Toxic Gas Adds to a Long History of Pollution in Southwest Memphis
MEMPHIS, Tenn. — For many years, Rose Sims had no idea what was going on inside a nondescript brick building on Florida Street a couple of miles from her modest one-story home on the southwestern side of town.
Like other residents, she got an unwelcome surprise in October 2022 at a public forum held by the Environmental Protection Agency at the historic Monumental Baptist Church, known for its role in the civil rights movement. The EPA notified the predominantly Black community that Sterilization Services of Tennessee —which began operations in the brick building in the 1970s — had been emitting unacceptably high levels of ethylene oxide, a toxic gas commonly used to disinfect medical devices.
Airborne emissions of the colorless gas can increase the risk of certain medical conditions, including breast cancer. Sims, who is 59 and Black, said she developed breast cancer in 2019, despite having no family history of it, and she suspects ethylene oxide was a contributing factor.
“I used to be outside a lot. I was in good health. All of a sudden, I got breast cancer,” she said.
Local advocates say the emissions are part of a pattern of environmental racism. The term is often applied when areas populated primarily by racial and ethnic minorities and members of low-socioeconomic backgrounds, like southwest Memphis, are burdened with a disproportionate amount of health hazards.
The drivers of environmental racism include the promise of tax breaks for industry to locate a facility in a heavily minority community, said Malini Ranganathan, an urban geographer at American University in Washington, D.C. The cheaper cost of land also is a factor, as is the concept of NIMBY — or “not in my backyard” — in which power brokers steer possible polluters to poorer areas of cities.
A manager at Sterilization Services’ corporate office in Richmond, Virginia, declined to answer questions from KFF Health News. An attorney with Leitner, Williams, Dooley & Napolitan, a law firm that represents the company, also declined to comment. Sterilization Services, in a legal filing asking for an ethylene oxide-related lawsuit to be dismissed, said the use of the gas, which sterilizes about half the medical devices in the U.S., is highly regulated to ensure public safety.
Besides southwest Memphis, there are nearly two dozen locales, mostly small cities — from Athens, Texas, to Groveland, Florida, and Ardmore, Oklahoma — where the EPA said in 2022 that plants sterilizing medical devices emit the gas at unusually high levels, potentially increasing a person’s risk of developing cancer.
The pollution issue is so bad in southwest Memphis that even though Sterilization Services planned to close shop by April 30, local community leaders have been hesitant to celebrate. In a letter last year to a local Congress member, the company said it has always complied with federal, state, and local regulations. The reason for its closure, it said, was a problem with renewing the building lease.
But many residents see it as just one small win in a bigger battle over environmental safety in the neighborhood.
“It’s still a cesspool of pollution,’’ said Yolonda Spinks, of the environmental advocacy organization Memphis Community Against Pollution, about a host of hazards the community faces.
The air in this part of the city has long been considered dangerous. An oil refinery spews a steady plume of white smoke. A coal plant, which is now closed, leaked components of coal ash, such as arsenic, into the ground and groundwater, according to a corrective action report from the Tennessee Valley Authority. The TVA is proposing to gut an existing gas plant and replace turbines in the facility with new ones. A continual stream of heavy trucks chug along nearby highways and roads. Other transportation sources of air pollution include the Memphis International Airport and barge traffic on the nearby Mississippi River.
Lead contamination is also a concern, not just in drinking water but in the soil from now-closed lead smelters, said Chunrong Jia, a professor of environmental health at the University of Memphis. Almost all the heavy industry in Shelby County — and the associated pollutants — are located in southwest Memphis, Jia added.
Sources of pollution are often “clustered in particular communities,” said Darya Minovi, a senior analyst with the Union of Concerned Scientists, a nonprofit that advocates for environmental justice. When it comes to sterilizing facilities that emit ethylene oxide, areas inhabited largely by Black, Hispanic, low-income, and non-English-speaking people are disproportionately exposed, the group has found.
Four sites that the EPA labeled high-risk are in low-income areas of Puerto Rico. Seven sterilizer plants operate in that U.S. territory.
The EPA, responding to public concerns and to deepened scientific understanding of the hazards of ethylene oxide, recently released rules that the agency said would greatly reduce emissions of the toxic gas from sterilizing facilities.
KeShaun Pearson, who was born and raised in south Memphis and has been active in fighting environmental threats, said he is frustrated that companies with dangerous emissions are allowed to create “toxic soup” in minority communities.
In the area where the sterilization plant is located, 87% of the residents are people of color, and, according to the Southern Environmental Law Center, life expectancy there is about 10 years lower than the average for the county and state. The population within 5 miles of the sterilizer plant is mostly low-income, according to the Union of Concerned Scientists.
Pearson was part of Memphis Community Against the Pipeline, a group formed in 2020 to stop a crude oil pipeline that would have run through Boxtown, a neighborhood established by emancipated slaves and freedmen after the signing of the Emancipation Proclamation of 1863.
That campaign, which received public support from former Vice President Al Gore and actress-activist Jane Fonda, succeeded. After the ethylene oxide danger surfaced in 2022, the group changed the last word of its name from “pipeline” to “pollution.”
Besides breast and lymphoid cancers, animal studies have linked inhaling the gas to tumors of the brain, lungs, connective tissue, uterus, and mammary glands.
Last year, with the help of the Southern Environmental Law Center, the south Memphis community group urged the Shelby County Health Department to declare the ethylene oxide situation a public health emergency and shut down the sterilizing plant. But the health department said the company had complied with its existing air permit and with the EPA’s rules and regulations.
A health department spokesperson, Joan Carr, said Shelby County enforces EPA regulations to ensure that companies comply with the federal Clean Air Act and that the agency has five air monitoring stations around the county to detect levels of other pollutants.
When the county and the Tennessee Department of Health did a cancer cluster study in 2023, the agencies found no evidence of the clustering of high rates of leukemia, non-Hodgkin lymphoma, or breast or stomach cancer near the facility. There were “hot and cold spots” of breast cancer found, but the study said it could not conclude that the clusters were linked to the facility.
Scientists have criticized the study’s methodology, saying it did not follow the Centers for Disease Control and Prevention’s recommendations for designing a cancer cluster investigation.
Meanwhile, several people have sued the sterilizing company, claiming their health has been affected by the ethylene oxide emissions. In a lawsuit seeking class-action status, Reginaé Kendrick, 21, said she was diagnosed with a brain tumor at age 6. Chemotherapy and radiation have stunted her growth, destroyed her hair follicles, and prevented her from going through puberty, said her mother, Robbie Kendrick.
In response to proposed stricter EPA regulations, meanwhile, the Tennessee attorney general helped lead 19 other state AGs in urging the agency to “forgo or defer regulating the use of EtO by commercial sterilizers.”
Sims said she’s glad her neighborhood will have one less thing to worry about once Sterilization Services departs. But her feelings about the closure remain tempered.
“Hope they don’t go to another residential area,” she said.
[Clarification: This article was updated at 3:15 p.m. ET on May 1, 2024, to specify which substances leaked into the ground and groundwater and what changes will occur related to the Tennessee Valley Authority’s activities in Shelby County, Tennessee.]
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 1 month ago
Public Health, Race and Health, States, Disparities, Environmental Health, Florida, Oklahoma, Tennessee, texas, Virginia
Rare human case of highly contagious bird flu confirmed in Texas
The Centers for Disease Control and Prevention announced Monday that a person in Texas has tested positive for highly pathogenic avian influenza, otherwise known as H5N1 bird flu.
The Centers for Disease Control and Prevention announced Monday that a person in Texas has tested positive for highly pathogenic avian influenza, otherwise known as H5N1 bird flu.
"This person had exposure to dairy cattle in Texas presumed to be infected with HPAI A(H5N1) viruses. The patient reported eye redness (consistent with conjunctivitis), as their only symptom, and is recovering," the CDC said in a statement. "The patient was told to isolate and is being treated with an antiviral drug for flu."
The CDC said this is the second case of a human testing positive for H5N1 in the United States, after a previous case was observed in Colorado in 2022.
"This infection does not change the H5N1 bird flu human health risk assessment for the U.S. general public, which CDC considers to be low," it added. "However, people with close or prolonged, unprotected exposures to infected birds or other animals (including livestock), or to environments contaminated by infected birds or other animals, are at greater risk of infection."
US TUBERCULOSIS CASES IN 2023 WERE AT HIGHEST LEVEL IN A DECADE, CDC SAYS
Last week, dairy cows in Texas and Kansas were reported to be infected with bird flu – and federal agriculture officials later confirmed infections in a Michigan dairy herd that had recently received cows from Texas.
This bird flu was first identified as a threat to people during a 1997 outbreak in Hong Kong, according to the Associated Press. More than 460 people have died in the past two decades from bird flu infections, the World Health Organization says.
PUERTO RICO HEALTH OFFICIALS DECLARE DENGUE FEVER A PUBLIC HEALTH EMERGENCY
Texas officials did not identify the newly infected person, nor release any details about what brought them in contact with the cows.
The CDC said it is "working with state health departments to continue to monitor workers who may have been in contact with infected or potentially infected birds/animals and test those people who develop symptoms."
"Human illnesses with H5N1 bird flu have ranged from mild (e.g., eye infection, upper respiratory symptoms) to severe illness (e.g., pneumonia) that have resulted in death in other countries," the CDC also said.
The Associated Press contributed to this report.
1 year 2 months ago
infectious-disease, texas, Health
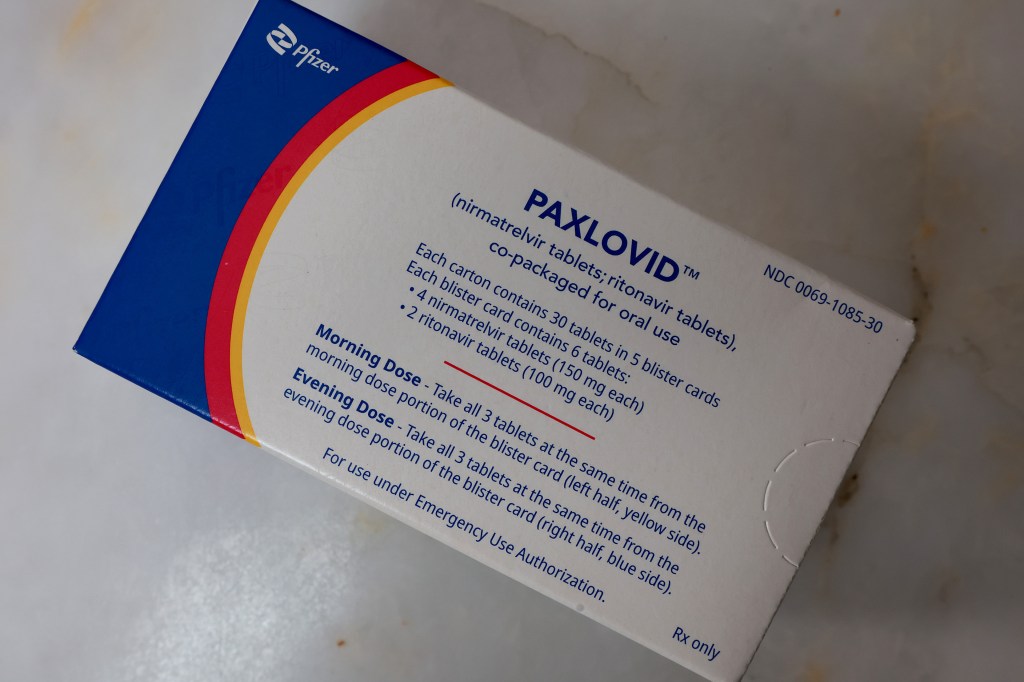
Why Covid Patients Who Could Most Benefit From Paxlovid Still Aren’t Getting It
Evangelical minister Eddie Hyatt believes in the healing power of prayer but “also the medical approach.” So on a February evening a week before scheduled prostate surgery, he had his sore throat checked out at an emergency room near his home in Grapevine, Texas.
A doctor confirmed that Hyatt had covid-19 and sent him to CVS with a prescription for the antiviral drug Paxlovid, the generally recommended medicine to fight covid. Hyatt handed the pharmacist the script, but then, he said, “She kept avoiding me.”
She finally looked up from her computer and said, “It’s $1,600.”
The generally healthy 76-year-old went out to the car to consult his wife about their credit card limits. “I don’t think I’ve ever spent more than $20 on a prescription,” the astonished Hyatt recalled.
That kind of sticker shock has stunned thousands of sick Americans since late December, as Pfizer shifted to commercial sales of Paxlovid. Before then, the federal government covered the cost of the drug.
The price is one reason Paxlovid is not reaching those who need it most. And patients who qualify for free doses, which Pfizer offers under an agreement with the federal government, often don’t realize it or know how to get them.
“If you want to create a barrier to people getting a treatment, making it cost a lot is the way to do it,” said William Schaffner, a professor at Vanderbilt University School of Medicine and spokesperson for the National Foundation for Infectious Diseases.
Public and medical awareness of Paxlovid’s benefits is low, and putting people through an application process to get the drug when they’re sick is a non-starter, Schaffner said. Pfizer says it takes only five minutes online.
It’s not an easy drug to use. Doctors are wary about prescribing it because of dangerous interactions with common drugs that treat cholesterol, blood clots, and other conditions. It must be taken within five days of the first symptoms. It leaves a foul taste in the mouth. In one study, 1 in 5 patients reported “rebound” covid symptoms a few days after finishing the medicine — though rebound can also occur without Paxlovid.
A recent JAMA Network study found that sick people 85 and older were less likely than younger Medicare patients to get covid therapies like Paxlovid. The drug might have prevented up to 27,000 deaths in 2022 if it had been allocated based on which patients were at highest risk from covid. Nursing home patients, who account for around 1 in 6 U.S. covid deaths, were about two-thirds as likely as other older adults to get the drug.
Shrunken confidence in government health programs is one reason the drug isn’t reaching those who need it. In senior living facilities, “a lack of clear information and misinformation” are “causing residents and their families to be reluctant to take the necessary steps to reduce covid risks,” said David Gifford, chief medical officer for an association representing 14,000 health care providers, many in senior care.
The anti-vaxxers spreading falsehoods about vaccines have targeted Paxlovid as well. Some call themselves anti-paxxers.
“Proactive and health-literate people get the drug. Those who are receiving information more passively have no idea whether it’s important or harmful,” said Michael Barnett, a primary care physician at Brigham and Women’s Hospital and an associate professor at Harvard, who led the JAMA Network study.
In fact, the drug is still free for those who are uninsured or enrolled in Medicare, Medicaid, or other federal health programs, including those for veterans.
That’s what rescued Hyatt, whose Department of Veterans Affairs health plan doesn’t normally cover outpatient drugs. While he searched on his phone for a solution, the pharmacist’s assistant suddenly appeared from the store. “It won’t cost you anything!” she said.
As Hyatt’s case suggests, it helps to know to ask for free Paxlovid, although federal officials say they’ve educated clinicians and pharmacists — like the one who helped Hyatt — about the program.
“There is still a heaven!” Hyatt replied. After he had been on Paxlovid for a few days his symptoms were gone and his surgery was rescheduled.
About That $1,390 List Price
Pfizer sold the U.S. government 23.7 million five-day courses of Paxlovid, produced under an FDA emergency authorization, in 2021 and 2022, at a price of around $530 each.
Under the new agreement, Pfizer commits to provide the drug for the beneficiaries of the government insurance programs. Meanwhile, Pfizer bills insurers for some portion of the $1,390 list price. Some patients say pharmacies have quoted them prices of $1,600 or more.
How exactly Pfizer arrived at that price isn’t clear. Pfizer won’t say. A Harvard study last year estimated the cost of producing generic Paxlovid at about $15 per treatment course, including manufacturing expenses, a 10% profit markup, and 27% in taxes.
Pfizer reported $12.5 billion in Paxlovid and covid vaccine sales in 2023, after a $57 billion peak in 2022. The company’s 2024 Super Bowl ad, which cost an estimated $14 million to place, focused on Pfizer’s cancer drug pipeline, newly reinforced with its $43 billion purchase of biotech company Seagen. Unlike some other recent oft-aired Pfizer ads (“If it’s covid, Paxlovid”), it didn’t mention covid products.
Connecting With Patients
The other problem is getting the drug where it is needed. “We negotiated really hard with Pfizer to make sure that Paxlovid would be available to Americans the way they were accustomed to,” Department of Health and Human Services Secretary Xavier Becerra told reporters in February. “If you have private insurance, it should not cost you much money, certainly not more than $100.”
Yet in nursing homes, getting Paxlovid is particularly cumbersome, said Chad Worz, CEO of the American Society of Consultant Pharmacists, specialists who provide medicines to care homes.
If someone in long-term care tests positive for covid, the nurse tells the physician, who orders the drug from a pharmacist, who may report back that the patient is on several drugs that interact with Paxlovid, Worz said. Figuring out which drugs to stop temporarily requires further consultations while the time for efficacious use of Paxlovid dwindles, he said.
His group tried to get the FDA to approve a shortcut similar to the standing orders that enable pharmacists to deliver anti-influenza medications when there are flu outbreaks in nursing homes, Worz said. “We were close,” he said, but “it just never came to fruition.” “The FDA is unable to comment,” spokesperson Chanapa Tantibanchachai said.
Los Angeles County requires nursing homes to offer any covid-positive patient an antiviral, but the Centers for Medicare & Medicaid Services, which oversees nursing homes nationwide, has not issued similar guidance. “And this is a mistake,” said Karl Steinberg, chief medical officer for two nursing home chains with facilities in San Diego County, which also has no such mandate. A requirement would ensure the patient “isn’t going to fall through the cracks,” he said.
While it hasn’t ordered doctors to prescribe Paxlovid, CMS on Jan. 4 issued detailed instructions to health insurers urging swift approval of Paxlovid prescriptions, given the five-day window for the drug’s efficacy. It also “encourages” plans to make sure pharmacists know about the free Paxlovid arrangement.
Current covid strains appear less virulent than those that circulated earlier in the pandemic, and years of vaccination and covid infection have left fewer people at risk of grave outcomes. But risk remains, particularly among older seniors, who account for most covid deaths, which number more than 13,500 so far this year in the U.S.
Steinberg, who sees patients in 15 residences, said he orders Paxlovid even for covid-positive patients without symptoms. None of the 30 to 40 patients whom he prescribed the drug in the past year needed hospitalization, he said; two stopped taking it because of nausea or the foul taste, a pertinent concern in older people whose appetites already have ebbed.
Steinberg said he knew of two patients who died of covid in his companies’ facilities this year. Neither was on Paxlovid. He can’t be sure the drug would have made a difference, but he’s not taking any chances. The benefits, he said, outweigh the risks.
Reporter Colleen DeGuzman contributed to this report.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 3 months ago
COVID-19, Pharmaceuticals, Public Health, Misinformation, Pandemic Disparities, texas
Pregnancy Care Was Always Lacking in Jails. It Could Get Worse.
It was about midnight in June 2022 when police officers showed up at Angela Collier’s door and told her that someone anonymously requested a welfare check because they thought she might have had a miscarriage.
Standing in front of the concrete steps of her home in Midway, Texas, Collier, initially barefoot and wearing a baggy gray T-shirt, told officers she planned to see a doctor in the morning because she had been bleeding.
Police body camera footage obtained by KFF Health News through an open records request shows that the officers then told Collier — who was 29 at the time and enrolled in online classes to study psychology — to turn around.
Instead of taking her to get medical care, they handcuffed and arrested her because she had outstanding warrants in a neighboring county for failing to appear in court to face misdemeanor drug charges three weeks earlier. She had missed that court date, medical records show, because she was at a hospital receiving treatment for pregnancy complications.
Despite her symptoms and being about 13 weeks pregnant, Collier spent the next day and a half in the Walker County Jail, about 80 miles north of Houston. She said her bleeding worsened there and she begged repeatedly for medical attention that she didn’t receive, according to a formal complaint she filed with the Texas Commission on Jail Standards.
“There wasn’t anything I could do,” she said, but “just lay there and be scared and not know what was going to happen.”
Collier’s experience highlights the limited oversight and absence of federal standards for reproductive care for pregnant women in the criminal justice system. Incarcerated people have a constitutional right to health care, yet only a half-dozen states have passed laws guaranteeing access to prenatal or postpartum medical care for people in custody, according to a review of reproductive health care legislation for incarcerated people by a research group at Johns Hopkins School of Medicine. And now abortion restrictions might be putting care further out of reach.
Collier’s arrest was “shocking and disturbing” because officers “blithely” took her to jail despite her miscarriage concerns, said Wanda Bertram, a spokesperson for the Prison Policy Initiative, a nonprofit organization that studies incarceration. Bertram reviewed the body cam footage and Collier’s complaint.
“Police arrest people who are in medical emergencies all the time,” she said. “And they do that regardless of the fact that the jail is often not equipped to care for those people in the way an emergency room might be.”
After a decline during the first year of the pandemic, the number of women in U.S. jails is once again rising, hitting nearly 93,000 in June 2022, a 33% increase over 2020, according to the Department of Justice. Tens of thousands of pregnant women enter U.S. jails each year, according to estimates by Carolyn Sufrin, an associate professor of gynecology and obstetrics at Johns Hopkins School of Medicine, who researches pregnancy care in jails and prisons.
The health care needs of incarcerated women have “always been an afterthought,” said Dana Sussman, deputy executive director at Pregnancy Justice, an organization that defends women who have been charged with crimes related to their pregnancy, such as substance use. For example, about half of states don’t provide free menstrual products in jails and prisons. “And then the needs of pregnant women are an afterthought beyond that,” Sussman said.
Researchers and advocates worry that confusion over recent abortion restrictions may further complicate the situation. A nurse cited Texas’ abortion laws as one reason Collier didn’t need care, according to her statement to the standards commission.
Texas law allows treatment of miscarriage and ectopic pregnancies, a life-threatening condition in which a fertilized egg implants outside the uterus. However, different interpretations of the law can create confusion.
A nurse told Collier that “hospitals no longer did dilation and curettage,” Collier told the commission. “Since I wasn’t hemorrhaging to the point of completely soaking my pants, there wasn’t anything that could be done for me,” she said.
Collier testified that she saw a nurse only once during her stay in jail, even after she repeatedly asked jail staffers for help. The nurse checked her temperature and blood pressure and told her to put in a formal request for Tylenol. Collier said she completed her miscarriage shortly after being released.
Collier’s case is a “canary in a coal mine” for what is happening in jails; abortion restrictions are “going to have a huge ripple effect on a system already unequipped to handle obstetric emergencies,” Sufrin said.
‘There Are No Consequences’
Jail and prison health policies vary widely around the country and often fall far short of the American College of Obstetricians and Gynecologists’ guidelines for reproductive health care for incarcerated people. ACOG and other groups recommend that incarcerated women have access to unscheduled or emergency obstetric visits on a 24-hour basis and that on-site health care providers should be better trained to recognize pregnancy problems.
In Alabama, where women have been jailed for substance use during pregnancy, the state offers pregnancy tests in jail. But it doesn’t guarantee a minimum standard of prenatal care, such as access to extra food and medical visits, according to Johns Hopkins’ review.
Policies for pregnant women at federal facilities also don’t align with national standards for nutrition, safe housing, and access to medical care, according to a 2021 report from the Government Accountability Office.
Even when laws exist to ensure that incarcerated pregnant women have access to care, the language is often vague, leaving discretion to jail personnel.
Since 2020, Tennessee law has required that jails and prisons provide pregnant women “regular prenatal and postpartum care, as necessary.” But last August a woman gave birth in a jail cell after seeking medical attention for more than an hour, according to the Montgomery County Sheriff’s Office.
Pregnancy complications can quickly escalate into life-threatening situations, requiring more timely and specialized care than jails can often provide, said Sufrin. And when jails fail to comply with laws on the books, little oversight or enforcement may exist.
In Louisiana, many jails didn’t consistently follow laws that aimed to improve access to reproductive health care, such as providing free menstrual items, according to a May 2023 report commissioned by state lawmakers. The report also said jails weren’t transparent about whether they followed other laws, such as prohibiting the use of solitary confinement for pregnant women.
Krishnaveni Gundu, as co-founder of the Texas Jail Project, which advocates for people held in county jails, has lobbied for more than a decade to strengthen state protections for pregnant incarcerated people.
In 2019, Texas became one of the few states to require that jails’ health policies include obstetrical and gynecological care. The law requires jails to promptly transport a pregnant person in labor to a hospital, and additional regulations mandate access to medical and mental health care for miscarriages and other pregnancy complications.
But Gundu said lack of oversight and meaningful enforcement mechanisms, along with “apathy” among jail employees, have undermined regulatory protections.
“All those reforms feel futile,” said Gundu, who helped Collier prepare for her testimony. “There are no consequences.”
Before her arrest, Collier had been to the hospital twice that month experiencing pregnancy complications, including a bladder infection, her medical records show. Yet the commission found that Walker County Jail didn’t violate minimum standards. The commission did not consider the police body cam footage or Collier’s personal medical records, which support her assertions of pregnancy complications, according to investigation documents obtained by KFF Health News via an open records request.
In making its determination, the commission relied mainly on the jail’s medical records, which note that Collier asked for medical attention for a miscarriage once, in the morning on the day she was released, and refused Tylenol.
“Your complaint of no medical care is unfounded,” the commission concluded, “and no further action will be taken.”
Collier’s miscarriage had ended before she entered the jail, argued Lt. Keith DeHart, jail lieutenant for the Walker County Sheriff’s Office. “I believe there was some misunderstanding,” he said.
Brandon Wood, executive director of the commission, wouldn’t comment on Collier’s case but defends the group’s investigation as thorough. Jails “have a duty to ensure that those records are accurate and truthful,” he said. And most Texas jails are complying with heightened standards, he said.
Bertram disagrees, saying the fact that care was denied to someone who was begging for it speaks volumes. “That should tell you something about what these standards are worth,” she said.
Last year, Chiree Harley spent six weeks in a Comal County, Texas, jail shortly after discovering she was pregnant and before she could get prenatal care, she said.
I was “thinking that I was going to be well taken care of,” said Harley, 37, who also struggled with substance use.
Jail officials put her in the infirmary, Harley said, but she saw only a jail doctor and never visited an OB-GYN, even though she had previous pregnancy complications including losing multiple pregnancies at around 21 weeks. This time she had no idea how far along she was.
She said that she started leaking amniotic fluid and having contractions on Nov. 1, but that jail officials waited nearly two days to take her to a hospital. Harley said officers forced her to sign papers releasing her from jail custody while she was having contractions in the hospital. Harley delivered at 23 weeks; the baby boy died less than a day later in her arms.
The whole experience was “very scary,” Harley said. “Afterwards we were all very, very devastated.”
Comal County declined to send Harley’s medical and other records in response to an open records request. Michael Shaunessy, a partner at McGinnis Lochridge who represents Comal County, said in a statement that, “at all times, the Comal County Jail provided Chiree Harley with all appropriate and necessary medical treatment for her and her unborn child.” He did not respond to questions about whether Harley was provided specialized obstetric care.
‘I Trusted Those People’
In states like Idaho, Mississippi, and Louisiana that installed near-total abortion bans after the Supreme Court eliminated the constitutional right to abortion in 2022, some patients might have to wait until no fetal cardiac activity is detected before they can get care, said Kari White, the executive and scientific director of Resound Research for Reproductive Health.
White co-authored a recent study that documented 50 cases in which pregnancy care deviated from the standard because of abortion restrictions even outside of jails and prisons. Health care providers who worry about running afoul of strict laws might tell patients to go home and wait until their situations worsen.
“Obviously, it’s much trickier for people who are in jail or in prison, because they are not going to necessarily be able to leave again,” she said.
Advocates argue that boosting oversight and standards is a start, but that states need to find other ways to manage pregnant women who get caught in the justice system.
For many pregnant people, even a short stay in jail can cause lasting trauma and interrupt crucial prenatal care.
Collier remembers being in “disbelief” when she was first arrested but said she was not “distraught.”
“I figured I would be taken care of, that nothing bad was gonna happen to me,” she said. As it became clear that she wouldn’t get care, she grew distressed.
After her miscarriage, Collier saw a mental health specialist and started medication to treat depression. She hasn’t returned to her studies, she said.
“I trusted those people,” Collier said about the jail staff. “The whole experience really messed my head up.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 3 months ago
States, Alabama, Idaho, Louisiana, Mississippi, Pregnancy, Prison Health Care, Tennessee, texas, Women's Health
Ouch. That ‘Free’ Annual Checkup Might Cost You. Here’s Why.
When Kristy Uddin, 49, went in for her annual mammogram in Washington state last year, she assumed she would not incur a bill because the test is one of the many preventive measures guaranteed to be free to patients under the 2010 Affordable Care Act.
The ACA’s provision made medical and economic sense, encouraging Americans to use screening tools that could nip medical problems in the bud and keep patients healthy.
So when a bill for $236 arrived, Uddin — an occupational therapist familiar with the health care industry’s workings — complained to her insurer and the hospital. She even requested an independent review.
“I’m like, ‘Tell me why am I getting this bill?’” Uddin recalled in an interview. The unsatisfying explanation: The mammogram itself was covered, per the ACA’s rules, but the fee for the equipment and the facility was not.
That answer was particularly galling, she said, because, a year earlier, her “free” mammogram at the same health system had generated a bill of about $1,000 for the radiologist’s reading. Though she fought that charge (and won), this time she threw in the towel and wrote the $236 check. But then she dashed off a submission to the KFF Health News-NPR “Bill of the Month” project:
“I was really mad — it’s ridiculous,” she later recalled. “This is not how the law is supposed to work.”
The ACA’s designers might have assumed that they had spelled out with sufficient clarity that millions of Americans would no longer have to pay for certain types of preventive care, including mammograms, colonoscopies, and recommended vaccines, in addition to doctor visits to screen for disease. But the law’s authors didn’t reckon with America’s ever-creative medical billing juggernaut.
Over the past several years, the medical industry has eroded the ACA’s guarantees, finding ways to bill patients in gray zones of the law. Patients going in for preventive care, expecting that it will be fully covered by insurance, are being blindsided by bills, big and small.
The problem comes down to deciding exactly what components of a medical encounter are covered by the ACA guarantee. For example, when do conversations between doctor and patient during an annual visit for preventive services veer into the treatment sphere? What screenings are needed for a patient’s annual visit?
A healthy 30-year-old visiting a primary care provider might get a few basic blood tests, while a 50-year-old who is overweight would merit additional screening for Type 2 diabetes.
Making matters more confusing, the annual checkup itself is guaranteed to be “no cost” for women and people age 65 and older, but the guarantee doesn’t apply for men in the 18-64 age range — though many preventive services that require a medical visit (such as checks of blood pressure or cholesterol and screens for substance abuse) are covered.
No wonder what’s covered under the umbrella of prevention can look very different to medical providers (trying to be thorough) and billers (intent on squeezing more dollars out of every medical encounter) than it does to insurers (who profit from narrower definitions).
For patients, the gray zone has become a billing minefield. Here are a few more examples, gleaned from the Bill of the Month project in just the past six months:
Peter Opaskar, 46, of Texas, went to his primary care doctor last year for his preventive care visit — as he’d done before, at no cost. This time, his insurer paid $130.81 for the visit, but he also received a perplexing bill for $111.81. Opaskar learned that he had incurred the additional charge because when his doctor asked if he had any health concerns, he mentioned that he was having digestive problems but had already made an appointment with his gastroenterologist. So, the office explained, his visit was billed as both a preventive physical and a consultation. “Next year,” Opasker said in an interview, if he’s asked about health concerns, “I’ll say ‘no,’ even if I have a gunshot wound.”
Kevin Lin, a technology specialist in Virginia in his 30s, went to a new primary care provider to take advantage of the preventive care benefit when he got insurance; he had no physical complaints. He said he was assured at check-in that he wouldn’t be charged. His insurer paid $174 for the checkup, but he was billed an additional $132.29 for a “new patient visit.” He said he has made many calls to fight the bill, so far with no luck.
Finally, there’s Yoori Lee, 46, of Minnesota, herself a colorectal surgeon, who was shocked when her first screening colonoscopy yielded a bill for $450 for a biopsy of a polyp — a bill she knew was illegal. Federal regulations issued in 2022 to clarify the matter are very clear that biopsies during screening colonoscopies are included in the no-cost promise. “I mean, the whole point of screening is to find things,” she said, stating, perhaps, the obvious.
Though these patient bills defy common sense, room for creative exploitation has been provided by the complex regulatory language surrounding the ACA. Consider this from Ellen Montz, deputy administrator and director of the Center for Consumer Information and Insurance Oversight at the Centers for Medicare & Medicaid Services, in an emailed response to queries and an interview request on this subject: “If a preventive service is not billed separately or is not tracked as individual encounter data separately from an office visit and the primary purpose of the office visit is not the delivery of the preventive item or service, then the plan issuer may impose cost sharing for the office visit.”
So, if the doctor decides that a patient’s mention of stomach pain does not fall under the umbrella of preventive care, then that aspect of the visit can be billed separately, and the patient must pay?
And then there’s this, also from Montz: “Whether a facility fee is permitted to be charged to a consumer would depend on whether the facility usage is an integral part of performing the mammogram or an integral part of any other preventive service that is required to be covered without cost sharing under federal law.”
But wait, how can you do a mammogram or colonoscopy without a facility?
Unfortunately, there is no federal enforcement mechanism to catch individual billing abuses. And agencies’ remedies are weak — simply directing insurers to reprocess claims or notifying patients they can resubmit them.
In the absence of stronger enforcement or remedies, CMS could likely curtail these practices and give patients the tools to fight back by offering the sort of clarity the agency provided a few years ago regarding polyp biopsies — spelling out more clearly what comes under the rubric of preventive care, what can be billed, and what cannot.
The stories KFF Health News and NPR receive are likely just the tip of an iceberg. And while each bill might be relatively small compared with the stunning $10,000 hospital bills that have become all too familiar in the United States, the sorry consequences are manifold. Patients pay bills they do not owe, depriving them of cash they could use elsewhere. If they can’t pay, those bills might end up with debt-collection agencies and, ultimately, harm their credit score.
Perhaps most disturbing: These unexpected bills might discourage people from seeking preventive screenings that could be lifesaving, which is why the ACA deemed them “essential health benefits” that should be free.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 4 months ago
Health Care Costs, Health Industry, Legislation, Minnesota, Obamacare Plans, Preventive Services, texas, Virginia, Washington
KFF Health News' 'What the Health?': New Year, Same Abortion Debate
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
It’s a new year, but the abortion debate is raging like it’s 2023, with a new federal appeals court ruling that doctors in Texas don’t have to provide abortions in medical emergencies, despite a federal requirement to the contrary. The case, similar to one in Idaho, is almost certainly headed for the Supreme Court. Meanwhile, Congress returns to Washington with only days to avert a government shutdown by passing either full-year or temporary spending bills. And with almost no progress toward a spending deal since the last temporary bill passed in November, this time a shutdown might well happen.
This week’s panelists are Julie Rovner of KFF Health News, Lauren Weber of The Washington Post, Shefali Luthra of The 19th, and Victoria Knight of Axios.
Panelists
Victoria Knight
Axios
Shefali Luthra
The 19th
Lauren Weber
The Washington Post
Among the takeaways from this week’s episode:
- New year, same Congress. It’s likely lawmakers will fall short of their early-year goals to pass necessary spending bills, prompting another government shutdown or yet another short-term extension. And funding for pediatric medical training is among the latest casualties of the clash over gender-affirming care, raising the odds of a political fight over the federal health budget.
- The emergency abortion care decision out of Texas this week underscores the difficult position health care providers are in: Now, a doctor could be brought up on charges in Texas for performing an abortion in a medical emergency — or brought up on federal charges if they abstain.
- A new law in California makes it easier for out-of-state doctors to receive reproductive health training there, a change that could benefit medical residents in the 18 states where it is effectively impossible to be trained to perform an abortion. But some doctors say they still fear breaking another state’s laws.
- Another study raises questions about the quality of care at hospitals purchased by private equity firms, an issue that has drawn the Biden administration’s attention. From the Journal of the American Medical Association, new findings show that those private equity-owned hospitals experienced a 25% increase in adverse patient events from three years before they were purchased to three years after.
- And “This Week in Medical Misinformation”: Robert F. Kennedy Jr. earned PolitiFact’s 2023 Lie of the Year designation for his “campaign of conspiracy theories.” The anti-vaccination message he espouses has been around a while, but the movement is gaining political traction — including in statehouses, where more candidates who share RFK Jr.’s views are winning elections.
Also this week, Rovner interviews Sandro Galea, dean of the Boston University School of Public Health, about how public health can regain the public’s trust.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: Politico’s “Why Democrats Can’t Rely on Abortion Ballot Initiatives to Help Them Win,” by Alice Miranda Ollstein, Jessica Piper, and Madison Fernandez.
Lauren Weber: The Washington Post’s “Can the Exhausted, Angry People of Ottawa County Learn to Live Together?” by Greg Jaffe.
Victoria Knight: Politico’s “Georgia Offered Medicaid With a Work Requirement. Few Have Signed Up.” by Megan Messerly and Robert King.
Shefali Luthra: Stat News’ “Medical Marijuana Companies Are Using Pharma’s Sales Tactics With Little of the Same Scrutiny,” by Nicholas Florko.
Also mentioned in this week’s episode:
- Law Dork’s “ADF Is Providing Free Legal Representation to Idaho in Anti-Abortion, Anti-Trans Cases,” by Chris Geidner.
- JAMA Network Open’s “Barriers to Family Building Among Physicians and Medical Students,” by Zoe King, Qiang Zhang, Jane Liang, et al.
- The Journal of the American Medical Association’s “Changes in Hospital Adverse Events and Patient Outcomes Associated With Private Equity Acquisition,” by Sneha Kannan, Joseph Dov Bruch, and Zirui Song.
- KFF Health News’ “RFK Jr.’s Campaign of Conspiracy Theories Is PolitiFact’s 2023 Lie of the Year,” by Madison Czopek, PolitiFact, and Katie Sanders, PolitiFact.
click to open the transcript
Transcript: New Year, Same Abortion Debate
KFF Health News’ ‘What the Health?’Episode Title: New Year, Same Abortion DebateEpisode Number: 328Published: Jan. 4, 2024
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello, Happy New Year, and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News. And I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, Jan. 4, at 10 a.m. As always, news happens fast, and things might have changed by the time you hear this, so here we go. Today we are joined via video conference by Lauren Weber of The Washington Post.
Lauren Weber: Hello, hello.
Rovner: Victoria Knight of Axios News.
Victoria Knight: Hey, everyone.
Rovner: And Shefali Luthra of The 19th.
Shefali Luthra: Hello.
Rovner: An entire panel of KFF Health News alums. I’m pretty sure that is a first. Later in this episode, we’ll have my interview with Boston University School of Public Health dean Dr. Sandro Galea. He has a new and pretty provocative prescription for how public health can regain public trust. But first, there was plenty of news over the holiday break, in addition to my Michigan Wolverines going to the national championship — sorry, Lauren — plenty of health news, that is. So we shall get to it. We will start on Capitol Hill, where Congress is poised to come back into session — apparently no closer to a deal on the appropriations bills that keep the government open than they were when they left for Christmas, and now it’s only two weeks until the latest continuing resolution ends. Victoria, are we looking at a shutdown again?
Knight: I was texting a lot of people yesterday trying to feel out the vibes. I think a lot of people think a shutdown seems pretty likely. A reminder that we have another member of Congress that is leaving on the Republican side in the House, so now the Republicans can only lose two votes if they’re trying to pass a bill. So when you have House Freedom Caucus members saying, “Hey, we don’t want to agree to any appropriations bills without doing something about the border,” and Democrats unlikely to agree to any border demands that the Freedom Caucus is wanting, it seems like we may be at a standstill. I know there is some reporting this morning that possibly they may just do another fiscal year continuing resolution until …
Rovner: You mean like the last couple of years we’ve done a full-year CR?
Knight: Yeah, exactly. So …
Rovner: The thing they swore they wouldn’t do.
Knight: And [House] Speaker [Mike] Johnson said, he promised he wouldn’t do that, so it’ll be interesting to see how that all plays out. As far as I’ve heard the latest, there’s no top-line funding number, but it does seem like a shutdown may be looming.
Rovner: Well, assuming there is a spending deal at some point, and the fact that 2024 is an election year where not much gets passed, a lot of lawmakers have a lot of things they would like to attach to a moving spending train, assuming there is a moving spending train. What’s the outlook for the bill that we were talking about all of December on PBMs [pharmacy benefit managers] and health transparency and some extensions of some expiring programs That’s still kicking around, right?
Knight: Yeah. That’s definitely still kicking around. So there are some extenders like for community health centers and averting some cuts to safety-net hospitals. Those are really high priority for lawmakers. I think those will make their way onto any kind of deal most likely. What seems more up in the air is the transparency measures for PBMs and for hospitals and for insurers. That was the big, as you mentioned, the big pass the House in December. The Senate has introduced their own versions of the bill and there’s talk that maybe some of that could ride onto if there is some kind of funding deal, but it’s also possible that maybe it’s more likely to be punted to the lame duck session. So, post-election, when Republicans are trying in the House and Senate Democrats are trying to do their last hurrah before the new Congress comes in. So we’ll see. Latest I heard yesterday there were some negotiations around the transparency stuff, so it’s still possible, but who knows?
Rovner: Congress is the ultimate college student. They don’t do anything until they have a deadline. Meanwhile, we have yet another health program caught up in the culture wars, this time the Children’s Hospital Graduate Medical Education [Payment] program. Because most medical residencies are funded by Medicare and because Medicare doesn’t have a lot of patients in children’s hospitals, this program was created in 1999 to remedy that. Yes, I covered it at the time. Republicans in the House are happy to reauthorize it or just to fund it through the appropriations process, which keeps the money flowing, but only if it bans funding for children’s hospitals that don’t provide gender-affirming care for transgender minors. It appears that has killed the reauthorization bill that was moving for this year. Is that the kind of thing that could also threaten the HHS [Department of Health and Human Services] spending bill?
Knight: Yeah, I mean there are provisions within the HHS bill to ban Medicare, Medicaid paying for gender-affirming care. I don’t know. We haven’t done much debate on the Labor-HHS bill. It’s been the one that’s been put to the side. It hasn’t even gone through the full committee, so we haven’t …
Rovner: In the House, right?
Knight: Yeah, in the House, yes. Yeah. But yeah, I think it’s definitely possible. Just broader picture, this is an issue that Republicans are trying to make a bigger thing that they’re running on in different congressional districts, talking about banning gender-affirming care. So I think even if we don’t see it now, it’s probably something that we’re going to continue seeing.
Rovner: Well, we will obviously talk more as Congress comes back and tries to do things. So new year, same old abortion debate. This week’s big entry is a decision by a panel of the 5th Circuit Court of Appeals ruling that EMTALA, the federal law that requires hospitals to at least screen and provide stabilizing care to anyone who presents in their emergency room, does not supersede Texas’ abortion ban. In other words, if a pregnant woman needs an abortion to stabilize her condition, she’d also have to meet one of the exceptions in the Texas abortion ban. Given that we don’t really know what the Texas exceptions are, since we’ve had litigation on that, that could be a tall order, right, Shefali?
Luthra: Yes. Doctors have basically said that the Texas exceptions in the state law are unworkable. And I think it’s worth noting that what EMTALA would require and what is in effect in other states with abortion bans is again very narrow. We are talking about the smallest subset of abortions, the smallest subset of medical emergency abortions, because this doesn’t apply to someone with a fetal anomaly who cannot give birth to a viable child. This doesn’t apply to someone who maybe is undergoing chemotherapy and can’t stay pregnant. This is for people who have situations such as sepsis or preterm premature membrane rupture. These are really, really specific instances, and even then, Texas is arguing and the 5th Circuit says, hospitals don’t have to provide care that would by all accounts be lifesaving.
Rovner: This puts doctors, particularly in Texas, in an untenable situation where if a woman presents, say, with an ectopic pregnancy, which is neither going to produce a live baby and is likely or could definitely kill the woman, if they perform that abortion, they could be brought up on charges in Texas, but if they don’t perform the abortion, they could be brought up on federal charges.
Luthra: And this is the bind that doctors have found themselves in over and over again. And I do want to reiterate that this isn’t actually unique to Texas because even in states where the EMTALA guidance is in effect, doctors and hospitals remain very afraid of coming up against the very onerous abortion penalties that their laws have. I was talking to a physician from Tennessee earlier this week, and she made the point that what your doctor feels safe doing, it comes down to luck in a lot of ways. Which city you happen to live in, which hospital you happen to go to, what the lawyers on that hospital staff happen to think the law says. It’s really untenable for physicians, for hospitals, and more than anyone else for patients.
Rovner: Now, despite Justice [Samuel] Alito’s hope in his Dobbs opinion overturning Roe that the Supreme Court would no longer have to adjudicate this issue, that’s exactly what’s going to happen. There’s already an emergency petition at SCOTUS from Idaho wanting to reverse a 9th Circuit ruling, preventing them from enforcing their abortion ban over EMTALA. In other words, the 9th Circuit basically said, no, we’re going to put this Idaho ban on hold to the extent that it conflicts with EMTALA until it’s all the way through the courts. Not to mention the mifepristone case that could roll back availability of the abortion pill. Is it fair to say that Justice Alito’s reasoning backfired here, or was he being disingenuous when he … did he know this was going to come back to the court?
Luthra: Not one of us can see inside any individual justice’s heart or mind, but I think we can say that anyone who seriously thought that overturning Roe v. Wade, which had been in effect for almost 50 years, would bring up no legal questions to be answered again and again by the courts clearly hadn’t thought this through. I was talking to scholars this week who think that we’ll be spending the next decade answering through the courts all of the new questions that have been instigated by the decision.
Rovner: Yeah, that’s definitely not going to lower their workload. Well, speaking of Idaho, the “Law Dork” blog has an interesting story this week about how the Alliance Defending Freedom — it’s a self-identified Christian law firm that represents mostly anti-abortion and other conservative groups in court — is now providing free representation to the state of Idaho in its effort to keep its state abortion ban in place. ADF is also representing Idaho in a case about bathroom use by transgender people. Now, conservative organizations and states often work together on cases, as do liberal organizations in states, that is not rare. But in this case, ADF is actually representing the state, which poses all kinds of conflicts-of-interest questions, right? Lauren, you’re nodding.
Weber: Yeah, I mean it’s pretty wild to see this kind of overlap. As you pointed out, Julie, it’s not rare for attorney general’s offices to seek outside legal help, that happens all the time. They’re understaffed. There’s a lot of problems they can address. But to fully turn over a case essentially to an ideological group is something different altogether because it also implies that that group is giving a gift to the government. It implies that they may be able to take on more cases because if it’s for free, then who knows? And I want to point out that this group really is at the forefront of many of the battles that we’re seeing play out in health issues legally across the country. I mean, they’re involved in a lot of the gender-affirming care cases and even in dealing with some of the groups that are promoting some of the legislation in places across the country. So this is quite a novel step and something to definitely be on the lookout for as we pay attention to many court cases that are going to play out over the next couple of years.
Rovner: Yeah, this was something I hadn’t really focused on until I saw this story and I was like, “Oh, that is a little bit different from what we’ve seen.” Well, while we were on the subject of doctors and lawsuits and the 5th Circuit Court of Appeals, a panel there kept alive a case filed by three doctors against the FDA, charging that it overstepped its authority by recommending that doctors not prescribe ivermectin, an anti-parasite drug, for covid. We’ve talked a lot about how the mifepristone case could undermine FDA’s drug approval process. Obviously, if anyone can sue to effectively get a drug approval reversed, this case could basically stop the FDA from telling the public about evidence-based research, couldn’t it?
Weber: This case is quite wild. I mean, as someone that covers misinformation and disinformation and has extensively covered the ivermectin sagas over the last couple of years, the idea that the FDA cannot come out and say, “Look, this drug is not recommended,” it would be a severe restricting of its authority. I mean, government agencies are known to give advice, which does not always have to be neutral. Historically, that is what has been considered just the status quo legally. And so for the court to restrict the FDA’s authority in this way — if this does, it’s obviously still up for appeal, so who knows? But if it were to be successful, essentially everything the FDA ever put out would have to say, “But go talk to your physician,” which would lead to a little bit more of a wild, wild West when it comes to evidence-based medicine as we know it today.
Rovner: Back on the abortion beat, the news isn’t all about bans in California. The new year is bringing several new laws aimed at making abortion easier to access. Shefali, tell us about some of those.
Luthra: California is really interesting because they really position themselves as the antithesis of states banning abortion. And the law that you’re discussing here, Julie, this is part of a real concern that a lot of physicians have, which is that in states with abortion bans, it’ll be harder for medical residents to be trained in appropriate health care. That means providing abortion care. It means providing comprehensive OB-GYN care in general, right? Miscarriage management, you learn how to do that in part by providing abortions. California has implemented a law this year that would try to help more out-of-state doctors come to California to get trained in how to provide this kind of care.
I think where this gets tricky and where doctors I’ve spoken to remain concerned, confused, it’s not a panacea, is the concern about whether any single state in and of itself can do enough to rectify what is happening in 18 states across the country. That’s a very, very tall order, and it comes with other concerns of: Will residents feel safe, able to come to California? Will their institutions want to send them? These are all open questions, and I think this California law, this project that they’re taking on, is incredibly interesting. I think it’ll take some time for us to see both what the impact is and what the kinks and challenges are that emerge along the way.
Rovner: I was also interested in a California law that says that California officials don’t have to cooperate with out-of-state investigations into doctors prescribing abortion pills or gender-affirming care.
Luthra: This is, again, really interesting, and I mean, I think what we are going to see is individual state laws continuing to run up against each other and questions over whose authority applies in what situations. This has come up for doctors constantly, right? The ones who live in states with abortion protections but want to provide care in other states. What happens if they are flying across the country and have a layover in a state with an abortion ban? What happens if they have a medical emergency in a state that they have maybe broken the law of, whose law applies there? These are things that have left a lot of doctors really concerned. I know I’ve spoken to physicians who say that even despite the legal protections in their states, in a state like California for instance, they still don’t feel safe actively breaking another state’s laws. And again, this is just one of those questions we’re going to keep watching and seeing play out. Who ultimately is able to decide what happens and what role would the federal government eventually have to play?
Rovner: I think these were things, these were the kinds of questions that I don’t think the Supreme Court really considered when they overturned Roe. There’s so many ramifications that we just didn’t expect. I mean, there were some that we did, but this seems to be an extent that it’s gone to that was not anticipated.
Luthra: It’s just a whole mess of, if not undesired, then perhaps unanticipated or not fully planned-for questions and concerns that are now emerging.
Rovner: So I wanted to call out a survey in the Journal of the American Medical Association about reproduction more broadly, not about abortion. How hard it is for medical students and young doctors to build families early in their careers — a time when most people are building their families. Medical training takes so long in many cases that women, in particular, may find it much more difficult or impossible to get pregnant if they wait until after their training is done. And the pace of medical care delivery and the patriarchal structure of most medical practice frowns on women doing things like getting pregnant and having babies and trying to raise children. I vividly remember a doctor retreat I spoke at in 2004 when a 30-something OB-GYN said that when she got pregnant, her residency adviser accused her of wasting a residency spot that could have gone to someone who wasn’t going to take time out of their career. I think things have progressed since then, but apparently not all that much, according to this survey.
Luthra: And this, I think, is really interesting because especially after the covid pandemic, we saw obviously, health care workers leave the field in droves. We saw more women leave the field than men. And what that spoke to was, in part, that working through covid was really taxing. Women were more often in positions that were on the front lines, but what it also spoke to is that the culture of medicine has long been very unfriendly toward the family-building burdens that often fall on women, and that hasn’t gotten better. If anything, it’s gotten worse because child care is even harder to come by. Moms, in particular, have way more to juggle and to balance than they once did. And the support, it’s not even fair to say it hasn’t caught up. It was never there to begin with.
Weber: And just to add on that, I mean, I find it — that study is great, and I will say I have family members that struggle with this currently. It’s wild to me that the American Academy of Pediatrics recommends a 12-week parental leave, and you possibly couldn’t finish your residency or qualify for a surgery residency if you take more than six weeks. I mean, I think that, in itself, that factoid really says exactly what Shefali was getting at. The culture of medicine is not at all friendly to folks that are considering this whatsoever.
Rovner: There’s so many women in medicine now. Now it’s making a problem not just for the women in medicine, but for everybody who wants medical care. So maybe that will get some attention paid to it. Moving on to “This Week in Private Equity,” we have another study from the Journal of the American Medical Association. It found that hospitals that were bought by private equity firms had a 25% increase in adverse events in the three years following their acquisition. Adverse events include things like falls, hospital-acquired infections, and other harm that, in theory, could or should have been prevented. It’s not really hard to connect the dots here, right? Private equity wants to raise more money, and that tends to want to cut staff, so bad things happen. I see you nodding, Victoria.
Knight: Yeah, I mean, I think this is an ongoing issue. It’s something that the Biden administration has said they want to look into, just decreasing quality of care in places that are taken over by private equity. I’m not sure there’s a really good solution to it at this point in time. And I think it also speaks to the broader issues of consolidation among the health care industry and the business of health care and what that means in regards to quality for patients. But yeah, I think this study is just another piece in building up a case of why sometimes private equity doesn’t always seem to equate to the best care for patients.
Luthra: If we go back in time a little bit, there is more evidence that shows the role that private equity has played in not only reduction in quality of care, but in the opposition between the health care industry and consumers. And the example I’m thinking of is air ambulances and surprise billing by those ER staffing firms, all of which were eventually owned by private equity firms that have their own set of incentives that is at odds with the goal of providing care that people can afford and can access, and that keeps them healthy.
Rovner: Indeed. Well, following “This Week in Private Equity,” we have “This Week in Health Misinformation.” My winner this week is Robert F. Kennedy Jr., who was awarded the “Lie of the Year” from PolitiFact for not just his repeated and repeatedly debunked claims about vaccines, but other fanciful conspiracy theories about covid-19, mass shootings, and the rise in gender dysphoria. I will post the link so I don’t have to repeat all of those things here. Which brings us to the story I asked Lauren here to talk about, how the anti-vax movement is quietly gaining a foothold in state houses. Lauren, tell us what you found.
Weber: Well, I found that it’s becoming very politically advantageous, to some extent. Political clout around anti-vaccine movement is growing. So you’re seeing more and more state legislators get elected that have anti-vaccine or vaccine-skeptical views. And I went down to Baton Rouge and 29 folks that were supported by Stanford Health Freedom, which is against vaccine mandates, got elected in this year’s off-cycle elections. So who knows what will happen next year, but you’re already seeing this reflected in other states. In Iowa, legislators this year stopped the requirement that you can talk about the HPV vaccines in schools. In Tennessee, home-schooled kids no longer have vaccine requirements. In Florida, they banned any possible requiring of covid vaccines, which experts said they worry if you just strike “covid” from that, that could lead to the banning of other requirements for vaccines. You’re seeing this momentum grow, and as you mentioned, Julie, RFK Jr. has played a role in this.
As I talk about in my story, back in 2021, he went down to Louisiana and really riled up some anti-vaccine fever in a legislative hearing about the covid vaccine. And so it’s a combination of things. People are reacting to a lot of misinformation that was spread during covid about the covid vaccine. And that distrust of the covid vaccine is seeping into childhood vaccinations. I mean, this year we saw data that came out that said in the 2022-2023 school year, we saw the highest rate of exemption rates for kindergartners getting their vaccinations. That’s a bad trend for the United States when it comes to herd immunity to protect against things like measles or other preventable diseases. So we will see how the next year plays out legislatively, but as it stands right now, I expect to see much more anti-vaccine movement in the statehouses in 2024.
Rovner: I’ve been covering the anti-vax movement for, I don’t know, 25, 30 years. There’s always been an anti-vax movement. It’s actually this combination of people on the far left and people on the far right, they tend to both be anti-vax, but I think this is the first time we’ve really seen it come into actual legislating way. In fact, the trend over the last couple of years has been to get rid of things like religious exemptions for families getting their children vaccinated in order to attend public school. So now we’re expecting to see the reverse, right?
Weber: Yeah, as you said, this is a horseshoe political issue that it’s been far left, far right, but now it’s really seeped into the far-right conservative consciousness in a way that has become a political advantage for some candidates. And so you’re seeing stuff that would previously be, not even make it to the floor for a vote, have to be vetoed, make it out of a committee, where previously some of these things would’ve looked at the signs and said, this is just not true. Now there’s more political power behind the ideology of some of these anti-mandate freedom pushes. So it’s really going to be something to track in this upcoming year.
Rovner: I think the other trend we’re seeing is actual health officials talking about these kinds of things, led by the Florida Surgeon General, Dr. [Joseph] Ladapo. He’s now moved on beyond recommending that young men not get the covid vaccine, right?
Weber: Yeah. So yesterday he sent out a health bulletin, and I just want to take a step back to say this is incredibly unprecedented because this is a state health officer sending out a bulletin to the state saying that he does not recommend anyone … he wants to halt the use of mRNA covid vaccinations. Now, that is not a position that any other state health officer has taken. It’s not a position that any national health agency has taken. He made it based on claims that have been debunked. He primarily based it on a study that several of the experts I talked to said it is not one that they would base assumptions on.
His claims were implausible, but needless to say, I mean, he’s the health director for the third-largest state in the union. I mean, his words carry weight, and his political patron is Ron DeSantis. Now, DeSantis has not commented publicly yet on this, but oftentimes it seems that they both have worked hand in hand to fight against vaccine mandates and to cause a ruckus around things like this. So it needs to be seen the politicization of this as this continues to play out.
Rovner: Well, that is a wonderful segue into our interview this week with Dr. Sandro Galea about the future of public health. So we will play that now and then we will come back and do our extra credits.
I am pleased to welcome to the podcast Dr. Sandro Galea, dean of the Boston University School of Public Health. Longtime listeners will know I’ve been concerned about the state of public health since even before the pandemic. Dr. Galea has a new book of essays called “Within Reason: A Liberal Public Health for an Illiberal Time” that takes a pretty provocative look at what’s gone wrong for public health and how it might win back the support of the actual public. Dr. Galea, thank you so much for joining us.
Sandro Galea: Thank you for having me.
Rovner: So I want to start with your diagnosis of what it is that ails public health in 2024.
Galea: Well, I suppose I start from the data, and the data show that there is a tremendous loss of trust in science broadly, in public health more specifically. Data from Pew that came out just a few months ago show, really, a 25-point drop in trust in medicine and in health from before the pandemic. So the question becomes why is that? What’s going on? And what I try to do in the book is to identify a number of things that I think have really hurt us, and I could numerate those. No. 1, it is we took a very narrow approach to our perception of what should have been done without leaving space for a plurality of voices that weigh different inputs differently.
No. 2, that through the mediation of social media as a way of extending our voice, we were perhaps inhabited false certitude much more than we ever meant to or much more than we do when we think about our science. And No. 3, we allowed ourselves to become politicized in a way that’s unhealthy. Perhaps partisanized is an even better term because public health is always political, but we allowed ourselves to become blue versus red, and that doesn’t serve anybody because public health should be there to serve the whole public. And I think those three big buckets, obviously in the book I write about them in much more detail, but I think they capture the fundamental problems that then have resulted in this loss of trust we face right now.
Rovner: So I’ve had experts note that the lack of public trust in public health isn’t necessarily because of anything the public health community has done. It’s because of a broader pushback against elites and people in power of all kinds. Do you think that’s the case, or has public health also contributed to its own, I won’t say downfall, but lack of status?
Galea: I feel like the answer to that is “and,” meaning that, yes, there’s no question that there are forces that have tried to undermine public health, forces that tried to undermine science. And in the book, I’m very clear that I do realize there are outside forces that have had mal intent, that they have not acted in good faith and they have tried to undermine public health and science, but that’s not what the book is about. I say that is there, I recognize it’s there, but I wanted to write about public health from within public health. It would be shortsighted of us not to realize that we are contributing to how public perceives us. In many respects, I feel like we should have the agency and the confidence to say, well, there are things that we are doing that we should look at. And now, after the acute phase of the pandemic, is the time to look at that.
I was clear in my other writing that I did not write this book in 2021 or 2022 intentionally, because it was too close. But I feel like now that we’re over the acute phase of the pandemic, now is the time to ask hard questions and to say, “What should we be learning?” And I do that in the book, very much looking forward. I’m not naming names, I’m not pointing fingers. All I’m simply saying is we now have the benefit of time passing. Let us see what we should have done better so we can learn how to be better in future.
Rovner: One of the things I think that frustrated me as a journalist, as somebody who communicates to a lay audience for a living, is that public health and science in general during the pandemic seemed unable to say that yes, as we learn more, we’re going to change what we recommend. It becomes, to the public, well, they said this and now they’re saying that, so they were wrong. Does public health need to show its work more?
Galea: This is the term that I use, which is false certitude, which is that we conveyed confidence when we should not have conveyed confidence. Now, there are many reasons for that. Things were happening quickly. It was a fast-moving pandemic. Everybody was scared. And, also, our communication was mediated through social media, which was a new medium for communication of public health. And that does not leave space for the asterisk, for the caveat. And I think our mistake was not recognizing how much harm it was going to do and not being upfront about this is what we know today, but tomorrow we may know more, and we may then have to change our recommendations. And as one pauses and thinks about how should we do better, surely this is front and center to learn how to communicate by saying, “Today, based on what we know, this is what we think is best, but we reserve the right to come back tomorrow and be clear, tell you that the data have changed, hence the recommendations have changed.”
Rovner: Do you think public health has been slow to embrace things like social media? I mean, there are organizations on social media. I think one that comes to mind is the Consumer Product Safety Commission, the National Park Service. I mean that they’re very cheeky, but they get out really important information in a very quick and understandable way. Is that something that public health needs to be doing better?
Galea: Perhaps. I’m not sure I’m willing to say that public health is any worse than the National Park Service on social media. I think we are all, as a society, struggling with communicating important facts rapidly in a time of crisis. One analogy, which I use in the book, is the analogy to 9/11, meaning in 9/11, it was the first national crisis that was lived through in a time of 24/7 cable news. And as a result, there was a lot of noise on cable news that was happening that was distorting how we dealt with the event. Similarly, covid-19 was the first national crisis that was lived through the lens of social media, and we did not really know how to use it. So, at the same time as I’m labeling this as a real challenge that public health faced, I’m also trying to understand and have the compassion to realize that in public health we were struggling to learn how to do this as everybody else was.
Rovner: So let’s turn to the future. What should public health do first to try and regain some of the trust that it’s lost?
Galea: Well, I suppose first we should be having this conversation, and I’m grateful to you for having a conversation, but I actually mean that, at a large scale, I actually think that I meant my book to be a place marker. And I say in it clearly, I expect people will disagree with elements of the book, and that’s OK. And I hope that the book encourages others to write their books that talks about the things, how they see it. Because I do think that this conversation should open up space for public health to say, what are the things that we didn’t do well? What are the things that we should do better? Because from that is going to emerge a new consensus about how we should act.
If the only thing that emerges is simply this, what you and I just talked about, which is communicating with due humility, recognizing the complexity of rapidly evolving facts, and being clear with the population that things may change. If that’s the only thing that emerges, we’ve already made progress. So I think the first thing that should happen is having the conversation, opening this up, being honest that there are things that public health did that it should do better. That is going to lead us to a new consensus about how we should do better.
Rovner: And beyond the conversation, is there one thing that you wish that policymakers could do that could help public health regain its prominence and its trust? I mean, there really is no other word here.
Galea: I think the one thing that I would want to see in policy is a moving away from abolishing of the notion that we can “follow the science.” One of my least favorite things that happened during the pandemic was this notion that we could “follow the science.” Now, why do I say that? I’m a scientist! But I say that because “follow the science” implies that science leads to linear answers, to linear solutions. And that phrase, “follow the science,” became a fig leaf for policymakers, saying, “Well, the science says we should do X, therefore we’re going to do X.” That is simply false. Policymaking should rest on multiple inputs, science being one of them, but also values, but also the importance of other sectors of the economy.
And I would like us to see as a society being honest about that, that policymaking shouldn’t take science into account centrally. I agree with that. As I said, it’s my bread and butter, it’s what I do. But to pretend that science has the answer is simply wrong. We elect people in elected positions, and there are people who are appointed in decision-making positions in other circumstances. It is their job to weigh all the inputs, science being one of those inputs.
Rovner: Well, Dr. Galea, thank you so much. I will do my part to keep the conversation going. I’m sure you will do yours as well.
Galea: I will. And thank you for doing the part you’re doing.
Rovner: OK. We are back and it’s time for our extra-credit segment. That’s when we each recommend a story we read this week we think you should read, too. As always, don’t worry if you miss it. We will post the links on the podcast page at kffhealthnews.org and in our show notes on your phone or other mobile device. Shefali, why don’t you go first this week?
Luthra: Sure. My story is from Stat by Nicholas Florko. The headline is “Medical Marijuana Companies Are Using Pharma’s Sales Tactics With Little of the Same Scrutiny.” And I think this is such a smart investigation, and I’m so grateful that Nicholas wrote it. It really gets into the fact that medical marijuana is a tremendous industry now, right? It’s not just in the Colorados or the Californias or Massachusetts that you think of. It’s all over the country and it’s a huge business. And because it’s so new, it hasn’t gotten the same scrutiny in terms of how it markets its products to consumers, the relationship it has with providers, et cetera. I think this is just a really important topic, and it’s something that we should all be paying attention to as the industry continues to grow in the coming years.
Rovner: Indeed. Victoria?
Knight: Yeah. So my extra credit this week is a Politico story by Megan Messerly and Robert King titled “Georgia Offered Medicaid With a Work Requirement. Few Have Signed Up.” And so it’s talking about just the rollout of Georgia implementing a work requirement for their Medicaid program, which they did expand Medicaid, but they included a work requirement. So I thought this was just really stunning. It said through the first four months, only 1,800 people have enrolled when the governor, Brian Kemp, expected 31,000 people to sign up.
Rovner: Contrast that with North Carolina, which expanded Medicaid without the work requirement and got, like, 200,000 people to sign up.
Knight: Yeah. So that’s just a stunning number. And they’re talking about in the story there. They’re not sure why all the reasons are, but part of it is that there is a lot of paperwork involved. And so I think it was just a really interesting example. Obviously, we have seen work requirements play out before, but we haven’t seen it in a while. And so it’s interesting to see how difficult it can be for people to access Medicaid if this is put in place. And I also think it’s important to remind people that last year, in 2023, during the debt ceiling debate, Republicans did for a while talk about wanting to implement work requirements in Medicaid again. And so, if this was something that they put into place, it would mean probably a lot of people would drop off the rolls. So it’s an idea that resurfaces. So just important to remember that.
Rovner: Indeed. Lauren.
Weber: I was obsessed with Greg Jaffe story from The Washington Post titled “Can the Exhausted, Angry People of Ottawa County Learn to Live Together?” And it’s this incredible portrait of this Michigan county where the county public health officer, Adeline Hambley, has come under tremendous pressure and threat from the conservative county board. And this is a story we have seen play out in different iterations all around the country in the wake of covid. It’s the “we don’t believe in masks, we don’t believe in shutdowns” versus the county public health folks who are trying to follow the science and how does that play out at a people level, which Greg just does a fantastic way of showing. And it’s interesting, the board was so fed up with her and making such political statements that they offered her $4 million to quit. Now this fell apart because the county doesn’t seem to have the money that would affect them, et cetera.
But it just goes to show how deep the divisions are between what used to be a very non-politicized, normal government job of being a public health officer who keeps your water safe and tries to keep you from catching bad diseases at restaurants, to the post-covid era, where [they’re] just absolutely vilified and hated, really, it seems in some of these comments in the story — so much so that they would be paid this much money to quit. So I think this speaks a lot to the tension that we see in America around public health today, and I really recommend everybody to give it a read.
Rovner: Yeah, it’s a really remarkable story. Well, my extra credit this week is from our podcast pal Alice [Miranda] Ollstein, along with her colleagues Jessica Piper and Madison Fernandez at Politico. It’s called Why Democrats Can’t Rely on Abortion Ballot Initiatives to Help Them Win.” And it’s a warning for Democrats not to get too smug about the popularity and success of abortion rights ballot measures around the country. They dug into the numbers and found that in many of those states, the very same voters who supported the abortion rights measures also turned around and voted for Republican candidates. As usual, in politics, things are rarely as simple as they seem.
All right, that is our show for this first week of 2024. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left us a review; that helps other people find us, too. Special thanks, as always, to our technical guru, Francis Ying, and our editor, my fellow Wolverine, Emmarie Huetteman. As always, you can email us your comments or questions. We’re at whatthehealth@kff.org, or you can still find me at X, @jrovner, or @julierovner at Bluesky and @julie.rovner at Threads. Shefali, where are you these days?
Luthra: I am @shefalil on X and Blue Sky, and then on Threads, I’m @shefali.luthra.
Rovner: Victoria.
Knight: I’m @victoriaregisk on X and Threads.
Luthra: Lauren.
Weber: And then I’m @LaurenWeberHP on X and clearly still need to work on my social media game.
Rovner: We will be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 5 months ago
california, Courts, Multimedia, States, Abortion, Hospitals, KFF Health News' 'What The Health?', Misinformation, Podcasts, texas, U.S. Congress
‘Financial Ruin Is Baked Into the System’: Readers on the Costs of Long-Term Care
Thousands of readers reacted to the articles in the “Dying Broke” series about the financial burden of long-term care in the United States. They offered their assessments for the government and market failures that have drained the lifetime savings of so many American families. And some offered possible solutions.
Thousands of readers reacted to the articles in the “Dying Broke” series about the financial burden of long-term care in the United States. They offered their assessments for the government and market failures that have drained the lifetime savings of so many American families. And some offered possible solutions.
In more than 4,200 comments, readers shared their struggles in caring for spouses, older parents, and grandparents. They expressed anxieties about getting older themselves and needing help to stay at home or in institutions like nursing homes or assisted living facilities.
Many suggested changes to U.S. policy, like expanding the government’s payments for care and allowing more immigrants to stay in the country to help meet the demand for workers. Some even said they would rather end their lives than become a financial burden to their children.
Many readers blamed the predominantly for-profit nature of American medicine and the long-term care industry for depleting the financial resources of older people, leaving the federal-state Medicaid programs to take care of them once they were destitute.
“It is incorrect to say the money isn’t there to pay for elder care,” Jim Castrone, 72, a retired financial controller in Placitas, New Mexico, commented. “It’s there, in the form of profits that accrue to the owners of these facilities.”
“It is a system of wealth transference from the middle class and the poor to the owners of for-profit medical care, including hospitals and the long-term care facilities outlined in this article, underwritten by the government,” he added.
Other readers pointed to insurance policies that, despite limitations, had helped them pay for services. And some relayed their concerns that Americans were not saving enough and were unprepared to take care of themselves as they aged.
What Other Nations Provide
Other countries’ treatment of their older citizens was repeatedly mentioned. Readers contrasted the care they observed older people receiving in foreign countries with the treatment in the United States, which spends less on long-term care as a portion of its gross domestic product than do most wealthy nations.
Marsha Moyer, 75, a retired teaching assistant in Memphis, Tennessee, said she spent 12 years as a caregiver for her parents in San Diego County and an additional six for her husband. While they had advantages many don’t, Moyer said, “it was a long, lonely job, a sad job, an uphill climb.”
By contrast, her sister-in-law’s mother lived to 103 in a “fully funded, lovely elder care home” in Denmark during her last five years. “My sister-in-law didn’t have to choose between her own life, her career, and helping her healthy but very old mother,” Moyer said. “She could have both. I had to choose.”
Birgit Rosenberg, 58, a software developer in Southampton, Pennsylvania, said her mother had end-stage dementia and had been in a nursing home in Germany for more than two years. “The cost for her absolutely excellent care in a cheerful, clean facility is her pittance of Social Security, about $180 a month,” she said. “A friend recently had to put her mother into a nursing home here in the U.S. Twice, when visiting, she has found her mother on the floor in her room, where she had been for who knows how long.”
Brad and Carol Burns moved from Fort Worth, Texas, in 2019 to Chapala, Jalisco, in Mexico, dumping their $650-a-month long-term care policy because care is so much more affordable south of the border. Brad, 63, a retired pharmaceutical researcher, said his mother lived just a few miles away in a memory care facility that costs $2,050 a month, which she can afford with her Social Security payments and an annuity. She is receiving “amazing” care, he said.
“As a reminder, most people in Mexico cannot afford the care we find affordable and that makes me sad,” he said. “But their care for us is amazing, all health care, here, actually. At her home, they address her as Mom or Barbarita, little Barbara.”
Insurance Policies Debated
Many, many readers said they could relate to problems with long-term care insurance policies, and their soaring costs. Some who hold such policies said they provided comfort for a possible worst-case scenario while others castigated insurers for making it difficult to access benefits.
“They really make you work for the money, and you’d better have someone available who can call them and work on the endless and ever-changing paperwork,” said Janet Blanding, 62, a technical writer in Fancy Gap, Virginia.
Derek Sippel, 47, a registered nurse in Naples, Florida, cited the $11,000 monthly cost of his mother’s nursing home care for dementia as the reason he bought a policy. He pays about $195 a month with a lifetime benefit of $350,000. “I may never need to use the benefit[s], but it makes me feel better knowing that I have it if I need it,” he said in his comment. He said he could not make that kind of money by investing on his own.
“It’s the risk you take with any kind of insurance,” he said. “I don’t want to be a burden on anyone.”
Pleas for More Immigrant Workers
One solution that readers proposed was to increase the number of immigrants allowed into the country to help address the chronic shortage of long-term care workers. Larry Cretan, 73, a retired bank executive in Woodside, California, said that over time, his parents had six caretakers who were immigrants. “There is no magic bullet,” he said, “but one obvious step — hello, people — we need more immigrants! Who do you think does most of this work?”
Victoria Raab, 67, a retired copy editor in New York, said that many older Americans must use paid help because their grown children live far away. Her parents and some of their peers rely on immigrants from the Philippines and Eritrea, she said, “working loosely within the margins of labor regulations.”
“These exemplary populations should be able to fill caretaker roles transparently in exchange for citizenship because they are an obvious and invaluable asset to a difficult profession that lacks American workers of their skill and positive cultural attitudes toward the elderly,” Raab said.
Federal Fixes Sought
Other readers called for the federal government to create a comprehensive, national long-term care system, as some other countries have. In the United States, federal and state programs that finance long-term care are mainly available only to the very poor. For middle-class families, sustained subsidies for home care, for example, are fairly nonexistent.
“I am a geriatric nurse practitioner in New York and have seen this story time and time again,” Sarah Romanelli, 31, said. “My patients are shocked when we review the options and its costs. Medicaid can’t be the only option to pay for long-term care. Congress needs to act to establish a better system for middle-class Americans to finance long-term care.”
John Reeder, 76, a retired federal economist in Arlington, Virginia, called for a federal single-payer system “from birth to senior care in which we all pay and profit-making [is] removed.”
Other readers, however, argued that people needed to take more responsibility by preparing for the expense of old age.
Mark Dennen, 69, in West Harwich, Massachusetts, said people should save more rather than expect taxpayers to bail them out. “For too many, the answer is, ‘How can we hide assets and make the government pay?’ That is just another way of saying, ‘How can I make somebody else pay my bills?’” he said, adding, “We don’t need the latest phone/car/clothes, but we will need long-term care. Choices.”
Questioning the Value of Life-Prolonging Procedures
A number of readers condemned the country’s medical culture for pushing expensive surgeries and other procedures that do little to improve the quality of people’s few remaining years.
Thomas Thuene, 60, a consultant in Boston’s Roslindale neighborhood, described how a friend’s mother who had heart failure was repeatedly sent from the elder care facility where she lived to the hospital and back, via ambulance. “There was no arguing with the care facility,” he said. “However, the moment all her money was gone, the facility gently nudged my friend to think of end-of-life care for his mother. It seems the financial ruin is baked into the system.”
Joan Chambers, 69, an architectural draftsperson in Southold, New York, said that during a hospitalization on a cardiac unit she observed many fellow patients “bedridden with empty eyes,” awaiting implants of stents and pacemakers.
“I realized then and there that we are not patients, we are commodities,” she said. “Most of us will die from heart failure. It will take courage for a family member to refuse a ‘simple’ procedure that will keep a loved one’s heart beating for a few more years, but we have to stop this cruelty.
“We have to remember that even though we are grateful to our health care professionals, they are not our friends. They are our employees and we can say no.”
One physician, James Sullivan, 64, in Cataumet, a neighborhood of Bourne, Massachusetts, said he planned to refuse hospitalization and other extraordinary measures if he suffered from dementia. “We spend billions of dollars, and a lot of heartache, treating demented people for pneumonia, urinary tract infections, cancers, things that are going to kill them sooner or later, for no meaningful benefit,” Sullivan said. “I would not want my son to spend his good years, and money, helping to maintain me alive if I don’t even know what’s going on,” he said.
Considering ‘Assisted Dying’
Others went further, declaring they would rather arrange for their own deaths than suffer in greatly diminished capacity. “My long-term care plan is simple,” said Karen Clodfelter, 65, a library assistant in St. Louis. “When the money runs out, I will take myself out of the picture.” Clodfelter said she helped care for her mother until her death at 101. “I’ve seen extreme old age,” she said, “and I’m not interested in going there.”
Some suggested that medically assisted death should be a more widely available option in a country that takes such poor care of its elderly. Meridee Wendell, 76, of Sunnyvale, California, said: “If we can’t manage to provide assisted living to our fellow Americans, could we at least offer assisted dying? At least some of us would see it as a desirable solution.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 5 months ago
Aging, Health Care Costs, Health Industry, Aid In Dying, california, Dying Broke, Florida, Legislation, Long-Term Care, Massachusetts, Missouri, New Mexico, New York, Pennsylvania, Tennessee, texas, Virginia
Many Autoimmune Disease Patients Struggle With Diagnosis, Costs, Inattentive Care
After years of debilitating bouts of fatigue, Beth VanOrden finally thought she had an answer to her problems in 2016 when she was diagnosed with Hashimoto’s disease, an autoimmune disorder.
For her and millions of other Americans, that’s the most common cause of hypothyroidism, a condition in which the thyroid, a butterfly-shaped gland in the neck, doesn’t produce enough of the hormones needed for the body to regulate metabolism.
There’s no cure for Hashimoto’s or hypothyroidism. But VanOrden, who lives in Athens, Texas, started taking levothyroxine, a much-prescribed synthetic thyroid hormone used to treat common symptoms, like fatigue, weight gain, hair loss, and sensitivity to cold.
Most patients do well on levothyroxine and their symptoms resolve. Yet for others, like VanOrden, the drug is not as effective.
For her, that meant floating from doctor to doctor, test to test, and treatment to treatment, spending about $5,000 a year.
“I look and act like a pretty energetic person,” said VanOrden, 38, explaining that her symptoms are not visible. “But there is a hole in my gas tank,” she said. And “stress makes the hole bigger.”
Autoimmune diseases occur when the immune system mistakenly attacks and damages healthy cells and tissues. Other common examples include rheumatoid arthritis, lupus, celiac disease, and inflammatory bowel disease. There are more than 80 such diseases, affecting up to an estimated 50 million Americans, disproportionately women. Overall, the cost of treating autoimmune diseases is estimated at more than $100 billion annually in the U.S.
Despite their frequency, finding help for many autoimmune diseases can prove frustrating and expensive. Getting diagnosed can be a major hurdle because the range of symptoms looks a lot like those of other medical conditions, and there are often no definitive identifying tests, said Sam Lim, clinical director of the Division of Rheumatology at Emory University School of Medicine in Atlanta. In addition, some patients feel they have to fight to be believed, even by a clinician. And after a diagnosis, many autoimmune patients rack up big bills as they explore treatment options.
“They’re often upset. Patients feel dismissed,” Elizabeth McAninch, an endocrinologist and thyroid expert at Stanford University, said of some patients who come to her for help.
Insufficient medical education and lack of investment in new research are two factors that hinder overall understanding of hypothyroidism, according to Antonio Bianco, a University of Chicago endocrinologist and leading expert on the condition.
Some patients become angry when their symptoms don’t respond to standard treatments, either levothyroxine or that drug in combination with another hormone, said Douglas Ross, an endocrinologist at Massachusetts General Hospital in Boston. “We will have to remain open to the possibility that we’re missing something here,” he said.
Jennifer Ryan, 42, said she has spent “thousands of dollars out-of-pocket” looking for answers. Doctors did not recommend thyroid hormone medication for the Huntsville, Alabama, resident — diagnosed with Hashimoto’s after years of fatigue and weight gain — because her levels appeared normal. She recently switched doctors and hopes for the best.
“You don’t walk around hurting all day long and have nothing wrong,” Ryan said.
And health insurers typically deny coverage of novel hypothyroidism treatments, said Brittany Henderson, an endocrinologist and founder of the Charleston Thyroid Center in South Carolina, which sees patients from all 50 states. “Insurance companies want you to use the generics even though many patients don’t do well with these treatments,” she said.
Meanwhile, the extent of Americans’ thyroid problems can be seen in drug sales. Levothyroxine is among the five most prescribed medications in the U.S. every year. Yet research points to some overprescribing of the drug for those with mild hypothyroidism.
A recent study, paid for by AbbVie — maker of Synthroid, a brand-name version of levothyroxine — said a medical and pharmacy claims database showed that the prevalence of hypothyroidism, including milder forms, rose from 9.5% of Americans in 2012 to 11.7% in 2019.
The number of people diagnosed will rise as the population ages, said McAninch. Endocrine disruptors — natural or synthetic chemicals that can affect hormones — could account for some of that increase, she said.
In their search for answers, patients sometimes connect on social media, where they ask questions and describe their thyroid hormone levels, drug regimens, and symptoms. Some online platforms offer information that’s dubious at best, but overall, social media outlets have increased patients’ understanding of hard-to-resolve symptoms, Bianco said.
They also offer one another encouragement.
VanOrden, who has been active on Reddit, has this advice for other patients: “Don’t give up. Continue to advocate for yourself. Somewhere out there is a doctor who will listen to you.” She has started an alternative treatment — desiccated thyroid medication, an option not approved by the FDA — plus a low dose of the addiction drug naltrexone, though the data is limited. She’s feeling better now.
Research of autoimmune thyroid disease gets little funding, so the underlying causes of immune dysfunction are not well studied, Henderson said. The medical establishment hasn’t fully recognized hard-to-treat hypothyroid patients, but increased acknowledgment of them and their symptoms would help fund research, Bianco said.
“I would like a very clear, solid acknowledgment that these patients exist,” he said. “These people are real.”
For an illustrated version of this article, click here.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 6 months ago
Health Care Costs, Health Industry, Insurance, Pharmaceuticals, Alabama, Autoimmune Diseases, Chronic Disease Care, Doctors, Patient Advocacy, texas, Women's Health
Trabajadores sufren mientras el Congreso y empresarios debaten la necesidad de normas contra el calor
A veces el calor te hace vomitar, contó Carmen García, trabajadora agrícola en el Valle de San Joaquín, en California. Ella y su marido pasaron el mes de julio en los campos de ajo, arrodillados sobre la tierra ardiente mientras las temperaturas superaban los 105 grados.
El cansancio y las náuseas de su marido fueron tan intensas que no fue a trabajar por tres días. Pero bebió agua con lima en lugar de ir al médico porque no tienen seguro médico. “A mucha gente le pasa esto”, agregó.
No existen normas federales para proteger a los trabajadores como los García cuando los días son excesivamente calurosos. Y sin el apoyo bipartidista del Congreso, incluso con la atención urgente de la administración Biden, es posible que el alivio no llegue en años.
El presidente Joe Biden encargó en 2021 a la Administración de Seguridad y Salud Ocupacional (OSHA) la elaboración de normas para prevenir los accidentes y las enfermedades causados por el calor.
Pero ese proceso de 46 pasos puede llevar más de una década y podría estancarse si un republicano es elegido presidente en 2024, porque el Partido Republicano se ha opuesto generalmente a las regulaciones de salud laboral en los últimos 20 años.
Estas normas podrían obligar a los empleadores a proporcionar abundante agua potable, descansos y un espacio para refrescarse a la sombra o con aire acondicionado cuando las temperaturas superen un determinado umbral.
El 7 de septiembre, OSHA comenzó reuniones con propietarios de pequeñas empresas para discutir sus propuestas, incluidas las medidas que deberían adoptar las empresas cuando las temperaturas llegan a los 90 grados.
Como este verano se han batido récords de calor, la congresista Judy Chu (demócrata de California) y otros miembros del Congreso han impulsado una legislación que aceleraría el proceso de elaboración de normas de OSHA.
El proyecto de ley lleva el nombre de Asunción Valdivia, una trabajadora agrícola que se desmayó mientras recogía uvas en California en un día de 105 grados en 2004. Su hijo la recogió del campo y Valdivia murió de un golpe de calor en el trayecto a su casa.
“Ya sea en una granja, conduciendo un camión o trabajando en un almacén, los trabajadores como Asunción mantienen nuestro país en funcionamiento mientras soportan algunas de las condiciones más difíciles”, dijo Chu en declaraciones en julio en la que instaba al Congreso a aprobar el proyecto de ley.
Las organizaciones profesionales que representan a los empresarios se han opuesto a las normas, calificándolas de “exageradas”. También afirman que faltan datos que justifiquen regulaciones generales, dada la diversidad de trabajadores y lugares de trabajo, desde restaurantes de comida rápida hasta granjas.
La Cámara de Comercio de Estados Unidos, uno de los grupos de presión más poderosos de Washington, argumentó que tales medidas carecen de sentido “porque cada empleado experimenta el calor de forma diferente”. Además, según la Cámara, normas como los ciclos de trabajo-descanso “amenazan con perjudicar directa y sustancialmente… la productividad de los empleados y, por lo tanto, la viabilidad económica de su empleador”.
“Muchos de los problemas relacionados con el calor no son consecuencia del trabajo agrícola ni de la mala gestión del empresario, sino del moderno estilo de vida de los empleados”, escribió el Consejo Nacional del Algodón en su respuesta a la legislación propuesta.
Por ejemplo, el aire acondicionado hace más difícil que las personas se adapten a un ambiente caluroso después de haber estado en una vivienda o un vehículo fríos, y señaló que “los trabajadores más jóvenes, más acostumbrados a un estilo de vida más sedentario, no pueden aguantar un día trabajando al aire libre”.
La Asociación de Recursos Forestales, que representa a los propietarios de terrenos forestales, la industria maderera y los aserraderos, agregó que “las enfermedades y muertes relacionadas con el calor no figuran entre los riesgos laborales más graves a los que se enfrentan los trabajadores”. Citaron cifras de OSHA: la agencia documentó 789 hospitalizaciones y 54 muertes relacionadas con el calor a través de investigaciones e infracciones de 2018 a 2021.
OSHA admite que sus datos son cuestionables. Ha dicho que sus cifras “sobre enfermedades, accidentes y muertes relacionadas con el calor en el trabajo son probablemente grandes subestimaciones”.
Los accidentes y enfermedades no siempre se registran, las muertes provocadas por las altas temperaturas no siempre se atribuyen al calor, y los daños relacionados con el calor pueden ser acumulativos, provocando infartos, insuficiencia renal y otras dolencias después de que la persona haya abandonado su lugar de trabajo.
El efecto de la temperatura
Para establecer normas, OSHA debe conocer los efectos del calor en los que trabajan en interiores y al aire libre. La justificación es una parte necesaria del proceso, porque las normativas aumentarán los costos para los empresarios que necesiten instalar sistemas de aire acondicionado y ventilación en el interior, y para aquellos cuya productividad pueda bajar si se permite a los que trabajan a la intemperie tomar descansos o reducir las jornadas cuando suban las temperaturas.
Lo ideal sería que los empresarios tomaran medidas para proteger a los trabajadores del calor independientemente de las normas, afirmó Georges Benjamin, director ejecutivo de la Asociación Americana de Salud Pública. “Tenemos que hacer un mejor trabajo para convencer a los empresarios de que hay una compensación entre la eficiencia y los trabajadores enfermos”, dijo.
García y su marido sufrieron los síntomas del golpe de calor: vómitos, náuseas y fatiga. Pero sus casos forman parte de los miles que no se contabilizan cuando la gente no va al hospital ni presenta denuncias por miedo a perder su empleo o estatus migratorio.
Los trabajadores agrícolas están notoriamente subrepresentados en las estadísticas oficiales sobre accidentes y enfermedades laborales, según David Michaels, epidemiólogo de la Universidad George Washington y ex administrador de OSHA.
Investigadores que encuestaron a trabajadores agrícolas de Carolina del Norte y Georgia encontraron que más de un tercio presentaba síntomas de enfermedad por calor durante los veranos analizados, una cifra muy superior a la registrada por OSHA. En particular, el estudio de Georgia reveló que el 34% de los trabajadores agrícolas no tenía descansos regulares, y una cuarta parte no tenía acceso a espacios con sombra.
Incluso los casos en los que los trabajadores son hospitalizados pueden no atribuirse al calor si los médicos no documentan la conexión. Muchos estudios relacionan los accidentes laborales con el estrés térmico, que puede causar fatiga, deshidratación y vértigo.
En un estudio realizado en el estado de Washington, se observó que los trabajadores agrícolas se caían de las escaleras con más frecuencia en junio y julio, unos de los meses más calurosos y húmedos. Y en un informe de 2021, investigadores calcularon que las temperaturas más cálidas causaron aproximadamente 20,000 accidentes laborales al año en California entre 2001 y 2018, según los reclamos de compensación de los trabajadores.
Las lesiones renales por calor también aparecen en la base de datos de OSHA de trabajadores lesionados gravemente en el trabajo, como el caso de un empleado de una planta de procesamiento de carne hospitalizado por deshidratación y lesión renal aguda en un caluroso día de junio en Arkansas.
Sin embargo, la investigación revela que el daño renal provocado por el calor también puede ser gradual. Un estudio de trabajadores de la construcción que estuvieron durante un verano en Arabia Saudita reveló que el 18% presentaba signos de lesión renal, lo que los ponía en riesgo de insuficiencia renal futura.
Además de cuantificar las lesiones y muertes causadas por el calor, OSHA trata de atribuirles un costo para poder calcular el ahorro potencial derivado de la prevención. “Hay que medir las cosas, como ¿cuánto vale una vida?”, afirmó Michaels.
Para los trabajadores y sus familias, el sufrimiento tiene consecuencias de largo alcance que son difíciles de enumerar. Los gastos médicos son más obvios. Por ejemplo, OSHA calcula que el costo directo de la postración por calor (sobrecalentamiento debido a insolación o hipertermia), es de casi $80,000 en costos directos e indirectos por caso.
Si esto parece elevado, hay que pensar en un trabajador de la construcción de Nueva York que perdió el conocimiento en un día caluroso y se cayó de una plataforma, y sufrió una laceración renal, fracturas faciales y varias costillas rotas.
El precio de los golpes de calor
Investigadores también han intentado determinar el costo que supone para los empresarios la pérdida de productividad. El trabajo es menos eficiente cuando suben las temperaturas, y si los trabajadores se ausentan por enfermedad y tienen que ser reemplazados, la producción disminuye mientras se entrena a nuevos trabajadores.
Cullen Page, cocinero de Austin, Texas, y miembro del sindicato Restaurant Workers United, trabaja durante horas frente a un horno de pizza, donde, según dijo, las temperaturas oscilaron entre los 90 y los 100 grados cuando las olas de calor golpeaban la ciudad en agosto.
“Es brutal. Afecta tu forma de pensar. Estás confundido”, dijo. “Me dio un sarpullido por calor que no se me quitaba”. Como hace tanto calor, agregó, el restaurante tiene un alto índice de rotación de empleados. Una campana extractora adecuada sobre los hornos y un mejor aire acondicionado ayudarían, pero los propietarios aún no han hecho las mejoras, dijo.
Via 313, la cadena de pizzerías en la que trabaja Page, no respondió al pedido de comentario.
Page no es el único. Una organización que representa a los empleados de restaurantes, Restaurant Opportunities Centers United, encuestó a miles de trabajadores, muchos de los cuales informaron de condiciones inseguras por el calor: el 24% de los trabajadores de Houston, por ejemplo, y el 37% de los de Philadelphia.
“Los trabajadores estuvieron expuestos a temperaturas de hasta 100 grados después de que se rompieron los aparatos de aire acondicionado y los ventiladores de las cocinas, lo que les dificultaba respirar”, escribió el Sindicato Internacional de Empleados de Servicios, que incluye a trabajadores del sector de comida rápida, en una nota a OSHA. “No hay razón para retrasar más la creación de una norma cuando conocemos la magnitud del problema y sabemos cómo proteger a los trabajadores”, dijeron.
Investigadores del Atlantic Council calculan que Estados Unidos perderá una media de $100,000 millones anuales por la baja de la productividad laboral inducida por el calor a medida que el clima se vuelve más cálido. “A los empresarios les cuesta mucho dinero no proteger a sus trabajadores”, afirmó Juley Fulcher, defensora de salud y seguridad de los trabajadores de Public Citizen, organización de Washington D.C. que aboga por que el proyecto de ley Asunción Valdivia permita a OSHA promulgar normas el año que viene.
Como modelo, Fulcher sugirió fijarse en California, Maryland, Nevada, Oregon y Washington, los únicos estados con normas que obligan a que todos los trabajadores al aire libre tengan acceso a agua, descanso y sombra.
Aunque las normas no siempre se hacen cumplir, parece que surten efecto. Después de que California instaurara la suya en 2005, se registraron menos accidentes en los reclamos de indemnización de los trabajadores cuando las temperaturas superaban los 85 grados.
Michaels afirmó que OSHA ha demostrado que puede actuar con más rapidez de lo habitual cuando el Congreso se lo permite.
En los primeros días de la epidemia de VIH/SIDA, la agencia aprobó rápidamente normas para evitar que médicos, enfermeras y dentistas se infectaran accidentalmente con agujas. Ahora existe una urgencia similar, dijo. “Dada la crisis climática y la prolongación de los períodos de calor extremo”, señaló, “es imperativo que el Congreso apruebe una legislación que permita a OSHA promulgar rápidamente una norma que salve vidas”.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 9 months ago
Noticias En Español, Public Health, Rural Health, Arkansas, Biden Administration, california, Environmental Health, Georgia, Legislation, Maryland, Nevada, North Carolina, Oregon, texas, U.S. Congress, Washington
KFF Health News' 'What the Health?': A Not-So-Health-y GOP Debate
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
For the first time since 2004, it appears health insurance coverage will not be a central issue in the presidential campaign, at least judging from the first GOP candidate debate in Milwaukee Wednesday night. The eight candidates who shared the stage (not including absent front-runner Donald Trump) had major disagreements over how far to extend abortion restrictions, but there was not even a mention of the Affordable Care Act, which Republicans have tried unsuccessfully to repeal since it was passed in 2010.
Meanwhile, a new poll from KFF finds that health misinformation is not only rampant but that significant minorities of the public believe things that are false, such as that more people have died from the covid vaccine than from the covid-19 virus.
This week’s panelists are Julie Rovner of KFF Health News, Joanne Kenen of the Johns Hopkins Bloomberg School of Public Health and Politico, Victoria Knight of Axios, and Margot Sanger-Katz of The New York Times.
Panelists
Joanne Kenen
Johns Hopkins Bloomberg School of Public Health and Politico
Victoria Knight
Axios
Margot Sanger-Katz
The New York Times
Among the takeaways from this week’s episode:
- The first Republican presidential debate of the 2024 cycle included a spirited back-and-forth about abortion, but little else about health care — and that wasn’t a surprise. During the primary, Republican presidential candidates don’t really want to talk about health insurance and health care. It’s not a high priority for their base.
- The candidates were badly split on abortion between those who feel decisions should be left to the states and those who support a national ban of some sort. Former Vice President Mike Pence took a strong position favoring a national ban. The rest revealed some public disagreement over leaving the question completely to states to decide or advancing a uniform national policy.
- Earlier this summer, Stanford University’s Hoover Institute unveiled a new, conservative, free-market health care proposal. It is the latest sign that Republicans have moved past the idea of repealing and replacing Obamacare and have shifted to trying to calibrate and adjust it to make health insurance a more market-based system. The fact that such plans are more incremental makes them seem more possible. Republicans would still like to see things like association health plans and other “consumer-directed” insurance options. Focusing on health care cost transparency could also offer an opportunity for a bipartisan moment.
- In a lawsuit filed this week in U.S. District Court in Jacksonville, two Florida families allege their Medicaid coverage was terminated by the state without proper notice or opportunity to appeal. It seems to be the first such legal case to emerge since the Medicaid “unwinding” began in April. During covid, Medicaid beneficiaries did not have to go through any kind of renewal process. That protection has now ended. So far, the result is that an estimated 5 million people have lost their coverage, many because of paperwork issues, as states reassess the eligibility of everyone on their rolls. It seems likely that more pushback like this is to come.
- A new survey released by KFF this week on medical misinformation found that the pandemic seems to have accelerated the trend of people not trusting public health and other institutions. It’s not just health care. It’s a distrust of expertise. In addition, it showed that though there are people on both ends — the extremes — there is also a muddled middle.
- Legislation in Texas that was recently signed into law by Republican Gov. Greg Abbott hasn’t gotten a lot of notice. But maybe it should, because it softens some of the state’s anti-abortion restrictions. Its focus is on care for pregnant patients; it gives doctors some leeway to provide abortion when a patient’s water breaks too early and for ectopic pregnancies; and it was drafted without including the word “abortion.” It bears notice because it may offer a path for other states that have adopted strict bans and abortion limits to follow.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week they think you should read, too:
Julie Rovner: KFF Health News’ “Doctors and Patients Try to Shame Insurers Online to Reverse Prior Authorization Denials,” by Lauren Sausser.
Margot Sanger-Katz: KFF Health News’ “Life in a Rural ‘Ambulance Desert’ Means Sometimes Help Isn’t on the Way,” by Taylor Sisk.
Joanne Kenen: The Atlantic’s “A Simple Marketing Technique Could Make America Healthier,” by Lola Butcher.
Victoria Knight: The New York Times’ “The Next Frontier for Corporate Benefits: Menopause,” by Alisha Haridasani Gupta.
Also mentioned in this week’s episode:
- NPR’s “Two Families Sue Florida for Being Kicked off Medicaid in ‘Unwinding’ Process,” by Selena Simmons-Duffin
- NPR’s “Texas Has Quietly Changed Its Abortion Law,” by Selena Simmons-Duffin.
- KFF’s “Poll: Most Americans Encounter Health Misinformation, and Most Aren’t Sure Whether It’s True or False.”
Click to open the transcript
Transcript: A Not-So-Health-y GOP Debate
[Editor’s note: This transcript, generated using transcription software, has been edited for style and clarity.]
Julie Rovner: Hello and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News. And I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, Aug. 24, at 10 a.m. As always, news happens fast, and things might have changed by the time you hear this. So, here we go. We are joined today via video conference by Margot Sanger-Katz of The New York Times.
Margot Sanger-Katz: Good morning.
Rovner: Joanne Kenen of the Johns Hopkins Bloomberg School of Public Health and Politico.
Joanne Kenen: Hi, everybody.
Rovner: And Victoria Knight of Axios News.
Victoria Knight: Hello, everyone.
Rovner: No interview this week, but we’ll have an entire interview episode next week. More on that later. First, we will get to this week’s news. Well, Wednesday night saw the first Republican presidential debate of the 2024 cycle, minus front-runner Donald Trump, in what could only be called a melee, on Fox News Channel. And while there was a spirited debate about abortion, which we’ll get to in a minute, I didn’t hear a single word about anything else health-related — not Medicare or Medicaid, nor any mention of the Affordable Care Act. Was anybody surprised by that? For the record, I wasn’t. I wasn’t really expecting anything except abortion.
Kenen: Well, somebody, I think it was [former New Jersey Gov. Chris] Christie actually pointed out that nobody was talking about it.
Knight: Mike Pence. It was [former Vice President] Mike Pence, actually.
Kenen: Oh, Pence. OK. “Nobody’s talking about Medicare and Social Security.” And then he didn’t talk about it, and nobody mentioned the ACA.
Rovner: Is the ACA really gone as a Republican issue, for this cycle, do we think?
Kenen: Well, I think it’s become, like, a guerrilla warfare. Like, they’re still trying to undermine it. They’re not trying to repeal it, but they’re looking at its sort of soft underbelly, so to speak, and trying to figure out where they can put more market forces on, which we can sort of come back to later. But they spent 10 years trying to repeal it, and they just figured out what they’ve got to do now is pretend it’s not there. Right now, abortion is their topic.
Rovner: Well, let us turn to that.
Sanger-Katz: Yeah, I was just going to say that we’ve been seeing this happen a little bit over the last couple of cycles. In the 2020 race — I went through the transcripts of all of the speakers during the Republican National Convention and was really staggered by how few mentions of Obamacare there were relative to the way that the issue had been discussed in the past. But I think — just a note, that this is the Republican debate. Republicans don’t really want to be talking about health insurance and health care, because they don’t really have affirmative plans to put forward and because I think that they see that there are some real political liabilities in staking out a strong position on these issues. But in a general election, I think it will be impossible for them to avoid it, because, I think, Joe Biden has a lot of things that he wants to say. I think he is very committed to, in particular, broadcasting that he wants to protect Medicare. I think he’s quite proud of the expansions that he’s made of the Affordable Care Act. And so, this is a little bit of a weird moment in the race because, you know, we really only have one party that’s having a primary, and its leading candidate is not participating in the debates. And so, I think these candidates are trying to focus elsewhere. But it is — I will say, as someone who’s covered a couple of these now — it is a weird experience to have health care and health policy feel like a second-tier issue, because it was so central — Obamacare, in particular — was just so central to so many of these election cycles and such an animating and unifying issue among Republican voters, that this kind of post-failure-of “repeal and replace” era feels very different.
Kenen: One really quick thing is, they’re going to hit Biden on inflation. Economically, it’s his most vulnerable point, and health care costs are a burden. And I was a little surprised, without going into Obamacare and repeal and all that stuff, they mentioned the price of food, the price of gas, they mentioned interest rates and housing. It would have been really easy, and I expect that at some point they will start doing it, to talk about the cost of health care, because Biden’s done a huge amount on coverage and making insurance more affordable and accessible. But the cost of health care, as we all know, is still high in America.
Rovner: And at very least, the cost of prescription drugs, which has been a bipartisan issue going back many, many years. All right. Well, the one health issue that, not surprisingly, did get a lot of attention last night was abortion. With the exception of Mike Pence, who has been an anti-abortion absolutist for his entire tenure in Congress, as governor of Indiana, and as vice president, everyone else looked pretty uncomfortable trying to walk the line between the very anti-abortion base of the party and the recognition that anti-abortion absolutism has been a losing electoral strategy since the Supreme Court overturned Roe last year. What does this portend for the rest of the presidential race and for the rest of the down-ballot next year? Rather than trying to bury the fact that they all disagree, they all just publicly disagreed?
Knight: And I think they also, like, if you listened, [former U.S. ambassador to the United Nations] Nikki Haley kind of skirted around how she would address it. She talked about some other things, like contraception and saying that there just weren’t enough votes in the Senate to pass any kind of national abortion ban. [Florida Gov.] Ron DeSantis also, similarly, said he was proud of his six-week bill but didn’t quite want to answer about a national abortion ban. There were the few that did say, like, Hey, we’re into that. And some said, You know, it needs to go back to the states. So there definitely was kind of this slew of reactions on the stage, which I think just shows that the Republican Party is figuring out what message, and they don’t have a unified one on abortion, for sure.
Rovner: I do want to talk about Nikki Haley for a second, because this is what she’s been saying for a long time that she thinks that there’s a middle ground on abortion. And, you know, bless her heart. I’ve been covering this for almost 40 years and there has never been a middle ground. And she says, well, everybody should be for contraception. Well, guess what? There’s a lot of anti-abortion stalwarts who think that many forms of contraception are abortion. So there isn’t even a consensus on contraception. Might she be able to convince people that there could be a middle ground here?
Sanger-Katz: Oh, what I found sort of interesting about her answers: I think on their face they were kind of evasive. They were like, I don’t need to answer this question because there’s not a political consensus to do these things. But I do think it was sort of revealing of where the political consensus is and isn’t that I think she’s right. Like, realistically, there aren’t the votes to totally ban abortion; there aren’t the votes to renew the Roe standard. And I think she was in some ways very honestly articulating the bind that Republicans find themselves in, where they, and I think a lot of their voters, have these very strong pro-life values. At the same time, they recognize that getting into discussions about total abortion bans gives no favors politically and also isn’t going to happen in the near future. So, I felt like, as a journalist, you know, thinking about how I would feel having asked her that question, I felt very dissatisfied by her answer, because she really didn’t answer what she would like to do. But I do think she channeled the internal debate that all these candidates are facing, which is, like, is it worth it to go all the way out there with a policy that I know will alienate a lot of American voters when I know that it cannot be achieved?
Rovner: I was actually glad that she said that because I’ve been saying the opposite is true also — everybody says, well, why didn’t, you know, Congress enshrine abortion rights when they could have? The fact is, they never could have. There have never been 60 votes in the Senate for either side of this debate. That’s why they tried early after Roe to do national bans and then a constitutional amendment. They could never get enough votes. And they tried to do the Freedom of Choice Act and other abortion rights bills, and they couldn’t get those through either. And this is where I get to remind everybody, for the 11,000th time, the family planning law, the Title X, the federal Family Planning [Services and Public Research] Act, hasn’t been reauthorized since 1984 because neither side has been able to muster the votes even to do that. Sorry, Joanne, you wanted to say something.
Kenen: No, I thought Haley’s response on abortion was actually really pretty interesting on two points, right? She didn’t technically answer the question, but she also said this question is a fantasy — you know, face it. And, you know, she said that, and then she mentioned the word contraception. She did not dwell on it. She sort of said it sort of quickly. She missed an opportunity, maybe, just for one or two more sentences. You know, she said we need to make sure that contraception … she’s the only woman on that stage. She’s a mother; she’s got two kids. And, you know, there is uncertainty. After Dobbs there were advocacy groups saying, you know, they’re going to ban contraception tomorrow, and that didn’t happen. And we still don’t know how that fight will play out and what types of contraception will be debated. But I noticed that she said that on a stage full of Republicans, and I noticed that nobody else — all men — didn’t pick up on it.
Rovner: The big divide seemed to be, do you want to leave it completely to the states or do you want to have some kind of national floor of a ban? And they seemed, yeah —
Kenen: Yeah, and the moderators didn’t pick up on that. I mean, there was such a huge brouhaha on the stage. You know, the moderators had a lot of trouble moderating last night. It wouldn’t have been easy for them to get off of abortion and follow up on contraception. But I thought it was just sort of an interesting thing that she noted it.
Sanger-Katz: I will say also, and I agree with Julie: With the possible exception of Mike Pence, even the candidates that were endorsing some kind of national abortion policy, we’re talking about a 15-week gestational limit. There really wasn’t anyone who was coming out and saying, “Let’s ban all abortions. Let’s even go to six weeks,” which many of the states, including Florida, have done. So I do think, again, like, even the candidates that were more willing to take an aggressive stand on whether the federal government should get involved in this issue were moderating the position that you might have expected for them before Dobbs.
Kenen: But even 15 weeks shows how the parameters of this conversation have changed, because what the Republicans had been doing pre-Dobbs was 20 weeks, with their so-called fetal-pain bills. So 15 weeks, which would have sounded extremely radical two years ago — compared to six weeks, 15 sounds like, oh, you know, this huge opportunity for the pro-choice people. And it is another sign of how this space has shrunk.
Sanger-Katz: Yeah, no, I don’t mean that it’s a huge opportunity for the pro-choice people, but I think it reflects that even the candidates who were willing to go the most out on the limb in wanting to enforce a national abortion restriction understand the politics do not permit them to openly advocate going all the way towards a full ban.
Rovner: While we are on the subject of Republicans and health, there actually is a new Republican plan to overhaul the health system. Sort of. It’s from the Hoover Institution at Stanford, from which a lot of conservative policy proposals emanate. And it’s premised on the concept that consumers should have better control of the money spent on their health care and a better idea of what things cost. Now, this has basically been the theme of Republican health plans for as long as I can remember. And the lead author of this plan is Lanhee Chen, who worked for Republicans in the Senate and then led presidential candidate Mitt Romney’s policy shop, and whose name has been on a lot of conservative proposals. But I find this one notable more for its timing. Republicans, as we mentioned, appear to have internalized the idea that the only thing they can agree on when it comes to health care is that they don’t like the Affordable Care Act. Is that changing or is this just sort of hope from the Republican side of the policy wonk shop?
Sanger-Katz: I think this is connected to the discussion that we had about the debate, but it feels to me like we are in a bit of a post Obamacare era where the fights about “Are we going to continue to have Obamacare or not?” have sort of faded from the mainstream of the discussion. But there’s still plenty of discussion to be had about the details. The Democrats clearly want to expand Obamacare in various ways. Some of those they have done in a temporary fashion. Others are still on the wish list. And I think this feels very much like the kind of calibration adjustment, you know, small changes, tinkers on the Republican side to try to make the health insurance market a little bit more market-based. But this is not a big overhaul kind of plan. This is not a repeal-and-replace plan. This is not a plan that is changing the basic architecture of how most Americans get their insurance and how it is paid for. This is a plan that is making small changes to the regulation of insurance and to the way that the federal government finances certain types of insurance. That said, I think the fact that it’s more incremental makes it feel like these are things that are more likely to potentially happen because they feel like there are things that you could do without having a huge disruptive effect and a big political backlash and that you could maybe develop some political consensus around.
Rovner: It does, although I do feel like, you know, this is a very 2005 plan. This is the kind of thing that we would have seen 15 years ago. But as Democrats have gotten the Affordable Care Act and discovered that the details make it difficult, Republicans have actually gotten a lot on the transparency side and, you know, helping people understand what things cost. And that hasn’t worked very well either. So there’s a long way to go, I think, on both sides to actually make some of these things work. Victoria, did you want to add something?
Knight: Yeah, I’ve been talking to Republicans a lot, trying to figure out like what is their next go-to going to be. And I think they’re pretty understanding that ACA is set in place, but they still don’t want to give up that there are alternative types of health insurance that they want to put out there. And I think that seems that’s kind of what they realize they can accomplish if they get another Republican president and they’re going to try to do association health plans again. They’re going to try to expand some of these what they call health reimbursement arrangements, things like that, to just like kind of try to add some other types of health insurance options, because I think they know that ACA is just too entrenched and that there’s not much else they can do outside of that. And then, yeah, I think focus a little more on the transparency and cost because they know that’s a winning message and that is the one thing in Congress right now on the health care end that seems to have bipartisan momentum for the most part.
Rovner: Yeah, I think you’re absolutely right. Well, another issue that could have come up in last night’s debate but didn’t was the unwinding of Medicaid coverage from the pandemic. The news this week is that the first lawsuit has been filed accusing a state of mistreating Medicaid beneficiaries. The suit filed against Florida by the National Health Law Program and other groups is on behalf of two kids, one with a disability, and a mom who recently gave birth. All would seem to still be eligible, and the mom says she was never told how to contest the eligibility determination that she was no longer eligible, and that she was cut off when she tried to call and complain. State officials say their materials have been approved by the Centers for Medicare & Medicaid Services, which they have, and that Florida, in fact, has a lower procedural disenrollment rate than the average state, which is also true. But with 5 million people already having been dropped from Medicaid, I imagine we’re going to start to see a little more pushback from advocacy groups about people who are, in all likelihood, still eligible and have been wrongly dropped. I’m actually a little surprised that it took this long.
Kenen: Many of the people who have been dropped, if they’re still eligible, they can get recertified. I mean, there’s no open enrollment season for Medicaid. If you’re Medicaid-eligible, you’re Medicaid-eligible. The issue is, obviously, she didn’t understand this. It’s not being communicated well. If you show up at the hospital, they can enroll you. But people who are afraid that they aren’t covered anymore may be afraid of going to the hospital even if they need to. So there’s all sorts of bad things that happen. In some of these cases, there are simple solutions if the person walks in the door and asks for help. But there are barriers to walking in the door and asking for help.
Rovner: I was going to say one of the plaintiffs in this lawsuit is a child with a disease …
Kenen: Cystic fibrosis.
Rovner: Right. That needs expensive drugs and had not been able to get her drugs because she had been cut off of Medicaid. So there’s clearly stuff going on here. It’s probably true that Florida is better than the average state, which means that the average state is probably not doing that well at a lot of these things. And I think we’re just starting to see, you know, it’s sort of mind-numbing to say, oh, 5 million people have been separated from their health insurance. And again, we have no idea how many of those have gotten other health insurance, how many of those don’t even know and won’t know until they show up to get health care and find out they’re no longer covered. And how many people have been told they’re no longer covered but can’t figure out how to complain and get back on?
Sanger-Katz: And it’s this very extreme thing that’s happening right now. But it is, in many ways, the normal system on steroids. You know, if you’ve been covering Medicaid for any period of time, as all of us have, like, people get disenrolled all of the time from Medicaid for these administrative reasons, because of some weird hiccup in the system, they move, their income didn’t match in some database. This is a problem that a lot of states face because they have financial incentives often to drop people off of Medicaid because they have to pay a portion of the cost of providing health care. And a lot of them have rickety systems, and they’re dealing with a population that often has unstable housing or complicated lives that make it hard for them to do a lot of paperwork and respond to letters in a timely way. And so part of the way that I’ve been thinking about this unwinding is that there’s a particular thing that’s happening now, and I think there’s a lot of scrutiny on it, appropriately. And I think that there should be to make sure that the states are not cutting any corners. But I also think in some ways it’s sort of like a way of pressure-testing the normal system and reminding us of all of the people who slip through the cracks in normal times and will continue to do so after this unwinding is over. And these stories in Florida, to me, do not feel that dissimilar from the kinds of stories that I have heard from patients and advocates in states long before this happened.
Rovner: Yeah, I think you’re right. It’s just shining a light on what happens. I mean, it was the oddity that they were … states were not allowed to redetermine eligibility during the pandemic because normally states are required to redetermine eligibility at least once a year. And I think some do it twice a year. So it’s, you know, these redeterminations happen. They just don’t happen all in a huge pile the way they’re happening now. And I think that’s the concern.
Sanger-Katz: And it also, I think, really shines a light on the way that Medicaid is structured, where the Affordable Care Act simplified it quite a lot because, [for example], you’re in an expansion state and you earn less than a certain amount of money, then you can get Medicaid. But there are all of these categories of eligibility where, you know, you have to be pregnant, you have to be the parent of a child of a certain age. You have to demonstrate that you have a certain disability. And I think [it] is a reminder that this is a pretty complicated safety net, Medicaid. You know, there’s lots of things that beneficiaries have to prove to states in order to stay eligible. And there’s lots of things, honestly, you know, if states really want to make sure that they are reserving resources for the people who need them, that they do need to be checking on. And so I think we’re all just sort of seeing that this is a messy, complicated process. And I think we’re also seeing that there are these gaps and holes in who Medicaid covers. And it’s not the case that we have a perfect and seamless system of universal coverage in this country. We have this patchwork and people do fall between the cracks.
Kenen: And this is one of the most vulnerable populations, obviously. Some of the elderly are also very vulnerable, but these are people who may not speak either English or Spanish. They don’t have access to computers necessarily. I mean, we’re giving the least assistance to the population that needs the most assistance. And, you know, I mean, I think if Biden wanted to be really savvy about fixing it, he’d come out with some slogan about “Instead of Medicare unwinding, it’s time to have Medicare rewinding,” or something like that, because they’re going to have to figure … I mean, they have taken some steps, but it’s a huge mess, and the uninsurance rate is going to go up, and hospitals are going to have patients that are no longer covered, and it’s not going to be good for either the health care system or certainly the people who rely on Medicaid.
Rovner: I think it’s noteworthy how much the administration has been trying not to politicize this, that apparently, you know, we keep hearing that they won’t even tell us which states, although you can … people can sort of start to figure it out. But, you know, states that are having a more difficult time keeping eligible people on the rolls, shall we say, when the administration could have … I mean, they could be trumpeting, you know, which states are doing badly and trying to shame them. And they are rather very purposely not doing that. So I do think that there’s at least an attempt to keep this as collegial, if you will, as possible in a presidential election year. So my colleagues here at KFF have a depressing, but I guess not all that surprising, poll out this week about medical misinformation and how much of the public believes things that simply aren’t true — like that more people died from the covid vaccine than covid itself, or that ivermectin is a useful treatment for the virus. It’s not. It’s for parasites. And the survey didn’t just ask about covid. People have been exposed to, and a significant percentage believe, things like that it’s harder to get pregnant if you’ve been on birth control and stop. It isn’t. Or that people who keep guns in their house are less likely to be killed by a gun than those who don’t. They’re not. But what’s really depressing is the fact that the pandemic seems to have accelerated an already spiraling trend in distrust of public institutions in general: government, local and national media, and social media. Are we ever going to be able to start to get that back? I mean, you know, we talk about the woes with public health, but this goes a lot deeper than that, doesn’t it?
Kenen: And it’s not just health care. When you look at historical metrics about trust — which I’ve had to for a course I teach — we were never a very trusting society, it turns out. We’ve had large sectors of the population haven’t been trusting of many institutions and sectors of society for decades. We’re just not too huggy in this country. It’s gotten way worse. And what you said is right, but it’s broad. It’s not just doctors. It’s not just vaccines, it’s expertise. This distrust is really corrosive. But of all the things in that survey, one that really blew me away was we’re like, what, 13 years since Obamacare was passed? Only 7% or 8% — “only,” I should say only in quotes, you know — only 7% or 8% still thought there were death panels, but something like 70% wasn’t sure if there were death panels. Like, has anyone known anyone who went before a death panel? Since 2010? And yet 70% — I mean, I may be a little off, I didn’t write it down — but it’s something like 70% weren’t sure. And that is a mind-blowing number. It just says, you know, they weren’t ready to come out and say, yes, there are death panels. But that meant that a lot of Democrats also weren’t sure if there were death panels There are no death panels.
Knight: I was just gonna say, I also thought it was interesting that it showed people do use social media to get a lot of their information, but then they also don’t trust the information that they get on there. So it’s kind of like, yeah …
Rovner: And they’re right not to!
Knight: Yeah, they’re absolutely right not to. But then it’s also like, well, they’re then just not getting health information at all, or if they’re getting it, they just don’t trust it. So just showcasing how difficult it is to fill that void of health information, like, people just aren’t getting it or don’t trust it.
Rovner: I feel like some of this is social literacy. I mean, you know, we talk about health literacy and things that people can understand, but, you know, people don’t understand the way journalism works, the difference between the national news and what you see on Facebook. And I think that’s, Joanne, going back to your point about people not trusting expertise, it’s also not being able to figure out what expertise is and who has expertise. I mean, that’s really sort of the bottom line of all this, isn’t it?
Kenen: Well, I mean, I was doing some research — I can’t remember the exact details, this was something I read several months ago — but there was one survey maybe a couple of years ago where the majority of people said they don’t trust the news they read, but they’re still getting their news from something that they don’t trust. So it sounds sort of funny, but it’s actually not. I mean, it’s really a crisis of people don’t know what to believe. The uncertainty is corrosive, and it’s health care and politics, this widening chasm of people with alternative sets of facts — or alternative worldviews, anyway. So it’s not good. I mean, it was a really good survey, it was a really interesting survey, but some of it wasn’t so surprising. I mean, that there’s still people who, like, the fertility issues and the vaccines. You can sort of understand why those have lingered in the environment we’re in. I had actually had a conversation the other day with a political scientist who had studied the death panel rumors 10 years ago. And I said, what about now? And, you know, he was sort of … he hadn’t looked at it and he was sort of saying, well, you know, there aren’t any. And people have probably figured that out by now. Well, no. I have to email him the study, right?
Sanger-Katz: Anytime that I read a study like this, I am also reminded — and I think it is useful for all of us to be reminded of this and probably most people who are listening to the podcast — that the average American is just not as tuned in on the news and on the Washington debate and on the minutia of public policy, as all of us are. So, you know, and I think that that is part of the reason why you see so many people not sure about these things. It’s clearly the case that they are being exposed to bad information and that is contributing to their uncertainty. And I think the rise of misinformation about both health policy and about actual, you know, health care, in the case of covid, is a bad and relatively newer phenomenon. But I also think a lot of people just aren’t paying that close attention, you know, and it’s good to be reminded of that.
Kenen: The book I just read that I referred to — it’s by an MIT political scientist named Adam Berinsky, and it’s called “Political Rumors.” And it just came out, and he was talking about exactly that, that we’re all exposed to misinformation. We can’t avoid it. It’s everywhere. And that for people who aren’t as engaged with day-to-day politics, they end up uncertain. That’s this messy middle, which they also use in the KFF survey. They came up with a very similar conclusion about the “muddled middle,” I think was the phrase they used. And what this political scientist said to me the other day was that, you know, pollsters tend to not look at the “I don’t know, I’m uncertain, no opinion.” They sort of shunt them aside and they look at the “yes” or “no” people. And he was saying, no, no, no, you know, this is the population we really need to pay attention to, the “Uncertains” because they’re probably the ones you can reach more. And in the real world, we saw that with vaccination, right? I mean, in the primary series — I mean, booster takeup was low — but in the primary when there was a lot of uncertainty about the vaccines, the people who said “no way I am ever going to get the vaccine” — I mean, KFF was surveying this every month — most of them didn’t. You know, a few on the margins did, but most of them who were really militantly against the vaccine didn’t take it. The ones who were “I don’t know” and “I’m a little scared” and “I’m waiting and seeing” … a lot of them did take it. They were reached. And that’s sort of an important lesson to shift the focus as we deal with distrust, as we deal with disinformation and we deal with messaging, which is good, and truth-building and confidence-building, it is that muddled middle that’s going to have to be more of a target than we have traditionally thought.
Rovner: Well, in the interest of actually giving good information, we have a couple of updates on the reproductive health front. For those of you keeping score, abortion bans took effect this week in South Carolina and Indiana after long drawn-out court battles. Meanwhile, in Texas, an update to our continuing discussion of women with pregnancy complications who’ve been unable to get care because doctors fear running afoul of that state’s ban, a couple of weeks ago, reports Selena Simmons-Duffin at NPR, Texas Gov. Greg Abbott very quietly signed a law that created a couple of exceptions to the ban for ectopic pregnancies and premature rupture of membranes, both of which are life-threatening to the pregnant woman, but just not necessarily immediately life-threatening. I had not heard a word about this change in the law until I saw Selena’s story. Had any of you?
Kenen: In fact, it should have come up because of this court case in Texas about, you know, a broader health exception — it’s not even “health,” it’s life-threatening. It’s like, at what point do you get sick enough that your life is in danger as opposed to, you know, should you be treating that woman before … you see what direction it’s going, and you don’t let them go to the brink of death? I mean, that was the court case and Abbott fought that. But yeah, it was interesting.
Rovner: It was a really interesting story that was also, you know, pushed by a state legislator who was trying very hard not to … never to say the word abortion and to just make sure that, you know, this was about health care and not abortion. It’s an interesting story, we will link to it.
Sanger-Katz: I wonder if other states will do this as well. It seems like, as we’ve discussed, you know, abortion bans are not as popular as I think many Republican politicians thought they would [be]. And I do think that these cases of women who face really terrible health crises and are unable to get treated are contributing to the public’s dislike of these policies. And on the one hand, I think that there is a strong dislike of exceptions among people who support abortion bans because they don’t want the loopholes to get so big that the actual policy becomes meaningless. On the other hand, it seems like there is a real incentive for them in trying to fix these obvious problems, because I think it contributes to bad outcomes for women and children. And I think it also contributes to political distaste for the abortion ban itself.
Kenen: But it’s very hard to legislate every possible medical problem … I mean, what Texas did in this case was they legislated two particular medical problems. And some states … they have the ectopic — I mean, ectopic is not … there’s no stretch of the imagination that that’s viable. Right? The only thing that happens with an ectopic pregnancy is it either disintegrates or it hemorrhages. I mean, the woman is going to have a problem, but making a list of “you get this condition, you can have a medical emergency abortion, but if you have that condition and your state legislator didn’t happen to think about it, then you can’t.” I mean, the larger issue is: How do you balance the legal restrictions and medical judgments? And that’s … I don’t think any state that has a ban has completely figured that out.
Rovner: Right. And we’re back to legislators practicing medicine, which is something that I think the public does seem to find distasteful.
Sanger-Katz: I mean, I don’t think that this solves the problem at all, but I think it does show a surprising responsiveness to the particular bad outcomes that are getting the most publicity and a sort of new flexibility among the legislators who support these abortion bans. So it’s interesting.
Rovner: All right. Meanwhile, another shocking story about pregnant women being treated badly. The Centers for Disease Control and Prevention reported this week that a survey conducted this April found that 1 in 5 women reported being mistreated by medical professionals during pregnancy or delivery. For women of color, the rate was even higher: more than 1 in 4. Mistreatment included things like getting no response to calls for help, being yelled at or scolded, and feeling coerced into accepting or rejecting certain types of treatment. We know a lot of cases where women in labor or after birth reported problems that went ignored. Among the most notable, of course, was tennis legend Serena Williams, who gave birth to her second child this week after almost not surviving the birth of her first. We’re hearing so much about the high maternal mortality rate in the U.S. What is it going to take to change this? This isn’t something that can be solved by throwing more money at it. This has got to be sort of a change in culture, doesn’t it?
Kenen: No. I mean, it’s … if someone who’s just given birth, particularly if it’s the first time and you don’t know what’s normal and what’s not and what’s dangerous and what’s not dangerous, and, you know, it’s a trauma to your body. I mean, you know, I had a very much-wanted child, but labor is tough, right? I always say that evolution should have given us a zipper. But the philosophy should be, if someone who’s just been through this physical and emotional ordeal, has discomfort or a question or a fear, that you respect it and that you calm it down, you don’t dismiss it or yell at somebody. When you’re pregnant, you read all these books and you go to Lamaze workshops and you learn all this stuff about labor and delivery. You learn nothing about what happens right after. And it’s actually quite uncomfortable. And no one had ever told me what to expect. And I didn’t know. And I always, like, when younger women are having babies, I let them know that, you know, talk to your doctor or learn about this or be prepared for this, because that is a really vulnerable point. And that this survey — and it’s more Black and poor women, and Latina women in this survey, it’s not that … it’s disproportionate like everything else in health care — they’re being disrespected and not listened to. And some of them are going to have bad medical outcomes because of that.
Rovner: As we are seeing. All right. Well, that is this week’s news now. We will take a quick break. Then we will come back and do our extra credit.
Hey, “What the Health?” listeners: You already know that few things in health care are ever simple. So if you like our show, I recommend you also listen to “Tradeoffs,” a podcast that goes even deeper into our costly, complicated, and often counterintuitive health care system. Hosted by longtime health journalist and my friend Dan Gorenstein, “Tradeoffs” digs into the evidence and research data behind health care policies and tells the stories of real people impacted by decisions made in C-suites, doctors’ offices, and even Congress. Subscribe wherever you get your podcasts.
OK, we’re back. It’s time for our extra-credit segment. That’s when we each recommend a story we read this week we think you should read too. As always, don’t worry, if you missed it; we will post the links on the podcast page at KFFHealthNews.org and in our show notes on your phone or other mobile device. Victoria, why don’t you go first this week?
Knight: So my extra credit is from The New York Times, and the story is called “The Next Frontier for Corporate Benefits: Menopause.” It basically details how a lot of companies are realizing that, you know, as more women get into leadership positions, high-level leadership, executive positions, they’re in their 40s, late 40s, early 50s, that’s when menopause or perimenopause starts happening. And that’s something that can last for a while. I didn’t realize the stories, that it can last almost 10 years sometimes. And so it was talking about how, you know, it affects women for a long period of time. It can also affect their productivity in the workplace and their comfort and being able to accomplish things. And so they were realizing, you know, we kind of need to do something to help these women stay in these positions. And there was actually an interesting tidbit at the very end where it was talking about some companies may even be, like, legally compelled to make accommodations. And that’s due to the new Pregnant Workers Fairness Act, which says that employers have to provide accommodations for people experiencing pregnancy but also related medical conditions. They’re saying menopause could be included in that. And just some of the benefits some of these companies were offering were access to virtual specialists, but they were talking about, like, if they need to do other things like cooling rooms and stuff like that. So I thought it was kind of interesting. And another employer benefit that maybe some employers are thinking about adding.
Kenen: I think all offices should have, like, little nap cubicles and man-woman, pregnant-not pregnant. And, you know, just like “life is rough.” [laughter]
Knight: I agree.
Kenen: Just a little corner!
Rovner: Joanne, why don’t you go next?
Kenen: Mine is from The Atlantic. It’s by Lola Butcher. And it is “A Simple Marketing Technique Could Make America Healthier.” And it’s basically talking about how some medical practices are doing what we in the news business and the tech industry knows of as “A-B testing.” You know, a tech company may try a big button or a little button and see which one consumers like. Newsrooms change headlines— headline A, headline B and see which one draws more readers — and that hospitals and medical practices have been trying to do. In some cases, it’s text messaging two different kinds of reminders to figure out, you know … one example was the message with something like 78 characters got women to book a mammogram, but a message with 155 characters did not. Two text messages were better than one for booking children’s vaccines. So some people are very excited about this. It’s getting people to do preventive care and routine care. And some people think this is just not the problem with health care, that it’s way deeper and more systemic and that this isn’t really going to move the needle. But it was an interesting piece.
Rovner: Any little thing helps.
Kenen: Right. This was an interesting piece.
Rovner: Margot.
Sanger-Katz: I wanted to talk about an article in KFF Health News from Taylor Sisk. The headline is “Life in a Rural ‘Ambulance Desert’ Means Sometimes Help Isn’t on the Way,” and it’s a really interesting exploration of some of the challenges of ambulance care in rural areas, which is a topic that is near and dear to my heart. Because when I was a reporter in New Hampshire covering rural health care delivery, I spent the better part of a year writing about ambulance services and the challenges there. And I think this story is highlighting a real challenge for people in these communities. And I think it’s also really a reminder that the ambulance system is this weird, off-to-the-side part of our health care system that I think is often not well integrated and not well thought of. It tends to be regulated as transportation, not as health care. It tends to be provided by local governments or by contractors hired by local governments as opposed to health care institutions. It tends to have a lot of difficulty with billing a very high degree of surprise billing for its patients, and also just a real lack of health services research about best practices for how fast ambulances should arrive, what level of care they should provide to people, and on and on. And I just think that it’s good that she’s highlighted this issue. And also, I think it is a reminder to me that ambulances are probably worth a little bit more attention from reporters overall.
Rovner: Well, my story is also something that’s near and dear to my heart because I’ve been covering it for a long time. It’s from my KFF Health News colleague Lauren Sausser. It’s called “Doctors and Patients Try to Shame Insurers Online to Reverse Prior Authorization Denials.” And it is a wonderful 2023 update to a fight that Joanne and I have been covering since, what, the late 1990s. It even includes comments from Dr. Linda Peeno, who testified about inappropriate insurance company care denials to Congress in 1996. I was actually at that hearing. The twist, of course, now is that while people who were wrongly denied care at the turn of the century needed to catch the attention of a journalist or picket in front of the insurance company’s headquarters. Today, an outrage post on Instagram or TikTok or X can often get things turned around much faster. On the other hand, it’s depressing that after more than a quarter of a century, patients are still being caught in the middle of appropriateness fights between doctors and insurance companies. Maybe prior authorization will be the next surprise medical bill fight in Congress. We shall see. All right. That is our show for the week. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left us a review; that helps other people find us, too. Special thanks, as always, to our amazing engineer, Francis Ying. Also, as always, you can email us your comments or questions. We’re at whatthehealth@kff.org. Or you can tweet me or X me or whatever. I’m @jrovner, also on Bluesky and Threads. Joanne?
Kenen: I am also on Twitter, @JoanneKenen; and I’m on Threads, @joannekenen1; and Bluesky, JoanneKenen.
Rovner: Margot.
Sanger-Katz: I’m @sangerkatz.
Rovner: Victoria.
Knight: I’m @victoriaregisk on X and Threads.
Rovner: Well, we’re going to take a week off from the news next week, but watch your feed for a special episode. We will be back with our panel after Labor Day. Until then, be healthy.
Credits
Francis Ying
Audio producer
Stephanie Stapleton
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ ‘What the Health?’ on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 9 months ago
Courts, COVID-19, Elections, Medicaid, Multimedia, States, The Health Law, Abortion, KFF, KFF Health News' 'What The Health?', Misinformation, Podcasts, Polls, Pregnancy, texas, Women's Health