Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Alveolar ridge preservation after extraction may obviate need for additional augmentation during implant placement: Study
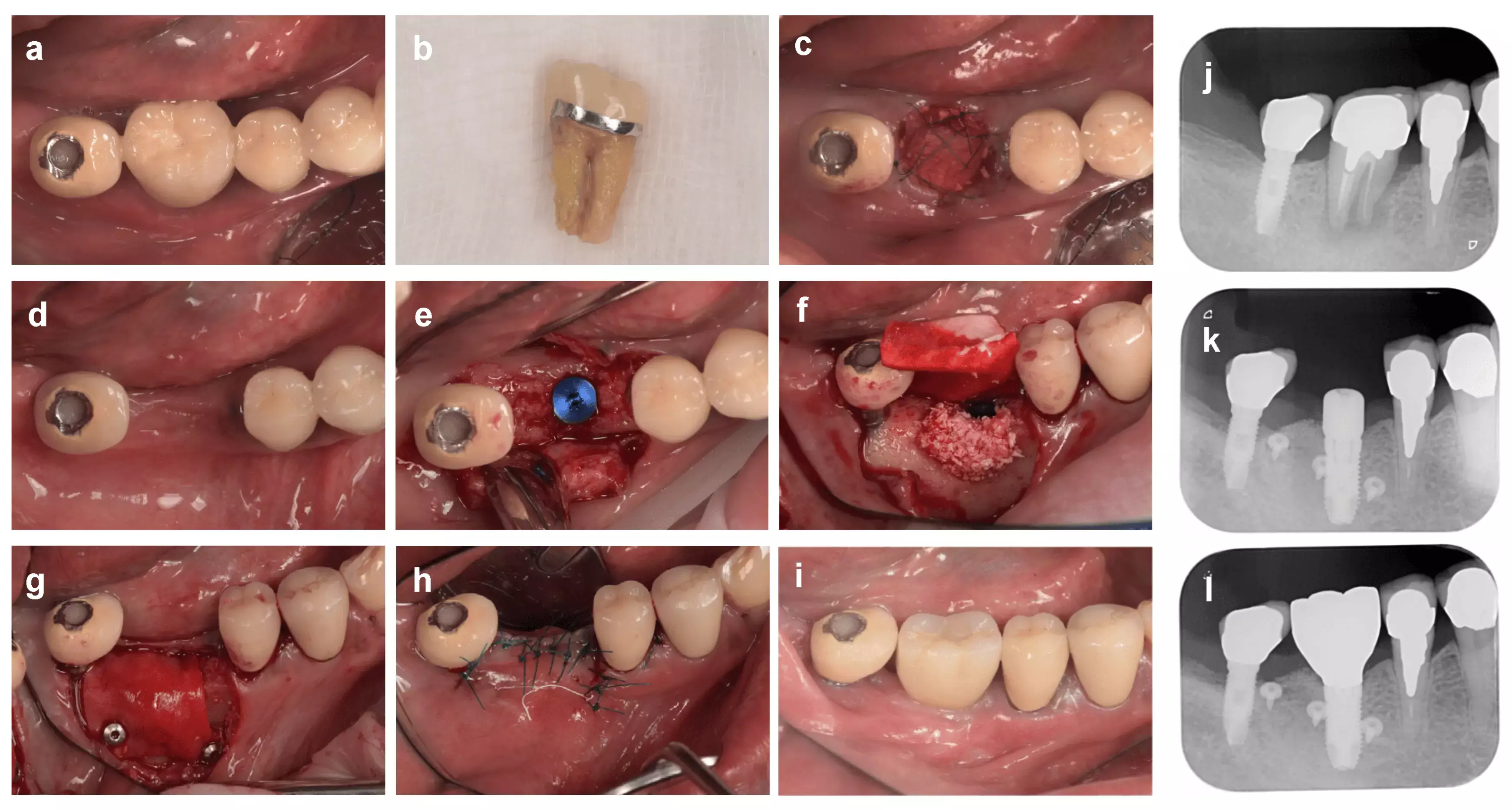
Alveolar ridge preservation after extraction may obviate the need for additional augmentation during implant placement suggests a study published in the Clinical Oral Implant Research.
This systematic review and meta-analyses aimed to evaluate the outcomes of alveolar ridge preservation (ARP) following extraction of non-molar teeth in comparison to early implant placement (EIP) in terms of clinical and radiographic changes, need for additional augmentation at the time of implant placement, patient-reported outcomes, and implant failure rate. Electronic databases were searched to identify randomized and non-randomized studies that compared ARP to EIP. The risk of bias was assessed using the Cochrane Collaboration's Risk of Bias tool. Data were analyzed using a statistical software program.
Results: A total of 106 studies were identified, of which five studies with 198 non-molar extraction sockets in 198 participants were included. Overall meta-analysis showed significant differences in changes in midfacial mucosal margin (mean difference (MD) −0.09; 95% confidence interval (CI) −0.17 to −0.01; p = .03) and ridge width (MD −1.70; 95% CI −3.19 to −0.20; p = .03) in favor of ARP. The use of ARP was also associated with less need for additional augmentation at implant placement, but the difference was not statistically significant. Within the limitation of this review, ARP following extraction of non-molar teeth has short-term positive effects on soft tissue contour, mucosal margin and thickness, and alveolar ridge width and height. It can also simplify future implant treatment by minimizing the need for additional augmentation.
Reference:
Atieh, M. A., Shah, M., Hakam, A., AlAli, F., Aboushakra, I., & Alsabeeha, N. H. M. (2024). Alveolar ridge preservation versus early implant placement in single non-molar sites: A systematic review and meta-analysis. Clinical Oral Implants Research, 00, 1–17. https://doi.org/10.1111/clr.14314
1 year 1 week ago
Dentistry News and Guidelines,Top Medical News,Dentistry News
N.J. county confirms its 3rd rabid raccoon of the season - NJ.com
- N.J. county confirms its 3rd rabid raccoon of the season NJ.com
- Rabid Raccoon Reported on Deans Lane in South Brunswick TAPinto.net
- Rabid Raccoon Fought With Dogs In South Brunswick: Police Daily Voice
- Rabid Raccoon Confirmed In South Brunswick South Brunswick, NJ Patch
- NJ resident’s dog finds a rabid animal, the 3rd in the county this year New Jersey 101.5 FM
1 year 1 week ago
Foods that promote and relieve sinus congestion
Several foods that can be consumed regularly to help ease the effects of sinusitis and congestion include pineapples, garlic, peppers, spicy foods and turmeric and ginger
View the full post Foods that promote and relieve sinus congestion on NOW Grenada.
Several foods that can be consumed regularly to help ease the effects of sinusitis and congestion include pineapples, garlic, peppers, spicy foods and turmeric and ginger
View the full post Foods that promote and relieve sinus congestion on NOW Grenada.
1 year 1 week ago
Health, PRESS RELEASE, congestion, gfnc, grenada food and nutrition council, sinus, sinusitis
PAHO/WHO | Pan American Health Organization
Addressing health equity is key to ensuring better pandemic preparedness, PAHO Director says
Addressing health equity is key to ensuring better pandemic preparedness, PAHO Director says
Oscar Reyes
30 Jul 2024
Addressing health equity is key to ensuring better pandemic preparedness, PAHO Director says
Oscar Reyes
30 Jul 2024
1 year 1 week ago
STAT+: Pharmalittle: We’re reading about the U.K. nixing coverage for a cancer drug, sharing bird flu vaccine data, and more
Top of the morning to you, and a fine one it is, despite the gray skies hovering over the Pharmalot campus.
We are doing our best to maintain sunny spirits, though, because once again, we recall some helpful wisdom from the Morning Mayor, who taught us that “Every new day should be unwrapped like a precious gift.” To celebrate the notion, we are brewing still more cups of stimulation and inviting you to join us. Our choice today is maple bourbon. Remember, a prescription is not required. So no need to fret over whether rebates are being passed along. Meanwhile, here are a few items of interest. Hope you have a meaningful and productive day and, of course, do stay in touch. …
Four pharmaceutical companies involved in the negotiations over prices for Medicare do not expect a significant impact on their businesses after seeing confidential suggested prices from the government for their drugs that will take effect in 2026, Reuters writes. Executives from Bristol Myers Squibb, Johnson & Johnson, AbbVie, and AstraZeneca, which have 5 of the 10 drugs chosen for the first wave of negotiations, described their views on quarterly conference calls. “I think the drugmakers were frightened (these prices) would be a big deal. But now, the ones who have reported or commented have actually said it seems to be OK and in line with expectations,” UBS analyst Trung Huynh.
The U.K.’s cost-effectiveness watchdog blocked the National Health Service from providing an innovative treatment for a form of advanced breast cancer, blaming AstraZeneca and Daiichi Sankyo for being “unwilling” to offer their Enhertu drug at a low enough price, The Financial Times tells us. Helen Knight, director of medicines evaluation at the National Institute for Health and Care Excellence, said cost was to blame for the decision, the first breast cancer treatment NICE rejected in six years. If a drug is not recommended by NICE, it cannot be made available on the NHS. The decision also shows the challenge for stretched health care systems to fund complex, novel medicines.
1 year 1 week ago
Pharma, Pharmalot, pharmalittle, STAT+
Sandals Foundation and Great Shape! Inc. Health Care Missions to include eye care services
The iCare clinics seek to serve at least 300 people per day with free eye exams, laser treatments for glaucoma, and free prescription glasses, reading glasses and sunglasses
1 year 1 week ago
Community, Health, PRESS RELEASE, Travel/Tourism, great shape inc, heidi clarke, icare clinic, sandals foundation
Biological clocks tick faster after losing loved ones - Study Finds
- Biological clocks tick faster after losing loved ones Study Finds
- Bereavement in early life may accelerate ageing, research shows The Guardian
- Loss of a loved one early in life may accelerate aging: Study The Hill
- Experiencing the death of a family member may age you faster Scimex
- Losing a Loved One May Speed Up Aging, Study Finds Columbia University's Mailman School of Public Health
1 year 1 week ago
En California, legisladores presionan para que inspectores de salud locales visiten instalaciones de inmigración
Brotes de covid-19, paperas y varicela. Agua contaminada, comida con moho y conductos de aire que despiden polvo negro.
Estas amenazas a la salud se han documentado dentro de las instalaciones de detención de inmigrantes administradas de manera privada en California a través de demandas, auditorías federales y estatales, y quejas presentadas por los mismos detenidos.
Brotes de covid-19, paperas y varicela. Agua contaminada, comida con moho y conductos de aire que despiden polvo negro.
Estas amenazas a la salud se han documentado dentro de las instalaciones de detención de inmigrantes administradas de manera privada en California a través de demandas, auditorías federales y estatales, y quejas presentadas por los mismos detenidos.
Pero los oficiales de salud pública locales que inspeccionan de manera rutinaria las cárceles del condado y las prisiones estatales dicen que no tienen autoridad bajo la ley estatal para inspeccionar los centros de detención operados por compañías privadas, incluidos los seis centros federales de inmigración en California.
La senadora estatal María Elena Durazo (demócrata de Los Ángeles) quiere zanjar esa laguna legal con una legislación que permitiría a los oficiales de salud de los condados realizar inspecciones en las instalaciones si lo considerasen necesario.
Durazo dijo que muchos detenidos viven en condiciones infrahumanas, y que las enfermedades contagiosas que se propagan en estas instalaciones podrían representar un riesgo para las comunidades circundantes.
“Desafortunadamente, a nuestros detenidos se los trata como si no fueran seres humanos”, dijo. “No queremos excusas. Queremos que los funcionarios estatales y de salud pública entren siempre que fuera necesario”.
No está claro cuánta autoridad tendrían los oficiales de salud locales para implementar cambios, pero expertos en salud pública dicen que podrían actuar como observadores independientes para documentar violaciones que de otro modo el público no conocería.
El Senado estatal aprobó el proyecto de ley, SB 1132, por unanimidad a finales de mayo. Ahora está bajo consideración en la Asamblea estatal.
La inmigración está regulada por el gobierno federal. GEO Group, el contratista privado de prisiones más grande del país, opera los centros federales de California, ubicados en cuatro condados. En conjunto, pueden albergar hasta 6,500 personas en espera de deportación o audiencias de inmigración.
Durante su campaña en 2020, el presidente Joe Biden prometió poner fin a la detención de inmigrantes con fines de lucro. Pero más del 90% de las aproximadamente 30,000 personas detenidas por la agencia de Inmigración y Control de Aduanas de Estados Unidos (ICE) en un día cualquiera permanecen en instalaciones privadas, según un análisis de 2023 de la Unión Americana de Libertades Civiles.
Miembros del Congreso en ambas cámaras han presentado legislaciones para eliminar gradualmente los centros de detención privados, mientras que otros legisladores, incluidos al menos dos en julio, han pedido investigaciones sobre la atención médica y de salud mental deficientes, y las muertes.
En 2023, legisladores en el estado de Washington aprobaron una ley para imponer supervisión estatal de las instalaciones de detención privadas, pero el GEO Group demandó, y la medida está atascada en los tribunales. Los legisladores de California han intentado repetidamente regular estas instalaciones, con resultados mixtos.
En 2019, el gobernador de California, el demócrata Gavin Newsom, firmó una medida que prohíbe que las prisiones y centros de detención privados operen en California. Pero luego un tribunal federal declaró la ley inconstitucional en lo que respecta a los centros de detención de inmigrantes, diciendo que interfería con las funciones federales.
En 2021, los legisladores estatales aprobaron un proyecto de ley que exige que los centros de detención privados cumplan con las órdenes de salud pública estatales y locales, y las regulaciones de seguridad y salud de los trabajadores.
Esa medida se adoptó en el apogeo de la pandemia de covid-19, cuando el virus arrasaba con las instalaciones de detención donde las personas estaban hacinadas en dormitorios sin, o con poca, protección contra los virus transmitidos por aire.
Por ejemplo, en el Centro de Detención de Otay Mesa, en San Diego, un brote al comienzo de la pandemia infectó a más de 300 miembros del personal y a detenidos.
La Asociación de Oficiales de Salud de California, que representa a los oficiales de salud pública de los 61 departamentos de salud locales del estado, apoya la legislación de Durazo.
“Estas investigaciones desempeñan un papel fundamental en la identificación y abordaje de preocupaciones de salud e higiene dentro de estas instalaciones, mitigando así los riesgos para los detenidos, el personal y las comunidades circundantes”, indica una carta de Kat DeBurgh, directora ejecutiva de la asociación.
Bajo la medida, los oficiales de salud pública determinarían si las instalaciones están cumpliendo con las reglas ambientales, como garantizar una ventilación adecuada, y ofrecer atención básica de salud mental y física, tratamiento de emergencia y alimentos preparados de manera segura.
A diferencia de las instalaciones correccionales públicas, que los oficiales de salud locales inspeccionan cada año, los centros de detención privados serían inspeccionados a necesidad, según lo determine el oficial de salud.
Christopher Ferreira, vocero de GEO Group, y Richard Beam, vocero de ICE, se negaron a comentar sobre la medida.
Georges Benjamin, director ejecutivo de la Asociación Americana de Salud Pública, dijo que los oficiales de salud pública están bien posicionados para inspeccionar estas instalaciones porque entienden cómo hacer que los espacios confinados sean más seguros para grandes poblaciones.
Aunque probablemente no puedan obligar a los centros de detención a cumplir con sus recomendaciones, sus informes podrían proporcionar información valiosa para los funcionarios públicos, abogados y otros que quieran explorar opciones como litigar, dijo. “Cuando el sistema no funciona, los tribunales pueden desempeñar un papel muy importante”, agregó Benjamin.
El sistema federal que monitorea la atención médica y la transmisión de enfermedades contagiosas dentro de los centros de detención de inmigrantes está roto, dijo Annette Dekker, profesora clínica asistente de medicina de emergencia en UCLA, que estudia la atención médica en estas instalaciones.
Tradicionalmente, personal del ICE realiza las inspecciones de los centros de detención y, hasta 2022, también un auditor privado.
En un artículo publicado en junio, Dekker y otros investigadores mostraron que los funcionarios de inmigración y el auditor realizaban inspecciones con poca frecuencia —al menos una vez cada tres años— y proporcionaban poca información pública sobre las deficiencias y cómo se abordaban.
“Hay mucho daño que está ocurriendo en los centros de detención que no podemos documentar”, dijo Dekker.
ICE y el GEO Group han sido objeto de demandas y cientos de quejas que alegan condiciones deficientes dentro de las instalaciones de California desde que comenzó la pandemia. Algunas de estas demandas están pendientes, pero una parte significativa de las quejas ha sido desestimada, según una base de datos mantenida por la Unión Americana de Libertades Civiles.
Las demandas más recientes de los detenidos alegan condiciones de hacinamiento e insalubridad, negación de atención médica y de salud mental adecuadas, negligencia médica y muerte por suicidio.
La División de Seguridad y Salud Ocupacional de California multó al GEO Group con unos $100,000 en 2022 por no mantener procedimientos escritos para reducir la exposición a covid. El GEO Group ha impugnado la multa.
“He experimentado condiciones de vida realmente inhumanas”, dijo Dilmer Lovos, de 28 años, a KFF Health News por teléfono desde el centro de detención de inmigración Golden State Annex en McFarland, en el condado de Kern. Lovos ha estado detenido allí desde enero mientras espera una audiencia de inmigración.
Lovos, quien nació en El Salvador y usa los pronombres ellos/ellas, ha sido residente permanente legal durante 15 años y fue detenido por oficiales de inmigración mientras estaba en libertad condicional.
A principios de julio, Lovos y otros 58 detenidos del Golden State Annex y el Centro de Procesamiento de ICE Mesa Verde, en Bakersfield, comenzaron una huelga de hambre y laboral exigiendo el fin de las malas condiciones de vida, el confinamiento solitario y los servicios médicos y de salud mental inadecuados.
Lovos describió una habitación abarrotada, filtros de aire obstruidos, ratones y cucarachas correteando en la cocina, agua goteando del techo y detenidos con síntomas parecidos a los de la gripe que no podían acceder a medicamentos ni a una prueba de covid cuando lo pedían.
Los protocolos del ICE requieren pruebas a los detenidos con síntomas al ingresar a las instalaciones sin hospitalizaciones ni muertes por covid en la semana anterior. En las instalaciones con dos o más hospitalizaciones o muertes en la semana anterior, se evalúa a todos los detenidos durante el proceso de admisión. Después de eso, depende de los proveedores médicos de cada instalación decidir cuándo es necesaria una prueba.
Después que Lovos presentara una queja ante el GEO Group en junio, alegando negligencia médica y de salud mental, dijeron que los pusieron en confinamiento solitario durante 20 días sin un inodoro que funcionara correctamente. “Olía mi orina y heces porque no podía tirar de la cadena”.
El vocero Ferreira se negó a abordar las acusaciones de Lovos pero dijo por correo electrónico que los detenidos reciben “acceso las 24 horas del día a atención médica”, incluidos médicos, dentistas, psicólogos y derivaciones a especialistas externos.
“GEO rechaza las acusaciones infundadas que se han hecho con respecto al acceso a los servicios de salud en los Centros de Procesamiento del ICE contratados por GEO”, dijo.
Una inspección sorpresa de funcionarios federales de inmigración en abril de 2023 encontró que los empleados de Golden State Annex no respondieron dentro de las 24 horas a las quejas médicas, lo que, según el informe, podría afectar negativamente la salud de los detenidos, y no archivaron de manera adecuada sus registros médicos.
Lovos dijo que nadie ha abordado sus preocupaciones y que las condiciones solo han empeorado.
“Por favor, vengan a revisar estos lugares”, dijo Lovos en una súplica a los oficiales de salud locales.
Esta historia fue producida por KFF Health News, una redacción nacional que produce periodismo en profundidad sobre temas de salud y es uno de los principales programas operativos de KFF, la fuente independiente de investigación de políticas de salud, encuestas y periodismo. KFF Health News edita California Healthline, un servicio editorialmente independiente de la California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 1 week ago
Noticias En Español, States, Immigrants, Latinos
Readers Weigh In on Abortion and Ways To Tackle the Opioid Crisis
Letters to the Editor is a periodic feature. We welcome all comments and will publish a selection. We edit for length and clarity and require full names.
Debunking Abortion Myths
Letters to the Editor is a periodic feature. We welcome all comments and will publish a selection. We edit for length and clarity and require full names.
Debunking Abortion Myths
I want to send a big THANK YOU to Matt Volz for writing a fact-checking article on the nonsense rhetoric around “abortion up until and after birth” that has run wild and unchallenged in the media (“GOP’s Tim Sheehy Revives Discredited Abortion Claims in Pivotal Senate Race,” July 9). Thanks for putting abortion later in pregnancy in context and debunking false assumptions.
I am a near-third-trimester abortion patient (nonviable pregnancy, terminated at 26 weeks), and I am so sick of hearing politicians like Tim Sheehy talk about something they have never experienced or bothered to learn about. It is as though I am watching the entire nation maliciously gossip about me and other parents like me. Those of us in the termination for medical reasons (TFMR) community have walked through hell only to have our voices, at best, be ignored or, more commonly, be insulted and threatened.
And I imagine watching this political circus is just as hurtful for parents who lost an infant shortly after birth and had to provide palliative care. That is who they are talking about with “abortion after birth”; they are talking about comfort care for infants who will not survive.
Thank you again for bringing a dose of reality to a conversation that never should have become political. These are impossible decisions that only parents should make. It was really refreshing to read Volz’s article and know that some journalists are still willing to fact-check the absurd claims floating around. It was encouraging to know that someone does see us.
— Anne Angus, Bozeman, Montana
A physician and Yale professor of radiology and biomedical imaging took to the social platform X to share feedback:
.@SenatorTester is a great Senator. And his opponent is a great liar. Both the GOP presidential candidate and Tim Sheehy have perpetuated this lie. Please push back every time you hear it. https://t.co/1LBGPgOA2u
— (((Howard Forman))) (@thehowie) July 9, 2024
— Howard Forman, New Haven, Connecticut
I just read your article at PolitiFact on Republican Senate candidate Tim Sheehy’s statement about abortion, and I would like to point out (what I believe) are a couple of errors.
1. In paragraph 10, you quote KFF’s Alina Salganicoff saying that “in the good-faith medical judgment of the treating health care provider, continuation of the pregnancy would pose a risk to the pregnant patient’s life or health.” Now, you may know that almost at the same time that the Roe v. Wade decision was released, there was a decision called Doe v. Bolton that interpreted “health” to mean almost anything. That broad interpretation of health is found in your article in paragraph 24: “Women have abortions later in pregnancy either because they find out new information or because of economic or political barriers,” [Katrina] Kimport said.
When a woman can have an abortion after viability because she offers any reason that can be interpreted as “health,” then abortion would be legal throughout all nine months of pregnancy. I believe that you are wrong in your interpretation. Democrats do not want to name any restriction on abortion during all nine months, and every mention of “health” is a fig leaf that does not restrict abortion at all. Every abortion advocate knows that.
2. Whether late-term abortions are rare or not is logically irrelevant to whether late-term abortions should be restricted.
Why don’t you know these things?
— Darryl A. Linde, Tahlequah, Oklahoma
An Air Force veteran added his two cents on X:
Dems have the facts. Republicans spread fear and lies.https://t.co/6CWfKhqxJZ
— James Knight (@jamesUSAF_vet) July 12, 2024
— James Knight, Reno, Nevada
Making a Healthy Difference for the Homeless
Thank you for printing this story (“A California Medical Group Treats Only Homeless Patients — And Makes Money Doing It,” July 19). It really piqued my interest and portrayed a positive solution for getting care to the people.
Up here in the Bay Area, I believe there are a couple of groups who go out and find what needs doing instead of waiting for people to come to them — but nothing like this. Makes me curious about what we actually have going on here.
— Laurie Lippe, El Cerrito, California
A self-described “nurse turned health tech nerd” commended the effort on X:
"They distribute GPS devices so they can track their homeless patients. They keep company credit cards on hand in case a patient needs emergency food or water, or an Uber ride to the doctor"This is healthcare at its best 💕https://t.co/UhM1dgTPH7
— Rik Renard (@rikrenard) July 22, 2024
— Rik Renard, New York City
A senior policy director at the National Health Care for the Homeless Council shared the post on X — while stressing that her tweets reflected her own opinions and not those of her organization:
I’m with @DrJimWithers: “I do worry about the corporatization of street medicine and capitalism invading what we’ve been building, largely as a social justice mission outside of the traditional health care system.” https://t.co/IOjazvrvqP
— Barbara DiPietro (@BarbaraDiPietro) July 19, 2024
— Barbara DiPietro, Baltimore
On X, a physician who says she champions “physicians, patients, public health, and the patient-physician relationship” reacted to our coverage surrounding the Federal Trade Commission’s rule banning the use of noncompete agreements in employment contracts:
FTC #noncompete crackdown may not protect doctors and nurses at ~64% of US community hospitals that are tax-exempt nonprofits or government-owned.But, @FTC said some nonprofits could be bound by the rule if they do not operate as true charities. https://t.co/9fDbfVflTH
— Marilyn Heine (@MarilynHeineMD) May 28, 2024
— Marilyn Heine, Langhorne, Pennsylvania
Without a Noncompete Ban on All Employers, Rural Access to Care Suffers
When news broke that the Federal Trade Commission would be banning noncompete agreements in employment contracts, many of us in the medical profession celebrated. However, until nonprofit hospitals and health care facilities benefit from the same ban, access to care — particularly in rural regions — will suffer.
As reported in “Health Worker for a Nonprofit? The New Ban on Noncompete Contracts May Not Help You” (June 5), about two-thirds of U.S. community hospitals are nonprofit or government-owned. This means that most hospitals nationwide may continue to enforce noncompete agreements among their employees, a practice that will have an outsize impact on rural medical professionals.
As a rheumatologist in a rural area, I’ve seen how detrimental limited access to care is for patients. Noncompete agreements serve only to further limit access to much-needed care. Due to the physician shortage being particularly acute in rural America, there are oftentimes only a few specialty physicians servicing a large region. Suppose one of these specialists is employed by a large health system and wants to transition to a private practice. It reduces the number of accessible specialists in the area when their noncompete agreement prohibits them from practicing near any of the health care facilities associated with the system. And increasing consolidation across health care means many rural regions may have only a single health system that operates across the entire state and surrounding areas. A geographically limiting noncompete agreement essentially stops a physician or medical professional from practicing entirely in the area, or they must uproot their life and move away from the major health system.
I hope the FTC takes further action to include nonprofit health care employers in its noncompete ban. I also urge nonprofit employers to consider their rural patients’ access to care when requiring providers to sign noncompete agreements. It’s in the best interest of our patient’s health to get rid of these agreements entirely.
— Chris Phillips, chair of the American College of Rheumatology’s Committee on Rheumatologic Care, Paducah, Kentucky
The president of the Texas Medical Board also posted on X with feedback:
Is it a coincidence that this affects everyone, except those who work for nonprofit hospitals and health care facilities, which employs the largest number of medical professionals?The FTC and it's selective enforcement and rules is blatantly obvious! https://t.co/RzXInqiJ8D
— Sherif Zaafran, MD (@szaafran) June 16, 2024
— Sherif Zaafran, Houston
Repurposing Newspaper Boxes for Public Health
I recently read your article by Mara Silvers regarding the state’s intended use of public health vending machines (PHVMs) to help fight the opioid overdose epidemic (“Montana’s Plan To Curb Opioid Overdoses Includes Vending Machines,” July 18). Working on the covid-19 response for almost four years now, and with our American Rescue Plan Act funding coming to an end, we recently used a byline in our equipment budget to purchase and place “resource kiosks” in the community.
In 2022, after researching the use of vending machines for test distribution, we discovered vending machines have high barrier-to-entry costs and high maintenance costs. And even if purchasing isn’t possible, rental contracts come with high fees. We decided it was better to use a lower-cost resource that could be purchased in greater quantity, easily placed with community partners, and required no maintenance: the refurbished newspaper kiosk.
We decided to purchase double-decker boxes, which have a secondary door, creating another shelf, for roughly $410 apiece and stocked them with covid tests, nasal naloxone, injectable naloxone, fentanyl test strips, xylazine test strips, various types of condoms, and lubrication packets. We are in the process of securing a supply of gun locks and adding links to our pilot landing page for individual free gun lock deliveries, as well as links for free sexually transmitted infection test kits. We have investigated providing dental supplies and other items, but long-term funding is a constant concern. Grant money for most programs (likely all ARPA dollars) is running out, so the viability of these types of pilot programs is tentative without a buy-in from state or federal agencies.
Mara’s article hinted at criteria for possible placements and, similarly, we didn’t use locational overdose data, which can be “othering” to communities, but instead placed these kiosks with community partners that have been accomplished supporters of their at-risk populations throughout the covid response. Each community partner helped protect the communities they served through increased access to resources and provided information as trusted messengers. Truly meeting people where they are.
While money quickly appeared to fight the covid pandemic, and states spirited away dollars for pet projects, that sea of funding has dried up, and there doesn’t seem to be a plan for any continued funding. Covid-related functions have all been folded back into communicable disease epidemiology programs, which were already underfunded; in our state, the money funding the naloxone bulk fund is also drying up. Covid deaths might be down, but there is always a new bug (H5N1), STI infections are up, and gun-related deaths grow year over year. Funding population-level health interventions is our next pandemic.
With enough funding, kiosk-sized PHVMs could be swiftly added to any public health agency’s or community program’s quiver of tools to help increase access to resources and information for the most vulnerable residents.
Thank you for publishing a great article about the emerging opportunities to respond to changing public health needs!
— Christopher Howk, Arapahoe County Public Health’s covid-19 testing and logistics coordinator, Greenwood Village, Colorado
A retiree with a PhD in quantum chemistry tweeted his surprise over the news:
Montana’s Plan To Curb Opioid Overdoses Includes Vending Machineshttps://t.co/kNxYjnIOEO(What???!! Vending machines for opioids?)
— John Lounsbury (@jlounsbury59) July 18, 2024
— John Lounsbury, Lake Frederick, Virginia
Misappropriation of Opioid Settlement Funds
OK, so I see how all these states got all these lump sums of money for people like us who became addicted and whose lives were devastated by Purdue Pharma, Vicodin, and all the pharmacies (“Lifesaving Drugs and Police Projects Mark First Use of Opioid Settlement Cash in California,” July 12). How come all these states got all the money but those of us who have suffered have to wait, hire lawyers, and wait years for the money that was just handed over to these states? We’re the ones whose lives were devastated. My son was hooked, I was hooked, and my wife, and yet we must sit here penniless after the addiction, while all these states take the money — and they don’t do what they’re supposed to with it, and everyone knows it.
— Michael Stewart, Des Moines, Iowa
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 1 week ago
Health Industry, Public Health, Rural Health, Abortion, Homeless, Letter To The Editor, Misinformation, Opioids, Substance Misuse, Women's Health
Q&A: CDC issues warning amid surge in dengue virus
In March, Puerto Rico declared a public health emergency after recording 549 cases of dengue virus since the start of 2024.
The number rose to more than 1,900 cases as of July 24, according to the CDC.In June, the CDC issued a health alert about an increased risk of dengue infection in the United States, noting that the global incidence of the mosquito-borne disease in 2024 is the highest on record at this point of the year.According to the Pan American Health Organization, there have been more than 10.7 million suspected cases of dengue in the Americas this year as of July 25 — a 233%
1 year 1 week ago
“Cuida tu Salud Mental” contact center extends service hours
Santo Domingo.- In a commitment to enhance mental health services and improve quality of life, Minister of Health Víctor Atallah, in coordination with First Lady Raquel Arbaje, announced the extended operating hours of the “Cuida tu Salud Mental” Contact Center.
Santo Domingo.- In a commitment to enhance mental health services and improve quality of life, Minister of Health Víctor Atallah, in coordination with First Lady Raquel Arbaje, announced the extended operating hours of the “Cuida tu Salud Mental” Contact Center.
Starting September 1, the center will be open from 8 AM to midnight, including weekends, to provide greater support for those in need. To support this expansion, additional healthcare staff will be hired to ensure the availability of more professionals offering psychological counseling and support.
The center can be reached at 809-200-1400 for consultations with trained behavioral health specialists. This initiative aims to improve access to mental health services nationwide.
Minister Atallah reaffirmed his commitment to transforming mental health services during a visit to the Padre Billini Psychosocial Rehabilitation Center and meetings with the Society of Psychiatry and the Dominican College of Psychologists.
The Ministry of Health is also updating protocols for managing depressive disorders in adults, substance use in children and adolescents, and autism spectrum disorders (ASD) in minors. Technical committees composed of various institutions and specialists are overseeing these updates.
Additionally, efforts are underway to update the National Mental Health Plan and Mental Health Law 12-06, with support from the Pan American Health Organization (PAHO) and other institutions, ensuring policies align with international best practices and local needs.
Strategic guidelines for suicide prevention are being developed, reviewed by technical committees and specialized consultancies, and will be implemented through decentralized units, including provincial, municipal, and health area offices.
The Ministry is also preparing a mental health bulletin and a study to characterize homeless individuals, aiming to provide updated information for decision-making and the implementation of appropriate intervention strategies.
1 year 1 week ago
Health, Local
Acalabrutinib regimens improve PFS vs. standard care in untreated CLL
Fixed-duration acalabrutinib plus venetoclax, with or without obinutuzumab, improved survival compared with standard chemoimmunotherapy for certain adults with leukemia, according to a topline data announcement.The randomized phase 3 AMPLIFY trial included adults with previously untreated chronic lymphocytic leukemia without deletion 17p or TP53 mutations.Researchers randomly assigned patients
half of the patients to acalabrutinib (Calquence, AstraZeneca) plus venetoclax (Venclexta, AbbVie), with or without obinutuzumab (Gazyva, Genentech). The other half received investigator’s choice
1 year 1 week ago
PAHO/WHO | Pan American Health Organization
New initiative launched to advance mRNA vaccine development against human avian influenza (H5N1)
New initiative launched to advance mRNA vaccine development against human avian influenza (H5N1)
Cristina Mitchell
29 Jul 2024
New initiative launched to advance mRNA vaccine development against human avian influenza (H5N1)
Cristina Mitchell
29 Jul 2024
1 year 1 week ago
Why Many Nonprofit (Wink, Wink) Hospitals Are Rolling in Money
One owns a for-profit insurer, a venture capital company, and for-profit hospitals in Italy and Kazakhstan; it has just acquired its fourth
One owns a for-profit insurer, a venture capital company, and for-profit hospitals in Italy and Kazakhstan; it has just acquired its fourth for-profit hospital in Ireland. Another owns one of the largest for-profit hospitals in London, is partnering to build a massive training facility for a professional basketball team, and has launched and financed 80 for-profit start-ups. Another partners with a wellness spa where rooms cost $4,000 a night and co-invests with “leading private equity firms.”
Do these sound like charities?
These diversified businesses are, in fact, some of the country’s largest nonprofit hospital systems. And they have somehow managed to keep myriad for-profit enterprises under their nonprofit umbrella — a status that means they pay little or no taxes, float bonds at preferred rates, and gain numerous other financial advantages.
Through legal maneuvering, regulatory neglect, and a large dollop of lobbying, they have remained tax-exempt charities, classified as 501(c)(3)s.
“Hospitals are some of the biggest businesses in the U.S. — nonprofit in name only,” said Martin Gaynor, an economics and public policy professor at Carnegie Mellon University. “They realized they could own for-profit businesses and keep their not-for-profit status. So the parking lot is for-profit; the laundry service is for-profit; they open up for-profit entities in other countries that are expressly for making money. Great work if you can get it.”
Many universities’ most robust income streams come from their technically nonprofit hospitals. At Stanford University, 62% of operating revenue in fiscal 2023 was from health services; at the University of Chicago, patient services brought in 49% of operating revenue in fiscal 2022.
To be sure, many hospitals’ major source of income is still likely to be pricey patient care. Because they are nonprofit and therefore, by definition, can’t show that thing called “profit,” excess earnings are called “operating surpluses.” Meanwhile, some nonprofit hospitals, particularly in rural areas and inner cities, struggle to stay afloat because they depend heavily on lower payments from Medicaid and Medicare and have no alternative income streams.
But investments are making “a bigger and bigger difference” in the bottom line of many big systems, said Ge Bai, a professor of health care accounting at the Johns Hopkins University Bloomberg School of Public Health. Investment income helped Cleveland Clinic overcome the deficit incurred during the pandemic.
When many U.S. hospitals were founded over the past two centuries, mostly by religious groups, they were accorded nonprofit status for doling out free care during an era in which fewer people had insurance and bills were modest. The institutions operated on razor-thin margins. But as more Americans gained insurance and medical treatments became more effective — and more expensive — there was money to be made.
Not-for-profit hospitals merged with one another, pursuing economies of scale, like joint purchasing of linens and surgical supplies. Then, in this century, they also began acquiring parts of the health care systems that had long been for-profit, such as doctors’ groups, as well as imaging and surgery centers. That raised some legal eyebrows — how could a nonprofit simply acquire a for-profit? — but regulators and the IRS let it ride.
And in recent years, partnerships with, and ownership of, profit-making ventures have strayed further and further afield from the purported charitable health care mission in their community.
“When I first encountered it, I was dumbfounded — I said, ‘This not charitable,’” said Michael West, an attorney and senior vice president of the New York Council of Nonprofits. “I’ve long questioned why these institutions get away with it. I just don’t see how it’s compliant with the IRS tax code.” West also pointed out that they don’t act like charities: “I mean, everyone knows someone with an outstanding $15,000 bill they can’t pay.”
Hospitals get their tax breaks for providing “charity care and community benefit.” But how much charity care is enough and, more important, what sort of activities count as “community benefit” and how to value them? IRS guidance released this year remains fuzzy on the issue.
Academics who study the subject have consistently found the value of many hospitals’ good work pales in comparison with the value of their tax breaks. Studies have shown that generally nonprofit and for-profit hospitals spend about the same portion of their expenses on the charity care component.
Here are some things listed as “community benefit” on hospital systems’ 990 tax forms: creating jobs; building energy-efficient facilities; hiring minority- or women-owned contractors; upgrading parks with lighting and comfortable seating; creating healing gardens and spas for patients.
All good works, to be sure, but health care?
What’s more, to justify engaging in for-profit business while maintaining their not-for-profit status, hospitals must connect the business revenue to that mission. Otherwise, they pay an unrelated business income tax.
“Their CEOs — many from the corporate world — spout drivel and turn somersaults to make the case,” said Lawton Burns, a management professor at the University of Pennsylvania’s Wharton School. “They do a lot of profitable stuff — they’re very clever and entrepreneurial.”
The truth is that a number of not-for-profit hospitals have become wealthy diversified business organizations. The most visible manifestation of that is outsize executive compensation at many of the country’s big health systems. Seven of the 10 most highly paid nonprofit CEOs in the United States run hospitals and are paid millions, sometimes tens of millions, of dollars annually. The CEOs of the Gates and Ford foundations make far less, just a bit over $1 million.
When challenged about the generous pay packages — as they often are — hospitals respond that running a hospital is a complicated business, that pharmaceutical and insurance execs make much more. Also, board compensation committees determine the payout, considering salaries at comparable institutions as well as the hospital’s financial performance.
One obvious reason for the regulatory tolerance is that hospital systems are major employers — the largest in many states (including Massachusetts, Pennsylvania, Minnesota, Arizona, and Delaware). They are big-time lobbying forces and major donors in Washington and in state capitals.
But some patients have had enough: In a suit brought by a local school board, a judge last year declared that four Pennsylvania hospitals in the Tower Health system had to pay property taxes because its executive pay was “eye popping” and it demonstrated “profit motives through actions such as charging management fees from its hospitals.”
A 2020 Government Accountability Office report chided the IRS for its lack of vigilance in reviewing nonprofit hospitals’ community benefit and recommended ways to “improve IRS oversight.” A follow-up GAO report to Congress in 2023 said, “IRS officials told us that the agency had not revoked a hospital’s tax-exempt status for failing to provide sufficient community benefits in the previous 10 years” and recommended that Congress lay out more specific standards. The IRS declined to comment for this column.
Attorneys general, who regulate charity at the state level, could also get involved. But, in practice, “there is zero accountability,” West said. “Most nonprofits live in fear of the AG. Not hospitals.”
Today’s big hospital systems do miraculous, lifesaving stuff. But they are not channeling Mother Teresa. Maybe it’s time to end the community benefit charade for those that exploit it, and have these big businesses pay at least some tax. Communities could then use those dollars in ways that directly benefit residents’ health.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 2 weeks ago
Health Care Costs, Health Care Reform, Health Industry, Hospitals
Health – Demerara Waves Online News- Guyana
Former West Indies Guyanese cricket captain asks CARICOM to focus on prostate cancer
Former West Indies cricket captain, Sir Clive Lloyd on Sunday appealed to Caribbean Community (CARICOM) leaders to focus on combatting prostate cancer. Speaking at his investiture with the Order of the Caribbean Community (OCC) award that coincided with the opening of the summit of regional leaders in Grenada, Sir Clive hoped that the same emphasis ...
Former West Indies cricket captain, Sir Clive Lloyd on Sunday appealed to Caribbean Community (CARICOM) leaders to focus on combatting prostate cancer. Speaking at his investiture with the Order of the Caribbean Community (OCC) award that coincided with the opening of the summit of regional leaders in Grenada, Sir Clive hoped that the same emphasis ...
1 year 2 weeks ago
Health, News, appeal, Caribbean Community (CARICOM), investiture, Order of the Caribbean Community (OCC), prostate cancer, Sir Clive Lloyd
Deyalsingh: Six-20 age group most vulnerable to dengue - TT Newsday
- Deyalsingh: Six-20 age group most vulnerable to dengue TT Newsday
- Don’t invite dengue home Trinidad & Tobago Express Newspapers
- Trinidad and Tobago reports sudden surge in dengue cases Caribbean News Now!
- Trinidad records five dengue-related deaths Jamaica Observer
- Health Ministry reports 5th dengue death TT Newsday
1 year 2 weeks ago
SINAVE reports 8,484 suspected cases of dengue fever
Santo Domingo – The Epidemiological Surveillance System (SINAVE) reports that as of week 27, 8,484 dengue cases had been registered, and nine deaths had been reported.
However, it states that as of week 27, only 941 cases and nine deaths have been confirmed in the Dominican Republic.
Santo Domingo – The Epidemiological Surveillance System (SINAVE) reports that as of week 27, 8,484 dengue cases had been registered, and nine deaths had been reported.
However, it states that as of week 27, only 941 cases and nine deaths have been confirmed in the Dominican Republic.
The provinces with the highest incidence of cases are Santiago (255), Puerto Plata (133), and Duarte (99). The official data for cases can be verified.
The most affected sex is males between the ages of 10 and 19. Six cases were reported last week.
Dengue is transmitted through the bite of an infected mosquito. It is a disease that affects people of all ages, with symptoms ranging from a mild fever to an incapacitating fever, accompanied by intense headache, pain behind the eyes, muscle and joint pain, and erythema.
Malaria
The total number of suspected malaria cases under investigation is 28,007.
Malaria is an acute febrile illness caused by parasites of the Plasmodium genus that are spread to people through the bite of mosquitoes of the Anopheles genus. It is a preventable and curable disease. According to Epidemiology, it is not contagious and cannot be transmitted from one person to another. National data establish that for week 27 of this year -2024, 618 suspected malaria cases were reported, of which 9 cases were confirmed, eight male and one female, within the age group of 10 to 19 years old. These cases correspond to the active outbreaks in the provinces of San Juan, with eight cases, and Azua, with one case.
Covid-19 cases
In the last week, 159 cases of COVID-19 were reported, and as of week 27, 636 cases have been confirmed.
Leptospirosis
In the Dominican Republic, up to week 27, 323 probable cases of leptospirosis were reported; this represents an increase of 318% in the variation of the rate compared to 2023, when it was 154%.
The provinces with the highest incidence are Santo Domingo (55), Monte Cristi (43), Santiago (28) and Distrito Nacional with 15 cases.
The most affected sex is male, within the age group of 20 to 29 years old.
The Epidemiology Department keeps up to date with its weekly bulletins.
1 year 2 weeks ago
Health, Local
Maternal mortality figures in the official spotlight; dengue fever
Santo Domingo – During one week, week 28, the Epidemiological Surveillance System recorded three maternal deaths from three provinces. Their ages ranged from 21 to 29 years old.
Santo Domingo – During one week, week 28, the Epidemiological Surveillance System recorded three maternal deaths from three provinces. Their ages ranged from 21 to 29 years old.
Nine deaths remain from dengue. The system indicates that as of the 28th epidemiological week of the year 2024, 135 suspected cases and 16 confirmed cases have been registered. Dengue is a disease transmitted by the bite of the Aedes aegypti mosquito. It is notifiable.
Maternal mortality
The three maternal deaths came from the Peravia, Espaillat, and Monte Cristi provinces.
The health centers that reported cases were Maternidad Nuestra Señora La Altagracia, Centro Médico Guadalupe, and Clínica Unión Médica del Norte.
Sixty-seven percent or two out of three cases reported this epidemiological week, are of Dominican nationality.
The accumulated number of maternal deaths up to week 28 is 88 deaths, involving women between 17 and 44 years of age who resided in the Metropolitan region with 34 deaths, North Cibao, 15, East 15, Valdesia, eight, El Valle, five, Enriquillo, three, Northeast Cibao, three, Western Cibao, three and Central Cibao, two.
Of the 88 deaths reported, 45%, or 40 out of the 88 deaths, were Haitian women in labor.
Concern
Maternal and neonatal mortality remains a major concern, with many preventable deaths that have not decreased significantly in recent years. The World Health Organization stresses the importance of adequate maternal care for short- and long-term well-being. Although there has been progress, challenges persist.
Dengue fever
To date, 8,602 suspected cases of dengue have been reported.
The last week, 13.3%, or 18 of the 135 cases reported in the last week are concentrated in Hermanas Mirabal, 12.6%, or 17 of 135 in Duarte province and 10.4%, involving 14 of 135) in Santiago province. The cumulative incidence is 17.05 per 100,000 inhabitants, the province with the highest cumulative incidence is Hermanas Mirabal with 655.16 suspected cases per 100,000 inhabitants. A total of 8,602 suspected cases of febrile illness have been reported. Of the total number of suspected cases. Fifty-three percent of the suspected cases (4,523 out of 8,602) were male and affected the 10-19-year-old age group.
A total of 83.2% of the cases received care in a health facility, with 54% showing alarm signs and 45% without. Up to week 28, 4,475 dengue tests have been processed at the National Public Health Reference Laboratory.
This is a communicable disease indicator that is monitored by the authorities. Notification is mandatory.
1 year 2 weeks ago
Health, Local