Even Grave Errors at Rehab Hospitals Go Unpenalized and Undisclosed
Rehab hospitals that help people recover from major surgeries and injuries have become a highly lucrative slice of the health care business.
But federal data and inspection reports show that some run by the dominant company, Encompass Health Corp., and other for-profit corporations have had rare but serious incidents of patient harm and perform below average on two key safety measures tracked by Medicare.
Yet even when inspections reveal grave cases of injury, federal health officials do not inform consumers or impose fines the way they do for nursing homes. And Medicare doesn’t provide easy-to-understand five-star ratings as it does for general hospitals.
In the most serious problems documented by regulators, rehab hospital errors involved patient deaths.
In Encompass Health’s hospital in Huntington, West Virginia, Elizabeth VanBibber, 73, was fatally poisoned by a carbon monoxide leak during construction at the facility.
At its hospital in Jackson, Tennessee, a patient, 68, was found dead overnight, lying on the floor in a “pool of blood” after an alarm that was supposed to alert nurses that he had gotten out of bed had been turned off.
In its hospital in Sioux Falls, South Dakota, a nurse gave Frederick Roufs, 73, the wrong drug, one of 26 medication errors the hospital made over six months. He died two days later at another hospital.
“I can still see Fred laying in the bed as they shut each little machine off,” said his widow, Susan Roufs. “They clicked four of them, and then the love of my life was gone.”
Encompass, which owns 168 hospitals and admitted 248,000 patients last year, has led the transformation of this niche industry. In 2023, stand-alone for-profit medical rehabilitation hospitals overtook nonprofits as the places where the majority of annual patient admissions occur, a KFF Health News and New York Times analysis found. A third of all admissions were to Encompass hospitals. Such facilities are required to provide three hours of therapy a day, five days a week.
Across the nation, there are now nearly 400 stand-alone rehab hospitals, the bulk of which are for-profit. These hospitals collectively generate profits of 10%, more than general hospitals, which earn about 6%, and far more than skilled nursing homes, which make less than 0.5%, according to the most recent data from the Medicare Payment Advisory Commission, an independent congressional agency.
At the same time, the number of small, specialized units within acute care hospitals — where most rehab used to be provided — has dwindled. There are now around 800 of those, and most are nonprofits.
In its latest annual report, Encompass, which is publicly traded, reported an 11% net profit in 2024, earning $597 million last year on revenues of $5.4 billion.
Federal data on the performance of about 1,100 of the rehab facilities show Encompass tends to be better at helping most patients return home and remain there. In a two-year period ending in September 2023, Medicare rated 233 rehab facilities as performing better than the national rate for this major metric, called “discharge to community.” Most rehabs with better community discharge rates are for-profit, and Encompass owns 79 of them.
But data from Medicare also reveals Encompass owns many of the rehabs with worse rates of potentially preventable, unplanned readmissions to general hospitals. Medicare evaluates how often patients are rehospitalized for conditions that might have been averted with proper care, including infections, bedsores, dehydration, and kidney failures.
Encompass accounts for about 1 in 7 rehab facilities nationally, but owned 34 of the 41 inpatient rehab facilities that Medicare rated as having statistically significantly worse rates of potentially preventable readmissions for discharged patients. (Overall, rates of readmission after discharge ranged from 7% to 12%, with a median of 9%.)
And it owned 28 of the 87 rehab facilities — 65 of which were for-profit — that had worse rates of potentially preventable readmissions to general hospitals during patient stays. (The median for these kinds of readmissions was 5%, and rates for individual rehabs ranged from 3% to 9%.)
Patrick Darby, the executive vice president and general counsel of Encompass, strongly defended the company’s record in written responses to questions. He dismissed Medicare’s readmissions ratings of “better,” “worse,” and “no different than the national rate” as “a crude scoring measure” and said “performance is so similar across the board.” He called the violations found during health inspections “rare occurrences” that “do not support an inference of widespread quality concerns.”
“The simplest and most accurate reason for EHC’s success is that our hospitals provide superior care to patients,” he said, referring to Encompass by its corporate initials.
Chih-Ying Li, an associate professor of occupational therapy at the University of Texas Medical Branch at Galveston School of Health Professions, said in an interview that a research study she conducted found the profit status of a rehab facility was the only characteristic associated with higher unplanned readmissions.
“The finding is pretty robust,” she said. “It’s not like huge, huge differences, but there are differences.”
VanBibber was admitted to Encompass’ Huntington hospital in 2021 for therapy to strengthen her lungs. At the time, the hospital was undergoing a $3 million expansion, and state regulators had warned the company that areas of the hospital occupied by patients had to be isolated from the construction “using airtight barriers,” according to a health inspection report.
In her room, which was about 66 feet from the construction zone, she began having trouble breathing, the report said. When she told the staff, they ignored her and shut her door, according to a lawsuit brought by her estate. Staff members eventually noticed that she was “lethargic and gasping for air,” and called 911.
When the emergency medical squad arrived, the carbon monoxide detectors they wore sounded. By that time, VanBibber’s blood oxygen levels were dangerously low, the inspection report said. She died three days later from respiratory failure and carbon monoxide poisoning, according to the inspection report and the lawsuit. A plumber had been using a gas-powered saw in the construction area, but there were no carbon monoxide detectors in the hallways, the report said.
In court papers, Encompass and its construction contractors denied negligence for VanBibber’s death. The case is pending.
Inspectors determined Encompass failed to maintain a safe environment for all patients during construction and didn’t properly evaluate other patients for signs of poisoning, the report said.
Since 2021, the federal Centers for Medicare and Medicaid Services, or CMS, which oversees health inspections, has found that 10 Encompass hospitals, including the one that cared for VanBibber, had immediate jeopardy violations, federal records show. Such violations — like the ones that Medicare also found in connection with the deaths of Roufs and the patient who fell after leaving his bed — mean a hospital’s failure to comply with federal rules has put patients at risk for serious injury, serious harm, serious impairment, or death.
Darby, the general counsel for Encompass, said the company regretted any clinical problems and had promptly addressed all such findings to the satisfaction of inspectors. He said Encompass that has an “excellent compliance record,” including superior results from its accreditation agency, and that its overall number of health citations was tiny given how many hospitals Encompass owns and how many patients it treats.
Six other corporate-operated for-profit hospitals were also cited, while none of the 31 stand-alone nonprofit rehab hospitals received such violations from 2021 to 2024. (Inspection reports for general hospitals do not systematically specify in which part of the building a violation occurred, so rehab unit violations cannot be identified.)
An alert called a bed alarm was at the root of immediate jeopardies at Encompass hospitals in Morgantown, West Virginia, and Jackson, Tennessee. The devices are pressure- and motion-sensitive and emit a sound and display a light to alert staff members that someone at a high risk of falls has left his or her bed.
In its Morgantown hospital, a nurse technician discovered a patient face down on the floor with a large gash on her head after a defective alarm did not go off, an inspection report said. After she died, the nurse told inspectors: “We are having a lot of problems with the bed alarms.”
Medicare is not authorized by law to fine rehab hospitals for safety rule violations, even ones involving deaths uncovered during inspections, as it has done with nearly 8,000 nursing homes during the last three years, imposing average fines of about $28,000.
The only option is to entirely cut off a rehab hospital’s reimbursement for all services by Medicare and Medicaid, which cover most patients. That step would most likely put it out of business and is almost never used because of its draconian consequences.
“Termination is typically a last resort after working with the provider to come back into compliance,” Catherine Howden, a CMS spokesperson, said in an email.
As a result, because there’s no graduated penalty, even the most serious — and rare — immediate jeopardy violations effectively carry no punishments so long as the hospital puts steps in place to avert future problems.
“Only having a nuclear weapon has really hurt patient safety,” said Michael Millenson, a medical quality advocate.
One immediate jeopardy incident did result in a punishment, but only because the hospital was in California, which allows its health department to issue penalties. Encompass’ Bakersfield hospital paid a $75,000 fine last year for failing to control the blood sugar of a patient who died after her heart stopped.
Rapid Growth and a Troubled History
Encompass has accelerated its expansion in recent years and now operates in 38 states and Puerto Rico. It plans to open 17 more hospitals in Arizona, Connecticut, Florida, Georgia, Maine, Pennsylvania, South Carolina, Texas, and Utah by the end of 2027, according to its latest report.
It frequently moves into new markets by persuading local nonprofit hospitals to shutter their rehab units in exchange for an equity stake in a newly built Encompass hospital, company executives have told investors.
The president of Encompass, Mark Tarr, calls it a “win-win proposition”: The local hospitals can use their emptied space for a more lucrative line of service and Encompass gets a “jump start” into a new market, with partner hospitals often referring patients.
Tarr, who was paid $9.3 million in compensation last year, told investors that Encompass requires that the existing hospitals sign a noncompete deal. Sixty-seven Encompass hospitals are joint ventures, mostly with nonprofit hospitals as investors, according to the company’s June financial filing, the most recent available.
Darby said the company’s profits allow it to build hospitals in areas that lack intensive inpatient rehabilitation and improve existing hospitals. “High-quality patient care is not only consistent with shareholder return, but quality and shareholder return are in fact critical to one another,” he said.
The success of Encompass is particularly notable given that it barely survived what experts said was one of the largest modern accounting scandals in 2003.
The Securities and Exchange Commission charged that the company, then known as HealthSouth, overstated earnings by $2.7 billion to meet Wall Street analyst quarterly expectations, leading to the ouster of its founder and directors. In 2004, the company agreed to pay the government $325 million to settle Medicare fraud allegations without admitting wrongdoing. Darby credited the company’s new leaders for obtaining a $2.9 billion judgment on behalf of shareholders against the company’s founder.
The company changed its name to Encompass in 2018 after acquiring Encompass Home Health and Hospice. In 2019, the Justice Department announced the company had agreed to pay $48 million to settle whistleblower lawsuit claims that it misdiagnosed patients to get higher Medicare reimbursements, and admitted patients who were too sick to benefit from therapy. The company denied any wrongdoing, blaming independent physicians who worked at its hospitals. Darby said Encompass settled the case only to “avoid more years of expense and disruption.” He said the Justice Department never filed a lawsuit despite years of investigation.
Medication Harms
Rehab hospital inspection reports are not posted on Care Compare, Medicare’s online search tool for consumers. KFF Health News had to sue CMS under the Freedom of Information Act to obtain all its inspection reports for rehab hospitals. In contrast, Care Compare publishes all nursing home inspection reports and assigns each facility a star rating for its adherence to health and safety rules.
So people now choosing a rehab hospital would not know that at the Encompass hospital in Sioux Falls, South Dakota, in 2021, a nurse accidentally gave Roufs a blood pressure drug called hydralazine instead of hydroxyzine, his prescribed anti-anxiety medication, according to an inspection report. Roufs went into cardiac arrest. This type of error, called a “look-alike/sound-alike,” is one hospitals and staff members are supposed to be especially alert to.
Months before, an internal safety committee had identified a trend of medication errors, including when a nurse accidentally gave a patient 10 times the prescribed amount of insulin, sending him to the hospital, the inspection report said. The nurse had misread four units as 40. Since Roufs’s death, inspectors have faulted the hospital six times for various lapses, most recently in April 2024 for improper wound care.
An Encompass hospital in Texarkana, Texas, misused antipsychotic medications to pacify patients, resulting in an immediate jeopardy finding from CMS, the report said. And the company’s hospital in Erie, Pennsylvania, was issued an immediate jeopardy violation for not keeping track of medication orders in 2023, when a patient had a cardiac arrest after not receiving all of his drugs, according to the inspection report.
The federal government’s overall quality oversight efforts are limited. Medicare docks payment to rehab facilities for patients readmitted to a general hospital during shorter-than-average rehab stays, but unlike at general hospitals, there are no financial penalties when recently discharged rehab patients are hospitalized for critical health issues.
The Biden administration announced last year it intended to develop a rating scale of 1 to 5 stars for rehab facilities. The industry’s trade association, the American Medical Rehabilitation Providers Association, requested a delay in the creation of star ratings until the current quality measures were refined. The Trump administration has not determined whether it will continue the effort to rate rehab facilities, according to a CMS spokesperson.
Deadly Bedsores
The family of Paul Webb Jr., 74, claimed in a lawsuit that the Encompass hospital in Erie left Webb unattended in a wheelchair for hours at a time, putting pressure on his tailbone, in 2021. His medical records, provided to reporters by the family, list a sitting tolerance of one hour.
Webb — who had been originally hospitalized after a brain bleed, a type of stroke — developed skin damage known as a pressure sore, or bedsore, on his bottom, the lawsuit said. The suit said the sore worsened after he was sent to a nursing home, which the family is also suing, then home, and he died later that year. In his final weeks, Webb was unable to stand, sit, or move much because of the injury, the lawsuit said.
In court papers, Encompass and the nursing home denied negligence, as Encompass has in some other pending and closed lawsuits that accused it of failing to prevent pressure sores because nurses and aides failed to regularly reposition patients, or notice and treat emerging sores. Darby said Webb’s death occurred three months after his Encompass stay and was not related to his care at Encompass. He said no hospital with long-term patients could prevent every new or worsening pressure sore, but that Encompass’ rates were similar to the 1% national average.
One of Webb’s sons, Darel Webb, recalled a warning given to the family as they left an appointment their father had with wound specialists: A doctor brought up Christopher Reeve, the actor who played Superman in movies in the 1970s and 1980s.
“He goes, ‘Remember, Superman was paralyzed from falling off the horse, but he died from a bedsore,’” he said.
Jordan Rau has been writing about hospital safety since 2008. Irena Hwang is a New York Times data reporter who uses computational tools to uncover hidden stories and illuminate the news.
METHODOLOGY
To examine the medical rehabilitation hospital industry, we obtained and analyzed a database of inspection reports of freestanding rehabilitation hospitals from the federal Centers for Medicare & Medicaid Services, or CMS. We also obtained inspection reports from several states through public records requests.
We analyzed inpatient rehabilitation facility characteristics and patient volume data contained in hospital data files from the Rand Corp., a nonprofit research organization. This dataset compiles cost reports all hospitals submit each year to CMS. For each facility for the years 2012 to 2023, we categorized annual discharges by facility type (freestanding rehabilitation hospital or unit within an acute care hospital); facility ownership status (for-profit, nonprofit, or government); and which hospitals were owned by Encompass Health under its current or prior name, HealthSouth.
Financial information about Encompass Health was obtained from the company’s Securities and Exchange Commission disclosure filings.
We examined the readmission rates for all inpatient rehabilitation facilities that CMS publishes in its quality data. CMS evaluates the frequency with which Medicare patients were readmitted for potentially preventable reasons to an acute care hospital during their rehab stay. Separately, CMS also evaluates the frequency of potentially preventable readmissions to an acute care hospital within 30 days of discharge from rehab. We also examined the rate of successful return to home or community. Figures for all three metrics were available for about 1,100 of the roughly 1,200 rehab facilities in the CMS data. The most recent readmission data covered Medicare discharges from October 2021 through September 2023.
We examined nursing home penalties from the last three years from CMS’ data on nursing homes.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 week 2 days ago
Health Industry, Insurance, Medicare, Multimedia, Arizona, california, CMS, Connecticut, Florida, Georgia, Hospitals, Investigation, Maine, New York, Pennsylvania, South Carolina, South Dakota, Tennessee, texas, Utah, West Virginia
As Mosquito Season Peaks, Officials Brace for New Normal of Dengue Cases
As summer ushers in peak mosquito season, health and vector control officials are bracing for the possibility of another year of historic rates of dengue.
As summer ushers in peak mosquito season, health and vector control officials are bracing for the possibility of another year of historic rates of dengue. And with climate change, the lack of an effective vaccine, and federal research cuts, they worry the disease will become endemic to a larger swath of North America.
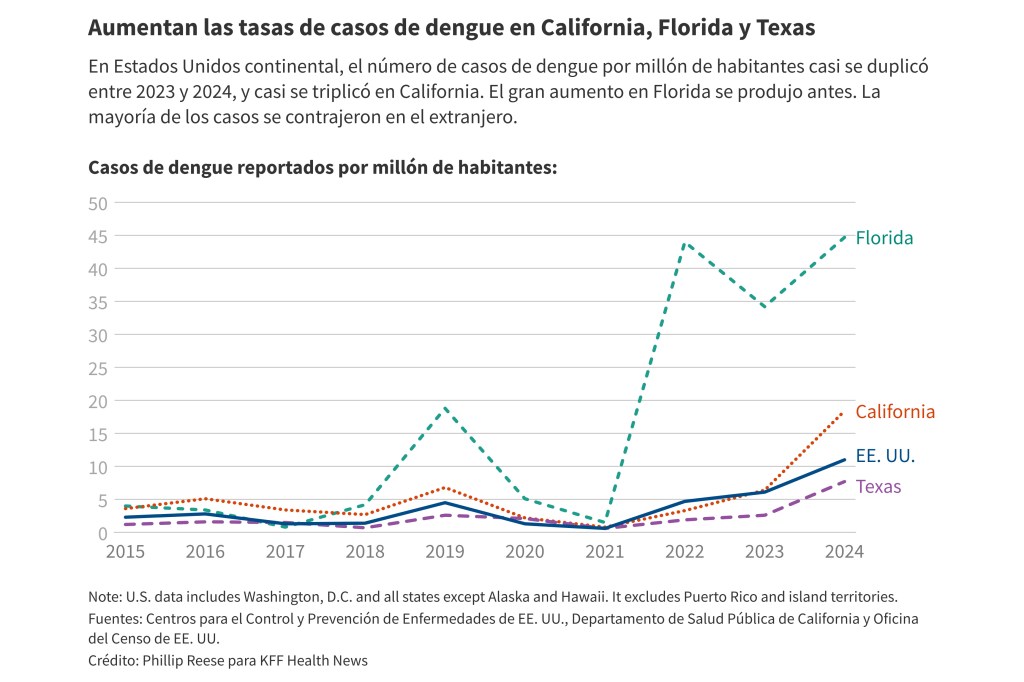
About 3,700 new dengue infections were reported last year in the contiguous United States, up from about 2,050 in 2023, according to the Centers for Disease Control and Prevention. All of last year’s cases were acquired abroad, except for 105 cases contracted in California, Florida, or Texas. The CDC issued a health alert in March warning of the ongoing risk of dengue infection.
“I think dengue is here with us to stay,” said infectious disease specialist Michael Ben-Aderet, associate medical director of hospital epidemiology at Cedars-Sinai in Los Angeles, about dengue becoming a new normal in the U.S. “These mosquitoes aren't going anywhere.”
Dengue is endemic — a label health officials assign when diseases appear consistently in a region — in many warmer parts of the world, including Latin America, India, and Southeast Asia. Dengue cases increased markedly last year in many of those places, especially in Central and South America.
The disease, which can spread when people are bitten by infected Aedes mosquitoes, was not common in the contiguous United States for much of the last century. Today, most locally acquired (meaning unrelated to travel) dengue cases in the U.S. happen in Puerto Rico, which saw a sharp increase in 2024, triggering a local public health emergency.
Most people who contract dengue don’t get sick. But in some people symptoms are severe: bleeding from the nose or mouth, intense stomach pain, vomiting, and swelling. Occasionally, dengue causes death.
California offers a case study in how dengue is spreading in the U.S. The Aedes aegypti and Aedes albopictus mosquitoes that transmit dengue weren’t known to be in the state 25 years ago. They are now found in 25 counties and more than 400 cities and unincorporated communities, mostly in Southern California and the Central Valley.
The spread of the mosquitoes is concerning because their presence increases the likelihood of disease transmission, said Steve Abshier, president of the Mosquito and Vector Control Association of California.
From 2016 through 2022, there were an average of 136 new dengue cases a year in California, each case most likely brought to the state by someone who had traveled and been infected elsewhere. In 2023, there were about 250 new cases, including two acquired locally.
In 2024, California saw 725 new dengue cases, including 18 acquired locally, state data shows.
Climate change could contribute to growth in the Aedes mosquitoes’ population, Ben-Aderet said. These mosquitoes survive best in warm urban areas, often biting during the daytime. Locally acquired infections often occur when someone catches dengue during travel, then comes home and is bitten by an Aedes mosquito that bites and infects another person.
“They've just been spreading like wildfire throughout California,” Ben-Aderet said.
Dengue presents a challenge to the many primary care doctors who have never seen it. Ben-Aderet said doctors who suspect dengue should obtain a detailed travel history from their patients, but confirming the diagnosis is not always quick.
“There's no easy test for it,” he said. “The only test that we have for dengue is antibody tests.” He added that “most labs probably aren't doing it commercially, so it's usually like a send-out test from most labs. So you really have to suspect someone has dengue.”
Best practices for avoiding dengue include eliminating any standing pools of water on a property — even small pools — and using mosquito repellent, Abshier said. Limiting activity at dusk and dawn, when mosquitoes bite most often, can also help.
Efforts to combat dengue in California became even more complicated this year after wildfires ripped through Los Angeles. The fires occurred in a hot spot for mosquito-borne illnesses. San Gabriel Valley Mosquito and Vector Control District officials have worked for months to treat more than 1,400 unmaintained swimming pools left in the wake of fire, removing potential breeding grounds for mosquitoes.
San Gabriel vector control officials have used local and state resources to treat the pools, said district spokesperson Anais Medina Diaz. They have applied for reimbursement from the Federal Emergency Management Agency, which has not historically paid for vector control efforts following wildfires.
In California, vector control agencies are often primarily funded by local taxes and fees on property owners.
Some officials are pursuing the novel method of releasing sterilized Aedes mosquitoes to reduce the problem. That may prove effective, but deploying the method in a large number of areas would be costly and would require a massive effort at the state level, Abshier said. Meanwhile, the federal government is pulling back on interventions: Several outlets have reported that the National Institutes of Health will stop funding new climate change-related research, which could include work on dengue.
This year, reported rates of dengue in much of the Americas have declined significantly from 2024. But the trend in the United States likely won’t be clear until later in the year, after the summer mosquito season ends.
Health and vector control researchers aren't sure how bad it will get in California. Some say there may be limited outbreaks, while others predict dengue could get much worse. Sujan Shresta, a professor and infectious disease researcher at the La Jolla Institute for Immunology, said other places, like Nepal, experienced relatively few cases of dengue in the recent past but now regularly see large outbreaks.
There is a vaccine for children, but it faces discontinuation from a lack of global demand. Two other dengue vaccines are unavailable in the United States. Shresta’s lab is hard at work on an effective, safe vaccine for dengue. She hopes to release results from animal testing in a year or so; if the results are positive, human trials could be possible in about two years.
“If there's no good vaccine, no good antivirals, this will be a dengue-endemic country,” she said.
Phillip Reese is a data reporting specialist and an associate professor of journalism at California State University-Sacramento.
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
3 weeks 1 day ago
california, Multimedia, Public Health, States, Environmental Health, Florida, texas
Con el verano hay más mosquitos y, temen oficiales, más casos de dengue
Con el verano marcando el comienzo de la temporada alta de mosquitos, autoridades sanitarias y de control de vectores se preparan para la posibilidad de otro año con tasas históricas de dengue.
Con el verano marcando el comienzo de la temporada alta de mosquitos, autoridades sanitarias y de control de vectores se preparan para la posibilidad de otro año con tasas históricas de dengue. Y con el cambio climático, la falta de una vacuna eficaz y los recortes federales en la investigación, les preocupa que la enfermedad se vuelva endémica en una franja más amplia de Norteamérica.
El año pasado se reportaron alrededor de 3.700 nuevas infecciones por dengue en Estados Unidos, frente a las 2.050 de 2023, según los Centros para el Control y Prevención de Enfermedades (CDC). Todos los casos de 2024 se adquirieron en el extranjero, excepto 105 contraídos en California, Florida o Texas. Los CDC emitieron una alerta sanitaria en marzo advirtiendo sobre el riesgo continuo de infección por dengue.
"Creo que el dengue ha llegado para quedarse", declaró Michael Ben-Aderet, especialista en enfermedades infecciosas y director médico asociado de epidemiología hospitalaria del Cedars-Sinai de Los Ángeles, sobre la posibilidad de que el dengue se convierta en la nueva normalidad en el país. "Estos mosquitos no se irán a ninguna parte".
El dengue es endémico —una etiqueta que las autoridades de salud pública asignan cuando las enfermedades aparecen de forma constante en una región— en muchas zonas más cálidas del mundo, como Latinoamérica, India y el sudeste asiático. Los casos de dengue aumentaron notablemente el año pasado en muchos de esos lugares, especialmente en Centro y Sur América.
La enfermedad, que puede propagarse por la picadura de mosquitos Aedes que portan el virus, no fue común en Estados Unidos continental durante gran parte del siglo pasado. Actualmente, la mayoría de los casos de dengue adquiridos localmente (es decir, no relacionados con viajes) en el país se registran en Puerto Rico, donde se registró un fuerte aumento en 2024, lo que desencadenó una emergencia de salud pública local.
La mayoría de las personas que desarrollan dengue no se enferman. Sin embargo, en algunas, los síntomas son graves: sangrado por la nariz o la boca, dolor de estómago intenso, vómitos e hinchazón. En ocasiones, el dengue causa la muerte.
California ofrece un caso centinela sobre la propagación del dengue en el país. Hace 25 años, no se conocía la presencia de los mosquitos Aedes aegypti y Aedes albopictus, que transmiten el dengue, en el estado. Actualmente, se encuentran en 25 condados y más de 400 ciudades y comunidades no incorporadas, principalmente en el sur de California y en el Valle Central.
La propagación de los mosquitos es preocupante porque su presencia aumenta la probabilidad de transmisión de enfermedades, afirmó Steve Abshier, presidente de la Mosquito and Vector Control Association of California.
Entre 2016 y 2022, se registró un promedio de 136 nuevos casos de dengue al año en California, cada uno de los cuales probablemente traído al estado por alguien que viajó y se infectó en otro lugar. En 2023, se registraron alrededor de 250 casos nuevos, incluyendo dos adquiridos localmente.
En 2024, California registró 725 nuevos casos de dengue, incluyendo 18 adquiridos localmente, según datos estatales.
El cambio climático podría contribuir al aumento de la población de mosquitos Aedes, afirmó Ben-Aderet. Estos mosquitos sobreviven mejor en zonas urbanas cálidas, y suelen picar durante el día. Las infecciones de transmisión local suelen ocurrir cuando alguien contrae dengue durante un viaje, regresa a casa y lo pica un mosquito Aedes que, a su vez, pica e infecta a otra persona.
"Se han propagado rápidamente por toda California", explicó Ben-Aderet.
El dengue representa un desafío para muchos médicos de atención primaria que nunca lo han visto. Ben-Aderet dijo que los médicos que sospechan dengue deben obtener un historial de viaje detallado de sus pacientes, pero confirmar el diagnóstico no siempre es rápido.
"No existe una prueba sencilla para detectarlo", afirmó. "La única prueba que tenemos para el dengue son las pruebas de anticuerpos". Agregó que "la mayoría de los laboratorios probablemente no lo estén comercializando, por lo que suele ser una prueba que se debe analizar en otra instalación. Por lo tanto, es fundamental sospechar que alguien tiene dengue".
Las mejores prácticas para evitar el dengue incluyen eliminar cualquier agua estancada en una propiedad, aunque sea poca, y usar repelente de mosquitos, dijo Abshier. Limitar la actividad al atardecer y al amanecer, cuando los mosquitos pican con mayor frecuencia, también puede ayudar.
Los esfuerzos para combatir el dengue en California se complicaron aún más este año después de que los incendios forestales arrasaran Los Ángeles.
Los incendios ocurrieron en una zona de alta incidencia de enfermedades transmitidas por mosquitos. Funcionarios del San Gabriel Valley Mosquito and Vector Control District han trabajado durante meses para tratar más de 1.400 piscinas sin mantenimiento que quedaron tras el incendio, eliminando así posibles criaderos de mosquitos.
Estos oficiales han utilizado recursos locales y estatales para tratar las piscinas, dijo Anais Medina Díaz, vocera del distrito. Han solicitado un reembolso a la Agencia Federal para el Manejo de Emergencias (FEMA), que históricamente no ha financiado las iniciativas de control de vectores luego de incendios forestales.
En California, las agencias de control de vectores suelen financiarse principalmente con impuestos y tasas locales que pagan los propietarios.
Algunos funcionarios están implementando el novedoso método de liberar mosquitos Aedes esterilizados para reducir el problema. Eso puede resultar eficaz, pero implementar el método en un gran número de áreas sería costoso y requeriría un esfuerzo masivo a nivel estatal, dijo Abshier.
Mientras tanto, el gobierno federal está reduciendo sus intervenciones: varios medios han informado que los Institutos Nacionales de Salud dejarán de financiar nuevas investigaciones relacionadas con el cambio climático, que podrían incluir trabajos sobre el dengue.
Este año, las tasas de dengue reportadas en gran parte del continente americano han disminuido significativamente desde 2024. Sin embargo, es probable que la tendencia en Estados Unidos no se esclarezca hasta finales de año, después que termine la temporada de mosquitos de verano.
Los investigadores de salud y control de vectores no están seguros de la gravedad de la situación en California.
Algunos afirman que podría haber brotes limitados, mientras que otros predicen que el dengue podría empeorar mucho. Sujan Shresta, profesor e investigador de enfermedades infecciosas en el Instituto de Inmunología de La Jolla, señaló que otros lugares, como Nepal, experimentaron relativamente pocos casos de dengue en el pasado reciente, pero ahora se registran brotes grandes con regularidad.
Existe una vacuna para niños, pero está siendo discontinuada debido a la falta de demanda mundial. Otras dos vacunas no están disponibles en Estados Unidos. El laboratorio de Shresta trabaja arduamente en una vacuna eficaz y segura contra el dengue. Espera publicar los resultados de las pruebas en animales en aproximadamente un año; si son positivos, los ensayos en humanos podrían ser posibles en unos dos años.
"Si no hay una buena vacuna ni buenos antivirales, este será un país endémico para dengue", afirmó.
Phillip Reese es especialista en reportaje de datos y profesor asociado de Periodismo en la Universidad Estatal de California-Sacramento.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
3 weeks 1 day ago
Global Health Watch, Noticias En Español, Public Health, States, california, Florida, Latinos, texas
KFF Health News' 'What the Health?': Supreme Court Upholds Bans on Gender-Affirming Care
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
The Supreme Court this week ruled in favor of Tennessee’s law banning most gender-affirming care for minors — a law similar to those in two dozen other states.
Meanwhile, the Senate is still hoping to complete work on its version of President Donald Trump’s huge budget reconciliation bill before the July Fourth break. But deeper cuts to the Medicaid program than those included in the House-passed bill could prove difficult to swallow for moderate senators.
This week’s panelists are Julie Rovner of KFF Health News, Victoria Knight of Axios, Alice Miranda Ollstein of Politico, and Sandhya Raman of CQ Roll Call.
Panelists
Victoria Knight
Axios
Alice Miranda Ollstein
Politico
Sandhya Raman
CQ Roll Call
Among the takeaways from this week’s episode:
- The Supreme Court’s ruling on gender-affirming care for transgender minors was relatively limited in its scope. The majority did not address the broader question about whether transgender individuals are protected under federal anti-discrimination laws and, as with the court’s decision overturning the constitutional right to an abortion, left states the power to determine what care trans youths may receive.
- The Senate GOP unveiled its version of the budget reconciliation bill this week. Defying expectations that senators would soften the bill’s impact on health care, the proposal would make deeper cuts to Medicaid, largely at the expense of hospitals and other providers. Republican senators say those cuts would allow them more flexibility to renew and extend many of Trump’s tax cuts.
- The Medicare trustees are out this week with a new forecast for the program that covers primarily those over age 65, predicting insolvency by 2033 — even sooner than expected. There was bipartisan support for including a crackdown on a provider practice known as upcoding in the reconciliation bill, a move that could have saved a bundle in government spending. But no substantive cuts to Medicare spending ultimately made it into the legislation.
- With the third anniversary of the Supreme Court decision overturning Roe v. Wade approaching, the movement to end abortion has largely coalesced around one goal: stopping people from accessing the abortion pill mifepristone.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: The New York Times’ “The Bureaucrat and the Billionaire: Inside DOGE’s Chaotic Takeover of Social Security,” by Alexandra Berzon, Nicholas Nehamas, and Tara Siegel Bernard.
Victoria Knight: The New York Times’ “They Asked an A.I. Chatbot Questions. The Answers Sent Them Spiraling,” by Kashmir Hill.
Alice Miranda Ollstein: Wired’s “What Tear Gas and Rubber Bullets Do to the Human Body,” by Emily Mullin.
Sandhya Raman: North Carolina Health News and The Charlotte Ledger’s “Ambulance Companies Collect Millions by Seizing Wages, State Tax Refunds,” by Michelle Crouch.
Also mentioned in this week’s podcast:
- KFF’s “KFF Health Tracking Poll: Views of the One Big Beautiful Bill,” by Ashley Kirzinger, Lunna Lopes, Marley Presiado, Julian Montalvo III, and Mollyann Brodie.
- The Associated Press’ “Trump Administration Gives Personal Data of Immigrant Medicaid Enrollees to Deportation Officials,” by Kimberly Kindy and Amanda Seitz.
- The Guardian’s “VA Hospitals Remove Politics and Marital Status From Guidelines Protecting Patients From Discrimination,” by Aaron Glantz.
click to open the transcript
Transcript: Supreme Court Upholds Bans on Gender-Affirming Care
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News, and I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Friday, June 20, at 10 a.m. As always, news happens fast and things might have changed by the time you hear this. So, here we go.
Today we are joined via videoconference by Alice Miranda Ollstein of Politico.
Alice Miranda Ollstein: Hello.
Rovner: Sandhya Raman of CQ Roll Call.
Sandhya Raman: Good morning.
Rovner: And Victoria Knight of Axios News.
Victoria Knight: Hello, everyone.
Rovner: No interview this week but more than enough news to make up for it, so we will go right to it. It is June. That means it is time for the Supreme Court to release its biggest opinions of the term. On Wednesday, the justices upheld Tennessee’s law banning gender-affirming medical care for trans minors. And presumably that means similar laws in two dozen other states can stand as well. Alice, what does this mean in real-world terms?
Ollstein: So, this is a blow to people’s ability to access gender-affirming care as minors, even if their parents support them transitioning. But it’s not necessarily as restrictive a ruling as it could have been. The court could have gone farther. And so supporters of access to gender-affirming care see a silver lining in that the court didn’t go far enough to rule that all laws discriminating against transgender people are fine and constitutional. A few justices more or less said that in their separate opinions, but the majority opinion just stuck with upholding this law, basically saying that it doesn’t discriminate based on gender or transgender status.
Rovner: Which feels a little odd.
Ollstein: Yes. So, obviously, many people have said, How can you say that laws that only apply to transgender people are not discriminatory? So, been some back-and-forth about that. But the majority opinion said, Well, we don’t have to reach this far and decide right now if laws that discriminate against transgender people are constitutional, because this law doesn’t. They said it discriminates based on diagnosis — so anyone of any gender who has the diagnosis of gender dysphoria for medications, hormones, that’s not a gender discrimination. But obviously the only people who do have those diagnoses are transgender, and so it was a logic that the dissenters, the three progressive dissenters, really ripped into.
Rovner: And just to be clear, we’ve heard about, there are a lot of laws that ban sort of not-reversible types of treatments for minors, but you could take hormones or puberty blockers. This Tennessee law covers basically everything for trans care, right?
Ollstein: That’s right, but only the piece about medications was challenged up to the Supreme Court, not the procedures and surgeries, which are much more rare for minors anyways. But it is important to note that some of the conservatives on the court said they would’ve gone further, and they basically said, This law does discriminate against transgender kids, and that is fine with us. And they said the court should have gone further and made that additional argument, which they did not at this time.
Rovner: Well, I’m sure the court will get another chance sometime in the future. While we’re on the subject of gender-affirming care in the courts, in Texas on Wednesday, conservative federal district judge Matthew Kacsmaryk — that’s the same judge who unsuccessfully tried to repeal the FDA’s [Food and Drug Administration’s] approval of the abortion pill a couple of years ago — has now ruled that the Biden administration’s expansion of the HIPAA [Health Insurance Portability and Accountability Act] medical privacy rules to protect records on abortion and gender-affirming care from being used for fishing expeditions by conservative prosecutors was an overreach, and he slapped a nationwide injunction on those rules. What could this mean if it’s ultimately upheld?
Ollstein: I kind of see this in some ways like the Trump administration getting rid of the EMTALA [Emergency Medical Treatment and Labor Act] guidance, where the underlying law is still there. This is sort of an interpretation and a guidance that was put out on top of it, saying, We interpret HIPAA, which has been around a long time, to apply in these contexts, because we’re in this brave new world where we don’t have Roe v. Wade anymore and states are seeking records from other states to try to prosecute people for circumventing abortion bans. And so, that wasn’t written into statute before, because that never happened before.
And so the Biden administration was attempting to respond to things like that by putting out this rule, which has now been blocked nationwide. I’m sure litigation will continue. There are also efforts in the courts to challenge HIPAA more broadly. And so, I would be interested in tracking how this plays into that.
Rovner: Yeah. There’s plenty of efforts sort of on this front. And certainly, with the advent of AI [artificial intelligence], I think that medical privacy is going to play a bigger role sort of as we go forward. All right. Moving on. While the Supreme Court is preparing to wrap up for the term, Congress is just getting revved up. Next up for the Senate is the budget reconciliation, quote, “Big Beautiful Bill,” with most of President [Donald] Trump’s agenda in it. This week, the Senate Finance Committee unveiled its changes to the House-passed bill, and rather than easing back on the Medicaid cuts, as many had expected in a chamber where just a few moderates can tank the entire bill, the Finance version makes the cuts even larger. Do we have any idea what’s going on here?
Knight: Well, I think mostly they want to give themselves more flexibility in order to pursue some of the tax policies that President Trump really wants. And so they need more savings, basically, to be able to do that and be able to do it for a longer amount of years. And so that’s kind of what I’ve heard, is they wanted to give themselves more room to play around with the policy, see what fits where. But a lot of people were surprised because the Senate is usually more moderate on things, but in this case I think it’s partially because they specifically looked at a provision called provider taxes. It’s a way that states can help fund their Medicaid programs, and so it’s a tax levied on providers. So I think they see that as maybe — it could still affect people’s benefits, but it’s aimed at providers — and so maybe that’s part of it as well.
Rovner: Well, of course aiming at providers is not doing them very much good, because hospitals are basically freaking out over this. Now there is talk of creating a rural hospital slush fund to maybe try to quell some of the complaints from hospitals and make some of those moderates feel better about voting for a bill that the Congressional Budget Office still says takes health insurance and food aid from the poor to give tax cuts to the rich. But if the Senate makes a slush fund big enough to really protect those hospitals, wouldn’t that just eliminate the Medicaid savings that they need to pay for those tax cuts, Victoria? That’s what you were just saying. That’s why they made the Medicaid cuts bigger.
Knight: Yeah. I think there’s quite a few solutions that people are throwing around and proposing. Yeah, but, exactly. Depending on if they do a provider relief fund, yeah, then the savings may need to go to that. I’ve also heard — I was talking to senators last week, and some of them were like, I’d rather just go back to the House’s version. So the House’s version of the bill put a freeze on states’ ability to raise the provider tax, but the Senate version incrementally lowers the amount of provider tax they can levy over years. The House just freezes it and doesn’t allow new ones to go higher. Some senators are like: Actually, can we just do that, go back to that? And we could live with that.
Even Sen. Josh Hawley, who has been one of the biggest vocal voices on concern for rural hospitals and concern for Medicaid cuts, he told me, Freeze would be OK with me. And so, I don’t know. I could see them maybe doing that, but we’ll see. There’s probably more negotiations going on over the weekend, and they’re also going to start the “Byrd bath” procedure, which basically determines whether provisions in the bill are related to the budget or not and can stay in the bill. And so, there’s actually gender-affirming care and abortion provisions in the bill that may get thrown out because of that. So—
Rovner: Yeah, this is just for those who don’t follow reconciliation the way we do, the “Byrd bath,” named for the former Sen. [Robert] Byrd, who put this rule in that said, Look, if you’re going to do this big budget bill with only 50 votes, it’s got to be related to the budget. So basically, the parliamentarian makes those determinations. And what we call the “Byrd bath” is when those on both sides of a provision that’s controversial go to the parliamentarian in advance and make their case. And the parliamentarian basically tells them in private what she’s going to do — like, This can stay in, or, This will have to go out. If the parliamentarian rules it has to go out, then it needs to overcome a budget point of order that needs 60 votes. So basically, that’s why stuff gets thrown out, unless they think it’s popular enough that it could get 60 votes. And sorry, that’s my little civics lesson for the day. Finish what you were saying, Victoria.
Knight: No, that was a perfect explanation. Thank you. But I was just saying, yeah, I think that there are still some negotiations going on for the Medicaid stuff. And where also, you have to remember, this has to go back to the House. And so it passed the House with the provider tax freeze, and that still required negotiations with some of the more moderate members of House Republicans. And some of them started expressing their concern about the Senate going further. And so they still need to — it has to go back through the House again, so they need to make these Senate moderates happy and House moderates happy. There’s also the fiscal conservatives that want deeper cuts. So there’s a lot of people within the caucus that they need to strike a balance. And so, I don’t know if this will be the final way the bill looks yet.
Rovner: Although, I think I say this every week, we have all of these Republicans saying: I won’t vote for this bill. I won’t vote for this bill. And then they inevitably turn around and vote for this bill. Do we believe that any of these people really would tank this bill?
Knight: That’s a great point. Yeah. Sandhya, go ahead.
Raman: There are at least a couple that I don’t think, anything that we do, they’re not going to change their mind. There is no courting of Rep. [Thomas] Massie in the House, because he’s not going to vote for it. I feel like in the Senate it’s going to be really hard to get Rand Paul on board, just because he does not want to raise the deficit. I think the others, it’s a little bit more squishy, depends kind of what the parliamentarian pulls out. And I guess also one thing I’m thinking about is if the things they pull out are big cost-savers and they have to go back to the drawing board to generate more savings. We’ve only had a few of the things that they’ve advised on so far, but it’s not health, and we still need to see — health are the big points. So, I think—
Rovner: Well, they haven’t started the “Byrd bath” on the Finance provisions—
Raman: Yes, or—
Rovner: —which is where all the health stuff is.
Raman: Yeah.
Knight: But that is supposed to be over the weekend. It’s supposed to start over the weekend.
Raman: Yes.
Rovner: Right.
Raman: Yeah. So, I think, depending on that, we will see. Historically, we have had people kind of go back and forth. And even with the House, there were people that voted for it that then now said, Well, I actually don’t support that anymore. So I think just going back to just what the House said might not be the solution, either. They have to find some sort of in-between before their July Fourth deadline.
Rovner: I was just going to say, so does this thing happen before July Fourth? I noticed that that Susie Wiles, the White House chief of staff said: Continue. It needs to be on the president’s desk by July Fourth. Which seems pretty nigh impossible. But I could see it getting through the Senate by July Fourth. I’m seeing some nods. Is that still the goal?
Knight: Yeah. I think that’s the goal. That’s what Senate Majority Leader [John] Thune has been telling people. He wants to try to pass it by mid-, or I think start the process by, midweek. And then it’s going to have to go through a “vote-a-rama.” So Democrats will be able to offer a ton of amendments. It’ll probably go through the night, and that’ll last a while. And so, I saw some estimate, maybe it’ll get passed next weekend through the Senate, but that’s probably if everything goes as it’s supposed to go. So, something could mess that up.
But, yeah, I think the factor here that has — I think everyone’s kind of been like: They’re not going to be able to do it. They’re not going to be able to do it. With the House, especially — the House is so rowdy. But then, when Trump calls people and tells them to vote for it, they do it. There’s a few, yeah, like Rand Paul and Massie — they’re basically the only ones that will not vote when Trump tells them to. But other than that — so if he wants it done, I do think he can help push to get it done.
Rovner: Yeah. I noticed one change, as I was going through, in the Senate bill from the House bill is that they would raise the debt ceiling to $5 trillion. It’s like, that’s a pretty big number. Yeah. I’m thinking that alone is what says Rand Paul is a no. Before we move on, one more thing I feel like we can’t repeat enough: This bill doesn’t just cut Medicaid spending. It also takes aim at the Affordable Care Act and even Medicare. And a bunch of new polls this week show that even Republicans aren’t super excited about this bill. Are Republican members of Congress going to notice this at some point? Yeah, the president is popular, but this bill certainly isn’t.
Raman: When you look at some of the town halls that they’ve had — or tried to have — over the last couple months and then scaled back because there was a lot of pushback directly on this, the Medicaid provisions, they have to be aware. But I think if you look at that polling, if you look at the people that identify as MAGA within Republicans, it’s popular for them. It’s just more broadly less popular. So I think that’s part of it, but—
Ollstein: I think that people are very opposed to the policies in the bill, but I also think people are very overwhelmed and distracted right now. There’s a lot going on, and so I’m not sure there will be the same national focus on this the way there was in 2017 when people really rallied in huge ways to protect the Affordable Care Act and push Congress not to overturn it. And so I think maybe that could be a factor in that outrage not manifesting as much. I also think that’s a reason they’re trying to do this quickly, that July Fourth deadline, before those protest movements have an opportunity to sort of organize and coalesce.
Just real quickly on the rural hospital slush fund, I saw some smart people comparing it to a throwback, the high-risk pools model, in that unless you pour a ton of funding into it, it’s not going to solve the problem. And if you pour a ton of funding into it, you don’t have the savings that created the problem in the first place, the cuts. And all that is to say also, how do we define rural? A lot of suburban and urban hospitals are also really struggling currently and would be subject to close. And so now you get into the pitting members and districts against each other, because some people’s hospitals might be saved and others might be left out in the cold. And so I just think it’s going to be messy going forward.
Rovner: I spent a good part of the late ’80s and early ’90s pulling out of bills little tiny provisions that would get tucked in to reclassify hospitals as rural so they could qualify, because there are already a lot of programs that give more money to rural hospitals to keep them open. Sorry, Victoria, we should move on, but you wanted to say one more thing?
Knight: Oh, yeah. No. I was just going to say, going back to the unpopularity of the bill based on polling, and I think that we’ll see at least Democrats — if Republicans get this done and they have the work requirements and the other cuts to Medicaid in the bill, cuts to ACA, no renewal of premium tax credits — I think Democrats will really try to make the midterms about this, right? We already are seeing them messaging about it really hardcore, and obviously the Democrats are trying to find their way right now post-[Joe] Biden, post-[Kamala] Harris. So I think they’ll at least try to make this bill the thing and see if it’s unpopular with the general public, what Republicans did with health care on this. So we’ll see if that works for them, but I think they’re going to try.
Rovner: Yeah, I think you’re right. Well, speaking of Medicare, we got the annual trustees report this week, and the insolvency date for Medicare’s Hospital Insurance Trust Fund has moved up to 2033. That’s three years sooner than predicted last year. Yet there’s nothing in the budget reconciliation bill that would address that, not even a potentially bipartisan effort to go after upcoding in Medicare Advantage that we thought the Finance Committee might do, that would save money for Medicare that insurers are basically overcharging the government for. What happened to the idea of going after Medicare Advantage overpayments?
Knight: My general vibe I got from asking senators was that Trump said, We’re not touching Medicare in this bill. He did not want that to happen. And I think, again, maybe potentially thinking about the midterms, just the messaging on that, touching Medicare, it kind of always goes where they don’t want to touch Medicare, because it’s older people, but Medicaid is OK, even though it’s poor people.
Rovner: And older people.
Ollstein: And they are touching Medicare in the bill anyway.
Rovner: Thank you. I know. I think that’s the part that makes my head swim. It’s like, really? There are several things that actually touch Medicare in this bill, but the thing that they could probably save a good chunk of money on and that both parties agree on is the thing that they’re not doing.
Knight: Exactly. It was very bipartisan.
Rovner: Yes. It was very bipartisan, and it’s not there. All right. Moving on. Elon Musk has gone back to watching his SpaceX rockets blow up on the launchpad, which feels like a fitting metaphor for what’s been left behind at the Department of Health and Human Services following some of the DOGE [Department of Government Efficiency] cuts. On Monday, a federal judge in Massachusetts ruled that billions of dollars in cuts to about 800 NIH [National Institutes of Health] research grants due to DEI [diversity, equity, and inclusion] were, quote, “arbitrary and capricious” and wrote, quote, “I’ve never seen government racial discrimination like this.” And mind you, this was a judge who was appointed by [President] Ronald Reagan. So what happens now? It’s been months since these grants were terminated, and even though the judge has ordered the funding restored, this obviously isn’t the last word, and one would expect the administration’s going to appeal, right? So these people are just supposed to hang out and wait to see if their research gets to continue?
Raman: This has been a big thing that has come up in all of the appropriations hearings we’ve had so far this year, that even though the gist of that is to look forward at the next year’s appropriations, it’s been a big topic of just: There is funding that we as Congress have already appropriated for this. Why isn’t it getting distributed? So I think that will definitely be something that they push back up on the next ones of those. Some of the different senators have said that they’ve been looking into it and how it’s been affecting their districts. So I would say that. But I think the White House in response to that called the decision political, which I thought was interesting given, like you said, it was a Reagan appointee that said this. So it’ll definitely be something that I think will be appealed and be a major issue.
Ollstein: Yeah, and the folks I’ve talked to who’ve been impacted by this stress that you can’t flip funding on and off like a switch and expect research to continue just fine. Once things are halted, they’re halted. And in a lot of cases, it is irreversible. Samples are thrown out. People are laid off. Labs are shut down. Even if there’s a ruling that reverses the policy, that often comes too late to make a difference. And at the same time, people are not waiting around to see how this back-and-forth plays out. People are getting actively recruited by universities and other countries saying: Hey, we’re not going to defund you suddenly. Come here. And they’re moving to the private sector. And so I think this is really going to have a long impact no matter what happens, a long tail.
Rovner: And yet we got another reminder this week of the major advances that federally funded research can produce, with the FDA approval of a twice-a-year shot that can basically prevent HIV infection. Will this be able to make up maybe for the huge cuts to HIV programs that this administration is making?
Raman: It’s only one drug, and we have to see what the price is, what cost—
Rovner: So far the price is huge. I think I saw it was going to be like $14,000 a shot.
Raman: Which means that something like PrEP [pre-exposure prophylaxis] is still going to be a lot more affordable for different groups, for states, for relief efforts. So I think that it’s a good step on the research front, but until the price comes down, the other tools in the toolbox are going to be a lot more feasible to do.
Rovner: Yeah. So much for President Trump’s goal to end HIV. So very first-term. All right. Well, turning to abortion, it’s been almost exactly three years since the Supreme Court overturned the nationwide right to abortion in the Dobbs case. In that time we’ve seen abortion outlawed in nearly half the states but abortions overall rise due to the expanded use of abortion medication. We’ve seen doctors leaving states with bans, for fear of not being able to provide needed care for patients with pregnancy complications. And we’ve seen graduating medical students avoiding taking residencies in those states for the same reason. Alice, what’s the next front in the battle over abortion in the U.S.?
Ollstein: It’s been one of the main fronts, even before Dobbs, but it’s just all about the pills right now. That’s really where all of the attention is. So whether that’s efforts ongoing in the courts back before our friend Kacsmaryk to try to challenge the FDA’s policies around the pills and impose restrictions nationwide, there’s efforts at the state level. There’s agitation for Congress to do something, although I think that’s the least likely option. I think it’s much more likely that it’s going to come from agency regulation or from the courts or from states. So I would put Congress last on the list of actors here. But I think that’s really it. And I think we’re also seeing the same pattern that we see in gender-affirming care battles, where there’s a lot of focus on what minors can access, what children can access, and that then expands to be a policy targeting people of any age.
So I think it’s going to be a factor. One thing I think is going to slow down significantly are these ballot initiatives in the states. There’s only a tiny handful of states left that haven’t done it yet and have the ability to do it. A lot of states, it’s not even an option. So I would look at Idaho for next year, and Nevada. But I don’t think you’re going to see the same storm of them that you have seen the last few years. And part of that is, like I said, there’s just fewer left that have the ability. But also some people have soured on that as a tactic and feel that they haven’t gotten the bang for the buck, because those campaigns are extremely expensive, extremely resource-intensive. And there’s been frustration that, in Missouri, for instance, it’s sort of been — the will of the people has sort of been overturned by the state government, and that’s being attempted in other states as well. And so it has seemed to people like a very expensive and not reliable protection, although I’m not sure in some states what the other option would even be.
Rovner: Of course the one thing that is happening on Capitol Hill is that the House Judiciary Committee last week voted to repeal the 1994 Freedom of Access to Clinic Entrances Act, or FACE. Now this law doesn’t just protect abortion clinics but also anti-abortion crisis pregnancy centers. This feels like maybe not the best timing for this sort of thing, especially in light of the shootings of lawmakers in Minnesota last weekend, where the shooter reportedly had in his car a list of abortion providers and abortion rights supporters. Might that slow down this FACE repeal effort?
Ollstein: I think it already was going to be an uphill battle in the Senate and even maybe passing the full House, because even some conservatives say, Well, I don’t know if we should get rid of the FACE Act, because the FACE Act also applies to conservative crisis pregnancy centers. And lest we forget, only a few short weeks ago, an IVF [in vitro fertilization] clinic was bombed, and it would’ve applied in that situation, too. And so some conservatives are divided on whether or not to get rid of the FACE Act. And so I don’t know where it is going forward, but I think these recent instances of violence certainly are not helping the efforts, and the Trump administration has already said they’re not really going to enforce FACE against people who protest outside of abortion clinics. And so that takes some of the heat off of the conservatives who want to get rid of it. Of course, they say it shouldn’t be left for a future administration to enforce, as the Biden administration did.
Raman: It also applies to churches, which I think if you are deeply religious that could also be a point of contention for you. But, yeah, I think just also with so much else going on and the fact that they’ve kind of slowed down on taking some of these things up for the whole chamber to vote on outside of in January, I don’t really see it coming up in the immediate future for a vote.
Rovner: Well, at the same time, there are efforts in the other direction, although the progress on that front seems to be happening in other countries. The British Parliament this week voted to decriminalize basically all abortions in England and Wales, changing an 1861 law. And here on this side of the Atlantic, four states are petitioning the FDA to lift the remaining restrictions on the abortion pill, mifepristone, even as — Alice, as you mentioned — abortion foes argue for its approval to be revoked. You said that the abortion rights groups are shying away from these ballot measures even if they could do it. What is going to be their focus?
Ollstein: Yeah, and I wouldn’t say they’re shying away from it. I’ve just heard a more divided view as a tactic and whether it’s worth it or not. But I do think that these court battles are really going to be where a lot is decided. That’s how we got to where we are now in the first place. And so the effort to get rid of the remaining restrictions on the abortion pill, the sort of back-and-forth tug here, that’s also been going on for years and years, and so I think we’re going to see that continue as well. And I think there’s also going to be, parallel to that, a sort of PR war. And I think we saw that recently with anti-abortion groups putting out their own not-peer-reviewed research to sort of bolster their argument that abortion pills are dangerous. And so I think you’re going to see more things like that attempting to — as one effort goes on in court, another effort in parallel in the court of public opinion to make people view abortion pills as something to fear and to want to restrict.
Rovner: All right. Well, finally this week, a couple of stories that just kind of jumped out at me. First, the AP [Associated Press] is reporting that Medicaid officials, over the objections of some at the agency, have turned over to the Department of Homeland Security personal data on millions of Medicaid beneficiaries, including those in states that allow noncitizens to enroll even if they’re not eligible for federal matching funds, so states that use their own money to provide insurance to these people. That of course raises the prospect of DHS using that information to track down and deport said individuals. But on a broader level, one of the reasons Medicaid has been expanded for emergencies and in some cases for noncitizens is because those people live here and they get sick. And not only should they be able to get medical care because, you know, humanity, but also because they may get communicable diseases that they can spread to their citizen neighbors and co-workers. Is this sort of the classic case of cutting off your nose despite your face?
Ollstein: I think we saw very clearly during covid and during mpox and measles, yes. What impacts one part of the population impacts the whole population, and we’re already seeing that these immigration crackdowns are deterring people, even people who are legally eligible for benefits and services staying away from that. We saw that during Trump’s first term with the public charge rule that led to people disenrolling in health programs and avoiding services. And that effect continued. There’s research out of UCLA showing that effect continued even after the Biden administration got rid of the policy. And so fear and the chilling effect can really linger and have an impact and deter people who are citizens, are legal immigrants, from using that as well. It’s a widespread impact.
Rovner: And of course, now we see the Trump administration revoking the status of people who came here legally and basically declaring them illegal after the fact. Some of this chilling effect is reasonable for people to assume. Like the research being cut off, even if these things are ultimately reversed, there’s a lot of — depends whether you consider it damage or not — but a lot of the stuff is going to be hard. You’re not going to be able to just resume, pick up from where you were.
Ollstein: And one concern I’ve been hearing particularly is around management of bird flu, since a lot of legal and undocumented workers work in agriculture and have a higher likelihood of being exposed. And so if they’re deterred from seeking testing, seeking treatment, that could really be dangerous for the whole population.
Rovner: Yeah. It is all about health. It is always all about health. All right. Well, the last story this week is from The Guardian, and it’s called “VA Hospitals Remove Politics and Marital Status From Guidelines Protecting Patients From Discrimination.” And it’s yet another example of how purging DEI language can at least theoretically get you in trouble. It’s not clear if VA [Department of Veterans Affairs] personnel can now actually discriminate against people because of their political party or because they’re married or not married. The administration says other safeguards are still in place, but it is another example of how sweeping changes can shake people’s confidence in government programs. I imagine the idea here is to make people worried about discrimination and therefore less likely to seek care, right?
Raman: It’s also just so unusual. I have not heard of anything like this before in anything that we’ve been reporting, where your political party is pulled into this. It just seems so out of the realm of what a provider would need to know about you to give you care. And then I could see the chilling effect in the same way, where if someone might want to be active on some issue or share their views, they might be more reluctant to do so, because they know they have to get care. And if that could affect their ability to do so, if they would have to travel farther to a different VA hospital, even if they aren’t actually denying people because of this, that chilling effect is going to be something to watch.
Rovner: And this is, these are not sort of theoretical things. There was a case some years ago about a doctor, I think he was in Kentucky, who wouldn’t prescribe birth control to women who weren’t married. So there was reason for having these protections in there, even though they are not part of federal anti-discrimination law, which is what the Trump administration said. Why are these things in there? They’re not required, so we’re going to take them out. That’s basically what this fight is over. But it’s sort of an — I’m sure there are other places where this is happening. We just haven’t seen it yet.
All right, well, that is this week’s news. Now it’s time for our extra-credit segment. That’s where we each recognize the story we read this week we think you should read, too. Don’t worry if you miss it. We will put the links in our show notes on your phone or other mobile device. Victoria, why don’t you go first this week?
Knight: Sure thing. My extra credit, it’s from The New York Times. The title is, “They Asked an A.I. Chatbot Questions. The Answers Sent Them Spiraling,” by Kashmir Hill, who covers technology at The Times. I had seen screenshots of this article being shared on X a bunch last week, and I was like, “I need to read this.”
Basically it shows that different people who, they may be going through something, they may have a lot of stress, or they may already have a mental health condition, and they start messaging ChatGPT different things, then ChatGPT can kind of feed into their own delusions and their own misaligned thinking. That’s because that’s kind of how ChatGPT is built. It’s built to be, like, they call it in the story, like a sycophant. Is that how you say it? So it kind of is supposed to react positively to what you’re saying and kind of reinforce what you’re saying. And so if you’re feeding it delusions, it will feed delusions back. And so it was really scary because real-life people were impacted by this. There was one individual who thought he was talking to — had found an entity inside of ChatGPT named Juliet, and then he thought that OpenAI killed her. And so then he ended up basically being killed by police that came to his house. It was just — yeah, there was a lot of real-life effects from talking to ChatGPT and having your own delusions reinforced. So, and so it was just an effect of ChatGPT on real-life people that I don’t know if we’ve seen illustrated in a news story yet. And so it was very illuminating, yeah.
Rovner: Yeah. Not scary much. Sandhya.
Raman: My extra credit was “Ambulance Companies Collect Millions by Seizing Wages, State Tax Refunds.” It’s by Michelle Crouch for The Charlotte Ledger [and North Carolina Health News]. It’s a story about how some different ambulance patients from North Carolina are finding out that their income gets tapped for debt collection by the state’s EMS agencies, which are government entities, mostly. So the state can take through the EMS up to 10% of your monthly paycheck, or pull from your bank account higher than that, or pull from your tax refunds or lottery winnings. And it’s taking some people a little bit by surprise after they’ve tried to pay off this care and having to face this, but something that the agencies are also saying is necessary to prevent insurers from underpaying them.
Rovner: Oh, sigh.
Raman: Yeah.
Rovner: The endless stream of really good stories on this subject. Alice.
Ollstein: So I chose this piece in Wired by Emily Mullin called “What Tear Gas and Rubber Bullets Do to the Human Body,” thinking a lot about my hometown of Los Angeles, which is under heavy ICE [Immigration and Customs Enforcement] enforcement and National Guard and Marines and who knows who else. So this article is talking about the health impacts of so-called less-lethal police tactics like rubber bullets, like tear gas. And it is about how not only are they sometimes actually lethal — they can kill people and have — but also they have a lot of lingering impacts, especially tear gas. It can exacerbate respiratory problems and even cause brain damage. And so it’s being used very widely and, in some people’s view, indiscriminately right now. And there should be more attention on this, as it can impact completely innocent bystanders and press and who knows who else.
Rovner: Yeah. There’s a long distance between nonlethal and harmless, which I think this story illustrates very well. My extra credit this week is also from The New York Times. It’s called “The Bureaucrat and the Billionaire: Inside DOGE’s Chaotic Takeover of Social Security,” by Alexandra Berzon, Nicholas Nehamas, and Tara Siegel Bernard. It’s about how the White House basically forced Social Security officials to peddle a false narrative that said 40% of calls to the agency’s customer service lines were from scammers — they were not — how DOGE misinterpreted Social Security data and gave a 21-year-old intern access to basically everyone’s personal Social Security information, and how the administration shut down some Social Security offices to punish lawmakers who criticized the president. This is stuff we pretty much knew was happening at the time, and not just in Social Security. But The New York Times now has the receipts. It’s definitely worth reading.
OK. That is this week’s show. Thanks as always to our editor, Emmarie Huetteman, and our producer-engineer, Francis Ying. Also, as always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left us a review. That helps other people find us, too. You can email us your comments or questions. We’re at whatthehealth@kff.org. Or you can find me still on X, @jrovner, or on Bluesky, @julierovner. Where are you guys hanging these days? Sandhya.
Raman: @SandhyaWrites on X and the same on Bluesky.
Rovner: Alice.
Ollstein: @alicemiranda on Bluesky and @AliceOllstein on X.
Rovner: Victoria.
Knight: I am @victoriaregisk on X.
Rovner: We will be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 month 3 days ago
Courts, Health Care Costs, Health Industry, Insurance, Medicaid, Medicare, Multimedia, Pharmaceuticals, Rural Health, States, Abortion, Children's Health, Hospitals, KFF Health News' 'What The Health?', LGBTQ+ Health, Podcasts, Privacy, Tennessee, texas, Transgender Health, Trump Administration, U.S. Congress, Veterans' Health
In a Dusty Corner of California, Trump’s Threatened Cuts to Asthma Care Raise Fears
Esther Bejarano’s son was 11 months old when asthma landed him in the hospital. She didn’t know what had triggered his symptoms — neither she nor her husband had asthma — but she suspected it was the pesticides sprayed on the agricultural fields near her family’s home.
Pesticides are a known contributor to asthma and are commonly used where Bejarano lives in California’s Imperial Valley, a landlocked region that straddles two counties on the U.S.-Mexico border and is one of the main producers of the nation’s winter crops. It also has some of the worst air pollution in the nation and one of the highest rates of childhood asthma emergency room visits in the state, according to data collected by the California Department of Public Health.
Bejarano has since learned to manage her now-19-year-old son’s asthma and works at Comite Civico del Valle, a local rights organization focused on environmental justice in the Imperial Valley. The organization trains health care workers to educate patients on proper asthma management, enabling them to avoid hospitalization and eliminate triggers at home. The course is so popular that there’s a waiting list, Bejarano said.
But the group’s Asthma Management Academy program and similar initiatives nationwide face extinction with the Trump administration’s mass layoffs, grant cancellations, and proposed budget cuts at the Department of Health and Human Services and the Environmental Protection Agency. Asthma experts fear the cumulative impact of the reductions could result in more ER visits and deaths, particularly for children and people in low-income communities — populations disproportionately vulnerable to the disease.
“Asthma is a preventive condition,” Bejarano said. “No one should die of asthma.”
Asthma can block airways, making it hard to breathe, and in severe cases can cause death if not treated quickly. Nearly 28 million people in the U.S. have asthma, and about 10 people still die every day from the disease, according to the Asthma and Allergy Foundation of America.
In May, the White House released a budget proposal that would permanently shutter the Centers for Disease Control and Prevention’s National Asthma Control Program, which was already gutted by federal health department layoffs in April. It’s unclear whether Congress will approve the closure.
Last year, the program allotted $33.5 million to state-administered initiatives in 27 states, Puerto Rico, and Washington, D.C., to help communities with asthma education. The funding is distributed in four-year grant cycles, during which the programs receive up to $725,000 each annually.
Comite Civico del Valle’s academy in Southern California, a clinician workshop in Houston, and asthma medical management training in Allentown, Pennsylvania — ranked the most challenging U.S. city to live in with asthma — are among the programs largely surviving on these grants. The first year of the current grant cycle ends Aug. 31, and it’s unknown whether funding will continue beyond then.
Data suggests that the CDC’s National Asthma Control Program has had a significant impact. The agency’s own research has shown that the program saves $71 in health care costs for every $1 invested. And the asthma death rate decreased 44% between the 1999 launch of the program and 2021, according to the American Lung Association.
“Losing support from the CDC will have devastating impacts on asthma programs in states and communities across the country, programs that we know are improving the lives of millions of people with asthma,” said Anne Kelsey Lamb, director of the Public Health Institute’s Regional Asthma Management and Prevention program. “And the thing is that we know a lot about what works to help people keep their asthma well controlled, and that’s why it’s so devastating.”
The Trump administration cited cost savings and efficiency in its April announcement of the cuts to HHS. Requests for comment from the White House and CDC about cuts to federal asthma and related programs were not answered.
The Information Wars
Fresno, in the heart of California’s Central Valley, is one of the country’s top 20 “asthma capitals,” with high rates of asthma and related emergencies and deaths. It’s home to programs that receive funding through the National Asthma Control Program. Health care professionals there also rely on another aspect of the program that is under threat if it’s shuttered: countrywide data.
The federal asthma program collects information on asthma rates and offers a tool to study prevalence and rates of death from the disease, see what populations are most affected, and assess state and local trends. Asthma educators and health care providers worry that the loss of these numbers could be the biggest impact of the cuts, because it would mean a dearth of information crucial to forming educated recommendations and treatment plans.
“How do we justify the services we provide if the data isn’t there?” said Graciela Anaya, director of community health at the Central California Asthma Collaborative in Fresno.
Mitchell Grayson, chair of the Asthma and Allergy Foundation’s Medical Scientific Council, is similarly concerned.
“My fear is we’re going to live in a world that is frozen in Jan. 19, 2025, as far as data, because that was the last time you know that this information was safely collected,” he said.
Grayson, an allergist who practices in Columbus, Ohio, said he also worries government websites will delete important recommendations that asthma sufferers avoid heavy air pollution, get annual flu shots, and get covid-19 vaccines.
Disproportionate Risk
Asthma disproportionately affects communities of color because of “historic structural issues,” said Lynda Mitchell, CEO of the Asthma and Allergy Network, citing a higher likelihood of living in public housing or near highways and other pollution sources.
She and other experts in the field said cuts to diversity initiatives across federal agencies, combined with the rollback of environmental protections, will have an outsize impact on these at-risk populations.
In December, the Biden administration awarded nearly $1.6 billion through the EPA’s Community Change Grants program to help disadvantaged communities address pollution and climate threats. The Trump administration moved to cut this funding in March. The grant freezes, which have been temporarily blocked by the courts, are part of a broader effort by the Trump EPA to eliminate aid to environmental justice programs across the agency.
In 2023 and 2024, the National Institutes of Health’s Climate Change and Health Initiative received $40 million for research, including on the link between asthma and climate change. The Trump administration has moved to cut that money. And a March memo essentially halted all NIH grants focused on diversity, equity, and inclusion, or DEI — funds many of the asthma programs serving low-income communities rely on to operate.
On top of those cuts, environmental advocates like Isabel González Whitaker of Memphis, Tennessee, worry that the proposed reversals of environmental regulations will further harm the health of communities like hers that are already reeling from the effects of climate change. Shelby County, home to Memphis, recently received an “F” on the American Lung Association’s annual report card for having so many high ozone days. González Whitaker is director of EcoMadres, a program within the national organization Moms for Clean Air that advocates for better environmental conditions for Latino communities.
“Urgent asthma needs in communities are getting defunded at a time when I just see things getting worse in terms of deregulation,” said González Whitaker, who took her 12-year-old son to the hospital because of breathing issues for the first time this year. “We’re being assaulted by this data and science, which is clearly stating that we need to be doing better around preserving the regulations.”
Back in California’s Imperial Valley — where the majority-Hispanic, working-class population surrounds California’s largest lake, the Salton Sea — is an area called Bombay Beach. Bejarano calls it the “forgotten community.” Homes there lack clean running water, because of naturally occurring arsenic in the groundwater, and residents frequently experience a smell like rotten eggs blowing off the drying lakebed, exposing decades of pesticide-tinged dirt.
In 2022, a 12-year-old girl died in Bombay Beach after an asthma attack. Bejarano said she later learned that the girl’s school had recommended that she take part in Comite Civico del Valle’s at-home asthma education program. She said the girl was on the waiting list when she died.
“It hit home. Her death showed the personal need we have here in Imperial County,” Bejarano said. “Deaths are preventable. Asthma is reversible. If you have asthma, you should be able to live a healthy life.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 month 2 weeks ago
california, Public Health, Rural Health, States, Children's Health, HHS, Pennsylvania, Tennessee, texas, Trump Administration
When Hospitals Ditch Medicare Advantage Plans, Thousands of Members Get To Leave, Too
For several years, Fred Neary had been seeing five doctors at the Baylor Scott & White Health system, whose 52 hospitals serve central and northern Texas, including Neary’s home in Dallas. But in October, his Humana Medicare Advantage plan — an alternative to government-run Medicare — warned that Baylor and the insurer were fighting over a new contract.
If they couldn’t reach an agreement, he’d have to find new doctors or new health insurance.
“All my medical information is with Baylor Scott & White,” said Neary, 87, who retired from a career in financial services. His doctors are a five-minute drive from his house. “After so many years, starting over with that many new doctor relationships didn’t feel like an option.”
After several anxious weeks, Neary learned Humana and Baylor were parting ways as of this year, and he was forced to choose between the two. Because the breakup happened during the annual fall enrollment period for Medicare Advantage, he was able to pick a new Advantage plan with coverage starting Jan. 1, a day after his Humana plan ended.
Other Advantage members who lose providers are not as lucky. Although disputes between health systems and insurers happen all the time, members are usually locked into their plans for the year and restricted to a network of providers, even if that network shrinks. Unless members qualify for what’s called a special enrollment period, switching plans or returning to traditional Medicare is allowed only at year’s end, with new coverage starting in January.
But in the past 15 months, the Centers for Medicare & Medicaid Services, which oversees the Medicare Advantage program, has quietly offered roughly three-month special enrollment periods allowing thousands of Advantage members in at least 13 states to change plans. They were also allowed to leave Advantage plans entirely and choose traditional Medicare coverage without penalty, regardless of when they lost their providers. But even when CMS lets Advantage members leave a plan that lost a key provider, insurers can still enroll new members without telling them the network has shrunk.
At least 41 hospital systems have dropped out of 62 Advantage plans serving all or parts of 25 states since July, according to Becker’s Hospital Review. Over the past two years, separations between Advantage plans and health systems have tripled, said FTI Consulting, which tracks reports of the disputes.
CMS spokesperson Catherine Howden said it is “a routine occurrence” for the agency to determine that provider network changes trigger a special enrollment period for their members. “It has happened many times in the past, though we have seen an uptick in recent years.”
Still, CMS would not identify plans whose members were allowed to disenroll after losing health providers. The agency also would not say whether the plans violated federal provider network rules intended to ensure that Medicare Advantage members have sufficient providers within certain distances and travel times.
The secrecy around when and how Advantage members can escape plans after their doctors and hospitals drop out worries Sen. Ron Wyden of Oregon, the senior Democrat on the Senate Finance Committee, which oversees CMS.
“Seniors enrolled in Medicare Advantage plans deserve to know they can change their plan when their local doctor or hospital exits the plan due to profit-driven business practices,” Wyden said.
The increase in insurer-provider breakups isn’t surprising, given the growing popularity of Medicare Advantage. The plans attracted about 54% of the 61.2 million people who had both Medicare Parts A and B and were eligible to sign up for Medicare Advantage in 2024, according to KFF, a health information nonprofit that includes KFF Health News.
The plans can offer supplemental benefits unavailable from traditional Medicare because the federal government pays insurers about 20% more per member than traditional Medicare per-member costs, according to the Medicare Payment Advisory Commission, which advises Congress. The extra spending, which some lawmakers call wasteful, will total about $84 billion in 2025, MedPAC estimates. While traditional Medicare does not offer the additional benefits Advantage plans advertise, it does not limit beneficiaries’ choice of providers. They can go to any doctor or hospital that accepts Medicare, as nearly all do.
Sanford Health, the largest rural health system in the U.S., serving parts of seven states from South Dakota to Michigan, decided to leave a Humana Medicare Advantage plan last year that covered 15,000 of its patients. “It’s not so much about the finances or administrative burden, although those are real concerns,” said Nick Olson, Sanford Health’s chief financial officer. “The most important thing for us is the fact that coverage denials and prior authorization delays impact the care a patient receives, and that’s unacceptable.”
The National Association of Insurance Commissioners, representing insurance regulators from every state, Puerto Rico, and the District of Columbia, has appealed to CMS to help Advantage members.
“State regulators in several states are seeing hospitals and crucial provider groups making decisions to no longer contract with any MA plans, which can leave enrollees without ready access to care,” the group wrote in September. “Lack of CMS guidance could result in unnecessary financial or medical injury to America’s seniors.”
The commissioners appealed again last month to Health and Human Services Secretary Robert F. Kennedy Jr. “Significant network changes trigger important rights for beneficiaries, and they should receive clear notice of their rights and have access to counseling to help them make appropriate choices,” they wrote.
The insurance commissioners asked CMS to consider offering a special enrollment period for all Advantage members who lose the same major provider, instead of placing the burden on individuals to find help on their own. No matter what time of year, members would be able to change plans or enroll in government-run Medicare.
Advantage members granted this special enrollment period who choose traditional Medicare get a bonus: If they want to purchase a Medigap policy — supplemental insurance that helps cover Medicare’s considerable out-of-pocket costs — insurers can’t turn them away or charge them more because of preexisting health conditions.
Those potential extra costs have long been a deterrent for people who want to leave Medicare Advantage for traditional Medicare.
“People are being trapped in Medicare Advantage because they can’t get a Medigap plan,” said Bonnie Burns, a training and policy specialist at California Health Advocates, a nonprofit watchdog that helps seniors navigate Medicare.
Guaranteed access to Medigap coverage is especially important when providers drop out of all Advantage plans. Only four states — Connecticut, Massachusetts, Maine, and New York — offer that guarantee to anyone who wants to reenroll in Medicare.
But some hospital systems, including Great Plains Health in North Platte, Nebraska, are so frustrated by Advantage plans that they won’t participate in any of them.
It had the same problems with delays and denials of coverage as other providers, but one incident stands out for CEO Ivan Mitchell: A patient too sick to go home had to stay in the hospital an extra six weeks because her plan wouldn’t cover care in a rehabilitation facility.
With traditional Medicare the only option this year for Great Plains Health patients, Nebraska insurance commissioner Eric Dunning asked for a special enrollment period with guaranteed Medigap access for some 1,200 beneficiaries. After six months, CMS agreed.
Once Delaware’s insurance commissioner contacted CMS about the Bayhealth medical system dropping out of a Cigna Advantage plan, members received a special enrollment period starting in January.
Maine’s congressional delegation pushed for an enrollment period for nearly 4,000 patients of Northern Light Health after the 10-hospital system dropped out of a Humana Advantage plan last year.
“Our constituents have told us that they are anticipating serious challenges, ranging from worries about substantial changes to cost-sharing rates to concerns about maintaining care with current providers,” the delegation told CMS.
CMS granted the request to ensure “that MA enrollees have access to medically necessary care,” then-CMS Administrator Chiquita Brooks-LaSure wrote to Sen. Angus King (I-Maine).
Minnesota insurance officials appealed to CMS on behalf of some 75,000 members of Aetna, Humana, and UnitedHealthcare Advantage plans after six health systems announced last year they would leave the plans in 2025. So many provider changes caused “tremendous problems,” said Kelli Jo Greiner, director of the Minnesota State Health Insurance Assistance Program, known as a SHIP, at the Minnesota Board on Aging. SHIP counselors across the country provide Medicare beneficiaries free help choosing and using Medicare drug and Advantage plans.
Providers serving about 15,000 of Minnesota’s Advantage members ultimately agreed to stay in the insurers’ networks. CMS decided 14,000 Humana members qualified for a network-change special enrollment period.
The remaining 46,000 people — Aetna and UnitedHealthcare Advantage members — who lost access to four health systems were not eligible for the special enrollment period. CMS decided their plans still had enough other providers to care for them.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
2 months 3 weeks ago
Aging, Health Care Costs, Health Industry, Insurance, Medicare, Rural Health, CMS, Connecticut, Delaware, Hospitals, Maine, Massachusetts, Medicare Advantage, Michigan, Minnesota, Nebraska, New York, South Dakota, texas
KFF Health News' 'What the Health?': The Ax Falls at HHS
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
As had been rumored for weeks, Health and Human Services Secretary Robert F. Kennedy Jr. unveiled a plan to reorganize the department. It involves the downsizing of its workforce, which formerly was roughly 80,000 people, by a quarter and consolidating dozens of agencies that were created and authorized by Congress.
Meanwhile, in just the past week, HHS abruptly cut off billions in funding to state and local public health departments, and canceled all research studies into covid-19, as well as diseases that could develop into the next pandemic.
This week’s panelists are Julie Rovner of KFF Health News, Maya Goldman of Axios News, Joanne Kenen of the Johns Hopkins Bloomberg School of Public Health and Politico Magazine, and Alice Miranda Ollstein of Politico.
Panelists
Maya Goldman
Axios
Joanne Kenen
Johns Hopkins University and Politico
Alice Miranda Ollstein
Politico
Among the takeaways from this week’s episode:
- As federal health officials reveal the targets of a significant workforce purge and reorganization, the GOP-controlled Congress has been notably quiet about the Trump administration’s intrusions on its constitutional powers. Many of the administration’s attempts to revoke and reorganize federally funded work are underway despite Congress’ previous approval of that funding. And while changes might be warranted, reviewing how the federal government works (or doesn’t) — in the public forums of congressional hearings and floor debate — is part of Congress’ responsibilities.
- The news of a major reorganization at HHS also comes before the Senate finishes confirming its leadership team. New leaders of the National Institutes of Health and the FDA were confirmed just this week; Mehmet Oz, the nominated director of the Centers for Medicare & Medicaid Services, had not yet been confirmed when HHS made its announcement; and President Donald Trump only recently named a replacement nominee to lead the Centers for Disease Control and Prevention, after withdrawing his first pick.
- While changes early in Trump’s second term have targeted the federal government and workforce, the impacts continue to be felt far outside the nation’s capital. Indeed, cuts to jobs and funding touch every congressional district in the nation. They’re also being felt in research areas that the Trump administration claims as priorities, such as chronic disease: The administration said this week it will shutter the office devoted to studying long covid, a chronic disease that continues to undermine millions of Americans’ health.
- Meanwhile, in the states, doctors in Texas report a rise in cases of children with liver damage due to ingesting too much vitamin A — a supplement pushed by Kennedy in response to the measles outbreak. The governor of West Virginia signed a sweeping ban on food dyes and additives. And a woman in Georgia who experienced a miscarriage was arrested in connection with the improper disposal of fetal remains.
Also this week, Rovner interviews KFF senior vice president Larry Levitt about the 15th anniversary of the signing of the Affordable Care Act and the threats the health law continues to face.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: CNN’s “State Lawmakers Are Looking To Ban Non-Existent ‘Chemtrails.’ It Could Have Real-Life Side Effects,” by Ramishah Maruf and Brandon Miller.
Alice Miranda Ollstein: The New York Times Wirecutter’s “23andMe Just Filed for Bankruptcy. You Should Delete Your Data Now,” by Max Eddy.
Maya Goldman: KFF Health News’ “‘I Am Going Through Hell’: Job Loss, Mental Health, and the Fate of Federal Workers,” by Rachana Pradhan and Aneri Pattani.
Joanne Kenen: The Atlantic’s “America Is Done Pretending About Meat,” by Yasmin Tayag.
Also mentioned in this week’s podcast:
- The New York Times’ “West Virginia Bans 7 Artificial Food Dyes, Citing Health Concerns,” by Alice Callahan.
- The Washington Post’s “Why I Left My Job Leading Public Health Messaging for the CDC,” by Kevin Griffis.
- Politico’s “The Limits of RFK Jr.’s Power,” by Joanne Kenen.
Click to open the transcript
Transcript: The Ax Falls at HHS
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News, and I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, March 27, at 10 a.m. As always, news happens fast — really fast this week — and things might well have changed by the time you hear this. So, here we go.
Today we are joined via videoconference by Alice Miranda Ollstein of Politico.
Alice Miranda Ollstein: Hello.
Rovner: Maya Goldman of Axios News.
Maya Goldman: Great to be here.
Rovner: And Joanne Kenen of the Johns Hopkins Bloomberg School of Public Health and Politico Magazine.
Joanne Kenen: Hi everybody.
Rovner: Later in this episode we’ll have my interview with KFF Senior Vice President Larry Levitt, who will riff on the 15th anniversary of the signing of the Affordable Care Act and what its immediate future might hold. But first, this week’s news.
So for this second week in a row, we have news breaking literally as we sit down to tape, this time in the form of an announcement from the Department of Health and Human Services with the headline “HHS Announces Transformation to Make America Healthy Again.” The plan calls for 10,000 full-time employees to lose their jobs at HHS, and when combined with early retirement and other reductions, it will reduce the department’s workforce by roughly 25%, from about 82,000 to about 62,000. It calls for creation of a new “Administration for a Healthy America” that will combine a number of existing HHS agencies, including the Health Resources and Services Administration, the Agency for Toxic Substances and Disease Registry, and the National Institute for Occupational Safety and Health under one umbrella.
Reading through the announcement, a lot of it actually seems to make some sense, as many HHS programs do overlap. But the big overriding question is: Can they really do this? Isn’t this kind of reorganization Congress’ job?
Ollstein: Congress has not stood up for itself in its power-of-the-purse role so far in the Trump administration. They have stood by, largely, the Republican majorities in the House and Senate, or they’ve offered sort of mild concerns. But they have not said, Hey guys, this is our job, all of these cuts that are happening. There’s talk of a legislative package that would codify the DOGE [Department of Government Efficiency] cuts that are already happening, rubber-stamping it after the fact. But Congress has not made moves to claw back its authority in terms of saying, Hey, we approved this funding, and you can’t just go back and take it. There’s lawsuits to that effect, but not from the members — from outside groups, from labor unions, from impacted folks, but not our dear legislative branch.
Rovner: You know, Joanne, you were there for a lot of this. We covered the creation of a lot of these agencies. Agency for Healthcare Research and Quality, I covered the creation of its predecessor agency, which there were huge compromises that went into this, lots of policymaking. It just seems that RFK [Robert F. Kennedy] Jr. going to say: We don’t actually care all these things you did. We’re just going to redo the whole thing.
Kenen: As many of the listeners know, many laws that Congress passes have to be reauthorized every five years or every 10 years. Five is the most typical, and they often don’t get around to it and they extend and blah, blah, blah, blah, blah. But basically the idea is that things do change and things do need to be reevaluated. So, normally when you do reauthorization — we all just got this press release announcing all these mergers of departments and so forth at HHS. None of us are experts in procurement and IT. Maybe those two departments do need to be merged. I mean, I don’t know. That’s the kind of thing that, reauthorization, Congress looks at and Congress thinks about. Well, and agencies and legislation do get updated. Maybe the NIH [National Institutes of Health] doesn’t need 28 institutes and they should have 15 or whatever. But it’s just sort of this, somebody coming in and waving a magic DOGE wand, and Congress is not involved. And there’s not as much public input and expert input as you’d have because Congress holds hearings and listens to people who do have expertise.
So it’s not just Congress not exercising power to make decisions. It’s also Congress not deliberating and learning. I mean all of us learned health policy partly by listening to experts at congressional panels. We listen to people at Finance, and Energy and Commerce, and so forth. So it’s not just Congress’ voice being silenced. It’s this whole review and fact-based — and experts don’t always agree and Congress makes the final call. But that’s just been short-circuited. And I mean we all know there’s duplication in government, but this isn’t the process we have historically used to address it.
Rovner: You know, one other thing, I think they’re merging agencies that are in different locations, which on the one hand might make sense. But if you have one central IT or one central procurement agency in Washington or around Washington, you’ve got a lot of these organizations that are outside of Washington. And they’re outside of Washington because members of Congress put them there. A lot of them are in particular places because they were parochial decisions made by Congress. That may or may not make sense, but that’s where they are. It might or might not make sense. Maya, sorry I interrupted you.
Goldman: No, I was just going to add to Joanne’s point. Julie, I think before we started recording you mentioned that the administration is saying: We’ve thought this all out. These are well-researched decisions. But they’ve been in office for two months. How much research can you really do in that time and how intentional can those decisions really be in that time frame?
Ollstein: Especially because all of the leaders aren’t even in place yet. Some people were just confirmed, which we’re going to talk about. Some people are on their way to confirmation but not there yet. They haven’t had the chance to talk to career staff, figure out what the redundancies are, figure out what work is currently happening that would be disrupted by various closures and mergers and stuff. So Maya’s exactly right on that.
Goldman: You know there’s — the administration chose a lead for HRSA and other offices. And so what happens to those positions now? Do they just get demoted effectively because they’re no longer heads of offices? I would be pretty—
Rovner: But we have a secretary of education whose job is to close the department down, so—.
Goldman: Good point.
Rovner: That’s apparently not unprecedented in this administration. Well, as Alice was saying, into this maelstrom of change comes those that President [Donald] Trump has selected to lead these key federal health agencies. The Senate Tuesday night confirmed policy researcher Jay Bhattacharya to head the NIH and Johns Hopkins surgeon and policy analyst Marty Makary to head the Food and Drug Administration. Bhattacharya was approved on a straight party-line vote, while Makary, who I think it’s fair to say was probably the least controversial of the top HHS nominees, won the votes of three Democrats: Minority Whip Dick Durbin of Illinois and New Hampshire’s Democrats, [Sens.] Maggie Hassan and Jeanne Shaheen, along with all of the Republicans. What are any of you watching as these two people take up their new positions?
Kenen: Well, I mean, the NIH, Bhattacharya — who I hope I’ve learned to pronounce correctly and I apologize if I have not yet mastered it — he’s really always talked about major reorganization, reprioritization. And as I said, maybe it’s time to look at some overlap, and science has changed so much in the last decade or so. I mean are the 28 — I think the number’s 28 — are the 28 current institutes the right—
Rovner: I think it’s 27.
Kenen: Twenty-seven. I mean, are there some things that need to be merged or need to be reorganized? Probably. You could make a case for that. But that’s just one thing. The amount of cuts that the administration announced before he got there, and there is a question in some things he’s hinted at, is he going to go for that? His background is in academia, and he does have some understanding of what this money is used for. We’ve talked before, when you talk to a layperson, when you hear the word “overhead,” “indirect costs,” what that conjures up to people as waste, when in fact it’s like paying for the electricity, paying for the staff to comply with the government regulations about ethical research on human beings. It’s not parties. It’s security. It’s cleaning the animal cages. It’s all this stuff. So is he going to cut as deeply as universities have been told to expect? We don’t know yet. And that’s something that every research institution in America is looking at.
The FDA, he’s a contrarian on certain things but not across the board. I mean, as you just said, Julie, he’s a little less controversial than the others. He is a pancreatic surgeon. He does have a record as a physician. He has never been a regulator, and we don’t know exactly where his contrarian views will be unconventional and where — there’s a lot of agreement with certain things Secretary Kennedy wants to do, not everything. But there is some broad agreement on, some of his food issues do make sense. And the FDA will have a role in that.
Rovner: I will say that under this reorganization plan the FDA is going to lose 3,500 people, which is a big chunk of its workforce.
Kenen: Well things like moving SAMHSA [the Substance Abuse and Mental Health Services Administration], which is the agency that works on drug abuse within and drug addiction within HHS, that’s being folded into something else. And that’s been a national priority. The money was voted to help with addiction on a bipartisan basis several times in recent years. The grants to states, that’s all being cut back. The subagency with HHS is being folded into something else. And we don’t know. We know 20,000 jobs are being cut. The 10 announced today and the 10 we already knew about. We don’t know where they’re all coming from and what happens to the expertise and experience addressing something like the addiction crisis and the drug abuse crisis in America, which is not partisan.
Rovner: All right. Well we’ll get to the cuts in a second. Also on Tuesday, the Senate Finance Committee voted, also along party lines, to advance to the Senate floor the nomination of Dr. Mehmet Oz to head the Centers for Medicare & Medicaid Services. And while he would seem likely to get confirmed by the full Senate, I did not have on my bingo card Dr. Oz’s nomination being more in doubt due to Republicans than Democrats. Did anybody else?
Ollstein: Based on our reporting, it’s not really in doubt. [Sen.] Josh Hawley has raised concerns about Dr. Oz being too squishy on abortion and trans health care, but it does not seem that other Republicans are really jumping on board with that crusade. It sort of reminds me of concerns that were raised about RFK Jr.’s background on abortion that pretty much just fizzled and Republicans overwhelmingly fell in line. And that seems to be what’s going to happen now. Although you never know.
Rovner: At least it hasn’t been, as you point out, it hasn’t failed anybody else. Well, the one nominee who did not make it through HHS was former Congressman Dave Weldon to head the CDC [Centers for Disease Control and Prevention]. So now we have a new nominee. It’s actually the acting director, Susan Monarez, who by the way has a long history in federal health programs but no history at the CDC. Who can tell us anything about her?
Goldman: She seems like a very interesting and in some ways unconventional pick, especially for this administration. She was a career civil servant, and she worked under the Obama administration. And it’s interesting to see them be OK with that, I think. And she also has a lot of health care background but not in CDC. She’s done a lot of work on AI in health care and disaster preparedness, I think. And clearly she’s been leading the CDC for the last couple months. So she knows to that extent. But it will be very interesting when she gets around to confirmation hearings to hear what her priorities are, because we really have no idea.
Rovner: Yeah, she’s not one of those good-on-Fox News people that we’ve seen so many of in this administration. So while Monarez’s nomination seems fairly noncontroversial, at least so far, the nominee to be the new HHS inspector general is definitely not. Remember that President Trump fired HHS IG Christi Grimm just days after he took office, along with the IGs of several other departments. Grimm is still suing to get her job back, since that firing violated the terms of the 1978 Inspector General Act. But now the administration wants to replace her with Thomas Bell, who’s had a number of partisan Republican jobs for what’s traditionally been a very nonpartisan position and who was fired by the state of Virginia in 1997 for apparently mishandling state taxpayer funds. That feels like it might raise some eyebrows as somebody who’s supposed to be in charge of waste, fraud, and abuse. Or am I being naive?
Goldman: My eyebrows were definitely raised when I saw that news. I, to be honest, don’t know very much about him but will be very interested to see how things go, especially given that fraud, waste, and abuse and rooting out fraud, waste, and abuse are high priorities for this administration, but also things that are very up to interpretation in a certain way.
Ollstein: Yes, although it’s clearly been very mixed on that front because the administration is also dismantling entire agencies that go after fraud and abuse—
Goldman: Exactly.
Ollstein: —like the Consumer Financial Protection Bureau. So there is some mixed messaging on that front for sure.
Rovner: Well, as Joanne mentioned, the DOGE cuts continue at the NIH. In just the last week, billions of dollars in grants have been terminated that were being used to study AIDS and HIV, covid and other potential pandemic viruses, and climate change, among other things. The NIH also closed its office studying long covid. Thank you, Alice, for writing that story. This is, I repeat, not normal. NIH only generally cancels grants that have been peer reviewed and approved for reasons of fraud or scientific misconduct, yet one termination letter obtained by Science Magazine simply stated, quote, “The end of the pandemic provides cause to terminate COVID-related grant funds.” Why aren’t we hearing more about this, particularly for members of Congress whose universities are the ones that are being cut?
Kenen: I mean, the one Republican we heard at the very beginning was [Sen.] Katie Britt because the University of Alabama is a big, excellent, and well-respected national medical and science center, and they were targeted for a lot of cuts. She’s the only Republican, really, and she got quiet. I mean, she raised her voice very loud and clear. We may go into a situation — and everybody sort of knows this is how Washington sometimes works — where individual universities will end up negotiating with NIH over their funds and that—
Rovner: Columbia. Cough, cough.
Kenen: Right. And Alabama may come out great and Columbia might not, or many other leading research institutions. But these job cuts affect people in every congressional district across the country. And the funding cuts affect every congressional district across the country. So it’s not just their constitutional responsibilities. It’s also, like, their constituents are affected, and we’re not hearing it.
Rovner: And as I point out for the millionth time, it’s not a coincidence that these things are located in every congressional district. Members of Congress, if not the ones who are currently in office then their predecessors, lobbied and worked to get these funds to their states and to their district. And yet the silence is deafening.
Ollstein: To state the obvious, one, covid is not over. People are still contracting it. People are still dying from it. But not only that, a lot of this research was about preparing for the inevitable next pandemic that we know is coming at some point and to not be caught as unawares as we were this past time, to be more prepared, to have better tools so that there don’t have to be widespread lockdowns, things can remain open because we have more effective prevention and treatment efforts. And that’s what’s being defunded here.
Kenen: The other thing is that long covid is in fact a chronic disease and even though it’s caused by an infectious disease, a virus. But people have long covid but it is a chronic disease, and HHS says that’s their priority, chronic disease, but they’re not including long covid. And there’s also more and more. When we think of long covid, we think of brain fog and being short of breath and tired and unable to function. There’s increasing evidence or conversation in the medical world about other problems people have long-term that probably stem from covid infections or multiple covid infections. So this is affecting millions of Americans as a chronic disease that is not well understood, and we’ve just basically said, That one doesn’t count, or: We’re not going to pay attention to that one. We’re going to, you know, we’re looking at diabetes. Yeah, we need to look at diabetes. That’s one of the things that Kennedy has bipartisan support. This country does not eat well. I wrote about this about a week ago. But what he can and can’t do, because he can’t wave a magic wand and have us all eating well. But it’s very selective in how we’re defining both the causes of diseases and what diseases we’re prioritizing. We basically just shrunk addiction.
Goldman: In the press release announcing the reorganization this morning, there was a line talking about how the HHS is going to create this new Administration for a Healthy America to investigate chronic disease and to make sure that we have, I think it was, wholesome food, clean water, and no environmental toxins, in order to prevent chronic disease. And those are the only three things that it mentions that lead to chronic disease.
Rovner: And none of which are under HHS’ purview.
Goldman: Right, right. Yeah.
Rovner: With the exception of—
Goldman: There are things that HHS does in that space. But yeah, we’re being very selective about what constitutes a chronic disease and what causes a chronic disease. If you’re trying to actually solve a problem, maybe you should be more expansive.
Kenen: So HHS has some authority over food, not significant authority of it, but it is shared with the USDA [U.S. Department of Agriculture]. Like school lunches are USDA, the nutritional guidelines are shared between USDA and HHS, things like that. So yeah, it has some control about, over food but not entirely control over food.
And then EPA [Environmental Protection Agency], which has also been completely reoriented to be a pro-fossil-fuel agency, is in charge of clean water and the environmental contaminants. That’s not an HHS bailiwick. And Kennedy is not aligned with other elements of the administration on environmental issues. And also genetics, right? Genetics is also, you know, who knows? That’s NIH? But who knows what’s going to happen to the National Cancer Institute and other genetic research at NIH? We don’t know.
Rovner: Yes. Clearly much to be determined. Well, speaking of members of Congress whose states and districts are losing federal funds, federal aid is also being cut by the CDC. In a story first reported by NBC News, CDC is reportedly clawing back more than $11 billion in covid-related grants. Among other things, that’s impacting funding that was being used in Texas to fight the ongoing measles outbreak. How exactly does clawing back this money from state and local public health agencies make America healthy again?
Goldman: That’s a great question, and I’m curious to see how it plays out. I don’t have the answer.
Rovner: And it’s not just domestic spending. The fate of PEPFAR [the President’s Emergency Plan for AIDS Relief], the international AIDS/HIV program that’s credited with saving more than 20 million lives, remains in question. And The New York Times has gotten hold of a spreadsheet including more global health cuts, including those for projects to fight malaria and to pull the U.S. out of Gavi. That’s the global vaccine alliance that’s helped vaccinate more than 1.1 billion children in 78 countries. Wasn’t there a court order stopping all of these cuts?
Ollstein: So there was for some USAID [U.S. Agency for International Development] work, but not all of these things fall under that umbrella. And that is still an ongoing saga that has flipped back and forth depending on various rulings. But I think it’s worth pointing out, as always, that infectious diseases don’t respect international borders, and any pullback on efforts to fight various things abroad inevitably will impact Americans as well.
Rovner: Yeah. I mean, we’ve seen these measles cases obviously in Texas, but now we’re getting measles cases in other parts of the country, and many of them are people coming from other countries. We had somebody come through Washington, D.C.’s Union Station with measles, and we’ve had all of these alerts. I mean, this is what happens when you don’t try and work with infectious diseases where they are, then they spread. That’s kind of the nature of infectious disease.
Well, at the same time, HHS Secretary RFK Jr. is putting his Make America Healthy Again agenda into practice in smaller ways as well. First up, remember that study that Kennedy promised again to look into any links between childhood vaccines and autism? It will reportedly be led by a vaccine skeptic who was disciplined by the Maryland Board of Physicians for practicing medicine without a license and who has pushed the repeatedly debunked assertion that autism can be caused by the preservative thimerosal, which used to be used in childhood vaccines but has long since been discontinued. One autism group referred to the person who’s going to be running this study as, quote, “a known conspiracy theorist and quack.” Sen. [Bill] Cassidy seemed to promise us that this wasn’t going to happen.
Kenen: Well, we think that Sen. Cassidy was promised it wouldn’t happen, and it’s all happening. And in fact, when a recent hearing, he was very outspoken that there’s no need to research the autism link, because it’s been researched over and over and over and over and over again and there’s a lot of reputable scientific evidence establishing that vaccination does not cause autism. We don’t know what causes autism, so—
Rovner: But we know it’s not thimerosal.
Kenen: Right, which has been removed from many vaccines, in fact, and autism rates went up. So Cassidy has not come out and said, Yeah, I’m the guy who pulled the plug on Weldon. But it’s sort of obvious that he had, at least was, a role in. It is widely understood in Washington that he and a few other Republicans, [Sens. Lisa] Murkowski and [Susan] Collins, I believe — I think Murkowski said it in public — said that the CDC could not go down that route.
Rovner: Well, I would like to be inadvertently invited to the Signal chat between Secretary Kennedy and Sen. Cassidy. I would very much wish to see that conversation.
Meanwhile, in Texas, where HHS just confiscated public health funding, as we said, a hospital in Lubbock says it’s now treating children with liver damage from too much vitamin A, which Secretary Kennedy recommended as a way to prevent and or treat measles. Which it doesn’t, by the way. But that points to, that some of these — I hesitate of how to describe these people who are “making America healthy again.” But some of the things that they point to can be actively dangerous, not just not helpful.
Goldman: Yeah. And I think it also shows how much messaging from the top matters, right? People are listening to what Secretary Kennedy says, which makes sense because he’s the secretary of health and human services. But if he’s pedaling misinformation or disinformation, that can have real harmful effects on people.
Kenen: And his messages are being amplified even if some people are not, their parents, who aren’t maybe directly tuned in to what Kennedy personally is saying, but they follow various influencers on health who are then echoing what Kennedy’s saying about vitamin A. Yeah, we all need vitamin A in our diet. It’s something, part of healthy nutrition. But this supplement’s unnecessary, or excess supplements, vitamin A or cod liver oil or other things that can make them sick, including liver damage. And that’s what we’re seeing now. Vitamin A does have a place in measles under very specific circumstances, under medical supervision in individual cases. But no, people should not be going to the drugstore and pouring huge numbers of tablets of vitamin C down their children’s throat. It’s dangerous.
Rovner: And actually the head of communications at the CDC not only quit his job this week but wrote a rather impassioned op-ed in The Washington Post, which I will post in our show notes, talking about he feels like he cannot work for an agency that is not giving advice that is based in science and that that’s what he feels right now. Again, that’s before we get a new head of the CDC. Well, MAHA is apparently spreading to the states as well. West Virginia Republican Gov. Patrick Morrisey this week signed a bill to ban most artificial food coloring and two preservatives in all foods sold in the state starting in 2028. Nearly half the rest of the states are considering similar types of bans. But unless most of those other states follow, companies aren’t going to remake their products just for West Virginia, right?
Kenen: West Virginia is not big enough, but they sometimes do remake their products for California, which is big. The whole food additive issue is, traditionally the food manufacturers have had a lot of control over deciding what’s safe. It’s the industry that has decided. Kennedy has some support across the board and saying that’s too loose and we should look at some of these additives that have not been examined. There are others, including some preservatives, that have been studied and that are safe. Some preservatives have not been studied and should be studied. There are others that have been studied and are safe and they keep food from going rotten or they can prevent foodborne disease outbreaks. Something that does make our food healthy, we probably want to keep them in there. So, and are there some that—
Rovner: I think people get mixed up between the dyes and the preservatives. Dyes are just to make things look more attractive. The preservatives were put there for a reason.
Kenen: Right. And there’s some healthy ways of making dyes, too, if you need your food to be red. There’s berry abstracts instead of chemical extracts. So things get overly simplified in a way that does not end up necessarily promoting health across the board.
Rovner: Well, not all of the news is coming from the Trump administration. The Supreme Court next week will hear a case out of South Carolina about whether Medicaid recipients can sue to enforce their right to get care from any qualified health care providers. But this is really another case about Planned Parenthood, right, Alice?
Ollstein: Yep. If South Carolina gets the green light to kick Planned Parenthood out of its Medicaid program, which is really what is at the heart of this case, even though it’s sort of about whether beneficiaries can sue if their rights are denied. A right isn’t a right if you can’t enforce it, so it’s expected that a ruling in that direction would cause a stampede of other conservative states to do the same, to exclude Planned Parenthood from their Medicaid programs. Many have tried already, and that’s gone around and around in the courts for a while, and so this is really the big showdown at the high court to really decide this.
And as I’ve been writing about, this is just one of many prongs of the right’s bigger strategy to defund Planned Parenthood. So there are efforts at the federal level. There are efforts at the state level. There are efforts in the courts. They are pushing executive actions on that front. We can talk. There was some news on Title X this week.
Rovner: That was my next question. Go ahead.
Ollstein: Some potential news.
Rovner: What’s happening with Title X?
Ollstein: Yeah. So HHS told us when we inquired that nothing’s final yet, but they’re reviewing tens of millions of Title X federal family planning grants that currently go to some Planned Parenthood affiliates to provide subsidized contraception, STI [sexually transmitted infection] screenings, various non-abortion services. And so they are reviewing those grants now. They are supposed to be going out next week, so we’ll have to see what happens there. There was some sort of back-and-forth in the reporting about whether they’re going to be cut or not.
Rovner: What surprises me about the Title X grant, and there has been, there have been efforts, as you point out, going back to the 1980s to kick Planned Parenthood out of the Title X program. That’s separate from kicking Planned Parenthood out of Medicaid, which is where Planned Parenthood gets a lot more money.
But the first Trump administration did kick Planned Parenthood out of Title X, and they went through the regulatory process to do it. And then the Biden administration went through the regulatory process to rescind the Trump administration regulations that kicked them out. Now it looks like the Trump administration thinks that it can just stop it without going through the regulatory process, right?
Ollstein: That’s right. So not only are they going around Congress, which approves Title X funding every year, they are also going around their own rulemaking and just going for it. Although, again, it has not been finally announced whether or not there will be cuts. They’re just reviewing these grants.
Rovner: But I repeat for those in the back, this is not normal. It’s not how these things are supposed to work it.
Kenen: It’s normal now, Julie.
Rovner: Yeah, clearly it’s becoming normal. Well, finally this week, another case of a woman arrested for a poor pregnancy outcome. This happened in Georgia where the woman suffered a natural miscarriage, not an abortion, which was confirmed by the medical examiner, but has been arrested on charges of improperly disposing of the fetal remains. Alice, this is turning into a trend, right?
Ollstein: Yes. And it’s important for people to remember that this was happening before Dobbs. This was happening when Roe v. Wade was still in place. This has happened since then in states where abortion is legal. Some prosecutors are finding other ways to charge people. Whether it’s related to, yeah, the disposal of the fetus, whether it’s related to substance abuse, substance use during pregnancy, even sometimes the use of substances that are actually legal, but people have been charged, arrested for using them during pregnancy. So yes, it’s important to remember that even if there’s not a quote-unquote “abortion ban” on the books, there are still efforts underway in many places to criminalize pregnancy loss however it happens, naturally or via some abortifacient method.
Rovner: Well, something else we’ll be keeping an eye on. All right, that’s as much news as we have time for this week. Now, we will play my interview with KFF’s Larry Levitt. Then we’ll come back and do our extra credits.
So, last Sunday was the 15th anniversary of President Barack Obama’s signing of the original Affordable Care Act. And before you ask, yes, I was there in the White House East Room that day. Anyway, to discuss what the law has meant to the U.S. health system over the last decade and a half and what its future might be, I am so pleased to welcome back to the podcast my KFF colleague Larry Levitt, executive vice president for health policy.
Larry, thanks for joining us again.
Larry Levitt: Oh, thanks for having me.
Rovner: So, [then-House Speaker] Nancy Pelosi was mercilessly derided when she said that once the American people learned exactly what was in the ACA, they would come to like it. But that’s exactly what’s happened, right?
Levitt: It is. Yes. I think people took her comments so out of context, but the ACA was incredibly controversial and divisive when it was being debated. Frankly, after a pass, the ACA became pretty unpopular. If you go back to 2014, just before the main provisions of the ACA were being implemented, there was all this controversy over the individual mandate, over people’s plans being canceled because they didn’t comply with the ACA’s rules. And then, of course, healthcare.gov, the website, didn’t work. So the ACA was very underwater in public opinion. And even after it first went into effect and people started getting coverage, that didn’t necessarily turn around immediately, there was still a lot of divisiveness over the law.
What changed is, No. 1, over time, more and more people got covered, people with preexisting conditions, people who couldn’t afford health insurance, people who turned 26 or could stay on their parents’ plans until 26 and then could enroll in the ACA or Medicaid after turning 26. All these people got coverage and started to see the benefits of the law. The other thing that happened was in 2017, Republicans tried unsuccessfully to repeal and replace the ACA, and people really realized what they could be missing if the law went away.
Rovner: So what’s turned out to be the biggest change to the health care system as a result of the ACA? And is it what you originally thought it would be?
Levitt: Well, yeah, in this case it was not a surprise, I think. The biggest change was the number of people getting covered and a big decrease in the number of people uninsured. We have been at the lowest rate of uninsurance ever recently due to the ACA and some of the enhancements, which we’ll probably talk about. And that was what the law was intended to do, was to get more people covered. And I think you’d have to call that a success, in retrospect.
Rovner: I will say I was surprised by how much Medicaid dominated the increased coverage. I know now it’s sort of balanced out because of reductions in premiums for private coverage, I think in large part. But I think during the 2017 fight to undo the ACA, that was the first time since I’ve been covering Medicaid that I think people really realized how big and how important Medicaid is to the health care system.
Levitt: No, that’s right. I mean the ACA marketplace, healthcare.gov, the individual mandate, preexisting condition protections, I mean, those are the things that got a lot of the public attention. But in fact, yeah, in the early years of the ACA, I mean really up until just the last couple years, the Medicaid expansion in the ACA was really the engine of coverage. And that’s not what a lot of people expected. In fact, Congressional Budget Office in their original projections kind of got that wrong, too.
Rovner: So what was the biggest disappointment about something the ACA was supposed to do but didn’t do or didn’t do very well?
Levitt: Yeah, I mean, I would have to point to health care costs as the biggest disappointment. The ACA really wasn’t intended to address health care costs head-on. And that was both a policy judgment but also a political decision. If you go back to the debate over the Clinton health plan in the early ’90s, which failed spectacularly — you and I were both there — it addressed health care costs aggressively, took on every segment of the health care industry, and died under that political weight. The political judgment of Obama and Democrats in Congress with the ACA was to not take on those vested health care interests and not really address health care costs head-on. That’s what enabled it to get passed. But it sort of lacked teeth in that regard. There were some things in the ACA like expansion of ACOs, accountable care organizations, which maybe had some promise but frankly have not done a whole lot.
Rovner: And of course, Congress undoing what teeth there were in the ensuing years probably didn’t help very much, either.
Levitt: No. I mean there was this provision in the ACA called the Cadillac plan tax, right? The idea was to tax so-called Cadillac health plans, very generous health plans. That probably would’ve had an effect. I’m not sure it would’ve done what people intended for it to do. I mean, I think it would’ve actually shifted costs to workers and caused deductibles to rise even higher. But no one but economists liked that Cadillac plan tax, and it was repealed.
Rovner: So, as you mentioned, you and I are both also veterans of the 1993, 1994 failed effort by President Bill Clinton to overhaul the nation’s health care system, which, like the fight over the ACA, featured large-scale, deliberate mis- and disinformation by opponents about what a major piece of health legislation could do. In fact, and I have done lots of stories on this, scare tactics about the possible impact of providing universal health insurance coverage date back to the early 1900s and have been a feature of every single major health care debate since then. What did we learn from the ACA debate about combating this kind of deliberate misinformation?
Levitt: Yeah, you’re so right about the disinformation, and I was actually looking yesterday — we have a timeline of health policy over the decades in our KFF headquarters in San Francisco, and we have an ad up there from the debate over the Truman health plan. You and I were not there for that debate.
Rovner: Thank you.
Levitt: And the AMA [American Medical Association] opposed that as socialized medicine and ran these ads featuring robots who were going to be your doctor if the Truman plan passed. So this is certainly nothing new. And we saw it in the ACA with death panels, right? I mean, which just spread like wildfire through the media and over social media. I would kind of hope we learned some lessons from the ACA. I’m not sure we have. And I kind of worry that with declining trust in institutions, particularly government institutions, I just wonder whether we’ll get back to a place where, yeah, we’ll disagree about policy. There will be spin, there will be scare tactics, but at least there’s some trusted source of facts and data that we can rely on, and I’m not so hopeful there.
Rovner: Somebody asked former [HHS] Secretary Kathleen Sebelius at a 15th-anniversary event what she regretted most about not having in the ACA, and she said, With all the talk of our actually taking over the health care system, we should have just taken over the health care system, since that’s what everybody was accusing it of. It might’ve worked better.
Levitt: Yeah, there is — we could have a whole other session on “Medicare for All” and single payer and the pros and cons of that. But one thing I think we did learn from the ACA, that complexity is just a huge problem. Even what’s supposed to be the simplest part of our health care system now, Medicare, has become incredibly complex with Part A and Part B and Part C and Part D. Seniors kind of scratch their heads trying to figure out what to do, and the ACA even more so.
And I think back to your original question, part of what made the ACA so hard for people to grasp is there was not one single, Oh, I’m going to sign up for the ACA. There were so many pieces of it. And over time, I’m not even sure people identify those pieces with the ACA anymore.
Rovner: Yeah. Oh, no, I am surprised at how many younger people have no idea of what the insurance market was like before the ACA and how many people were simply redlined out of getting coverage.
Levitt: Right. No. I mean, once you fix those problems, then people don’t see them anymore.
Rovner: So let’s look forward quickly. It seemed at least for a while after the Republicans failed in 2017 to repeal and replace the law that efforts to undo it were finally over. But while this administration isn’t saying directly that they want to end it, they do have some big targets for undoing big pieces of it. What are some of those and what are the likelihood of them happening?
Levitt: Yeah, in some ways we have an ACA repeal-and-replace debate going on right now, just not in name. And there are really kind of two big pieces on the table. One, of course, is potential cuts to Medicaid. The House has passed a budget resolution calling for $880 billion in cuts, by the Energy and Commerce Committee, which has jurisdiction over Medicaid. The vast majority of those cuts would have to be in Medicaid. The math is simply inescapable. And a big target on the table is that expansion of Medicaid that was in the ACA.
And interestingly, you’re even hearing Republicans on the Hill talking about repealing the enhanced federal matching payments for the ACA Medicaid expansion and saying: Well, that’s not Medicaid cuts. That’s Obamacare. That’s not Medicaid. But 20 million people are covered under that Medicaid expansion. So it would lead to the biggest increase in the number of people uninsured we’ve ever had, if that gets repealed.
The other issue really has not gotten a lot of attention yet this year, which is the extra premium assistance that was passed under [President Joe] Biden and by Democrats in Congress. And that’s led to a dramatic increase in ACA marketplace enrollment. ACA enrollment has more than doubled to 24 million since 2020. Those subsidies expire at the end of this year. So if Congress does nothing, people would be faced with very big out-of-pocket premium increases. And I suspect it’s going to get more attention as we get closer to the end of the year, but so far there hasn’t been a big debate over it yet.
Rovner: Well, we’ll continue to talk about it. Larry Levitt, thank you so much.
Levitt: Oh, thanks. Great conversation.
Rovner: OK, we’re back. Now it’s time for our extra-credit segment. That’s where we each recognize the story we read this week we think you should read, too. Don’t worry if you miss it. We will put the links in our show notes on your phone or other mobile device. Joanne, why don’t you go first this week?
Kenen: There’s a piece in The Atlantic this week called “America Is Done Pretending About Meat,” by Yasmin Tayag, and it’s basically saying that half of the people who said they were vegan or vegetarian were lying and that meat is very much back in fashion. That the new pejorative term — some of us may remember from 20 years or so ago, the “quiche eaters” —now it’s the “soy boy.” And that one of the new “in” foods, and I think this is the first for the podcast to use the phrase, raw beef testicles. So when we’re talking about political red meat, it’s not just political red meat. America is, we’re eating a lot more meat than we said we did, and we’re no longer saying that we’re not eating it.
Rovner: Real red meat for the masses.
Ollstein: For what it’s worth, “soy boy” has been a slur since the Obama administration.
Kenen: Well, it’s just new to me. Thank you. I welcome the—
Ollstein: I unfortunately have been in the online fever swamps where people say things like that.
Kenen: Thank you, Alice. Now I know.
Rovner: Maya, why don’t you go next?
Goldman: My extra credit is a KFF Health News article by Rachana Pradhan and Aneri Pattani called “‘I Am Going Through Hell’: Job Loss, Mental Health, and the Fate of Federal Workers.” And I think it’s just worth remembering that there are real consequences, real mental health consequences to mass upheaval at the scale of what’s going on in the federal government right now with so many people losing their jobs and just not sure if their jobs are stable, especially in light of this morning’s news about HHS reorganizations. But also I think this article does a really good job of highlighting how this chaos and instability is only going to exacerbate already ongoing mental health crises that some of these workers that have been laid off were trying to help solve. And so it’s just this cycle that keeps running through. It’s worth remembering.
Rovner: The chaos is the point. Alice.
Ollstein: So, I have a piece from the New York Times Wirecutter section called “23andMe Just Filed for Bankruptcy. You Should Delete Your Data Now.” And it’s what it says. The company that millions and millions of people have sent samples of their DNA to over the years to find out what percent European they are and all this stuff and their propensity for various inherited diseases, that company is going bankrupt, and there is the expectation that it will be sold off for parts, including people’s very sensitive DNA. And the article points out that because they are not a health care provider, they are not subject to HIPAA [Health Insurance Portability and Accountability Act]. And so many elected officials and privacy advocates are recommending that people, very quickly, if they have given their DNA to this company, go and delete their information now before it gets sold off to who knows who.
Rovner: And for who knows what reason. My extra credit this week is something I really did think at first was from The Onion. It’s actually from CNN, and it’s called “State Lawmakers Are Looking to Ban Non-Existent ‘Chemtrails.’ It Could Have Real-Life Side Effects,” by Ramishah Maruf and Brandon Miller, who’s a CNN meteorologist. It seems that several states are moving to ban those white lines the jets leave behind them, on the theory that they are full of toxic chemicals and/or intended to manipulate the weather. In fact, they’re mostly just water vapor. They’re called contrails because the con is for condensation. But these laws could outlaw some new types of technologies that are aimed at addressing things like climate change. Clearly we need to teach more science along with more civics.
OK, that is this week’s show. As always, if you enjoy the podcast, you can subscribe wherever you get your podcast. We’d appreciate it if you left us a review. That helps other people find us, too. Thanks, as always, to our producer, Francis Ying, and our editor, Emmarie Huetteman. As always, you could email us your comments or questions. We’re at whatthehealth@kff.org. Or you can still find me at X, @jrovner, and at Bluesky, @julierovner. Where are you folks hanging these days? Maya?
Goldman: I am on X and Bluesky. If you search Maya Goldman, you’ll find me. And also increasingly on LinkedIn. Find me there.
Rovner: Hearing that a lot. Alice.
Ollstein: I am on X, @AliceOllstein, and Bluesky, @alicemiranda.
Rovner: Joanne.
Kenen: I’m mostly at Bluesky, and I’m also using LinkedIn a lot. @joannekenen at Bluesky. LinkedIn is reverberating more.
Rovner: All right, we’ll be back in your feed next week with still more breaking news. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
3 months 4 weeks ago
Courts, Health Industry, Multimedia, Public Health, States, Abortion, CDC, Georgia, HHS, KFF Health News' 'What The Health?', Misinformation, NIH, Podcasts, Pregnancy, reproductive health, texas, Trump Administration, U.S. Congress, vaccines, Women's Health
KFF Health News' 'What the Health?': Federal Health Work in Flux
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
Two months into the new administration, federal workers and contractors remain off-balance as the Trump administration ramps up its efforts to cancel jobs and programs — even as federal judges declare many of those efforts illegal and/or unconstitutional.
As it eliminates programs deemed duplicative or unnecessary, however, President Donald Trump’s Department of Government Efficiency is also cutting programs and workers aligned with Health and Human Services Secretary Robert F. Kennedy Jr.’s “Make America Healthy Again” agenda.
This week’s panelists are Julie Rovner of KFF Health News, Jessie Hellmann of CQ Roll Call, Sarah Karlin-Smith of the Pink Sheet, and Rachel Roubein of The Washington Post.
Panelists
Jessie Hellmann
CQ Roll Call
Sarah Karlin-Smith
Pink Sheet
Rachel Roubein
The Washington Post
Among the takeaways from this week’s episode:
- Kennedy’s comments this week about allowing bird flu to spread unchecked through farms provided another example of the new secretary of health and human services making claims that lack scientific support and could instead undermine public health.
- The Trump administration is experiencing more pushback from the federal courts over its efforts to reduce and dismantle federal agencies, and federal workers who have been rehired under court orders report returning to uncertainty and instability within government agencies.
- The second Trump administration is signaling it plans to dismantle HIV prevention programs in the United States, including efforts that the first Trump administration started. A Texas midwife is accused of performing illegal abortions. And a Trump appointee resigns after being targeted by a Republican senator.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: The Washington Post’s “The Free-Living Bureaucrat,” by Michael Lewis.
Rachel Roubein: The Washington Post’s “Her Research Grant Mentioned ‘Hesitancy.’ Now Her Funding Is Gone.” by Carolyn Y. Johnson.
Sarah Karlin-Smith: KFF Health News’ “Scientists Say NIH Officials Told Them To Scrub mRNA References on Grants,” by Arthur Allen.
Jessie Hellmann: Stat’s “NIH Cancels Funding for a Landmark Diabetes Study at a Time of Focus on Chronic Disease,” by Elaine Chen.
Also mentioned in this week’s podcast:
- The Wall Street Journal’s “Trump Administration Weighing Major Cuts to Funding for Domestic HIV Prevention,” by Liz Essley White, Dominique Mosbergen, and Jonathan D. Rockoff.
- The Washington Post’s “Disabled Americans Fear Losing Protections if States’ Lawsuit Succeeds,” by Amanda Morris.
click to open the transcript
Transcript: Federal Health Work in Flux
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello, and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News, and I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, March 20, at 10 a.m. As always, news happens fast and things might have changed by the time you hear this. So, here we go.
Today we are joined via videoconference by Rachel Roubein of The Washington Post.
Rachel Roubein: Hi.
Rovner: Sarah Karlin-Smith of the Pink Sheet.
Sarah Karlin-Smith: Hi, everybody.
Rovner: And Jessie Hellmann of CQ Roll Call.
Jessie Hellmann: Hello.
Rovner: No interview today, but, as usual, way more news than we can get to, so let us jump right in. In case you missed it, there’s a bonus podcast episode in your feed. After last week’s Senate Finance Committee confirmation hearing for Dr. Mehmet Oz to head the Centers for Medicare & Medicaid Services, my KFF Health News colleagues Stephanie Armour and Rachana Pradhan and I summarized the hearing and caught up on all the HHS [Department of Health and Human Services] nomination actions. It will be the episode in your feed right before this one.
So even without Senate-confirmed heads at — checks notes — all of the major agencies at HHS, the department does continue to make news. First, Robert F. Kennedy Jr., the new HHS secretary, speaks. Last week it was measles. This week it was bird flu, which he says should be allowed to spread unchecked in chicken flocks to see which birds are resistant or immune. This feels kind of like what some people recommended during covid. Sarah, is there any science to suggest this might be a good idea?
Karlin-Smith: No, it seems like the science actually suggests the opposite, because doctors and veterinary specialists are saying basically every time you let the infection continue to infect birds, you’re giving the virus more and more chances to mutate, which can lead to more problems down the road. The other thing is they were talking about the way we raise animals, and for food these days, there isn’t going to be a lot of genetic variation for the chickens, so it’s not like you’re going to be able to find a huge subset of them that are going to survive bird flu.
And then the other thing I thought is really interesting is just it doesn’t seem economically to make the most sense either as well, both for the individual farmers but then for U.S. industry as a whole, because it seems like other countries will be particularly unhappy with us and even maybe put prohibitions on trading with us or those products due to the spread of bird flu.
Rovner: Yeah, it was eyebrow-raising, let us say. Well, HHS this week also announced its first big policy effort, called Operation Stork Speed. It will press infant formula makers for more complete lists of ingredients, increase testing for heavy metals in formula, make it easier to import formula from other countries, and order more research into the health outcomes of feeding infant formula. This feels like maybe one of those things that’s not totally controversial, except for the part that the FDA [Food and Drug Administration] workers who have been monitoring the infant formula shortage were part of the big DOGE [Department of Government Efficiency] layoffs.
Roubein: I talked to some experts about this idea, and, like you said, they thought it kind of sounded good, but they basically needed more details. Like, what does it mean? Who’s going to review these ingredients? To your point, some people did say that the agency would need to staff up, and there was a neonatologist who is heading up infant formula that was hired after the 2022 shortage who was part of the probationary worker terminations. However, when the FDA rescinded the terminations of some workers, so, that doctor has been hired back. So I think that’s worth noting.
Rovner: Yes. This is also, I guess, where we get to note that Calley Means, one of RFK Jr.’s, I guess, brain trusts in the MAHA movement, has been hired as, I guess, in an Elon Musk-like position in the White House as an adviser. But this is certainly an area where he would expect to weigh in.
Hellmann: Yeah, I saw he’s really excited about this on Twitter, or X. There’s just been concerns in the MAHA movement, “Make America Healthy Again,” about the ingredients that are in baby formula. And the only thing is I saw that he also retweeted somebody who said that “breast is best,” and I’m just hoping that we’re not going back down that road again, because I feel like public health did a lot of work in pushing the message that formula and breast milk is good for the child, and so that’s just another angle that I’ve been thinking about on this.
Rovner: Yes, I think this is one of those things that everybody agrees we should look at and has the potential to get really controversial at some point. While we are on the subject of the federal workforce and layoffs, federal judges and DOGE continue to play cat-and-mouse, with lots of real people’s lives and careers at stake. Various judges have ordered the reinstatement, as you mentioned, Rachel, of probationary and other workers. Although in many cases workers have been reinstated to an administrative leave status, meaning they get put back on the payroll and they get their benefits back, but they still can’t do their jobs. At least one judge has said that does not satisfy his order, and this is all changing so fast it’s basically impossible to keep up. But is it fair to say that it’s not a very stable time to be a federal worker?
Karlin-Smith: That’s probably the nicest possible way to put it. When you talk to federal workers, everybody seems stressed and just unsure of their status. And if they do have a job, it’s often from their perspective tougher to do their job lately, and then they’re just not sure how stable it is. And many people are considering what options they have outside the federal government at this point.
Rovner: So for those lucky federal workers who do still have jobs, the Trump administration has also ordered everyone back to offices, even if those offices aren’t equipped to accommodate them. FDA headquarters here in Maryland’s kind of been the poster child for this this week.
Karlin-Smith: Yeah, FDA is an interesting one because well before covid normalized working from home and transitioned a lot of people to working from home, FDA’s headquarters couldn’t accommodate a lot of the new growth in the agency over the years, like the tobacco part of the FDA. So it was typical that people at least worked part of their workweek at home, and FDA really found once covid gave them additional work-from-home flexibilities, they were able to recruit staff they really, really needed with specialized degrees and training who don’t live near here, and it actually turned out to be quite a benefit from them.
And now they’re saying everybody needs to be in an office five days a week, and you have people basically cramped into conference rooms. There’s not enough parking. People are trying to review technical scientific data, and you kind of can’t hear yourself think. Or you’re a lawyer — I heard of a situation where people are basically being told, Well, if you need to do a private phone call because of the confidentiality around what you’re doing, go take the call in your car. So I think in addition to all of the concerns people have around the stability of their jobs, there’s now this element of, on a personal level, I think for many of them it’s just made their lives more challenging. And then they just feel like they’re not actually able to do, have the same level of efficiency at their work as they normally would.
Rovner: And for those who don’t know, the FDA campus is on a former military installation in the Maryland suburbs. It’s not really near any public transportation. So you pretty much have to drive to get there. And I think that the parking lots are not that big, because, as you pointed out, Sarah, the workforce is now bigger than the headquarters was created to accommodate it. And we’re seeing this across the government. This week it happened to be FDA. You have to ask the question: Is this really just an effort to make the government not work, to make federal workers, if they can’t fire them, to make them quit?
Hellmann: I definitely think that’s part of the underlying goal. If you see some of the stuff that Elon Musk says about the federal workforce, it’s very dismissive. He doesn’t seem to have a lot of respect for the civil servants. And they’ve been running into a lot of pushback from federal judges over many lawsuits targeting these terminations. And so I think just making conditions as frustrating as possible for some of these workers until they quit is definitely part of the strategy.
Roubein: And I think this is overlaid with the additional buyout offers, the additional early retirement offers. There’s also the reduction-in-force plans that federal workers have been unnerved about, bracing for future layoffs. So it’s very clear that they want to shrink the size of the federal workforce.
Rovner: Yeah, we’ve seen a lot of these people, I’ve seen interviews with them, who are being reinstated, but they’re still worried that now they’re going to be RIF-ed. They’re back on the payroll, they’re off the payroll. I mean there’s nothing — this does not feel like a very efficient way to run the federal government.
Karlin-Smith: Right. I think that’s what a lot of people are talking about is, again, going back to offices, for many of these people, is not leading to productivity. I talked to one person who said: I’m just leaving my laptop at the office now. I’m not going to take it home and do the extra hours of work that they might’ve normally gotten from me. And that includes losing time to commute. FDA is paying for parking-garage spaces in downtown Silver Spring [Maryland] near the Metro so that they can then shuttle people to the FDA headquarters. I’ve taken buses from that Metro to FDA headquarters. In traffic, that’s a 30-minute drive. They’re spending money on things that, again, I think are not going to in the long run create any government efficiency.
And in fact, I’ve been talking to people who are worried it’s going to do the opposite, that drug review, device review, medical product review times and things like that are going to slow. We talked about food safety. I think The New York Times had a really good story this week about concerns about losing the people. We need to make sure that baby formula is actually safe. So there’s a lot of contradictions in the messaging of what they’re trying to accomplish and how the actions actually are playing out.
Rovner: Well, and finally, I’m going to lay one more layer on this. There’s the question of whether you can even put the toothpaste back in the tube if you wanted to. After weeks of back-and-forth, the federal judge ruled on Tuesday that the dissolution of USAID [the U.S. Agency for International Development] was illegal and probably unconstitutional, and ordered email and computer access restored for the remaining workers while blocking further cuts. But with nearly everybody fired, called back from overseas, and contracts canceled, USAID couldn’t possibly come close to doing what it did before DOGE basically took it apart, right?.
Karlin-Smith: You hear stories of if someone already takes a new job, they’re lucky enough to find a new job, why are they going to come back? Again, even if you’re brought back, my expectation is a lot of people who have been brought back are probably looking for new jobs regardless because you don’t have that stability. And I think the USAID thing is interesting, too, because again, you have people that were working in all corners of the world and you have partnerships with other countries and contractors that have to be able to trust you moving forward. And the question is, do those countries and those organizations want to continue working with the U.S. if they can’t have that sort of trust? And as people said, the U.S. government was known as, they could pay contractors less because they always paid you. And when you take that away, that creates a lot of problems for negotiating deals to work with them moving forward.
Rovner: And I think that’s true for federal workers, too. There’s always been the idea that you probably could earn more in the private sector than you can working for the federal government, but it’s always been a pretty stable job. And I think right now it’s anything but, so comes the question of: Are we deterring people from wanting to work for the federal government? Eventually one would assume there’s still going to be a federal government to work for, and there may not be anybody who wants to do it.
Roubein: Yeah, you saw various hiring authorities given to try and recruit scientists and other researchers who make a lot, lot more in the public health sector, and some of those were a part of the probationary workforce because they had been hired recently under those authorities.
Rovner: Yeah, and now this is all sort of coming apart. Well, meanwhile, the cuts are continuing even faster than federal judges can rule against them. Last week, the administration said it would reduce the number of HHS regional offices from 10 to four. Considering these are where the department’s major fraud-fighting efforts take place, that doesn’t seem a very effective way of going after fraud and abuse in programs like Medicare and Medicaid. Those regional offices are also where lots of beneficiary protections come from, like inspections of nursing homes and Head Start facilities. How does this serve RFK Jr.’s Make America Healthy Again agenda?
Karlin-Smith: I think it’s not clear that it does, right? You’re talking about, again, the Department of Government Efficiency has focused on efficiency, cost savings, and Medicare and Medicaid does a pretty good job of fighting fraud and making HHS OIG [Office of Inspector General], all those organizations, they collect a lot of money back. So when you lose people—
Rovner: And of course the inspector general has also been laid off in all of this.
Karlin-Smith: Right. It’s not clear to me, I think one of the things with that whole reorganization of their chief counsel is people are suggesting, again, this is sort of a power move of HHS wanting to get a little bit more control of the legal operations at the lower agencies, whether it’s NIH [the National Institutes of Health] or FDA and so forth. But, right, it’s reducing head count without really thinking about what people’s roles actually were and what you lose when you let them go.
Rovner: Well, the Trump administration is also continuing to cut grants and contracts that seem like they’d be the kind of things that directly relate to Make America Healthy Again. Jessie, you’ve chosen one of those as your extra credit this week. Tell us about it.
Hellmann: Yeah. So my story is from Stat [“NIH Cancels Funding for a Landmark Diabetes Study at a Time of Focus on Chronic Disease”], and it’s about a nationwide study that tracks patients with prediabetes and diabetes. And it was housed at Columbia University, which as we know has been the subject of some criticism from the Trump administration. They had lost about $400 million in grants because the administration didn’t like Columbia’s response to some of the protests that were on campus last year. But that has an effect on some research that really doesn’t have much to do with that, including a study that looked at diabetes over a really long period of time.
So it was able to over decades result in 200 publications about prediabetes and diabetes, and led to some of the knowledge that we have now about the interventions for that. And the latest stage was going to focus on dementia and cognitive impairment, since some of the people that they’ve been following for years are now in their older ages. And now they have to put a stop to that. They don’t even have funding to analyze blood samples that they’ve done and the brain scans that they’ve collected. So it’s just another example of how what’s being done at the administration level is contradicting some of the goals that they say that they have.
Rovner: Yeah, and it’s important to remember that Columbia’s funding is being cut not because they deemed this particular project to be not helpful but because they are, as you said, angry at Columbia for not cracking down more on pro-Palestinian protesters after Oct. 7.
Well, meanwhile, people are bracing for still more cuts. The Wall Street Journal is reporting the administration plans to cut domestic AIDS-HIV programming on top of the cuts to the international PEPFAR [President’s Emergency Plan for AIDS Relief] program that was hammered as part of the USAID cancellation. Is fighting AIDS and HIV just way too George W. Bush for this administration?
Hellmann: It’s interesting because President [Donald] Trump unveiled the Ending the HIV Epidemic initiative in his first term, and the goal was to end the epidemic in the United States. And so if they were talking about reducing some of that funding, or I know there were reports that maybe they would move the funding from CDC [the Centers for Disease Control and Prevention] to HRSA [the Health Resources and Services Administration], it’s very unclear at this point. Then it raises questions about whether it would undermine that effort. And there’s already actions that the Trump administration has done to undermine the initiative, like the attacks on trans people. They’ve canceled grants to researchers studying HIV. They have done a whole host of things. They canceled funding to HIV services organizations because they have “trans” in their programming or on their websites. So it’s already caused a lot of anxiety in this community. And yeah, it’s just a total turnaround from the first administration.
Rovner: I know the Whitman-Walker clinic here in Washington, which has long been one of the premier AIDS-HIV clinics, had just huge layoffs. This is already happening, and as you point out, this was something that President Trump in his first term vowed to end AIDS-HIV in the U.S. So this is not one would think how one would go about that.
Well, it’s not just the administration that’s working to constrict rights and services. A group of 17 states, led by Texas, of course, are suing to have Biden-era regulations concerning discrimination against trans people struck down, except as part of that suit, the states are asking that the entirety of Section 504 of the Rehabilitation Act be declared unconstitutional. Now, you may never have heard of Section 504, but it is a very big deal. It was the forerunner of the Americans With Disabilities Act, and it prevents discrimination on the basis of disability in all federally funded activities. It is literally a lifeline for millions of disabled people that enables them to live in the community rather than in institutions. Are we looking at an actual attempt to roll back basically all civil rights as part of this war on “woke” and DEI [diversity, equity, and inclusion] and trans people?
Hellmann: The story is interesting, because it seems like some of the attorneys general are saying, That’s not our intent. But if you look at the court filings, it definitely seems like it is. And yeah, like you said, this is something that would just have a tremendous impact. And Medicaid coverage of home- and community-based services is one of those things that states are constantly struggling to pay for. You’re just continuing to see more and more people need these services. Some states have waiting lists, so—
Rovner: I think most states have waiting lists.
Hellmann: Yeah. It’s something, you have to really question what the intent is here. Even if people are saying, This isn’t our intent, it’s pretty black-and-white on paper in the court records, so—
Rovner: Yeah, just to be clear, this was a Biden administration regulation, updating the rules for Section 504, that included reference to trans people. But in the process of trying to get that struck down, the court filings do, as you say, call for the entirety of Section 504 to be declared unconstitutional. This is obviously one of those court cases that’s still before the district court, so it’s a long way to go. But the entire disability community, certainly it has their attention.
Well, we haven’t had any big abortion news the past couple of weeks, but that is changing. In Texas, a midwife and her associate have become the first people arrested under the state’s 2022 abortion ban. The details of the case are still pretty fuzzy, but if convicted, the midwife who reportedly worked as an OB-GYN doctor in her native Peru and served a mostly Spanish-speaking clientele, could be sentenced to up to 20 years in prison. So, obviously, be watching that one. Meanwhile, here in Washington, Hilary Perkins, a career lawyer chosen by FDA commissioner nominee Marty Makary to serve as the agency’s general counsel, resigned less than two days into her new position after complaints from Missouri Sen. Josh Hawley that she defended the Biden administration’s position on the abortion pill mifepristone.
Now, Hilary Perkins is no liberal trying to hide out in the bureaucracy. She’s a self-described pro-life Christian conservative hired in the first Trump administration, but she was apparently forced out for the high crime of doing her job as a career lawyer. Is this administration really going to try to evict anyone who ever supported a Biden position? Will that leave anybody left?
Roubein: I think what’s notable is Sen. Josh Hawley here, who expressed concerns and I had heard expressed concerns to the White House, and the post on X from the FDA came an hour before the hearing. There were concerns that he was not going to make it out of committee and—
Rovner: Before the Marty Makary hearing.
Roubein: Yes, sorry, before the vote in the HELP [Health, Education, Labor and Pensions] Committee on Marty Makary. And Hawley said because of that, he would vote to support him. What was interesting is two Democrats actually ended up supporting him, so he could have passed without Hawley’s vote. But I think in general it poses a test for Marty Makary when he’s an FDA commissioner, and how and whether he’s going to get his people in and how he’ll respond to different pressure points in Congress and with HHS and with the White House.
Rovner: And of course, Hawley’s not a disinterested bystander here, right?
Karlin-Smith: So his wife was one of the key attorneys in the recent big Supreme Court case that was pushed down to the lower courts for a lack of standing, but she was trying to essentially get tighter controls on the abortion pill mifepristone. But it seems like almost maybe Hawley jumped too soon before doing all of his research or fully understanding the role of people at Justice. Because even before this whole controversy erupted, I had talked to people the day before about this and asked them, “Should we read into this, her being involved in this?” And everybody I talked to, including, I think, a lot of people that have different views than Perkins does on the case, that they were saying she was in a role as a career attorney. You do what your boss, what the administration, wants.
If you really, really had a big moral problem with that, you can quit your job. But it’s perfectly normal for an attorney in that kind of position to defend a client’s interest and then have another client and maybe have to defend them wrongly. So it seems like if they had just maybe even picked up the phone and had a conversation with her, the whole crisis could have been averted. And she was on CNN yesterday trying to plead her case and, again, emphasize her positions because perhaps she’s worried about her future career prospects, I guess, over this debacle.
Rovner: Yeah, now she’s going to be blackballed by both sides for having done her job, basically. Anyway, all right, well, one big Biden initiative that looks like it will continue is the Medicare Drug Price Negotiation program. And we think we know this because CMS announced last week that the makers of all of the 15 drugs selected for the second round of negotiations have agreed to, well, negotiate. Sarah, this is news, right? Because we were wondering whether this was really going to go forward.
Karlin-Smith: Yeah, they’ve made some other signals since taking over that they were going to keep going with this, including last week at his confirmation hearing, Dr. Oz, for CMS, also indicated he seemed like he would uphold that law and they were looking for ways to lower drug costs. So I think what people are going to be watching for is whether they yield around the edges in terms of tweaks the industry wants to the law, or is there something about the prices they actually negotiate that signal they’re not really trying to get them as low as they can go? But this seems to be one populist issue for Trump that he wants to keep leaning into and keep the same consistency, I think, from his first administration, where he always took a pretty hard line on the drug industry and drug pricing.
Rovner: And I know Ozempic is on that list of 15 drugs, but the administration hasn’t said yet. I assume that’s Ozempic for its original purpose in treating diabetes. This administration hasn’t said yet whether they’ll continue the Biden declaration that these drugs could be available for people for weight loss, right?
Karlin-Smith: Correct. And I think that’s going to be more complicated because that’s so costly. So negotiating the price of drugs saves money. So yes, basically because Ozempic and Wegovy are the same drug, that price should be available regardless of the indication. But I’m more skeptical that they continue that policy, because of the cost and also just because, again, HHS Secretary Robert F. Kennedy seems to be particularly skeptical of the drugs, or at least using that as a first line of defense, widespread use, reliance on that. He tends to, in general, I think, support other ways of medical, I guess, treatment or health treatments before turning to pharmaceuticals.
Rovner: Eating better and exercising.
Karlin-Smith: Correct, right. So I think that’s going to be a hard sell for them because it’s just so costly.
Rovner: We will see. All right, that is as much news as we have time for this week. Now, it is time for our extra-credit segment, that’s where we each recognize the story we read this week we think you should read, too. Don’t worry if you miss it. We will put the links in our show notes on your phone or other mobile device. Jessie, you’ve done yours already this week. Rachel, why don’t you go next?
Roubein: My extra credit, the headline is “Her Research Grant Mentioned ‘Hesitancy.’ Now Her Funding Is Gone.” In The Washington Post by my colleague Carolyn Y. Johnson. And I thought the story was particularly interesting because it really dove into the personal level. You hear about all these cuts from a high level, but you don’t always really know what it means and how it came about. So the backstory is the National Institutes of Health terminated dozens of research grants that focused on why some people are hesitant to accept vaccines.
And Carolyn profiled one researcher, Nisha Acharya, but there was a twist, and the twist was she doesn’t actually study how to combat vaccine hesitancy or ways to increase vaccine uptake. Instead, she studies how well the shingles vaccine works to prevent the infection, with a focus on whether the shot also prevents the virus from affecting people’s eyes. But in the summary of her project, she had used the word “hesitancy” once and used the word “uptake” once. And so this highlights the sweeping approach to halting some of these vaccine hesitancy research grants.
Rovner: Yeah that was like the DOD [Department of Defense] getting rid of the picture of the Enola Gay, the plane that dropped the atomic bomb, because it had the word “Gay” in it. This is the downside, I guess, of using AI for these sorts of things. Sarah.
Karlin-Smith: I took a look at a KFF story by Arthur Allen, “Scientists Say NIH Officials Told Them to Scrub mRNA References on Grants,” and it’s about NIH officials urging people to remove any reference to mRNA vaccine technology from their grants. And the story indicates it’s not yet clear if that is going to translate to defunding of such research, but the implications are quite vast. I think most people probably remember the mRNA vaccine technology is really what helped many of us survive the covid pandemic and is credited with saving millions of lives, but the technology promise seems vast even beyond infectious diseases, and there’s a lot of hope for it in cancer.
And so this has a lot of people worried. It’s not particularly surprising, I guess, because again, the anti-vaccine movement, which Kennedy has been a leader of, has been particularly skeptical of the mRNA technology. But it is problematic, I think, for research. And we spent a lot of time on this call talking about the decimation of the federal workforce that may happen here, and I think this story and some of the other things we talked about today also show how we may just decimate our entire scientific research infrastructure and workforce in the U.S. outside of just the federal government, because so much of it is funded by NIH, and the decisions they’re making are going to make it impossible for a lot of scientists to do their job.
Rovner: Yeah, we’re also seeing scientists going to other countries, but that’s for another time. Well, my extra credit this week, probably along the same lines, also from The Washington Post. It’s part of a series called “Who Is Government?” This particular piece [“The Free-Living Bureaucrat”] is by bestselling author Michael Lewis, and it’s a sprawling — and I mean sprawling — story of how a mid-level FDA employee who wanted to help find new treatments for rare diseases ended up not only figuring out a cure for a child who was dying of a rare brain amoeba but managed to obtain the drug for the family in time to save her. It’s a really good piece, and it’s a really excellent series that tells the stories of mostly faceless bureaucrats who actually are working to try to make the country a better place.
OK, that’s this week’s show. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left us a review. That helps other people find us, too. Thanks as always to our producer, Francis Ying, and our editor, Emmarie Huetteman. As always, you can email us your comments or questions. We’re at whatthehealth@kff.org, or you can still find me at X, @jrovner, and at Bluesky, @julierovner. Where are you guys these days? Sarah?
Karlin-Smith: A little bit everywhere. X, Bluesky, LinkedIn — @SarahKarlin or @sarahkarlin-smith.
Rovner: Jessie.
Hellmann: I’m @jessiehellmann on X and Bluesky, and I’m also on LinkedIn more these days.
Rovner: Great. Rachel.
Roubein: @rachelroubein at Bluesky, @rachel_roubein on X, and also on LinkedIn.
Rovner: We will be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
4 months 5 days ago
Courts, Health Care Costs, Medicare, Multimedia, Pharmaceuticals, Public Health, States, Abortion, Children's Health, CMS, Disabilities, Drug Costs, FDA, Food Safety, HHS, HIV/AIDS, KFF Health News' 'What The Health?', Podcasts, Prescription Drugs, texas, Trump Administration, vaccines
KFF Health News' 'What the Health?': Live from Austin, Examining Health Equity
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
The term “health equity” means different things to different people. It’s about access to medical care — but not only access to medical care. It’s about race, ethnicity, and gender; income, wealth, and class; and even geography — but not only those things. And it’s about how historical and institutional racism, manifested in things like over-policing and contaminated drinking water, can inflict health problems years and even generations later.
In a live taping on Sept. 6 at the Texas Tribune Festival, special guests Carol Alvarado, the Texas state Senate’s Democratic leader, and Ann Barnes, president and CEO of the Episcopal Health Foundation, along with KFF Health News’ Southern bureau chief Sabriya Rice and Midwest correspondent Cara Anthony, joined KFF Health News’ chief Washington correspondent, Julie Rovner, to discuss all that health equity encompasses and how current inequities can most effectively be addressed.
Anthony also previewed “Silence in Sikeston,” a four-part podcast and documentary debuting this month exploring how a history of lynching and racism continues to negatively affect the health of one rural community in Missouri.
Panelists
Carol Alvarado
Texas state senator (D-Houston)
Cara Anthony
Midwest correspondent, KFF Health News
Ann Barnes
President and CEO, Episcopal Health Foundation
Sabriya Rice
Southern bureau chief, KFF Health News
Also mentioned on this week’s podcast, from KFF Health News’ “Systemic Sickness” project:
- “A Teen’s Murder, Mold in the Walls: Unfulfilled Promises Haunt Public Housing,” by Fred Clasen-Kelly and Renuka Rayasam.
- “Med Schools Face a New Obstacle in the Push To Train More Black Doctors,” by Lauren Sausser.
- “‘I Feel Dismissed’: People Experiencing Colorism Say Health System Fails Them,” by Chaseedaw Giles.
- “As Record Heat Sweeps the US, Some People Must Choose Between Food and Energy Bills,” by Melba Newsome.
- “Black Hospitals Vanished in the U.S. Decades Ago. Some Communities Have Paid a Price,” by Lauren Sausser.
click to open the transcript
Transcript: Live from Austin, Examining Health Equity
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello, and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News, and usually I’m joined by some of the best and smartest health reporters in Washington. But today we have a special episode for you all about health equity taped before a live audience at the Texas Tribune Festival on Sept. 6, 2024. I hope you enjoy it. We’ll be back with our regular panel and all the news on Sept. 12. So here we go.
I am pleased to be joined on this panel by two of my KFF Health News colleagues, Southern bureau chief Sabriya Rice, who’s right here next to me, and Midwest correspondent Cara Anthony, down at the end. We are also honored to be joined by two guests with a lot of combined expertise on this issue, [Texas] Senate Democratic leader Carol Alvarado, who represents the 6th District of Texas, which includes parts of Houston, and Dr. Ann Barnes, president and CEO of the Episcopal Health Foundation, also based in Houston.
We’re going to talk amongst ourselves for the next, I don’t know, 40 minutes or so. Then we will go to you in the audience for your questions. So go ahead and be thinking. I have to say I am personally really excited about this episode because health equity is something I think about a lot, but I’ve never been able to accurately define, even for myself. I know it’s about race and ethnicity and gender, but it’s not just about race and ethnicity and gender. It’s about income and wealth and class, but it’s not just about income and wealth and class. It’s about geography, but not just about geography. And it’s about medical care, but not just about medical care. So I want to kick off this discussion by asking each of you how you define health equity. And why don’t we just sort of go down the row? So we’ll start with you, Sabriya.
Sabriya Rice: Really great question and it gave me a lot of things to think about. And I want to start with a little anecdote from something that happened yesterday evening. I was having a conversation with a group of visitors from South Africa who work for an investigative news site there called The Daily Maverick, and my colleague, Aneri Pattani, who’s also a KFF Health News reporter. We were explaining some of the things about the U.S. health care system and just some basic stuff like how a lot of people can’t afford to just go for preventive care, how you may or may not have access to care in your neighborhood, and what that means in terms of your health outcomes.
And in the middle, they paused us and were like, “Wait a minute, wait a minute. This doesn’t make any sense. We have these things in South Africa.” It’s something you hear regularly from other people who are visiting here and they’re like, “But you’re like the wealthiest country in the world. How do you not have these things?” And I was thinking about that and thinking of, in terms of your question. So, for me, I think of health equity as just creating the opportunity for everyone to be able to achieve their optimal health no matter their background. And I think that’s something we could really work on in the U.S.
Ann Barnes: Great.When I think about health equity, I share a similar definition where folks have a just and fair opportunity to live their healthiest lives. And this is largely from the Robert Wood Johnson Foundation’s definition of health equity. But coupled with that is the requirement to dismantle barriers to health. And so we have to remember that that is part of the equation, not just dreaming that we all have optimal health, but thinking about how we’re going to eliminate the barriers, especially for populations that are most vulnerable.
Carol Alvarado: I think about accessibility and affordability. And if you don’t have those two things in health care, then you create this environment of the haves and the have-nots, those who can afford to have health insurance and those who can’t. Maybe it’s because of their job, their social economic status. And I also think that we have to take partisanship and politics out of health care. I mean, when did that become such a divisive issue that really reached the height during the Obamacare debate and the many, many times to repeal it? And I know we’re going to dive into this a little bit more, but health care and access should never be political.
Cara Anthony: When I think about health equity, I agree with all of the panelists here today, but I’m also thinking about the future and the next generation. I’m a single mom. I have a 7-year-old daughter, and I think about how is she going to be able to live a longer and healthier life than previous generations. I’m going back home tomorrow and one of the first things that I’m going to do is sign my daughter up for a swim lesson, right? That’s health equity because I’m also signing up for a lesson as well. Why? Because I never learned to swim. It’s about each generation doing better. And why didn’t I learn to swim? Because my parents were born in 1948 in the South and did not have access to swimming pools. So it’s those daily practical applications that I think about when I think about health equity. So yeah.
Rovner: Sen. Alvarado and Dr. Barnes, I want to talk about Texas a little bit since, obviously, we’re sitting here. Texas is, we try not to think about just insurance when we talk about health equity, although it’s a big deal, and in Texas it’s still a big deal as opposed to a lot of other states. What impact does Texas’ failure to, so far at least, expand Medicaid have on health equity in this state?
Barnes: Well, we know that health care and access to health care is critically important to health. It accounts for 20% of a person’s health, and nonmedical drivers account for the other 80%. But 20% is important. We still have the highest rate of uninsured. So that means that there are parts of our community that can’t get the preventive care that they need, that can’t talk to people who might connect them to social services to support their nonmedical needs. And so the larger conversation is about increasing health coverage overall in Texas. And certainly expansion of Medicaid is one piece of that. About 5 million people are uninsured right now in our state, and so we’ve got a lot of ground to cover. Affordable Care Act is one way, Medicaid expansion is another. And so a lot of work to do, for sure.
Alvarado: And I’ll pick up where you left off. Medicaid expansion has been, believe it or not, a hot political hot potato here in Texas. I’ve been filing, along with many of my colleagues, bills every session since 2009, maybe. We can’t get hearings. And no one really gives you a good explanation why. They’ll have things that really don’t make a lot of sense that there are too many strings attached. Well, somehow 40 other states don’t have that problem.
And we’ve seen that the cost that we’re leaving on the table, millions of dollars. I think the last number I saw was 2023, maybe $11 billion just there on the table; other states are utilizing it. And then here in Texas, it’s kind of complicated. I’ll just give you the elevator speech on that. But they kept the Medicaid enrollment going during the pandemic, and then afterwards they did this winding, what they called winding down, and almost 2 million people were left without Medicaid. And a good portion of that are children, and a good portion of those children are Black and brown kids who are already living in environments where they don’t have access to green space or grocery stores, fresh fruits and vegetables. So you pile all of that together and that’s why we are in this place of many uninsured, almost twice the number of the national rate, which is at 8[%]. We’re at 17[%]. Yeah, everything’s bigger in Texas especially the number of uninsured.
Rovner: So, Dr. Barnes, I want you to talk about what it is that your foundation does. I find it fascinating that even though you would think that you’re all about medical care, you’re really not all about medical care, right?
Barnes: No, that’s right. So we are committed to promoting equity by addressing health and not just health care. And so we use our resources in partnership with community members and organizations and change-makers to address factors that occur outside of the clinical setting and the doctor’s office. And representative [Sen.] Alvarado listed so many of them: housing, food security, employment, education. All of these are critically important to health. And so we use our resources to help address those needs because we know that that will set people up for a healthy life and not just a sick life that ends them up in clinical care at the very tail end of their illness. One of the things I wanted to share, I’m a physician by training, in internal medicine and primary care, and my patients taught me so much when I saw them and I prescribed medicines for diabetes or high blood pressure. It was the stories about their lives outside of the clinic that really helped me understand what was impacting their health, which is why I got into this space of health and not just the clinical side.
Rovner: Cara, you’re about to debut a project that you’ve been working on for four years that has to do with exactly this, with sort of the nonmedical implications of other things and the lack of health equity. So why don’t you tell us a little bit about it?
Anthony: Yeah, so coming up next week, we’re going to premiere a new podcast, and also it’s a documentary film, called “Silence in Sikeston.” It focuses on police violence and police killings, but looking at them not as crime stories, but more as a public health threat. Also looking at the lynchings of yesterday as a public health threat. Maybe people didn’t use those terms back then, but certainly we recognize them as such now.
And so I hope everyone checks this out because it really talks about how racism and chronic stress are linked. And so oftentimes it can weigh not only on your mental health — anxiety, depression, you can become suicidal because of these things — but also you can have physical health effects as well, higher rates of high blood pressure, cancer, et cetera. And so I’ve been traveling for the last four years to Sikeston, Missouri. It’s a small community in rural Missouri where there was a man who was lynched there in 1942. His name was Cleo Wright. This is America’s first federally investigated lynching, the first time the FBI decided to look at lynching as a federal crime. They came to Sikeston, Missouri. But the story has never really been told and not in this way, not looking at it as a public health story, because as public health reporters we’re tasked with looking at what makes a community sick, what’s harming a community, and sometimes that can be something like lynching, something like police killings. And so we’re looking at that head-on and talking about the health impacts there.
Rovner: And Sabriya, obviously this is a big project that we’ve been working on, but we’ve been working on a lot of other health equity stories that you’re sort of in charge of. So why don’t you tell us about some of those?
Rice: Yeah, certainly. And it’s a great parallel to the work that Cara’s been doing. I came to KFF in 2022, and my charge was to start up a Southern bureau and look at the health equity disparities that happen across the South. So my team ranges from Texas to Florida up until North Carolina, and we meet weekly and have conversations. And one thing I was constantly hearing from the reporters — I’m not a policy expert and I’m not a statistician, but I’m a people person and I listen to people — and my reporters were saying over and over again, “Yeah, we spoke to this expert about Medicaid expansion, but they were like, ‘Yeah, we could do that, but it’s not going to stop the root of the problem, which is racism.’”
“Yeah, we wrote about maternal mortality or infant mortality, but still at the root of this is racism.” So that term kept coming up. And so we decided this year to take a look at systemic racism in the health care system, and our series is called “Systemic Sickness,” and it looks at some of the things that Cara talked about, including policing, but we also look at redlining or the history of redlining, of public housing challenges. We’re looking modern-day, like attacks on diversity, equity, and inclusion programs in education, specifically the field of medicine. So that’s the nature of our project that we have for this year. And it’s been just a real fascinating experience.
Rovner: I think I’ve heard this come up a couple of times in the panels we’ve had this morning about some of the other issues that really impact this in a bigger way than many people think. And I think housing is definitely one of those. You talked about redlining. A lot of this is historic racism and literal redlining: “You cannot live here. If you live here, you cannot get a mortgage.” There’s been a lot of that. How significant, I assume, the problem is here in Texas?
Barnes: Yeah, it is significant in a lot of those racist structures. We continue to experience the aftereffects of those. Even today, those neighborhoods are still under-resourced, and that includes, like you mentioned, grocery stores, safe spaces to play, green spaces, good transportation options. And so those old and, I suppose, acceptable forms of structural racism that were enacted are still playing out today in the health of people.
Alvarado: It’s very important. And housing doesn’t get a lot of attention. It’s not a very glamorous or sexy issue, but I’m glad to hear presidential candidate Kamala Harris, she talked about housing and what she would like to see to build more affordable housing, or I guess we’re calling it “workforce housing” now. And then our state comptroller, Glenn Hegar, recognizing how many people we have moving to Texas all the time. And to accommodate that, we’d need about 300,000 new units or housing. So people don’t have a place to lie their head that’s comfortable and a place to cook meals. And then if they don’t have those safety nets, then their last concern is probably, “Oh, am I getting my workout in today?” Or “Am I eating enough fruits and vegetables?” when they’re in survival mode.
Rice: And I’ll piggyback on what representative [Sen.] Alvarado said. It’s hard for people to see how this kind of plays out in real time. And two of our reporters on the Southern team just recently looked at a community in Savannah, Georgia, called Yamacraw Village. It’s a public housing community that started around World War II. And historically, at that time, the residents were white. Disinvestment happened within this community over the years and the population of the community changed.
So now it’s a predominantly Black and Latino community, but what you see is a large amount of disinvestment. People can’t get things fixed, so you’re living in very unhealthy housing, when you do have housing. There’s no playgrounds, there’s no green space, there’s an extreme amount of violence. But one man told our reporters, “The walls sweat like working men.” This person moved into this community and got vouchers to be able to live there and immediately developed asthma and has been taking medication even years after he left the community. So when you think about how the system is harming people, these communities are there and they’re not being invested in. Instead, people are given things like Section 8, if they can get the vouchers, and then if you can find affordable living that will take your Section 8 voucher. So it’s a really big problem. And housing is often not talked about as a public health crisis.
Barnes: Absolutely. And not just the place that you lay your head, but high-quality housing, not substandard that actually can impact your health.
Rovner: One of the things we’ve seen, I guess in the last couple of years, are these extraordinarily hot summers. And I know the government has always helped underwrite heating assistance in the winter, but apparently air-conditioning assistance is not considered of the same importance. I just read Phoenix has been 100 degrees every day for the last hundred days. I know that here in Texas you’ve had some pretty extended heat waves. I mean, how big an issue is heat as a public health and equity issue?
Alvarado: It’s a big problem, and especially when we’ve had things like power outages, storms that we had very close to one another. We had the derecho in May and then we had followed by the Hurricane Beryl, and that was tough. I mean, people were out of power anywhere from a couple of days to 10 days, and for some, it’s life or death, especially if they have medical equipment that they have to be hooked up to. We’re going to be tackling some of those issues in this session, but our city does a good job in our county of opening cooling centers so that people have a place to go and retreat and charge their devices. But the weather is getting much more turbulent. The summers are getting hotter, the hurricane season is more active. And until people realize that there’s a reason all this is happening and people don’t want to talk about it or put policy forth that addresses what’s taking place in our environment. So they go hand in hand.
Barnes: One of the other things, as we talk about communities where there isn’t investment, is that there are these heat islands, and typically they are where people are low-income communities of color where simple things like trees being planted that could cool the temperature in the area, these neighborhoods don’t have those amenities. So there are efforts in Texas and in Houston to try to green up some of those communities, but it requires investment and attention and acknowledging that we have these disparities across the community.
Rovner: Yeah, there was a study, I think it was in Baltimore a couple of years ago, where the temperature differential was like 15 degrees. I mean, it would be 85 in the suburbs and it would be 100 in some of these sort of concrete jungles downtown where the buildings hold onto the heat. And, of course, those are places where people live and often can’t afford their utilities, and obviously their utility bills would be higher because it’s going to cost more to cool those places.
Barnes: And as representative [Sen.] Alvarado mentioned, heat, when you have chronic conditions, so the elderly in particular, these are the communities that have the greatest burden of those conditions. And so it’s particularly alarming. That need is there and we really have to pay attention to it.
Rice: One of the things we just looked at in a story was this idea of energy poverty. And one interesting factoid that I learned from that that I was unaware of myself is the idea that many of our federal policies tend to focus on cold weather and that this idea, in federal and state, so for example in North Carolina where the story was centered, there are requirements that apartments and other kind of housing that they mandate that you have heat in the winter. It’s not the same for AC in the summer, and that’s probably something that should be looked at.
Rovner: I want to talk about women. When we talk about health equity differences between men and women, where one of the first places we saw before the Affordable Care Act, insurers were allowed to charge women more simply because they were women and they lived longer and had more health expenses associated with being pregnant and having children. That was eliminated. But, obviously, there are still a lot of inequities between men and women and it’s there. I know that they’re exacerbated by race, but it’s not purely race. I mean, how big an issue is this still? Obviously, reproductive health in general, abortion in specific, is the central health issue in this year’s campaigns. So where does it fall in the pantheon of health equity?
Alvarado: I think if we had more women elected to office, definitely in Texas and in statewide positions, that things like Medicaid would pass, expansion of Medicaid. And it does matter who is at the table, who is making the decisions. And this happened just on one side of the aisle, but just 12-month postpartum for women, so that they can take advantage of Medicaid, and it finally got done. But that’s the only piece that we’ve been able to do. And they were two women, Democrat and Republican, Toni Rose and Sen. Huffman, who led that effort. And I just know if we had more women in the right places, that issues like health care wouldn’t be so partisan and divisive.
Barnes: Yeah, I was going to say the same thing. We finally got 12 months of coverage postpartum, and it’s really unfortunate that we have to piecemeal the care that women need. I think about the fact that we expect good pregnancy outcomes when someone hasn’t had care until they’re pregnant, and up until recently, only eight weeks after they were pregnant. And so yeah, there are a lot of disparities, and for many women being pregnant is their ticket to Medicaid. And so it just perpetuates this fragmented continuum of health, and women are falling out of it regularly.
Alvarado: And especially with women of color, 64% of Latinas and 62% of African American women will at some point be on Medicaid.
Anthony: I just want to chime in here too. You talk about reproductive rights. I considered, Julie, writing a personal essay about, at the time I was 35, I went on … I’m only 37 now, but as a Black woman in the U.S., going on birth control for the first time in my life. Now, I mentioned I’m a single mom, so that wasn’t always my story, but I think we’re in an era of progress and education that is still really, really important. So I just wanted to share that.
Rovner: So I want to talk a little bit about the actual inequities within medical care. One thing, Stat News has a wonderful story that’s part of a series they’re starting this week on algorithms that are embedded into care — when doctors make a diagnosis and then the algorithm comes up and shows all the things you should consider in deciding what kind of treatment. And a lot of these now have: Is the patient Black? And some of them, I think, were originally, I assume most of them, were originally born out of some sort of thought that there’s a differential in risk depending on skin color, but obviously a lot of them … have been completely overturned by science and yet they’re still there. What impact does embedded racism in medicine, in general, have on health equity?
Barnes: Yeah, specific to that, in particular, what it resulted in is individuals who had evidence of risk, because they were Black there was a higher threshold that had to be crossed before they got additional testing or additional treatment, which means that there are populations of people who didn’t get timely care because of those embedded algorithms. One of the other things, there’s not an overriding body — I guess CMS could be that overriding body — but right now no one is standing up saying, “Absolutely you cannot use race-based algorithms.” And so it’s really up to individual health systems. States could implement penalties if you use them, but right now it’s up to an individual institution, and it takes a lot to undo an algorithm and change an electronic medical record. But we are at the threshold, I think, of that beginning to happen.
Anthony: And it’s such a common issue. I spent the last few years looking particularly at kidney disease testing, and if you put a Black person’s kidney on a table and you put a white person’s kidney on the table, you would not be able to tell the difference. People really need to understand that race and biology are not the same, but for years, I mean decades, people have mixed this up and it has delayed care from people who are not getting the treatment that they need.
We wrote a story a couple of years ago about a Black man who needed a kidney, a white woman read the story and decided to donate a kidney to him, but that’s not everybody’s case. I can only write about so many patients that are in that same scenario. And so there’s still a lot of work that needs to be done, but progress is being made. The hospital in particular that we were looking at in St. Louis, they’ve made some policy changes since we published that particular article, but we still have a long way to go. I can’t say that enough. Race and biology are not the same.
Rovner: I mentioned at the top geography, and we talk about people who are grouped together because they have to be, but it’s also about where people decide to live, in rural versus urban. I mean, how can we look population-wide and try to even out, I mean, we talk constantly about the closures of rural hospitals and the difficulty of getting care in far-flung areas, and obviously Texas has a lot of far-flung areas, I know. That is another issue that sort of plays into this whole thing, right?
Alvarado: Oh, absolutely. And one of the arguments, again, this all keeps going back to Medicaid expansion, but you’re talking to my colleagues on the other side of the aisle, I said, your districts, some of your rural districts are suffering the most. Hospitals have shut down. They have to drive to the next big city. It might be Houston or Dallas or San Antonio, but it has, I think, disproportionately hurt rural areas. And until folks want to own that, embrace that, and try to fix it, we’re going to continue to be in this place and probably the gap will widen even more.
Rice: And I’d say we saw this kind of play out in Georgia this week. I live in Atlanta, and there was the unfortunate school shooting incident that happened there. And the community that that school is in had no hospital in that area. So the closest place would’ve been 40 miles away in either direction to Athens, Georgia, which is about 40 miles from the Barrow County and then Atlanta. So even in an incident like that, just coordinating to get people treatment in a major incident is just another example of why we need to do something, right? It’s not just Black communities or Hispanic communities. I think it’s all of us and any given moment may need access to care. And if you think about it, in light of that, 40 miles is no easy feat on Atlanta highways in rush-hour traffic or even being airlifted, it’s still a distance and you have a small window of time to save a life.
Barnes: And there’s been specific conversations in Texas about access to maternal health care in rural communities. And so again, the distance that someone would have to drive is hard for many of us to imagine, especially in a time of crisis.
Rovner: One of the other continuing issues when we talk about health equity is the desire of people to be treated by people who look like them or people who have similar backgrounds to them. That’s obviously been an issue for years that the medical community has been trying to deal with. I want to ask specifically what impact the Supreme Court’s decision banning affirmative action is going to have on the future of the medical workforce and the few strides that have been made to get more people of color, not just into medical school, but into practice.
Rice: I’d say that was pretty immediate, and especially in some of our Southern states, given the history. But I think there were immediate bans on DEI programs or dismantling of those at schools across the South. I can think of Alabama, Mississippi, Texas, even Georgia introduced a bill. It didn’t pass, but I think we saw that happen pretty immediately. And the doctors that at least reporters on my team have spoken to have said, even in their programs, they can’t even say, “We’re trying to increase the number of Black doctors or Hispanic doctors or Native American doctors.” You can’t target those groups to come to special programs, to have access to visitations to schools or that sort of thing. You can’t even say it. So they’re having to kind of circumvent how they reach people to increase the low numbers of doctors of these ethnic groups.
Alvarado: I think we’ve only begun to see the consequences that have taken place because of that. When you mentioned the medical center, we have people that come from all over the world and having physicians that they can relate to or just speaking the language, 48% of people from Houston speak other languages other than English at home. So Houston is known for being very international, very diverse, and it’s only going to continue to grow. So having the language barrier also contributes to many other issues regarding your health. But having that comfort with someone that understands your background, may understand your challenges, that’s important. And I don’t think that the people who were coming up with DEI legislation here in Texas and, those things don’t cross their mind because they’re shortsighted. They’re trying to check a box or get that “A-plus” on their whatever scorecard by whatever group in their party.
Rovner: But people think, well, a doctor is a doctor is a doctor. Why does it matter if that doctor, if you’re able to relate to that doctor, how important is it really to have a medical community that looks like the community it’s serving?
Barnes: Yeah, I would say it’s a huge trust issue. I remember having patients in my practice, African American patients, and there was a wonderful trust that we had with one another. And then I would refer them to a specialist who didn’t look like them, and they would ask me questions, “Do you really think they’re going to do the procedure that they said?” And I was just thinking, “Oh my gosh, I am taking for granted that someone would trust me.” And when we think about how we make recommendations to patients, if the trust isn’t there, why would they listen to what you had to say? And then that will, of course, put you at a disadvantage from a health perspective. And in terms of eliminating affirmative action, I don’t know the medical school data, but a lot of higher education institutions are already reporting lower numbers in their incoming classes. And that certainly is going to be the same in medical schools, nursing schools, PA schools.
Rovner: I did have in my notes that medical schools are freaked out by this.
Anthony: And it’s really …
Barnes: Absolutely.
Anthony: And what you’re talking about, and I’ve written a lot about this topic, and just to name it, we’re talking about “culturally competent care,” and culturally competent care is really, really hard to find because the numbers are low, because there has been a shift. But I think the conversation is also shifting towards culturally humble care or cultural humility in health care. So even if I can’t find a doctor who looks like me, I need someone who’s culturally humble to say, “You know what? I don’t understand everything that you’re going through as a Black woman raising a child in America, but I can admit that, I can say that out loud, and I can maybe direct you towards someone who can be more helpful. Or maybe we could just have a really candid conversation about that.” And so I just want to give people the terminology that I think could be useful if you want to learn more.
Rice: We also just did a story looking at colorism in the U.S. and the impact that that has on people. Interviewed a woman, for example, who had been bleaching her skin for all of these years, had these side effects from that, but clinicians weren’t catching it. They didn’t know to look for specific things. So there were mental health challenges there because of feeling unhappy being in her own body, but there were also manifestations on her physical health because the chemicals that she was introducing were causing harm. So I think that kind of cultural competence, someone that looked like her and could relate to her background might be like, “Wait a minute, is this what’s happening here?” And that’s what happened in the case of that particular patient.
Rovner: So at our session this morning on why does care cost so much? My colleague Noam Levey talked about something he calls a culture of greed in health care, it does seem as if every aspect of the system is or has been monetized. I mean, it really is all about the money. How does that impact health equity? I mean, you could think that if the incentives were in the right place, it might be able to help.
Alvarado: And it drives up the cost of insurance too. I mean, if you’ve ever had a loved one in the hospital, they don’t want you to bring your medications from home. So you have to take what they have there. And it is the same thing, but it’s very expensive. You can buy a bottle of Advil for 5, 6 bucks; each pill is about that much, and then it drives up cost of insurance, and it has an economic impact that trickles down to the consumer.
Barnes: And then it becomes a barrier. So if you are paying out-of-pocket and things are incredibly expensive and you also have to buy food and pay your rent, you may forgo or delay care, which again is going to leave you in a worse situation from a health standpoint and just perpetuate the disparities.
Rovner: Now we have managed-care companies who serve not just most of the Medicare population, but most of the Medicaid population, who get paid for presumably the incentive there was, you’re going to take care of these people and we’re going to pay you, and the more people you can find to take care of, the more we’re going to pay you. And in theory, they have adequate networks where people can actually find care, which is not always the case with Medicaid. It’s hard to find providers who will take Medicaid. I’ve started seeing ads for managed-care companies for people who are eligible for both Medicare and Medicaid, the “dual eligibles.” They don’t call them that, but it’s like, “Wow, I’m looking at TV ads for dual eligibles.” Somebody must be making some amount of money off of these people. Is anything good coming from it?
Alvarado: I mean, the pharmaceutical companies are raking it in pretty good. And in some countries you can’t even have direct promotion for pharmaceuticals from the pharmaceutical company to the consumer.
Rovner: Most other countries.
Alvarado: Yeah, except I mean every commercial. I mean, you pick your drug, what is it, Skyrizi or Cialis, whatever. I mean, it’s out there.
Rovner: Yes, we all know the names of the drugs now.
Alvarado: Something for everybody.
Rovner: I’m going turn it over to questions in a minute, but before I do, I don’t want this to be a complete downer. So I would like each of you to talk about something that you’ve seen in the last year or two that’s made you optimistic about being able to at least address the issue of health equity.
Rice: I mean, the fact that we’re having these conversations more, I think, is something that brings optimism, for me. I don’t remember my family having these conversations as a kid. It was just like, “Well, this is just the way it is. Or “This is how the system is.” And I think it’s positive that we’re having conversations not just about how the system is currently, but about changing it, as Cara mentioned, for the next generation.
Barnes: As a philanthropy, I can talk about some specific investments that we’ve made that have allowed community health workers to work with women throughout their pregnancy period. And so in a small way, for those women, we have increased the opportunity for them to have a healthy outcome. But we’ve also done some policy work. We were part of a large coalition of folks pushing for 12 months of Medicaid coverage postpartum. And those system-level changes affect millions of Texans. And so again, we felt that was really an important way to change the health equity equation.
Alvarado: And thank you for your work on that. Many of us on my side of the aisle have been filing those bills to get it extended to 12 months. But again, everything goes back to politics. They weren’t going to let somebody in the minority party carry it. And at that point, you don’t care who gets the credit, just get it done. Or as we say in Texas, “Git-er-done” and take care of folks. But another thing that we’ve been talking about on our side of the aisle was the tampon tax, the pink tax, and wow, all of a sudden my colleagues on the other side thought, “Oh, that’s a good idea.” And so anyway, we didn’t get to carry it. They passed it, OK, it’s done. So we’ve got to play this game, dance this dance here, and we’ll do it. The most important thing is to make things accessible and affordable to people.
And one of the other things too, we didn’t get to talk about this much, but when you talk about the environment and health impacts, my district has so many concrete batch plants. And so we are seeing more people become aware of particulate matter and the negative impact that these facilities have. And they’re almost all, I’d say 99% all, located in African American and Latino neighborhoods. And Harris County has the largest number of concrete batch plants in any other county in Texas. And a third of those concrete batch plants are walking distance to schools and to day cares. We have more work to do in this area, but at least now the public is holding people accountable and we’re putting more pressure on the agencies that regulate these facilities.
Anthony: We often think about data and there’s negativity associated with that. But one thing that I’ve learned, particularly in the last four years, is that there’s good data too. There’s change that is happening, right? I mentioned early on in our conversation about the swim lesson with my daughter, and that’s progress, right? There’s institutional change happening as well. We talk about the algorithms and the issues there, but we know that there are institutions that have said, “Yes, this is a mistake.” I have concerns, and this is another conversation about what’s going to happen with AI. But I think that there are positive ways to look at that as well. So change is happening, and we have to think about also moving forward, and we want to tell those stories too.
Rovner: All right, well, I’m going to turn it over to the audience now. I see we already have someone waiting to ask a question. Please, before you ask your question, tell us who you are and where you’re from and please make it a question. Go ahead.
Abimisola: Hi, my name is Abimisola. I am from Nigeria, but I live in Austin, Texas. My question is about education. I feel like a big part of access and equity is education. So what are we doing to let people know that there are some services that are available to help them access the care that they need? I imagine that as, I guess, working through the pandemic, health literacy is not really a thing in the public. And so what are we doing to let people know that some of these services exist? And then also on the cultural humility end of things, what are we doing to make sure that providers are aware of this gap and how can they be helpful in their own way to make sure that equitable care does exist when people come in?
Barnes: So I think that we are at a moment of awakening when it comes to recognizing that you need trusted messengers in communities to actually engage in conversations about navigating health care systems or engaging in preventive health measures. Community health workers are really starting to have their day, and there is recent legislation that will actually allow them to be reimbursed for case management services related to their care of pregnant women. And so we are in a moment, that same legislation will also cover doulas and their case management services. But I think to your point, education, health literacy, having someone you trust who can walk you through that process is so critically important and those caregivers are finally getting the recognition that they deserve and being elevated and reimbursed. And so I think that that is a great step.
Linda Jackson: Hello, thank you for the information that you’ve provided. So I’m Linda Jackson and I’m with Huston-Tillotson University, which is a historically Black university a few miles from here. And I want to talk about the speed. One thing that happened again during the coronavirus is that because the university had systems in place, for example, the university was able to move from on-campus, on-ground, to online almost immediately with all of those funds and programs that were available. We’re in that same situation now with what we’re experiencing now, we have an increase in the number of students who want to attend college, an increase in our enrollment. We are a pipeline for the health industry, for some of the issues that we have to deal with, but the issue is that we can move quickly, but to get to all of those entities that are out there that can provide the funding that’s needed.
We have students we turned away who are waiting to get into college, and they’re interested in computer science and they’re interested in the health care industry and they’re interested in all those fields, but it’s the speed. We are here waiting, but the speed for which all of those resources have to come into place. And for example, we had entities who came to us with a doula program, with a doula idea, and we offer a certificate in the doula program to ensure that there are more doulas to provide that culturally sensitive care. And so my question is we’re here. We’re waiting. The resources need to come faster. And so I guess that’s a statement as opposed to a question.
Rovner: But thank you for raising the topic.
Barnes: I will just say, well, first off, my mother and my aunt are both graduates of Huston-Tillotson. So very excited to have you here. I think connecting the industries that need the workforce with the institutions who can provide the training is a key connection that we haven’t figured out how to do well because that’s where your resources would come to be able to support students getting trained to then fill the jobs where we have needs in the health care setting.
Rovner: And this is not just a health equity issue, this is the entire health system writ large.
Barnes: Absolutely.
Rovner: The difficulties with matching workforce needs with patient needs.
Robert Lilly: Good afternoon. Thank you very much for this lively conversation. My name is Robert Lilly. I am a criminal justice participatory defense organizer with Grassroots Leadership, and I’m also justice-impacted, formerly incarcerated, 54 years old with 21 years of my life spent in some institution or another. I want to just comment or not comment, but inquire from the two points that were made about equity. You mentioned that you wanted to, equity was about optimal health, no matter the background of the individual and also to eliminate barriers, especially for populations that are most vulnerable.
Texas has over 110 prisons, 135,000 people currently incarcerated, 600,000 every year exiting the system. Medicaid expansion is a challenge in Texas. My question before you is, in this era of mass incarceration, what options do we have? If policy can’t fix this problem, what other options exist? With the creative minds that you have, the thoughtful insights that you’re gaining from your research and reflection, how can you advise us to move, if our legislature won’t move? Do we depend on them alone to solve these problems, or is there an alternative route that supersedes them? And the last thing I’ll ask is how much of what we’re experiencing today, and we know America’s been historically racist, but how much of what we experiencing is a backlash to George Floyd?
Rovner: Oh, excellent question. Somebody want to take him on?
Anthony: I really think about if policy can’t do it, what can? And that’s where I think about for me, often it’s the institution of the Black family and starting young, what conversations do we need to have with our children as we move forward? That’s one thing that I, in particular, think about because I really think it comes down to literacy, education, being made aware, and also thinking about what can we do as individuals? But it really requires institutional change. I don’t want to act like that’s not at the core of the issue, but really want to talk about our future a lot and think about our future a lot. And so I think it starts at a really young age.
Rice: I wish we could tackle the whole iceberg all at once and just tear the whole thing down and start over. But the reality is we have to chip at it. And I think as we continue to do that, I think it starts to dismantle. And I don’t know that that offers much hope, but I think it’s kind of where we’re at and what we have to do is to keep moving because we wouldn’t have had this progress without that kind of fight.
Rovner: But … go ahead.
Rice: And vote.
Carley Deardorff: Hi, y’all. My name is Carley Deardorff, born and raised in Texas. I have lived in Texas my whole life, except I ran away to Spain for a little bit. Born in Lubbock, been in Austin for about 15 years now. I want to say one, thank you so much for your question previously. My question involves both formerly incarcerated but also aging. So aging parents, aging families. My partner and I were both raised by single moms, and so the outcomes for them, health-wise and also financially in terms of retirement and things like that are very, very slim. And so now in this next phase of life, navigating equity and health outcomes for them, it’s really scary because I don’t know. So before I cry, what do y’all have as opportunities and resources as you help someone age, and what that can look like in the space of life?
Barnes: So, thank you for being so vulnerable in talking about how incredibly challenging navigating the health care system and the systems that address nonmedical factors are for individuals. I don’t have an easy answer. There are organizations, and some that we have funded, that provide navigation services so that folks who know how to walk their way through these complicated systems can be helpful and maybe we can talk offline after we’re done. Again, they rely on trusted messengers in the communities who know what’s going on in the environment and then can actually help with the complicated side of things as well. And I think that’s probably the best bet for traversing something that doesn’t have to be as complicated as it is, but it is what it is at this point.
Meer Jumani: Do we have time for one more?
Barnes: We do.
Jumani: Perfect.
Rovner: Go ahead.
Jumani: So Meer Jumani, I work as a public health policy adviser to Commissioner Adrian Garcia, Harris County, Precinct 2. Sen. Alvarado’s District and Precinct 2 overlap a ton, but Precinct 2 has approximately 1.1 million constituents, of which 65% are Hispanic. We also have some of the most vast health disparities ranging from the highest mortality rate to the lowest home ownership rate. We touched on that amongst others, and despite launching programs ranging from free community-based clinics to lead abatement programs, we see a trend that these are most underutilized by the most vulnerable populations. So my question is, can you speak to what measures can be taken or what folks are not doing to change the mindset of these populations from a curative mindset to a preventative mindset?
Rice: I think it’s, as you mentioned before, trust, right? Those community navigators and making sure they’re out there giving voice to the community and sharing what resources are there. During covid, there was a community in northeast Georgia with a large immigrant population, and they actually ended up having some of the lowest rates of covid for the state because of those community navigators. They really hit the ground and it was kind of amazing what they did, going door to door if they had to, having weekly events and having conversations, making screenings accessible to everyone, and having navigators that spoke various different languages. I think those kind of things continue to help with that kind of outreach.
Anthony: I totally agree. And acknowledging painful history too. I think we have to realize who is tasked to do the fixing, and are we really giving agency and empowering those that need help the most? I’m thinking about particularly in Sikeston, Missouri, where the police chief tried to institute a program where people were to come, particularly Black residents in town. He wanted to have meetings with them and have conversations, but it just didn’t take off. But part of the reason why is because the level of mistrust, but also some acknowledgment of the history of racial violence that had gone on in the past in that community that people were still trying to heal from today. So I think that there’s so much work that has to be done in institutions. One of the first steps that they can take is acknowledging painful history as a way to move forward because we have to acknowledge our pain to have some joy too.
Rovner: I think that’s a wonderful place to leave it. I want to thank our panel so much and thank you to the audience for your great questions.
I hasten to add, if you enjoyed the podcast, you can subscribe wherever you get your podcasts. We’d always appreciate it if you left us a review; that helps other people find us, too. Special thanks, as always, to our technical guru back in Washington, D.C., Francis Ying, and our editor, Emmarie Huetteman. And thanks to the kind folks here at TribFest for helping us put this all together. We’ll be back in D.C. with our regular panel and all the news on Sept. 12. Until then, everyone, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
10 months 2 weeks ago
Multimedia, Public Health, Race and Health, States, Disparities, KFF Health News' 'What The Health?', Podcasts, texas
Inside Conservative Activist Leonard Leo’s Long Campaign To Gut Planned Parenthood
A federal lawsuit in Texas against Planned Parenthood has a web of ties to conservative activist Leonard Leo, whose decades-long effort to steer the U.S. court system to the right overturned Roe v. Wade, yielding the biggest rollback of reproductive health access in half a century.
A federal lawsuit in Texas against Planned Parenthood has a web of ties to conservative activist Leonard Leo, whose decades-long effort to steer the U.S. court system to the right overturned Roe v. Wade, yielding the biggest rollback of reproductive health access in half a century.
Brought by an anonymous whistleblower and later joined by Texas Attorney General Ken Paxton, the suit alleges the Planned Parenthood Federation of America and three Planned Parenthood affiliates defrauded the Texas and Louisiana Medicaid programs by collecting $17 million for services provided while it fought state efforts to remove it as an approved provider.
The suit claims violations of the False Claims Act, an obscure but powerful law protecting the government from fraud, and seeks $1.8 billion in penalties from Planned Parenthood, according to a motion that lawyers for the whistleblower filed in federal court in 2023.
The lawsuit builds on efforts over years by the religious right and politicians who oppose abortion to deliver blows to Planned Parenthood — which provides sexual and reproductive health care at nearly 600 sites nationwide — now bolstered by Leo’s work reshaping the American judiciary.
Anti-abortion groups and their allies secured a generational victory in 2022 when the Supreme Court overturned Roe v. Wade, which ended the constitutional right to abortion and paved the way for bans or severe restrictions in 20 states. The court challenge in Texas demonstrates how the forces behind the end of Roe threaten access to other health and family planning services.
The Planned Parenthood clinics being sued do not provide abortions. They are in Texas and Louisiana, which banned nearly all abortions, respectively, in 2021 and 2022.
Leo, an anti-abortion Catholic, is connected to the key players in the Texas lawsuit — the whistleblower plaintiff, an attorney general, and the judge — according to a KFF Health News review of tax records, court documents from multiple lawsuits, statements to lawmakers, and website archives.
Leo provided legal counsel to the anti-abortion group at its center, and he has financial and other connections to Paxton.
They filed the case in federal court in Amarillo, Texas, where Matthew Kacsmaryk is the only judge. He is a longtime member of the Federalist Society, the conservative legal juggernaut for which Leo has worked for over 25 years in various capacities and currently serves as co-chair.
Kacsmaryk’s rulings have curtailed access to reproductive health since the Senate confirmed him in 2019. He suspended the FDA’s approval of mifepristone, a drug used in medication abortion, propelling the issue to the Supreme Court, which ultimately threw out the case. In another case, Kacsmaryk ruled to limit young people’s access to birth control through a federal family planning program.
Leo did not respond to questions for this article and a spokesperson declined to comment. Through a court spokesperson, Kacsmaryk declined to comment for this article.
The anonymous whistleblower in 2021 accused the Planned Parenthood Federation of America and Planned Parenthood affiliates of defrauding the Medicaid programs of Texas and Louisiana. Paxton, who has repeatedly acted to thwart abortion rights and joined the case in 2022, alleges in the lawsuit that clinics received payments they weren’t entitled to from Texas Medicaid from early 2017 to early 2021 as the state was pushing to end Planned Parenthood’s status as a Medicaid provider. Louisiana and the Department of Justice have not joined the complaint.
The lawsuit’s origins go back a decade. The anonymous whistleblower, between 2013 and 2015, “conducted an undercover investigation to determine whether Planned Parenthood’s fetal tissue procurement practices were continuing, and if they were legal and/or ethical,” according to the whistleblower’s complaint filed in 2021.
The explanation mimics how the Center for Medical Progress, a California-based anti-abortion group founded by activist David Daleiden in 2013, has publicly described its work. “The Human Capital project is a 30-month-long investigative journalism study by The Center for Medical Progress, documenting how Planned Parenthood sells the body parts of aborted babies,” the group states on its website.
In a November 2022 court order, Kacsmaryk said the private party initiating the lawsuit is “the president of CMP,” the title Daleiden held at that time, according to a Center for Medical Progress tax filing.
The Center for Medical Progress and Daleiden did not respond to requests for comment.
By law, federal funds can’t pay for abortions unless the pregnancy threatens the life of a woman or is the result of rape or incest, but the program reimburses for other care such as contraception, screenings for sexually transmitted infections, and cancer screenings. Medicaid, which provides health coverage for people with low incomes, is jointly financed by states and the federal government.
According to its 2022-23 annual report, Planned Parenthood affiliate clinics provided 9.13 million health care services to 2.05 million patients nationally in 2022. Testing and treatment for sexually transmitted infections accounted for about half of those services, contraception amounted to a quarter, and abortions constituted 4%.
Planned Parenthood Gulf Coast, which operates clinics in Texas and Louisiana, is among the branches Paxton and the whistleblower are suing. From July 2022 to June 2023, its clinics provided patients more than 86,000 tests for sexually transmitted infections, 44,000 visits for birth control, and nearly 7,000 cancer screening and prevention services, CEO Melaney Linton told KFF Health News.
“All of these services and more are at risk in this politically motivated lawsuit,” Linton said. The lawsuit’s allegations “are false. Planned Parenthood did not commit Medicaid fraud.”
Linton has said the lawsuit’s purpose is clear: “trying to shut Planned Parenthood down.”
Texas terminated Planned Parenthood’s Medicaid participation in March 2021. Until then, affiliates “were entitled to receive reimbursement” for services to Medicaid patients because their provider agreements with Texas’ Medicaid program were valid, attorneys for the Planned Parenthood clinics wrote in a February 2023 court filing in support of their motion for summary judgment.
Louisiana has not removed Planned Parenthood from its Medicaid program.
Leo served as legal counsel to the Center for Medical Progress, according to documents produced as part of a separate lawsuit Planned Parenthood filed in federal court in California against the anti-abortion group. Among those, a July 2018 document lists 25 emails Leo and Daleiden traded in June and July 2015, including in the days before the anti-abortion group released its first video.
Paxton’s ties to Leo can be traced back at least a decade to when the former state senator and rising conservative star was about to begin his first term as attorney general.
In 2014, Leo, then executive vice president of the Federalist Society, was a rare non-Texan named to Paxton’s attorney general transition advisory team. Tax filings show that the Concord Fund, one of several Leo-linked groups that spend money to influence elections and aren’t required to disclose their donors, gave $20.3 million from July 2014 through June 2023 to the Republican Attorneys General Association, the political nonprofit that works to elect Republicans as states’ top law enforcement officers. Known as RAGA, the group funneled more than $1.2 million to Paxton’s campaign over three election cycles from 2014 to 2022, Texas campaign finance records show.
Texas government officials knew the state was reimbursing Planned Parenthood clinics for medical services from 2017 to 2021, which renders the state’s argument that clinics violated the False Claims Act “without merit,” said Jacob Elberg, a professor at Seton Hall Law School and an expert in health care fraud.
The law is intended for situations “where essentially someone submits a claim for payment or keeps money that they’re not entitled to where they have information that the government doesn’t have,” Elberg said. “And they essentially know that if the government knew the truth, the government wouldn’t pay them or would be demanding money back.”
But with Planned Parenthood, “everything involved here happened out in the open,” Elberg said. “They were submitting bills and the government knew what was going on and was paying those bills.”
The plaintiffs’ arguments are a “tortured use” of the False Claims Act, said Sarah Saldaña, a former U.S. attorney for the Northern District of Texas.
“Things like this, which have these obvious political overtones, tend to undermine further the view of the public of the judicial courts system,” Saldaña said.
The office of the attorney general did not respond to requests for comment.
Anti-abortion groups support the Paxton lawsuit even though abortion is essentially outlawed in the Lone Star State. Planned Parenthood “is still a pro-abortion organization,” said John Seago, president of Texas Right to Life. Even though Planned Parenthood provides other care, “all of those services are tainted by their pro-abortion mindset,” he said.
“Planned Parenthood is a danger to Texans. We wish that Planned Parenthood didn’t have a single location within our state,” Seago said. “Whenever the state pays Planned Parenthood to do something, even if it’s a good service, we are building up their brand and giving them more reach into our Texas communities.”
Roughly three dozen Planned Parenthood clinics in Texas continue to provide non-abortion services like birth control and STI screenings. The $1.8 billion the whistleblower is seeking is equivalent to nearly 90% of Planned Parenthood’s annual revenue, according to its most recent annual report.
The Campaign Against Planned Parenthood
The Center for Medical Progress was little known in 2015 when it began releasing videos containing explosive allegations that Planned Parenthood was illegally selling tissue from aborted fetuses, which Planned Parenthood denies.
The group and Daleiden had ties to powerful anti-abortion organizations. They include Live Action, where Daleiden worked before creating the Center for Medical Progress, and Operation Rescue, the Kansas-based group that staged demonstrations against George Tiller’s abortion clinic in that state before a gunman killed the physician in 2009.
“The evidence I am gathering deeply implicates Planned Parenthood affiliates across the country in multiple felonies and can trigger severe legal and financial consequences for PP and their associates, while providing new justifications for state defunding efforts and turning public opinion against Planned Parenthood and abortion,” Daleiden wrote in a May 2013 email produced as part of the litigation Planned Parenthood brought in California. The subject line: “Meeting to Take Down PP.”
Texas tried to remove Planned Parenthood clinics from its Medicaid program following the center’s release of the undercover videos, a move that was part of a larger political firestorm. Roughly a dozen states launched investigations into the reproductive health provider, and Republicans in Congress renewed calls to strip Planned Parenthood of government funding.
Paxton made his feelings clear about abortion as he pursued an investigation of Planned Parenthood in Texas. During a July 29, 2015, legislative hearing, he said “the true abomination in all of this is the institution of abortion.”
“We are rightfully horrified by what we’ve seen on these videos,” Paxton said. “However these videos also serve as a larger reminder that, as a society, we’ve turned a blind eye to the gruesome horrors that occur in abortion clinics across America every single day. They remind us that this industry as a whole has lost the perspective of humanity.”
Planned Parenthood denied selling fetal tissue and other claims in the videos, some of which contained graphic footage. It said the videos were “deceptive” and heavily edited to be misleading. A grand jury in Texas cleared Planned Parenthood of wrongdoing.
Daleiden worked on the center’s “Human Capital Project” for years, receiving advice from Leo and his associates, according to the Center for Medical Progress’ website, and Daleiden’s email correspondence and other documents produced as part of the separate lawsuit in federal court in California.
The July 2018 document filed as part of the litigation in California describes emails between Leo and Daleiden as “providing legal communication with counsel regarding legal planning” and “for counsel to provide legal advice regarding investigative journalism methods and the legality of fetal tissue procurement practices,” among other descriptions. Daleiden sent one email to Leo “regarding legal planning” on July 13, 2015, the day before the Center for Medical Progress released its first video.
A November 2018 letter from the Center for Medical Progress’ lawyers stated “CMP was receiving legal advice” from Leo, as well as other conservative lawyers and organizations. Lawyers representing the center and Daleiden in a December 2018 legal filing said Leo “provided legal advice on how to ensure successful prosecutions of the criminal actors which CMP identified.”
In its defense, Planned Parenthood has said it billed the Texas Medicaid program for reimbursement for “lawfully provided” services from February 2017 to March 2021 as a participating Medicaid provider in the state.
In 2015 and 2017, federal courts in Louisiana and Texas blocked those states from terminating Planned Parenthood’s Medicaid provider agreements. Judge John deGravelles of the U.S. District Court for the Middle District of Louisiana said the state was prohibited “from suspending Medicaid payments to [Planned Parenthood Gulf Coast] for services rendered to Medicaid beneficiaries.”
The 5th Circuit Court of Appeals in November 2020 vacated the Texas and Louisiana injunctions, but the court never weighed in on clawing back Medicaid funds that had been paid to clinics. Texas terminated Planned Parenthood in March 2021, following a state court ruling.
Texas and the whistleblower argue that, once the court injunctions were lifted, Planned Parenthood’s termination from each state’s Medicaid program became effective years earlier — 2015 in Louisiana and 2017 in Texas — due to the dates that state officials gave clinics final notice.
Planned Parenthood has argued that it is under no obligation to return payments received while injunctions were in place. Kacsmaryk disagrees. In a recently unsealed summary judgment order in the case, the judge wrote that Planned Parenthood clinics “had an obligation to repay the government payments they received as a matter of law.”
The order was unsealed after attorneys for the Reporters Committee for Freedom of the Press intervened. The committee argued the public has a presumptive and constitutional right to access judicial records, and that Kacsmaryk’s stated concerns — which included the tainting of a potential jury pool or jeopardizing the safety of those involved in the lawsuit — didn’t justify keeping the document secret.
Kacsmaryk’s brief justification for sealing the document, contained in the order itself, “was very thin,” said Katie Townsend, legal director for the Reporters Committee for Freedom of the Press.
She said his decision to seal such an important document was “highly unusual” and “very troubling.”
“Those orders are almost always completely public,” she said.
What Paxton Gains
Paxton has publicly toyed with the idea of pursuing federal office, and former President Donald Trump has said he’d consider him for U.S. attorney general should Trump return to the White House.
For Republicans in Texas, there are political benefits to going after Planned Parenthood, said Mark Jones, a political scientist at Rice University in Houston. “Doing anything punitive against Planned Parenthood and anything that would reduce the ability of Planned Parenthood to be active and effective in Texas is going to be greeted with near-universal consensus within the Republican primary electorate,” Jones said. “There’s no downside to it.”
The Republican Attorneys General Association, which can accept unlimited political donations that it distributes to candidates, is a Paxton supporter. Campaign finance records show it gave more than $730,000 to Paxton’s attorney general campaigns in 2014 and 2018.
Tax filings show that the Marble Freedom Trust, a political nonprofit where Leo serves as trustee and chair, gave the Concord Fund $100.9 million from May 2020 through April 2023. During the 2022 election cycle, the Concord Fund gave $6.5 million to RAGA, which then contributed $500,000 to Paxton’s campaign. It was tied as the highest contribution to the Texas attorney general, matched by a $500,000 contribution from a political action committee backed by conservative Texas billionaires, according to Transparency USA, a nonprofit that tracks spending in state politics.
RAGA has praised Leo’s role, calling him its “greatest champion.”
“Leonard Leo has helped shape the trajectory of RAGA and the conservative legal movement more than anyone else. As RAGA’s greatest champion, Leonard Leo reimagined the role of the state attorney general and promoted men and women dedicated to the persistence of the rule of law and the original meaning of the Constitution,” reads a RAGA website post from 2019 that has since been deleted.
“You want access to Leo because Leo gives you access to money,” said Chris Toth, former executive director of the National Association of Attorneys General.
In many conservative states like Texas, Toth said, “the issue is worrying about getting primaried. And that is where playing nice with Leonard Leo and the Concord Fund come in because if you’re on their side, basically, you’re going to have no problem getting reelected.”
The Concord Fund gave $4 million to RAGA between July 1, 2022, and June 30, 2023, four times what it gave the prior fiscal year.
Abortion rights supporters have warned that they anticipate ongoing reproductive health battles in Texas and beyond, with access to contraception, fertility services, and other types of care under threat.
As an example, some point to the Griswold v. Connecticut decision from 1965, in which the Supreme Court legalized the use of contraception among married couples. The high court ruled that a state law violated a constitutional right to privacy, a rationale that was central to Roe v. Wade eight years later.
In a 2017 speech at the Acton Institute, a conservative think tank, Leo criticized Griswold as a decision amounting to “the creation of rights found nowhere in the text or structure of the Constitution.”
The Planned Parenthood lawsuit in Texas is expected to go to trial, potentially this year. The central question is whether Planned Parenthood knowingly withheld money owed to the government.
All the while the public is expressing greater uncertainty about rights once considered constitutionally guaranteed. In a KFF poll conducted in February, 1 in 5 adults said the right to use contraception is threatened and likely to be overturned.
Fewer than half of adults considered it to be secure.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
11 months 1 week ago
Courts, States, Abortion, Contraception, Privacy, reproductive health, texas, Women's Health