risks to consumers.
The official elaborated that these laboratory examinations were prompted by complaints appearing in various media outlets alleging contamination of rice with heavy metals like mercury, copper, arsenic, and lead. “However, such concerns have been dispelled by the findings of these studies, which we are disclosing today,” he emphasized in a press release.
Alcántara clarified that the tests encompassed several domestic and imported rice brands sourced from supermarkets, grocery stores, warehouses, and other establishments. “This initial study of the marketed brands in the country ensures peace of mind and food sovereignty,” he added.
As the market surveillance authority, Alcántara affirmed that upon receiving reports from certain media outlets, they promptly collected samples for laboratory analysis. “As soon as we obtained these initial results, we are sharing them with the public,” he affirmed.
He asserted Pro Consumidor’s commitment to conducting further tests on other rice brands available in the national market until a comprehensive review is completed. Alcántara reiterated that if the presence of heavy metals is detected in any other rice brands, the responsible parties will face sanctions, and the product will be removed from the market, in accordance with consumer protection law 358-05.
He underscored that the regulations stipulate that “products and services must be supplied or provided in such a manner that, when consumed or used under normal or foreseeable conditions, they do not pose any danger, harmfulness, or unforeseen risks to the health and safety of the consumer or user.”
1 year 4 months ago
Health, Local
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Pfizer Emblaveo gets European Commission marketing nod for patients with multidrug-resistant infections and limited treatment options
New York: Pfizer Inc. has announced that the European Commission (EC) has granted marketing authorization for EMBLAVEO (aztreonam-avibactam) for the treatment of adult patients with complicated intra-abdominal infections (cIAI), hospital-acquired pneumonia (HAP), including ventilator-associated pneumonia (VAP), and complicated urinary tract infections (cUTI), including pyelonephritis.
It is also indicated for the treatment of infections due to aerobic Gram-negative organisms in adult patients with limited treatment options.
“For healthcare teams treating patients with serious Gram-negative bacterial infections, the prospect of running out of effective treatment options is a daunting but very real threat,” said Yehuda Carmeli, Head, National Institute for Antibiotic Resistance and Infection Control, Tel Aviv Medical Center, Israel, and an investigator in the REVISIT study. “The approval of EMBLAVEO is welcome news for the infectious disease community and provides new hope to critically ill patients affected by antimicrobial resistance.”
Antimicrobial resistance (AMR) – when bacteria, viruses, fungi, and parasites change and find ways to resist the effects of antimicrobial drugs – is recognized as one of the biggest threats to global health. If AMR continues to rise unchecked, minor infections could become life-threatening, and many routine medical procedures such as caesarean sections and hip replacements could become too risky to perform. Multidrug-resistant Gram-negative bacteria are of particular concern due to the high rates of morbidity and mortality they cause. Metallo-β-lactamases (MBLs) are a type of enzyme produced by certain bacteria that can result in resistance to antibiotics, and MBL-producing Gram-negative bacteria are on the rise globally. Developing new treatments for infections caused by Gram-negative bacteria has been prioritized by the World Health Organization (WHO) as a critical area of focus due to their increasing spread.
“The European Medicines Agency’s accelerated review of EMBLAVEO reflects the urgent need for new treatments to address the threat of antimicrobial resistance,” said Alexandre de Germay, Chief International Commercial Officer, Executive Vice President, Pfizer. “With this approval, Pfizer is proud to take another step forward in its commitment to developing and bringing breakthrough health solutions to patients impacted by serious infectious diseases around the world.”
This approval is based on results from the previously reported Phase 3 program comprising the REVISIT (NCT03329092) and ASSEMBLE (NCT03580044) studies evaluating the efficacy, safety, and tolerability of EMBLAVEO in treating serious bacterial infections due to Gram-negative bacteria, including MBL-producing multidrug-resistant pathogens for which there are limited or no treatment options. Data support that EMBLAVEO is effective and well-tolerated, with no new safety findings and a similar safety profile to aztreonam alone.
The marketing authorization of EMBLAVEO is valid in all 27 European Union (EU) member states, as well as in Iceland, Liechtenstein, and Norway. Marketing authorization applications for EMBLAVEO are planned for submission in other countries.
EMBLAVEO combines aztreonam, a monobactam β-lactam, with avibactam, a recent broad-spectrum β-lactamase inhibitor. MBLs are a class of β-lactamase enzymes that are not inhibited by current β-lactamase inhibitors and hydrolyze nearly all β-lactam antibiotics, with an exception being monobactams such as aztreonam. However, monobactams are degraded by other β-lactamases that are frequently co-produced with MBLs, limiting the clinical usefulness of aztreonam monotherapy.
The combination of aztreonam with avibactam restores aztreonam’s activity against bacteria that co-produce MBLs and other β-lactamases and provides a well-tolerated and effective treatment option against multidrug-resistant Gram-negative bacteria. These multidrug-resistant Gram-negative bacteria include MBL-producing Enterobacterales, which have been highlighted as a critical priority pathogen by the WHO, and S. maltophilia. EMBLAVEO is the β-lactam/β-lactamase inhibitor combination for treating serious bacterial infections in adult patients caused by multidrug-resistant Gram-negative bacteria, including MBL-producing bacteria, approved for use in the EU.
EMBLAVEO was jointly developed with AbbVie. Pfizer holds the global rights to commercialize this therapy outside of the U.S. and Canada, where the rights are held by AbbVie. Development of EMBLAVEO was also supported by public-private partnerships between Pfizer and the U.S. Department of Health and Human Services; Administration for Strategic Preparedness and Response; Biomedical Advanced Research and Development Authority (BARDA) under OTA number HHSO100201500029C; and through the EU’s Innovative Medicines Initiative(IMI) – a partnership between the EU and the European pharmaceutical industry – under a project called COMBACTE-CARE (Combatting Bacterial Resistance in Europe – Carbapenem Resistance). The COMBACTE-CARE consortium is a unique public-private collaboration that unites the knowledge and capabilities of leading drug-resistant bacterial infection experts and is supported by the COMBACTE pan-European clinical and laboratory networks.
Read also: Pfizer Gets CDSCO Panel Nod To study anti-cancer drug Lorlatinib
1 year 4 months ago
News,Industry,Pharma News,Latest Industry News