What is POTS, the disease affecting Olympic swimmer Katie Ledecky?
After nearly a decade of keeping it under wraps, Olympic medalist Katie Ledecky has shared her POTS diagnosis with the world.
The athlete, who has won 14 Olympic medals for swimming, the most of any female Olympian, said she has POTS (postural orthostatic tachycardia syndrome).
After nearly a decade of keeping it under wraps, Olympic medalist Katie Ledecky has shared her POTS diagnosis with the world.
The athlete, who has won 14 Olympic medals for swimming, the most of any female Olympian, said she has POTS (postural orthostatic tachycardia syndrome).
In "Just Add Water: My Swimming Life," Ledecky's new memoir, which was published by Simon & Schuster in June, she wrote that the disease can cause "dizziness, fainting and exhaustion."
US OLYMPIAN SAMMY SULLIVAN SAYS ARMY SERVICE HELPED HER WIN BRONZE MEDAL FOR RUGBY
Here's more.
POTS is a disturbance in the autonomic nervous system, which controls some of the normal regulatory functions of the body, according to Dr. Blair Grubb, a cardiologist and expert on POTS at The University of Toledo College of Medicine and Life Sciences.
"When the person stands, gravity will try to displace downward roughly 20% to 30% of the body's blood volume," he told Fox News Digital.
In response to this displacement, the brain tells the heart to beat faster and more forcibly, and tells the blood vessels in the lower half of the body to tighten, or constrict, to three times the level they were previously, the doctor said.
"This allows for accumulation of much more blood than normal in the lower half of the body," Grubb said.
SLEEP DOCTORS SAY OLYMPIC ATHLETES' CARDBOARD BEDS COULD HAVE ‘DISASTROUS’ IMPACT
As more blood is displaced downward, the brain gets less and less oxygen.
Ledecky discussed this effect in her book. She wrote, "I pool blood in the vessels below my heart when I stand. My body then releases extra norepinephrine or epinephrine, which adds additional stressors on my heart, making it beat faster."
Individuals with a genetic trait called Ehlers-Danlos syndrome (also known as joint hypermobility syndrome) appear to be more susceptible to developing this condition, according to Grubb.
"However, POTS is frequently triggered by a viral infection, such as Epstein-Barr virus or COVID-19," he told Fox News Digital.
One of these infections can trigger an autoimmune response, in which the body's immune system attacks itself and produces antibodies that interfere with the ability of blood vessels to tighten, the doctor said.
POTS can also occur on its own, without any obvious triggers.
A POTS patient’s symptoms will depend on how much blood is displaced downward, experts say.
"It can vary from mild cases where your heart races and you get a little dizzy upon standing, all the way to presenting as a disabling condition, disallowing patients from being upright," Valerie Iovine, PT, a physical therapist at Strive Physical Therapy in Philadelphia, told Fox News Digital.
"It can also change over the course of life, but can also change day to day or week to week."
The disorder’s name — postural orthostatic tachycardia syndrome — literally translates to "when you become more upright, your heart races," noted Iovine, who treats many patients with POTS and also has the disorder herself.
"The heart will flutter in an attempt to properly oxygenate the brain," she said.
"But in addition to the dizziness, headaches, passing out or near passing out, many with this disorder don't realize that it can account for other issues, like temperature dysregulation, blood pressure dysregulation and GI dysfunction."
In more extreme cases, patients may have difficulty thinking, concentrating or remembering — sometimes called brain fog, according to Grubb.
WITH SOME OLYMPIC EVENTS POSTPONED, SEINE RIVER WATER QUALITY POSES CONCERNS
People may also experience blurred vision, black spots in their visual field, tunnel vision and headache.
"Even greater displacement of blood can cause the individual to lose consciousness," Grubb said.
The primary treatment for POTS is increasing water and salt intake, Grubb said.
"It is also important to recondition the patient through exercise, building the strength in their lower extremities," he said.
Some medications, such as midodrine and droxidopa — known as vasoconstrictors — can work to tighten blood vessels and increase blood return to the heart, according to Grubb.
WHAT IS ANGELMAN SYNDROME? COLIN FARRELL’S SON IS LIVING WITH THIS RARE DISEASE
Still other drugs, such as fludrocortisone or desmopressin, work by increasing the volume of fluids available for the heart to pump.
"Medications such as pyridostigmine facilitate nerve transmission and help the nervous system work more effectively to maintain normal vascular function," Grubb added.
Many often use the term "exercise intolerance" when describing symptoms of POTS, but Iovine said that "poorly prescribed and dosed exercise" is the problem.
"Exercise is the best management for POTS," she said.
"I would argue that for these patients, movement is medicine."
In her book, Ledecky noted that swimming can be an effective treatment for POTS, writing that "reclined aerobic exercise, such as swimming, and strengthening your core, can provide relief."
Seeking care from a cardiologist and a physical therapist is essential, according to Iovine.
The cardiologist can help to get vital signs like heart rate and blood pressure under control, she said, while a knowledgeable physical therapist can help to manage symptoms and increase upright tolerance.
"Things like proper hydration, extra electrolytes, and being able to keep cool can also help manage symptoms," Iovine advised.
"The heat will make the blood vessels expand, making it harder to get the blood up the head against gravity," she said.
"POTS can be a challenge for anyone — from people with complicated pre-existing conditions, all the way to the top athletes, like Katie Ledecky," Iovine told Fox News Digital.
The disease can often cause a flu-like feeling after exercise, something called post-exertional malaise/post-exertional symptom exacerbation (PEM/PESE).
"This is when the autonomic nervous system can have a reflexive reaction to stress or exercise, either making existing symptoms worse or creating a new host of issues in people with POTS," Iovine said.
"This can pose an issue in the sense of rigorous exercise for an Olympic athlete — or in other cases, exertion may be as simple as getting out of bed and walking to the kitchen."
POTS causes a "dynamic disability," Iovine noted.
"One day, it may allow you to swim like an Olympic athlete, and other days, [it will] have you stuck in bed or even in a wheelchair."
POTS is particularly challenging in athletic activities that involve frequent "start and stop" activities, such as basketball, volleyball, soccer and field hockey, added Grubb.
Both experts emphasized that POTS is a "real illness."
"People who were previously quite healthy develop severe limitations and disabilities," Grubb said.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
"They can experience disabling fatigue, exercise intolerance, heat intolerance, palpitations, lightheadedness, dizziness, fainting and brain fog."
Iovine said that due to the "invisibility" of the disease combined with the high heart rate and variability of presentations, it is often dismissed as a function of mental health.
"Patients are often turned away from proper care, made to believe it is all in their heads," she said.
"POTS is a very real condition, and the good news is that there are very real management strategies as well," Iovine went on.
For more Health articles, visit www.foxnews/health
While there is no cure for POTS, many patients are able to manage their symptoms and return to their daily activities.
Added Iovine, "Build up your care team and your confidence to advocate for your health and keep to your regimented routines for management."
11 months 2 weeks ago
Health, health-care, lifestyle, Sports, heart-health, rare-diseases, fatigue, olympics
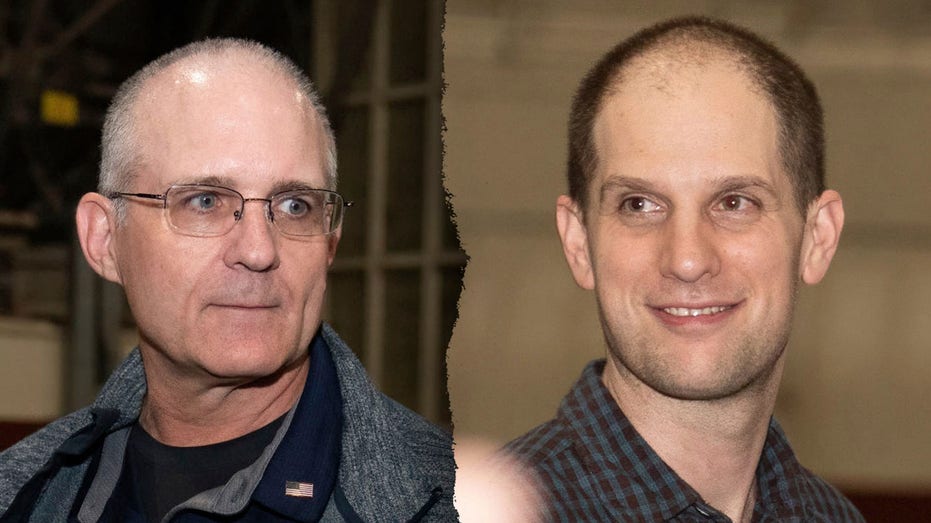
Freed American prisoners Gershkovich and Whelan may face ‘disruptive’ trauma, say mental health experts
While Thursday's release of American prisoners from Russia was marked by celebration and relief, the former captives could face future health challenges, experts say.
Wall Street Journal reporter Evan Gershkovich and American veteran Paul Whelan were among those released from Russia on Thursday in a large prisoner swap.
A third U.S. citizen, Russian-American journalist Alsu Kurmasheva, was also released.
US-RUSSIAN PRISONER EXCHANGES OVER THE YEARS: SEE THE LIST
A plane carrying the freed Americans landed at Joint Base Andrews in Maryland late Thursday night, where they were greeted by President Joe Biden and Vice President Kamala Harris.
The newly released prisoners were then flown to San Antonio, Texas, for evaluation and rehabilitation at Brooke Army Medical Center, a premier military medical facility, according to reports.
Although the prisoners are safely back on U.S. soil and have been reunited with their families, they may experience mental health challenges stemming from the trauma of detainment, said experts.
"Besides the obvious threats to one’s safety and the horrifying prospect of confinement, a situation like this is fraught with uncertainty," Dr. Norman Blumenthal, director of the Ohel Zachter Family National Trauma Center in New York, told Fox News Digital.
WSJ REPORTER EVAN GERSHKOVICH RELEASED BY RUSSIA IN PRISONER SWAP; PAUL WHELAN ALSO BEING FREED
"Ambiguity in and of itself induces stress — and that, coupled with their very predicament, can create a marked escalation of trauma." (None of the experts cited here have treated the released Americans.)
Dr. Karen DeCocker, a psychiatric mental health nurse practitioner director at Stella Centers in Chicago, noted that being held captive can lead to several types of trauma.
"This varies from person to person based on prior history and the experiences encountered during captivity," she told Fox News Digital.
While each person reacts differently to trauma, Blumenthal predicted that the freed prisoners would likely experience an "initial thrill and exhilaration" from their liberation.
"The celebrations and enthusiastic reunions with loved ones can temporarily overshadow the trauma," he noted.
"As life returns to normal and routines set in, that is often when the frightening flashbacks and intrusive recollections can become disruptive and destabilizing."
Dr. Marc Siegel, senior medical analyst for Fox News and clinical professor of medicine at NYU Langone Medical Center, said it is likely the prisoners experienced physical and mental abuse, sleep deprivation, dehydration, malnutrition and possibly infections.
Jonathan Alpert, a psychotherapist and author based in New York City, said that Gershkovich, Whelan and Kurmasheva, along with the other released prisoners, may suffer from both acute stress disorder (ASD) and post-traumatic stress disorder (PTSD).
WHAT IS PTSD? SYMPTOMS THAT CAN EMERGE AFTER EXPERIENCING A TRAUMATIC EVENT
ASD is a short-term mental health condition that typically occurs within a month after a traumatic experience, according to Cleveland Clinic’s website.
"Acute stress disorder may include flashbacks, nightmares, intense fear and high anxiety," Alpert told Fox News Digital.
It can also include feelings of numbness or detachment.
PTSD occurs when such symptoms persist for a month or longer, and the anxiety becomes chronic, according to Alpert.
FDA PANEL REJECTS MDMA-ASSISTED THERAPIES FOR PTSD DESPITE HIGH HOPES FROM VETERANS
PTSD may include many of the same symptoms as ASD, and can impair the person’s ability to function in daily activities.
The freed prisoners may also experience depression, anger and difficulty trusting others, said Alpert.
"I've also seen people have trouble focusing and making decisions in light of a trauma," he added.
It could also be challenging for the former prisoners to reintegrate into their normal environments and social groups, Alpert said.
Symptoms of trauma are "not universal," Siegel told Fox News Digital.
"There are differences, and not everyone experiences PTSD," he said.
"Common symptoms include flashbacks, nightmares, depersonalization and derealization, anxiety and depression."
DeCocker noted that symptoms can be both mental and physical — including the following five points.
"Individuals may experience dissociation, where they feel disconnected from their thoughts, feelings or sense of identity," DeCocker told Fox News Digital.
"This can manifest as feeling detached from oneself (depersonalization) or from the world around them (derealization)."
Some trauma survivors may feel a sense of guilt for having survived a traumatic experience when others did not, or for putting themselves or others in situations that led to captivity, DeCocker said.
They may also feel guilty about the stress and anxiety that family members and loved ones experienced during their imprisonment.
"Issues with trust, intimacy and personal relationships often occur with survivors and their families," DeCocker told Fox News Digital.
"The impact of their captivity often comes from their inability to relate the experience to others."
Trauma survivors may experience feelings of shame, worthlessness or confusion about their identity, according to DeCocker.
"In this case, where there was an exchange of prisoners, there may be added complexity," she said.
It's not uncommon for trauma survivors to have negative beliefs about themselves or the world, according to DeCocker.
"Generalizations about the world being unsafe or out of their control can occur," she said. "Threats are often seen in everyday experiences."
Potential physical symptoms could include chronic pain, such as headaches or muscle pain, in addition to persistent fatigue and lack of energy, according to Nikki Bishop, a licensed clinical psychologist and clinical director at SunCloud Health in Chicago.
"A person may also experience gastrointestinal issues such as stomach pain, nausea and changes in appetite," she told Fox News Digital.
"Additionally, cardiovascular risks could occur, such as increased blood pressure, heart palpitations and increased risk of heart disease."
To cope with painful feelings, people can sometimes turn to substance use, process addictions, eating disorders and even food addiction as a means of trying to numb the pain, Bishop added.
Given the high-profile release, Gershkovich and Whelan will likely receive a large amount of media attention, Alpert noted — "but it’s important that they have the space and privacy they need to process this on their own timeline."
DeCocker agreed, stressing the importance of taking extensive time to heal and recover.
"There is no rush to reintegrate," she told Fox News Digital. "Time is best devoted toward rest and restoring a sense of balance and normalcy."
Embracing daily routines and structure can help with that, DeCocker said.
The freed prisoners may also want to avoid spending too much time on social media and the news in the early days to avoid retriggering discussions and events, she advised.
One "tried-and-true method" of coping is to retell the events to supportive people who act as listeners, not solvers, according to Blumenthal.
"Putting the experience into words can help with healing and adjusting to the more mundane aspects of life and routine," he said.
If symptoms are interfering with day-to-day functioning, Alpert recommends seeking professional help.
"In the case of a severe trauma, such as being held prisoner and wrongly convicted, symptoms may not surface right away," he pointed out.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
"It can be helpful to get ahead of it and speak to a specialist."
All forms of professional help are useful, DeCocker noted. Those include talk therapy, psychiatric support, interventional treatment modalities specific to treating trauma, and physical treatments and therapies to heal the body.
Other treatments may include cognitive behavioral therapy, relaxation techniques, and medications such as beta blockers, antidepressants and potentially psychedelics, according to Siegel.
Support from loving family members and friends is also key, the doctor added.
For more Health articles, visit www.foxnews/health
Most people do have an "inherent resilience and capacity to hope," Blumental said.
"These and other freed hostages may, on their own, mobilize and harness strength and heroic reformulations of their recent incarceration to go on and resume normal functioning."
Scott McDonald of Fox News Digital contributed reporting.
11 months 3 weeks ago
mental-health, stress-and-anxiety, depression, russia, lifestyle, Health, World, ptsd
Biden cognitive health concerns: What did Kamala Harris know? Experts warn of denial dangers
A majority of voters believe that Vice President Kamala Harris knew about — and covered up — President Biden’s reported cognitive health issues.
That’s according to a YouGov/Times of London poll that surveyed 1,170 registered voters on July 22 and July 23.
A majority of voters believe that Vice President Kamala Harris knew about — and covered up — President Biden’s reported cognitive health issues.
That’s according to a YouGov/Times of London poll that surveyed 1,170 registered voters on July 22 and July 23.
Among those who believe Biden’s health issues were kept under wraps, 92% said they think the vice president was well aware of the situation.
DOCTORS REACT AFTER BIDEN'S LIVE ADDRESS TO THE NATION: A CONCERNING ‘LACK OF EMOTION'
Overall, 68% of respondents believe Biden’s decline was on Harris’ radar.
"There's no way for me to know what went through Kamala's head or what her experience has been dealing with Joe Biden," Jonathan Alpert, a psychotherapist and author based in New York City, told Fox News Digital.
"Perhaps seeing him on a regular basis made it difficult for her to pick up on any changes," said Alpert, who has not treated Biden.
"Of course, this is just speculation, and we do not know of any formal diagnosis."
Judy Gaman, CEO of Executive Medicine of Texas, a luxury medical services provider in Southlake, previously spoke with Fox News Digital about the failure of those around Biden to seek help for the president.
"Either they are in denial and have watched this take place over a period of time, so they are less sensitive to the contrast, or they are fully aware but can’t bear the thought of what happens to the family (on many levels) if Joe is no longer president," said Gaman, who also has never treated the current commander-in-chief.
Although there's long been debate about potential signs of cognitive decline, the issue came to the forefront after the June 27 presidential debate, when Biden sparked concerns with his sometimes incoherent speech and unclear train of thought on national live television.
The president, who is 81, has also appeared to "freeze" on stage during public appearances on more than one occasion.
In mid-July, Biden tested positive for COVID-19, and was said to experience upper respiratory symptoms that included "rhinorhea (runny nose) and non-productive cough, with general malaise," according to a statement on the White House's website.
On July 23, Dr. Kevin O’Connor, the president’s personal physician, released a letter stating that Biden’s symptoms had resolved and that he would "continue to be monitored for any recurrence of illness."
White House press secretary Karine Jean-Pierre has stated that Biden has seen a neurologist multiple times as part of routine health exams, but that he is not being treated for any neurological disorders.
Outside the political arena, it is common for family members and loved ones to avoid facing signs of cognitive decline and potential dementia, experts say.
"Ask any family who has dealt with Alzheimer’s, dementia or Parkinson’s, and they will tell you that what we are seeing play out [here] is classic with most families who face this," said Gaman, whose own mother struggled with Alzheimer’s disease.
"His story just happens to be playing out on the big stage," Gaman added. "Remember, everyone rallying around Biden and covering up the truth has something personal to gain by him continuing to hold office."
In some cases, Alpert noted, signs may be genuinely missed.
EARLY DEMENTIA OFTEN HAS A SURPRISING WARNING SIGN, REPORT SAYS: 'FINANCIAL CONSEQUENCES'
"Generally speaking, family members who see their loved one on a regular basis don't always pick up on the cognitive decline as perceptively as those who might just see someone on occasion," he said.
"For example, someone seeing Grandma once a year during the holiday season is more likely to pick up on a decline than if they were seeing her monthly."
That’s because cognitive decline is usually gradual in the beginning, he noted.
"Early signs might be subtle and perhaps mistaken as normal aging or stress."
In other cases, the person experiencing the decline may find ways to adapt and develop strategies to compensate for the cognitive difficulties, according to Alpert, which can make the symptoms less obvious to close family and friends.
Experts agree that a denial of someone’s cognitive decline doesn’t do the person any favors.
"If family members and close associates are in denial about a loved one's cognitive decline, it can delay diagnosis and treatment of the person," Alpert warned.
FDA APPROVES NEW DRUG FOR ALZHEIMER'S DISEASE
"Dismissing an obvious issue as ‘just a bad day’ or saying ‘everyone forgets from time to time’ doesn't help the person, and will only slow access to resources and proper management of the condition," he added.
Delaying treatment can also pose safety risks, experts agree.
"Although in the short term it might be easier to look the other way, ultimately denial leads to more stress for the loved one as the condition worsens," Alpert said.
"Sometimes, getting a proper medical diagnosis provides the clinical validation necessary for the patient to actually feel understood."
In Alpert’s practice, he said he sometimes has patients who experience a host of symptoms, but don’t know exactly what is going on.
"Once I confirm the diagnosis, they feel a bit relieved to know that their symptoms are real and part of a medical or psychological disorder, and not just made up," he said.
In Biden’s case, denial of a possible cognitive disorder isn’t just dangerous for the president, but also for the country as a whole, experts say.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
If Biden is experiencing cognitive decline, failure to get him the medical attention he needs could be putting his health in danger, according to Gaman.
"From the standpoint of the country, we need to address this as a health crisis and not a political crisis," she said.
Gaman also noted that if Biden does have one of these conditions, he may not understand the need to ask for help.
"This is a prime opportunity to increase funding for research, raise awareness and encourage others dealing with this to come out of denial."
Gaman noted that she is not claiming to diagnose the president, but rather asking that the country open up the discussion on neurodegenerative disease, "especially since it’s on the rise."
Fox News Digital reached out to the Harris campaign requesting comment but did not receive a response.
For more Health articles, visit www.foxnews/health
In response to earlier outreach from Fox News Digital, the White House press office said that "health was not a factor" in Biden's decision to withdraw from the 2024 presidential race.
"He looks forward to finishing his term and delivering more historic results for the American people," the White House said in its statement.
11 months 3 weeks ago
Health, alzheimers, geriatric-health, health-care, joe-biden, biden-cover-up, presidential, lifestyle, kamala-harris
Joe Biden's health: Leadership ability questions mount as Oval Office speech gave no reason for exiting race
During a live address on Wednesday night, President Biden spoke of his decision to exit the 2024 race, endorsed Vice President Kamala Harris for the Democratic nomination, and announced his intent to stay in office for the rest of his term, which is 178 days at this point.
During a live address on Wednesday night, President Biden spoke of his decision to exit the 2024 race, endorsed Vice President Kamala Harris for the Democratic nomination, and announced his intent to stay in office for the rest of his term, which is 178 days at this point.
He did not, however, mention his health status or his recent COVID battle.
Dr. Kevin O’Connor, Biden’s personal physician, told reporters on Thursday that Biden’s health and mental cognition were both "excellent," yet some experts have been expressing concerns that remaining in office could take a physical and mental toll on the president.
DOCTORS REACT AFTER BIDEN'S LIVE ADDRESS TO THE NATION: A CONCERNING 'LACK OF EMOTION'
Here's what some doctors are saying.
Health experts said the high-pressure nature of the presidency could pose "significant health risks" for Biden, who has recently displayed signs of cognitive challenges.
"I am definitely concerned about the stress, and am worried he could be depressed while apparently continuing to fail cognitively," Dr. Marc Siegel, clinical professor of medicine at NYU Langone Medical Center and a Fox News medical contributor, told Fox News Digital on Thursday.
He has not treated Biden.
He also said, "I am furious that the White House is in denial mode and is not giving us any details, and that the White House doctor is not coming forward," adding that he "feels compassion" for the president.
BIDEN HEALTH CONCERNS PERSIST AS HE MAKES FIRST APPEARANCE AFTER ENDING CAMPAIGN
Dr. Brett Osborn, a Florida neurosurgeon and longevity expert, reiterated that the "immense, demanding and relentless" stress of the presidency can significantly impact physical and cognitive health.
"For President Biden, who has a history of cognitive issues, the toll of such stress is particularly concerning," he told Fox News Digital, expressing his professional opinion. Osborn has not examined or treated the president.
Stress can worsen cognitive issues by causing a spike in cortisol, the primary stress hormone, Osborn said.
"Prolonged exposure to high cortisol levels can accelerate the deterioration of brain regions, such as the frontal and temporal lobes, which are crucial for cognitive functions like memory, decision-making and impulse control," he said.
"This suggests that the demanding nature of the presidency could further accelerate any existing cognitive decline in President Biden, potentially diminishing his ability to fulfill the complex and high-stakes responsibilities of his office."
AFTER BIDEN DROPS OUT OF RACE, DOCTORS REVEAL WHY THE DECISION MAY HAVE BEEN BEST FOR HIS HEALTH
Dr. Earnest Lee Murray, a board-certified neurologist at Jackson-Madison County General Hospital in Jackson, Tennessee, also surmised that in the presence of any type of dementia, it may be more difficult to process stressors and handle stressful situations, which can lead to worsening cognitive abilities.
"In the long run, this can affect overall physical health," Murray told Fox News Digital.
Even with cognitively healthy presidents, Murray said, the high-pressure job has been known to have physical ramifications. (Murray and other doctors referenced here have not treated Biden.)
"If you look through presidential history, [you can] compare pictures of presidents at the beginning of their term to pictures of them at the end of their term," he said.
"It's obvious that the aging process has likely occurred at a faster rate than the normal population due to the immense pressure and stress the presidency brings on a daily basis," he also said.
"This would be accentuated in someone with cognitive limitations."
Although continued public scrutiny could also lead to increased stress, the fact that Biden has bowed out of the presidential race means that a significant stressor in his life has been eliminated, according to Jonathan Alpert, a psychotherapist and author based in New York City.
"Biden might actually feel a bit of relief now that he has stopped running for president," he told Fox News Digital.
"The intense pressure and stress from constant attacks by the opposing side and scrutiny from within his own party will be lessened significantly, and he will likely be better able to focus on his role and responsibilities," Alpert added.
Doctors who shared professional opinions with Fox News Digital agreed that in their view, Biden should receive ongoing medical care and monitoring.
"Given the noticeable decline in the president's health, my hope would be that he is closely monitored by his physician and that the team brings in any experts necessary to properly evaluate any new issues that might arise in coming months," Alpert said.
"President Biden should be given full treatment and support that's honest and transparent, as the remainder of his term plays out."
Neurologist Murray said that a patient of his with a certain degree of dementia "needs fairly consistent supervision."
He added, "I would not recommend making large financial decisions or higher-level executive decisions without advice from family members who are looking out for the best interests of the patient."
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
It is essential that the president receives appropriate medical care and stress management for the remainder of his term, Osborn said.
"While President Biden's commitment to serving his country is commendable, the potential health risks associated with continuing in such a high-pressure role cannot be ignored," the neurosurgeon said.
It is crucial for Biden to prioritize health and well-being, according to Osborn, even if it means stepping back from demanding roles.
Healthy lifestyle behaviors — such as daily exercise, stress management, and proper nutrition and supplements — are also important, he advised, as well as a "robust support system of professionals, including a neurologist who specializes in Alzheimer’s disease and Parkinson’s disease and a physical therapist."
"These are crucial steps in maintaining his health and, by extension, the effective governance of the nation, which he otherwise places at extreme risk," Osborn added.
For more Health articles, visit www.foxnews/health
In response to earlier outreach from Fox News Digital, the White House press office said that "health was not a factor" in the president's decision to withdraw from the 2024 race.
"He looks forward to finishing his term and delivering more historic results for the American people," the White House said in its statement.
12 months 3 days ago
Health, joe-biden, presidential, biden-brink, biden-cover-up, geriatric-health, lifestyle, wellness, white-house
‘Reversing’ Alzheimer’s: Here are exercises to make the brain more resilient
Can Alzheimer’s disease be reversed?
Dr. Heather Sandison, a renowned expert in Alzheimer’s disease and related dementia care, believes that reversal isn’t just possible — but that it’s already happening in multiple patients.
Can Alzheimer’s disease be reversed?
Dr. Heather Sandison, a renowned expert in Alzheimer’s disease and related dementia care, believes that reversal isn’t just possible — but that it’s already happening in multiple patients.
In her new book "Reversing Alzheimer's: The New Tool Kit to Improve Cognition and Protect Brain Health," which was published by HarperCollins on June 11, Sandison — who is based in California — offers a step-by-step guide to helping Alzheimer’s patients improve their overall brain health.
NEW ALZHEIMER’S TREATMENT ACCELERATES REMOVAL OF PLAQUE FROM THE BRAIN IN CLINICAL TRIALS
One of the core elements of Sandison’s program is a focus on exercise as one of the most important lifestyle factors in preventing and controlling dementia.
Research has shown that physical activity can reduce the likelihood and progression of Alzheimer’s.
In the excerpt below, Sandison offers some specific recommendations for the types of exercise that can benefit patients living with the disease.
Dr. Heather Sandison: Need a new motivation to be active? Exercise is medicine for the brain and provides an amazing array of benefits.
Most obviously, exercise increases blood flow throughout the body, including to the brain. That means getting your body moving will deliver more oxygen and nutrients to your brain while also flushing away more waste products.
Exercise also strengthens the heart and cardiovascular system, which helps improve blood flow even when you’re not working out; it also reduces the risk of arterial plaques that might disrupt blood flow to the brain and contribute to dementia.
ALL ABOUT ALZHEIMER'S DISEASE: SIGNS, SYMPTOMS AND STAGES
The overarching reason that exercise is such a powerful health protector is that it is what’s known as a hormetic, or a beneficial stressor.
Basically, when you put your body through its paces, the body is forced to use up resources, and your tissues can even be broken down a bit. (That’s what happens when you lift weights: Your muscles tear a tiny bit.)
In that sense, you’re introducing stress to your system, but that stress is a force for good, because it triggers your body to get more efficient at using its resources and your tissues to grow back even stronger. In other words, exercise makes your body — including your brain — more resilient.
Exercise benefits several of the root causes of neurological disease.
It improves structure by increasing your cardiovascular capacity and boosting circulation, which delivers oxygen and nutrients to the brain.
It reduces stress in multiple ways — by giving you an outlet to blow off steam, by producing feel-good hormones such as endorphins and lowering the stress hormone cortisol, and, depending on what kind of exercise you choose, getting you outside and into nature, which is a well-known stress reliever.
It can also be social, and a great way to spend time with friends or even meet new people, which helps address the loneliness and social isolation that The Lancet lists as one of the modifiable risk factors for Alzheimer’s disease.
It improves sleep by tiring you out.
It strengthens immune function, which reduces the risk and effects of infection — all those muscular contractions and moving against gravity improves the flow of lymphatic fluid, which delivers immune cells and flushes away invader cells.
It promotes detox, both through increased circulation and through sweating.
It improves signaling, as challenging and strengthening your muscles triggers the release of multiple signaling molecules, known as exerkines, that have demonstrated neuroprotective functions.
If you do only one thing: Change up your current exercise routine in a way that challenges your brain and amps up the intensity.
If you are a devoted walker, find a new route that includes hills or stairs. If you’re open to trying something different, check out a new exercise class that you’ve been meaning to try.
There are four types of exercise that you want to prioritize. Four may sound like a lot, but they are not mutually exclusive.
You can combine at least two types of exercise in one session — you can turn strength training into cardio by performing your strength moves in high-intensity intervals, or you can make your cardio dual task by doing something that requires your mental focus while you move.
Aerobic exercise is what we think of as "cardio" — it gets your heart and blood pumping and includes forms of exercise such as walking, jogging, biking, dancing and swimming.
Aerobic exercise strengthens your heart, and what’s good for your heart is also good for your brain, because your heart sends the brain the blood, oxygen, and nutrients that your brain relies on to function.
EXPERIMENTAL ALZHEIMER’S DRUG GETS FDA ADVISORY PANEL'S THUMBS-UP: ‘PROGRESS IS HAPPENING’
Your first goal with adding more exercise to your life is to get 150 to 200 minutes of aerobic exercise each week so that you get your heart rate into the vigorous zone of 70-85% of maximum heart rate.
Listening to your body and adjusting your intensity level based on your perceived exertion is one of the best ways to know if you are pushing yourself hard enough.
Strength training — also known as resistance training — is just what it sounds like: using weights or other forms of resistance to build muscle tissue.
Building muscle — particularly in the big muscle groups of the legs, hips, and torso — is directly related to brain health, because these muscles generate brain-derived neurotrophic factor (BDNF), a "fertilizer" for the brain, cueing it to create new neuronal connections and promoting neuroplasticity.
You want to aim for at least two strength-training sessions per week. Strength training doesn’t have to involve your standard barbells and bench pressing your body weight.
You can use resistance bands, light dumbbells, or even the weight of your own body in exercises like squats, lunges and planks.
Even climbing stairs or hills counts as strength training and cardio in one activity, because they get your heart rate up as they also keep the muscles of the legs and hips strong.
This next-level form of exercise combines physical movement with a cognitive challenge. The simplest form of this is walking and talking.
What is a cognitive challenge will vary from person to person, but if you’re in prevention mode, listening to a foreign language lesson or a nonfiction book while you walk outside or ride the stationary bike, and then pausing the recording to recap what you’ve just learned every few minutes, is a good option.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
For some people, going to a Pilates or yoga class or other class where you really have to pay attention to the teacher’s cues constitutes dual-task training — but not if it’s something you’ve been doing for long enough that you can zone out.
And if you have already started experiencing measurable cognitive decline, dual-task training may look like going on a walk while pointing out the names of the plants that you pass along the way, or having someone quiz you on the names of family members, or recalling family stories or important dates.
Wherever you are, you want to be working right on your edge — you can almost feel the wheels of your brain turning in order to stay focused.
This relatively unique form of training alternates the amount of oxygen in the air you breathe as you exercise — an approach that encourages the tiniest blood vessels (known as your microvasculature) throughout your body, including your brain, to open up, resulting in greatly enhanced blood flow.
It’s similar to going to altitude to train and build your aerobic capacity, and it is incredibly valuable for cognitive function.
This type of exercise does require specialized gear. You can buy the device, or go find a clinic near you where you can try it out. It does require you to wear a mask that is hooked up to a machine while you exercise, and when the oxygen saturation is low, it can be intense because you have to work harder to bring in enough air.
In other words, contrast oxygen therapy is not for everyone. But if you are willing and able, it can be dramatically helpful.
For more Health articles, visit www.foxnews/health
Honestly, exercise is such a powerful health intervention that if we could just bottle it, we could probably get rid of chronic disease.
Exercise does take time and effort, but making this one activity a regular part of your life addresses so many causal factors of dementia that it can profoundly reduce your risk.
Excerpted with permission from the new book, "Reversing Alzheimer's: The New Tool Kit to Improve Cognition and Protect Brain Health" (HarperCollins) by Dr. Heather Sandison, copyright © 2024 by Dr. Heather Sandison. All rights reserved.
1 year 1 month ago
Health, alzheimers, mental-health, healthy-living, lifestyle, wellness, Fitness, fitness-and-wellbeing, lifestyle-books
Michigan mom: ‘I had a stroke at 39 — and the warning signs weren’t what you’d expect’
Jenna Gibson was just 39 when she was training for a marathon five years ago — but her plans were cut short by a stroke that almost took her life.
Jenna Gibson was just 39 when she was training for a marathon five years ago — but her plans were cut short by a stroke that almost took her life.
Nearly 60% of stroke deaths occur in women, according to a recent study by Mayo Clinic — and now Gibson, a Michigan mother of two, aims to help others to be more aware and prioritize their health.
"Once I learned that strokes are happening to younger people, I had to share my story," she told Fox News Digital.
5 WOMEN’S HEALTH TIPS TO PREVENT AND DETECT STROKES, ACCORDING TO CARDIOLOGISTS
"In most cases, strokes are preventable if you know what to look for."
On the day of Gibson’s stroke, she was feeling great.
It was a beautiful day, she’d nailed a presentation at work, and she was enjoying a walk outside with her mother after dinner.
"We were talking about how I was training for the Detroit marathon for my 40th birthday, and then all of a sudden, out of the blue, it felt like I was hit with a ton of bricks," she told Fox News Digital.
DOG ALERTS FAMILY, SAVES TEXAS TEENAGER FROM LIFE-THREATENING STROKE: 'KEEPING GUARD'
Gibson stopped walking, then suddenly fell over into the grass.
Her mother thought she was joking at first. "She actually took a picture of me lying in the grass, saying, ‘C’mon, get up, what are you doing?’"
Her mother helped her up, but Gibson couldn’t walk straight.
"I felt like I was drunk — something just wasn't right," she said.
Even so, Gibson did not experience any of the textbook symptoms of a stroke, such as the facial droop, severe headache or vision disturbances.
They made it back home, where Gibson assumed she was having a migraine. She took some headache medicine and went to bed.
"A couple of hours later, I woke up and still didn't feel right — I couldn't get out of bed, I couldn't move," she recalled.
TIAS AND MINI-STROKE RISKS: CARDIOLOGIST SHARES WARNING SIGNS AND PREVENTION TIPS
That’s when they headed to the emergency room. Gibson’s mother told the medical team that her daughter was having trouble walking and might be having a stroke.
"They checked me over, did all the tests, and didn't see the typical signs that they would be looking for," Gibson said. "Part of it was because I was young."
She added, "I didn't have the facial droop. I could walk, although not very well. I could get some words out."
After a CT scan, the medical team decided that Gibson was likely having an optic migraine. The next morning, when she still wasn’t feeling right, the neurologist ordered another scan with contrast — and that time, the stroke finally showed up.
"They could see that there was a blockage on the left side of my brain, and I was actively having a stroke," she said.
Gibson was immediately airlifted to another hospital, where she had emergency brain surgery to remove the blood clot.
"There was obviously a risk of death — if we didn't move fast enough, the time frame would be over," she said.
As she was flown to the hospital, Gibson said she felt certain she was going to die and would never again see her husband or her daughters, who were just 8 and 4 at the time.
"I thought I’d never get to see my children grow up and get married, or that I’d have to live in some kind of vegetative state and would never work again."
"I was thinking, ‘Did I tell my girls enough times that Mommy loves them? Does my husband know how proud I am of him?’"
The next thing she knew, Gibson was waking up from surgery in the ICU — and facing a long road to recovery.
"At first, I couldn't speak at all. I couldn't move my right side. I was trapped in my head — I could see what was happening and hear people asking me questions, but I couldn't answer."
Over the next few days, Gibson said her capabilities slowly started coming back.
She received speech therapy, occupational therapy and physical therapy — and over time began to regain movement on her right side.
REPORTS REVEAL THE RISK FOR STROKES IS ON THE RISE IN YOUNG ADULTS
Her first "assignment" was to tell her daughters that she loved them and that "Mommy’s going to be OK."
After a couple of weeks, Gibson returned home and continued with outpatient therapy for three hours a day, three days a week for a four-month period.
"It was during the first six weeks that we saw the quickest improvement, and then after that, it was slower and slower," she said.
"I had to relearn everything. And now, by the grace of God, I can do all the things."
Today, Gibson is still completely numb on the entire right side of her body. She also still sometimes struggles with finding the right words while speaking, she said, especially when she’s tired or stressed.
"But if you saw me, I look like a normal person," she said.
And in a full-circle moment, Gibson was finally able to complete the half-marathon last October.
Dr. Annie Tsui, chief of neurology at Access TeleCare, who is based in Texas, emphasized the prevalence of strokes among women and urged awareness.
"Strokes can occur for various reasons across different age groups and genders," Tsui, who was not involved in Gibson’s care, told Fox News Digital. "Even though strokes can occur at any age, women between the ages of 20 and 39 are at twice the risk compared to men."
While the primary risk factors for stroke are high blood pressure, high cholesterol, heart disease, obesity and diabetes, the causes for strokes in younger age groups differ from those typically associated with older people, Tsui noted.
Those may include cardiac issues, blood clotting disorders, genetic predispositions, vascular abnormalities or trauma.
"Although no one is completely immune to the risk of stroke, individuals at higher risk should work with their doctor to develop a prevention plan," Tsui advised. "In general, maintaining a healthy lifestyle is crucial, as up to 80% of strokes can be prevented."
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
It's crucial to be aware of the symptoms to receive treatment as quickly as possible, according to Tsui.
She recommends using the FAST acronym, shown below, as a convenient tool for identifying stroke indicators.
"The chances of survival and positive outcomes are highest when the patient receives prompt medical attention," Tsui told Fox News Digital.
Some stroke treatments are only effective if administered within three hours of when symptoms begin, she warned — with the risk of permanent brain damage or death rising with each passing minute.
"It's important to be vigilant in recognizing stroke symptoms and to seek medical assistance immediately at the first sign," Tsui said.
"Every second counts in reducing the risk of brain injury, permanent disability or even death."
1 year 1 month ago
Health, stroke, womens-health, health-care, lifestyle, family, parenting, medical-tech
Melanoma patients reveal dramatic stories for Skin Cancer Awareness Month: ‘I thought I was careful’
Skin cancer is the most common type of cancer in the U.S. — with one in five Americans developing the disease by the age of 70.
Melanoma is the deadliest form of skin cancer, expected to take the lives of more than 8,200 people in the U.S. this year.
Skin cancer is the most common type of cancer in the U.S. — with one in five Americans developing the disease by the age of 70.
Melanoma is the deadliest form of skin cancer, expected to take the lives of more than 8,200 people in the U.S. this year.
This May, for Skin Cancer Awareness Month, two melanoma patients are sharing their stories of how they overcame this invasive form of the disease.
SKIN CANCER CHECKS AND SUNSCREEN: WHY THESE (STILL) MATTER VERY MUCH FOR GOOD HEALTH
One even wrongly assumed that what she was experiencing "was just a normal part of aging and sun exposure." Here's what others can learn.
Melanoma is a type of skin cancer that starts in the melanocytes, which are the cells that produce the skin’s pigmentation (color).
Most cases — but not all — are caused by exposure to ultraviolet light. Melanoma can affect people of all skin tones and types.
"Melanoma is one of the most common type of cancer in younger patients," Nayoung Lee, M.D., assistant professor of dermatology at NYU Langone Health, told Fox News Digital.
The prognosis is "very good" when melanoma is detected early, but the survival rate falls steeply when it is detected at a more advanced stage, she noted.
"Melanoma can spread through the bloodstream to your lymph nodes and distant organs, so it is crucial to do regular skin exams to try to catch it at an early stage," Lee said.
Abby Weiner, 43, a wife and mother of three young boys living in Washington, D.C., had always been careful about protecting her skin from the sun — which is why her Oct. 2023 melanoma diagnosis was such a shock, she said.
"I had a spot on my cheek that started as a freckle and began getting darker and larger," she told Fox News Digital.
"I assumed it was just a normal part of aging and sun exposure."
VACCINE FOR DEADLY SKIN CANCER SHOWS ‘GROUNDBREAKING’ RESULTS IN CLINICAL TRIAL
Weiner’s sister encouraged her to get it checked out — which led to a biopsy and diagnosis.
"I was obviously shocked and frightened at first," said Weiner.
Her melanoma was removed using Mohs surgery, a procedure in which thin layers of skin are removed one at a time.
"I required two procedures to remove the cancer and surrounding margins," she said. "Now, most people don't even know I had surgery."
To others, Weiner’s advice is to remember to seek shade, wear sun-protective clothing, and apply a broad-spectrum, water-resistant sunscreen with an SPF of 30 or higher on a daily basis all year long.
"I thought I was careful about protecting myself from sun exposure by wearing a hat or applying sunscreen when my family was at the pool or planning to be outdoors — but if we were eating outdoors and there wasn't a table in the shade, I would end up sitting in the sun."
Now, Weiner said she will wait a little longer for a shaded table, and she always keeps a hat and sunscreen with her.
"My sons used to have difficulty applying sunscreen and wearing hats, but now that they've seen the impact skin cancer had on me, they are more cooperative," she said.
CANCER SCREENINGS: HERE ARE 5 TYPES AND CRITICAL INFORMATION TO KNOW ABOUT EACH
Weiner also recommends that everyone gets yearly skin checks with a board-certified dermatologist.
"I have so many friends — and even my sister, who probably saved my life — who didn't regularly see a dermatologist for a yearly skin check before they learned about my melanoma."
Steve Murray, 68, of the greater Washington, D.C. area, has worked in construction for several decades.
During his childhood, Murray spent summers at the beach in Ocean City, New Jersey, and winter visits to Florida, where he was exposed to the sun and didn’t do much to protect himself.
In the late 1990s, Murray was diagnosed with basal cell carcinoma, the most common type of skin cancer, and squamous cell carcinoma, a variation of skin cancer that tends to develop in people who have had a lot of sun exposure.
In 2008, he was diagnosed with melanoma.
"My initial symptoms included itching and scaling on my head, followed by irritation," he told Fox News Digital.
"Then there was discoloration and irregularity in the shape of my moles."
Initially, Murray feared the worst — "mainly death" — but his dermatologist determined that the melanoma was only on his scalp and hadn’t traveled to his lymph nodes.
Like Weiner, Murray had Mohs surgery to get rid of the cancer — and he was cleared.
VIRGINIA HIGH SCHOOL STUDENT CREATES SOAP TO FIGHT SKIN CANCER, IS AWARDED $25K: 'REMARKABLE EFFORT'
Since that diagnosis, Murray has had several more bouts of skin cancer.
In 2024, he underwent two surgeries for squamous cell carcinoma on his hand and back.
Now, Murray visits the dermatologist every three to six months. Also, he always wears a hat, sunscreen and long sleeves whenever possible to protect himself from the sun.
Murray’s advice to others is to make sun protection a priority when outdoors.
"You don’t notice at the time of initial exposure, but it haunts you later in life when you start developing pre-cancers and skin cancers like squamous cell carcinoma and melanoma that require immediate attention," he told Fox News Digital.
"Capturing these pre-cancers and cancers of the skin must be diagnosed early with regular checkups," he added. "Failure to do so could lead to death."
Dr. Lee of NYU Langone Health shared five tips to help prevent potentially deadly skin cancers like melanoma.
"Avoiding a burn is really only half the battle — there is no such thing as a base tan," Lee said. "Damaged skin is damaged skin."
For a safer way to achieve a sun-kissed glow on your first beach day of the summer, Lee recommends using self-tanning products.
When applying sunscreen, Lee recommends using 1 ounce, which would fill a shot glass.
IF YOU OR YOUR CHILDREN HAVE FRECKLES, HERE'S WHAT YOUR SKIN IS TRYING TO TELL YOU
"It should have a sun protection factor (SPF) of 30 and say ‘broad-spectrum’ on the label, which protects against the sun’s UVA and UVB rays," she said.
Reapply at least every 80 minutes, or more often if you’re sweating or swimming.
Physical sunscreen contains zinc or titanium, which is superior in efficacy to chemical sunscreen, according to Lee.
"Check your skin regularly so you know what’s normal and to notice any changes or new growths," Lee advised.
"Seek a dermatologist’s evaluation if you notice a changing, bleeding or persistently itchy spot."
This is the best way to determine if any mole or blemish is cancerous, according to Lee.
The ABCDE rule tells you what to look for when examining your skin.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
The A stands for asymmetrical. "Noncancerous moles are typically symmetrical," Lee said.
B is for border, as the border of a cancerous spot or mole may be irregular or blurred.
C stands for color. "A typical mole tends to be evenly colored, usually a single shade of brown," Lee noted.
"Not all melanomas are dark and scary-appearing. They can be amelanotic, which means they can be more skin colored or pink."
D stands for diameter of the spot or mole, which may be a warning sign if it’s larger than 6 millimeters, according to Lee.
If the spot is evolving, which is what E stands for, it might be of concern.
Lee added, "Because melanomas can vary in appearance, it is important to see a dermatologist regularly for skin exams if you have a history of significant sun exposure, have many atypical appearing moles, or a family or personal history of melanoma so that you have an experienced set of eyes looking at any spots of concern."
1 year 2 months ago
Health, Cancer, skin-cancer, beauty-and-skin, healthy-living, lifestyle, health-care
As cholera cases rise worldwide, health officials sound 'concerning' alarm about vaccine shortages
As cholera continues to surge — and as vaccines remain in short supply — experts are warning about the global risk.
Cholera is a bacterial disease typically spread by food and water, leading to severe diarrhea and dehydration. It has been on the rise around the world since 2021.
As cholera continues to surge — and as vaccines remain in short supply — experts are warning about the global risk.
Cholera is a bacterial disease typically spread by food and water, leading to severe diarrhea and dehydration. It has been on the rise around the world since 2021.
Each year, there are some 1.3 to 4 million cases of cholera worldwide, according to the World Health Organization (WHO). Approximately 21,000 to 143,000 deaths occur as a result.
HIGH LEVELS OF RESISTANT BACTERIA FOUND IN UNCOOKED MEATS AND RAW DOG FOOD: ‘RED FLAG’
Around 473,000 cases were reported to WHO in 2022, which was twice as many cases as the prior year.
Reported cases for 2023 are expected to exceed 700,000.
"It is concerning to see an increase in the number of cholera cases worldwide, with the majority of the cases in Asia, Africa and Latin America," Dr. Renuga Vivekanandan, M.D., assistant dean and professor at the Creighton University School of Medicine in Omaha, Nebraska, told Fox News Digital.
The countries most affected include the Democratic Republic of the Congo, Ethiopia, Haiti, Somalia, Sudan, Syria, Zambia and Zimbabwe, according to UNICEF.
Although cholera cases were prevalent in the U.S. in the 1800s, water treatment systems have largely eliminated the disease, per the CDC.
In rare cases, people in the U.S. have contracted the disease from consuming raw or undercooked shellfish from the Gulf of Mexico, the agency stated on its website.
AMID BIRD FLU SPREAD, EXPERTS REVEAL IF IT'S SAFE TO DRINK MILK: 'INDIRECT CONCERN'
"In the U.S., the cases have remained very small and are usually from travel exposure," Vivekanandan noted.
Cholera is typically spread when someone drinks water or eats food that is contaminated with the bacterium Vibrio cholerae, according to the CDC.
The disease can spread quickly in locations where there is insufficient treatment of drinking water and sewage, the agency warned.
It is not typically transmitted from person to person.
UNICEF noted in a statement that the rise in cholera is driven by "persistent gaps in access to safe water and sanitation."
"I think the cases might be increasing due to climate change, displacements of homes due to disasters, and not having good sanitary conditions, such as poor water sources," Vivekanandan told Fox News Digital.
Around 10% of the people who are infected with cholera will develop severe symptoms, including watery diarrhea, vomiting and leg cramps, according to the U.S. Centers for Disease Control and Prevention (CDC).
Advanced symptoms include shock and dehydration.
Without treatment, the disease can be fatal.
"Dehydration is the biggest concern with cholera, and rehydration is the most important component of treatment," said Vivekanandan.
"Most patients with cholera will have mild diarrhea, but 10% will have severe diarrhea and will need rehydration and treatment with antibiotics."
WITH WHOOPING COUGH CASES ON THE RISE, DO YOU NEED A BOOSTER VACCINE?
Some groups are more susceptible to the disease, according to the CDC.
"Individuals with achlorhydria (the absence of hydrochloric acid in digestive stomach juices), blood type O, chronic medical conditions, and those without ready access to rehydration therapy and medical services are more likely to have severe disease from cholera and suffer poor outcomes," the agency noted.
The most effective treatment for cholera is "immediate replacement of the fluid and salts lost through diarrhea," the CDC stated.
This is achieved by giving patients a mixture of sugar and salts mixed with 1 liter of water.
In some severe cases, the patient may require intravenous (IV) fluids.
Some patients also receive antibiotics to make symptoms less severe.
"Persons who develop severe diarrhea and vomiting in countries where cholera occurs should seek medical attention promptly," per the CDC.
There is a single-dose vaccine for cholera, called Vaxchora (lyophilized CVD 103-HgR).
CDC WARNS OF INVASIVE BACTERIAL OUTBREAK AMID SPIKE IN CASES AND FATALITY RATES: 'RARE BUT SEVERE'
Those who are between the ages of 2 and 64 and who are traveling to "an area of active cholera transmission" are eligible to receive it.
There are three other cholera vaccines, but they are not available in the U.S.
There is a "severe gap" in the number of available vaccine doses compared to the level of current need, said UNICEF on its website.
"Between 2021 and 2023, more doses were requested for outbreak response than the entire previous decade," UNICEF noted.
While cholera vaccines used to be administered in two doses, the International Coordinating Group (ICG) changed the recommendation to a single dose in Oct. 2022 due to the ongoing shortage.
Vivekanandan called the vaccine shortage "very concerning."
NEW ANTIBIOTIC KILLS DEADLY, DRUG-RESISTANT BACTERIA IN ‘SCIENTIFIC BREAKTHROUGH’
"This is a serious infection, and we must invest financial and other resources to reduce the worldwide burden," he told Fox News Digital.
"International resources need to be committed, and partnerships with pharmaceutical companies need to happen to help produce more vaccines."
Vivekanandan also urged people who are traveling from the U.S. to other countries to review the CDC’s travel guidance and get any required vaccines.
"I would also recommend that people follow good travel medicine guidance, such as drinking bottled water, eating well-cooked food and making sure to have good hand hygiene," he added.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
"As the WHO has stated, we need to have multi-pronged approaches, with a combination of surveillance, water, sanitation and hygiene, social mobilization, treatment, and oral cholera vaccines available for communities at high risk."
On the U.S. Food and Drug Administration (FDA) website, Vaxchora is listed as a "resolved shortage."
The FDA noted that Emergent Travel Health, manufacturer of the vaccine, announced in May 2021 the temporary discontinuation and distribution of Vaxchora, "due to a significant reduction of international travel caused by the COVID-19 pandemic."
The shortage is listed as having been resolved in May 2023.
Fox News Digital reached out to WHO, the FDA and Emergent requesting comment.
1 year 2 months ago
Health, outbreaks, Bacteria, viruses, lifestyle, health-care, infectious-disease, World
Pennsylvania mom seeks ‘perfect match’ bone marrow donor to cure daughter’s rare disorder: ‘Crucial need’
A 10-year-old girl in Pennsylvania is in dire need of a bone marrow transplant — and her mother is on a mission to find the perfect match.
A 10-year-old girl in Pennsylvania is in dire need of a bone marrow transplant — and her mother is on a mission to find the perfect match.
Lani Walter suffers from a disease called DOCK8 deficiency (dedicator of cytokinesis 8 deficiency), an immunodeficiency syndrome that can cause recurrent, life-threatening infections.
DOCK8 is very rare, with only 250 people worldwide currently diagnosed, statistics show. The only cure for DOCK8 is a bone marrow transplant — also known as a hematopoietic stem cell transplant (HSCT).
YOUNG GIRL SURVIVES CANCER THANKS TO LITTLE SISTER’S LIFESAVING DONATION: 'A PERFECT MATCH'
Ashleigh Walter, a kindergarten teacher, is pleading for people to join the bone marrow/blood stem cell registry to help her daughter find a donor by summer.
"Time is of the essence," she told Fox News Digital.
Walter’s daughter was diagnosed with DOCK8 when she was 7½ years old, the culmination of a long series of symptoms and illnesses.
"Lani’s health issues started at just a couple of months old," Walter told Fox News Digital during an interview. "As a baby, she had full-body eczema from head to toe and continuous ear infections."
At 11 months old, she was diagnosed with severe allergies to eggs, milk, peanuts, tree nuts and many other foods. She's also experienced continuous skin infections and staph infections.
In Jan. 2021, the family was invited to a clinic at the Children’s Hospital of Philadelphia (CHOP), where Walter’s daughter was able to see specialists from immunology, allergy and dermatology together in one appointment.
NEW JERSEY WOMAN RECOVERING AFTER RECEIVING SUCCESSFUL PIG KIDNEY TRANSPLANT
"They all came together to try and figure out what might be going on," Walter said. "Each of the specialties ran their own special bloodwork to see what was going on with Lani."
The results showed some abnormalities in the immune system, and doctors recommended doing genetic testing.
A few months later, the family received the news that Walter’s daughter has two variants of the DOCK8 gene.
"If you have issues on both sides of the gene, that's when you present with the disorder," Walter said. "Testing showed that both my husband and I are recessive carriers to the DOCK8 variant, which we passed down to Lani."
She added, "So that was when we found out that all of the health issues Lani has experienced throughout her entire life were not unrelated."
Dr. Marc Siegel, clinical professor of medicine at NYU Langone Medical Center and a Fox News medical contributor, was not involved in Lani Walter’s care but commented on the condition.
"DOCK 8 is a rare immune condition where the bone marrow doesn't make enough immune cells and the immune cells that are made have trouble penetrating into dense tissue, like skin," he told Fox News Digital.
After the diagnosis, Walter’s daughter was invited to visit the National Institute of Health in Maryland, where researchers are studying DOCK8 deficiency.
"We go there about every six months to see how Lani is doing, and what they recommend as she gets older," Walter said.
The symptoms of DOCK8 deficiency tend to get more severe as the child grows into late adolescence and early adulthood, doctors have said.
Some of the biggest concerns are respiratory difficulties and a higher risk of various cancers, along with the ongoing risk of infections.
FOUR TEXAS RESIDENTS FOREVER CONNECTED BY TWO KIDNEY DONATIONS IN DIFFERENT CITIES: 'SUPERBLY TIMED'
To help manage her condition, Walter’s daughter has been getting weekly intravenous immune globulin (IVIG) infusions, which add human antibodies to help fight off infections.
She also takes daily antibiotics to help prevent pneumonia, uses an inhaler to help her respiratory system and takes other medications to treat different illnesses she experiences as a result of her DOCK8 deficiency.
"That's probably one of the least favorite parts of her day, when I tell her that she needs to take her medicine," Walter said.
Since the only cure for her condition is a bone marrow transplant, "her doctors recommend that Lani has [the] transplant to help cure the DOCK8 before she gets older."
Dr. Brett Osborn, a Florida neurologist and longevity expert at Senolytix, described HSCT as a "transformative reset button" for patients suffering from DOCK8 deficiency.
Osborn is not involved in Lani Walter’s care.
"Imagine your immune system as a computer plagued by a virus," he told Fox News Digital.
"HSCT removes the compromised ‘software’ and installs new, functional cells. For individuals with DOCK8 deficiency — who typically face frequent infections, severe allergies and increased cancer risk — HSCT can mean a dramatic shift toward immunologic normalcy, providing a new lease on life."
Siegel also emphasized the procedure’s importance, calling it a "crucial life-saving procedure."
The average wait for a transplant is about three months, according to Siegel.
"They are very expensive — about $190,000," he said. "Insurance generally covers the procedure, but not the cost of finding a donor."
There is around a 25% chance that a sibling will be a match. In Lani Walter’s case, her 14-year-old sister was not a match.
PENNSYLVANIA MOTHER AND SON BOTH BORN WITH RARE GENETIC DISEASE: 'CLOSER BECAUSE OF THIS'
"The overall chance of finding a match in the world is 1/3 to 2/3," Siegel said.
The organization known as NMDP, formerly the National Marrow Donor Program/Be the Match, maintains a registry of people who are willing to donate. The Walter family found a 90% match on the registry, but the optimal situation would be to find a 100% match.
"There's much less risk with the bone marrow transplant if you can find that perfect match," Walter told Fox News Digital.
Lani Walter’s doctors recommend that she receives the donation before she starts middle school. Next year, she will start fifth grade.
"Ideally, we would do it before Lani sees significant issues with other organs in her body," said Ashleigh Walter.
If the family does not find a perfect match, Walter said she will donate to her daughter, as parents are always half-matches.
"Obviously, we would still love for her to be able to find a full match on the donor registry, which is much less of a risk," she said. "But if that's not possible, we can move forward with a half match."
With partial matches, there is a higher risk of "graft versus host disease," which is a complication that occurs when donor bone marrow or stem cells attack the recipient.
"It can cause different issues throughout the body, similar to an organ transplant rejection," Walter said.
If her daughter receives a successful bone marrow transplant, Walter said — she will be cured of DOCK8.
"She won't have an immune deficiency anymore," she said. "She'll adopt the immune system of the donor, and we won't have to worry about any of those increased risks at all."
Walter is hopeful that her daughter — whom she describes as "a little kid at heart" — will soon be healthy and able to return to the activities she loves, including swimming.
"Lani has been on a swim team since kindergarten, and this will be her first summer not doing it," Walter said.
She also enjoys bike-riding, crafting, and spending time with her friends and pets.
There are millions of potential donors on the bone marrow registry — with more than 300,000 Americans joining just last year — but Walter noted that the likelihood of someone finding a perfect match is very low.
"The more people who join the registry, the more likely that a perfect match will be there for you," she said.
THE GIRL WHO CAN’T SMILE: HOW A RARE DISORDER BECAME A YOUNG WOMAN'S ‘GREATEST GIFT’
As a neurosurgical trauma surgeon, Osborn of Florida said he can attest to the dire need for blood and bone marrow donors.
"There is a critical shortage of both," he said. "In emergency and surgical settings, the availability of blood products can be the difference between life and death."
It’s "vital" to have diversity in the bone marrow registry, Osborn noted.
"A closely matched donor reduces complications and improves outcomes," he said.
"This emphasizes why everyone should consider joining the registry. We can all manufacture these potentially life-saving blood products, and by donating, we fulfill a crucial societal need."
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
While some have the misconception that donation is difficult, Osborn said that’s not the case.
"Donating bone marrow is a low-risk, outpatient procedure associated with only minor discomfort. It’s a great way to pay it forward."
People can join the bone marrow registry by visiting the NMDP’s website to order a test kit.
"It’s a really simple cheek swab kit that they'll send to your house and then you send it back," Walter said. "You don't have to pay any money for anything."
"The more people that join, the more people who can find their perfect match."
"For conditions like DOCK8 deficiency, a bone marrow transplant can offer a chance at a healthier life," Osborn added.
"Joining the bone marrow registry could be your most profound gift, potentially saving a life with your healthy cells."
1 year 2 months ago
Health, transplants, rare-diseases, health-care, lifestyle, childrens-health, family, Pennsylvania
5 women’s health tips to prevent and detect strokes, according to cardiologists
One in five women between ages 55 and 75 will experience a stroke in their lifetime, according to the American Heart Association.
There are two main types of strokes.
One in five women between ages 55 and 75 will experience a stroke in their lifetime, according to the American Heart Association.
There are two main types of strokes.
With an ischemic stroke, a blockage prevents blood from flowing properly to the brain. With a hemorrhagic stroke, a blood vessel bursts in the brain and causes bleeding, which damages brain cells.
While some risk factors such as age, race and family history can’t be changed, others can be mitigated through healthy lifestyle choices.
DOG ALERTS FAMILY, SAVES TEXAS TEENAGER FROM LIFE-THREATENING STROKE: 'KEEPING GUARD'
Parag Shah, M.D., a physical medicine and rehabilitation specialist who practices at Brooks Rehabilitation in Jacksonville, Florida, shared some specific tips about how women can reduce their risk.
Here are five tips.
Research has shown that air pollution tends to impact women more than men in terms of inflammation, infection and heart disease.
CDC WARNS OF EXTREME HEAT DANGERS AMID ‘RECORD-BREAKING HIGH TEMPERATURES’
"According to a recent review, elevated levels of ambient air pollution — even just short-term exposure — can increase the likelihood of strokes," said Shah, who specializes in stroke rehabilitation.
"Health experts recommend checking the air quality in your area and, on high-pollution days, limiting time outside, turning on exhaust fans in kitchens and bathrooms, and using an air purifier in the home," he also said.
The Mediterranean diet — a plant-based nutrition plan that mimics the regional cuisines of the countries along the Mediterranean Sea, such as Italy and Greece — can reduce the health risks associated with strokes, according to Shah.
"Current research on preventing strokes is exploring an array of lifestyle factors," he told Fox News Digital.
"This includes the Mediterranean diet, which highlights the consumption of fruits, vegetables, whole grains, nuts, olive oil and foods rich in omega-3 fatty acids like fatty fish, walnuts and flaxseed."
MEDITERRANEAN, MIND DIETS SHOWN TO REDUCE SIGNS OF ALZHEIMER’S IN THE BRAIN, STUDY FINDS
Practicing exercises that promote heart health and lessen stress can help reduce the possibility of stroke, Shah suggested.
"Participating in physical activities like yoga, tai chi and strength training, while also giving importance to mindfulness techniques such as meditation and deep breathing exercises, could provide additional advantages in lowering the risk of strokes," he told Fox News Digital.
Sudden confusion, difficulty understanding, slurred speech, double vision, and numbness or weakness, especially on one side of the body, are often overlooked signs of strokes, Shah warned.
TIAS AND MINI-STROKE RISKS: CARDIOLOGIST SHARES WARNING SIGNS AND PREVENTION TIPS
"Recognizing these signs is crucial, because quick identification and immediate medical attention greatly enhance the chances of recovery for stroke patients," he said.
Beyond the more obvious "textbook" stroke symptoms, there are some warning signs that tend to be overlooked until it’s too late.
"Factors like pregnancy, giving birth and hormonal changes such as menopause can heighten the likelihood of having a stroke," Shah told Fox News Digital.
The use of oral contraceptives and hormone therapy can also raise this risk, the doctor added, as can hidden biological factors that make women more susceptible.
"Scheduling regular health check-ups and staying knowledgeable about stroke symptoms and prevention methods are essential for maintaining good health," Shah said.
"Preventing most strokes is similar to the prevention of heart attacks," Dr. Laxmi Mehta, a cardiologist and director of preventative cardiology and women's cardiovascular health at The Ohio State University Wexner Medical Center, told Fox News Digital.
In her practice, Mehta typically recommends following the American Heart Association’s Life’s Essential 8, which provides steps to improve or maintain cardiovascular health.
These include four healthy behaviors and four health factors, as listed below.
1. Quit tobacco. Avoid cigarettes, vaping and other nicotine products, which have been proven to increase the risk of strokes and heart attacks.
2. Eat better. Following a healthy eating pattern that includes plenty of fresh fruits and veggies, whole grains, lean protein, nuts and seeds can reduce stroke risk.
3. Be more active. Experts recommend participating in 150 minutes of moderate intensity or 75 minutes of vigorous physical activity weekly.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
4. Get healthy sleep. Adults should aim for seven to nine hours of sleep per night to reduce stroke risk, according to experts.
5. Manage blood pressure. A "normal" blood pressure is defined as a systolic pressure of less than 120 and a diastolic pressure of less than 80, according to the National Institutes of Health.
6. Manage cholesterol. High cholesterol levels have a proven link to stroke risk. A healthy range for LDL ("bad") cholesterol is 100 mg/dL or lower, as published in the Journal of the American College of Cardiology.
7. Manage blood sugar. Excessive levels of glucose in the blood can increase the risk of fatty deposits or clots, which are a factor in strokes.
8. Achieve and maintain a healthy weight. Being overweight or obese is one of the biggest risk factors and is linked to nearly one in five strokes, according to the World Stroke Organization.
1 year 3 months ago
Health, stroke, womens-health, heart-health, lifestyle, healthy-living, health-care, wellness, healthy