CDC warns of mosquito-driven virus as cases spike
The Centers for Disease Control and Prevention has issued a fresh warning about an increased risk of dengue virus infections as a "record-breaking number" of cases are being reported in the Americas.
The Centers for Disease Control and Prevention has issued a fresh warning about an increased risk of dengue virus infections as a "record-breaking number" of cases are being reported in the Americas.
From January 1 to June 24 of this year, more than 9.7 million dengue cases were recorded among countries in the Americas, which is more than double the 4.6 million infections recorded throughout 2023, according to the CDC.
"Global incidence of dengue in 2024 has been the highest on record for this calendar year; many countries are reporting higher-than-usual dengue case numbers," it also said. "In 2024, countries in the Americas have reported a record-breaking number of dengue cases, exceeding the highest number ever recorded in a single year."
The CDC describes the dengue virus as the "most common" mosquito-borne disease in the world. In the U.S., Florida has reported the most cases so far this year with 197, followed by New York with 134, Massachusetts with 50 and California with 40.
TIGER MOSQUITOES BLAMED FOR SPREAD OF DENGUE FEVER
"Six U.S. territories and freely associated states are classified as areas with frequent or continuous dengue transmission: Puerto Rico, American Samoa, the U.S. Virgin Islands, the Federated States of Micronesia, the Republic of Marshall Islands, and the Republic of Palau," the CDC adds.
The health agency says one in every four dengue infections are symptomatic, with effects including fever and "nausea, vomiting, rash, muscle aches, joint pain, bone pain, pain behind the eyes, headache, or low white blood cell counts."
"Severe disease, with associated severe bleeding, shock or respiratory distress caused by plasma leakage, or end-organ impairment, develops in 1 in 20 people with symptomatic dengue," according to the CDC.
PUERTO RICO HEALTH OFFICIALS DECLARE DENGUE FEVER A PUBLIC HEALTH EMERGENCY
It said infants under the age of one, pregnant women and adults over the age of 65 carry an "increased risk of severe dengue" and that "transmission peaks during the warmer and wetter months in many tropical and subtropical regions."
There is not currently a medication to treat dengue, the CDC says.
Infected people are advised to rest, take acetaminophen for pain and fever, stay hydrated and see a doctor.
Fox News’ Melissa Rudy contributed to this report.
1 year 1 month ago
infectious-disease, americas, california, new-york, Florida, Massachusetts, Health
Health Archives - Barbados Today
Gibbs frustrated at lack of action to improve safety at 60-year-old QEH
One of the nation’s most respected structural engineers has sounded the alarm over fire and structural safety at the island’s sole general hospital, warning that lives could be lost if a blaze were to break out on any of the wards.
Tony Gibbs, who conducted a vulnerability study of the Queen Elizabeth Hospital (QEH) in 1998, told Barbados TODAY that the hospital remains insufficiently safe, particularly regarding fire protection and roofing and suspended floor slabs.
But the QEH top brass countered that a recent PAHO Safe Hospital study index gave the state-owned healthcare facility a B rating.
“The index is the result of an all-encompassing study, which includes a review of fire potential and fire protection systems,” Chief Executive Officer Neil Clark told Barbados TODAY.
The 600-bed Martindale’s Road facility, which replaced the General Hospital after 120 years, marks its 60th anniversary in November.
Gibbs revealed that his 1998 study had proposed short-term measures to be implemented within 12 months, at an estimated cost of $1 million.
“They did nothing,” he said, expressing frustration at the lack of action. “The short-term measures would have cost in 1998, $1 million; not more than that.”
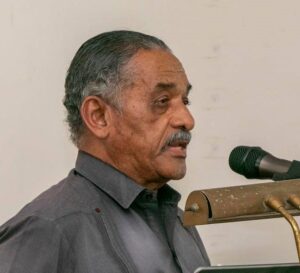
Respected Structural Engineer Tony Gibbs. (FP)
Gibbs, 86, who was awarded the Companion of Honour in 2020 for his contributions to engineering in Barbados and the Caribbean, said that while some structural changes have been made since the hospital’s opening, most of the building remains in its original state.
“The focus of the study was a vulnerability analysis to see how safe the building is. It is not safe enough,” Gibbs stated.
He explained that while the steel frame is protected and would not collapse in a fire, major safety issues persist with the floors.
The engineer highlighted concerns about the SB slabs, made from Barbados clay, steel and concrete, which were popularly used when the hospital was built.
“That floor system is all over the Queen Elizabeth Hospital. There have been failures there. There have been failures there even in recent times,” he said, noting that these involve clay blocks spontaneously breaking and falling.
“So, I have written about that in 1998, and nothing has been done about it. They still have those SB blocks on the floors of the QEH.”
Gibbs cited similar failures in other Barbadian buildings, including banks, schools and warehouses. He recounted a particularly alarming incident at Victoria Hospital in Saint Lucia where roof slabs failed in a paediatric ward shortly after it had been evacuated due to plumbing issues.
The structural expert also pointed out fire safety deficiencies at the QEH, including a lack of fire doors for compartmentalisation and an absence of sprinklers on the wards.
“I think people will die if there is a fire in that hospital,” he warned. “But things can be done about it.”
Gibbs, who designed the Tom Adams Financial Centre housing the Central Bank of Barbados, noted that while the original 1964 structure forms the bulk of the QEH, there have been some additions.
“There have been some additions since then which probably are as good as the 1964 building,” he noted, referring to newer sections like the Lions Eye Care Centre and an extension on the western side.
But these additions do little to reduce the overall fire risk, according to the engineer.
He stressed that modern hospital design standards emphasise building facilities that eliminate the need for evacuation during fires.
This is typically achieved through a combination of sprinklers, compartmentalisation, and careful selection of construction materials.
“The Queen Elizabeth Hospital needs some work done for fire protection. The wards are not separated with fire doors, so you can’t compartmentalise the Queen Elizabeth Hospital,” Gibbs explained.
“We can reasonably be talking about installing sprinklers which would be expensive, but not as expensive as human lives. And we could compartmentalise it. You could do horizontal evacuation from the area which is on fire to another part of the same floor which is not on fire.”
Drawing on his extensive experience assessing Caribbean hospitals for the Pan American Health Organisation (PAHO), Gibbs expressed surprise that even newer hospitals in the region, such as the Mount St John’s Medical Centre in Antigua, have incorporated necessary fire safety features like fire-rated doors, smoke detectors and sprinkler systems.
“So, even a Third World country can do it; must do it,” he said.
But while the QEH’s Chief Executive said management accepted that the hospital’s infrastructure is dated, he drew attention to the PAHO study and other mitigating measures to improve safety at the medical facility.
“It is important to note that the Pan-American Health Organisation conducts periodic assessments on hospitals regionally and in September 2023, the agency conducted its Safe and Green Assessment at the QEH,” Clark said.
“From this most recent assessment, PAHO’s Safe Hospital Index rating for the QEH is a B.
“In addition to this, the QEH routinely conducts inspection and maintenance programmes, and simulation exercises to test the hospitals preparedness and response to incidents that may arise as a consequence of the facilities’ age.”
The hospital boss, who has been on the job since March, stated that almost a year ago, the QEH’s fire response mechanisms were tested and its teams, with assistance from the Barbados Fire Service, were able to contain the situation.
Clark also suggested that the concerns highlighted by structural engineer Gibbs could also be resolved by building a new hospital.
“While these mitigation measures and contingencies have been established across the QEH to protect patients and staff, there is acknowledgement from management that a new hospital with modern design would also address the concerns raised by Mr Gibbs,” the CEO declared.
emmanueljoseph@barbadostoday.bb
The post Gibbs frustrated at lack of action to improve safety at 60-year-old QEH appeared first on Barbados Today.
1 year 1 month ago
Health, Local News
Climate change and the critical impact on Jamaica’s public health system
AMID RISING concerns over the effects of climate change on small island developing states (SIDS), key stakeholders convened to address the critical impact on Jamaica’s public health system at the Health National Adaptation Plan (HNAP) Stakeholder...
AMID RISING concerns over the effects of climate change on small island developing states (SIDS), key stakeholders convened to address the critical impact on Jamaica’s public health system at the Health National Adaptation Plan (HNAP) Stakeholder...
1 year 1 month ago
The weight loss backsliding challenge
WHILE ACHIEVING weight loss is an important goal for millions of people across the globe, an equally if not more difficult challenge is to retain the weight lost over a long period of time. Weight loss backsliding, that is, regaining lost weight,...
WHILE ACHIEVING weight loss is an important goal for millions of people across the globe, an equally if not more difficult challenge is to retain the weight lost over a long period of time. Weight loss backsliding, that is, regaining lost weight,...
1 year 1 month ago
Dual-target CAR-T allows researcher to ‘dream big’ about a cure for high-risk leukemia
Jae Park, MD, compared the moment to a baby being born.The first infusion of a phase 1 study using a novel chimeric antigen receptor T-cell therapy for patients with relapsed or refractory acute myeloid leukemia is about to happen and Park could feel his anticipation building.“It’s mixed feelings.
It’s certainly the excitement, obviously — kind of nervous, too,” Park, chief of the cellular therapy service and a hematologist/oncologist specializing in leukemia at Memorial Sloan Kettering Cancer Center, told Healio that morning. “It’s finally happening
1 year 1 month ago
Saharan dust arrives in Dominican Republic
Santo Domingo.- Meteorologist Jean Suriel announced via social media that a Saharan dust cloud will arrive in the Dominican Republic on Tuesday afternoon. He indicated that precipitation will primarily affect areas in the northwest, north, and Central Mountain Range, with showers expected in the northeast, south, and southeast between 5 and 8 PM.
Santo Domingo.- Meteorologist Jean Suriel announced via social media that a Saharan dust cloud will arrive in the Dominican Republic on Tuesday afternoon. He indicated that precipitation will primarily affect areas in the northwest, north, and Central Mountain Range, with showers expected in the northeast, south, and southeast between 5 and 8 PM. Additionally, Wave number 12 will traverse the Caribbean Sea.
Suriel cautioned individuals allergic to Saharan dust particles to take preventive measures due to the heightened risk of allergic reactions.
Looking ahead to Wednesday, he forecasted a very hazy sky and hot conditions due to the Saharan cloud. Remnants of the wave may lead to scattered rains in the northeast, northwest, mountainous regions, and the south.
By Thursday, the intensity of the Saharan dust is expected to diminish slightly, although it will still contribute to respiratory allergies and oppressive heat. Increased precipitation is anticipated in the Cibao and mountainous areas.
Moving into Friday and Saturday, Suriel predicted reduced Saharan dust levels and the arrival of Tropical Wave number 14, which could bring extended periods of rain and raise the potential for localized flooding.
He concluded that on Sunday, remnants of the tropical wave will likely continue to bring moderate to heavy rainfall across the Dominican Republic.
1 year 1 month ago
Health
PAHO/WHO | Pan American Health Organization
Over 3 million annual deaths due to alcohol and drug use, majority among men
Over 3 million annual deaths due to alcohol and drug use, majority among men
Cristina Mitchell
25 Jun 2024
Over 3 million annual deaths due to alcohol and drug use, majority among men
Cristina Mitchell
25 Jun 2024
1 year 1 month ago
Health Archives - Barbados Today
Gastro cases on the rise
Gastrointestinal illness has increased in adults and children since late April, and health officials have identified a new virus cause among lab samples – rotavirus.
The Ministry of Health and Wellness reported on Monday that for the diarrhoeal samples tested, three samples from late May and early June showed the presence of rotavirus, in addition to the bacterial foodborne pathogens that have been previously identified.
The uptick in cases in persons older than five years moved from 34 at the end of April, to 76 cases in the week ending May 11. Since then, weekly numbers have been falling, most recently to 46 cases in the week ending June 15, but are still above the alert threshold. At this time of the year, the alert level for this age group is fewer than eight cases.
In children under five years old, the number of cases moved from eight for the week ending April 27, to 27 cases in the week ending May 18.
Rotavirus is a very contagious agent spread by contact with objects or persons contaminated with infected stool. Vomiting was a prominent symptom for many persons, according to health authorities.
Members of the public are urged to employ proper hand hygiene methods such as washing their hands regularly, especially before eating, and to continue to be cautious when purchasing ready-to-eat food items.
(BGIS)
The post Gastro cases on the rise appeared first on Barbados Today.
1 year 1 month ago
Health, Local News
Celiac disease: Hiding in plain sight
A 44-year-old man presents as a new patient because he is worried that he has lost weight for no obvious reason and has been noticeably more fatigued recently. He is very worried that he has cancer.He reports to the medical assistant (MA) that he recently moved to the area and has lost about 8 lbs since he arrived 3 months ago, despite having a normal appetite.
After moving to the area, he joined the local newcomer’s volleyball club to meet people. He notes that his stamina has decreased significantly over those 3 months. He is otherwise healthy and is on no medications except for
1 year 1 month ago
PAHO/WHO | Pan American Health Organization
El Comité Ejecutivo de la OPS comienza a debatir temas prioritarios, como inteligencia epidémica y cambio climático y sector salud
PAHO Executive Committee opens to discuss priority issues, including epidemic intelligence and health sector action on climate change
Cristina Mitchell
24 Jun 2024
PAHO Executive Committee opens to discuss priority issues, including epidemic intelligence and health sector action on climate change
Cristina Mitchell
24 Jun 2024
1 year 1 month ago
Jóvenes latinos gay ven un porcentaje cada vez mayor de nuevos casos de VIH; piden financiación específica
Charlotte, Carolina del Norte. — Cuatro meses después de buscar asilo en Estados Unidos, Fernando Hermida comenzó a toser y a sentirse cansado. Primero pensó que estaba resfriado. Luego aparecieron llagas en su ingle y empezó a empapar su cama de sudor. Se hizo una prueba.
El día de Año Nuevo de 2022, a los 31 años, supo que tenía VIH.
Charlotte, Carolina del Norte. — Cuatro meses después de buscar asilo en Estados Unidos, Fernando Hermida comenzó a toser y a sentirse cansado. Primero pensó que estaba resfriado. Luego aparecieron llagas en su ingle y empezó a empapar su cama de sudor. Se hizo una prueba.
El día de Año Nuevo de 2022, a los 31 años, supo que tenía VIH.
“Pensé que me iba a morir”, dijo, recordando el escalofrío que le recorrió el cuerpo cuando revisaba sus resultados. Luchó por navegar un nuevo y complicado sistema de atención médica. A través de una organización de VIH que encontró en internet, recibió una lista de proveedores médicos en Washington, DC, donde estaba en ese momento. Pero no le devolvieron las llamadas durante semanas.
Hermida, que solo habla español, no sabía a dónde ir.
Para cuando Hermida recibió su diagnóstico, el Departamento de Salud y Servicios Humanos de Estados Unidos (HHS) llevaba adelante desde hacía unos tres años una iniciativa federal para acabar con la epidemia de VIH en la nación, invirtiendo cada año cientos de millones de dólares en ciertos estados, condados y territorios con las tasas de infección más altas.
El objetivo era llegar a las aproximadamente 1.2 millones de personas que viven con VIH, incluidas algunas que ni siquiera lo saben.
En general, las tasas estimadas de nuevas infecciones por VIH han disminuido un 23% desde 2012 hasta 2022. Pero un análisis de KFF Health News y Associated Press comprobó que la tasa no ha bajado para los latinos (que pueden ser de cualquier raza) tanto como para otros grupos raciales y étnicos.
Si bien en general los afroamericanos continúan teniendo las tasas más altas de VIH en el país, los latinos representaron la mayor parte de los nuevos diagnósticos e infecciones de VIH entre hombres gays y bisexuales en 2022, según los datos disponibles más recientes, en comparación con otros grupos raciales y étnicos.
Los latinos, que constituyen aproximadamente el 19% de la población de Estados Unidos, representaron alrededor del 33% de las nuevas infecciones por VIH, según los Centros para el Control y Prevención de Enfermedades (CDC). El análisis halló que los latinos están experimentando un número desproporcionado de nuevas infecciones y diagnósticos en todo el país, con las tasas de diagnóstico más altas en el sureste.
Oficiales de salud pública en el condado de Mecklenburg, en Carolina del Norte, y el condado de Shelby, en Tennessee, donde los datos muestran que las tasas de diagnóstico han aumentado entre los latinos, dijeron a KFF Health News y AP que no tienen planes específicos para abordar el problema del VIH en esta población, o que éstos aún no se han finalizado.
Incluso en lugares con buena cantidad de recursos como San Francisco, en California, las tasas de diagnóstico de VIH aumentaron entre los latinos en los últimos años mientras disminuían entre otros grupos raciales y étnicos, a pesar de los objetivos del condado de reducir las infecciones entre los latinos.
“Las disparidades de VIH no son inevitables”, dijo en un comunicado Robyn Neblett Fanfair, directora de la División de Prevención del VIH de los CDC. Señaló las inequidades sistémicas, culturales y económicas, como el racismo, las diferencias de idioma y la desconfianza en los médicos.
Y aunque los CDC proporcionan algunos fondos para grupos minoritarios, defensores de las políticas de salud para los latinos quieren que el HHS declare una emergencia de salud pública con la esperanza de dirigir más dinero a las comunidades latinas, argumentando que los esfuerzos actuales no son suficientes.
“Nuestra invisibilidad ya no es tolerable”, dijo Vincent Guilamo-Ramos, co-presidente del Consejo Asesor Presidencial sobre VIH/SIDA.
Perdido sin un intérprete
Hermida sospecha que contrajo el virus mientras estaba en una relación abierta con un compañero masculino antes de llegar a Estados Unidos. A fines de enero de 2022, meses después que comenzaran sus síntomas, fue a una clínica en la ciudad de Nueva York que un amigo lo ayudó a encontrar para finalmente recibir tratamiento para el VIH.
Demasiado enfermo para cuidarse solo, Hermida finalmente se mudó a Charlotte, Carolina del Norte, para estar más cerca de su familia y con la esperanza de recibir atención médica más constante. Se inscribió en una clínica de Amity Medical Group que recibe fondos del Programa Ryan White de VIH/SIDA, un plan de la red de seguridad federal que atiende a más de la mitad de los diagnosticados con VIH en la nación, independientemente de su estatus migratorio.
Después que se conectó con gestores de casos, su VIH se volvió indetectable. Pero dijo que, con el tiempo, la comunicación con la clínica se volvió menos frecuente y no recibía ayuda regular de un intérprete durante las visitas con su médico, que hablaba inglés.
Un representante de Amity confirmó que Hermida fue cliente, pero no respondió preguntas sobre su experiencia en la clínica.
Hermida dijo que tuvo dificultades para completar el papeleo para mantenerse inscrito en el programa Ryan White, y cuando su elegibilidad expiró, en septiembre de 2023, no pudo obtener su medicación.
Dejó la clínica y se inscribió en un plan de salud a través del mercado de seguros de la Ley de Cuidado de Salud a Bajo Precio (ACA). Pero Hermida no se dio cuenta que la aseguradora le exigía pagar una parte de su tratamiento para el VIH.
En enero, el conductor de Lyft recibió una factura de $1,275 por su antirretroviral, el equivalente a 120 viajes, dijo. Pagó la factura con un cupón que encontró en línea. En abril, recibió una segunda cuenta que no pudo pagar. Durante dos semanas, dejó de tomar la medicación que mantiene al virus indetectable, y por ende no transmisible.
“Estoy que colapso”, dijo. “Tengo que vivir para pagar la medicación”. Una forma de prevenir el VIH es la profilaxis previa a la exposición, o PrEP, que se toma regularmente para reducir el riesgo de contraer el VIH a través del sexo o el uso de drogas intravenosas. Fue aprobada por el gobierno federal en 2012, pero la adopción no ha sido uniforme entre los diferentes grupos raciales y étnicos: los datos de los CDC muestran tasas de cobertura de PrEP mucho más bajas entre los latinos que entre los estadounidenses blancos no hispanos.
Los epidemiólogos dicen que el buen uso de PrEP y el acceso constante al tratamiento son necesarios para construir resistencia a nivel comunitario.
Carlos Saldana, especialista en enfermedades infecciosas y ex asesor médico del Departamento de Salud de Georgia, ayudó a identificar cinco grupos de transmisión rápida de VIH que involucró a unos 40 latinos gay y hombres que tienen sexo con hombres desde febrero de 2021 hasta junio de 2022. Muchas personas en el grupo dijeron a los investigadores que no habían tomado PrEP y que les resultaba difícil entender el sistema de salud.
Saldana dijo que también experimentaron otras barreras, incluida la falta de transporte y el miedo a la deportación si buscaban tratamiento.
Defensores de políticas de salud para los latinos quieren que el gobierno federal redistribuya los fondos para la prevención del VIH, incluyendo pruebas y acceso a PrEP. De los casi $30 mil millones en dinero federal que se destinaron a servicios de atención médica para el VIH, tratamiento y prevención en 2022, solo el 4% se dirigió a la prevención, según un análisis de KFF.
Los defensores sugieren que más dinero podría ayudar a llegar a las comunidades latinas a través de esfuerzos como la divulgación basada en la fe en iglesias, pruebas en clubes durante fiestas latinas, y en capacitar a personal bilingüe para que realice las pruebas.
Aumentan las tasas latinas
El Congreso ha asignado $2.3 mil millones a lo largo de cinco años para la iniciativa Ending the HIV Epidemic, y las jurisdicciones que reciben el dinero deben invertir el 25% en organizaciones comunitarias.
Pero esta iniciativa no requiere dirigirse a determinados grupos, incluidos los latinos: delega en las ciudades, condados y estados la tarea de idear estrategias específicas.
En 34 de las 57 áreas que reciben dinero, los casos van en la dirección equivocada: las tasas de diagnóstico entre los latinos aumentaron de 2019 a 2022 mientras que disminuían en otros grupos raciales y étnicos, halló el análisis de KFF Health News-AP.
A partir del 1 de agosto, los departamentos de salud estatales y locales deberán presentar informes anuales de gastos sobre el financiamiento en lugares que representan el 30% o más de los diagnósticos de VIH, dijeron los CDC. Antes, solo se requería esto en un pequeño número de estados.
En algunos estados y condados, el financiamiento de la iniciativa no ha sido suficiente para cubrir las necesidades de los latinos. Carolina del Sur, que vio las tasas entre latinos casi duplicarse de 2012 a 2022, no ha expandido las pruebas móviles de VIH en áreas rurales, donde la necesidad es alta entre los latinos, dijo Tony Price, gerente del programa de VIH en el departamento de salud del estado.
Carolina del Sur solo puede pagar a cuatro trabajadores comunitarios de salud enfocados en la divulgación sobre el VIH, y no todos son bilingües.
En el condado de Shelby, Tennessee, hogar de Memphis, la tasa de diagnóstico de VIH entre los latinos aumentó un 86% de 2012 a 2022. El Departamento de Salud dijo que recibió $2 millones en financiamiento de la iniciativa en 2023 y, aunque el plan del condado reconoce que los latinos son un grupo objeto, la directora del departamento, Michelle Taylor, dijo: “No hay campañas específicas solo entre los latinos”.
Hasta ahora, el condado de Mecklenburg, en Carolina del Norte, no incluyó objetivos específicos para abordar el VIH en la población latina, donde las tasas de nuevos diagnósticos se han más que duplicado en una década, pero disminuyeron ligeramente entre otros grupos raciales y étnicos.
El departamento de salud ha utilizado fondos para campañas de marketing bilingües y concientización sobre la PrEP.
Mudarse por la medicina
Cuando llegó el momento para Hermida de empacar y mudarse a la tercera ciudad en dos años, su prometido, que está tomando PrEP, sugirió buscar atención en Orlando, Florida.
La pareja, que eran amigos en la escuela secundaria en Venezuela, tenía algunos familiares y amigos en Florida, y habían escuchado sobre Pineapple Healthcare, una clínica de atención primaria sin fines de lucro dedicada a apoyar a los latinos que viven con VIH.
La clínica está en un consultorio al sur del centro de Orlando. El personal, mayoritariamente latino, viste camisetas turquesa con estampado de piñas, y se escucha con más frecuencia español que inglés en los cuartos de atención y en los pasillos.
“En su esencia, si la organización no es dirigida por y para personas de color, entonces solo somos una idea de último momento”, dijo Andres Acosta Ardila, director de divulgación comunitaria en Pineapple Healthcare, quien fue diagnosticado con VIH en 2013.
“¿Te mudaste reciente [mente], ya por fin?”, preguntó la enfermera Eliza Otero, quien comenzó a tratar a Hermida cuando todavía vivía en Charlotte. “Hace un mes desde la última vez que nos vimos”.
Todavía necesitan trabajar en bajar su colesterol y presión arterial, le dijo. Aunque su carga viral sigue siendo alta, Otero dijo que debería mejorar con atención regular y constante.
Pineapple Healthcare, que no recibe dinero de la iniciativa federal, ofrece atención primaria completa principalmente a hombres latinos. Allí, Hermida obtiene su medicación para el VIH sin costo porque la clínica es parte de un programa federal de descuento de medicamentos.
En muchos sentidos, la clínica es un oasis. La tasa de nuevos diagnósticos para los latinos en el condado de Orange, Florida, que incluye Orlando, aumentó alrededor de un tercio desde 2012 hasta 2022, mientras que disminuyó un tercio para otros. Florida tiene la tercera población latina más grande de Estados Unidos y tuvo la séptima tasa más alta de nuevos diagnósticos de VIH entre latinos en la nación en 2022.
Hermida, que tiene pendiente su caso de asilo, nunca imaginó que obtener medicación sería tan difícil, dijo durante el viaje de 500 millas de Carolina del Norte a Florida. Después de habitaciones de hotel, trabajos perdidos y despedidas familiares, espera que su búsqueda de tratamiento consistente para el VIH, que ha definido su vida en los últimos dos años, finalmente pueda llegar a su fin.
“Soy un nómade a la fuerza, pero bueno, como dicen mi prometido y mis familiares, yo tengo que estar donde me den buenos servicios médicos”, dijo.
Esa es la prioridad ahora, agregó.
KFF Health News y The Associated Press analizaron datos de los Centros para el Control y Prevención de Enfermedades de Estado Unidos sobre el número de nuevos diagnósticos e infecciones de VIH entre estadounidenses de 13 años y más a nivel local, estatal y nacional.
Esta historia utiliza principalmente datos de tasas de incidencia —estimaciones de nuevas infecciones— a nivel nacional y datos de tasas de diagnóstico a nivel estatal y de condados.
Bose produjo esta historia desde Orlando, Florida. Reese, desde Sacramento, California. La periodista de video Laura Bargfeld colaboró con este informe.
The Associated Press Health and Science Department recibe apoyo de la Fundación Robert Wood Johnson. AP es responsable de todo el contenido.
Esta historia fue producida por KFF Health News, que publica California Healthline, un servicio editorialmente independiente de la California Health Care Foundation.
Un proyecto de KFF Health News y The Associated PressCo-publicado por Univisión Noticias
CRÉDITOS
Reporteros:Vanessa G. SánchezDevna BosePhillip ReeseCinematografía:Laura BargfeldFotografía:Laura BargfeldPhelan M. EbenhackEdición de video:Federica NarancioKathy YoungEsther PovedaVideo adicional:Federica NarancioEsther PovedaProducción de video:Eric HarkleroadLydia Zuraw
Editores:Judy LinErica HunzingerEditor de datos:Holly HackerRedes sociales:Patricia VélezFederica NarancioEsther PovedaCarolina AstuyaNatalia BravoJuan Pablo VargasKyle ViterboSophia EppolitoHannah NormanChaseedaw GilesTarena LoftonTraducción:Paula Andalo Corrección:Gabe Brison-Trezise
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 1 month ago
california, Noticias En Español, Public Health, Race and Health, States, Florida, HIV/AIDS, Latinos, LGBTQ+ Health, New York, North Carolina, Sexual Health, South Carolina, Tennessee
Health Archives - Barbados Today
UWI student wins NCD Commission’s competition
Akebulan Thuo, a student at The University of the West Indies (UWI), Cave Hill Campus, has emerged as the winner of the National NCD Commission’s polo shirt design competition.
The Commission, in its effort to reach various segments of the population, through the theme “A Healthier Barbados, A Healthier Me”, engaged young people in a polo shirt design competition. Some 40 submissions were received from students from primary and secondary schools, both public and private, and The UWI.
The initiative builds on the implementation of the National School Nutrition Policy, by supporting the expansion of the health message across and throughout the school environments.
Entrants were judged by members of the NCD Commission in two rounds, with final tailoring by a Graphic Artist of B3 Imaging, who printed the polo shirts.
Thuo won two day passes for two persons each, to the Sam Lord’s Castle Wyndham Grand Resort. Second and third-place winners were Brooklyn Mascoll of the St Alban’s Primary School and Hayley Scott of Christ Church Foundation School, respectively. They received prizes of one day pass for two persons each, to the Sam Lord’s Castle Wyndham Grand Resort.
The post UWI student wins NCD Commission’s competition appeared first on Barbados Today.
1 year 1 month ago
Health, Local News
Health – Demerara Waves Online News- Guyana
New law to go after sale of unprescribed antibiotics, fake medicines
Health Minister Dr Frank Anthony on Sunday warned that pharmacies that sell antibiotics without prescriptions would soon be shut down, as Guyana joins the rest of the world in reducing the resistance to antibiotics and other types of prescription drugs. He said the Health Ministry has received reports that a number of pharmacies have been ...
Health Minister Dr Frank Anthony on Sunday warned that pharmacies that sell antibiotics without prescriptions would soon be shut down, as Guyana joins the rest of the world in reducing the resistance to antibiotics and other types of prescription drugs. He said the Health Ministry has received reports that a number of pharmacies have been ...
1 year 1 month ago
Business, Health, News, Politics, antimicrobial resistance, fake medicines, Guyana Pharmacists Association, medicine regulations law, unprescribed antibiotics
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Managing gestational diabetes earlier in pregnancy can prevent complications and improve outcomes: Lancet
A shift in testing for and managing Gestational Diabetes Mellitus (GDM) to much earlier in pregnancy (before 14 weeks) can prevent health complications for both the mother and baby, according to a new Series published in The Lancet.
A shift in testing for and managing Gestational Diabetes Mellitus (GDM) to much earlier in pregnancy (before 14 weeks) can prevent health complications for both the mother and baby, according to a new Series published in The Lancet. Series authors challenge the current approach to GDM management – which focuses on late GDM (24 weeks+) – and call for better detection and prevention efforts alongside a personalised, integrated life-course approach for those who experience or are at risk for GDM.
GDM, also known as gestational diabetes – a type of diabetes that is found during pregnancy where blood glucose levels are higher than average but not as high as diabetes – is the most common medical pregnancy complication worldwide, affecting one in seven (14%) of pregnancies. As obesity and other metabolic conditions continue to increase around the world, more women of reproductive age will experience some degree of abnormal glucose/insulin regulation, which leads to higher risks of pregnancy complications as well as health conditions later in life, such as type 2 diabetes (T2D) and cardiovascular disease.
“Our new Series emphasises the urgent need for a major shift in how GDM is first diagnosed and managed, not only during pregnancy but throughout the lifetime of mothers and their babies,” said Series lead Prof. David Simmons of Western Sydney University, Australia. “GDM is an increasingly complex condition, and there isn’t a one-size-fits-all approach to managing it. Instead, a patient’s unique risk factors and metabolic profile should be considered to help guide them through pregnancy and support them afterward to achieve the best health outcomes for women and babies everywhere.”
GDM and its complications are on the rise
As obesity continues to increase worldwide, along with impaired glucose tolerance and T2D rates in women of reproductive age, GDM prevalence has also increased two to threefold across multiple countries over the last 20 years. The current GDM prevalence rates range from over 7% in North America and the Caribbean region to almost 28% in the Middle East and North Africa region.
Between 30% and 70% of women with GDM experience high blood glucose (hyperglycemia) from early pregnancy (20 weeks gestation or sooner, also known as early GDM). These women have worse pregnancy outcomes compared to women whose GDM is not present until later in pregnancy (24-28 weeks). Even later in pregnancy, in studies where GDM was not managed adequately (e.g., where insulin was needed but not used), GDM was associated with increased risks of cesarean delivery (16%), preterm delivery (51%), and large for gestational age babies (57%). Other studies that looked at GDM pregnancies requiring insulin therapy found it was associated with a more than two-fold increased risk of neonatal intensive care unit admission.Women diagnosed with GDM have a 10-fold higher risk of developing T2D later in life compared to women who did not experience GDM.
They are also more likely to have co-existing hypertension, dyslipidemia (high blood lipid levels), obesity, and fatty liver, with a two-fold higher risk for developing cardiovascular disease during their lifetime. Women with GDM also experience more significant risks of mental health conditions, including stress, depression, and anxiety, along with stigma and feelings of guilt and shame related to GDM during pregnancy. Beyond their own impacts, these feelings of guilt and shame can lead to additional adverse outcomes if patients avoid testing glucose levels or taking insulin because of them.
Recent studies have suggested that GDM diagnosis may be associated with an increased risk of subsequent postpartum depression. Conversely, treatment of late GDM is associated with lower rates of depression at three months postpartum, while treatment of early GDM is associated with improvement of quality of life at 24 to 28 weeks gestation.
“GDM is a tremendous public health challenge. Women who experience it need support from the medical community, policymakers, and society as a whole to ensure they can effectively access proper treatment, reduce the stigma associated with GDM, and improve their overall pregnancy experience,” said Series author Dr Yashdeep Gupta of the All India Institute of Medical Science.
Early diagnosis for a lifetime of better health outcomes
GDM has historically been considered a pregnancy complication involving the treatment of high blood glucose levels late in the second trimester. The World Health Organization’s current diagnostic criteria for GDM recommends testing at 24-28 weeks gestation without prior screening.
However, recent evidence suggests that GDM has foundations before pregnancy and can be present in early pregnancy. Overall, 30-70% of GDM can be found early using oral glucose tolerance testing and includes those at most significant risk of requiring insulin therapy and experiencing pregnancy complications.
Recent studies, such as the TOBOGM RCT , showed that among women with early GDM, identification, and treatment before 20 weeks gestation (compared to 24-28 weeks) not only reduced pregnancy complications and postpartum complications, including neonatal respiratory distress and length of stay in neonatal intensive care units, but also improved quality of life mid-pregnancy and increased breastfeeding initiation, which can reduce the likelihood of developing obesity, T2D, and other long-term conditions. “The benefits of early GDM detection are clear – we can keep mothers and babies healthier during pregnancy and hopefully continue that path for a lifetime. What is needed now is earlier testing and an approach to managing GDM that takes the available resources, circumstances, and personal wishes of the patient into consideration,” said Series author Dr Helena Backman of Örebro University, Sweden.
New strategies are urgently needed to improve GDM management
A better understanding of GDM and its effects can help researchers, clinicians, and policymakers develop new management approaches that focus on improved prevention and treatment of GDM complications from pre-conception through pregnancy and beyond.
The recommended strategies developed by the Series authors include:
• Early GDM testing of those with risk factors, ideally before 14 weeks gestation.
• Promoting health at the population level that prepares women, especially those with risk factors for a healthy pregnancy and, after that, for healthy aging. - Improve antenatal care that includes postpartum screening for glycemic status.
• Tailored annual assessments in women with prior GDM to prevent or better manage complications such as T2D (particularly in subsequent pregnancies) and cardiovascular disease.
• More research into GDM and how to improve outcomes of women with GDM and their children across the life course.
“It is past time to move from ‘late pregnancy’ focused services to an integrated, personalized life-course strategy across both high- and low-resource settings. This includes new, systematic approaches to prevention, early GDM treatment, identifying and overcoming barriers to uptake, better health system integration, and more research to better understand how GDM affects women and their children during pregnancy and throughout their lives,” said Prof. Simmons.
Reference:
Marie-France Hivert, Helena Backman, Katrien Benhalima, Prof Patrick Catalano, Prof Gernot Desoye, Jincy Immanuel, Christopher J D McKinlay, Prof Claire L Meek, Prof Christopher J Nolan, Pathophysiology from preconception, during pregnancy, and beyond, The Lancet, https://doi.org/10.1016/S0140-6736(24)00827-4.
1 year 1 month ago
Diabetes and Endocrinology,Obstetrics and Gynaecology,Diabetes and Endocrinology News,Obstetrics and Gynaecology News,Top Medical News,Latest Medical News
Health Archives - Barbados Today
Fogging In St James and St Thomas this week
A number of communities in St James and St Thomas will be fogged this week, when the Ministry of Health’s Vector Control Unit conducts its mosquito reduction exercise.
The Unit will concentrate its efforts in St James for the first three days of the week. On Monday, Wanstead Gardens, Husbands Heights, Santa Rosa Drive, Mid-Summer Drive, and Dracaena Avenue will be targeted.
A number of communities in St James and St Thomas will be fogged this week, when the Ministry of Health’s Vector Control Unit conducts its mosquito reduction exercise.
The Unit will concentrate its efforts in St James for the first three days of the week. On Monday, Wanstead Gardens, Husbands Heights, Santa Rosa Drive, Mid-Summer Drive, and Dracaena Avenue will be targeted.
The team will then go into Dairy Meadows Road, John Plains, St John The Baptist Road, and Bamboo Ridge, on Tuesday,.
The following day the Unit will spray Hoytes Village, Cavewood Road, Bagatelle Terrace with Avenues, and Hoytes Terrace. On Thursday, Center Lane, Kew Road, and Redman Village in St Thomas will be visited.
The fogging exercise will conclude on Friday in Welches, Welches Heights, Plum Tree Avenue, Terrace Drive, Padmore Village, and surrounding districts.
Fogging takes place from 4:30 to 8:30 p.m. daily. Householders are reminded to open their windows and doors to allow the spray to enter. Children should not be allowed to play in the spray.
Members of the public are advised that the completion of scheduled fogging activities may be affected by events beyond the Unit’s control. In such circumstances, the Unit will return to communities affected in the soonest possible time. (PR)
The post Fogging In St James and St Thomas this week appeared first on Barbados Today.
1 year 1 month ago
Health, Local News, News
New Cure for Heartbreak: A Headset That Zaps the Brain - Newser
- New Cure for Heartbreak: A Headset That Zaps the Brain Newser
- Electrical brain stimulation can ease heartbreak, study finds The Guardian
- Stimulating the brain with electricity can heal the pain of a broken heart Jamaica Gleaner
- Banish breakup blues: New headset zaps brain to ease heartbreak Interesting Engineering
- Broken Hearted? A Zap to the Brain Could Help, Study Says NDTV
1 year 1 month ago
Prostate cancer an emerging concern, but early diagnosis and treatment bring hope - ABS-CBN News
- Prostate cancer an emerging concern, but early diagnosis and treatment bring hope ABS-CBN News
- Early Detection of Prostate Cancer Can Save Lives AdventHealth
- Dignity Health: When to schedule a prostate screening KGET 17
- Prostate cancer treatment and recovery | Health Jamaica Gleaner
- HealthWatch: A PSA for prostate cancer WeAreGreenBay.com
1 year 1 month ago
Anthony says four dengue deaths recorded since January, 398 hospitalised - Stabroek News
- Anthony says four dengue deaths recorded since January, 398 hospitalised Stabroek News
- Health minister confirms dengue deaths in Guyana caribbeannationalweekly.com
- Man, 22, dies from dengue Stabroek News
1 year 1 month ago
KFF Health News' 'What the Health?': Live From Aspen: Health and the 2024 Elections
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
The presidential election is less than five months away, and while abortion is the only health policy issue expected to play a leading role, others are likely to be raised in the presidential and down-ballot races. This election could be critical in determining the future of key health care programs, such as Medicaid and the Affordable Care Act.
In this special episode of KFF Health News’ “What the Health?” taped at the Aspen Ideas: Health festival in Aspen, Colorado, Margot Sanger-Katz of The New York Times and Sandhya Raman of CQ Roll Call join Julie Rovner, KFF Health News’ chief Washington correspondent, to discuss what the election season portends for top health issues.
Panelists
Margot Sanger-Katz
The New York Times
Sandhya Raman
CQ Roll Call
Among the takeaways from this week’s episode:
- Policies surrounding abortion — and reproductive health issues, in general — likely will dominate in many races, as Democrats try to exploit an issue that is motivating their voters and dividing Republican voters. The topics of contraception and in vitro fertilization are playing a more prominent role in 2024 than they have in past elections.
- High prescription drug prices — which, for frustrated Americans, are a longtime symbol, and symptom, of the nation’s dysfunctional health care system — have been a priority for the Biden administration and, previously, the Trump administration. But the issue is so confusing and progress so incremental that it is hard to say whether either party has an advantage.
- The fate of many major health programs will be determined by who wins the presidency and who controls Congress after this fall’s elections. For example, the temporary subsidies that have made Affordable Care Act health plans more affordable will expire at the end of 2025. If the subsidies are not renewed, millions of Americans will likely be priced out of coverage again.
- Previously hot-button issues like gun violence, opioid addiction, and mental health are not playing a high-profile role in the 2024 races. But that could change case by case.
- Finally, huge health issues that could use public airing and debate — like what to do about the nation’s crumbling long-term care system and the growing shortage of vital health professionals — are not likely to become campaign issues.
click to open the transcript
Transcript: Live From Aspen: Health and the 2024 Elections
KFF Health News’ ‘What the Health?’ Episode Title: ‘Live From Aspen: Health and the 2024 Elections’Episode Number: 352Published: June 21, 2024
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Mila Atmos: The future of America is in your hands. This is not a movie trailer and it’s not a political ad, but it is a call to action. I’m Mila Atmos and I’m passionate about unlocking the power of everyday citizens. On our podcast “Future Hindsight,” we take big ideas about civic life and democracy and turn them into action items for you and me. Every Thursday we talk to bold activists and civic innovators to help you understand your power and your power to change the status quo. Find us at futurehindsight.com or wherever you listen to podcasts.
Julie Rovner: Hello, and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent at KFF Health News, and I’m joined by some of the best and smartest health reporters in Washington. I am joined tonight by a couple of our regular panelists: Margot Sanger-Katz, The New York Times.
Sanger-Katz: Hey, everybody.
Rovner: And Sandhya Raman of CQ Roll Call.
Raman: Good evening everyone.
Rovner: For those of you who aren’t regular listeners, we have a rotating panel of more than a dozen health policy reporters, all of whom just happen to be women, and every week we recap and analyze the week’s top health news. But tonight we’ve been given a slightly different assignment to talk about how health policy is likely to shape the 2024 elections and, vice versa, how the elections are likely to shape health policy.
So, this is actually my 10th presidential election season as a health reporter, which is terrifying, and I can say with some experience that health is one of those issues that’s always part of the political debate but is relatively rarely mentioned when pollsters ask voters what their top issue is. Of those of you who went to the pollsters session this afternoon might’ve seen that or said we’re not going to… it’s not going to be a health election this year.
This year, though, I think will be slightly different. As you’ll hear, I’ve divided these issues into three different buckets: Those that are likely to be pivotal or very important to how people vote; those that are likely to come up over the next few months in the presidential and/or congressional and Senate races; and finally, a couple of issues that aren’t as likely to come up but probably should. It would be good to have a debate about them.
So we will start with the political elephant in the room: reproductive health. Since the Supreme Court overturned Roe v. Wade two years ago next week, abortion has been front and center in just about every political contest, usually, though not always, with the abortion-right side prevailing. How do you two see abortion playing out both at the presidential and congressional level these next couple of months?
Raman: I see it playing out in kind of two different ways. We see already at the presidential level that President Joe Biden has been really going in, all in, that this is his No. 1 issue, and I think this will continue to play out, especially next week with the anniversary of the Dobbs [v. Jackson Women’s Health Organization] decision.
And a lot of the Democrats in the Senate have kind of been taking lead from that and also really amping up the issue. They’ve been doing kind of messaging votes on things within the reproductive health spectrum and it seems like they’re going to continue that in July. So we’re going to see it really focused on there. On the Republican side, they’ve been not focused on this issue as much.
Rovner: They’ve been ducking this issue.
Raman: Yes, they’ve been ducking this issue, so I think it’ll just be continued to be downplayed. They’ve really been going in on immigration more than any other of the issues that they’ve got this year.
Sanger-Katz: If you look at the public polling, abortion is one of really the only issues where the Democrats and Joe Biden seem to have a real advantage over the Republicans and Donald Trump. And so I think that that tells you that they’re going to have to be hitting it a lot. This is an issue where the voters are with the Democrats. They trust Biden more. They agree more with the policies the Democrats are promoting around reproductive health care. So it’s just impossible for me to imagine a scenario in which we don’t see Democrats kind of up and down the ticket really taking advantage of this issue, running ads on it, talking about it, and trying to really foreground it.
I think for Biden, in particular, it’s a hard issue. I think he has always had some personal ambivalence about abortion. He’s a Catholic. He, early in his career, had opposed certain abortion rights measures that other Democrats had endorsed, and you can kind of see him slowly getting comfortable with this issue. I think he said the word abortion for the first time just in the last six months. I think I would anticipate a real ramping up of discussion of this issue among Democrats. The other dynamic that I think is pretty important is that there are a number of states that have ballot initiatives to try to kind of permanently enshrine abortion rights into state constitutions.
And some of those are in states that are not pivotal to the election, and they will be important in those states, and for those state senate races and governor races and other things, because they may pull in more of these voters who care a lot about reproductive rights. But there are some of these ballot measures that are in pivotal states for the presidential race, the kind of battleground states that we’re all watching. And so there’s a big emphasis on those as well. And I think there’s some interesting tensions with those measures because abortion rights actually are valued by people across the political spectrum.
So I think we tend to think of this as a Democrat-Republican issue where Republicans want to restrict abortion rights, and Democrats want to promote them. But we’re seeing in the public polling now that’s not really true. There are a lot of Republicans that are uncomfortable with the kind of abortion bans that we’re seeing in certain parts of the country now. So it’s this question: Are they going to come out and vote and split their ticket where they’ll vote for constitutional measure to protect abortion rights and still vote for President Trump? Or will the abortion issue mobilize them so much that they will vote across the board as Democrats?
And I think that’s a big question, and I think it’s a big challenge. In fact, for many of the people that are running these campaigns to get these ballot measures passed, how much they want to kind of lean into the Democratic messaging and try to help prop up Democratic candidates in their state. And how much they want to just take a step back and try to get Republicans to support their particular measure, even if it doesn’t help Democratic candidates on the ticket.
Rovner: Well, of course, it’s not just abortion that’s on the ballot, literally and figuratively. There’s a not-insignificant portion of the anti-abortion movement that not only wants to ban abortion nationwide but wants to establish in law something called personhood. The concept that a person with full legal rights is created at fertilization.
That would result in outlawing many forms of contraception, as well as if we have seen rather vividly this spring, IVF. Unlike abortion, contraception and IVF are very widely supported, not nearly as divisive as abortion itself is. Are we potentially looking at a divorce between the Republican Party and its longtime absolutist, anti-abortion backers?
Raman: I think that Republicans have been toeing the line on this issue so far. We’ve seen them not support some of the Democrats’ bills on the state level, the federal level, that are related to IVF, but at the same time, kind of introducing their counterparts or issuing broad statements in support of IVF, in support of contraception. Even just like a couple of weeks ago, we had Sen. Rick Scott of Florida release an IVF-themed full ad.
And so we have a lot of messaging on this, but I think at the same time a lot of these are tiptoeing the line in that they might not add any new protections. They might not codify protections for any of these procedures. They might just issue support or not address some of the other issues there that people have been going back and forth with the personhood issue.
Sanger-Katz: I think this is a big challenge for the Republican Party, not just over the course of this particular election cycle, but I think thinking further into the future. The pro-life movement has been such a pivotal group of activists that have helped elect Republicans and have been so strongly allied with various other Republican interest groups across the last few decades. And you can see that those activists helped overturn Roe after nearly 50 years of having a constitutional right to abortion.
Many of them don’t want to give up there. They really want to abolish abortion. They think it’s a morally abhorrent and something that shouldn’t happen in this country. And they’re concerned that certain types of contraception are similar to abortion in certain ways and that IVF is also morally abhorrent. And we saw recently with the [Southern] Baptist Convention that there was a vote basically to say that they did not support in vitro fertilization and assisted reproductive technologies.
Yet, at the same time, you can see in public polling and in the way that the public responds to these kinds of messages that the activists are way out further than the typical voter and certainly way out further than the typical Republican voter. And there’s this interesting case study that happened a few months ago where the Alabama Supreme Court issued a ruling — the implications of which suggested that IVF might be imperiled in that state — and it was kind of uncertain what the result that would be.
And what happened, in fact, is that Republicans and the Alabama State Legislature and the Republican governor of Alabama, many of whom had sort of longtime pro-life connections and promises, immediately passed a bill to protect in vitro fertilization because they saw that it was something that their voters really cared about and that’s something that could really hurt them politically if they were being seen as being allied with a movement that wanted to ban it.
But the activists in this movement are really important part of the Republican coalition, and they’re very close to leadership. And I think this is going to be a real tension going forward about how does the party accommodate itself to this? Do they win hearts and minds? They figure out a way to get the public on their side? Or do they kind of throw over these people who have helped them for so long, and these ideological commitments that I do think that many Republican politicians really deeply do hold?
Rovner: How much wild card is Donald Trump can be in this? He’s been literally everywhere on this issue, on reproductive rights in general. He is not shy about saying he thinks that abortion is a loser of an issue for Republicans. He wants to just continue to say, “Let the states do whatever they want.”
But then, of course, when the states do things like perhaps ban IVF — that I would think would even make Donald Trump uncomfortable — he seems to get away with being anywhere he wants with these very strong evangelical and pro-life groups who have supported him because, after all, he appointed the two Supreme Court justices that overturned Roe. But I’m wondering if, down-ballot, how all these other candidates are going to cope with the forever sort of changing position of the head of their ticket.
Sanger-Katz: I think it’s pretty interesting. I was talking with a colleague about this recently. It seems like Trump’s strategy is to just have every position. If you look at his statements, he said just about every possible thing that you could possibly say about abortion and where he stands on it. And I think it’s actually quite confusing to voters in a way that may help him because I think if you’re only looking for the thing that you want to hear, you can find it.
If you’re someone who’s really a pro-life activist who cares a lot about restricting abortion, he brags about having been responsible for overturning Roe. And if you’re someone who really cares about protecting IVF, he’s said that he wants that. If you’re someone who want… lives in a state that has… continues to have legal abortion, he said, “We’re going to leave that up to the states.”
If you’re in a state that has banned abortion, that has very extreme bans, he said something that pleases you. And so, I don’t know. I did a story a few weeks ago where I interviewed voters who had been part of a New York Times/Siena poll, and these were voters who, they were asked a question: Who do you find responsible for the Dobbs decision for the overturning of Roe v. Wade? And these were voters who supported abortion rights but thought that Joe Biden was responsible. And there’re like… it’s not a lot of people, but it’s …
Rovner: But it’s like 20%, isn’t it?
Sanger-Katz: Yeah, it’s like 10[%], 15% of voters in battleground states, people whose votes are really going to matter and who support abortion rights. They don’t know who was responsible. They don’t really understand the dynamics of where the candidates are on this issue. And I think for those of us who are very politically engaged and who are following it closely, it’s kind of hard to imagine. But they’re just a lot of people who are not paying close attention.
And so I think that makes Trump being everywhere on the issue, it makes it easier for those people to not really engage with abortion. And I think that’s again why I think we’re going to see the Biden campaign and other Democrats kind of hitting it over and over and over again. “This is Trump’s fault. We are going to protect abortion rights.” Because I think that there are a lot of voters who don’t really know what to make of the candidates and don’t know what to make of Trump on this particular issue.
Rovner: Well, Sandhya, they keep trying to bring it up in Congress, but I don’t think that’s really breaking through as a big news story.
Raman: No, and I think that for Congress, we’ve seen the same thing this year, but we’ve also seen it in previous years where they coalesce around a certain week or a certain time and bring up different bills depending on who’s in control of that chamber to message on an issue. But it hasn’t really moved the needle either way that we get similar tallies, whether it was this year or three years ago or 10 years ago.
One thing that I think activists are really looking at on the pro-life side is just really Trump’s record on these issues. Regardless of what he’s saying this week or last week or in some of these different interviews that’s a little all over the place. They’ve pointed to a lot of things that he’s done, like different things that he’s expanded more than previous Republican presidents. And for them, that might be enough.
That’s if it’s just the dichotomy of Biden versus Trump, that to get to their end goal of more pro-life policies, then Trump is the easy choice. And in the past years, the amount of money that they have poured into these elections to just really support issues… candidates that are really active on these issues, has grown astronomically. So I don’t know that necessarily if he does make some of these statements it’s going to make a huge difference in their support.
Sanger-Katz: And I think it also comes back to Julie’s opening point, which is I think abortion is an issue on which the Democrats have a huge edge, and I do think it is an issue that is very mobilizing for certain types of voters. But I also think that this is an election in which a lot of voters, whatever their commitments are on abortion, may be deciding who to vote for based on another set of issues. Those people that I talked to who were kind of confused about abortion, they really cared a lot about the economy.
They were really concerned about the cost of groceries. And so I think for those people, they may have a preference on abortion. If they could sort of pick each individual issue, they might pick something different. But I think the fact that they supported abortion rights did not necessarily mean that even if they really understood where the candidates were that they were necessarily going to vote for Joe Biden. I think a lot of them were going to vote for Donald Trump anyway because they thought he was better on the issues that were affecting their daily lives more.
Rovner: Well, Margot, to your point about voters not knowing who’s responsible for what, I think another big issue in this campaign is going to be prescription drug prices. As we know, drug prices are kind of the stand-in for everything that’s currently wrong with the nation’s health care system. The system is byzantine. It can threaten people’s health and even their lives if they can’t afford it.
And just about every other country does it better than we do. Interestingly, both President Biden and former President Trump made drug prices a top health priority, and both have receipts to show what they have done, but it’s so confusing that it’s not clear who’s going to get credit for these things that have gotten done.
Trump said that Biden was lying when Biden said that he had done the insulin cap for Medicare, which in fact was done by the Democrats, although Trump had done sort of a precursor to it. So, who wins this point, or do you think it’s going to end up being a draw? Because people are not going to be able to figure out who was responsible for which parts of this. And by the way, we haven’t really fixed it anyway.
Raman: I would say it was a draw for two reasons. I think, one, when we deal with something like drug prices, it takes a while for you to see the effects. When we have the IRA [Inflation Reduction Act] that made it so that we can negotiate the price of some drugs under Medicare, the effects of that are over a long tailwind. And so it’s not as easy to kind of bring that up in political ads and that kind of thing when people aren’t seeing that when they go to the pharmacy counter.
And I think another thing is that for at least on the congressional level, there’s been a little bit of a gap in them being able to pass anything that kind of moves the point along. They made some efforts over the past year but weren’t able to get it over the finish line. I think it’s a lot more difficult to say, “Hey, we tried but didn’t get this done” without a … as a clear campaign message and to get votes on that.
Sanger-Katz: I also think it’s this issue that’s really quite hard because — setting aside $35 insulin, which we should talk about — most people have insurance, and so the price of the drug doesn’t always affect them in a direct way. A lot of times, when people are complaining about the high cost of drugs, they’re really complaining about the way that their insurance covers the drug. And so the price of the drug might, in fact, be astronomical, but it’s the $100 copayment that people are responding to.
And so it could be that the government is taking all these actions, or the companies by themselves, and the price has gone down, but if you’re still paying that $100 copayment, you’re not really experiencing the benefits of that change. So I do think that the Democrats and Joe Biden have done two things that are helpful in that regard. So, one, is this $35 cap on copayments for insulin. So that’s just for people in Medicare, so it’s not everyone. But I do think that is… it’s a great talking point. You can put that on an ad. It’s a real thing.
People are going to go to the pharmacy counter, and they’re not going to pay more than that. It’s easy to understand. The other thing that they did, and I think this is actually harder to understand, is they redesigned the drug benefit for people who have Medicare. So it used to be in Medicare that if you had a really expensive set of drugs that you took, like, say, you had cancer and you were taking one of these newer cancer drugs that cost tens of thousands dollars a year, you could be on the hook for tens of thousands of dollars a year out of your own pocket, on top of what your insurance covered.
If you took less-expensive drugs, your insurance kind of worked the way it works for people in the commercial market where you have some copayments, not that you don’t pay anything, but it wasn’t sort of unlimited. But for really high-cost drugs in Medicare, people in Medicare were on the hook for quite a lot of money, and the Inflation Reduction Act changed that. They changed the Medicare drug benefit, and now these people who have these really expensive health conditions have a limit. They only have to pay a couple of thousand dollars a year.
Rovner: But it doesn’t start until next year.
Sanger-Katz: But it doesn’t start until next year. So I just think a lot of this stuff around drug prices is, people feel this sense of outrage that the drugs are so expensive. And so I think that’s why there’s this huge appetite for, for example, having Medicare negotiate the price of drugs. Which is another thing that the Inflation Reduction Act enabled, but it’s not going to happen in time for the election.
But I don’t think that really hits people at the pharmacy counter. That is more the benefits of that policy are going to affect taxpayers and the government. They’re not going to affect individual people so much. And I think that’s part of why it’s such a hard issue. And I think that President Trump bumped up against this as well.
His administration was trying all of these little techniques deep in the works of the drug pricing and distribution system to try to find ways to lever down the prices of drugs. And some of them worked, and some of them didn’t. And some of them got finalized, and some of them didn’t. But I think very few of them had this obvious consumer impact. And so it was hard for them to go to the voters and say, “We did this thing. It affected your life.”
Rovner: I see some of these ads, “We’ve got to do something about the PBMs [Pharmacy Benefit Managers].” And I’m like, “Who’s this ad even aimed at? I cover this for a living, and I don’t really understand what you’re talking about.” I wonder, though, if some… if candidates really on both sides, I mean, this is a unique election in that we’ve got two candidates, both of whom have records behind them.
I mean, normally, you would have at least one who’s saying, “This is what I will do.” And, of course, when it comes to drug prices, the whipping boy has always been the drug companies. And I’m wondering if we’re not going to see candidates from both parties at all levels just going up against the drug companies because that’s worked in the past.
Raman: I think it’s kind of a difficult thing to do when I think so many candidates, congressional level especially, have good relationships with pharmaceutical companies as some of the top donors for their campaigns. And so there’s always that hesitation to go too hard on them when that is helping keep them in office.
So it’s a little bit more difficult there to see teeth-out going into an ad for something like that. I think when we go back to something like PBMs where it seems like everyone in Congress just has made that kind of the bully of this past couple years, then that might be something that’d be easier to throw into ads saying, “I will go after PBMs.”
Sanger-Katz: I think we’re likely to see, especially in congressional races, a lot of candidates just promising to lower your drug prices without a whole lot of detail under that.
I don’t know that it’s necessarily going to be like the evil pharmaceutical companies, and I don’t think it’s going to be detailed policy proposals for all the reasons I just said: because it’s complicated; doesn’t always affect people directly; it’s hard to understand. But I think it will be a staple promise that we’ll particularly see from Democrats and that I expect we will hear from President Trump as well because it’s something that has been part of his kind of staple of talking points.
Rovner: So let’s move on to some of the issues that are sort of the second-tier issues that I expect will come up, just won’t be as big as immigration and abortion. And I want to start with the Affordable Care Act. I think this is the first time in a presidential election year that it seems that the continuing existence of the ACA is no longer in question. If you disagree, do let me know, but that’s not to suggest …
Sanger-Katz: Maybe last time.
Rovner: Little bit. That’s not to suggest, though, that the fate of the Affordable Care Act is not also on the line in this election. The additional subsidies that the Democrats added in the Inflation Reduction Act, which will sunset at the end of next year unless they are renewed, are responsible in large part for the largest percentage of Americans with health insurance ever measured.
And conversely, the Congressional Budget Office estimates that enrollment would fall by an immediate 20% if the subsidies are allowed to expire. It’s hard to see how this becomes a campaign issue, but it’s obviously going to be really important to what… I mean who is elected is going to be really important to what happens on this issue, and it’s a lot of people.
Raman: Using the subsidies as a campaign point is a difficult thing to do. It’s a complicated issue to put in a digestible kind of ad thing. It’s the same thing with a lot of the prescription drug pricing policies where, to get it down to the average voter, is hard to do.
And I think had we not gotten those subsidies extended, we would’ve seen people more going into that in ads. But when it’s keeping the status quo, people aren’t noticing that anything has changed. So it’s an even more difficult thing to kind of get across.
Sanger-Katz: I think this is one of, in health care, one of the highest-stakes things. That I feel like there’s just a very obvious difference in policy depending on who is elected president. Whereas a lot of the things that we’ve talked about so far, drug prices, abortion, a little harder to predict. But just to get out of the weeds for a second, Congress increased the amount of money that poor and middle-class people can get when they buy their own health insurance on the Obamacare exchanges. And they also made it possible for way more people to get health insurance for free.
So there are a lot of Americans who were uninsured before who now have insurance that they don’t pay a single dollar for. And there are also a lot of Americans that are higher, the kind of people that were disadvantaged in the early years of Obamacare, sort of self-employed people, small business owners who bought their own insurance and used to just have sort of uncapped crazy premiums. People who earn more than $100,000 a year now have financial assistance for the first time ever. And that policy has been in place for several years, and we’ve seen record enrollment.
There’s lots more people with insurance now, and their insurance is more affordable than it’s ever been. And those things are, of course, related. I think it’s almost definitely going to go away if Trump is elected to the presidency and if Republicans take at least one house of Congress because basically it’s on a glide path to expiration. So if nothing is done, that money will go away. What needs to happen is for Congress to pass a new law that spends new money to extend those subsidies and for a president to sign it.
And I just think that the basic ACA, the stuff that passed in 2010, I think is relatively safe, as Julie says. But lots of people are going to face much more expensive insurance and maybe unaffordable insurance. And again, the CBO [Congressional Budget Office] projects that a lot of people will end up giving up their insurance as a result of those changes if these policies are allowed to expire. And so I don’t know. I think we don’t see candidates talking about it very much. But I don’t actually think it’s that hard to message on. You could just say, “If you vote for this guy, your insurance premiums are going to go up by 50% or whatever.”
That doesn’t seem like a terrible message. So I do wonder if we’ll see more of that, particularly as we get closer to the election. Because it does feel like a real pocketbook issue for people. The cost of health care, the cost of health insurance, like the cost of drugs, I think, is something that really weighs on people. And we’ve seen in these last few years that making insurance cheaper has just made it much more appealing, much more accessible for people. There’s lots more Americans who have health insurance now, and that’s at risk of going away.
Rovner: Well, also on the list of things that are likely to come up, probably not in the presidential race, but certainly lower down on the ballot, is gender-affirming care. Republicans are right now are all about parental control over what books their children read and what they’re taught in school, but not apparently about medical care for their children.
They want that to be determined by lawmakers. This is very much a wedge issue, but I’m wondering for which side. I mean, traditionally, it would’ve been the conservatives and the evangelicals sort of pushing on this. But as abortion has sort of flip-flopped in importance among voters, I’m wondering where this kind of falls into that.
Raman: I think that the messaging that I’ve seen so far has still prominently been from Republicans on this issue. Whether or not it’s bills that they’ve been introducing and kind of messaging on in Congress or just even in the ads, there’s still been a lot of parental safeguards and the language related to that with relation to gender-affirming care. I have not actually seen as many Democratic ads going super into this. I think they have been way more focused on abortion.
I’m thinking back to, I saw a statistic that 1 in 4 Democratic ads go into abortion, which is really high compared to previous years. And so I don’t know that it will be as big of an issue. I even see some people kind of playing it down because the more attention it gets, sometimes it rallies people up, and they don’t… It’s kind of the flip of Republicans not wanting to bring attention to the abortion issue. And I think a lot of Democrats are trying to shy away so that some of these things aren’t elevated, that we aren’t talking about some of the talking points and the messaging that Republicans are bringing up on the same thing.
Sanger-Katz: Yeah, it feels to me almost like a mirror image of the abortion issue in the sense that the Democrats have this challenge where their activists are out in front of their voters. There clearly are parts of the Democratic coalition that are really concerned about transgender rights and wanting to protect them and are very opposed to some of the action that we’re seeing at the state and local level, both in terms of what’s happening in schools, but also regulation of medical care. But I think voters I think are less comfortable with transgender rights.
Even Democratic voters, you see sort of there’s more of a generational split on this issue than on some of these other issues where I think older voters are just a little bit less comfortable. And so I do think that it is an issue where — particularly certain parts of it like transgender athletes — that seems to be an area where you see the Republican message really getting more traction among certain subsets of Democratic voters. And I think it’s a hard issue for Democrats except in the places where there’s really broad acceptance.
Rovner: So I want to move on to the things that are less likely to come up, but probably should. We’re going to start with Medicaid. During the pandemic, it grew to cover over 90 million Americans. That’s like a third more than Medicare, which most people still think of as the largest government health program.
But as states pare back their roles after the expiration of the public health emergency, it seems that lots of people — particularly children, who are still eligible — are getting dropped nonetheless. During the fight over repealing the Affordable Care Act in 2017, it was the fate of Medicaid in large part that saved the program.
Suddenly, people realized that their grandmother was getting Medicaid and that one out of every three births, maybe one of every two births, is paid for by Medicaid. But now it seems not so much. Has Medicaid gotten invisible again in national politics?
Raman: I think, in a way, it has. I mean, it doesn’t mean that it’s any less important, but I haven’t seen as big of a push on it, as many people talking about it. And I think it is more of a tricky thing to message on at this point, given that if you look at where the states that have been disenrolling a lot of people, a lot of the ones that are near the top, are blue states.
California is a bigger population, but it’s also the one where they’ve disenrolled the most people. And so messaging on this is going to be difficult. It’s a harder thing to kind of attack your opponent on if this is something that is also being … been difficult in your state. It’s something that states have been grappling with even before we even got to this point.
Sanger-Katz: I think this is another issue where, I think, the stakes of the election are actually quite high. I do think it’s relatively invisible as an issue. I think part of the reason is that we don’t really see the Republicans talking about it, and I think the Democrats don’t really know how to message on it. I think they were really good at, “We’re going to protect you. We’re going to prevent the Republicans from taking this away from you.” But I think they don’t have a good affirmative message about, “How we love this program and we want to support and extend it.”
I don’t think voters are really responding to that. But if you look at what President Trump did in his first administration, he had budgets every single year that proposed savage cuts to Medicaid, big changes to the structure and funding of the program. Those did not get enacted into law. But even after Obamacare repeal was abandoned, you did not see the Trump budgets and the Trump administration, economic officials and health officials, abandoning those plans to make significant cuts to Medicaid.
And I think there are quite a lot of people in the Republican health policy world who think that Medicaid is sort of a bloated and wasteful program that needs to be rethought in a kind of fundamental way, needs to be handed back to the states to give them more fiscal responsibility and also more autonomy to run the program in their own way. I think we will see that again. I also think it’s very hard to know, of course, I feel like anytime… whoever’s in power is always less concerned about the deficit than they are when they are running for election.
But something we haven’t talked about because it’s not a health care issue, is that the expiration of the Trump tax reform bill is going to come up next year, and all of our budget projections that we rely on now assume that those tax cuts are going to expire. I think we all know that most of them probably are not going to expire regardless of who is elected. But I think if Trump and the Republicans take power again, they’re going to want to do certainly a full renewal and maybe additional tax cuts.
And so I think that does put pressure, fiscal pressure on programs like Medicaid because that’s one of the places where there’s a lot of dollars that you could cut if you want to counterbalance some of the revenues that you’re not taking in when you cut taxes. I think Medicaid looks like a pretty ripe target, especially because Trump has been so clear that he does not want to make major cuts to Medicare or to Social Security, which are kind of the other big programs where there’s a lot of money that you could find to offset major tax cuts if you wanted to.
Rovner: Yet, the only big program left that he hasn’t promised not to cut, basically. I guess this is where we have to mention Project 2025, which is this 900-page blueprint for what could happen in a second Trump term that the Trump campaign likes to say, whenever something that’s gets publicized that seems unpopular, saying, “It doesn’t speak for us. That’s not necessarily our position.”
But there’s every suggestion that it would indeed be the position of the Trump administration because one of the pieces of this is that they’re also vetting people who would be put into the government to carry out a lot of these policies. This is another one that’s really hard to communicate to voters but could have an enormous impact, up and down, what happens to health.
Sanger-Katz: And I think this is true across the issue spectrum that I think presidential candidates, certainly congressional candidates and voters, tend to focus on what’s going to happen in Congress. What’s the legislation that you’re going to pass? Are you going to pass a national abortion ban, or are you going to pass a national protect-abortion law? But actually, most of the action in government happens in regulatory agencies. There’s just a ton of power that the executive branch has to tweak this program this way or that.
And so on abortion, I think there’s a whole host of things that are identified in that Project 2025 report that if Trump is elected and if the people who wrote that report get their way, you could see lots of effects on abortion access nationwide that just happened because the federal agencies change the rules about who can get certain drugs or how things are transported across state lines. What happens to members of the military? What kind of funding goes to organizations that provide contraception coverage and other related services?
So, in all of these programs, there’s lots of things that could happen even without legislation. And I think that always tends to get sort of undercovered or underappreciated in elections because sort of hard to explain, and it also feels kind of technical. I think, speaking as a journalist, one thing that’s very hard is that this Project 2025 effort is kind of unprecedented in the sense that we don’t usually have this detailed of a blueprint for what a president would do in all of these very detailed ways. They have, I mean, it’s 100…
Rovner: Nine-hundred …
Sanger-Katz: … 900-page document. It’s like every little thing that they could do they’ve sort of thought about in advance and written down. But it’s very hard to know whether this document actually speaks for Trump and for the people that will be in leadership positions if he’s reelected and to what degree this is sort of the wish casting of the people who wrote this report.
Rovner: We will definitely find out. Well, kind of like Medicaid, the opioid crisis is something that is by no means over, but the public debate appears to have just moved on. Do we have short attention spans, or are people just tired of an issue that they feel like they don’t know how to fix? Or the fact that Congress threw a lot of money at it? Do they feel like it’s been addressed to the extent that it can be?
Raman: I think this is a really difficult one to get at because it’s — at the same time where the problem has been so universal across the country — it has also become a little fragmented in terms of certain places, with different drugs becoming more popular. I think that, in the past, it was just so much that it was the prescription opioids, and then we had heroin and just different things. And now we have issues in certain places with meth and other drugs. And I think that some of that attention span has kind of deviated for folks. Even though we are still seeing over 100,000 drug-related deaths per year; it hasn’t dipped.
And the pandemic, it started going up again after we’d made some progress. And I’m not sure what exactly has shifted the attention, if it’s that people have moved on to one of these other issues or what. But even in Congress, where there have been a lot of people that were very active on changing some of the preventative measures and the treatment and all of that, I think some of those folks have also left. And then when there’s less of the people focused on that issue, it also just slowly trickles as like a less-hyped-up issue in Congress.
Sanger-Katz: I think it continues to be an issue in state and local politics. In certain parts of the country I think this is a very front-of-mind issue, and there’s a lot of state policy happening. There’s a lot also happening at the urban level where you’re seeing prosecutors, mayors, and others really being held accountable for this really terrible problem. And also with the ancillary problems of crime and homelessness associated with people who are addicted to drugs. So, at the federal level, I agree, it’s gotten a little bit sleepy, but I think in certain parts of the country, this is still a very hot issue.
And I do think this is a huge, huge, huge public health crisis that we have so many people who are dying of drug overdoses and some parts of the country where it is just continuing to get worse. I will say that the latest data, which is provisional, it’s not final from the CDC [Centers for Disease Control and Prevention], but it does look like it’s getting a little bit better this year. So it’s getting better from the worst ever by far. But it’s the first time in a long time that overdoses seem to be going down even a little. So I do think there’s a glimmer of hope there.
Raman: Yeah. But then the last time that we had that, it immediately changed again. I feel like everyone is just so hesitant to celebrate too much just because it has deviated so much.
Sanger-Katz: It’s definitely, it’s a difficult issue. And even the small improvements that we’ve seen, it’s a small improvement from a very, very large problem, so.
Rovner: Well, speaking of public health, we should speak of public health. We’re still debating whether or not covid came from a wet market or from a lab leak, and whether Dr. [Anthony] Fauci is a hero or a villain. But there seems to be a growing distrust in public health in general. We’ve seen from President Trump sort of threatened to take federal funds away from schools with vaccine mandates.
The context of what he’s been saying suggests he’s talking about covid vaccines, but we don’t know that. This feels like one of these issues that, if it comes up at all, is going to be from the point of view of do you trust or do you not trust expertise? I mean, it is bigger than public health, right?
Raman: Yeah. I think that… I mean, the things that I’ve seen so far have been largely on the distrust of whether vaccines are just government mandates and just ads that very much are aligning with Trump that I’ve seen so far that have gone into that. But it does, broader than expertise.
I mean, even when you go back to some of the gender-affirming care issues, when we have all of the leading medical organizations that are experts on this issue speaking one way. And then we having to all of the talking points that are very on the opposite spectrum of that. It’s another issue where even if there is expertise saying that this is a helpful thing for a lot of folks that it’s hard to message on that.
Sanger-Katz: And we also have a third-party candidate for the presidency who is, I think, polling around 10% of the electorate — and polling both from Democratic and Republican constituencies — whose kind of main message is an anti-vaccine message, an antipublic health message.
And so I think that reflects deep antipublic health sentiments in this country that I think, in some ways, were made much more prominent and widespread by the covid pandemic. But it’s a tough issue for that reason.
I think there is a lot of distrust of the public health infrastructure, and you just don’t see politicians really rushing into defend public health officials in this moment where there’s not a crisis and there’s not a lot of political upside.
Rovner: Finally, I have a category that I call big-picture stuff. I feel like it would be really refreshing to see broad debates over things like long-term care. How we’re going to take care of the 10,000 people who are becoming seniors every day. The future solvency of Medicare. President Trump has said he won’t cut Medicare, but that’s not going to help fix the financial issues that still ail at end, frankly, the structure of our dysfunctional health care system.
Everything that we’ve talked about in terms of drug prices and some of these other things is just… are all just symptoms of a system that is simply not working very well. Is there a way to raise these issues, or are they just sort of too big? I mean, they’re exactly the kinds of things that candidates should be debating.
Raman: That is something that I have been wondering that when we do see the debate next week, if we already have such a rich background on both of these candidates in terms of they’ve both been president before, they have been matched up before, that if we could explore some of the other issues that we haven’t had yet. I mean, we know the answers to so many questions. But there are certain things like these where it would be more refreshing to hear some of that, but it’s unclear if we would get any new questions there.
Rovner: All right. Well, I have one more topic for the panel, and then I’m going to turn it over to the audience. There are folks with microphones, so if you have questions, be thinking of them and wait until a microphone gets to you.
One thing that we haven’t really talked about very much, but I think it’s becoming increasingly important, is data privacy in health care. We’ve seen all of these big hacks of enormous storages of people’s very personal information. I get the distinct impression that lawmakers don’t even know what to do. I mean, it’s not really an election issue, but boy, it almost should be.
Sanger-Katz: I did some reporting on this issue because there was this very large hack that affected this company called Change Healthcare. And so many things were not working because this one company got hacked. And the impression I got was just that this is just an absolute mess. That, first of all, there are a ton of vulnerabilities both at the level of hospitals and at the level of these big vendors that kind of cut across health care where many of them just don’t have good cybersecurity practices.
And at the level of regulation where I think there just aren’t good standards, there isn’t good oversight. There are a lot of conflicting and non-aligned jurisdictions where this agency takes care of this part, and this agency takes care of that part. And I think that is why it has been hard for the government to respond, that there’s not sort of one person where the buck stops there. And I think the legislative solutions actually will be quite technical and difficult. I do think that both lawmakers and some key administration officials are aware of the magnitude of this problem and are thinking about how to solve it.
It doesn’t mean that they will reach an answer quickly or that something will necessarily pass Congress. But I think this is a big problem, and the sense I got from talking to experts is this is going to be a growing problem. And it’s one that sounds technical but actually has pretty big potential health impacts because when the hospital computer system doesn’t work, hospitals can’t actually do the thing that they do. Everything is computerized now. And so when there’s a ransomware attack on a main computer electronic health record system, that is just a really big problem. That there’s documentation has led to deaths in certain cases because people couldn’t get the care that they need.
Rovner: They couldn’t … I mean, couldn’t get test results, couldn’t do surgeries. I mean, there was just an enormous implications of all this. Although I did see that there was a hack of the national health system in Britain, too. So, at least, that’s one of the things that we’re not alone in.
Sanger-Katz: And it’s not just health care. I mean, it’s like everything is hackable. All it takes is one foolish employee who gives away their password, and you think, often, the hackers can get in.
Raman: Well, that’s one of the tricky parts is that we don’t have nationally, a federal data privacy law like they do in the E.U. and stuff. And so it’s difficult to go and hone in on just health care when we don’t have a baseline for just, broadly … We have different things happening in different states. And that’s kind of made it more difficult to get done when you have different baselines that not everyone wants to come and follow the model that we have in California or some of the other states.
Rovner: But apparently Change Healthcare didn’t even have two-factor authentication, which I have on my social media accounts, that I’m still sort of processing that. All right, so let’s turn it over to you guys. Who has a question for my esteemed panel?
[Audience member]: Private equity and their impact on health care.
Rovner: Funny, one of those things that I had written down but didn’t ask.
Sanger-Katz: I think this is a really interesting issue because we have seen a big growth in the investment of private equity into health care, where we’re seeing private equity investors purchasing more hospitals, in particular, purchasing more doctors’ practices, nursing homes. You kind of see this investment across the health care sector, and we’re just starting to get evidence about what it means. There’s not a lot of transparency currently. It’s actually pretty hard to figure out what private equity has bought and who owns what.
And then we really don’t know. I would say there’s just starting to be a little bit of evidence about quality declines in hospitals that are owned by private equity. But it’s complicated, is what I would say. And I think in the case of medical practices, again, we just don’t have strong evidence about it. So I think policymakers, there are some who are just kind of ideologically opposed to the idea of these big investors getting involved in health care. But I think there are many who are… feel a little hands-off, where they don’t really want to just go after this particular industry until we have stronger evidence that they are in fact bad.
Rovner: Oh, there’ve been some pretty horrendous cases of private equity buying up hospital groups, selling off the underlying real estate. So now that the… now the hospital is paying rent, and then the hospitals are going under. I mean, we’ve now seen this.
Sanger-Katz: Yeah, there’s… No, there’s… There have clearly been some examples of private equity investments in hospitals and in nursing homes that have led to really catastrophic results for those institutions and for patients at those places. But I think the broader question of whether private equity as a structure that owns health care entities is necessarily bad or good, I think that’s what we don’t know about.
Rovner: Yeah, I mean, there’s an argument that you can have the efficiencies of scale, and that there may be, and that they can bring some business acumen to this. There are certainly reasons that it made sense when it started. The question is what the private equity is in it for.
Is it there to try to support the organization? Or is it there to do what a lot of private equity has done, which is just sort of take the parts, pull as much value as you can out of them, and discard the rest, which doesn’t work very well in the health care system.
Sanger-Katz: I also think one thing that’s very hard in this issue — and I think in others that relate to changes in the business structure of health care — is that it’s, like, by the time we really know, it’s almost too late. There’s all of this incredible scholarship looking at the effects of hospital consolidation, that it’s pretty bad that when you have too much hospital concentration; particularly in individual markets, that prices go up, that quality goes down. It’s really clear. But by the time that research was done so many markets were already highly consolidated that there wasn’t a way to go back.
And so I think there’s a risk for private equity investment of something similar happening that when and if we find out that it’s bad, they will have already rolled up so much of medical practice and changed the way that those practices are run that there’s not going to be a rewind button. On the other hand, maybe it will turn out to be OK, or maybe it will turn out to be OK in certain parts of the health care system and not in others. And so there is, I think, a risk of over-regulating in the absence of evidence that it’s a problem.
Raman: Yeah. And I would just echo one thing that you said earlier is that about the exploratory stages. Everything that I can rack my brain and think of that Congress has done on this has been very much like, “Let’s have a discussion. Let’s bring in experts,” rather than like really proposing a lot of new things to change it. I mean, we’ve had some discussion in the past of just changing laws about physician-owned practices and things like that, but it hasn’t really gone anywhere. And some of the proponents of that are also leaving Congress after this election.
Rovner: And, of course, a lot of this is regulated at the state level anyway, which is part of the difficulty.
Sanger-Katz: And there is more action at the state level. There are a bunch of states that have passed laws that are requiring more transparency and oversight of private equity acquisitions in health care. That seems to be happening faster at the state level than at the federal level.
Raman: And so many times, it trickles from the state level to the federal level anyway, too.
Rovner: Maybe the states can figure out what to do.
Sanger-Katz: Yes.
Rovner: More questions.
[Audience member]: Oh, yeah. I have a question about access to health care. It seems that for the past few years, maybe since covid, almost everybody you talked to says, “I can’t get an appointment with a doctor.” They call, and it’s like six months or three months. And I’m curious as to what you think is going on because … in this regard.
Raman: I would say part of it is definitely a workforce issue. We definitely have more and more people that have been leaving due to age or burnout from the pandemic or from other issues. We’ve had more antagonism against different types of providers that there’ve been a slew of reasons that people have been leaving while there’s been a greater need for different types of providers. And so I think that is just part of it.
Rovner: I feel like some of this is the frog in the pot of water. This has been coming for a long time. There have been markets where people have… people unable to get in to see specialists. You break your leg, and they say, “We can see you in November.” And I’m not kidding. I mean, that’s literally what happens. And now we’re seeing it more with primary care.
I mean that the shortages that used to be in what we called underserved areas, that more and more of the country is becoming underserved. And I think because we don’t have a system. Because we’re all sort of looking at these distinct pieces, I think the health care workforce issue is going kind of under the radar when it very much shouldn’t be.
Sanger-Katz: There’s also, I think, quite a lot of regional variation in this problem. So I think there are some places where there’s really no problem at all and certain specialties where there’s no problem at all. And then there are other places where there really are not enough providers to go around. And rural areas have long had a problem attracting and retaining a strong health care workforce across the specialties.
And I think in certain urban areas, in certain neighborhoods, you see these problems, too. But I would say it’s probably not universal. You may be talking to a lot of people in one area or in a couple of areas who are having this problem. But, as Julie said, I think it is a problem. It’s a problem that we need to pay attention to. But I think it’s not a problem absolutely everywhere in the country right now.
Rovner: It is something that Congress… Part of this problem is because Congress, in 1997, when they did the Balanced Budget Act, wanted to do something about Medicare and graduate medical education. Meaning why is Medicare paying for all of the graduate medical education in the United States, which it basically was at that point? And so they put in a placeholder. They capped the number of residences, and they said, “We’re going to come back, and we’re going to put together an all-payer system next year.”
That’s literally what they said in 1997. It’s now 27 years later, and they never did it, and they never raised the cap on residencies. So now we’ve got all these new medical schools, which we definitely need, and we have all of these bright, young graduating M.D.s, and they don’t have residencies to go to because there are more graduating medical school seniors than there are residency slots. So that’s something we’re… that just has not come up really in the past 10 years or so. But that’s something that can only be fixed by Congress.
Raman: And I think even with addressing anything in that bubble we’ve had more difficulty of late when we were… as they were looking at the pediatric residency slots, that whole discussion got derailed over a back-and-forth between members of Congress over gender-affirming care.
And so we’re back again to some of these issues that things that have been easier to do in the past are suddenly much more difficult. And then some of these things are felt down the line, even if we are able to get so many more slots this year. I mean, it’s going to… it takes a while to broaden that pipeline, especially with these various specialized careers.
Rovner: Yeah, we’re on a trajectory for this to get worse before it gets better. There’s a question over here.
[Audience member]: Hi. Thanks so much. I feel like everybody’s talking about mental health in some way or another. And I’m curious, it doesn’t seem to be coming at the forefront in any of the election spaces. I’m curious for your thoughts.
Raman: I think it has come up some, but not as much as maybe in the past. It has been something that Biden has messaged on a lot. Whenever he does his State of the Union, mental health and substance use are always part of his bipartisan plan that he wants to get done with both sides. I think that there has been less of it more recently that I’ve seen that them campaigning on. I mean, we’ve done a little bit when it’s combined with something like gun violence or things like that where it’s tangentially mentioned.
But front and center, it hasn’t come up as much as it has in the past, at least from the top. I think it’s still definitely a huge issue from people from the administration. I mean, we hear from the surgeon general like time and time again, really focusing on youth mental health and social media and some of the things that he’s worried about there. But on the top-line level, I don’t know that it has come up as much there. It is definitely talked about a lot in Congress. But again, it’s one of those things where they bring things up, and it doesn’t always get all the way done, or it’s done piecemeal, and so …
Rovner: Or it gets hung up on a wedge issue.
Raman: Yep.
Sanger-Katz: Although I do think this is an issue where actually there is a fair amount of bipartisan agreement. And for that reason, there actually has been a fair amount of legislation that has passed in the last few cycles. I think it just doesn’t get the same amount of attention because there isn’t this hot fight over it. So you don’t see candidates running on it, or you don’t see people that…
There’s this political science theory called the Invisible Congress, which is that sometimes, actually, you want to have issues that people are not paying attention to because if they’re not as controversial, if they’re not as prominent in the political discourse, you can actually get more done. And infrastructure, I think, is a kind of classic example of that, of something like it’s not that controversial. Everybody wants something in their district. And so we see bipartisan cooperation; we got an infrastructure bill.
And mental health is kind of like that. We got some mental health investments that were part of the pandemic relief packages. There was some mental health investment that was part of the IRA, I believe, and there was a pretty big chunk of mental health legislation and funding that passed as part of the gun bill.
So I do think there’s, of course, more to do it as a huge problem. And I think there are probably more creative solutions even than the things that Congress has done. But I think just because you’re not seeing it in the election space doesn’t mean that there’s not policymaking that’s happening. I think there has been a fair amount.
Rovner: Yeah, it’s funny. This Congress has been sort of remarkably productive considering how dysfunctional it has been in public. But underneath, there actually has been a lot of lawmaking that’s gone on, bipartisan lawmaking. I mean, by definition, because the House is controlled by Republicans and the Senate by Democrats. And I think mental health is one of those issues that there is a lot of bipartisan cooperation on.
But I think there’s also a limit to what the federal government can do. I mean, there’s things that Congress could fix, like residency slots, but mental health is one of those things where they have to just sort of feed money into programs that happen. I think at the state and local level, there’s no federal… Well, there is a federal mental health program, but they’re overseeing grants and whatnot. I think we have time for maybe one more question.
[Audience member]: Hi. To your point of a lot of change happens at the regulatory level. In Medicaid one of the big avenues for that is 1115 waivers. And let’s take aside block granting or anything else for a minute. There’s been big bipartisan progress on, including social care and whole-person care models. This is not just a blue state issue. What might we expect from a Trump administration in terms of the direction of 1115s, which will have a huge effect on the kind of opportunity space in states for Medicaid? And maybe that we don’t know yet, but I’m curious. Maybe that 900-page document says something.
Sanger-Katz: Yeah, I think that’s an example of we don’t know yet because I think the personnel will really matter. From everything that I know about President Trump, I do not think that the details of Medicaid 1115 waiver policy are something that he gets up in the morning and thinks about or really cares that much about. And so I think …
Rovner: I’m not sure it’s even in Project 2025, is it?
Sanger-Katz: I think work requirements are, so that was something that they tried to do the last time. I think it’s possible that we would see those come back. But I think a lot really depends on who is in charge of CMS [Centers for Medicare & Medicaid Services] and Medicaid in the next Trump administration and what are their interests and commitments and what they’re going to say yes and no to from the states. And I don’t know who’s on the shortlist for those jobs, frankly. So I would just put that in a giant question-mark bin — with the possible exception of work requirements, which I think maybe we could see a second go at those.
Raman: I would also just point to his last few months in office when there were a lot of things that could have been changed had he been reelected; where they wanted to change Medicaid drug pricing. And then we had some things with block grants and various things that had we had a second Trump presidency we could have seen some of those waivers come to a fruition. So I could definitely see a push for more flexibility in asking states to come up with something new that could fall for under one of those umbrellas.
Rovner: Well, I know you guys have more questions, but we are out of time. If you enjoyed the podcast tonight, I hope you will subscribe. Listen to “What the Health?” every week. You can get it wherever you get your podcast. So good night and enjoy the rest of the festival. Thanks.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 1 month ago
Aging, Elections, Health Care Costs, Health Industry, Insurance, Medicaid, Medicare, Multimedia, Public Health, Abortion, Biden Administration, KFF Health News' 'What The Health?', Podcasts, reproductive health, Trump Administration