Minister of Health introduces ‘More Health and Life Expectancy’ initiative
Santo Domingo.- The Minister of Public Health and Social Assistance, Víctor Atallah, introduced the “More Health and Life Expectancy” initiative, known as the Hearts Plan.
Santo Domingo.- The Minister of Public Health and Social Assistance, Víctor Atallah, introduced the “More Health and Life Expectancy” initiative, known as the Hearts Plan. This plan signifies a comprehensive transformation of the health system, aiming to enhance responsive and optimal primary care for users of public health services who rely on medications from the Essential Medicines Program (Promese/CAL).
Atallah emphasized that the Hearts Plan is based on a proven strategic health plan implemented in 33 countries. Officially endorsed by President Abinader on January 8, the initiative demonstrated success in preventive measures and risk reduction at the first level of primary care in other nations. The President urged immediate execution in the Dominican Republic after recognizing its effectiveness.
The Minister assured that the program will benefit the population by focusing on health promotion, disease prevention, and addressing health complications. Internationally approved protocols will guide the plan, receiving support from medical societies in managing conditions such as hypertension (HTN) and type two diabetes (DM), which significantly impact the health system.
Victor Atallah, expressing his commitment as the minister and overseer of the ministry, pledged to monitor the plan at all levels, emphasizing the collective effort required for its success. He underscored the importance of creating a healthier path for everyone, urging dedication from all stakeholders.
Adolfo Pérez, the General Director of Promese/CAL, highlighted President Abinader’s initiative to provide free medicines to the population. The Hearts Plan, an innovative tool, will soon be operational, offering significant benefits to users of community pharmacies.
1 year 6 months ago
Health
Saharan Dust brings unhealthy air quality
A major surge of Saharan Dust has moved across the Windward Islands, significantly reducing air quality and visibility across the region
View the full post Saharan Dust brings unhealthy air quality on NOW Grenada.
A major surge of Saharan Dust has moved across the Windward Islands, significantly reducing air quality and visibility across the region
View the full post Saharan Dust brings unhealthy air quality on NOW Grenada.
1 year 6 months ago
Environment, External Link, Health, Weather, sharan dust, significant dust haze advisory, tt weather centre
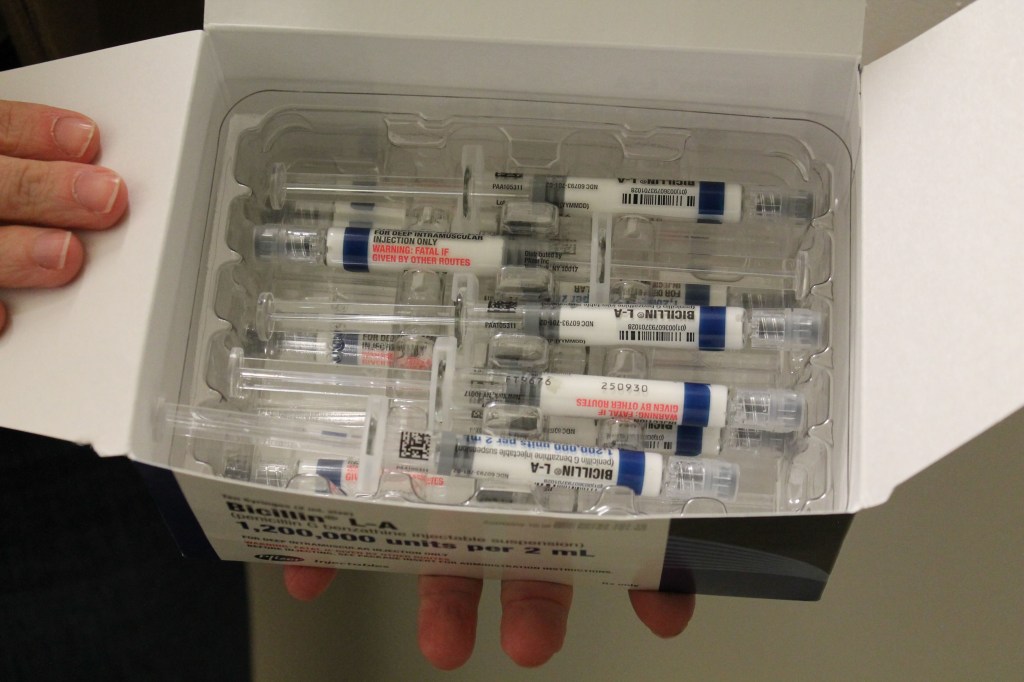
Surge in Syphilis Cases Leads Some Providers to Ration Penicillin
When Stephen Miller left his primary care practice to work in public health a little under two years ago, he said, he was shocked by how many cases of syphilis the clinic was treating.
For decades, rates of the sexually transmitted infection were low. But the Hamilton County Health Department in Chattanooga — a midsize city surrounded by national forests and nestled into the Appalachian foothills of Tennessee — was seeing several syphilis patients a day, Miller said. A nurse who had worked at the clinic for decades told Miller the wave of patients was a radical change from the norm.
What Miller observed in Chattanooga is reflective of a trend that is raising alarm bells for health departments across the country.
Nationwide, syphilis rates are at a 70-year high. The Centers for Disease Control and Prevention said Jan. 30 that 207,255 cases were reported in 2022, continuing a steep increase over five years. Between 2018 and 2022, syphilis rates rose about 80%. The epidemic of sexually transmitted infections — especially syphilis — is “out of control,” said the National Coalition of STD Directors.
The surge has been even more pronounced in Tennessee, where infection rates for the first two stages of syphilis grew 86% between 2017 and 2021.
But this already difficult situation was complicated last spring by a shortage of a specific penicillin injection that is the go-to treatment for syphilis. The ongoing shortage is so severe that public health agencies have recommended that providers ration the drug — prioritizing pregnant patients, since it is the only syphilis treatment considered safe for them. Congenital syphilis, which happens when the mom spreads the disease to the fetus, can cause birth defects, miscarriages, and stillbirths.
Across the country, 3,755 cases of congenital syphilis were reported to the CDC in 2022 — that’s 10 times as high as the number a decade before, the recent data shows. Of those cases, 231 resulted in stillbirth and 51 led to infant death. The number of cases in babies swelled by 183% between 2018 and 2022.
“Lack of timely testing and adequate treatment during pregnancy contributed to 88% of cases of congenital syphilis,” said a report from the CDC released in November. “Testing and treatment gaps were present in the majority of cases across all races, ethnicities, and U.S. Census Bureau regions.”
Hamilton County’s syphilis rates have mirrored the national trend, with an increase in cases for all groups, including infants.
In November, the maternal and infant health advocacy organization March of Dimes released its annual report on states’ health outcomes. It found that, nationwide, about 15.5% of pregnant people received care beginning in the fifth month of pregnancy or later — or attended fewer than half the recommended prenatal visits. In Tennessee, the rate was even worse, 17.4%.
But Miller said even those who attend every recommended appointment can run into problems because providers are required to test for syphilis only at the beginning of a pregnancy. The idea is that if you test a few weeks before birth, there is time to treat the infection.
However, that recommendation hinges on whether the provider suspects the patient was exposed to the bacterium that causes syphilis, which may not be obvious for people who say their relationships are monogamous.
“What we found is, a lot of times their partner was not as monogamous, and they were bringing it into the relationship,” Miller said.
Even if the patient tested negative initially, they may have contracted syphilis later in pregnancy, when testing for the disease is not routine, he said.
Two antibiotics are used to treat syphilis, the injectable penicillin and an oral drug called doxycycline.
Patients allergic to penicillin are often prescribed the oral antibiotic. But the World Health Organization strongly advises pregnant patients to avoid doxycycline because it can cause severe bone and teeth deformities in the infant.
As a result, pregnant syphilis patients are often given penicillin, even when they’re allergic, using a technique called desensitization, said Mark Turrentine, a Houston OB-GYN. Patients are given low doses in a hospital setting to help their bodies get used to the drug and to check for a severe reaction. The penicillin shot is a one-and-done technique, unlike an antibiotic, which requires sticking to a two-week regimen.
“It’s tough to take a medication for a long period of time,” Turrentine said. The single injection can provide patients and their clinicians peace of mind. “If they don’t come back for whatever reason, you’re not worried about it,” he said.
The Metro Public Health Department in Nashville, Tennessee, began giving all nonpregnant adults with syphilis the oral antibiotic in July, said Laura Varnier, nursing and clinical director.
Turrentine said he started seeing advisories about the injectable penicillin shortage in April, around the time the antibiotic amoxicillin became difficult to find and physicians were using penicillin as a substitute, potentially precipitating the shortage, he said.
The rise in syphilis has created demand for the injection that manufacturer Pfizer can’t keep up with, according to the American Society of Health-System Pharmacists. “There is insufficient supply for usual ordering,” the ASHP said in a memo.
Even though penicillin has been around a long time, manufacturing it is difficult, largely because so many people are allergic, said Erin Fox, associate chief pharmacy officer for the University of Utah health system and an adjunct professor at the university, who studies drug shortages.
“That means you can’t make other drugs on that manufacturing line,” she said. Only major manufacturers like Pfizer have the resources to build and operate such a specialized, cordoned-off facility. “It’s not necessarily efficient — or necessarily profitable,” Fox said.
In a statement, Pfizer confirmed the amoxicillin shortage and surge in syphilis increased demand for injectable penicillin by about 70%. Representatives said the company invested $38 million in the facility that produces this form of penicillin, hiring more staff and expanding the production line.
“This ramp up will take some time to be felt in the market, as product cycle time is 3-6 months from when product is manufactured to when it is available to be released to customers,” the statement reads. The company estimated the shortage would be significantly alleviated by spring.
In the meantime, Miller said, his clinic in Chattanooga is continuing to strategize. Each dose of injectable penicillin can cost hundreds of dollars. Plus, it has to be placed in cold storage, and it expires after 48 months.
Even with the dramatic increase in cases, syphilis is still relatively rare. More than 7 million people live in Tennessee, and in 2019, providers statewide reported 683 cases of syphilis.
Health departments like Miller’s treat the bulk of syphilis patients. Many patients are sent by their provider to the health department, which works with contact tracers to identify and notify sexual partners who might be affected and tests patients for other sexually transmitted infections, including HIV.
“When you diagnose in the office, think of it as just seeing the tip of the iceberg,” Miller said. “You need a team of individuals to be able to explore and look at the rest of the iceberg.”
This story is part of a partnership that includes WPLN, NPR, and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 6 months ago
Pharmaceuticals, Public Health, Rural Health, States, CDC, Sexual Health, Tennessee
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Medical Bulletin 1/February/2024
Here are the top medical news of the day:
Early Life Nutrition: A Key Factor in Reducing the Risk of Inflammatory Bowel Disease
A high quality diet at the age of 1 may curb the subsequent risk of inflammatory bowel disease, suggests a large long term study, published online in the journal Gut.
Here are the top medical news of the day:
Early Life Nutrition: A Key Factor in Reducing the Risk of Inflammatory Bowel Disease
A high quality diet at the age of 1 may curb the subsequent risk of inflammatory bowel disease, suggests a large long term study, published online in the journal Gut.
Plenty of fish and vegetables and minimal consumption of sugar-sweetened drinks at this age may be key to protection, the findings indicate. A linked editorial suggests that it may now be time for doctors to recommend a ‘preventive’ diet for infants, given the mounting evidence indicative of biological plausibility.
Cases of inflammatory bowel disease (IBD), which includes Crohn’s disease and ulcerative colitis, are increasing globally. Although there is no obvious explanation for this trend, changes in dietary patterns are thought to have a contributory role, because of their impact on the gut microbiome.
While various studies have looked at the influence of diet on IBD risk in adults, there is little in the way of research on the potential influence of early childhood diet on risk.
In a bid to plug this knowledge gap, the researchers drew on survey data from the All Babies in Southeast Sweden study (ABIS) and The Norwegian Mother, Father and Child Cohort Study (MoBa).
ABIS includes 21,700 children born between October 1997 and October 1999; MoBa includes 114, 500 children, 95,200 mothers, and 75,200 fathers recruited from across Norway between 1999 and 2008.
Parents were asked specific questions about their children’s diet when they were aged 12-18 months and 30-36 months. The final analysis included dietary information for 81,280 1 year olds: 11,013 (48% girls) from ABIS and 70, 267 (49% girls) from MoBa.
Diet quality, gleaned from measuring intake of meat, fish, fruit, vegetables, dairy, sweets, snacks, and drinks, was assessed using a modified version of the Healthy Eating Index (HEI) scoring system, adapted for children. The weekly frequency of specific food groups was also assessed.
Higher diet quality—a higher intake of vegetables, fruit, and fish, and a lower intake of meat, sweets, snacks, and drinks—was reflected in a higher HEI score. The total score was divided into thirds to indicate a low, medium, or high quality diet.
Reference: High quality diet in early life may curb subsequent inflammatory bowel disease risk; BMJ JOURNAL, Gut; DOI: 10.1136/gutjnl-2023-330971
Rise in annual cardiorespiratory fitness by 3%+ to lower prostate cancer risk by 35%
An increase in annual cardiorespiratory fitness by 3% or more is linked to a 35% lower risk of developing, although not dying from, prostate cancer, suggests research published online in the British Journal of Sports Medicine.
The findings prompt the researchers to conclude that men should be encouraged to improve their level of fitness to help lower their chances of getting the disease.
There are relatively few known risk factors for prostate cancer, note the researchers. And while there’s good evidence for the beneficial effects of physical activity on the risk of several cancers, the associations with prostate cancer are less clear-cut.
Most previously published studies have assessed fitness at only one time point, and none has looked at the potential impact of fitness on both the risk of developing and dying from prostate cancer, explain the researchers.
They therefore wanted to find out if improvements in cardiorespiratory fitness over time might influence these risks, drawing on a national occupational health profile assessment database.
The database collected information on physical activity, lifestyle, perceived health, measurement of body mass and height, and the results of at least 2 cardiorespiratory fitness tests, measured by peddling on a stationary cycle, for 57,652 men out of a total of 181,673.
Annual cardiorespiratory fitness measurements were expressed as absolute and relative V02 max---the amount (volume) of oxygen the body uses while exercising as hard as possible—and divided into groups according to whether these increased annually by more than 3%, fell by more than 3%, or remained stable.
An annual percentage increase in absolute cardiorespiratory fitness was associated with a 2% lower risk of prostate cancer, but not death, after accounting for potentially influential factors, including age, education level, year of test, weight (BMI), and smoking status.
When participants were grouped according to whether their cardiorespiratory fitness had increased, remained stable, or had fallen, those whose fitness had improved by 3% or more a year were 35% less likely to develop prostate cancer than those whose fitness had declined, after accounting for potentially influential factors.
Reference: Increase in annual cardiorespiratory fitness by 3%+ linked to 35% lower prostate cancer risk; British Journal of Sports Medicine; DOI: 10.1136/bjsports-2023-107007
Three daily servings of kimchi to lower men’s obesity risk
Eating up to three daily servings of the Korean classic, kimchi, may lower men’s overall risk of obesity, while radish kimchi is linked to a lower prevalence of midriff bulge in both sexes, finds research published in the open access journal BMJ Open.
Kimchi is made by salting and fermenting vegetables with various flavourings and seasonings, such as onion, garlic, and fish sauce.
Cabbage and radish are usually the main vegetables used in kimchi, which contains few calories and is rich in dietary fibre, microbiome enhancing lactic acid bacteria, vitamins, and polyphenols.
Previously published experimental studies have shown that Lactobacillus brevis and L. plantarum isolated from kimchi had an anti-obesity effect. And the researchers wanted to know if regular consumption might be associated with a reduction in the risk of overall and/or abdominal obesity, which is considered to be particularly harmful to health.
They drew on data from 115,726 participants (36,756 men; 78,970 women; average age 51) taking part in the Health Examinees (HEXA) study.
HEXA is a large, community-based long term study of the larger Korean Genome and Epidemiology Study, designed to examine environmental and genetic risk factors for common long term conditions among Korean adults over the age of 40.
Dietary intake for the previous year was assessed using a validated 106-item food frequency questionnaire for which participants were asked to state how often they ate a serving of each foodstuff, from never or seldom, up to 3 times a day.
Total kimchi included baechu (cabbage kimchi); kkakdugi (radish kimchi); nabak and dongchimi (watery kimchi); and others, such as mustard greens kimchi. A portion of baechu or kkahdugi kimchi is 50 g, while a portion of nabak or dongchimi kimchi is 95 g.
Height and weight, for BMI, and waist circumference were measured for each participant. A BMI of 18.5 was defined as underweight; normal weight 18.5 to 25; and obesity as above 25. Abdominal obesity was defined as a waist circumference of at least 90 cm for men and at least 85 cm for women. Some 36% of the men and 25% of the women were obese.
The results indicated a J-shaped curve, possibly because higher consumption is associated with higher intake of total energy, carbohydrates, protein, fat, sodium and cooked rice, say the researchers.
Compared with those who ate less than 1 daily serving of total kimchi, participants who ate 5 or more servings weighed more, had a larger waist size, and were more likely to be obese. They were also more likely to not be highly educated, have a low income, and to drink alcohol.
Reference: Up to three daily servings of kimchi may lower men’s obesity risk; BMJ Open; DOI:10.1136/bmjopen-2023-076650
1 year 6 months ago
MDTV,Channels - Medical Dialogues,Medical News Today MDTV,Medical News Today
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Early Life Nutrition: A Key Factor in Reducing the Risk of Inflammatory Bowel Disease
A high quality diet at the age of 1 may curb the subsequent risk of inflammatory bowel disease, suggests a large long term study, published online in the journal Gut.
Plenty of fish and vegetables and minimal consumption of sugar-sweetened drinks at this age may be key to protection, the findings indicate. A linked editorial suggests that it may now be time for doctors to recommend a ‘preventive’ diet for infants, given the mounting evidence indicative of biological plausibility.
Cases of inflammatory bowel disease (IBD), which includes Crohn’s disease and ulcerative colitis, are increasing globally. Although there is no obvious explanation for this trend, changes in dietary patterns are thought to have a contributory role, because of their impact on the gut microbiome.
While various studies have looked at the influence of diet on IBD risk in adults, there is little in the way of research on the potential influence of early childhood diet on risk.
In a bid to plug this knowledge gap, the researchers drew on survey data from the All Babies in Southeast Sweden study (ABIS) and The Norwegian Mother, Father and Child Cohort Study (MoBa).
ABIS includes 21,700 children born between October 1997 and October 1999; MoBa includes 114, 500 children, 95,200 mothers, and 75,200 fathers recruited from across Norway between 1999 and 2008.
Parents were asked specific questions about their children’s diet when they were aged 12-18 months and 30-36 months. The final analysis included dietary information for 81,280 1 year olds: 11,013 (48% girls) from ABIS and 70, 267 (49% girls) from MoBa.
Diet quality, gleaned from measuring intake of meat, fish, fruit, vegetables, dairy, sweets, snacks, and drinks, was assessed using a modified version of the Healthy Eating Index (HEI) scoring system, adapted for children. The weekly frequency of specific food groups was also assessed.
Higher diet quality—a higher intake of vegetables, fruit, and fish, and a lower intake of meat, sweets, snacks, and drinks—was reflected in a higher HEI score. The total score was divided into thirds to indicate a low, medium, or high quality diet.
Reference: High quality diet in early life may curb subsequent inflammatory bowel disease risk; BMJ JOURNAL, Gut; DOI: 10.1136/gutjnl-2023-330971
1 year 6 months ago
Gastroenterology,Gastroenterology News,Top Medical News,Gastroenterology Videos,MDTV,Gastroenterology MDTV,MD shorts MDTV,Gastroenterology Shorts MDTV,Channels - Medical Dialogues,MD Shorts
COVID-19 cases decrease, zero hospitalizations reported
Santo Domingo.- In a positive development, the Dominican Republic has experienced a significant decline in new COVID-19 cases over the past seven days. The reported number of new cases stands at 666, compared to 1,340 in the previous week, marking a noteworthy reduction of more than half.
Santo Domingo.- In a positive development, the Dominican Republic has experienced a significant decline in new COVID-19 cases over the past seven days. The reported number of new cases stands at 666, compared to 1,340 in the previous week, marking a noteworthy reduction of more than half. This encouraging trend was highlighted in the latest bulletin released by the Ministry of Public Health.
As of the latest update, there are currently 566 active COVID-19 cases in the country. Notably, no COVID-19 beds are currently occupied, and there is no requirement for ventilators.
The Dominican Republic conducted a total of 10,575 tests to detect the virus over the past week, resulting in a weekly positivity rate of 16.75%. The positivity rate over the last four weeks is reported at 14.96%, reflecting a sustained decrease in the spread of the virus.
Breaking down the geographical distribution of new cases, Santiago leads with 228 reported cases, followed by the National District with 75 cases, Espaillat with 69 cases, Santo Domingo with 46 cases, and Duarte with 45 cases.
Since the onset of the pandemic, the Dominican Republic has confirmed a total of 675,274 cases of COVID-19. Importantly, the country has reported no new COVID-19-related deaths since August 2022, emphasizing the success of ongoing public health measures and vaccination efforts. The Ministry of Public Health continues to monitor and report on the evolving situation, providing essential information to the public.
1 year 6 months ago
Health
Colon cancer hits young adults, plus advances in home fertility and AI drugs
NEVER TOO YOUNG – Brooks Bell was 38 when doctors told her she was too young for colon cancer – then she was diagnosed. Click to read her story. Continue reading…
NEVER TOO YOUNG – Brooks Bell was 38 when doctors told her she was too young for colon cancer – then she was diagnosed. Click to read her story. Continue reading…
IN NURSES WE TRUST – Find out why nurses are still the most trusted profession – even beating out doctors. Continue reading…
IBD INNOVATION – An AI-designed drug for inflammatory bowel disease has entered human clinical trials. Here's how it works. Continue reading…
CANCER ROLLER-COASTER – A Florida doctor wants to prepare people for the emotions surrounding a life-changing diagnosis. Continue reading…
OFF BALANCE – A doctor shares when losing your balance may be a sign of a more serious health issue. Continue reading…
FAST TRACK TO FERTILITY – The FDA has approved the first at-home, sterile insemination kit. Continue reading…
CANCER BREAKTHROUGH – A new ovarian cancer treatment could bring new hope for patients with aggressive forms of the disease. Continue reading…
PARTY PREP – Stock up before the big game with these 9 essentials from Amazon. Continue reading…
UNDER THE KNIFE – The CDC is warning of a spike in deaths among U.S. citizens traveling to the Dominican Republic for plastic surgery. Here's what to know. Continue reading…
Fox News LifestyleFox News Health
1 year 6 months ago
health-newsletter
No explanation for suspending visitation at Mt Gay Hospital
The last time there was a suspension of visitation at the Mt Gay Hospital was during the height of the Covid-19 pandemic
View the full post No explanation for suspending visitation at Mt Gay Hospital on NOW Grenada.
The last time there was a suspension of visitation at the Mt Gay Hospital was during the height of the Covid-19 pandemic
View the full post No explanation for suspending visitation at Mt Gay Hospital on NOW Grenada.
1 year 6 months ago
Health, chickenpox, coronavirus, COVID-19, linda straker, mt gay hospital
Belize News and Opinion on www.breakingbelizenews.com
Flu vaccines available at your nearest health facility
Posted: Wednesday, January 31, 2024. 9:50 am CST.
By Zoila Palma Gonzalez: The Ministry of Health and Wellness is reminding the public that the Seasonal Flu vaccine is available at all public clinics countrywide.
The vaccine is available for everyone from 6 months of age to those at age 65.
Get vaccinated today.
Posted: Wednesday, January 31, 2024. 9:50 am CST.
By Zoila Palma Gonzalez: The Ministry of Health and Wellness is reminding the public that the Seasonal Flu vaccine is available at all public clinics countrywide.
The vaccine is available for everyone from 6 months of age to those at age 65.
Get vaccinated today.
Protect yourself and your family.
Advertise with the mоѕt vіѕіtеd nеwѕ ѕіtе іn Belize ~ We offer fully customizable and flexible digital marketing packages. Your content is delivered instantly to thousands of users in Belize and abroad! Contact us at mаrkеtіng@brеаkіngbеlіzеnеwѕ.соm or call us at 501-601-0315.
© 2024, BreakingBelizeNews.com. Content is copyrighted and requires written permission for reprinting in online or print media. Theft of content without permission/payment is punishable by law.
Comments
jQuery(function() {var $breakslider565558313 = jQuery( ".break-slider-565558313" );$breakslider565558313.on( "unslider.ready", function() { jQuery( "div.custom-slider ul li" ).css( "display", "block" ); });$breakslider565558313.unslider({ delay:4000, autoplay:true, nav:false, arrows:false, infinite:true, animation:'fade', speed:0 });$breakslider565558313.on("mouseover", function(){$breakslider565558313.unslider("stop");}).on("mouseout", function() {$breakslider565558313.unslider("start");});});
jQuery(function() {var $breakslider299084061 = jQuery( ".break-slider-299084061" );$breakslider299084061.on( "unslider.ready", function() { jQuery( "div.custom-slider ul li" ).css( "display", "block" ); });$breakslider299084061.unslider({ delay:4000, autoplay:true, nav:false, arrows:false, infinite:true, animation:'fade', speed:0 });$breakslider299084061.on("mouseover", function(){$breakslider299084061.unslider("stop");}).on("mouseout", function() {$breakslider299084061.unslider("start");});});
jQuery(function() {var $breakslider444311813 = jQuery( ".break-slider-444311813" );$breakslider444311813.on( "unslider.ready", function() { jQuery( "div.custom-slider ul li" ).css( "display", "block" ); });$breakslider444311813.unslider({ delay:4000, autoplay:true, nav:false, arrows:false, infinite:true, animation:'fade', speed:0 });$breakslider444311813.on("mouseover", function(){$breakslider444311813.unslider("stop");}).on("mouseout", function() {$breakslider444311813.unslider("start");});});
window._taboola = window._taboola || [];
_taboola.push({
mode: 'thumbnails-a',
container: 'taboola-below-article-thumbnails-',
placement: 'Below Article Thumbnails',
target_type: 'mix'
});
The post Flu vaccines available at your nearest health facility appeared first on Belize News and Opinion on www.breakingbelizenews.com.
1 year 6 months ago
Health, last news
PAHO/WHO | Pan American Health Organization
PAHO releases toolkit to enhance management of cardiovascular risk and hypertension in the Americas
PAHO releases toolkit to enhance management of cardiovascular risk and hypertension in the Americas
Cristina Mitchell
31 Jan 2024
PAHO releases toolkit to enhance management of cardiovascular risk and hypertension in the Americas
Cristina Mitchell
31 Jan 2024
1 year 6 months ago
Health – Demerara Waves Online News- Guyana
Wear masks due to Sahara dust pollution in Guyana- EPA
The Environmental Protection Agency (EPA) is recommending that people in Guyana wear dust masks due to a high concentration of Sahara dust in parts of Guyana. Air quality monitoring stations list air quality in parts of Georgetown, East Bank Demerara and East Berbice as “unhealthy”. “The public is advised to limit their time spent outdoors ...
The Environmental Protection Agency (EPA) is recommending that people in Guyana wear dust masks due to a high concentration of Sahara dust in parts of Guyana. Air quality monitoring stations list air quality in parts of Georgetown, East Bank Demerara and East Berbice as “unhealthy”. “The public is advised to limit their time spent outdoors ...
1 year 6 months ago
Environment, Health, News
PAHO/WHO | Pan American Health Organization
PAHO calls for renewed surveillance and increased vaccination efforts as measles cases rise globally
PAHO calls for renewed surveillance and increased vaccination efforts as measles cases rise globally
Cristina Mitchell
31 Jan 2024
PAHO calls for renewed surveillance and increased vaccination efforts as measles cases rise globally
Cristina Mitchell
31 Jan 2024
1 year 6 months ago
Grenada headquarters Caribbean Family Planning Affiliation
CFPA looks forward to collaborating with WINDREF to facilitate research in the field of sexual and reproductive health and its linkages with family violence
View the full post Grenada headquarters Caribbean Family Planning Affiliation on NOW Grenada.
1 year 6 months ago
Health, caribbean family planning affiliation, curlan campbell, grenada planned parenthood association, leselle pierre romain, phillip telesford, tonia frame, windward islands research and education foundation
Insulin the answer to your weight management challenge?
MIGHT INSULIN provide the answer to your weight management challenge, when controlling calories does not help? The chances are that someone you know is struggling with weight management. It is the worldwide obesity epidemic! The World Global...
MIGHT INSULIN provide the answer to your weight management challenge, when controlling calories does not help? The chances are that someone you know is struggling with weight management. It is the worldwide obesity epidemic! The World Global...
1 year 6 months ago
How to promote proper insulin performance in your body
THE PANCREAS is a tiny gland that helps with digestion and controls sugar in your blood. It makes juices and hormones to keep you healthy. Now, the pancreas might struggle to produce enough insulin in conditions like type 1 diabetes, when the...
THE PANCREAS is a tiny gland that helps with digestion and controls sugar in your blood. It makes juices and hormones to keep you healthy. Now, the pancreas might struggle to produce enough insulin in conditions like type 1 diabetes, when the...
1 year 6 months ago
Caribbean Family Planning Affiliation relocates to Grenada
“The decision to relocate the CFPA secretariat to Grenada is the outcome of over a decade of organisational review”
View the full post Caribbean Family Planning Affiliation relocates to Grenada on NOW Grenada.
“The decision to relocate the CFPA secretariat to Grenada is the outcome of over a decade of organisational review”
View the full post Caribbean Family Planning Affiliation relocates to Grenada on NOW Grenada.
1 year 6 months ago
Health, PRESS RELEASE, caribbean family planning affiliation, cfpa, grenada planned parenthood association, patricia sheerattan-bisnauth, phillip telesford, rosmond adams, sgu, st george’s university, tonia frame
Plastic surgery deaths have spiked among US patients who traveled to Dominican Republic: CDC report
For a growing number of people, "medical tourism" can be dangerous — even fatal.
Twenty-nine U.S. citizens have died after they had cosmetic surgery in the Dominican Republic between 2009 and 2018, according to a Jan. 25 report from the Centers for Disease Control and Prevention (CDC).
For a growing number of people, "medical tourism" can be dangerous — even fatal.
Twenty-nine U.S. citizens have died after they had cosmetic surgery in the Dominican Republic between 2009 and 2018, according to a Jan. 25 report from the Centers for Disease Control and Prevention (CDC).
More alarming is that the deaths have spiked in recent years. Between 2009 and 2018, there were an average of 4.1 deaths per year. Between 2019 and 2022, that average rose to 13 per year — peaking at 17 deaths in 2020.
ASK A DOC: ‘WHAT SHOULD I DO, OR NOT DO, PRIOR TO SURGERY?’
The deaths were linked to "fat or venous thromboembolism," which is when a blood clot forms in a vein, the CDC reported.
Most of the patients had risk factors for the condition, such as obesity, diabetes, tobacco use and multiple surgical procedures being performed at once.
The Consular Section of the U.S. Embassy in the Dominican Republic has recorded cosmetic surgery-associated deaths among U.S. citizens since 2009.
The embassy contacted the CDC upon noticing the uptick in deaths — which sparked an investigation.
All but one of the deaths involved women, the report stated. The average age of the patients at the time of death was 40.
TOP PLASTIC SURGERIES: THESE WERE THE MOST IN-DEMAND PROCEDURES IN 2022
For the 24 deaths that occurred between 2019 and 2020, liposuction was performed on all of the patients, usually along with other procedures, including gluteal fat transfer, abdominoplasty and breast augmentation.
Fat embolism was the cause of death in 55% of the cases and pulmonary venous thromboembolism was the determining cause in 35% of the cases, the report said.
Josef Hadeed, M.D., chair of the Patient Safety Committee for the American Society of Plastic Surgeons (ASPS), who was not involved in the CDC investigation, noted that the CDC’s report highlights the dangers associated with destination procedures.
"Too often, patients will travel to other countries as the procedures are cheaper there," Hadeed, who is also a plastic surgeon with practices in Beverly Hills, California, and Miami, Florida, told Fox News Digital in an interview.
"However, there are a lot of risks associated with traveling to other countries for cosmetic procedures."
He added, "All surgery carries risk, but there are excessive deaths outlined in the report, most of which were presumably avoidable."
When it comes to the price of surgery, Hadeed advised patients that "you get what you pay for. Just because something is cheaper doesn't mean it is better for you."
He also said, "The most important issue in plastic surgery is patient safety."
Jonathan Kaplan, M.D., a board-certified plastic surgeon who practices at Pacific Heights Plastic Surgery in San Francisco, who was also not involved in the report, said the CDC’s latest findings are "sad but true."
"There are risks with any surgery, but in the U.S., you have a better sense of whether doctors are board-certified in the specialty they’re practicing in," he told Fox News Digital in an email.
"There is also the added risk of going to a facility in a foreign country that has no quality assurance or safety protocols as required by law in the U.S.," Kaplan added.
International travel automatically puts patients at a higher risk for thromboembolic events, where they can develop potentially fatal blood clots, Hadeed said.
Another consideration is that those having surgery outside the U.S. won’t be able to get any assistance from the doctor if any complications arise, Kaplan warned.
BBL NOT ALWAYS A-OK: WHY THE BRAZILIAN BUTT LIFT IS ONE OF THE DEADLIEST PLASTIC SURGERIES EVER
"Then you’ll have to find a doctor locally who will charge you an exorbitant amount to fix the problem and you’ll end up spending more than what you saved initially," he said.
While all surgeries carry some element of risk, the "Brazilian Butt Lift" (BBL) has been associated with the highest risk of death in plastic surgery, which is corroborated by the report, noted Hadeed.
"While I cannot specifically comment on what led to the deaths in the Dominican Republic, I can say that using an ultrasound is essential while performing a Brazilian Butt Lift," he told Fox News Digital.
When the fat is injected into one of the blood vessels within the gluteal muscle, it can enter the bloodstream and make its way to the blood vessels of the lungs, blocking off circulation and leading to immediate death — which constitutes a fat embolism, the doctor said.
ASK A DOC: 'WHAT SHOULD I KNOW BEFORE GETTING A BREAST LIFT?'
This can be prevented by using an ultrasound, he noted, which allows the plastic surgeon to visualize the gluteal muscle and ensure that the fat is placed above, and not within, the muscle.
"This has already become state law in Florida as of 2023," said Hadeed.
While Hadeed said it’s "better" to look for plastic surgeons within the U.S., if patients do decide to travel outside the country, they should carefully research a provider.
It is critical to find a plastic surgeon who is board-certified by the American Board of Plastic Surgery and is a member of the American Society of Plastic Surgeons, Hadeed emphasized.
The surgeon — as well as the entire surgical team, including the anesthesiologists, nurses and surgical techs — should be adequately trained in the specific procedures, the doctor added.
"It is equally important to ensure that the facility in which the procedure is being performed is fully accredited to the same standards that are found in the United States and has the proper safety measures in place," said Hadeed.
"Also remember that longer flights increase the risk of venous thromboembolism, and it is advised to wait several days after travel before undergoing a surgical procedure, which can add to the cost of the travel when you factor in additional days of staying in a hotel," he pointed out.
When asked for his advice on international surgery, Kaplan said simply, "Don’t do it."
"The money you save is not worth it if you have a complication, which is a very real possibility," he said.
"And remember, complications don’t have to be major — they can be minor, but still a nuisance if you don’t have a doctor locally to take care of it," he went on. "And even the smallest complication will be much more expensive to take care of in the U.S. if your original surgery was outside the country."
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
For those who are considering having an elective surgical procedure outside the U.S., the CDC recommends discussing the risks with a doctor here first.
The agency also emphasized the importance of surgeons conducting proper preoperative exams and only performing one procedure for each operation.
The study did have some limitations, the CDC acknowledged.
"No reliable statistics on the number of U.S. citizens who receive cosmetic surgery in the Dominican Republic each year are available, precluding calculation of the risk for perioperative death," the report stated.
Also, the data only included deaths that were reported to the U.S. Embassy — which means the actual number could be higher.
The mortality count also does not include deaths resulting from post-surgical infections, the CDC noted.
Fox News Digital reached out to the CDC requesting comment on the report.
1 year 6 months ago
Surgery, cosmetic-surgery, womens-health, lifestyle, health-care, beauty-and-skin, travel-safety, Health
Plastic surgery deaths have spiked among US patients who traveled to Dominican Republic: CDC report - Fox News
- Plastic surgery deaths have spiked among US patients who traveled to Dominican Republic: CDC report Fox News
- Over 90 Americans have died after cosmetic surgeries in the Dominican Republic, CDC says NBC News
- CDC Reports Deaths After Medical Tourism in the Dominican Republic Medpage Today
- 93 Americans died after cosmetic surgery in Dominican Republic over 14-year period, CDC says CBS News
1 year 6 months ago
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Medical Bulletin 29/January/2024
Here are the top medical news of the day:
Ebastine provides subjective relief among patients with non-constipated IBS
Ebastine may provide subjective relief among patients with non-constipated IBS suggests a new study published in the Gut.
Here are the top medical news of the day:
Ebastine provides subjective relief among patients with non-constipated IBS
Ebastine may provide subjective relief among patients with non-constipated IBS suggests a new study published in the Gut.
They evaluated the histamine 1 receptor antagonist ebastine as a potential treatment for patients with non-constipated irritable bowel syndrome (IBS) in a randomised, placebo-controlled phase 2 study. Non-constipated patients with IBS fulfilling the Rome III criteria were randomly assigned to 20 mg ebastine or placebo for 12 weeks. Subjects scored global relief of symptoms (GRS) and abdominal pain intensity (API). A subject was considered a weekly responder for global relief of symptoms if total or obvious relief was reported and a responder for abdominal pain intensity if the weekly average pain score was reduced by at least 30% vs baseline.
The primary endpoints were the proportion of subjects who were weekly responders for at least 6 out of the 12 treatment weeks for both global relief of symptoms and abdominal pain intensity 'GRS+API', composite endpoint) and for global relief of symptoms and abdominal pain intensity separately. Results: 202 participants (32±11 years, 68% female) were randomly allocated to receive ebastine (n=101) or placebo (n=101).
Treatment with ebastine resulted in significantly more responders (12%, 12/92) for global relief of symptoms+abdominal pain intensity compared with placebo (4%, 4/87, p=0.047) while the proportion of responders for global relief of symptoms and abdominal pain intensity separately was higher for ebastine compared with placebo, although not statistically significant (placebo vs ebastine, global relief of symptoms: 7% (6/87) vs 15%.
The study shows that ebastine is superior to placebo and should be further evaluated as a novel treatment for patients with non-constipated IBS.
Reference: Decraecker L, De Looze D, Hirsch DP, De Schepper H, Arts J, Caenepeel P, Bredenoord AJ, Kolkman J, Bellens K, Van Beek K, Pia F, Peetermans W, Vanuytsel T, Denadai-Souza A, Belmans A, Boeckxstaens G. Treatment of non-constipated irritable bowel syndrome with the histamine 1 receptor antagonist ebastine: a randomised, double-blind, placebo-controlled trial. Gut. 2024 Jan 8:gutjnl-2023-331634. doi: 10.1136/gutjnl-2023-331634. Epub ahead of print. PMID: 38191268.
Excessive gestational weight gain to cause higher risk of mortality in women
A recent study published in The Lancet revealed that excessive weight gain during pregnancy was associated with a 9% to 12% increase in all-cause mortality risk in women with BMI in the normal and overweight range respectively.
Weight gain is a common phenomenon during pregnancy, but excessive gain may be a sign of adverse health issues for mothers.
According to a study of pregnant women with low-risk pregnancy complications in Singapore, approximately 60% of them either gained too little or too much weight during pregnancy. Exceeding the recommended weight gain was associated with a higher risk of caesarean section (C-section) deliveries and the birth of larger babies – rendering this an increasingly alarming issue to be studied.
The impact of such weight gain is usually associated with greater postpartum weight retention, and pregnancy complications such as gestational diabetes, and pregnancy-induced hypertension, as well as a higher chance of requiring a C-section. However, its long-term implications have hitherto remained unknown.
Professor Cuilin Zhang from the Department of Gynaecology and Obstetrics at the Yong Loo Lin School of Medicine, National University of Singapore (NUS Medicine), and Director of the Global Center for Asian Women’s Health (GloW) at NUS Medicine and colleagues from the University of Pennsylvania and the US National Institutes of Health have investigated the association between weight gain during pregnancy, and mortality rate, with a follow-up period of over 50 years.
Excessive weight gain for women with a pre-pregnancy BMI in the underweight and normal range led to an 84% and 20% increased risk of mortality from cardiovascular disease respectively. At the same time, women with a BMI in the overweight range held a 77% increased risk of mortality from diabetes.
Considering current knowledge and the phenomenon of weight gain during pregnancy, the lack of studies and information on this renders the novel findings critical. The findings from this large well-characterised study, with more than 50 years of follow-up data, provide important evidence on the significance of women’s health for reproduction and their overall long-term health, wellbeing, and longevity.
“Promoting women’s health and achieving healthy longevity should start early in women’s lives. In particular, women’s health at their reproductive age and during pregnancy, are critical time windows that have long-term health impacts over their lifespan, as well as intergenerational impact on the offspring and the family,” said Prof Zhang, the principal investigator and last author of the study.
Reference: Stefanie N Hinkle, Prof Sunni L Mumford, Prof Katherine L Grantz, Prof Pauline Mendola, Gestational weight change in a diverse pregnancy cohort and mortality over 50 years: a prospective observational cohort study
1 year 6 months ago
MDTV,Channels - Medical Dialogues,Medical News Today MDTV,Medical News Today
Tackling hair loss can ‘transform your life’ | News - Jamaica Gleaner
Tackling hair loss can ‘transform your life’ | News
Jamaica Gleaner
1 year 6 months ago