An Arm and a Leg: Attack of the Medicare Machines
Covering the American health care system means we tell some scary stories. This episode of “An Arm and a Leg” sounds like a real horror movie.
It uses one of Hollywood’s favorite tropes: machines taking over. And the machines belong to the private health insurance company UnitedHealth Group.
Covering the American health care system means we tell some scary stories. This episode of “An Arm and a Leg” sounds like a real horror movie.
It uses one of Hollywood’s favorite tropes: machines taking over. And the machines belong to the private health insurance company UnitedHealth Group.
Host Dan Weissmann talks to Stat News reporter Bob Herman about his investigation into Medicare Advantage plans that use an algorithm to make decisions about patient care. The algorithm is owned by a subsidiary of UnitedHealth Group.
Herman tells Weissmann that some of UnitedHealth’s own employees say the algorithm creates a “moral crisis” in which care is unfairly denied.
Scary stuff! Such reporting even has caught the eye of powerful people in government, putting Medicare Advantage plans under scrutiny.
Dan Weissmann
Host and producer of "An Arm and a Leg." Previously, Dan was a staff reporter for Marketplace and Chicago's WBEZ. His work also appears on All Things Considered, Marketplace, the BBC, 99 Percent Invisible, and Reveal, from the Center for Investigative Reporting.
Credits
Emily Pisacreta
Producer
Adam Raymonda
Audio Wizard
Ellen Weiss
Editor
Click to open the Transcript
Transcript: Son of Medicare: Attack of the Machines
Note: “An Arm and a Leg” uses speech-recognition software to generate transcripts, which may contain errors. Please use the transcript as a tool but check the corresponding audio before quoting the podcast.
Dan: Hey there–
So this is kind of a horror story. But it’s not quite the kind of story it might sound like at first.
Because at first, it might sound like a horror story about machines taking over, making all the decisions– and making terrible, horrifying choices. Very age-of-Artificial Intelligence.
But this is really a story about decisions made by people. For money.
It’s also kind of a twofer sequel– like those movies that pit two characters from earlier stories against each other. Like Godzilla vs King Kong, or Alien vs Predator.
Although in this case, I’ve gotta admit, the two monsters are not necessarily fighting each other.
Let’s get reacquainted with them.
On one side, coming back from our very last episode, we’ve got Medicare Advantage: This is the version of Medicare that’s run by private insurance companies.
It’s got a bright and appealing side, compared to the traditional Medicare program run by the federal government, because: It can cost a lot less, month to month — saving people money on premiums. And it often comes with extra benefits, like dental coverage, which traditional Medicare doesn’t offer. [I know.]
But Medicare Advantage can have a dark side, which is basically: Well, you end up dealing with private insurance companies for the rest of your life. You need something — a test, a procedure, whatever — they might decide not to cover it.
Which can be scary.
Our other returning monster — am I really calling them a monster? — well, last time we talked about them, in 2023, we had an expert calling them a behemoth. That’s United HealthGroup. You might remember, they’re not only one of the biggest insurance companies
— and maybe not-coincidentally the very biggest provider of Medicare Advantage plans —
they’ve also got a whole other business– under the umbrella name Optum. And Optum has spent the last bunch of years buying up a gazillion other health care companies of every kind.
That includes medical practices — they employ more doctors than anyone else, by a huge margin. It includes surgery centers, and home-health companies, and every kind of middleman company you can imagine that works behind the scenes — and have their hands in a huge percentage of doctor bills and pharmacy visits.
A few years ago, United bought a company called NaviHealth, which provides services to insurance companies that run Medicare Advantage plans.
NaviHealth’s job is to decide how long someone needs to stay in a nursing home, like if you’re discharged from a hospital after surgery, but you’re not ready to go home yet.
And the horror story– the stories, as dug up by reporters — starts after United bought NaviHealth.
And according to their reports, it involves people getting kicked out of those nursing homes who aren’t ready to go home.
People getting sent home who can’t walk up the stairs in their house. Who can’t walk at all. Who are on feeding tubes. People who NaviHealth’s own employees are saying, “Wait. This person isn’t ready to go home.”
But their new bosses have told them: You’re not really making these decisions anymore.
This is where machines do enter the picture.
NaviHealth’s distinctive offering has always been its proprietary algorithm– an algorithm that makes predictions about how long any given patient might need to stay.
Before United bought the company, that algorithm was used as a guide, a first-guess. Humans weighed in with their own judgment about what patients needed.
After United bought the company, people inside have told reporters, that changed: The new owners basically told their employees, If the algorithm says someone can go home after x days, that’s when we’re cutting them off.
Like pretty much any horror movie, this story’s got people running around trying to tell everyone: HEY, WATCH OUT! THERE’S SOMETHING BIG AND DANGEROUS HAPPENING HERE.
And in this case, they’ve actually gotten the attention of some people who might have the power to do something about it. Now, what those people will do? We don’t know yet.
And, by the way: Yes, I said at the end of our last episode that we’d be talking about Medicaid this time around. That’s coming! But for now, strap in for this one.
This is An Arm and a Leg, a show about why health care costs so freaking much, and what we can maybe do about it. I’m Dan Weissmann. I’m a reporter, and I like a challenge. So our job on this show is to take one of the most enraging, terrifying, depressing parts of American life, and bring you something entertaining, empowering, and useful.
So. I said that, like every horror movie, this one has people who are seeing what’s going on and are trying to warn everybody?
Like those movies, we’re gonna follow one of those people, watch them discover the problem, see how deep it goes, and start ringing alarm bells. Let’s meet our guy.
Bob Herman: My name is Bob Herman. I’m a reporter at STAT News
Dan: Stat is an amazing medical news publication. Bob covers the business of medicine there. Bob started working on this story in November 2022, after talking to a source who runs nursing homes. Bob’s source was complaining about Medicare Advantage.
Bob Herman: There were a lot of payment denials. They just weren’t able to get paid. And just offhandedly, the source mentioned like, um, you know, and they’re attributing everything to this algorithm. This algorithm said, You know, only 17 days for our patients and then time’s up and I went running to Casey Ross
Dan: Casey is a reporter at Stat who focuses on tech and AI in healthcare. Bob said, hey, what do you think of this? Wanna team up?
Bob Herman: And he was hooked.
Dan: They started talking to people who worked at nursing homes, talking to experts, and talking to families. And it was clear: They were onto something.
Bob Herman: It took so many families by surprise to be like, what do you mean we’re going home? The, you know, my husband, my wife, my grandma, my grandpa, they can’t go to the bathroom on their own. Like, what do you? It was just, it was so confusing to people. It seemed like such a, a cold calculation,
Dan: One person they ended up talking with was Gloria Bent. Her husband Gary was sent to a nursing home for rehab after brain surgery for cancer. He was weak. He couldn’t walk. And he had something called “left neglect”: His brain didn’t register that there was a left side of his body. Here’s Gloria testifying before a Senate committee about how — when Gary arrived at the nursing home — the first thing he got was a discharge date. That is…
Gloria Bent: Before the staff of the facility could even evaluate my husband or develop a plan of care, I was contacted by someone who identified themselves as my Navi Health Care Coordinator
Dan: Gloria says when she told the nursing home staff she’d heard from NaviHealth, they groaned. And told her what to expect.
Gloria Bent: I was told that I had just entered a battlefield, that I could expect a series of notices of denial of Medicare payment accompanied by a discharge date that would be two days after I got that notice.
Dan: Yeah, they said she’d get two days notice. Gloria says the nursing home staff told her she’d have 24 hours to appeal each of those, but even if she won, the denials would keep coming. In fact, they said,
Gloria Bent: If we won a couple of appeals, then we could expect that the frequency with which these denials were going to come would increase.
Dan: All of which happened. NaviHealth started issuing denials July 15, 2022, after Gary had been at the home for a month.
Gloria appealed. She told senators what the doctor who evaluated the appeal found: Gary couldn’t walk. He couldn’t even move — like from bed to a chair — without help from two people.. That reviewer took Gloria’s side.
Her husband’s next denial came a week after the first. Gloria won that appeal too. She says the reviewer noted that Gary needed maximum assistance with activities of daily living.
The third denial came four days later, and this time Gloria lost.
Gary came home in an ambulance: As Gloria testified, he couldn’t get into or out of a car without assistance from someone with special training.
And when he got into the ambulance, he had a fever. The next morning, he wound up in another ambulance — headed to a hospital with meningitis. He lost a lot of the functioning he’d picked up at the nursing home.
He died at home a few months later. When Gloria testified in the Senate, all of it was still fresh. She told them that as awful as Gary’s illness and decline had been, the fights with insurance were an added trauma.
Gloria Bent: This should not be happening to families and patients. It’s cruel. Our family continues to struggle with the question that I hear you asking today. Why are people who are looking at patients only on paper or through the lens of an algorithm
making decisions that deny the services judged necessary by health care providers who know their patients.
Dan: Bob Herman calls Gloria’s story heartbreaking, like so many others he’s seen.
And his attention goes to one part of Gloria’s story beyond denial-by-algorithm.
Because: It’s not just one denial. It’s that series of denials. You can appeal, but as Gloria testified, the denials speed up. And you have to win every single time. The company only has to win once.
I mean, unless you’re ready to get a lawyer and take your chances in court– which, in addition to being a major undertaking, also means racking up nursing home bills and legal bills you may never get reimbursed for, while the court process plays out.
Bob Herman: This appeal system is designed in such a way that people will give up. If you have a job, you know, even if you don’t, and you’re, and you’re also trying to take care of a family member, um, it’s a rigorous monotonous process that will chew people up and spit them out and then the people are inevitably going to give up. And I think in some ways insurers know that.
Dan: Going out on a limb to say: I think so too. So Bob and Casey’s first story on NaviHealth came out in March of 2023. They were the characters in the movie who go, “HEY, I THINK THERE’S SOMETHING REALLY BAD HAPPENING HERE.”
And people started paying attention. Like the U.S. Senate. which held that hearing where Gloria Bent told her story.
And like the federal agency that runs Medicare — the Centers for Medicare and Medicaid Services, CMS.
CMS finalized a rule that told insurers: You can’t deny care to people just from using an algorithm.
And something else happened too: Bob and Casey started suddenly getting a lot MORE information.
Bob Herman: We received so many responses from people and it just opened the floodgates for former employees, just patients and family members, just everyone across the board.
Dan: And not just former employees. Current employees. And what they learned was: There was absolutely a strategy at work in how this algorithm was being used. It was strategy some people on the inside didn’t feel good about.
And this strategy got developed after United HealthGroup — and its subsidiary, Optum– bought NaviHealth in 2020. And here’s what NaviHealth employees started telling Casey and Bob about that strategy.
Bob Herman: For some of us, it’s creating this moral crisis. Like we know that we are having to listen to an algorithm to essentially kick someone out of a nursing home, even though we know that they can barely walk 20 feet.
Dan: What Bob and Casey learned from insiders– and how it connects to United’s role as a health care behemoth– that’s next.
This episode of An Arm and a Leg is produced in partnership with KFF Health News. That’s a nonprofit newsroom covering healthcare in America. Their reporters do amazing work, and I’m honored to work with them. We’ll have a little more about KFF Health News at the end of this episode.
So, NaviHealth — the company with the algorithm — got started in 2015.. And the idea behind it was to use data to get people home faster from nursing homes if they didn’t actually need to be there.
Because there was a lot of evidence that some people were being kept longer than they needed.
Bob Herman: There is some validity to the idea that there’s, there’s wasteful care in Medicare, like, you know, there’s been cases in the past proving that people stay in a nursing home for way longer than is necessary. And obviously there’s financial incentives for nursing homes to keep people as long as possible.
Dan: Traditional Medicare does have limits on nursing home care — but if you need “post-acute care” — help getting back on your feet after leaving a hospital traditional Medicare pays in full for 20 days– pretty much no questions asked. One of the selling points of Medicare Advantage — like selling points to policy nerds and politicians — was that it could cut waste, by asking those kinds of questions. NaviHealth and its algorithm were designed to help Medicare Advantage plans ask those questions in a smart way.
Bob Herman: There were… a lot of believers within NaviHealth that were like, okay, I think we’re doing the right thing. We’re trying to make sure people get home sooner because who doesn’t want to be at home.
Dan: And as those employees told Bob and Casey: Before United and Optum came in, the algorithm had been there as a guide — a kind of first guess — but not the final word.
NaviHealth has staff people who interact directly with patients. And back in the day, the pre-United day, Bob and Casey learned that those staff could make their own judgments.
Which made sense, because the algorithm doesn’t know everything about any individual case. It’s just making predictions based on the data it has.
Bob Herman: And there was just, just this noticeable change after United and OptiMentor that it felt more rigid. There’s no more variation.
Dan: If the algorithm says you go, you are pretty much going.
Bob Herman: United has said, no, that’s not the case, but obviously these documents and other communications that we’ve gotten kind of say otherwise.
Dan: Because these employees weren’t just talking. They were sharing. Internal memos. Emails. Training materials. All making clear: The company wanted people shipped out on the algorithm’s timetable.
Bob Herman: Documents came in showing that like this was a pretty explicit strategy. You know, UnitedHealth was telling its employees. Listen, we have this algorithm. We think it’s really good. So when it tells you how many, how many days someone should be in a nursing home, stick to it.
Dan: Stick to it or maybe be fired. Bob and Casey got documents — employee performance goals– saying: How close you stick to the algorithm’s recommendations? That’s part of how we’re evaluating your job performance.
Bob Herman: It’s okay. Algorithm said 17 days, you better not really go outside of that because your job is on the line.
Dan: Here’s how closely people were expected to stick to it. In 2022, employee performance goals shared with STAT showed that workers were expected to keep actual time in nursing homes to within three percent of what the algorithm said it should be. Across the board.
So, say you had 10 patients, and the algorithm said they each should get 10 days. That’s 100 days. Your job was to make sure that the total actual days for those patients didn’t go past 103 days.
Then, in 2023, the expectations got more stringent: Stay within one percent of the algorithm’s predictions. 10 patients, the algorithm says 100 days total? Don’t let it get past a hundred and one.
Bob Herman: Like that is, almost nothing. Like what, what, your hands are tied. If you’re that employee, what are you going to do? Are you going to get fired? Are you going to do what you’re told?
Dan: And one person who ended up talking, to did get fired.
Bob Herman: Correct. Yes. Uh, Amber Lynch did get fired And what she said was what we had also heard just more broadly was it, it created this internal conflict, like, Oh my God, what I’m doing doesn’t feel right.
Dan: Amber Lynch was a case manager. She told Bob and Casey about onepatient who couldn’t climb the stairs in his home after knee surgery. But the algorithm said he was ready. Amber’s supervisor said, “Have you asked the nursing home staff if they’ve tried to teach him butt bumping?” Amber grit her teeth and made the suggestion to the rehab director.
Amber Lynch: And she looked at me like I had two heads. She’s like, he is 78 years old. He’s not going to do that. He’s not safe to climb the stairs yet. He’s not doing it. We’re not going to have it butt bump the stairs.
Dan: Amber told Bob and Casey that when she got fired, it was partly for failing to hit the one percent target and partly for being late with paperwork– which she told Bob and Casey she fell behind because her caseload was so heavy.
She wasn’t the only one with that complaint.
Bob and Casey’s story shows another NaviHealth case manager– not named in the story because they’re still on the job — in their home office, struggling to keep up.
That week, they were supposed to work with 27 patients and their families. Gather documents, hold meetings. Another week, shortly before, they’d had 40 patients.
“Do you think I was able to process everything correctly and call everyone correctly the way I was supposed to?” the case manager asked. “No. It’s impossible. No one can be that fast and that effective and capture all of the information that’s needed.”
Bob and Casey watched this case manager fill out a digital form, feeding the algorithm the information it asked for on a man in his 80s with heart failure, kidney disease, diabetes and trouble swallowing, who was recovering from a broken shoulder.
A few minutes later, the computer spat out a number: 17 days.
The case manager didn’t have a lot of time or leeway to argue, but they were skeptical that the algorithm could get that number exactly right based on only the data it had.
And what data is the algorithm working with? What’s it comparing the data on any given patient TO? Bob Herman says that’s a big question.
Bob Herman: It’s something that for sure, like Casey and I, it’s been bothering us. Like, what, how is this whole system? Like, what is it based on? And we were never really given straight answers on that. NaviHealth and Optum and United have said it’s based on millions of patient records over time. The sources of that, it’s, it’s a little unclear, where all that’s coming from.
Dan: Bob and Casey talked with an expert named Ziad Obermeyer, a professor at the University of California Berkeley School of Public Health, who is not anti-algorithm. He actually builds algorithmic tools for decision making in public health.
AND he’s done research showing that some widely-used algorithms just scale up and automate things like racial bias.
He told Bob and Casey: Using an algorithm based on how long other, earlier patients have stayed in a nursing home — that’s not a great idea.
Because people get forced out of nursing homes, in his words, “because they can’t pay or because their insurance sucks.” He said, “So the algorightm is basically learning all the inequalities of our current system.”
And leaving aside that kind of bias, it seems unlikely to Bob that any algorithm could predict exactly what every single patient will need every single time.
No matter how much data it’s got, it’s predicting from averages.
Bob Herman: It reminds me of, like, a basketball game where let’s say someone averages 27 points per game. They don’t have 27 points every single, the game they go out there. It just varies from time to time.
Dan: But the NaviHealth algorithm doesn’t have to be right every time for United to make money using it.
Using it to make decisions can allow United to boost profits coming and going.
Bob Herman: United health and the other insurance companies that use Navi health. Are using this technology to more or less kick people out of nursing homes before they’re ready. And that is the claims denial side where it’s like, okay, let’s save as much money as we can instead of having to pay it to a nursing home.
Dan: And that’s just one side of it. The insurance side. Claims denial. But United isn’t just in the insurance business.
United’s Optum side is in every other part of health care.
Including — in the years since United took over NaviHealth — home health services. The kind of services you’re likely to need when you leave a nursing home.
In 2022, Optum bought one top home health company in what one trade publication called a “monster, jaw-dropping mega-deal” — more than 5 billion dollars. In 2023, Optum made a deal to buy a second mega-provider.
Bob and Casey’s story says NaviHealth’s shortening nursing home stays is integral to United’s strategy for these acquisitions. It does seem to open up new opportunities.
Bob Herman: You’re out of the nursing home because our algorithm said so. Now we’re going to send you to a home health agency or we’re going to send some home health aides into your home. And by the way, we own them.
Dan: Oh, right, because: If you’re in a Medicare Advantage plan, your insurer can tell you which providers are covered.
Bob Herman: So the real question becomes, how much is United potentially paying itself?
Dan: That is: How much might United end up taking money out of one pocket — the health insurance side — and paying itself into another pocket, Optum’s home-health services?
We don’t know the answer to how much United is paying itself in this way, or hoping to. And United has said its insurance arm doesn’t favor its in-house businesses.
But it seems like a reasonable question to ask. Actually, it’s a question the feds seem to be asking.
Optum hasn’t wrapped up its purchase of that second home-health company yet, and in February 2024, the Wall Street Journal and other outlets reported that the U.S. Department of Justice had opened an anti-trust investigation.
And you don’t have to be in a Medicare Advantage plan run by United to get kicked out of a nursing home on an algorithm’s say-so.
Bob Herman says NaviHealth sells its algorithm-driven services to other big insurance companies
He says, put together, the companies that use NaviHealth cover as many as 15 million people — about half of everybody in Medicare Advantage.
Bob Herman: Odds are, if you’re in a Medicare Advantage plan, there’s a, there’s a really good shot that your coverage policies, if you get really sick and need nursing home care, for example, or any kind of post acute care, an algorithm could be at play at some point.
Dan: This is the dark side of Medicare Advantage.
Bob Herman: Everyone loves their Medicare Advantage plan when they first sign up, right? Because it’s offering all these bells and whistles. It’s, here’s a gym membership. It’s got dental and vision, which regular Medicare doesn’t have. And it’s also just, it’s, it’s cheaper. Like, if it’s just from a financial point of view, if, if you’re a low income senior, How do you turn it down? There’s, there’s so many plans that offer like free, there’s no monthly premiums in addition to all the bells and whistles. But Nobody understands the trade offs , When you’re signing up for Medicare and Medicare Advantage, you’re on the healthier side of, of being a senior, right?
Dan: And none of us can count on staying healthy forever. When you sign up for Medicare you’re signing up your future self — whether that’s ten or twenty or more years out. That future you, might really need good medical care.
And at that point, as we explained in our last episode, if Medicare Advantage isn’t working for you, you may not be able to get out of it.
Bob Herman: You could potentially not fully get the care that you need. We shouldn’t assume that, that this couldn’t happen to us because it can.
Dan: So, yeah. Kind of a horror story. But: Unlike some horror movies, when Bob and Casey started publishing their stories, they started getting people’s attention.
We mentioned the new rules from the feds and the senate hearings after Bob and Casey’s first story in March 2023
Later in the year, when Bob and Casey published their story with documents and stories from inside NaviHealth, a class-action lawsuit got filed.
Since then, CMS has said it will step up audits under its new rules.
Bob Herman: There was a memo that CMS sent out to Medicare advantage plans that said, Hey, listen, we’re telling you again, do not deny care solely on any AI or algorithms. Like just don’t do it.
Dan: And in February 2024, the Senate held another hearing.
Here’s Senator Elizabeth Warren at that hearing, saying these CMS rules aren’t enough. We need stronger guardrails.
Elizabeth Warren: Until CMS can verify that AI algorithms reliably adhere to Medicare coverage standards by law, then my view on this is CMS should prohibit insurance companies from using them in their MA plans for coverage decisions. They’ve got to prove they work before they put them in place.
Dan: So people — people with at least some power– are paying some attention.
Bob Herman: I don’t think this is necessarily going to escape. Political scrutiny for a while.
Dan: So, basically, the story isn’t over.
This isn’t one of those horror movies where the monster’s been safely defeated at the end, and everybody just starts cleaning up the mess. And it’s not one where the monster is just on the loose, unleashing the apocalypse.
Because it’s not a movie. There’s no ending. There’s just all of us trying to figure out what’s going on, and what we can maybe do about it.
One last thing: I got a lot of emails after our last episode, where we laid out a lot of information about Medicare Advantage and traditional Medicare. Most of it was along the lines of, Thank you! That was really helpful! Which made me feel really good.
And we got a couple notes about things we could have done better. Especially this: We said Traditional Medicare leaves you on the hook for 20 percent of everything, without an out of pocket limit.
Which is true — but only for Medicare Part B: Doctor visits, outpatient surgeries and tests. Which can add up, for sure.
Medicare Part A — if you’re actually hospitalized — covers most services at 100 percent, after you meet the deductible. In 2024 that’s one thousand, six hundred thirty-two dollars.
Thanks to Clarke Lancina for pointing that out.
There have been a bunch of other, amazing notes in my inbox recently, and I want to say: Please keep them coming.
If you go to arm and a leg show dot com, slash, contact, whatever you type there goes straight to my inbox. You can attach stuff too: documents… voice memos.
Please let me hear from you. That’s arm and a leg show dot com, slash contact.
I’ll catch you in a few weeks.
Till then, take care of yourself.
This episode of an arm and a leg was produced by me, Dan Weissmann, with help from Emily Pisacreta, and edited by Ellen Weiss.
Adam Raymonda is our audio wizard. Our music is by Dave Weiner and blue dot sessions. Extra music in this episode from Epidemic Sound.
Gabrielle Healy is our managing editor for audience. She edits the first aid kit newsletter.
Bea Bosco is our consulting director of operations. Sarah Ballama is our operations manager.
And Arm and a Leg is produced in partnership with KFF Health News. That’s a national newsroom producing in depth journalism about healthcare in America and a core program at KFF, an independent source of health policy research, polling and journalism.
Zach Dyer is senior audio producer at KFF Health News. He’s editorial liaison to this show.
And thanks to the Institute for Nonprofit News for serving as our fiscal sponsor, allowing us to accept tax exempt donations. You can learn more about INN at INN. org.
Finally, thanks to everybody who supports this show financially– you can join in any time at arm and a leg show dot com, slash, support — and thanks for listening.
“An Arm and a Leg” is a co-production of KFF Health News and Public Road Productions.
To keep in touch with “An Arm and a Leg,” subscribe to the newsletter. You can also follow the show on Facebook and the social platform X. And if you’ve got stories to tell about the health care system, the producers would love to hear from you.
To hear all KFF Health News podcasts, click here.
And subscribe to “An Arm and a Leg” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 2 months ago
Health Care Costs, Health Industry, Insurance, Medicaid, Medicare, Multimedia, An Arm and a Leg, Podcasts
Adultos mayores, agotados por tener que organizar tanta atención médica
En enero, Susanne Gilliam, de 67 años, estaba yendo a recoger el correo afuera de su casa cuando se cayó al resbalar sobre una capa de hielo negro.
Sintió una punzada de dolor en la rodilla y el tobillo de la pierna izquierda. Después de llamar a su marido por teléfono, logró regresar a su casa con dificultad.
En enero, Susanne Gilliam, de 67 años, estaba yendo a recoger el correo afuera de su casa cuando se cayó al resbalar sobre una capa de hielo negro.
Sintió una punzada de dolor en la rodilla y el tobillo de la pierna izquierda. Después de llamar a su marido por teléfono, logró regresar a su casa con dificultad.
Y así comenzó el vaivén interminable que tantas personas enfrentan cuando tienen que navegar el desorganizado sistema de salud de Estados Unidos.
El cirujano ortopédico de Gilliam, que la había tratado antes por problemas en la misma rodilla, la vio esa tarde pero le aclaró: “Yo no me ocupo de tobillos”.
La derivó a un especialista en tobillos que ordenó nuevas radiografías y una resonancia magnética. Gilliam pidió hacerse las pruebas en un hospital cerca de su casa en Sudbury, Massachusetts, que le resultaba más conveniente. Pero cuando llamó para pedir una cita, el hospital no tenía la orden del doctor, que finalmente llegó después de varias llamadas más.
Coordinar la atención que necesita para recuperarse, incluyendo sesiones de fisioterapia, se convirtió en un trabajo de medio tiempo para Gilliam. (Los terapeutas trabajan solo en una parte del cuerpo por sesión, y por lo tanto Gilliam requiere visitas separadas para su rodilla y su tobillo, varias veces a la semana).
“El peso de organizar todo lo que necesito es enorme”, dijo Gilliam. “Te queda una sensación de agotamiento físico y mental”.
En algunos casos, las deficiencias del sistema de salud son el precio que se paga por avances extraordinarios en el campo de la medicina. Pero también ponen en evidencia las incoherencias entre las capacidades de los adultos mayores y las demandas del sistema.
“La buena noticia es que sabemos mucho más y podemos hacer mucho más por las personas con distintas afecciones”, dijo Thomas H. Lee, director médico de Press Ganey, una consultoría que hace seguimiento de las experiencias de los pacientes con el sistema de salud. “La mala noticia es que el sistema se ha vuelto tremendamente complejo”.
Esto se agrava por las múltiples guías para tratar afecciones, la super especialización médica, y los incentivos financieros que hacen que los pacientes reciban cada vez más atención, dijo Ishani Ganguli, profesora asociada en la Escuela de Medicina de Harvard.
“No es raro que pacientes mayores tengan tres o más cardiólogos que les programan citas y pruebas regulares”, dijo. Si alguien tiene varios problemas de salud (por ejemplo, enfermedades cardíacas, diabetes y glaucoma), las interacciones con el sistema se multiplican.
Ganguli es la autora de un nuevo estudio que muestra que los pacientes de Medicare dedican aproximadamente tres semanas al año a hacerse pruebas médicas, ver a doctores, someterse a tratamientos o procedimientos médicos, buscar atención en salas de emergencia o pasar tiempo en el hospital o en centros de rehabilitación. (Los datos son de 2019, antes de la pandemia de covid, que alteró los patrones de atención médica. Cada servicio recibido se contó como un día de contacto con el sistema de salud).
El estudio determinó que poco más de 1 de cada 10 personas mayores, incluyendo las que se estaban haciendo controles o recuperándose de enfermedades graves, pasaban más tiempo recibiendo atención médica: al menos 50 días al año.
“Hay aspectos de esto que son muy beneficiosos y valiosos para las personas, pero hay otros que son menos esenciales”, dijo Ganguli. “No hablamos lo suficiente sobre lo que les pedimos a los adultos mayores que hagan, y si tiene sentido”.
Victor Montori, profesor de medicina de la Clínica Mayo en Rochester, Minnesota, lleva muchos años advirtiendo sobre lo que llama la “carga de tratamiento” que enfrentan los pacientes.
Esto incluye el tiempo que dedican a recibir atención médica, programar citas, encontrar transporte para las visitas médicas, obtener y tomar medicamentos, comunicarse con las aseguradoras, pagar facturas médicas, monitorear su salud en casa y seguir consejos como cambios en la dieta.
Hace cuatro años, en un artículo titulado “¿Se siente mi paciente agobiado?”, Montori y sus colegas descubrieron que el 40% de los pacientes con enfermedades crónicas como asma, diabetes y trastornos neurológicos “sentían que su carga de tratamiento era insostenible”.
Cuando la carga de tratamiento es excesiva, las personas dejan de seguir las recomendaciones médicas y dicen que su calidad de vida empeora, según los investigadores. Los adultos mayores con múltiples afecciones médicas y bajo nivel de educación son especialmente vulnerables, ya que experimentan inseguridad económica y aislamiento social.
El uso cada vez más frecuente de sistemas telefónicos digitales y portales electrónicos para pacientes en los consultorios y la falta de tiempo por parte de los doctores profundizan las barreras. “Cada vez es más difícil para los pacientes acceder a doctores que puedan pasar tiempo con ellos, para ayudarlos a resolver problemas y responder sus preguntas”, dijo Montori.
Mientras tanto, los médicos rara vez preguntan a los pacientes sobre su capacidad para realizar las tareas que se les pide. “A menudo tenemos poca idea de qué tan compleja es la vida de nuestros pacientes”, escribieron médicos en un informe de 2022 sobre cómo reducir la carga de tratamiento.
Un ejemplo es lo que vivieron Jean Hartnett, de 53 años de Omaha, Nebraska, y sus ocho hermanos después que su madre de 88 años sufriera un derrame cerebral en febrero de 2021, mientras hacían compras en Walmart.
En ese momento, su madre estaba cuidando al padre de Hartnett, quien sufría de una enfermedad renal y necesitaba ayuda con las tareas diarias, como ducharse o ir al baño.
Durante el año posterior al derrame cerebral, los padres de Hartnett, ambos trabajadores agrícolas extremadamente independientes que vivían en Hubbard, Nebraska, sufrieron varios achaques y las crisis médicas se volvieron comunes.
Cuando un médico cambiaba el plan de atención de su mamá o su papá, eran necesarios nuevos medicamentos, suministros y equipos médicos, y programar nuevas sesiones de terapia ocupacional, física y del habla.
Ninguno de los padres podía quedarse solo si el otro necesitaba atención médica.
“No era inusual para mí estar llevando a uno de mis padres a su casa después del hospital o de la visita al médico y pasar una ambulancia o un familiar transportando al otro al doctor”, explicó Hartnett. “Se necesitaba muchísima coordinación”.
Hartnett se mudó a la casa de sus padres durante las últimas seis semanas de vida de su padre, cuando los médicos decidieron que estaba demasiado débil como para someterse a diálisis. Falleció en marzo de 2022. Su madre murió meses después, en julio.
Entonces, ¿qué pueden hacer los adultos mayores y sus cuidadores y familiares para aliviar la carga de la atención médica?
Para empezar, es importante sincerarse con el médico si el plan de tratamiento que recomienda no resulta factible, y explicarle por qué, dijo Elizabeth Rogers, profesora asistente de medicina interna en la Escuela de Medicina de la Universidad de Minnesota.
Recomendó preguntar sobre cuáles intervenciones serían las más importantes para mantenerse saludable y cuáles podrían ser prescindibles.
Los médicos pueden ajustar los planes, suspender los medicamentos que no producen beneficios significativos y programar visitas virtuales, en caso de que las personas puedan manejar la tecnología necesaria (muchos adultos mayores no pueden).
Pregunte también si un asistente de pacientes (también llamados navegadores) puede ayudarle a programar varias citas y exámenes en el mismo día, para minimizar la carga de ir y venir de los centros médicos. Estos profesionales también pueden ayudarlo a conectarse con recursos comunitarios, como servicios de transporte. (La mayoría de los centros médicos tienen personal de este tipo, pero los consultorios médicos no).
Si no entiende cómo hacer lo que su médico pide, pregunte: ¿Qué implicaría esto de mi parte? ¿Cuánto tiempo llevaría? ¿Qué necesitaré? Y pida materiales escritos, como guías de autocontrol del asma o la diabetes, que puedan ayudarle a comprender mejor los requisitos.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 2 months ago
Aging, Health Care Costs, Health Industry, Insurance, Medicare, Navigating Aging, Noticias En Español, Massachusetts, Nebraska
En California, la cobertura de salud ampliada a inmigrantes choca con las revisiones de Medicaid
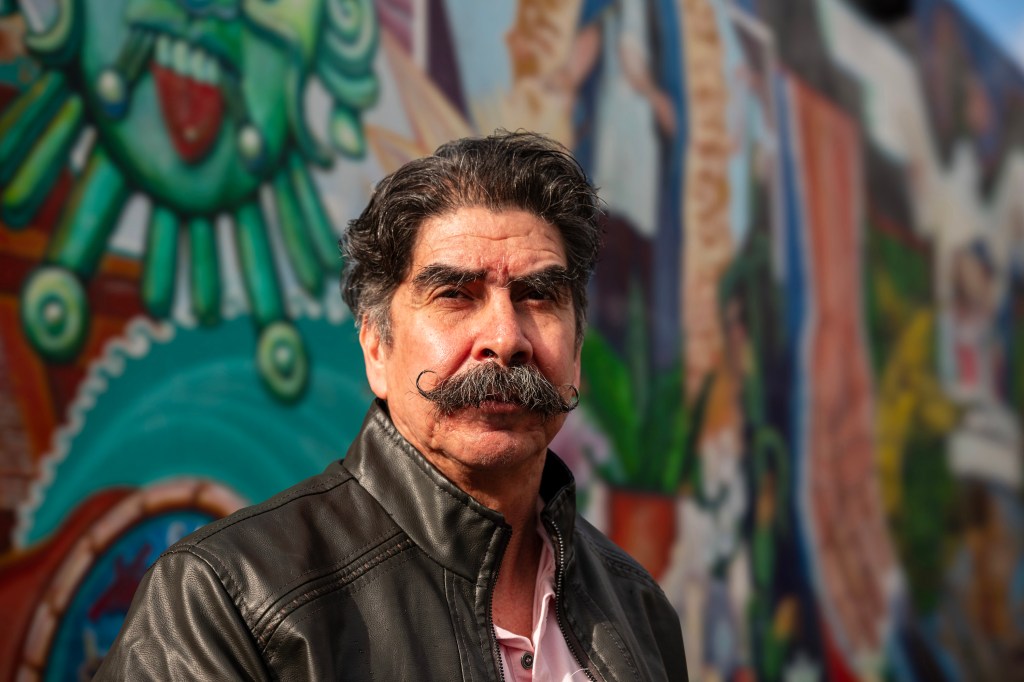
OAKLAND, California – El Medi-Cal llegó a Antonio Abundis cuando el conserje más lo necesitaba.
Poco después que Abundis pasara de tener cobertura limitada a una cobertura completa en 2022, bajo la expansión del Medi-Cal de California para adultos mayores sin papeles, fue diagnosticado con leucemia, un tipo de cáncer que afecta las células de la sangre.
OAKLAND, California – El Medi-Cal llegó a Antonio Abundis cuando el conserje más lo necesitaba.
Poco después que Abundis pasara de tener cobertura limitada a una cobertura completa en 2022, bajo la expansión del Medi-Cal de California para adultos mayores sin papeles, fue diagnosticado con leucemia, un tipo de cáncer que afecta las células de la sangre.
El padre de tres hijos, de voz suave, tomó la noticia con calma cuando su médico le dijo que sus análisis de sangre sugerían que su cáncer no estaba en una etapa avanzada. Sus siguientes pasos fueron hacerse más pruebas y tener un plan de tratamiento con un equipo de cáncer en Epic Care, en Emeryville.
Pero todo eso se fue por la borda cuando se presentó en julio pasado para hacerse un análisis de sangre en La Clínica de La Raza en Oakland, y le dijeron que ya no era beneficiario de Medi-Cal.
“Nunca mandaron una carta ni nada de que a mí me la había negado”, dijo Abundis, ahora de 63 años, sobre la pérdida de su cobertura.
Abundis es uno de los cientos de miles de latinos de California que han sido expulsados de Medi-Cal —el programa estatal de Medicaid para personas de bajos ingresos— a medida que los estados reanudaban las verificaciones de elegibilidad, que se habían suspendido en el punto más álgido de la pandemia de covid-19.
El proceso de redeterminación ha afectado de forma desproporcionada a los latinos, que constituyen la mayoría de los beneficiarios de Medi-Cal.
Según el Departamento de Servicios de Salud de California (DHCS), más de 613,000 de los 1,24 millones de residentes que fueron dados de baja se identifican como latinos. Algunos, incluido Abundis, habían obtenido la cobertura poco tiempo antes, cuando el estado comenzó a expandir Medi-Cal para ofrecer cobertura a inmigrantes indocumentados.
El choque entre las políticas estatales y las federales no sólo ha significado un duro golpe para los beneficiarios: también disparó la demanda de asistencia para realizar los trámites de inscripción.
Esto ocurre porque muchas personas son excluidas de Medi-Cal por cuestiones administrativas.
Los grupos de salud que trabajan con las comunidades latinas informan que están inundados de solicitudes de ayuda. Al mismo tiempo, una encuesta patrocinada por el estado sugiere que los hogares hispanos tienen más probabilidades que otros grupos étnicos o raciales de perder la cobertura porque tienen menos información sobre el proceso de renovación.
También pueden tener dificultades para defenderse por sí solos.
Algunos defensores de salud están presionando para que haya una pausa en este proceso. Advierten que las desafiliaciones no solo socavarán los esfuerzos del estado para reducir el número de personas sin seguro, sino que podrían exacerbar las disparidades en salud, especialmente para un grupo étnico que sufrió fuerte el peso de la pandemia.
Un estudio nacional encontró que los latinos en el país tuvieron tres veces más probabilidades de desarrollar covid y el doble de probabilidades de morir a causa de la enfermedad que la población en general, en parte porque tienden a vivir en hogares más hacinados o multigeneracionales y tienen trabajos en servicios, de cara al público.
“Estas dificultades nos colocan a todos como comunidad en un estatus más frágil, en el cual la red de seguridad es aún más significativa”, dijo Seciah Aquino, directora ejecutiva de la Latino Coalition for a Healthy California, una organización de defensa de salud.
La asambleísta Tasha Boerner (demócrata de Encinitas) ha presentado un proyecto de ley que desaceleraría las bajas permitiendo que las personas de 19 años o más mantengan automáticamente su cobertura durante 12 meses, y extendiendo las políticas flexibles de la era pandémica, como no requerir prueba de ingresos para renovar la cobertura en ciertos casos. Esto beneficiaría a los hispanos, que representan casi el 51% de la población de Medi-Cal en comparación con el 40% de la población total del estado.
La oficina del gobernador dijo que no comenta sobre proyectos legislativos que están aún en proceso.
Tony Cava, vocero del Departamento de Servicios de Atención Médica (DHCS), dijo en un correo electrónico que la agencia ha tomado medidas para aumentar el número de personas reinscritas automáticamente en Medi-Cal y no cree que sea necesaria una pausa. La tasa de desafiliación disminuyó un 10% de noviembre a diciembre, apuntó Cava.
Sin embargo, funcionarios estatales reconocen que se podría hacer más para ayudar a las personas a completar sus solicitudes. “Todavía no estamos llegando a ciertos sectores”, dijo Yingjia Huang, subdirectora adjunta de beneficios de atención médica y elegibilidad del DHCS.
California fue el primer estado en ampliar la elegibilidad de Medicaid a todos los inmigrantes que calificaran, sin importar su estatus migratorio, implementándolo gradualmente durante varios años: niños en 2016, adultos jóvenes de 19 a 26 años en 2020, personas de 50 años en adelante en 2022, y todos los adultos restantes este año.
Pero California, como otros estados, reanudó las verificaciones de elegibilidad en abril pasado, y se espera que el proceso continúe hasta mayo. El estado ahora está viendo que las tasas de desafiliación vuelven a los niveles previos a la pandemia, o el 19%-20% de la población de Medi-Cal cada año, según el DHCS.
Jane García, directora ejecutiva de La Clínica de La Raza, testificó ante el Comité de Salud de la Junta de Supervisores del condado de Alameda que las desafiliaciones siguen siendo un desafío, justo cuando su equipo intenta inscribir a residentes recién elegibles. “Es una carga enorme para nuestro personal”, les dijo a los supervisores en enero.
Aunque muchos beneficiarios ya no califican porque sus ingresos aumentaron, muchos más han sido eliminados de los registros por no responder a avisos o devolver documentos. En muchos casos, los paquetes de documentos para renovar la cobertura se enviaron a direcciones antiguas. Muchos se enteran de que perdieron la cobertura recién cuando van al médico.
“Sabían que algo estaba pasando”, dijo Janet Anwar, gerenta de elegibilidad en el Tiburcio Vásquez Health Center, en East Bay. “No sabían exactamente qué era, cómo los iba a afectar hasta que llegó el día y fueron desafiliados. Y estaban haciéndose un chequeo, o programando una cita, y luego… ‘Oye, perdiste tu cobertura'”.
Y la reinscripción es un desafío. Una encuesta patrocinada por el estado publicada el 12 de febrero por la California Health Care Foundation halló que el 30% de los hogares hispanos intentaron completar un formulario de renovación sin suerte, en comparación con el 19% de los hogares blancos no hispanos. Y el 43% de los hispanos informaron que les gustaría volver a comenzar con Medi-Cal, pero no sabían cómo, en comparación con el 32% de las personas en hogares blancos no hispanos.
La familia Abundis está entre las que no saben dónde obtener respuestas a sus preguntas. Aunque la esposa de Abundis envió la documentación de renovación de Medi-Cal para toda la familia en octubre, ella y dos hijos que aún viven con ellos pudieron mantener la cobertura; Abundis fue el único que la perdió.
No ha recibido una explicación de por qué lo sacaron de Medi-Cal ni ha sido notificado de cómo apelar o volver a solicitarlo.
Ahora se preocupa de que tal vez no califique por sí solo según sus ingresos anuales de aproximadamente $36,000, ya que el límite es de $20,121 para un individuo, pero de $41,400 para una familia de cuatro.
Es probable que un navegador pueda verificar si él y su familia califican como hogar para Medi-Cal. Covered California, el mercado de seguros de salud estatal, ofrece planes privados que pueden costar menos de $10 al mes en primas y permite una inscripción especial cuando las personas pierden Medi-Cal o la cobertura del empleador. Pero los inmigrantes que no viven legalmente en el estado no califican para los subsidios de Covered California. Abundis supone que no podrá pagar las primas ni los copagos, por lo que no presentó la solicitud.
Pero Abundis supone que no podrá pagar primas o copagos, así que no ha presentado una solicitud.
Abundis, quien visitó a un médico por primera vez en mayo de 2022 debido a una fatiga sin causa aparente, dolor constante en la espalda y las rodillas, falta de aliento y pérdida de peso inexplicable, teme no poder pagar la atención médica. La Clínica de La Raza, el centro de salud comunitario en donde le hicieron análisis de sangre, lo ayudó ese día a que no tuviera que pagar por adelantado, pero desde entonces dejó de buscar atención médica.
Más de un año después de su diagnóstico, todavía no sabe en qué etapa del cáncer se encuentra ni cuál debería ser su plan de tratamiento. Aunque la detección temprana del cáncer puede aumentar las posibilidades de supervivencia, algunos tipos de leucemia avanzan rápidamente. Sin más pruebas, Abundis no conoce su pronóstico.
Yo estoy mentalizado”, dijo Abundis sobre su cáncer. “Lo que pase, pase”.
Incluso aquellos que buscan ayuda se topan con desafíos. Marisol, una inmigrante mexicana sin papeles, de 53 años, que vive en Richmond, California, intentó restablecer la cobertura durante meses. Aunque el estado experimentó una caída del 26% en las bajas de diciembre a enero, la proporción de latinos a los que se les canceló la cobertura durante ese período permaneció casi igual, lo que sugiere que enfrentan más barreras para la renovación.
Marisol, quien pidió que se usara su nombre de pila por temor a la deportación, también calificó para la cobertura completa de Medi-Cal durante la expansión estatal a todos los inmigrantes de 50 años en adelante.
En diciembre, recibió un paquete informándole que los ingresos de su hogar excedían el umbral de Medi-Cal, algo que ella creyó que era un error. El esposo de Marisol está sin trabajo debido a una lesión en la espalda, dijo, y sus dos hijos mantienen a su familia principalmente con trabajos de medio tiempo en Ross Dress for Less.
Ese mes, Marisol visitó una sucursal de Richmond del Departamento de Empleo y Servicios Humanos del condado de Contra Costa, con la esperanza de hablar con un navegador. En cambio, le dijeron que dejara su documentación y que llamara a un número de teléfono para verificar el estatus de su solicitud.
Desde entonces, llamó muchas veces y pasó horas en espera, pero no ha podido hablar con nadie. Los funcionarios del condado reconocieron tiempos de espera más prolongados debido al aumento de llamadas, y dijeron que el tiempo promedio es de 30 minutos.
“Entendemos la frustración de los miembros de la comunidad cuando a veces tienen dificultades para comunicarse”, escribió la vocera Tish Gallegos en un correo electrónico. Gallegos señaló que el centro de llamadas aumenta la dotación de personal durante las horas pico.
Después que El Tímpano contactara al condado para hacer comentarios, Marisol dijo que un trabajador de elegibilidad la contactó, y le explicó que su familia fue dada de baja porque sus hijos habían presentado impuestos por separado, por lo que el sistema de Medi-Cal determinó su elegibilidad individualmente en lugar de como familia.
El condado reintegró a Marisol y a su familia el 15 de marzo. Marisol dijo que recuperar Medi-Cal fue un final alegre pero agridulce para una lucha de meses, especialmente sabiendo que otras personas son desafiliadas por cuestiones de procedimiento. “Tristemente, tiene que haber presión para que arreglen algo”, dijo.
Jasmine Aguilera de El Tímpano está participando de la Journalism & Women Symposium’s Health Journalism Fellowship, apoyada por The Commonwealth Fund. Vanessa Flores, Katherine Nagasawa e Hiram Alejandro Durán de El Tímpano colaboraron con este artículo.
[Corrección: este artículo se actualizó a la 1:30 pm (ET), el 26 de marzo de 2024, para corregir los detalles sobre la elegibilidad para recibir asistencia financiera para pagar las primas de los seguros. Los inmigrantes que no viven legalmente en California no califican para los subsidios de Covered California].
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 2 months ago
Health Care Costs, Insurance, Medi-Cal, Medicaid, Noticias En Español, Race and Health, States, Uninsured, Cancer, Latinos, Out-Of-Pocket Costs
Los hirieron en el desfile del Super Bowl: un mes después se sienten olvidados
Este año, Jason Barton no quería ir al desfile del Super Bowl. La noche anterior le dijo a un compañero de trabajo que estaba preocupado por que ocurriera un tiroteo masivo. Pero era San Valentín, su esposa es fanática de los Kansas City Chiefs y él no podía permitirse pagar las entradas a los partidos, que habían aumentado muchísimo tras la victoria del equipo en el campeonato de 2020.
Así que Barton condujo 50 millas desde Osawatomie, Kansas, hasta el centro de Kansas City, Missouri, con su esposa Bridget, Gabriella, su hija de 13 años, y una amiga del colegio de la niña. Cuando por fin regresaron esa noche a casa, tuvieron que limpiar sangre de las zapatillas de Gabriella y encontraron una bala en la mochila de Bridget.
Gabriella tenía quemaduras en las piernas por los chispazos de una bala que rebotó cerca de ella, Bridget había sido pisoteada mientras protegía a su hija en medio del caos, y Jason le había practicado masajes cardíacos a un hombre herido de bala: cree que era Lyndell Mays, uno de los dos acusados de asesinato.
“Se supone que San Valentín es un día en el que nos divertimos y celebramos a nuestros afectos. Pero ya nunca habrá un San Valentín en el que no me acuerde de esto”, dijo Gabriella.
Un mes después del desfile —en el que esa crisis de salud pública que es la violencia armada en el país se transmitió por televisión en vivo— los Barton siguen impactados por el papel que les tocó en el epicentro de los acontecimientos.
Se encontraban a escasos metros de Lisa López-Galván, de 43 años, que fue asesinada. Otras 24 personas resultaron heridas. Los Barton no están incluidos en el número oficial de víctimas, sin embargo, quedaron traumatizados, física y emocionalmente, y el dolor impregna sus vidas.
Ahora, Bridget y Jason prefieren quedarse juntos en casa y siguen cancelando planes para salir; Gabriella cambió de proyecto y en vez de tomar clases de baile se anotó en un club de boxeo.
Durante el primer mes, los líderes comunitarios de Kansas City han discutido cómo atender a las personas que quedaron atrapadas bajo el fuego cruzado y cómo distribuir los más de $2 millones donados a los fondos públicos para las víctimas bajo el doloroso impacto inicial.
Hay muchas preguntas: ¿cómo compensar a las personas por los gastos en atención médica y psicológica, por los tratamientos de recuperación, por los salarios perdidos? ¿Qué ocurre con quienes padecen síntomas de estrés post traumático (TEPT), que pueden durar años? ¿Cómo hace una comunidad para identificar y atender a los heridos, que son las víctimas que a menudo se pasan por alto en los primeros informes sobre un tiroteo masivo?
Y la lista de heridos podría aumentar. Mientras investigan a cuatro de los sospechosos del tiroteo, la fiscalía y la policía de Kansas City convocan a otras víctimas a presentarse.
“En concreto, buscamos personas que hayan sufrido heridas cuando intentaban escapar y se produjo la estampida”, explicó la fiscal del condado de Jackson, Jean Peters Baker. Alguien que, “mientras huía, se cayó, se torció un tobillo, se rompió un hueso o lo pisotearon”.
Mientras tanto, las personas que se encargaron de recaudar dinero y facilitar la atención de los heridos debaten los criterios para distribuirlo. Gracias a las cuantiosas donaciones de famosos como Taylor Swift y Travis Kelce, algunas víctimas o sus familias dispondrán de cientos de miles de dólares para gastos médicos. A otras es posible que solo se les cubra la terapia.
Una investigación reciente de la Facultad de Medicina de Harvard calcula que el costo económico global de las lesiones causadas por armas de fuego en Estados Unidos asciende a $557,000 millones anuales. El 88% de ese monto se explica por la pérdida de calidad de vida de las personas heridas y sus familias. El estudio revela que, solo en el primer año, cada lesión no mortal por arma de fuego genera unos $30,000 de gastos de salud directos por superviviente.
Inmediatamente después de los tiroteos, mientras aparecían páginas como GoFundMe para ayudar a las víctimas, los ejecutivos de United Way of Greater Kansas City se reunieron para idear una respuesta colectiva de donación. Se les ocurrieron “tres círculos concéntricos de víctimas”, explicó Jessica Blubaugh, directora de Filantropía de United Way, y lanzaron la campaña #KCStrong.
“Obviamente, en el primer círculo estás las personas que sufrieron directamente el impacto de los disparos. En el siguiente círculo se encuentran los que sufrieron un impacto físico —no necesariamente de los disparos—, por ejemplo, personas que fueron pisoteadas o se rompieron un ligamento cuando estaban huyendo”, dijo Blubaugh. “Luego, en tercer lugar, están las personas que se encontraban en las inmediaciones y los transeúntes, que quedaron psicológicamente muy afectados”.
Estrés post traumático, pánico y el eco de los disparos
Bridget Barton regresó a Kansas City al día siguiente del tiroteo para entregar la bala que había encontrado en su mochila y declarar en la comisaría.
Ella no lo sabía, pero el alcalde Quinton Lucas y los jefes de policía y bomberos acababan de terminar una rueda de prensa fuera del edificio. Bridget fue acosada por los periodistas allí reunidos, entrevistas que ahora le resultan borrosas. “No sé cómo hacen esto todos los días”, recuerda que le dijo a un detective cuando por fin pudo entrar.
Mientras atraviesan el trauma, los Barton se han visto abrumados, al punto del agotamiento, por las buenas intenciones de amigos y familiares. Bridget usó las redes sociales para explicar que no ignoraba los mensajes pero que los iba respondiendo en la medida que podía. Algunos días apenas puedo mirar el teléfono, contó.
Una amiga de la familia compró nuevas mantas de Barbie para Gabriella y su amiga; las que llevaron al desfile se perdieron o estropearon. Bridget había intentado reemplazar ella misma las mantas en Walmart. Pero alguien la empujó accidentalmente y le dio un ataque de pánico. Así que abandonó el carrito y condujo de vuelta a casa.
“Estoy intentando controlar mi ansiedad”, cuenta Bridget. Eso significa que necesita terapia. Antes del desfile ya consultaba a un terapeuta y planeaba empezar la desensibilización y reprocesamiento por movimientos oculares, un método asociado al tratamiento del TEPT. Ahora, de lo primero que quiere hablar en terapia es del tiroteo.
Desde que Gabriella, alumna de 8vo grado, volvió a la escuela, tiene que lidiar con la inmadurez propia de la adolescencia: compañeros que la instan a superar lo ocurrido, que la señalan con el dedo o que incluso le dicen que debería haber sido ella la asesinada. Pero sus amigos la contienen y le preguntan cómo está. Le gustaría que más gente hiciera lo mismo con su amiga, que salió corriendo cuando empezó el tiroteo y así evitó que la hirieran. Gabriella se siente culpable por haberla llevado a lo que se convirtió en una experiencia aterradora.
“Podemos decirle todo el día: ‘No fue culpa tuya. No es tu responsabilidad’, lo mismo que yo me digo: ‘No fue culpa mía, ni mi responsabilidad'”, explica Bridget. “Pero igualmente lloré en el hombro de la madre de la otra niña diciéndole lo mucho que sentía haber agarrado primero a mi hija”.
Desde el tiroteo, las dos niñas han pasado mucho tiempo hablando. Según Gabriella, eso la ayuda a aliviar su propio estrés. También la alivia pasar tiempo con su perro y con su lagartija, maquillarse y escuchar música: la actuación del rapero Tech N9ne fue para ella un momento culminante de la celebración del Super Bowl.
Además de que las chispas le quemaron las piernas, en la estampida Gabriella cayó sobre el cemento y eso le reabrió una quemadura que tenía en el abdomen, causada por una plancha de pelo. “Cuando veo eso, me imagino a mi madre intentando protegerme y a todo el mundo corriendo”, dijo Gabriella.
Es difícil no sentirse olvidada por la gente, opina Bridget. El tiroteo, y especialmente sus sobrevivientes, han desaparecido en gran medida de los titulares excepto en las fechas de los juicios. Desde el desfile hubo otros dos tiroteos de gran repercusión en la zona. Y se pregunta si a la comunidad no le importa que ella y su familia sigan viviendo con las secuelas a diario.
“Voy a decirlo de la forma más clara posible. Estoy muy, pero muy enojada porque mi familia haya tenido que pasar por algo traumático”, se desahogaba Bridget en una reciente publicación en las redes sociales. “En realidad no quiero otra cosa [que]: ‘Tu historia también importa y queremos saber cómo te va’. ¿Lo hemos conseguido? Absolutamente no.”
¿Qué se necesita?
Ayudados en parte por famosos como Swift y Kelce, las donaciones para la familia de López-Galván, la única víctima mortal, y para otras víctimas llegaron en masa inmediatamente después del tiroteo. Swift y Kelce donaron $100,000 cada uno. Con la ayuda de un aporte inicial de $200,000 de los Kansas City Chiefs, la campaña #KCStrong de United Way alcanzó el millón de dólares en las dos primeras semanas y ahora llega a los $1,2 millones.
Se crearon seis fondos GoFundMe verificados. Uno, destinado exclusivamente a la familia López-Galván, ha recaudado más de $406,000. Otros más pequeños fueron creados por un estudiante universitario local y por fans de Swift. Las iglesias también se comprometieron y una coalición local recaudó $183,000, dinero destinado al funeral de López-Galván, a solventar la terapia para cinco víctimas y a pagar facturas médicas del hospital Children’s Mercy Kansas City, según dijo Ray Jarrett, director ejecutivo de Unite KC.
Los líderes de esta iniciativa encontraron modelos en otras ciudades. Blubaugh, de United Way, consultó a funcionarios e instituciones que habían tenido que dar respuesta a las víctimas de sus propios tiroteos masivos en Orlando (Florida), Buffalo (Nueva York) y Newtown (Connecticut).
“La desafortunada realidad es que en todo el país existen comunidades que ya se han enfrentado a tragedias como ésta, explicó Blubaugh. Así que lamentablemente hay un protocolo que, en cierto modo, ya está en marcha”.
A partir de que Blubaugh informó que el dinero de #KCStrong podría empezar a pagarse a finales de marzo, cientos de personas llamaron a la línea 211 de las organizaciones sin fines de lucro. United Way está consultando con los hospitales y las fuerzas del orden para identificar a las víctimas, y ofrecerles los servicios que puedan necesitar.
El abanico de necesidades es asombroso: varias personas siguen recuperándose en su casa, y otras necesitan apoyo emocional y psicológico. Muchas, al principio, ni siquiera fueron contabilizadas. Por ejemplo, un agente de policía que ese día vestía de civil y resultó herido. Según el jefe de policía Stacey Graves, ya se encuentra bien.
Determinar quién es elegible para recibir asistencia fue una de las primeras conversaciones que tuvieron los funcionarios de United Way cuando crearon el fondo. Y decidieron priorizar tres áreas: primero a los heridos y sus familias; segundo a servicios de salud mental y a organizaciones que ya estuvieran ayudando a las víctimas en prevención de la violencia, y en tercer lugar a los socorristas.
En concreto, los fondos se destinarán a cubrir los costos médicos o los salarios perdidos de quienes no hayan podido trabajar desde los tiroteos, explicó Blubaugh. Y agregó que si bien el objetivo es ayudar rápidamente a la gente también se debe utilizar el dinero de una manera juiciosa y estratégica.
“No tenemos una visión clara del panorama al que nos enfrentamos”, dijo Blubaugh. “No sólo no sabemos de cuánto dinero disponemos sino cuál es el panorama de las necesidades. Hacen falta ambas cosas para tomar decisiones”.
Experiencia de la violencia cotidiana en Kansas City
Jason utilizó el único día de licencia que le quedaba para quedarse en casa con Bridget y Gabriella. Como técnico de automatización nocturna, es el principal sostén de la familia. “No puedo faltar al trabajo, explicó. Sucedió. Fue una porquería. Pero es hora de seguir adelante.”
“Es un hombre de verdad”, afirma Bridget.
La primera noche que Jason fue al trabajo, el ruido repentino de los platos al caer sobresaltó a Bridget y Gabriella, que se abrazaron llorando. “Son esos recuerdos los que nos están atormentando”, dijo Bridget, enojada.
En cierto modo, el tiroteo ha unido más a la familia que había pasado por muchas cosas recientemente: Jason sobrevivió a un ataque al corazón y a un cáncer el año pasado; y criar a un adolescente nunca es fácil.
Bridget agradece que la bala se alojara en su mochila y no la alcanzara, y que las chispas le hayan quemado las piernas a Gabriella pero que no le dispararan.
Jason está agradecido por otra razón: no ha sido un atentado terrorista, como temía al principio. En cambio, se trata del tipo de violencia armada a la que estaba acostumbrado porque creció en Kansas City, una ciudad que alcanzó su pico de muertes el año pasado. Aunque Jason nunca le había tocado tan de cerca.
“Esta basura ocurre todos los días, dijo. La única diferencia es que nosotros estábamos ahí para verlo”.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 2 months ago
Health Care Costs, Noticias En Español, Public Health, States, Emergency Medicine, Guns, Investigation, Kansas, Missouri
KFF Health News' 'What the Health?': The ACA Turns 14
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
The Affordable Care Act was signed into law 14 years ago this week, and Health and Human Services Secretary Xavier Becerra joined KFF Health News’ Julie Rovner on this week’s “What the Health?” podcast to discuss its accomplishments so far — and the challenges that remain for the health law.
Meanwhile, Congress appears on its way to, finally, finishing the fiscal 2024 spending bills, including funding for HHS — without many of the reproductive or gender-affirming health care restrictions Republicans had sought.
This week’s panelists are Julie Rovner of KFF Health News, Mary Agnes Carey of KFF Health News, Tami Luhby of CNN, and Alice Miranda Ollstein of Politico.
Panelists
Mary Agnes Carey
KFF Health News
Tami Luhby
CNN
Alice Miranda Ollstein
Politico
Among the takeaways from this week’s episode:
- The Supreme Court will hear oral arguments next week in a case that could decide whether the abortion pill mifepristone will remain easily accessible. The case itself deals with national restrictions rather than an outright ban. But, depending on how the court rules, it could have far-reaching results — for instance, preventing people from getting the pills in the mail and limiting how far into pregnancy the treatment can be used.
- The case is about more than abortion. Drug companies and medical groups are concerned about the precedent it would set for courts to substitute their judgment for that of the FDA regarding drug approvals.
- Abortion-related ballot questions are in play in several states. The total number ultimately depends on the success of citizen-led efforts to collect signatures to gain a spot. Such efforts face opposition from anti-abortion groups and elected officials who don’t want the questions to reach the ballot box. Their fear, based on precedents, is that abortion protections tend to pass.
- The Biden administration issued an executive order this week to improve research on women’s health across the federal government. It has multiple components, including provisions intended to increase research on illnesses and diseases associated with postmenopausal women. It also aims to increase the number of women participating in clinical trials.
- This Week in Medical Misinformation: The Supreme Court heard oral arguments in the case Murthy v. Missouri. At issue is whether Biden administration officials overstepped their authority when asking companies like Meta, Google, and X to remove or downgrade content flagged as covid-19 misinformation.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: The Washington Post’s “Arizona Lawmaker Tells Her Abortion Story to Show ‘Reality’ of Restrictions,” by Praveena Somasundaram. (Full speech here.)
Alice Miranda Ollstein: CNN’s “Why Your Doctor’s Office Is Spamming You With Appointment Reminders,” by Nathaniel Meyersohn.
Tami Luhby: KFF Health News’ “Georgia’s Medicaid Work Requirement Costing Taxpayers Millions Despite Low Enrollment,” by Andy Miller and Renuka Rayasam.
Mary Agnes Carey: The New York Times’ “When Medicaid Comes After the Family Home,” by Paula Span, and The AP’s “State Medicaid Offices Target Dead People’s Homes to Recoup Their Health Care Costs,” by Amanda Seitz.
Also mentioned on this week’s podcast:
- NPR’s “Standard Pregnancy Care Is Now Dangerously Disrupted in Louisiana, Report Reveals,” by Rosemary Westwood.
- The Washington Post’s “As the Cost of Storing Frozen Eggs Rises, Some Families Opt to Destroy Them,” by Amber Ferguson.
Click to open the transcript
Transcript: The ACA Turns 14
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello, and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News, and I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, March 21, at 10 a.m. As always, news happens fast and things might have changed by the time you hear this. So here we go.
We are joined today via video conference by Alice Miranda Ollstein of Politico.
Alice Miranda Ollstein: Hello.
Rovner: Tami Luhby of CNN.
Tami Luhby: Hello.
Rovner: And my KFF Health News colleague Mary Agnes Carey.
Mary Agnes Carey: It’s great to be here.
Rovner: Later in this episode to mark the 14th anniversary of the Affordable Care Act, we’ll have my interview with Health and Human Services Secretary Xavier Becerra, but first, this week’s news. So it appears our long national nightmare following the progress of the fiscal 2024 spending bill for the Department of Health and Human Services is nearly over, nearly halfway through the fiscal year. The White House, House, and Senate have, as far as we can tell, reached a compromise on the last tranche of spending bills, which is a good thing because the latest temporary spending bill runs out at midnight Friday. Funding for the Department of Health and Human Services, from what I’ve seen so far, is basically flat, which is a win for the Democrats because the Republicans had fought for a cut of something in the neighborhood of 22%.
Now, assuming this all happens, the House is scheduled to vote, as we speak now, on Friday at 11 a.m., leaving the Senate not very much time to avert a possible partial shutdown. Democrats seem also to have avoided adding all manner of new restrictions on reproductive and gender-affirming health care to the HHS part of the bill. It’s the last big train leaving the station likely until after the election. So Alice, we’ll get to the add-ons in a minute, but have you seen anything in the HHS funding worthy of note or did they manage to fend off everything that would’ve been significantly newsworthy?
Ollstein: Like you said, it is basically flat. It’s a small increase, less than 1% overall for HHS, and then a lot of individual programs are just completely flat, which advocacy groups argue is really a cut when you factor in inflation. The cost of providing services and buying medications and running programs and whatnot goes up. So flat funding is a cut in practice. I’m hearing that particularly from the Title X family planning folks that have had flat funding for a decade now even as demand for services and costs have gone up.
So I think that in the current environment, Democrats are ready to vote for this. They don’t want to see a shutdown. And in the House, the bill passage will depend on those Democratic votes because they are likely to lose a lot of Republicans. Republicans are mad that there weren’t deeper cuts to spending and, as you alluded to, they’re mad that they didn’t get these policy rider wins they were banking on.
Rovner: As I’ve mentioned, since this is a must-pass bill, there are always the efforts to add non-spending things to it. And on health care, apparently, the effort to add the PBM, pharmacy benefit regulation bill we’ve talked about so much failed, but lawmakers did finally get a one-year deal to extend PEPFAR, the international AIDS/HIV program. Alice, you’ve been dutifully following this since it expired last year. Remind us why it got held up and what they finally get.
Ollstein: What happened in the end is it is a one-year reauthorization that’s a so-called clean reauthorization, meaning they are not adding new anti-abortion restrictions and provisions that the Republicans wanted. So what we reported this week is, like any compromise, no one’s happy. So Republicans are upset that they didn’t get the anti-abortion restrictions they wanted, and I’ll explain more on that in a second, and Democrats are upset that this is just a one-year reauthorization. It’s the first reauthorization that’s this sort of short-term stopgap length. In the program’s decades of history, it’s always been a full five-year reauthorization up until now. But the fight over abortion and accusations that program funds were flowing to abortion providers really split Congress on this.
Even though you had mainstream leadership Republicans who were saying, “Look, we just want to reauthorize this as-is,” you had a small but very vocal contingent of hard-line anti-abortion lawmakers backed by some really influential groups like the Heritage Foundation and SBA [Susan B. Anthony Pro-Life America] who were saying, “No, we have to insist on a shorter-term reauthorization,” so that they hope Trump will be in office next year and can impose these exact same anti-abortion restrictions through executive action. So they’re basically trying to punt control of the program into what they hope is a more favorable environment, where either they’ll have the votes in Congress to make these changes and restrictions to the program or they can do it through the White House.
Rovner: So basically, the fight over PEPFAR, not over. So as I already mentioned, Saturday is the 14th anniversary of the Affordable Care Act, which you’ll hear more about in my interview with HHS Secretary Becerra, but I wanted to pose to you guys one of the questions that I posed to him. As Nancy Pelosi famously predicted, at least according to public opinion polls, the more people learned about the health law, indeed, the more they are liking it. But it still lacks the popularity and branding of big government health programs, like Medicare and Medicaid, and I think lots of people still don’t know that lots of the provisions that they like, things like letting your adult children stay on your health plan until they’re 26 or banning preexisting condition exclusions, those were things that came from the Affordable Care Act. Any theories as to why it is still so polarizing? Republicans didn’t love Medicare and Medicaid at the beginning either, so I don’t think it’s just that Republicans still talk about it.
Luhby: Part of it I think is because there are so many provisions and they’re not labeled the Affordable Care Act like Medicare is. Actually to some extent, Medicaid may not be as well known in some states because states have different Medicaid programs and different names and so do the ACA exchanges. So that’s part of it, but also, things like why do you get a free mammogram and why you get to go for a routine checkup every year; that’s not labeled as an Affordable Care Act provision, that’s just the preventive services. So I think that it would be difficult now after 14 years to bring all of that into the everyday branding by doctors and health providers. But that’s certainly what the administration and advocates are trying to do by sending out a lot of messages that list all of the benefits of the ACA.
Rovner: I will say this is the biggest full-court press I’ve seen an administration do on the ACA in quite a while. Obviously, it’s a presidential election year and it’s something that the Biden administration is proud of, but at least I would think that maybe just all the publicity might be part of their strategy. Mac, you wanted to say something.
Carey: No, absolutely. It’s going to be part of the Biden reelection campaign. They’re going to be pushing it, talking a lot about it. We have to remember we’ve had this ringside seat to all the Republican opposition to the Affordable Care Act. All the conversation about we’re going to repeal it and put something better in, former President Trump is still sending that message out to the electorate. I don’t know how much confusion, if any confusion, it creates, but to Tami’s point, you’ve got millions of people that have gotten coverage under the Affordable Care Act but millions more have benefited by all these provisions we’re talking about: the preventive care provisions, leaving adult kids up to 26 on your health insurance plan, that kind of thing.
Also, give it time. Fourteen years is a long time, but it’s not the time of Medicare, which was created in 1965, and Medicaid. So I think over time, the Affordable Care Act is part of the fabric and it will continue to be. But absolutely, for sure, President Biden is going to run on this, like you said, Julie, full-court press, talk extensively about it in the reelection campaign.
Ollstein: It makes sense that they’re leaning really hard on Obamacare as a message because, even if everyone isn’t familiar with it, a lot more people are familiar with it and like it than, polling shows, on the Biden administration’s other big health care accomplishment, which is drug price negotiation, which polling shows that most people, and even most seniors, who are the ones who are set to benefit the most, aren’t aware that it exists. And that makes sense because they’re not feeling the impact of the lower prices yet because this whole thing just started and it won’t be until 2026 that they’ll really actually experience cheaper medications. But people are already feeling the direct impact of Obamacare on their lives, and so it does make sense that they’re going to lean really hard on this.
Rovner: Of course, we went through the same thing with Obamacare, which also didn’t take full effect until, really, this is really the 10th anniversary of the full effect of the Affordable Care Act because it didn’t take effect until 2014. Tami, you wanted to add something.
Luhby: No, I was going to say it’s also the seventh anniversary of the Trump administration and congressional Republicans trying to tear apart the Affordable Care Act and repeal and replace it, which is the messaging that you’re seeing now is very similar to what you saw in 2017. It’s just surprising to me that with very intensive messaging on both sides at that time about what the Republicans saying what the problems are and the Democrats saying what all of the benefits are, — including the protections for people with preexisting conditions and the other things we’ve mentioned — that more people don’t associate those provisions with the ACA now. But the Biden administration is trying to revive all of that and remind people, as they did in 2018 in the successful midterm elections for the Democrats, that the ACA does provide a lot of the benefits that they are taking advantage of and appreciate.
Rovner: I think, in some ways, the 2017 fight was one of the best things that ever happened to the ACA in terms of helping people understand what actually was in it, because the Democrats managed to frighten people about things that they liked being taken away. Here we go again. All right, let us turn to abortion. There’s a new report out from the Guttmacher Institute that finds a dramatic jump in the use of medication abortion in 2023, the first full year since the Supreme Court reversed the nationwide right to abortion in the Dobbs [v. Jackson Women’s Health Organization] case, more than 60% of abortions use medication rather than a procedure last year. This news comes as the Supreme Court next week prepares to hear oral arguments in a case that could dramatically restrict availability of the abortion pill mifepristone. Alice, remind us what’s at stake in this case. It’s no longer whether they’re going to just outright cancel the approval.
Ollstein: That’s right. So the Supreme Court is taking up the narrowed version of this from the 5th Circuit. So what’s at stake are national restrictions on abortion pills, but not a national outright ban like you mentioned. But those restrictions could be really sweeping and really impactful. It would prevent people from getting the pills through the mail like they currently do. It would prevent people from potentially getting them in any other way other than directly from a doctor. So this would apply to red states and blue states alike. It would override abortion rights provisions in blue states that have done a lot to increase access to the pills. And it would also restrict their use back to the first seven weeks of pregnancy instead of 10, which is a big deal because people don’t often find out they’re pregnant until getting close to that line or beyond.
So this is a really big deal, and I think you can really see, especially from the flurry of amicus briefs have been filed, that anxiety about this case in the medical community and the pharmaceutical community, the scientific community, it goes way beyond the impact just on abortion. People are really worried about setting a precedent where the FDA’s scientific judgment is second-guessed by courts, and they worry that a win for the anti-abortion groups in this case would open the door to people challenging all kinds of other medications that they have an issue with: contraception, covid vaccines, HIV drugs, the list goes on and on, gender-affirming care medications, all sorts of things. So there are the bucket of potential impacts on abortion specifically, which are certainly significant, and then there’s the bigger slippery slope fears as well.
Rovner: Also, this is obviously still way political. More than just the abortion pill. It’s been a while since we’ve talked about state ballot measures. We, I think, feel like we spent all of last year talking about abortion state ballot measures. Alice, catch us up real quick on where we are. How many states have them? And what is this campaign against, by the anti-abortion people, to try to prevent them from getting on the ballot?
Ollstein: Check me if I’m wrong, but I don’t believe we know for sure about, especially the states that have citizen-led ballot initiatives where people are gathering signatures. So Florida had one of the earliest deadlines and they did meet their signature threshold. But they are now waiting on the state Supreme Court to say whether or not they have a green light to go forward this fall. A lot of other states are still collecting signatures. I think the only states we know for sure are the ones where the state legislature is the one that is ordering it to be put on the ballot, not regular citizens gathering signatures.
We still don’t know, but things are moving forward. I was just in Arizona reporting on their efforts. Things are moving forward there. Things are moving forward in Montana. They just got a court ruling in their favor to put something on the ballot. And things are moving forward in Missouri, a lot of places. So this could be really huge. Of course, like you mentioned, anti-abortion groups and anti-abortion elected officials are doing a lot of different things to try to prevent this from going on the ballot.
It’s interesting, you heard arguments over the last couple years against this being more along the lines of, “Oh, this is allowing these out-of-state big-money groups to swoop in and mislead and tell us what to do,” and those were the anti-abortion arguments against allowing people to vote on this directly. Now, you’re hearing, I’m hearing, more arguments along the lines of, “This shouldn’t be something subject to a popular vote at all. We shouldn’t put this up for a vote at all.” They consider this a human rights issue, and so I think that’s a really interesting evolution as well, particularly when the fall of Roe [v. Wade] was celebrated for returning the question of abortion access to the people, but maybe not these people specifically.
Rovner: I’ve been interested in seeing some of these anti-abortion groups trying to launch campaigns to get people not to put signatures on petitions. That’s moving it back a step I don’t think I’d ever seen. I don’t think I’ve ever seen a campaign to say, “Don’t sign the petition that would put this on the ballot to let people vote on it.” But that’s what we’re seeing, right?
Ollstein: Well, that’s what I went to Arizona to see firsthand is how that’s working, and it’s fascinating. They really worry that if it gets on the ballot, it’ll pass. It has in every state so far, so it’s reasonable for them to assume that. So they’re trying to prevent it from getting on the ballot. The way they’re doing that is they’re tracking the locations of signature gatherers and trying to go where they are and trying to intervene and hold up signs. I saw this firsthand. I saw it at a street fair. People were gathering signatures and several anti-abortion demonstrators were standing right in front of them with big signs and trying to argue with people and deter them from signing. It was not working, from what I observed. And from the overall signature count statewide, it was not working in Arizona. But it’s fascinating that they’re trying this.
Carey: I was going to say just our reporting from our KFF Health News colleagues found that 13 states are weighing abortion-related ballot measures, most of which would protect abortion rights. To your point, the scope is pretty extensive. And for all the reasons Alice just discussed, it’s quite the issue.
Rovner: Yeah, and we will obviously talk more about this as the election gets closer. I know we talk about Texas a lot on this podcast, but this week, I want to highlight a study from next door in Louisiana, also a very strong anti-abortion state. A new report from three groups, all of which support abortion rights, charges that, as in Texas, women with pregnancy complications are being forced to wait for care until their conditions become critical. And in some cases, women with nonviable pregnancies are being forced to have C-section surgery because their doctors don’t dare use medication or other less-risky procedures in case they could be accused of performing an abortion.
At some point, you have to think that somebody is going to have a malpractice case. Having a C-section because your doctor is afraid to terminate a nonviable pregnancy seems like pretty dangerous and rather aggressive way to go. This is the first I’ve ever heard of this. Alice, have you heard anything about this?
Ollstein: Not the C-section statistics specifically, but definitely the delays in care and some of the other impacts described in that report have absolutely been reported in other states and in legal challenges that have come up in Texas, in Oklahoma, in Tennessee, in Idaho by people who were denied abortions and experienced medical harms because of it. So I think that fits into the broader pattern. And it’s just more evidence about how this is having a chilling effect on doctors. And the exact letter of the law may be one thing, and you have elected officials pointing to exemptions and provisions in the law, but the chilling effect, the fear and the confusion in the medical community, is something in addition to that.
Rovner: As we put it out before, doctors have legitimate fears even if they don’t want to get dragged into court and have to hire lawyers and take time off — even if they’re innocent, even if they have what they consider to be pretty strong evidence that whatever it was that they did was legitimate under the law in terms of taking care of pregnant women. A lot of them, they don’t want to come under scrutiny, let’s put it that way, and it is hard to blame them about that.
Meanwhile, the backlash over the Alabama Supreme Court decision that fertilized embryos for IVF have legal rights is continuing as blue states that made themselves safe spaces for those seeking abortion are now trying to welcome those seeking IVF. Anybody think this is going to be as big a voting issue as abortion this fall? It’s certainly looking like those who support IVF, including some Republicans, are trying to push it.
Carey: I would think yes, it absolutely will be because it has been brought into the abortion debate. The actual Alabama issue is about an Alabama law and whether or not this particular, the litigants who sued were … it was germane and covered by the law, but it’s been brought into the abortion issue. The whole IVF thing is so compelling, about storage of the embryos and what people have to pay and all the restrictions around it and some of the choices they’re making. I guess that you could say more people have been touched by IVF perhaps than the actual abortion issue. So now, it’s very personal to them and it’s been elevated, and Republicans have tried to get around it by saying they support it, but then there’s arguments that whether or not that’s a toothless protection of IVF. It came out of nowhere I think for a lot of politicians and they’ve been scrambling and trying to figure it out. But to your point, Julie, I do wonder if it will be elevated in the election. And it was something they didn’t think they’d have to contend with, rather, and now they do.
Rovner: Obviously, it’s an issue that splits the anti-abortion community because now we’ve had all these very strong pro-lifers like Mike Pence saying, “I created my family using IVF.” Nikki Haley. There are a lot of very strong anti-abortion Republicans who have used IVF. So you’ve got some on the far … saying, “No, no, no, you can’t create embryos and then destroy them,” and then you’ve got those who are saying, “But we need to make sure that IVF is still available to people. If we’re going to call ourselves pro-life, we should be in favor of people getting pregnant and having babies, which is what IVF is for.” Alice, I see you nodding your head.
Ollstein: Yeah. So we’re having sort of a frustrating discourse around this right now because Democrats are saying, “Republicans want to ban IVF.” And Republicans are saying, “No, we don’t. We support IVF. We love IVF. IVF is awesome.” And neither is totally accurate. It’s just missing a lot of nuance. Republicans who say they support IVF also support a lot of different kinds of restrictions on the way it’s currently practiced. So they might correctly argue that they don’t want to ban it entirely, but they do want it practiced in a different way than it is now, such as the production of many embryos, some of which are discarded. So I think people are just not being asked the right questions right now. I think you got to get beyond, “Do you support IVF?” That gives people a way to dodge. I think you really have to drill into, “OK. How specifically do you want this regulated and what would that mean for people?”
Carey: Right, and the whole debate with some of the abortion rights opponents, some of them want the federal government to regulate it. Mike Johnson, speaker of the House, has come out and said, “No, no, that can be done at the state level.” So they’ve got this whole split internally in the party that is, again, a fight they didn’t anticipate.
Rovner: Well, Mac, something that you alluded to that I was struck by was a piece in The Washington Post this week about couples facing increasing costs to store their IVF embryos, often hundreds of dollars a year, which is forcing them to choose between letting the embryos go or losing a chance to possibly have another child. It’s obviously a big issue. I’m wondering what the anti-IVF forces think about that. As we’ve seen in Alabama, it’s not like you can just pick your embryos up in a cooler and move them someplace else. Moving them is actually a very big deal.
I don’t wish to minimize this, but I remember you have storage units for things, not obviously for embryos. One of the ways that they make money is that they just keep raising the cost because they think you won’t bother to move your things, so that you’ll just keep paying the increased cost. It feels like that’s a little bit of what’s happening here with these stored embryos, and at some point, it just gets prohibitively expensive for people to keep them in storage. I didn’t realize how expensive it was.
Carey: They’re all over the place. In preparing for this discussion, I’ve read things about people are paying $600 a year, other people are paying $1,200 a year. There’s big jumps from year to year. It can be an extremely expensive proposition. Oh, my goodness.
Rovner: IVF itself, I think as we’ve mentioned, is also extremely expensive and time-consuming, and emotionally expensive. It is not something that people enter into lightly. So I think we will definitely see more as we go. There’s also women’s health news this week that doesn’t have to do with reproduction. That’s new. Earlier this week, President Biden issued an executive order attempting to ensure that women are better represented in medical research. Tami, what does this order do and why was it needed?
Luhby: Well, it’s another attempt by the Biden administration, as we’ve discussed, to focus on reproductive health and reproductive rights. During the State of the Union address earlier this month, Biden asked Congress to invest $12 billion in new funding for women’s health research. And there are actually multiple components to the executive order, but the big ones are that it calls for supporting research into health and diseases that are more likely to occur midlife for women after menopause, such as rheumatoid arthritis, heart attacks, osteoporosis, and as well as ways to improve the management of menopause-related issues.
We are definitely seeing that menopause care is of increasing focus in a multitude of areas including employer health insurance, but the executive order also aims to increase the number of women participating in clinical trials since they’re poorly represented now. We know that certain medications and certain treatments have different effects on women than men, but we don’t really know that that well because they’re not as represented in these clinical trials. Then it also directs agencies to develop and strengthen research and data standards on women’s health across all of the relevant research and funding opportunities in the government.
Rovner: I’ll say that this is an issue I have very strong feelings about because I covered the debate in 1992 about including women in medical research. At the time, doctors didn’t want to have women in clinical trials because they were worried about hormones, and they might get pregnant, and we wouldn’t really know what that meant for whatever it was that we were testing. Someone suggested that “If you’re going to use these treatments and drugs on women, maybe you should test them on women too.” Then I won an award in 2015 for a story about how they still weren’t doing it, even though it was required by laws.
Carey: And here we are, 2024.
Rovner: Yeah, here we are. It just continues, but at least they’re trying. All right, finally, this week in medical misinformation, we travel to the Supreme Court, where the justices heard oral arguments in a case brought by two Republican state attorneys general charging that the Biden administration, quote, “coerced” social media platforms, Google, Meta, and X, into downgrading or taking down what public health officials deemed covid disinformation. I didn’t listen to the arguments, but all the coverage I saw suggested that the justices were not buying what the attorneys general were selling.
Yet another public-health-adjacent case to watch for a decision later this spring, but I think this is really going to be an important one in terms of what public officials can and cannot do using their authority as public health officials. We’re obviously in a bit of a public health trust crisis, so we will see how that goes.
All right, that is the news for this week. Now, we will play my interview with HHS Secretary Xavier Becerra, then we will be back with our extra credits.
I am so pleased to welcome back to the podcast Health and Human Services Secretary Xavier Becerra. I’ve asked him to join us to talk about the Affordable Care Act, which was signed into law 14 years ago this weekend. Mr. Secretary, thanks so much for coming back.
Xavier Becerra: Julie, great to be with you on a great week.
Rovner: So the Affordable Care Act has come a long way, not just in the 14 years since President Obama signed it into law, but in the 10 years since the healthcare.gov website so spectacularly failed to launch, but this year’s enrollment setting a record, right?
Becerra: That’s right, and you should have said, “You’ve come a long way, baby.”
Rovner: So what do we know about this year’s enrollment numbers?
Becerra: Another record breaker. Julie, every year that President Biden has been in office, we have broken records. Today, more Americans have health insurance than ever in the history of the country. More than 300 million people can now go to a doctor, leave their child in a hospital and know they won’t go bankrupt because they have their own health insurance. That’s the kind of peace of mind you can’t buy. Some 21.5 million Americans today look to the marketplace on the Affordable Care Act to get their coverage. By the way, the Affordable Care Act overall, some 45 million Americans today count on the ACA for their health care insurance, whether it’s through the marketplace, through Medicaid, or some of these basic plans that were also permitted under the ACA.
Rovner: Obviously, one of the reasons for such a big uptake is the expanded subsidies that were extended by the Inflation Reduction Act in 2022, but those expire at the end of next year, the end of 2025. What do you think would happen to enrollment if they’re not renewed?
Becerra: Well, and that’s the big question. The fact that the president made health care affordable was the big news. Because having the Affordable Care Act was great, but if people still felt it was unaffordable, they wouldn’t sign on. They now know that this is the best deal in town and people are signing up. When you can get health insurance coverage for $10 or less a month in your premiums, that’s a great deal. You can’t even go see a movie at a theater today for under $10. Now, you can get health care coverage for a full month, Julie. Again, as I always tell people, that doesn’t even include the popcorn and the refreshment at the movie theater, and so it’s a big deal. But without the subsidies, some people would still say, “Ah, it’s still too expensive.” So that’s why the president in his budget calls for extending those subsidies permanently.
Rovner: So there are still 10 states that haven’t taken up the federal government’s offer to pay 90% of the costs to expand Medicaid to all low-income adults in their states. I know Mississippi is considering a bill right now. Are there other states that you expect could join them sometime in the near future? Or are any of those 10 states likely to join the other 40?
Becerra: We’re hoping that the other 10 states join the 40 that have come on board where millions of Americans today have coverage. They are forsaking quite a bit of money. I was in North Carolina recently where Gov. [Roy] Cooper successfully navigated the passage of expansion for Medicaid. Not only was he able to help some 600,000-plus North Carolinians get health coverage, but he also got a check for $1.6 billion as a bonus. Not bad.
Rovner: No, not bad at all. So many years into this law, I feel like people now understand a lot of what it did: let adult children stay on their parents’ health plans until the age of 26; banning most preexisting condition exclusions in health coverage. Yet most people still don’t know that those provisions that they support were actually created by Obamacare or even that Obamacare and the Affordable Care Act are the same thing. Medicare has had such great branding success over the years. Why hasn’t the ACA?
Becerra: Actually, Julie, I think that’s changing. Today, about two-thirds of Americans tell you that they support the marketplaces in the Affordable Care Act. I think we’re actually now beginning an era where it’s no longer the big three, where you had Social Security, Medicare, and Medicaid and everyone protects those. Today, I think it’s the big four, the cleanup hitter being marketplace. Today, you would find tens of millions of Americans who would say, “Keep your dirty, stinking hands off of my marketplace.”
Rovner: Well, we will see as that goes forward. Obviously, President Biden was heavily involved in the development of the Affordable Care Act as vice president, as were you as a member of the House Ways and Means Committee at the time. What do you hope is this administration’s biggest legacy to leave to the health law?
Becerra: Julie, I think it’s making it affordable. The president made a commitment when he was first running to be president. He said on health care he was going to make it more affordable for more Americans with better benefits, and that’s what he’s done. The ACA is perfect proof. And Americans are signing up and signaling they agree by the millions. To go from 12 million people on the Affordable Care Act marketplace to 21.5 million in three years, that’s big news.
Rovner: So if I may, one question on another topic. Next week, the Supreme Court’s oral arguments occur in the case it could substantially restrict the availability of the abortion pill mifepristone. Obviously, this is something that’s being handled by the Justice Department, but what is it about this case that worries you most as HHS secretary, about the potential impact if the court rolls back FDA approval to the 2016 regulations?
Becerra: Well, Julie, as you well know from your years of covering health care, today there are Americans who have less protection, fewer rights, than many of us growing up. My daughters, my three daughters today, have fewer protections and access to health care than my wife had when she was their age. That’s not the America most of us know. To see another case where, now, medication abortion, which is used by millions of Americans — in fact, it’s the most common form of care that is received by a woman who needs to have abortion services — that is now at stake. But we believe that if the Supreme Court believes in science and it believes in the facts, because mifepristone has been used safely and effectively publicly for more than 20 years, that we’re going to be fine.
The thing that worries me as much, not just in the reduction of access to care for women in America, is the fact that mifepristone went through a process at the FDA similar to scores and scores of other medications that Americans rely on, that have nothing to do with abortion. And if the process is shut down by the Supreme Court for mifepristone, then it’s probably now at risk for all those other drugs, and therefore those other drugs that Americans rely on for diabetes, for cancer, who knows what, might also be challenged as not having gone through the right process.
Rovner: I know the drug industry is very, very worried about this case and watching it closely, and so will we. Mr. Secretary, thank you so much for joining us.
Becerra: Always good to be with you, Julie.
Rovner: OK, we are back. It’s time for our extra-credit segment. That’s when we each recommend a story we read this week we think you should read, too. As always, don’t worry if you miss it. We will post the links on the podcast page at kffhealthnews.org and in our show notes on your phone or other mobile device. Tami, why don’t you go first this week?
Luhby: OK, my extra credit this week is an article about Georgia’s unique Medicaid program from KFF Health News’ Andy Miller and Renuka Rayasam. It’s titled “Georgia’s Medicaid Work Requirement Costing Taxpayers Millions Despite Low Enrollment.” And I’m really glad they did this story. I and many others wrote about Georgia launching this program initially but haven’t done follow-up. So I was very happy to see this story.
As many of our listeners probably know, the Trump administration allowed multiple states to impose work requirements in Medicaid for the first time in the program’s history in 2018. But the efforts were eventually stopped by the courts in all states except Georgia. Georgia was allowed to proceed with adding its work requirement to Medicaid because it was actually going to expand coverage to allowing adults with incomes up to 100% of the poverty line to qualify. So the Georgia Pathways to Coverage initiative began last June.
Andy and Renuka took a look at how it’s faring, and the answer is actually not so well. Only about 3,500 people have signed up, far short of the 25,000 that the state projected for the first year. What’s more, the program has cost taxpayers at least $26 million so far, with more than 90% of that going towards administrative and consulting costs rather than actual medical care for low-income people.
By contrast, expanding Medicaid under the Affordable Care Act to people with 138% of the poverty line would make at least 359,000 uninsured Georgia residents newly eligible for coverage and reduce state spending by $710 million over two years. That’s what the advocates are pushing. So we’ll see what happens in coming months. One thing that’s also noted in the story is that about 45% of Pathways applications were still waiting to be processed.
Rovner: I will point out that we did talk a couple of weeks ago about the low enrollment in the Georgia program. What we had not seen was how much it’s actually costing the states per enrollee. So it is really good story. Alice, why don’t you go next?
Ollstein: Yeah, so I have some very relatable news from CNN. It’s called “Why Your Doctor’s Office Is Spamming You With Appointment Reminders.” It’s about why we all get so many obnoxious repeat reminders for every medical appointment. It both explains why medical practices that operate on such a tiny profit margin are so anxious about no-shows and last-minute cancellations, and so that’s part of it. But also part of it is that there are all these different systems that don’t communicate with one another. So the prescription drug system and the electronic medical records system and the doctor’s office’s own system are all operating in parallel and not coordinating with one another, and that’s why you get all these annoying multiple reminders. The medical community is becoming aware that it’s backfiring because the more you get, the more you start tuning them out and you don’t pay attention to which ones might be important. So they are working on it. So a somewhat hopeful piece of news.
Rovner: Raise your hand if you have multiple patient portals that you have to deal with for your multiple …
Ollstein: Oh, my God, yes.
Rovner: I will note that everybody’s hands go up. Mac?
Carey: I have not one but two stories on a very important issue: Medicaid estate recovery. The first is from Paula Span at The New York Times. The headline says it all, “When Medicaid Comes After the Family Home.” And the second story is an AP piece by Amanda Seitz, and that’s titled “State Medicaid Offices Target Dead People’s Homes to Recoup Their Health Care Costs.” Now, these stories are both about a program that’s been around since 1993. That’s when Congress mandated Medicaid beneficiaries over the age of 55 that have used long-term care services, and I’m talking about nursing homes or home care, that states must try to recover those expenses from the beneficiaries’ estates after their deaths.
As you can imagine, this might be a problem for the beneficiaries. They might have to sell a family home, try to find other ways to pay a big bill from Medicaid. Rep. Jan Schakowsky, she’s a Democrat of Illinois, has reintroduced her bill. It’s called the Stop Unfair Medicaid Recoveries Act. She’s trying to end the practice. She thinks it’s cruel and harmful, and her argument is, in fact, the federal and state governments spend way more than what they collect, and these collections often go after low-income families that can’t afford the bill anyway.
So even though it’s been around, it’s important to read up on this. A critical point in the stories was do states properly warn people that assets were going to be recovered if they enroll a loved one in Medicaid for long-term care and so on. So great reading, people should bone up on that.
Rovner: This is one of those issues that just keeps resurfacing and doesn’t ever seem to get dealt with. Well, my story this week is from The Washington Post, although I will say it was covered widely in dozens of outlets. It’s called “Arizona Lawmaker Tells Her Abortion Story to Show ‘Reality’ of Restrictions.” On Monday, Arizona State Sen. Eva Birch stood up on the Senate floor and gave a speech unlike anything I have ever seen. She’s a former nurse at a women’s health clinic. She’s also had fertility issues of her own for at least a decade, having both had a miscarriage and an abortion for a nonviable pregnancy in between successfully delivering her two sons.
Now, she’s pregnant again, but with another nonviable pregnancy, which she plans to terminate. Her point in telling her story in public on the Senate floor, she said, was to underscore how cruel — her words — Arizona’s abortion restrictions are. She’s been subject to a waiting period, required to undergo an invasive transvaginal ultrasound to obtain information she and her doctor already knew about her pregnancy, and to listen to a lecture on abortion, quote, “alternatives,” like adoption, which clearly don’t apply in her case.
While she gave the speech on the floor, several of her Democratic colleagues stood in the camera shot behind her, while many of the Republicans reportedly walked out of the chamber. I will link to the story, but I will also link to the entire speech for those who want to hear it.
OK, that is our show. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left us a review; that helps other people find us, too. Special thanks as always to our technical guru, Francis Ying, and our fill-in editor for today, Stephanie Stapleton. As always, you can email us your comments or questions. We’re at whatthehealth@kff.org, or you can still find me at X, @jrovner, or @julierovner at Bluesky and @julie.rovner at Threads. Mary Agnes, where are you hanging out these days?
Carey: I’m hanging out on X, @MaryAgnesCarey.
Rovner: Alice?
Ollstein: @AliceOllstein on X, and @alicemiranda on Bluesky.
Rovner: Tami?
Luhby: The best place to find me is at cnn.com.
Rovner: There you go. We will be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Stephanie Stapleton
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 2 months ago
Health Care Costs, Health Industry, Insurance, Medicaid, Medicare, Multimedia, Pharmaceuticals, Public Health, States, Abortion, Biden Administration, Drug Costs, KFF Health News' 'What The Health?', Misinformation, Podcasts, Pregnancy, Prescription Drugs, Women's Health
Cuando tu cobertura de salud dentro de la red… simplemente se esfuma
Sarah Feldman, de 35 años, recibió las primeras cartas amenazantes del Centro Médico Mount Sinai en noviembre pasado. El sistema hospitalario de Nueva York le advirtió que tenía problemas para negociar un acuerdo de precios con UnitedHealthcare, que incluye los planes de salud de Oxford, la aseguradora de Feldman.
“Estamos trabajando de buena fe con Oxford para alcanzar un nuevo acuerdo justo”, decía la carta, continuando con la frase tranquilizadora: “Sus médicos seguirán siendo parte de la red y debería mantener sus citas con sus proveedores”.
En los meses siguientes, llegaron una avalancha de comunicaciones sobre la disputa tanto del hospital como de la aseguradora. Pasaban de “tienes que preocuparte” a “no tienes que preocuparte'”, contó Feldman.
A fines de febrero, finalmente cayó la bomba: desde el 1 de marzo, el Mount Sinai ya no estaría en la red de la aseguradora de Feldman.
“De repente tuve que cambiar todos mis médicos, gran estrés”, dijo Feldman. Eso incluía no solo a un querido médico de atención primaria, sino también a un ginecólogo, un ortopedista y un fisioterapeuta.
Uno de los aspectos más injustos del seguro médico, en un sistema que a menudo parece diseñado para la frustración, es este: los pacientes solo pueden cambiar de seguro durante los períodos de inscripción abierta al final del año o cuando experimentan “eventos de vida” que califican para una inscripción especial, como un divorcio o un cambio de trabajo.
Pero los contratos de las aseguradoras con médicos, hospitales y farmacéuticas (o sus intermediarios, los llamados administradores de beneficios farmacéuticos) pueden cambiar abruptamente de la noche a la mañana.
Esto es particularmente irritante para los pacientes porque, ya sea que tengan cobertura a través de un empleador o compren un seguro en el mercado, generalmente eligen un plan en función de si cubre a sus médicos y hospitales preferidos, o a un medicamento costoso que necesitan.
Resulta que esa cobertura particular podría desaparecer en cualquier momento durante el término de la póliza.
Los consumidores están en riesgo, según un informe reciente de la Robert Wood Johnson Foundation, en la creciente guerra de precios entre grandes sistemas hospitalarios y mega aseguradoras en un mercado despiadado.
Estas disputas de contratos están aumentando rápidamente, el sitio web Becker’s Hospital Review cita 21 enfrentamientos entre aseguradoras y proveedores en el tercer trimestre de 2023, un aumento del 91% comparado con el mismo período el año anterior.
Por ejemplo, en septiembre pasado, los médicos de Baptist Health en Kentucky cortaron abruptamente la relación con los pacientes inscritos en los planes de Medicare Advantage de Humana, y los médicos de Vanderbilt Health en Tennessee rompieron los contratos lo hicieron con varios planes de Humana, en abril.
En ambos casos los pacientes desesperados tuvieron que buscar frenéticamente nuevos médicos dentro de la red en otros sistemas hospitalarios.
Y expertos predicen más cancelaciones de contratos en un mercado cruel. (las cancelaciones que ocurren dentro del período de inscripción, generalmente entre noviembre y enero por lo menos permite que los pacientes abandonados busquen un nuevo plan que cubra sus médicos y medicamentos).
“La respuesta humana correcta es que esto es horrible”, dijo Allison Hoffman, profesora de derecho de la Universidad de Pennsylvania, incluso si la práctica, por ahora, es “probablemente legal”.
Hoffman dijo que encontró una cláusula “enterrada” en la página 32 de su propio plan médico, de 60 páginas, que sugería que los contratos entre proveedores y aseguradoras pueden cambiar en cualquier momento.
Los reguladores estatales y federales tienen la autoridad para regular las redes de aseguradoras y podrían poner fin a la práctica, dijo Hoffman. Pero hasta ahora “no ha habido regulación federal sobre la continuidad de la cobertura”, especialmente sobre cómo definirla. Sospecha que el aparente aumento en disputas de contratos entre aseguradoras y proveedores se deriva de las regulaciones sobre la transparencia de los precios hospitalarios, que entraron en vigencia en 2022 y han permitido a los hospitales comparar tasas de reembolso entre sí.
De hecho, el Mount Sinai dijo que exigía un mejor reembolso de UnitedHealthcare porque descubrió que estaba recibiendo pagos considerablemente más bajos que otras “instituciones similares”.
Muchas aseguradoras dicen que continuarán pagando por un período después de que termine un contrato —en general de entre 60 a 90 días— o para completar un “episodio de atención” particular, como un embarazo.
Pero, por ejemplo, con el cáncer, ¿eso significaría una ronda de quimioterapia o el curso completo de un tratamiento, que podría durar muchos años? ¿Es continuidad de cobertura si un paciente debe cambiar de oncólogo en medio de una terapia, o si tiene que dejar a un terapeuta eficaz?
Erin Moses, que trabaja para una pequeña organización sin fines de lucro, encontró a un nuevo terapeuta que le gustó después que ella y su esposo se mudaron a la Costa Central de California en febrero del año pasado. En septiembre, recibió una factura de la práctica que decía que había terminado su contrato con Anthem porque la aseguradora era lenta con sus reembolsos. Esto la dejó con una factura de $814.
“No es que no pudiéramos pagarlo, pero mi esposo y yo estamos tratando de ahorrar para una casa, y eso es mucho dinero”, dijo.
A menudo, a los pacientes los toma desprevenidos, sin saber qué hacer. Cuando Laura Alley se cayó de una escalera en septiembre de 2020 y necesitó cirugía para reparar su pelvis quebrada, el hospital y el cirujano estaban en la red.
Alley escribió al proyecto “Bill of the Month” de KFF Health News y NPR y dijo: “Lo que no podía saber de ninguna manera era que el grupo que proporcionaba la anestesia estaba en disputa con el proveedor de seguros de nuestra firma, y que desde el 30 de julio de 2020, ya no estaban en la red”.
Se sintió “como un títere”, dijo. “Mientras trabajo para recuperarme de una lesión traumática, estoy atrapada en medio de una disputa entre una enorme compañía de seguros y un gran grupo de médicos”.
Alley es dueña de una pequeña firma de arquitectura con su esposo, y terminaron pagando “casi $10,000” por servicios de anestesia fuera de la red. (Este tipo de factura fuera de la red para el paciente ahora estaría prohibido por el No Surprises Act, vigente desde 2022).
Nada de esto será noticia para Feldman, la paciente del Mount Sinai que fue una inocente espectadora en la disputa del sistema hospitalario con Oxford Health Plans. Los padres de Feldman la llamaron recientemente, diciendo que recibieron una carta de su aseguradora, Anthem, diciendo que el 1 de mayo podría terminar su contrato con el Hospital NewYork-Presbyterian, en donde la madrastra de Feldman recibe tratamiento por un cáncer de mama.
Es malo para la salud —y para la cordura— de los pacientes que las promesas percibidas de atención en sus planes de seguro puedan desaparecer repentinamente a mitad de año. Y los reguladores pueden hacer algo al respecto: obligar a los proveedores y aseguradoras a mantener sus contratos entre sí durante todo el término de las pólizas de los pacientes, para que ninguno quedé atrapado en una guerra con la que no tienen nada que ver.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 2 months ago
Health Care Costs, Health Industry, Insurance, Noticias En Español, Hospitals, Insurers
They Were Injured at the Super Bowl Parade. A Month Later, They Feel Forgotten.
KFF Health News and KCUR are following the stories of people injured during the Feb. 14 mass shooting at the Kansas City Chiefs Super Bowl celebration. Listen to how one Kansas family is coping with the trauma.
Jason Barton didn’t want to attend the Super Bowl parade this year. He told a co-worker the night before that he worried about a mass shooting. But it was Valentine’s Day, his wife is a Kansas City Chiefs superfan, and he couldn’t afford to take her to games since ticket prices soared after the team won the championship in 2020.
So Barton drove 50 miles from Osawatomie, Kansas, to downtown Kansas City, Missouri, with his wife, Bridget, her 13-year-old daughter, Gabriella, and Gabriella’s school friend. When they finally arrived home that night, they cleaned blood from Gabriella’s sneakers and found a bullet in Bridget’s backpack.
Gabriella’s legs were burned by sparks from a ricocheted bullet, Bridget was trampled while shielding Gabriella in the chaos, and Jason gave chest compressions to a man injured by gunfire. He believes it was Lyndell Mays, one of two men charged with second-degree felony murder.
“There’s never going to be a Valentine’s Day where I look back and I don’t think about it,” Gabriella said, “because that’s a day where we’re supposed to have fun and appreciate the people that we have.”
One month after the parade in which the U.S. public health crisis that is gun violence played out on live television, the Bartons are reeling from their role at its epicenter. They were just feet from 43-year-old Lisa Lopez-Galvan, who was killed. Twenty-four other people were injured. Although the Bartons aren’t included in that official victim number, they were traumatized, physically and emotionally, and pain permeates their lives: Bridget and Jason keep canceling plans to go out, opting instead to stay home together; Gabriella plans to join a boxing club instead of the dance team.
During this first month, Kansas City community leaders have weighed how to care for people caught in the bloody crossfire and how to divide more than $2 million donated to public funds for victims in the initial outpouring of grief.
The questions are far-reaching: How does a city compensate people for medical bills, recovery treatments, counseling, and lost wages? And what about those who have PTSD-like symptoms that could last years? How does a community identify and care for victims often overlooked in the first flush of reporting on a mass shooting: the injured?
The injured list could grow. Prosecutors and Kansas City police are mounting a legal case against four of the shooting suspects, and are encouraging additional victims to come forward.
“Specifically, we’re looking for individuals who suffered wounds from their trying to escape. A stampede occurred while people were trying to flee,” said Jackson County Prosecutor Jean Peters Baker. Anyone who “in the fleeing of this event that maybe fell down, you were trampled, you sprained an ankle, you broke a bone.”
Meanwhile, people who took charge of raising money and providing services to care for the injured are wrestling with who gets the money — and who doesn’t. Due to large donations from celebrities like Taylor Swift and Travis Kelce, some victims or their families will have access to hundreds of thousands of dollars for medical expenses. Other victims may simply have their counseling covered.
The overall economic cost of U.S. firearm injuries is estimated by a recent Harvard Medical School study at $557 billion annually. Most of that — 88% — represented quality-of-life losses among those injured by firearms and their families. The JAMA-published study found that each nonfatal firearm injury leads to roughly $30,000 in direct health care spending per survivor in the first year alone.
In the immediate aftermath of the shootings, as well-intentioned GoFundMe pages popped up to help victims, executives at United Way of Greater Kansas City gathered to devise a collective donation response. They came up with “three concentric circles of victims,” said Jessica Blubaugh, the United Way’s chief philanthropy officer, and launched the #KCStrong campaign.
“There were folks that were obviously directly impacted by gunfire. Then the next circle out is folks that were impacted, not necessarily by gunshots, but by physical impact. So maybe they were trampled and maybe they tore a ligament or something because they were running away,” Blubaugh said. “Then third is folks that were just adjacent and/or bystanders that have a lot of trauma from all of this.”
PTSD, Panic, and the Echo of Gunfire
Bridget Barton returned to Kansas City the day after the shooting to turn in the bullet she found in her backpack and to give a statement at police headquarters. Unbeknownst to her, Mayor Quinton Lucas and the police and fire chiefs had just finished a press conference outside the building. She was mobbed by the media assembled there — interviews that are now a blur.
“I don’t know how you guys do this every day,” she remembered telling a detective once she finally got inside.
The Bartons have been overwhelmed by well wishes from close friends and family as they navigate the trauma, almost to the point of exhaustion. Bridget took to social media to explain she wasn’t ignoring the messages, she’s just responding as she feels able — some days she can hardly look at her phone, she said.
A family friend bought new Barbie blankets for Gabriella and her friend after the ones they brought to the parade were lost or ruined. Bridget tried replacing the blankets herself at her local Walmart, but when she was bumped accidentally, it triggered a panic attack. She abandoned her cart and drove home.
“I’m trying to get my anxiety under control,” Bridget said.
That means therapy. Before the parade, she was already seeing a therapist and planning to begin eye movement desensitization and reprocessing, a form of therapy associated with treating post-traumatic stress disorder. Now the shooting is the first thing she wants to talk about in therapy.
Since Gabriella, an eighth grader, has returned to middle school, she has dealt with the compounding immaturity of adolescence: peers telling her to get over it, pointing finger guns at her, or even saying it should have been her who was shot. But her friends are checking on her and asking how she’s doing. She wishes more people would do the same for her friend, who took off running when the shooting started and avoided injury. Gabriella feels guilty about bringing her to what turned into a horrifying experience.
“We can tell her all day long, ‘It wasn’t your fault. She’s not your responsibility.’ Just like I can tell myself, ‘It wasn’t my fault or my responsibility,’” Bridget said. “But I still bawled on her mom’s shoulder telling her how sorry I was that I grabbed my kid first.”
The two girls have spent a lot of time talking since the shooting, which Gabriella said helps with her own stress. So does spending time with her dog and her lizard, putting on makeup, and listening to music — Tech N9ne’s performance was a highlight of the Super Bowl celebration for her.
In addition to the spark burns on Gabriella’s legs, when she fell to the concrete in the pandemonium she split open a burn wound on her stomach previously caused by a styling iron.
“When I see that, I just picture my mom trying to protect me and seeing everyone run,” Gabriella said of the wound.
It’s hard not to feel forgotten by the public, Bridget said. The shooting, especially its survivors, have largely faded from the headlines aside from court dates. Two additional high-profile shootings have occurred in the area since the parade. Doesn’t the community care, she wonders, that her family is still living with the fallout every day?
“I’m going to put this as plainly as possible. I’m f—ing pissed because my family went through something traumatic,” Bridget vented in a recent social media post. “I don’t really want anything other [than], ‘Your story matters, too, and we want to know how you’re doing.’ Have we gotten that? Abso-f—lutely not.”
‘What Is the Landscape of Need?’
Helped in part by celebrities like Swift and Kelce, donations for the family of Lopez-Galvan, the lone fatality, and other victims poured in immediately after the shootings. Swift and Kelce donated $100,000 each. With the help of an initial $200,000 donation from the Kansas City Chiefs, the United Way’s #KCStrong campaign took off, reaching $1 million in the first two weeks and sitting at $1.2 million now.
Six verified GoFundMe funds were established. One solely for the Lopez-Galvan family has collected over $406,000. Smaller ones were started by a local college student and Swift fans. Churches have also stepped up, and one local coalition had raised $183,000, money set aside for Lopez-Galvan’s funeral, counseling services for five victims, and other medical bills from Children’s Mercy Kansas City hospital, said Ray Jarrett, executive director of Unite KC.
Money for Victims Rolls In
Donations poured in for those injured at the Super Bowl Parade in Kansas City after the Feb. 14 shootings. The largest, starting with a $200,000 donation from the Kansas City Chiefs, is at the United Way of Greater Kansas City. Six GoFundMe sites also popped up, due in part to $100,000 donations each from Taylor Swift and Travis Kelce. Here’s a look at the totals as of March 12.United Way#KCStrong: $1.2 million.Six Verified GoFundMe AccountsLisa Lopez-Galvan GoFundMe (Taylor Swift donated): $406,142Reyes Family GoFundMe (Travis Kelce donated): $207,035Samuel Arellano GoFundMe: $11,896Emily Tavis GoFundMe: $9,518Cristian Martinez’s GoFundMe for United Way: $2,967Swifties’ GoFundMe for Children’s Mercy hospital: $1,060ChurchesResurrection (Methodist) “Victims of Violence Fund”: $53,358‘The Church Loves Kansas City’: $183,000
Meanwhile, those leading the efforts found models in other cities. The United Way’s Blubaugh called counterparts who’d responded to their own mass shootings in Orlando, Florida; Buffalo, New York; and Newtown, Connecticut.
“The unfortunate reality is we have a cadre of communities across the country who have already faced tragedies like this,” Blubaugh said. “So there is an unfortunate protocol that is, sort of, already in place.”
#KCStrong monies could start being paid out by the end of March, Blubaugh said. Hundreds of people called the nonprofit’s 211 line, and the United Way is consulting with hospitals and law enforcement to verify victims and then offer services they may need, she said.
The range of needs is staggering — several people are still recovering at home, some are seeking counseling, and many weren’t even counted in the beginning. For instance, a plainclothes police officer was injured in the melee but is doing fine now, said Police Chief Stacey Graves.
Determining who is eligible for assistance was one of the first conversations United Way officials had when creating the fund. They prioritized three areas of focus: first were the wounded victims and their families, second was collaborating with organizations already helping victims in violence intervention and prevention and mental health services, and third were the first responders.
Specifically, the funds will be steered to cover medical bills, or lost wages for those who haven’t been able to work since the shootings, Blubaugh said. The goal is to work quickly to help people, she said, but also to spend the money in a judicious, strategic way.
“We don’t have a clear sightline of the entire landscape that we’re dealing with,” Blubaugh said. “Not only of how much money do we have to work with, but also, what is the landscape of need? And we need both of those things to be able to make those decisions.”
Firsthand Experience of Daily Kansas City Violence
Jason used his lone remaining sick day to stay home with Bridget and Gabriella. An overnight automation technician, he is the family’s primary breadwinner.
“I can’t take off work, you know?” he said. “It happened. It sucked. But it’s time to move on.”
“He’s a guy’s guy,” Bridget interjected.
On Jason’s first night back at work, the sudden sound of falling dishes startled Bridget and Gabriella, sending them into each other’s arms crying.
“It’s just those moments of flashbacks that are kicking our butts,” Bridget said.
Tell Us About Your Experience
We are continuing to report on the effects of the parade shooting on the people who were injured and the community as a whole. Do you have an experience you want to tell us about, or a question you think we should look into? Message KCUR’s text line at (816) 601-4777. Your information will not be used in an article without your permission.
In a way, the shooting has brought the family closer. They’ve been through a lot recently. Jason survived a heart attack and cancer last year. Raising a teenager is never easy.
Bridget can appreciate that the bullet lodged in her backpack, narrowly missing her, and that Gabriella’s legs were burned by sparks but she wasn’t shot.
Jason is grateful for another reason: It wasn’t a terrorist attack, as he initially feared. Instead, it fits into the type of gun violence he’d become accustomed to growing up in Kansas City, which recorded its deadliest year last year, although he’d never been this close to it before.
“This crap happens every single day,” he said. “The only difference is we were here for it.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 2 months ago
Health Care Costs, Public Health, States, Emergency Medicine, Guns, Investigation, Kansas, Missouri
The State of the Union Is … Busy
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
President Joe Biden is working to lay out his health agenda for a second term, even as Congress races to finish its overdue spending bills for the fiscal year that began last October.
Meanwhile, Alabama lawmakers try to reopen the state’s fertility clinics over the protests of abortion opponents, and pharmacy giants CVS and Walgreens announce they are ready to begin federally regulated sales of the abortion pill mifepristone.
This week’s panelists are Julie Rovner of KFF Health News, Sarah Karlin-Smith of the Pink Sheet, Alice Miranda Ollstein of Politico, and Sandhya Raman of CQ Roll Call.
Panelists
Sarah Karlin-Smith
Pink Sheet
Alice Miranda Ollstein
Politico
Sandhya Raman
CQ Roll Call
Among the takeaways from this week’s episode:
- Lawmakers in Washington are completing work on the first batch of spending bills to avert a government shutdown. The package includes a bare-bones health bill, leaving out certain bipartisan proposals that have been in the works on drug prices and pandemic preparedness. Doctors do get some relief in the bill from Medicare cuts that took effect in January, but the pay cuts are not canceled.
- The White House is floating proposals on drug prices that include expanding Medicare negotiations to more drugs; applying negotiated prices earlier in the market life of drugs; and capping out-of-pocket maximum drug payments at $2,000 for all patients, not just seniors. At least some of the ideas have been proposed before and couldn’t clear even a Democratic-controlled Congress. But they also keep up pressure on the pharmaceutical industry as it challenges the government in court — and as Election Day nears.
- Many in public health are expressing frustration after the Centers for Disease Control and Prevention softened its covid-19 isolation guidance. The change points to the need for a national dialogue about societal support for best practices in public health — especially by expanding access to paid leave and child care.
- Meanwhile, CVS and Walgreens announced their pharmacies will distribute the abortion pill mifepristone, and enthusiasm is waning for the first over-the-counter birth control pill amid questions about how patients will pay its higher-than-anticipated list price of $20 per month.
- Alabama’s governor signed a law protecting access to in vitro fertilization, granting providers immunity from the state Supreme Court’s recent “embryonic personhood” decision. But with opposition from conservative groups, is the new law also bound for the Alabama Supreme Court?
Also this week, Rovner interviews White House domestic policy adviser Neera Tanden about Biden’s health agenda.
Plus, for “extra credit” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: NPR’s “How States Giving Rights to Fetuses Could Set Up a National Case on Abortion,” by Regan McCarthy.
Sarah Karlin-Smith: Stat’s “The War on Recovery,” by Lev Facher.
Alice Miranda Ollstein: KFF Health News’ “Why Even Public Health Experts Have Limited Insight Into Stopping Gun Violence in America,” by Christine Spolar.
Sandhya Raman: The Journal’s “‘My Son Is Not There Anymore’: How Young People With Psychosis Are Falling Through the Cracks,” by Órla Ryan.
Also mentioned on this week’s podcast:
- NBC News’ “CDC Updates Covid Isolation Guidelines for People Who Test Positive,” by Erika Edwards.
- New York Magazine’s “Did Trump Really Vow to Defund Schools With Vaccine Mandates?” by Margaret Hartmann.
click to open the transcript
Transcript: The State of the Union Is … Busy
KFF Health News’ ‘What the Health?’Episode Title: The State of the Union Is … BusyEpisode Number: 337Published: March 7, 2024
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello, and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News, and I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, March 7, at 9 a.m. As always, news happens fast and things might have changed by the time you hear this, so here we go. We are joined today via video conference by Alice Miranda Ollstein, of Politico.
Alice Miranda Ollstein: Hello.
Rovner: Sarah Karlin-Smith, of the Pink Sheet.
Sarah Karlin-Smith: Hi, everybody.
Rovner: And Sandhya Raman, of CQ Roll Call.
Raman: Good morning.
Rovner: Later in this episode we’ll have my interview with White House domestic policy adviser Neera Tanden about the Biden administration’s health accomplishment so far and their priorities for 2024. But first, this week’s news. It is a big week here in the nation’s capital. In addition to sitting through President Biden’s State of the Union address, lawmakers appear on the way to finishing at least some of the spending bills for the fiscal year that began last Oct. 1. Good thing, too, because the president will deliver to Congress a proposed budget for the next fiscal year that starts Oct. 1, 2024, next Monday. Sandhya, which spending bills are getting done this week, and which ones are left?
Sandhya Raman: We’re about half-and-half as of last night. The House is done with their six-bill deal that they released. Congress came to a bipartisan agreement on Sunday and released then, so the FDA is in that part, in the agriculture bill. We also have a number of health extenders that we can …
Rovner: Which we’ll get to in a second.
Raman: Now it’s on to the Senate and then to Biden’s desk, and then we still have the Labor HHS [Department of Labor and Department of Health and Human Services] bill with all of the health funding that we’re still waiting on sometime this month.
Rovner: Yeah, it’s fair to say that the half that they’re getting done now are the easy ones, right? It’s the big ones that are left.
Ollstein: Although, if they were so easy, why didn’t they get them done a long time ago? There have been a lot of fights over policy riders that have been holding things up, in addition to disagreements about spending levels, which are perennial of course. But I was very interested to see that in this first tranche of bills, Republicans dropped their insistence on a provision banning mail delivery of abortion pills through the FDA, which they had been fighting for for months and months and months, and that led to votes on that particular bill being canceled multiple times. It’s interesting that they did give up on that.
Rovner: Yes. I shouldn’t say these were the easy ones, I should say these were the easier ones. Not that there’s a reason that it’s March and they’re only just now getting them done, but they have until the 22nd to get the rest of them done. How is that looking?
Raman: We still have not seen text on those yet. If they’re able to get there, we would see that in the next week or so, before then. And it remains to be seen, that traditionally the health in Labor HHS is one of the trickiest ones to get across the finish line in a normal year, and this year has been especially difficult given, like Alice said, all of the different policy riders and different back-and-forth there. It remains to be seen how that’ll play out.
Rovner: They have a couple of weeks and we will see. All right, well as you mentioned, as part of this first spending minibus, as they like to call it, is a small package of health bills. We talked about some of these last week, but tell us what made the final cut into this current six-bill package.
Raman: It’s whittled down a lot from what I think a lot of lawmakers were hoping. It’s pretty bare-bones in terms of what we have now. It’s a lot of programs that have traditionally been added to funding bills in the past, extending the special diabetes program, community health center funding, the National Health Service Corps, some sexual risk-avoidance programs. All of these would be pegged to the end of 2024. It kind of left out a lot of the things that Congress has been working on, on health care.
Rovner: Even bipartisan things that Congress has been working for on health care.
Raman: Yeah. They didn’t come to agreement on some of the pandemic and emergency preparedness stuff. There were some provisions for the SUPPORT Act — the 2018 really big opioid law — but a lot of them were not there. The PBM [pharmacy benefit managers] reform, all of that, was not, not this round.
Rovner: But at least judging from the press releases I got, there is some relief for doctor fees in Medicare. They didn’t restore the entire 3.3% cut, I believe it is, but I think they restored all but three-quarters of a percent of the cut. It’s made doctors, I won’t say happy, but at least they got acknowledged in this package and we’ll see what happens with the rest of them. Well, by the time you hear this, the president’s State of the Union speech will have come and gone, but the White House is pitching hard some of the changes that the president will be proposing on drug prices. Sarah, how significant are these proposals? They seem to be bigger iterations of what we’re already doing.
Karlin-Smith: Right. Biden is proposing expanding the Medicare Drug [Price] Negotiation program that Congress passed through the Inflation Reduction Act. He wants to go from Medicare being able to negotiate eventually up to 20 drugs a year to up to 50. He seems to be suggesting letting drugs have a negotiated price earlier in their life, letting them have less time on the market before negotiation. Also, thinking about applying some of the provisions of the IRA right now that only apply to Medicare to people in commercial plans, so this $2,000 maximum out-of-pocket spending for patients. Then also there are penalties that drugmakers get if they raise prices above inflation that would also apply to commercial plans. He’s actually proposed a lot of this before in previous budgets and actually Democrats, if you go back in time, tried to actually get some of these things in the initial IRA and even with a Democratic-controlled capital, could not actually get Democratic agreement to go broader on some of the provisions.
Rovner: Thank you, Sen. [Joe] Manchin.
Karlin-Smith: That said, I think it is significant that Biden is still pressing on this, even if they would really need big Democratic majorities and more progressive Democratic majorities to get this passed, because it’s keeping the pressure on the pharmaceutical industry. There were times before the IRA was passed where people were saying, “Pharma just needs to take this hit, it’s not going to be as bad as they think it is. Then they’ll get a breather for a while.” They’re clearly not getting that. The public is still very concerned about drug pricing, and they’re both fighting the current IRA in court. Actually, today there’s a number of big oral arguments happening. At the same time, they’re trying to get this version of the IRA improved somehow through legislation. All at the same time Democrats are saying, “Actually, this is just the start, we’re going to keep going.” It’s a big challenge and maybe not the respite they thought they might’ve gotten after this initial IRA was passed.
Rovner: But as you point out, still a very big voting issue. All right, well I want to talk about covid, which we haven’t said in a while. Last Friday, the Centers for Disease Control and Prevention officially changed its guidance about what people should do if they get covid. There’s been a lot of chatter about this. Sarah, what exactly got changed and why are people so upset?
Karlin-Smith: The CDC’s old guidance, if you will, basically said if you had covid, you should isolate for five days. If you go back in time, you’ll remember we probably talked about how that was controversial on its own when that first happened, because we know a lot of people are infectious and still test positive for covid much longer than five days. Now they’re basically saying, if you have covid, you can return to the public once you’re fever-free for 24 hours and your symptoms are improving. I think the implication here is, that for a lot of people, this would be before five days. They do emphasize to some degree that you should take precautions, masking, think about ventilation, maybe avoid vulnerable people if you can.
But I think there’s some in the public health world that are really frustrated by this. They feel like it’s not science- and evidence-based. We know people are going to be infectious and contagious in many cases for longer than periods of time where the CDC is saying, “Sure, go out in public, go back to work.” On the flip side, CDC is arguing, people weren’t really following their old guidance. In part because we don’t have a society set up to structurally allow them to easily do this. Most people don’t have paid sick time. They maybe don’t have people to watch their children if they’re trying to isolate from them. I think the tension is that, we’ve learned a lot from covid and it’s highlighted a lot of the flaws already in our public health system, the things we don’t do well with other respiratory diseases like flu, like RSV. And CDC is saying, “Well, we’re going to bring covid in line with those,” instead of thinking about, “OK, how can we actually improve as a society managing respiratory viruses moving forward, come up with solutions that work.”
I think there probably are ways for CDC to acknowledge some of the realities. CDC does not have the power to give every American paid sick time. But if CDC doesn’t push to say the public needs this for public health, how are we ever going to get there? I think that’s really a lot of the frustration in a lot of the public health community in particular, that they’re just capitulating to a society that doesn’t care about public health instead of really trying to push the agenda forward.
Rovner: Or a society that’s actively opposed to public health, as it sometimes seems. I know speaking for my NF1, I was sick for most of January, and I used up all my covid tests proving that I didn’t have covid. I stayed home for a few days because I felt really crappy, and when I started to feel better, I wore a mask for two weeks because, hello, that seemed to be a practical thing to do, even though I think what I had was a cold. But if I get sick again, I don’t have any more covid tests and I’m not going to take one every day because now they cost $20 a pop. Which I suspect was behind a lot of this. It’s like, “OK, if you’re sick with a respiratory ailment, stay home until you start to feel better and then be careful.” That’s essentially what the advice is, right?
Ollstein: Yeah. Although one other criticism I heard was specifically basing the new guidance on being fever-free, a lot of people don’t get a fever, they have other symptoms or they don’t have symptoms at all, and that’s even more insidious for allowing spread. I heard that criticism as well, but I completely agree with Sarah, that this seems like allowing public behavior to shape the guidance rather than trying to shape the public behavior with the guidance.
Rovner: Although some of that is how public health works, they don’t want to recommend things that they know people aren’t going to do or that they know the vast majority of people aren’t going to do. This is the difficulty of public health, which we will talk about more. While meanwhile, speaking in Virginia earlier this week, former President Donald Trump vowed to pull all federal funding for schools with vaccine mandates. Now, from the context of what he was saying, it seemed pretty clear that he was talking only about covid vaccine mandates, but that’s not what he actually said. What would it mean to lift all school vaccine mandates? That sounds a little bit scary.
Raman: That would basically affect almost every public school district nationwide. But even if it’s just covid shots, I think that’s still a little bit of a shift. You see Trump not taking as much public credit anymore for the fact that the covid vaccines were developed under his administration, Operation Warp Speed, that started under the Trump administration. It’s a little bit of a shift compared to then.
Rovner: I’m old enough to remember two cycles ago, when there were Republicans who were anti-vaccine or at least anti-vaccine curious, and the rest of the Republican Party was like, “No, no, no, no, no.” That doesn’t seem to be the case anymore. Now it seems to be much more mainstream to be anti-vax in general. Cough, cough. We see the measles outbreak in Florida, so we will clearly watch that space, too.
All right, moving on to abortion. Later this month, the Supreme Court will hear oral argument in the case that could severely restrict distribution of the abortion pill mifepristone. But in the meantime, pharmacy giants, CVS and Walgreens have announced they will begin distributing the abortion pill at their pharmacies. Alice, why now and what does this mean?
Ollstein: It’s interesting that this came more than a year after the big pharmacies were given permission to do this. They say it took this long because they had to get all of these systems up in place to make sure that only certified pharmacists were filling prescriptions from certified prescribing doctors. All of this is required because when the Biden administration, when the FDA, moved to allow this form of distribution of the abortion pill, they still left some restrictions known as REMS [risk evaluation and mitigation strategies] in place. That made it take a little more time, more bureaucracy, more box checking, to get to this point. It is interesting that given the uncertainty with the Supreme Court, they are moving forward with this. It’s this interesting state-versus-federal issue, because we reported a year ago that Walgreens and CVS would not distribute the pills in states where Republican state attorneys general have threatened them with lawsuits.
So, they’ve noted the uncertainty at the state level, but even with this uncertainty at the federal level with the Supreme Court, which could come in and say this form of distribution is not allowed, they’re still moving forward. It is limited. It’s not going to be, even in blue states where abortion is protected by law, they’re not going to be at every single CVS. They’re going to do a slower, phased rollout, see how it goes. I’m interested in seeing if any problems arise. I’m also interested in seeing, anti-abortion groups have vowed to protest these big pharmacy chains for making this medication available. They’ve disrupted corporate meetings, they’ve protested outside brick-and-mortar pharmacies, and so we’ll see if any of that continues and has an effect as well.
Rovner: It’s hard to see how the anti-abortion groups though could have enough people to protest every CVS and Walgreens selling the abortion pill. That will be an interesting numbers situation. Well, in a case of not-so-great timing, if only for the confusion potential, also this week we learned that the first approved over-the-counter birth control pill, called Opill, is finally being shipped. Now, this is not the abortion pill. It won’t require a prescription, that’s the whole point of it being over-the-counter. But I’ve seen a lot of advocacy groups that worked on this for years now complaining that the $20 per month that the pill is going to cost, it’s still going to be too much for many who need it. Since it’s over-the-counter, it’s not going to be covered by most insurance. This is a separate issue of its own that’s a little bit controversial.
Karlin-Smith: You can with over-the-counter drugs, if you have a flexible spending account or an HSA or something else, you may be able to use money that’s somehow connected to your health insurance benefit or you’re getting some tax breaks on it. However, I think this over-the-counter pill is probably envisioned most for people that somehow don’t have insurance, because we know the Affordable Care Act provides birth control methods with no out-of-pocket costs for people. So if you have insurance, most likely you would be getting a better deal getting a prescription and going that route for the same product or something similar.
The question becomes then, does this help the people who fall in those gaps who are probably likely to have less financial means to begin with? There’s been some polling and things that suggest this may be too high a price point for them. I know there are some discounts on the price. Essentially if you can buy three months upfront or even some larger quantities, although again that means you then have to have that larger sum of money upfront, so that’s a big tug of war. I think the companies argue this is pretty similar pricing to other over-the-counter drug products in terms of volume and stuff, so we’ll see what happens.
Rovner: I think they were hoping it was going to be more like $5 a month and not $20 a month. I think that came as a little bit of a disappointment to a lot of these groups that have been working on this for a very long time.
Ollstein: Just quickly, the jury is also still out on insurance coverage, including advocacy groups are also pressuring public insurance, Medicaid, to come out and say they’ll cover it as well. So we’ll keep an eye on that.
Rovner: Yeah, although Medicaid does cover prescription birth control. All right, well let us catch up on the IVF [in vitro fertilization] controversy in Alabama, where there was some breaking news over last night. When we left off last week, the Alabama Legislature was trying to come up with legislation that would grant immunity to fertility clinics or their staff for “damaging or killing fertilized embryos,” without overtly overruling the state Supreme Court decision from February that those embryos are, “extrauterine children.” Alice, how’s that all going?
Ollstein: Well, it was very interesting to see a bunch of anti-abortion groups come out against the bill that Alabama, mostly Republicans, put together and passed and the Republican governor signed it into law. The groups were asking her to veto it; they didn’t want that kind of immunity for discarding or destroying embryos. Now what we will see is if there’s going to be a lawsuit that lands this new law right back in front of the same state Supreme Court that just opened this whole Pandora’s box in the first place, that’s very possible. That’s one thing I’m watching. I guess we should also watch for other states to take up this issue. A lot of states have fetal personhood language, either in their constitutions or in statute or something, so really any of those states could become the next Alabama. All it would take is someone to bring a court challenge and try to get a similar ruling.
Rovner: I was amused though that the [Alabama] Statehouse passed the immunity law yesterday, Wednesday during the day. But the Senate passed it later in the evening and the governor signed it. I guess she didn’t want to let it hang there while these big national anti-abortion groups were asking her to veto it. So by the time I woke up this morning, it was already law.
Ollstein: It’s just been really interesting, because the anti-abortion groups say they support IVF, but they came out against the Democrats’ federal bill that would provide federal protections. They came out against nonbinding House resolutions that Republicans put forward saying they support IVF, and they came out against this Alabama fix. So it’s unclear what form of IVF, if any, they do support.
Rovner: Meanwhile, in Kentucky, the state Senate has overwhelmingly passed a bill that would permit a parent to seek child support retroactively to cover pregnancy expenses up until the child reaches age 1. So you have until the child turns 1 to sue for child support. Now, this isn’t technically a “personhood” bill, and it’s legit that there are expenses associated with becoming a parent even before a baby is born, but it’s skating right up to the edge of that whole personhood thing.
It brings me to my extra credit for this week, which I’m going to do early. It’s a story from NPR called, “How States Giving Rights to Fetuses Could Set Up a National Case on Abortion,” by Regan McCarthy of member station WFSU in Tallahassee. In light of Florida’s tabling of a vote on its personhood bill in the wake of the Alabama ruling last week, the story poses a question I hadn’t really thought about in the context of the personhood debate, whether some of these partway recognition laws, not just the one in Kentucky, but there was one in Georgia last year, giving tax deductions for children who are not yet born as long as you could determine a heartbeat in the second half of the year, because obviously in the first half of the year the child would’ve been born.
Whether those are part of a very long game that will give courts the ability to put them all together at some point and declare not just embryos but zygotes children. Is this in some ways the same playbook that anti-abortion forces use to get Roe [v. Wade] overturned? That was a very, very long game and at least this story speculates that that might be what they’re doing now with personhood.
Ollstein: Some anti-abortion groups are very open that it is what they want to do. They have been seeding the idea in amicus briefs and state policies. They’ve been trying to tuck personhood language into all of these things to eventually prompt such a ruling, ideally from the Supreme Court and, in their view. So whether that moves forward remains to be seen, but it’s certainly the next goal. One of many next goals on the horizon.
Rovner: Yes, one of many. All right, well moving on. Last week I called the cyberattack on Change Healthcare, a subsidiary of UnitedHealth Group, the biggest under-covered story in health care. Well, it is not under-covered anymore. Two weeks later, thousands of hospitals, pharmacies, and doctor practices still can’t get their claims paid. It seems that someone, though it’s not entirely clear who, paid the hackers $22 million in ransom. But last time I checked the systems were still not fully up. I saw a letter this morning from the Medicaid directors worrying about Medicaid programs getting claims fulfilled. How big a wake-up call has this been for the health industry, Sarah? This is a bigger deal than anybody expected.
Karlin-Smith: There’s certainly been cyberattacks on parts of the health system before in hospitals. I think the breadth of this, because it’s UnitedHealth [Group], is really significant. Particularly, because it seems like some health systems were concerned that the broader United network of companies and systems would get impacted, so they sort of disconnected from things that weren’t directly changed health care, and that ended up having broader ramifications. It’s one consequence of United being such a big monolith.
Then the potential that United paid a ransom here, which is not 100% clear what happened, is very worrisome. Again, because there’s this sense that, that will then increase the — first, you’re paying the people that then might go back and do this, so you’re giving them more money to hack. But also again, it sets up a precedent, that you can hack health systems and they will pay you. Because it is so dangerous, particularly when you start to get involved in attacking the actual systems that provide people care. So much, if you’ve been in a hospital lately or so forth, is run on computer systems and devices, so it is incredibly disruptive, but you don’t want to incentivize hackers to be attacking that.
Rovner: I certainly learned through this how big Change Healthcare, which I had never heard of before this hack and I suspect most people even who do health policy had never heard of before this attack, how embedded they are in so much of the health care system. These hackers knew enough to go after this particular system that affected so much in basically one hack. I’m imagining as this goes forward, for those who didn’t listen to last week’s podcast, we also talked about the Justice Department’s new investigation into the size of UnitedHealth [Group], an antitrust investigation for… It was obviously not prompted by this, it was prompted by something else, but I think a lot of people are thinking about, how big should we let one piece of the health care system get in light of all these cyberattacks?
All right, well we’ll obviously come back to this issue, too, as it resolves, one would hope. That is the news for this week. Now we will play my interview with White House domestic policy adviser Neera Tanden, and then we will come back with our extra credits.
I am so pleased to welcome to the podcast Neera Tanden, domestic policy adviser to President Biden, and director of the White House Domestic Policy Council. For those of you who don’t already know her, Neera has spent most of the last two decades making health policy here in Washington, having worked on health issues for Hillary Clinton, President Barack Obama, and now President Joe Biden. Neera, thank you so much for joining us.
Neera Tanden: It’s really great to be with you, Julie.
Rovner: As we tape this, the State of the Union is still a few hours away and I know there’s stuff you can’t talk about yet. But in general, health care has been a top-of-mind issue for the Biden administration, and I assume it will continue to be. First, remind us of some of the highlights of the president’s term so far on health care.
Tanden: It’s a top concern for the president. It’s a top issue for us, but that’s also because it’s really a top issue for voters. We know voters have had significant concerns about access, but also about costs. That is why this administration has really done more on costs than any administration. This is my third, as you noted, so I’m really proud of all the work we’ve done on prescription drugs, on lowering costs of health care in the exchanges, on really trying to think through the cost burden for families when it comes to health care.
When we talk about prescription drugs, it’s a wide-ranging agenda, there are things or policies that people have talked about for decades, like Medicare negotiating drug prices, that this president is the first president to truly deliver on, which he will talk about in the State of the Union. But we’ve also innovated in different policies through the Inflation Reduction Act, the inflation rebates, which ensure that drug companies don’t raise the price of drugs faster than inflation. When they do, they pay a rebate both to Medicare but also ultimately to consumers. Those our high-impact policies that will really take a comprehensive approach on lowering prices.
Rovner: Yet for all the president has accomplished, and people who listen to the podcast regularly will know that it has been way more than was expected given the general polarization around Washington right now. Why does the president seem to get so little credit for getting done more things than a lot of his predecessors were able to do in two terms?
Tanden: Well, I think people do recognize the importance of prescription drug coverage. And health care as an issue that the president — it’s not my place to talk about politics, but he does have significant advantages on issues like health care. That I think, is because we’ve demonstrated tangible results. People understand what $35 insulin means. What I really want to point to in the Medicare negotiation process is, Sept. 1, Medicare will likely have a list of drugs which are significantly lower costs, that process is underway. But my expectation, you know I’m not part of it, that’s being negotiated by CMS [Centers for Medicare & Medicaid Services] and HHS, but we expect to have a list of 10 drugs that are high-cost items for seniors in which they’ll see a price that is lower than what they pay now. That’s another way in which, like $35 insulin, we’ll have tangible proof points of what this administration will be delivering for families.
Rovner: There’s now a record number of people who have health insurance under the Affordable Care Act, which I remember you also worked on. But in surveys, as you noted, voters now say they’re less worried about coverage and more worried about not being able to pay their medical bills even if they have insurance. I know a lot of what you’re doing on the drug side is limited to Medicare. Now, do you expect you’re going to be able to expand that to everybody else?
Tanden: First and foremost, our drug prices will be public, as you know. And as you know, prices in Medicare have been able to influence other elements of the health care system. That is really an important part of this. Which is that again, those prices will be public and our hope is that the private sector adopts those prices, because they’re ones that are negotiated. We expect this to affect, not just seniors, but families throughout the country.
There are additional actions we’ll be taking on Medicare drug negotiation. That will be a significant portion of the president’s remarks on health care, not just what we’ve been able to do in Medicare drug negotiation, but how we can really build on that and really ensure that we are dramatically reducing drug costs throughout the system. I look forward to hearing the president on that topic.
Rovner: I know we’re also going to get the budget next week. Are there any other big health issues that will be a priority this year?
Tanden: The president will have a range of policies on issues like access to sickle cell therapies, ensuring affordable generic drugs are accessible to everybody, ensuring that we are building on the Affordable Care Act gains. You mentioned this, but I just really do want to step back and talk about access under the Affordable Care Act. Because I think if people started off at the beginning of this administration and said the ACA marketplaces close to double, people would’ve been shocked. You know this well, a lot of people thought the exchanges were maximizing their potential. There are a lot of people who may not be interested in that, but the president had, in working with Congress, made the exchanges more affordable.
We’ve seen record adoption: 21 million people covered through the ACA exchanges today, when it was 12 million when we started. That’s 9 million more people who have the security of affordable health care coverage. I think it’s a really important point, which is, why are people signing up? Because it is a lot more affordable? Most people can get a very affordable plan. People are saving on average $800, and that affordability is crucial. Of course we have to do more work to reduce costs throughout the health care system. But it’s an important reminder that when you lower drug costs, you also have the ability to lower premiums and it’s another way in which we can drive health care costs down. I would be genuinely honest with you, which is, I did not think we would be able to do all of these things at the beginning of the administration. The president has been laser-focused on delivering, and as you know from your work on the ACA, he did think it was a big deal.
Rovner: I have that on a T-shirt.
Tanden: A lot of people have talked about different things, but he has been really focused on strengthening the ACA. He’ll talk about how we need to strengthen it in the future, and how that is another choice that we face this year, whether we’re going to entertain repealing the ACA or build on it and ensure that the millions of people who are using the ACA have the security to know that it’s there for them into the future. Not just on access, but that also means protections for preexisting conditions, ensuring women can no longer be discriminated against, the lifetime annual limits. There’s just a variety of ways that ACA has transformed the health care system to be much more focused on consumers.
Rovner: Last question. Obviously reproductive health, big, big issue this year. IVF in particular has been in the news these past couple of weeks, thanks to the Alabama Supreme Court. Is there anything that President Biden can do using his own executive power to protect access to reproductive health technology? And will we hear him at some point address this whole personhood movement that we’re starting to see bubble back up?
Tanden: I think the president will be very forceful on reproductive rights and will discuss the whole set of freedoms that are at stake and reproductive rights and our core freedom at stake this year. You and I both know that attacks on IVF are actually just the effectuation of the attacks on Roe. What animates the attacks on Roe, would ultimately affect IVF. I felt like I was a voice in the wilderness for the last couple of decades, where people were saying … They’re just really focused on Roe v. Wade. It won’t have any impact on IVF or [indecipherable] they’re just scare tactics when you talk about IVF.
Obviously the ideological underpinnings of attacks on Roe ultimately mean that you would have to take on IVF, which is exactly what women are saying. I think the president will speak forcefully to the attacks on women’s dignity that women are seeing throughout this country, and how this ideological battle has translated to misery and pain for millions of women. Misery and pain for their families. And has really reached the point where women who are desperate to have a family are having their reproductive rights restricted because of the ideological views of a minority of the country. That is a huge issue for women, a huge issue for the country, and exactly why he’ll talk about moving forward on freedoms and not moving us back, sometimes decades, on freedom.
Rovner: Well, Neera Tanden, you have a lot to keep you busy. I hope we can call on you again.
Tanden: There’s few people who know the health care system as well as Julie Rovner, so it’s just a pleasure to be with you.
Rovner: OK, we are back. It’s time for our extra-credit segment. That’s when we each recommend a story we read this week we think you should read, too. As always, don’t worry if you miss it. We will post the links on the podcast page at kffhealthnews.org and in our show notes on your phone or other mobile device. I already did mine. Sandhya, why don’t you go next?
Raman: My extra credit this week is called “My Son Is Not There Anymore: How Young People With Psychosis Are Falling Through the Cracks,” and it’s by Órla Ryan for The Journal. This was a really interesting story about schizophrenia in Ireland and just how the earlier someone’s symptoms are treated the better the outcome. But a lot of children and minors with psychosis and schizophrenia struggle to get access to the care they need and just fall through the cracks of being transferred from one system to another, especially if they’re also dealing with disabilities. If some of these symptoms are treated before puberty, the severity is likely to go down a lot and they’re much less likely to experience psychosis. She takes a really interesting look at a specific case and some of the consequences there.
Rovner: I feel like we don’t look enough at what other countries health systems are doing because we could all learn from each other. Alice, why don’t you go next?
Ollstein: I have a piece by KFF Health News called “Why Even Public Health Experts Have Limited Insight Into Stopping Gun Violence in America.” It’s looking at the toll taken by the long-standing restrictions on federal funding for research into gun violence, investigating it as a public health issue. Only recently this has started to erode at the federal level and some funding has been approved for this research, but it is so small compared to the death toll of gun violence. This article sort of argues that lacking that data for so many years is why a lot of the quote-unquote “solutions” that places have tried to implement to prevent gun violence, just don’t work. They haven’t worked, they haven’t stopped these mass shootings, which continue to happen. So, arguing that, if we had better data on why things happen and how to make it less lethal, and safe, in various spaces, that we could implement some things that actually work.
Rovner: Yeah, we didn’t have the research just as this problem was exploding and now we are paying the price. Sarah.
Karlin-Smith: I looked at the first in a Stat News series by Lev Facher, “The War on Recovery: How the U.S. Is Sabotaging Its Best Tools to Prevent Deaths in the Opioid Epidemic.” It looks at why the U.S. has had access to cheap effective medicines that help reduce the risk of overdose and death for people that are struggling with opioid-use disorder haven’t actually been able, in most cases, to get access to these drugs, methadone and buprenorphine.
The reasons range from even people not being allowed to take the drugs when they’re in prison, to not being able to hold certain jobs if you’re taking these prescription medications, to Narcotics Anonymous essentially banning people from coming to those meetings if they use these drugs, to doctors not being willing or open to prescribing them. Then of course, there’s what always seems to come up these days, the private equity angle. Which is that methadone clinics are becoming increasingly owned by private equity and they’ve actually pushed back on and lobbied against policies that would make it easier for people to get methadone treatment. Because one big barrier to methadone treatment is, right now you largely have to go every day to a clinic to get your medicine, which it can be difficult to incorporate into your life if you need to hold a job and take care of kids and so forth.
It’s just a really fascinating dive into why we have the tools to make what is really a terrible crisis that kills so many people much, much better in the U.S. but we’re just not using them. Speaking of how other countries handle it, the piece goes a little bit into how other countries have had more success in actually being open to and using these tools and the differences between them and the U.S.
Rovner: Yeah, it’s a really good story. All right, that is our show. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left us a review; that helps other people find us, too. Special thanks as always to our technical guru, Francis Ying, and our editor, Emmarie Huetteman. As always, you can email us your comments or questions. We’re at whatthehealth@kff.org, or you can still find me at X, @jrovner, or @julierovner at Bluesky or @julie.rovner at Threads. . Sarah, where are you these days?
Karlin-Smith: Trying mostly to be on Blue Sky, but on X, Twitter a little bit at either @SarahKarlin or @sarahkarlin-smith.
Rovner: Alice.
Ollstein: @alicemiranda on Blue Sky, and @AliceOllstein on X.
Rovner: Sandhya.
Raman: @SandhyaWrites on X and on Blue Sky.
Rovner: We will be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 3 months ago
Courts, COVID-19, Elections, Health Care Costs, Insurance, Medicaid, Medicare, Multimedia, Pharmaceuticals, Public Health, States, Abortion, Alabama, Biden Administration, CDC, Children's Health, Contraception, Drug Costs, KFF Health News' 'What The Health?', Legislation, Podcasts, Prescription Drugs, U.S. Congress, vaccines, Women's Health
Readers Call on Congress to Bolster Medicare and Fix Loopholes in Health Policy
Letters to the Editor is a periodic feature. We welcome all comments and will publish a selection. We edit for length and clarity and require full names.
Occupational Therapists Change Lives. CMS Must Better Support Them.
Letters to the Editor is a periodic feature. We welcome all comments and will publish a selection. We edit for length and clarity and require full names.
Occupational Therapists Change Lives. CMS Must Better Support Them.
Occupational therapists are critical in helping patients adjust to new circumstances, empowering them with the tools they need to overcome barriers and regain control over their lives. Whether you’re transitioning from homelessness into a home (“In Los Angeles, Occupational Therapists Tapped to Help Homeless Stay Housed,” Jan. 24) or relearning how to do everyday tasks following a stroke, OTs are key to patients’ care plan.
But the critical care provided by OTs is being threatened by another year of payment cuts imposed by Medicare, our nation’s health care program for people age 65 and up. Many older patients treated by OTs access insurance coverage through Medicare, which typically reimburses providers at a lower rate than private insurers. And now, with payment cuts that went into effect on Jan. 1 — despite warnings and backlash from lawmakers, patients, and providers — OTs are struggling to deliver care with lower Medicare payment.
Investing in occupational therapy improves health outcomes for patients, has the potential to reduce the burden on hospitals and other health care clinicians, and keeps individuals healthy and independent. Medicare’s payment cuts only compromise the ability of providers to deliver comprehensive, compassionate care. Medicare must recognize the long-term patient benefits occupational therapy has to offer.
Luckily, Congress is considering a bill that would reverse these harmful payment cuts. The Preserving Seniors’ Access to Physicians Act of 2023 (HR 6683), would reverse the cuts that went into effect on Jan. 1, alleviating financial stress for occupational therapists and preserving patient access. I strongly urge lawmakers to prioritize and protect occupational therapy services and immediately pass HR 6683 for America’s Medicare patients.
— Doug Fosco, an occupational therapist practicing at Two Trees Physical Therapy in Ventura, California
An assistant professor at Ontario’s Western University weighed in on X.
Great to see the role of #occupationaltherapy with persons who experience #homelessness profiled in @latimes. Thanks #deborahpitts for your work in LA with @USC and #skidrowhousingtrust . Check it out @CAOT_ACE @OSOTvoice ! @CAEHomelessness https://t.co/S5s9jhgoxI
— Carrie Anne Marshall, PhD (@cannemarshall) January 24, 2024
— Carrie Anne Marshall, Sydenham, Ontario
Congress Must Finish the Job on Site-Neutral Payments
There’s an obvious solution to rein in government spending and patient out-of-pocket costs: Pay identical prices for identical care (“In Fight Over Medicare Payments, the Hospital Lobby Shows Its Strength,” Feb. 13).
As a community oncologist, it is clear to me how Medicare favors hospitals by paying more for services provided in hospital outpatient departments (HOPDs) than the same care delivered in community-based facilities. For example, last year, Medicare paid over 2.5 times as much in an HOPD as in a free-standing office for drug administration services. It’s not just Medicare paying too much; patients also face higher out-of-pocket costs for care provided in HOPDs. If the Lower Costs, More Transparency Act is signed into law, cancer patients would immediately pay less for treatments like chemotherapy.
One unintended consequence of current payment disparities is consolidation. To leverage higher reimbursements, health systems scoop up independent practices — a growing problem that is particularly pronounced in oncology. From 2008 to 2020, 435 community cancer clinics closed, while 722 contracted with or were acquired by hospitals. This consolidation is reducing patient access, particularly in rural areas, where many independent clinics operate small satellite sites that tend to be the first to close when hospitals acquire a community-based practice.
It’s time for Congress to finish the job through bills like the Lower Costs, More Transparency Act and the SITE Act, which would help level the playing field once and for all.
— Scott Rushing, Vancouver, Washington
The chief marketing officer of SKYGEN cut to the chase on X.
In the battle to control healthcare costs, hospitals are deploying their political power to protect their bottom lines. https://t.co/97r502KrpM
— Donald H. Polite (@DonaldPolite) February 15, 2024
— Donald H. Polite, Milwaukee
The ‘Gold Card’ Shuffle
Prior authorization, by definition, creates delays in care and bureaucratic barriers for physicians — which is why it is so troubling that many insurers now require prior authorization for large categories of procedures with no evidence of overuse or inappropriate use. With health insurers increasingly implementing questionable prior authorization policies, state and federal lawmakers are racing to erect safeguards that ensure patients’ access to timely care (“States Target Health Insurers’ ‘Prior Authorization’ Red Tape,” Feb. 12).
Much of the legislation to address this growing problem centers around the use of “Gold Cards” that exempt providers whose previous requests for prior authorization have been approved for a certain period. In general, these laws are important for patients who can’t afford to wait for care — especially in the field of gastroenterology where severe abdominal pain or blood in the stool could indicate a serious condition like cancer.
However, some insurance companies are co-opting the “Gold Card” term to justify new prior authorization requirements instead of streamlining existing ones. Consider the case of UnitedHealthcare, which announced it would roll out a “Gold Card” prior authorization program this year for most colonoscopies and endoscopies. No other insurer has levied such a policy, nor does the research suggest there is an overutilization of these vital services. Despite nearly a year of good faith efforts to seek transparency and guidance from UHC, the company has failed to release any data or justification that these services are improperly utilized.
If anything, diagnostic and surveillance colonoscopies and endoscopies may be underutilized. New research from the American Cancer Society shows an alarming spike in the number of younger Americans being diagnosed with and dying from colorectal cancer. Since symptoms of colorectal cancer don’t often appear until the disease is at a more advanced stage, early detection is key. Any disruption to surveillance colonoscopies (which follow removal of a precancerous polyp and are part of the screening continuum) caused by UHC’s forthcoming prior authorization policy would be dangerous for the company’s 27 million commercial beneficiaries.
The American Gastroenterological Association strongly urges UHC to rescind its “Gold Card” prior authorization policy. Policymakers must monitor how insurers are co-opting concepts meant to protect patients, in particular UHC’s faux “Gold Card,” which threatens patient access to a procedure proven to save lives.
— Barbara Jung, president of the American Gastroenterological Association, Seattle
In an X post, a senior fellow at the Manhattan Institute pointed out the value in requiring prior authorization.
Case-by-case prior authorization is never fun, but surely preferable to most other methods of eliminating needless spending (ex post denials of reimbursement, higher cost-sharing, capped global budgets, etc…) https://t.co/nYijeiAUtP
— Chris Pope (@CPopeHC) February 12, 2024
— Chris Pope, a senior fellow at the Manhattan Institute, New York City
Hospice in Prison: A Transformative View
I was so impressed with Markian Hawryluk’s exceptionally well-written article “Death and Redemption in an American Prison” (Feb. 21). I was privileged to serve as an inaugural member of the American Hospital Association’s Circle of Life Award committee, from 1999 to 2004. The awards were established to recognize the most outstanding hospice and palliative care programs in the U.S. The very first year, we received an application from the country’s largest maximum-security prison in Angola, Louisiana, the subject of Mr. Hawryluk’s wonderful article. The prison was one of the five finalists chosen for a site visit in 2000. I volunteered to be on team to visit and evaluate the prison’s hospice services.
Twenty-four years later, I still remember my conversation with one of the inmate volunteers who had just returned from bathing and feeding a dying prisoner. He told me the inmate said, “I love you.” Then the inmate volunteer stated, “I never heard those words before — not from my father, who I never met, nor from my mother.” In 2000, if one were sentenced to life at the Louisiana State Penitentiary, there was no chance for parole. When we met with the warden, he mentioned there was a waiting list of prisoners who wanted to be hospice volunteers.
Please convey my deep appreciation to Mr. Hawryluk for his outstanding article.
— Paul Hofmann, president of the Hofmann Healthcare Group, Moraga, California
A digital storyteller shared the article on X.
Your one, long read for today – it's beautifully and thoughtfully written and reported"Sometimes when you're in a dark place, you find out who you really are and what you wish you could be," Steven Garner said. "Even in darkness, I could be a light."https://t.co/57asjh11ZV
— Ameera B. ا ميرة بت 🪬 (@meerabee) February 19, 2024
— Ameera Butt, Los Angeles
Feeling Insecure Because of Social Security Tactics
When will you continue your series on the overpayments to the Social Security Administration (“Overpayment Outrage”)? People are still suffering without benefits because the agency says people were overpaid and wants the money back. Why is nobody else asking more questions?
People in this country worked hard and paid taxes. And when it is time to retire, the Social Security Administration refuses to pay if, all of a sudden, it discovers you have been overpaid. They have told me I owe them $30,000 from over 20 years ago, and I do not know what they are talking about, but they want to take my retirement money until it’s paid off. Or they want you to say it is OK to take a percentage out. Doing that would say you’re guilty and you owe the money — to me, that’s blackmail.
New immigrants get free phones, medical care, debit cards, food assistance, schooling … that comes to more than my little amount of retirement money. It seems the government can afford to take care of them, but not their own. Everyone who has had their Social Security taken away should be entitled to the free services they get, as we are in the same position — now we have nothing either.
— Thomas Troy, New York City
Lifelong Minnesotan and epidemiologist Eric Weinhandl chimed in on X.
Relatively severe incompetency. Social Security Chief Apologizes to Congress for Misleading Testimony on Overpaymentshttps://t.co/HYPcTU5tVW
— Eric Weinhandl (@eric_weinhandl) December 27, 2023
— Eric Weinhandl, Victoria, Minnesota
A Balanced View of the Law Curbing Surprise Bills
KFF Health News’ Elisabeth Rosenthal has long advocated for quality, patient-centric medical care. However, her recent article, “The No Surprises Act Comes with Some Surprises” (Feb. 14), falls short in its analysis of surprise medical billing and the federal No Surprises Act (NSA). While she places blame on physicians, the reality is more complicated.
Patients with health insurance should not be burdened with paying more than their normal in-network cost-sharing amount for unexpected out-of-network care. This is not controversial. The legislative debate was never about whether to act on surprise billing, but rather how to act. While insurers favored policies that would allow them to calculate the payment rate medical providers receive, with the NSA, Congress instead chose an approach intended to protect sustainable payment rates that would preserve patients’ access to care. The NSA removes patients from payment disputes between insurers and providers and is intended to encourage negotiations between insurers and providers, with an option for neutral arbitration.
Rosenthal’s article implies a “greedy doctor” narrative, omitting discussion of insurers as contributing to the problems with the NSA’s implementation. While the article notes that many requests for arbitration came from private equity-associated provider organizations, it neglected to note that a single insurance company (UnitedHealthcare) was involved in almost 40% of arbitration disputes. That is more than the rest of the top five insurance organizations combined. The article also quotes and references papers by Zack Cooper, whose undisclosed connections with UnitedHealthcare came to light through litigation. As reported, UnitedHealthcare not only provided data to Cooper, but helped frame the narrative of the work.
NSA rulemaking has financially incentivized insurers to leverage the NSA to unilaterally reduce existing contracted rates and push physicians out-of-network. As for the projected number of requests for arbitration in 2022 (which underestimated “providers’ ire by an order of magnitude”), that projection ignored existing data. In just the first six months of 2021, Texas alone had more than twice as many arbitration submissions for its state law as the federal government projected for the nation for a full year. More importantly, the article ignores the issue of why doctors request arbitration. Since arbitration is baseball-style and “loser pays,” there is a strong disincentive to request it without a solid reason. In the second quarter of 2023, providers won nearly 80% of disputes, reflecting the fact that doctors are going to arbitration when insurers’ actions are unreasonable.
Further, while it is true that before the NSA too many patients were receiving bills for unexpected out-of-network care, a report from the Department of Health and Human Services noted that out-of-network billing was actually declining prior to the NSA. Physician survey data suggests that post-NSA out-of-network care is now increasing due to some insurers’ actions.
The bipartisan NSA is a balanced solution to a complicated problem. Difficulties with the law’s implementation, including the volume of dispute submissions and backlog of cases, are due to unintended consequences from rulemaking. Addressing these challenges requires an honest conversation about their cause. Going forward, rulemaking is needed to promote fair network contracting, limit the need for arbitration, and, most importantly, protect patients’ access to care.
— Rich Heller, a pediatric radiologist and the associate chief medical officer for health policy, Radiology Partners, Chicago
Anesthetist-emergency physician-family doctor David Moniz, in an X post, warned of the “unseen consequences” of the No Surprises Act.
Check out the surprising outcomes of the No Surprises Act, designed to protect patients from unexpected medical bills. While it's successfully shielded many patients, there are unseen consequences. Read the full article here: https://t.co/YFa0xweRe7#health, #healthpolicy, #he…
— David Moniz (@DavidMoniz15) February 14, 2024
— David Moniz, Chilliwack, British Columbia
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 3 months ago
Health Care Costs, Health Industry, Insurance, Mental Health, Homeless, Letter To The Editor, Prison Health Care, U.S. Congress
An Arm and a Leg: Wait, Is Insulin Cheaper Now?
Pharmaceutical companies that manufacture insulin made headlines last year when they voluntarily agreed to provide discount cards that lower the monthly cost of insulin for many people to $35.
But getting your hands on this card — and persuading a pharmacist to accept it — can be a hassle.
Pharmaceutical companies that manufacture insulin made headlines last year when they voluntarily agreed to provide discount cards that lower the monthly cost of insulin for many people to $35.
But getting your hands on this card — and persuading a pharmacist to accept it — can be a hassle.
In this episode of “An Arm and a Leg,” producer Emily Pisacreta speaks with “insulin activists” and pharmaceutical experts to find out what this change in prices means for people with diabetes and why the fight for affordable insulin isn’t over yet.
Dan Weissmann
Host and producer of "An Arm and a Leg." Previously, Dan was a staff reporter for Marketplace and Chicago's WBEZ. His work also appears on All Things Considered, Marketplace, the BBC, 99 Percent Invisible, and Reveal, from the Center for Investigative Reporting.
Credits
Emily Pisacreta
Producer
Adam Raymonda
Audio Wizard
Ellen Weiss
Editor
Click to open the Transcript
Transcript: Wait, Is Insulin Cheaper Now?
Note: “An Arm and a Leg” uses speech-recognition software to generate transcripts, which may contain errors. Please use the transcript as a tool but check the corresponding audio before quoting the podcast.
Dan: Hey there. Right after the holidays, I got an email from a listener named Brianna.It started, “Happy new year Dan! I was just reading the news about the price of insulin going down to $35! Is that for everyone?”
And I was like, Huh. I had a sense that there was some news about the price of insulin, but 35 dollars a month for everyone? That sounded like a BIG reduction. And big news.I googled the latest stories, and I was… not totally sure what I was seeing.
I was definitely seeing some new stories about people paying 35 bucks from here on out. And there seemed to be some federal law involved, and politicians were patting themselves on the back. But it just wasn’t totally clear: Was insulin now 35 dollars for everyone? Did the outrageous price of insulin get solved while I wasn’t looking?
And I mean, I’ve kinda been looking. We’ve done a couple of episodes about the price of insulin already — because insulin is iconic. It represents the wild cost of prescription drugs in this country. More than 8 million Americans take insulin to treat their diabetes – and for some, going without it could actually kill you.
And its price got jacked up so much — huge multiples over like ten years — — that one in four of those people who couldn’t go without… took to rationing: Seeing how much they could go without, short of actually dying.
So I asked our senior producer Emily Pisacreta to take the case.
Emily: I feel more like the senior insulin correspondent, which is fine with me as the resident type 1 diabetic! And a lot has happened since the last time we talked about insulin on this show. We really do need an update.
Dan: This is an “Arm and a Leg”, a show about why healthcare costs so freaking much, and what we can maybe do about it. I’m Dan Weissmann, I’m a reporter and I like a challenge. So our job here is to take one of the most enraging, terrifying, depressing parts of American life, and bring you something entertaining, empowering and useful.
Today we have a question: what’s going on with insulin? Is it $35 now?
Emily: Well, there have been some BIG improvements — bigger than I thought when I started reporting. A lot of people can get their monthly supply of insulin for just $35. But it is oversimplified to say it just costs $35 now. And the people who have been fighting to lower the price of insulin over the past decade? They’re still very pissed. So let me walk you through what changed, what led to those changes, and what’s still unresolved.
Dan: OK!
Emily: For years now, there’s been a giant push from people with diabetes to get the federal government to do something about the high cost of insulin. In 2022, finally something came through. I’m talking about a provision in Inflation Reduction Act.
Dan: Yes– I remember this– the Inflation Reduction Act was a big infrastructure bill that included, like renewable energy subsidies, and– honestly, this is the reason that I remember the bill, because we did an episode about this part– letting medicare negotiate some drug prices?
Emily: Exactly. It said people on Medicare would be able to get a month’s supply of insulin for no more than $35 out of pocket. But of course that left a big gaping hole. BECAUSE that’s cool for people on Medicare, but what about the rest of us? And the pharma companies were feeling the heat. Here’s President Biden in his State of the Union last year:
President Biden: Big pharma has been unfairly charging people hundreds of dollars, four to $500 a month making record profits. Not anymore. Not anymore.
Emily: By the way, those pharma companies? There’s three of them who make insulin.
That’s the American company Eli Lilly, the Danish company Novo Nordisk, and the French company Sanofi. OK so: not long after Joe Biden talked about their record profits, the insulin makers were back in the news. …
Eli Lilly was the first to announce they were going to slash prices on several of their most popular insulins, and limit out of pocket spending to $35 a month.
Fox News: This is a big story.
Next, Novo Nordisk and Sanofi made similar announcements.
CNN: Millions of Americans are affected by this major news this morning for millions of people suffering from diabetes and high prescription drug costs.
Basically, the insulin manufacturers all said hey, you’re not covered by this Medicare thing? We’re going to bring your copay down to $35 ourselves. So if you have commercial insurance Print out this card, take it to the pharmacy, and your copay will be no more than $35 for a month’s supply of insulin.
Dan: And what if you’re uninsured?
Emily: Well, they have a card for that, too.
Dan: OK so what I’m hearing is you need a card.
DAN: Yes. How do you get one?
Emily: The insulin makers set special phone numbers you can call. Or you can visit their websites, fill out a little form, and download the card.
Dan: Sounds simple, unless I’m missing something?
Emily: In all honesty, I had no problem with those steps. But I wouldn’t assume that’s the case for everyone. And I’m also not rationing insulin right now.
Zoe Witt: When you are rationing insulin, maybe you aren’t even fully rationing insulin yet, but you don’t know how you’re going to get Your next prescription, your next fill of insulin…You are in crisis. Like, you, you do not have the capability to sift through these websites. It’s very confusing. It’s very overwhelming.
Emily: This is someone who frequently speaks to people struggling to afford insulin.
Zoe Witt: my name is Zoe Witt. I work with Mutual Aid Diabetes.
Emily: Mutual Aid Diabetes. That’s an all volunteer group that has banded together to help diabetics get what they need, when they need it. They help people with cash and with free diabetes supplies, including insulin, no questions asked. That means Zoe knows the ins and outs of every obstacle to getting insulin.
Zoe Witt: Our healthcare system is like a whack a mole from hell.
Emily: And Zoe reminds me: if you’re not taking enough insulin, you probably feel awful. Maybe not even thinking straight. And it can affect your eyes, making it hard to read.
Zoe Witt: It just is unmanageable
Emily: Zoe says they talk with people all the time who are too stressed out or too debilitated to download these cards and use them. Diabetes folks walk people through the process. And once someone has the card… Mutual Aid Diabetes gives people the 35 bucks, too, if they say they need it. Because $35 can be a barrier for a lot of people. And it’s actually $70 sometimes if you use 2 types of insulin at once, which lots of people do… myself included.
Dan: Wow. OK. But then once people have the cards they typically have no problem?
Emily: Well, your pharmacist has to know what they’re doing, too. So sometimes it means a patient having to educate their pharmacist– or even bring the doctor in to help troubleshoot — which is no picnic. And people with diabetes are always having to deal with insurance roadblocks at the pharmacy, so I don’t want to make anything sound simpler than it is.
Dan: It’s like a whack a mole from hell!
Emily: Exactly! And the cards don’t solve everything. Especially this: if you have insurance, these cards only apply to the insulin your insurance plan already covers. If you normally need a prior authorization to get the right insulin for you… that is still the case.
Dan: Right. Okay. like prior authorization is this roadblock to getting all kinds of treatment, that you and your doctor agree that you should have, and your insurance company can say, we disagree. We’re s not authorizing this. And then you’re stuck.
Emily: Right.
Dan:But in terms of what the pharma companies. can do to kind of offer you a deal. They’re basically doing it. Is that right?
Emily: I think that’s fair to say.
Dan: That’s super interesting. All right. So it’s not solved, but this is a big step forward. And what’s not solved is: some people are still on the hook for the list price for insulin — the price without any discounts or insurance or whatever. But you found big improvements there too, right?
Emily: Yes! When the companies announced all these discount cards, they announced a whole other big change, too. Slashing the list prices of a bunch of different insulins by up 75%. So a vial that once was north of $300 is now being listed at around $70.
Dan: OK, that sounds like a big improvement.
Emily: It’s a big, big deal. Actual price reductions are what diabetes advocates have been demanding all along. And… while these are still the highest prices in the world for these same insulins, to see them drop from triple to double digits, it’s wild.
Dan: I sense that there’s a “but” here.
Emily: Well, the Big Three didn’t lower the price of every type of insulin, only ones that have been around since the 1990s or early 2000s. Newer insulins that work faster or last longer are not included here.
Dan: And I’m guessing not all insulins work the same way.
Emily: Right. Some people can switch between types or brands of insulin easily. For other people, there can be allergies or one works better with their body with another kind. It’s complicated. It’s medicine! AND… there have been some issues with pharmacies actually stocking lower list price insulin. That is a whole ‘nother saga… an episode for another day. But the important thing is… a bunch of insulin is a lot cheaper now.
Dan: Wow. Emily, you said right at the top: The changes here are bigger and better than you realized before you started reporting.
Emily: Yes but there’s still a lot more to say.
Right. After the break, we’ll’ hear from you about why these changes happened NOW. And what it means for people with diabetes and really all of us…
[midroll]
So. We have seen some big changes in the last year — including DRUG COMPANIES expanding their discount programs and lowering the sticker prices on insulin, dramatically. Why now? I’m guessing this wasn’t because they had a big change of heart.
Emily: I can’t speak to what’s in pharma’s hearts. But I did talk to someone who knows a lot about pharma’s brain.
Ed Silverman: my name is Ed Silverman, and I work at Stat News, a health and life sciences website,
Emily: I’m a big fan of Stat News
Dan: Me too, man! Their reporting is great.
Emily: And Ed Silverman. He’s been covering the pharmaceutical industry for almost 30 years. He thinks activism from people with diabetes over the years created political pressure that played a big role in the decision to slash prices. But there was also something kind of hidden at work.
Ed Silverman: It’s not altruism, here was a real mechanism, government mechanism in place that helped change the equation and therefore the thinking back at the companies.
Dan: OK… what is he talking about?
Emily: So, Dan: do you remember the stimulus bill, the American Rescue Plan?
Dan: I’m starting to feel like this episode is a quiz on recent-ish legislation. And I think I’m gonna do pretty well here:.The American Rescue Plan was a trillion dollar stimulus that Joe Biden got passed right after he got into office– am I right?
Emily: OK, hotshot. Do you remember how in part 8 section 9816 they sunsetted the limit on the maximum rebate for single source drugs and innovator multiple source drugs?
Dan: Um, busted. No.
Emily: Ok so here’s the deal: it’s obviously kinda wonky so I’ll simplify– in that little section Congress made a tweak to Medicaid, basically raising penalties on drug-makers for jacking up prices too far, too fast. So if you’re a pharma company who has raised the price of a drug by a lot very quickly, which is true of insulin, and a lot of people on Medicaid use your drug, which is also true of insulin, then you have to pay a big penalty. In the case of insulin, that penalty would be more than you’d make selling the insulin to Medicaid. A LOT more: So, unless you bring the price back down, you’re going to owe Medicaid a lot of moolah. And those penalties were set to kick in January 1st 2024.
Dan: So you’re telling me: Part of what the pharma companies did here came right out of a small part of a giant federal law from 2021.
Emily: Yep. And there’s another big wheel turning in the background here. Novo Nordisk and Eli Lilly, two companies who really got their start by selling insulin, now make other diabetes drugs — drugs that are now increasingly used for weight loss. And it’s a bonanza.
GMA: It is literally the hottest drug in the country right now.
Fox News: all people are talking about these days is Ozempic, wegovy. Oh my gosh, this person lost 20 pounds. This person lost 50 pounds.
Ozempic Ad: [Jingle:] “Oh, Oh, Oh, Ozempic![Announcer:] Once weekly Ozempic is helping many people with type 2 diabetes like James lower their blood sugar.
Emily: Drugs like Ozempic, Wegovy, Mounjaro. They’ve been in super high demand. And there’s been a ton of hype about their various potential health benefits. For weight loss, for heart health. Scientists are even interested in whether it can help people with substance use disorders. Meanwhile, for Eli Lilly and Novo Nordisk, the returns on these drugs dwarf anything else they’re selling. Novo Nordisk even became the biggest company in Europe – for like a minute… but still.
Dan: OK, this is interesting, but what does it have to do with the price of insulin?
Emily: I’d wondered… maybe these companies can just better afford to buy some political peace by lowering insulin prices, because they are making so much bank on these new drugs, ? Ed Silverman had a take on that.
Ed Silverman: It makes perfect sense that these cash cows, these medicines that are used for diabetes and, weight loss are going to become increasingly important to their bottom line more than other medicines
Emily: More than insulin. And they’re selling so much so fast, they can hardly keep up with demand. Which could end up affecting people who need insulin.
Dan: Wait, how?
Emily: Look, for example, in November, Novo Nordisk said they were investing 3 and half billion dollars into ramping up production of injection pens for Wegovy, one of their top drugs in this category. Less than a week later, Novo announced they would be phasing out one of their insulin products from the US market – an insulin called Levemir. It’s one of the insulins whose prices they just dropped. And… coincidence… Levemir also comes in a pen.
Dan: So Novo Nordisk is phasing out an insulin pen so they can make more Wegovy pens?
Emily: Well, we don’t know that for sure. But Novo Nordisk did tell me that “manufacturing constraints” were part of why they’re dumping Levimir. They said it was one of several reasons and also wrote: “We made this decision after careful consideration and are confident that given the advanced notice, U.S. patients will have access to alternative treatments and can transition to other options.
Dan: Huh. OK.
Emily: But even if pulling this insulin Levemir off the market had nothing to do with their trouble meeting the demand for their big blockbuster drug… it brings to mind an important question about all the changes we talked about today — whether it’s the copay savings or the lowered list prices. Here’s Ed Silverman.
Ed Silverman there’s no guarantee that the companies will keep these in place. Maybe after time, some of the attention on insulin is diverted and maybe eighteen months from now, one company might quietly roll back some of the Benefits, if you want to use that word, there’s nothing requiring them to maintain the steps they’ve taken.
Emily: I asked all three insulin makers about this. None of them promised there would never be any backsies. Lilly wrote back “Lilly is committed to ensuring all patients can access any Lilly medicine they need” — and touted their efforts to date. Similarly, Sanofi wrote “We continually review our affordability offerings to support our aim that no one should struggle to pay for their insulin. Novo Nordisk’s response was “Novo Nordisk increases the price of some of our medicines each year, in response to changes in the healthcare system, market conditions, and the impact of inflation.”
Dan: Yeah, that especially does not sound like a pinky-swear, no-backsies kind of response.
Emily: AND that’s not much comfort for insulin activists. Folks like Shaina Kasper, who works for T1International. They’re a group that’s been at the forefront of this fight for years. I Asked her…
Emily-on-tape: So is this issue of high insulin prices just resolved now?
Shaina Kasper: No, it hasn’t been. It’s been really frustrating…
Emily Shaina and others are worried that the announcements from the manufacturers about savings cards and voluntary list price reductions will take the pressure off the government to do something more sweeping. Because for now…
Shaina: The manufacturers really hold all of the power here And if patients are counting on these programs to literally be able to survive, that has life and death consequences
Dan: This question about who holds the power, it reminds me of a story we did a few months ago… the one about how the writer John Green led a kind of online crusade targeting the drug-maker Johnson & Johnson. And how, even though the pressure campaign worked — J & J ended up allowing lower-priced versions of an important tuberculosis drug — activists who worked on the issue were like: It’s a problem that Johnson & Johnson has the power to say yes or no here..
Emily: Exactly. That which pharma giveth, pharma can taketh. At least the way things are set up now. Now I should say, all three companies told me they plan to continue their affordability offerings. But if insulin continues to be the poster child for high drug prices, prices virtually everyone in America agrees are too high…it does raise the question: are voluntary programs from pharmaceutical companies the solution we want? To Zoe from Mutual Aid Diabetes, the answer is no. They find these manufacturer savings cards kind of a bitter pill… no pun intended.
Zoe Witt: there’s certainly no justice in these programs,
Emily: And zoe for one would say that justice is overdue.
Zoe Witt: These companies have price gouged us. for years, making obscene amounts of money. Then, presumably, as, we’re often told is the justification for these ridiculous prices, they did research and development for more diabetes drugs, which are Ozempic, Monjoro, etc. And now, these companies, for, the next 15 years, are set to make, billions and billions of dollars, on these drugs,
Emily: I asked the big three insulin manufacturers about what Zoe said – about how angry folks like them are over the cost of insulin. Novo Nordisk said “we continually review and revise our offerings as well as work with diverse stakeholders to create solutions for differing patient needs. ” And Sanofi and Lily both said something very similar.
Emily: So… in the end– or at least for now– here’s the answer to our listener’s question…. There are more avenues than ever to get a month’s supply of insulin for $35. Great. It may be a lot easier to avoid rationing your insulin now than it was a couple years ago. That’s also really great. But people with diabetes do not think this fight is over.
Dan: So what DO they want?
Emily: Some people still want the federal government to just put a cap on what people pay for insulin, like by law.. Others are working to build alternatives to the existing pharmaceutical industry, like California’s CalRx program.
Dan: Cal Rx… now you’re calling back our story from the last time we talked about insulin.
Emily: Yep, Cal Rx is the state of California’s attempt to enter the insulin market, to introduce some low priced generics and sell them essentially at cost. Other states are joining in. Even if some of these specific plans fall apart — even if California somehow can’t get its government-sponsored insulin to market, even if Pharma rolls back some of the discounts…the past few years have been enormous for people with diabetes. Mostly because they’ve found each other.
Zoe Witt: I was rationing insulin in 2018, I didn’t even know that there was a term for it. I didn’t know other people were doing it. I know a lot of people died that year. And there were multiple occasions where I, in retrospect, definitely almost died. And the one good thing that has, that has happened between now and then is that people have been talking about it and People are now more comfortable telling others that they’re struggling, that they can’t get their insulin.
Emily: Connecting with Mutual Aid Diabetes or other networks to get or give help.
Zoe Witt: We’re all keeping each other alive, like to me, that’s the number one thing that has changed.
Emily: I think that’s a huge lesson here, and a takeaway that’s not new on this show. Keeping each other alive — or even just keeping each other from getting bankrupted by the medical system — is up to us. And while a mutual aid group modeled exactly like Mutual Aid Diabetes may not work for every disease or every drug, Zoe says they’re more than willing to talk to anyone who might be interested in trying.
Zoe Witt: I mean, we’ve even had people ask, like, is there like a mutual aid asthma or something like for inhalers?
Emily: Their advice?
Zoe Witt: I think that, you know, to start, you would want, like, probably at least, like, five to ten ”ride-or dies,” like, people that are really willing to, like, go the extra mile,
Dan: Five to ten– that just does not sound like that many! (I mean, I think.) One thing I’m taking away is: This is a lot of activism over a long time, that eventually had a big effect. Another thing I’m taking away here? Sneaky policy changes — like lifting the Medicaid rebate cap — can make a huge difference. God bless whatever nerds are writing the next little bit of law to sneak into a giant bill, like a hacker with a virus.
Emily: Totally. OK. I gotta take a shot, and eat my lunch.
Dan: Go for it. We’ll be back with a new episode in a few weeks. Till then, take care of yourself.
This episode of an arm and a leg was produced by Emily Pisacreta and me, Dan Weissman and edited by Ellen Weiss.
Adam Raymonda is our audio wizard. Our music is by Dave Weiner and blue dot sessions.
Gabrielle Healy is our managing editor for audience. She edits the first aid kit newsletter.
Bea Bosco is our consulting director of operations. Sarah Ballama is our operations manager.
And Arm and a Leg is produced in partnership with KFF Health News. That’s a national newsroom producing in depth journalism about healthcare in America and a core program at KFF, an independent source of health policy research, polling and journalism.
Zach Dyer is senior audio producer at KFF Health News. He’s editorial liaison to this show.
And thanks to the Institute for Nonprofit News for serving as our fiscal sponsor, allowing us to accept tax exempt donations. You can learn more about INN at INN. org.
Finally, thanks to everybody who supports this show financially– you can join in any time at arm and a leg show dot com, slash, support — and thanks for listening.
“An Arm and a Leg” is a co-production of KFF Health News and Public Road Productions.
To keep in touch with “An Arm and a Leg,” subscribe to the newsletter. You can also follow the show on Facebook and X, formerly known as Twitter. And if you’ve got stories to tell about the health care system, the producers would love to hear from you.
To hear all KFF Health News podcasts, click here.
And subscribe to “An Arm and a Leg” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 3 months ago
Health Care Costs, Multimedia, Pharmaceuticals, An Arm and a Leg, Chronic Disease Care, diabetes, Drug Costs, Podcasts