Global warming and health
TODAY we conclude our two-part series on the impact of global warming on health, highlighting the compounding issues of inequality and vulnerability and the need to have viable public health interventions and mitigation strategies to protect vulnerable individuals and communities.
Inequality and vulnerability
TODAY we conclude our two-part series on the impact of global warming on health, highlighting the compounding issues of inequality and vulnerability and the need to have viable public health interventions and mitigation strategies to protect vulnerable individuals and communities.
Inequality and vulnerability
Climate change exacerbates inequalities, such as those driven by systemic economic injustice and disproportionately affect poor and marginalised communities. Persons living in less developed countries bear the greatest burden of most vector-borne diseases, a circumstance that reinforces health inequities and impedes socio-economic development. Poverty, poor environmental conditions, inadequate housing and living conditions, and limited access to affordable quality health services exacerbate the effect. Children and the poor are particularly susceptible, owing in part to the effects of malnutrition; women and the elderly are also at increased risk. Vector-borne diseases during pregnancy are associated with particularly poor health outcomes among mothers and newborns from low-income or otherwise disadvantaged groups, as evidenced by the devastating effects of congenital infection with Zika virus during the explosive epidemic of Zika virus infection (which was spread by aedes mosquitoes) in Brazil in 2015.
Public health interventions
Improvements in the public awareness, detection, prevention, and treatment of vector borne diseases have been driven by investments in surveillance and control and form the basis of adaptation strategies for a changing climate. Appropriate specific measures vary according to disease, pathogen life cycle, and the level of risk and may include a combination of climate-informed, early-warning systems, enhanced and new land-use management strategies, improved access to prevention measures (eg, biologic mosquito control, personal protective measures, insecticides, and vaccines), and new and improved therapies. For public health interventions to have a successful outcome, there must be timely and adequate stakeholder engagement, community and household acceptance and equally important, appropriate, and sustainable long-term funding mechanisms. A 2017 survey of 1,083 US vector-control programmes showed that 84 per cent of the programmes were rated as "needs improvement" in one or more core competencies (eg, insecticide-resistance testing). The same year, the Centers for Disease Control and Prevention (CDC) established five regional centres of excellence to help respond to emerging vector borne diseases and to help create a new generation of vector experts.
Malaria highlights several challenges that can occur in the implementation of adaptation strategies. After two decades of concerted international and national investment and consistent declines in malaria cases and malaria-related deaths, worldwide funding has stagnated; malaria is now resurgent in several countries, owing in part to increasing drug and insecticide resistance. This has been worsened to some degree by service and supply chain disruptions resulting from the COVID-19 pandemic. Innovations and leadership are needed to keep up with biologic and socio-economic challenges and to ensure equitable access to high-quality treatment in low- and middle-income countries.
The prevention of dengue and West Nile virus infection relies mainly on community-level mosquito-control programmes; the implementation of such programmes varies according to several factors, including funding and operational management. Avoidance of the vector habitat during the transmission season as a result of public communication has long been an important prevention strategy for Lyme disease. Various personal protective measures (eg, insect repellent and protective clothing) and tick-control strategies (eg, the culling of deer) have been proposed as approaches to reduce the risk of Lyme disease, but evidence of effectiveness is generally lacking.
Vaccines have been successful in the prevention of three vector-borne diseases: yellow fever, Japanese encephalitis, and tick-borne encephalitis. Unfortunately, vaccines approved for malaria and dengue in the past several years have had only limited success. Scientists continue to work on developing new and more effective vaccines that target vector borne diseases with some promise. A recent phase 2 trial in Mali (West Africa) showed the effectiveness of a single infusion of a monoclonal antibody against Plasmodium falciparum infection over a six-month follow-up period during malaria season. Also promising is a new dengue vaccine which has shown promise in a phase three trial and regulatory approval by European authorities is being sought.
According to the Intergovernmental Panel on Climate Change, successful vaccine development and uptake have the potential to substantially offset the effect of climate change on vector borne diseases. There remains some challenge though with combating vaccine hesitancy which has become more pronounced since the COVID-19 pandemic.
Better surveillance data and early-warning systems are critical to enhance public awareness, facilitate the targeting of resources (human and financial) for improved responses, and identify knowledge gaps and research needs. Adaptation plans must be time-sensitive, culturally sensitive and context-specific while also considering factors such as shifting disease patterns, extreme weather events, and current and future climate variations and trends. This approach will require collaboration among various sectors, such as national and local health authorities, civic society groups, affected communities, urban planners, and climate experts.
Implications for clinical practice
With increased international travel, there is limited geographic confinement of any transmissible vector-borne illness. Increasing prevalence in any geographic locations puts the entire global community at risk. It is only a question of time before any vector-borne illness in one location is seen in other locations, as long as global warming creates the requisite environment. Improved education of health-care professionals and community workers is needed with respect to specific vector borne diseases, particularly in regions in which diseases are newly emerging or anticipated to emerge. In many locations, clinicians are likely to see more cases of vector borne diseases during longer transmission seasons, especially in regions with historically low levels of transmission. Awareness of local changes in disease rates and travel histories will be helpful in the evaluation process. The non-specific clinical manifestations of many vector borne diseases often make diagnosis difficult. Strategies for the prevention and treatment of vector-borne diseases should be reviewed regularly and systematically. To help address the additional burden of health care delivery created by a changing climate, health professionals can advocate for more climate-resilient health systems and for programs that focus on the current worldwide shortages of health professionals, including infectious-disease experts.
Mitigation of climate change
Reducing the risks of vector borne diseases and other health consequences of climate change requires not only adaptation but also a rapid and equitable transition from fossil fuels to more environmentally friendly alternative energy sources. The global carbon footprint currently is largely driven by emissions in the West. It is important that decarbonisation of climate is not done in a way that is detrimental to developing countries or impedes industrialisation and economic development in countries that are already severely underdeveloped. The current push to stagnate development in poorer countries is misguided.
The signing of the Inflation Reduction Act of 2022 represents a necessary (although insufficient) move toward decarbonising the US economy in line with the goals set under the Paris Agreement in 2015. The health-care sector, which contributes an estimated 4.9 per cent of the total carbon footprint worldwide, must be part of the process. As trusted voices, health professionals can weigh in regarding the importance and urgency of mitigation.
Conclusions
Climate change has substantial effects on pathogens, vectors, and reservoir hosts, with implications for the health sector worldwide. Many vectors are already expanding their latitude and altitude ranges, and the length of season during which they are active is increasing; these trends are expected to continue as the climate continues to warm. Changes at the local level will be context- and disease-specific. Clinicians must be well informed and constantly alert to changes in risk for the population they serve.
To protect health and equity in a warmer world, investments are needed in vector control with respect to tailoring measures to rapidly emerging situations and in new forms of technology and approaches, including vaccines. Unfortunately, adaptation strategies will not be viable as a long-term solution without the implementation of sufficient, urgent mitigation efforts to maintain global temperatures below critical thresholds.
Dr Ernest Madu, MD, FACC and Dr Paul Edwards, MD, FACC are consultant cardiologists for the Heart Institute of the Caribbean (HIC) and HIC Heart Hospital. HIC is the regional centre of excellence for cardiovascular care in the English-speaking Caribbean and has pioneered a transformation in the way cardiovascular care is delivered in the region. HIC Heart Hospital is registered by the Ministry of Health and Wellness and is the only heart hospital in Jamaica. Send correspondence to info@caribbeanheart.com or call 876-906-2107
2 years 5 months ago
Sagicor Life's Paramedic Unit now offering Pap smear services
SAGICOR Life Jamaica (SLJ), through its paramedic unit located at the SLJ Head Office, 24-48 Barbados Avenue, is now offering Pap smear services to insurance clients and prospective clients for insurance products.
During the official ribbon-cutting ceremony held on Tuesday, January 31, the company highlighted that the new service was created to help alleviate an overwhelming demand for the screening.
A Pap smear is a screening test that checks for abnormal cell changes of the cervix that may lead to cervical cancer.
Mark Chisholm, chief revenue officer and executive vice-president of Sagicor Life Jamaica, highlighted that the move was a welcome one in the fight against cancer.
"As industry leaders it is important that we continue to play our part in ensuring the total wellness of all Jamaicans. With this new Pap smear service our paramedic unit team is now able to provide a well-needed diagnostic service in cancer screening," he expressed. Chisholm also commended the Jamaica Cancer Society for the work it has done over the years.
A lunch and learn session was also held on opening day for clients and team members to be educated on Pap smear myths and facts. Dr Nicole Urquhart, resident doctor, Paramedic Unit, SLJ, stressed the importance of women over 18 years of age who are sexually active making a Pap smear test priority every two years.
"Women should know that despite popular belief, Pap smear screening is not a painful procedure and remains a vital tool in detecting early cervical changes. SLJ continues to meet the needs of our clients, and with the addition of our Pap smear service they can now enjoy a one-stop facility that gives them ease and convenience," shared Dr Urquhart.
In 2022 SLJ partnered with the Jamaica Cancer Society to offer free Pap smear screenings in recognition of Cervical Cancer Awareness Month.
2 years 5 months ago
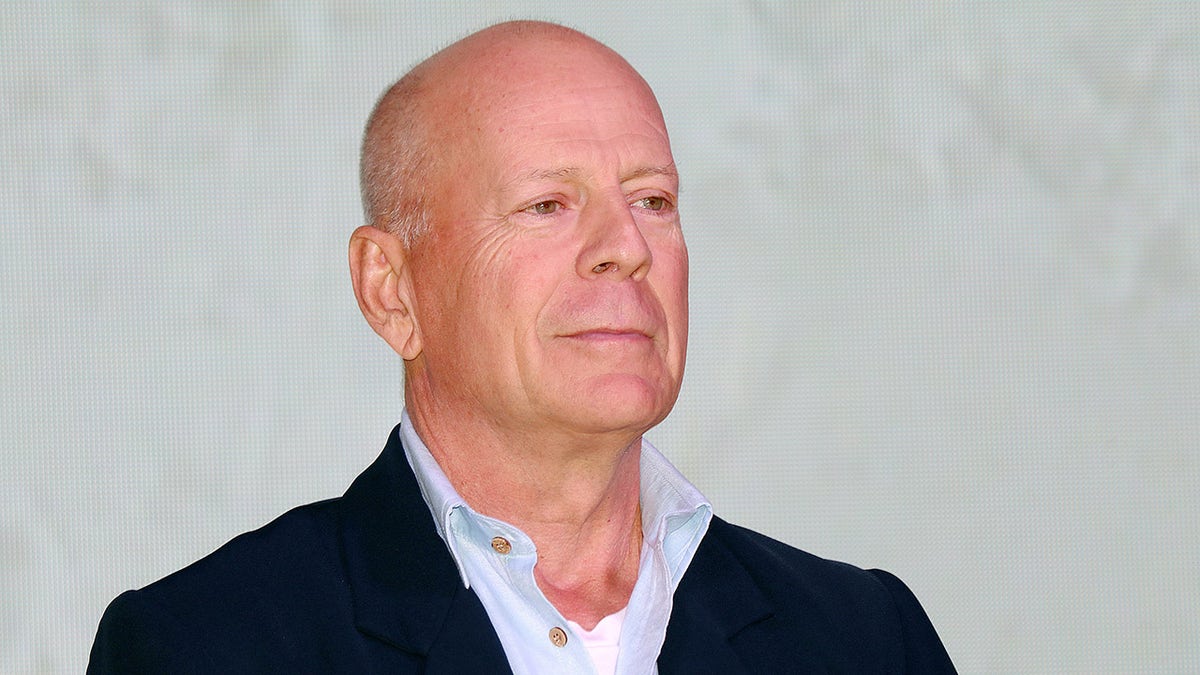
What is frontotemporal dementia, the diagnosis Bruce Willis has received?
The family of Bruce Willis, who is 67, announced this week that the actor has been diagnosed with frontotemporal dementia (FTD).
The news comes nearly a year after the announcement that Willis would be stepping away from acting due to a diagnosis of aphasia, a language disorder that impacts the ability to speak, read and write.
A study by researchers with New York City's Columbia University found that one in every 10 adults over 65 has some form of dementia.
BRUCE WILLIS' DEMENTIA BATTLE: ICONIC STAR'S JOURNEY FROM ACTION HERO TO FAMILY MAN
While most people are familiar with Alzheimer’s disease, which is the most common type, FTD is likely not as well-known.
FTD, as defined by Johns Hopkins Medicine in Baltimore, Maryland, is "a group of disorders that occur when nerve cells in the frontal and temporal lobes of the brain are lost. This causes the lobes to shrink. FTD can affect behavior, personality, language and movement."
FTD typically affects men and women between 40 and 65 years of age.
While symptoms of FTD can vary depending on what part of the brain is affected, most people with the condition experience some common symptoms, as listed on the Johns Hopkins Medicine website.
Behavior or personality changes are often the most obvious indicators. These may include public outbursts or socially inappropriate actions.
People with FTD also tend to have impaired judgment, a lack of empathy and lower self-awareness, Johns Hopkins states.
Others may notice sufferers losing interest in activities they used to enjoy or withdrawing emotionally from friends and family members.
This type of dementia is also marked by a reduced ability to understand or formulate language.
People may struggle to remember the names of objects, string words into sentences or even recall the meanings of words they used to know.
They may have trouble planning and organizing — and find that they are easily distracted.
FIRST DRUG PROVEN TO SLOW ALZHEIMER'S WON'T BE AVAILABLE TO MOST PATIENTS FOR SEVERAL MONTHS
Eventually, the person with FTD may end up speaking less frequently out of frustration. The condition can also lead to agitation, irritability and drastic mood swings.
Dr. Tiffany Chow, vice president of clinical development and neurology at Alector, Inc. in San Francisco, California, has spent most of her career working with patients and families living with dementia and investigating clinical trials for these illnesses.
"Most people aren’t expecting dementia to start in their 50s," she told Fox News Digital in an email.
"The earliest signs of FTD can be so subtle that they're often misinterpreted as a ‘midlife crisis,’ which then delays appropriate medical attention."
Dr Chow said that many family members have told her they remember their loved one acting in a way that was uncharacteristic.
In one example, someone who had handled tax returns capably for the last 25 years was suddenly unable to organize receipts and other paperwork.
NEW STUDY INDICATES DEMENTIA SIGNS CAN BE DETECTED NEARLY A DECADE BEFORE DIAGNOSIS
There was also a seasoned camper who found herself unable to set up her tent without help.
"The tricky part is that the change doesn't occur overnight, from normal to consistently disabled," said Dr. Chow.
"Isolated events are noticed maybe every few months, and it's hard to string those together into a major concern until the changes are seen on a daily basis," Dr. Chow also said.
If a clinician isn’t aware of FTD, there’s a risk it will be misdiagnosed as a midlife crisis or a psychiatric condition such as bipolar affective disorder.
"One of the big challenges in our field is to get the word out to primary care physicians about this relatively rare cause of dementia," Dr. Chow said.
The doctor said there are some new checklists and tools available to help patients pinpoint the changes they’re experiencing. Otherwise, there is no single universal screening test for FTD.
CONSUMING ULTRA-PROCESSED FOODS COULD INCREASE DEMENTIA RISK: STUDY
"This is very different from Alzheimer's disease, where memory testing and cerebrospinal fluid tests can help in diagnosing the disease," said Dr. Chow.
"For FTD, the assessment of changes in frontal lobe functions is more complex, requiring an objective history from someone who can help the clinician understand the person's ‘normal’ level of function and how social skills have changed."
Although there is no universal diagnostic test, there are genetic screenings that can flag someone as more likely to develop FTD.
Dr. Chow said genetic testing is most helpful in diagnosing behavioral FTD and primary progressive aphasia (PPA), which affects patients’ ability to use language.
For those cases, up to 40% of the patients share a common genetic mutation.
The first step is to meet with a genetics counselor who can explain the potential consequences of learning the results.
"Sometimes even the people who should know don't want to know — and we all have to respect that," said Dr. Chow.
Development efforts are ongoing, including clinical trials, but there is no current FDA-approved treatment for FTD, said Chow.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
"For now, to minimize the risk of FTD or any other dementia, people can adopt overall lifestyle improvements such as heart-healthy choices and avoiding head trauma, which also promotes brain health," the doctor said.
The condition typically progresses over time, Johns Hopkins states on its website.
Patients can also seek treatments to alleviate symptoms, such as speech therapy or the use of antidepressants.
Eventually, those with FTD may need full-time care.
Approximately 50,000-60,000 people may have FTD, per data from the Alzheimer’s Association, a nonprofit group based in Chicago.
In addition to Bruce Willis, other celebrities that have been diagnosed with dementia over the years have included Ronald Reagan, Rita Hayworth, Robin Williams, Casey Kasem and Charlton Heston.
2 years 5 months ago
Health, parkinsons-disease, lifestyle, bruce-willis, illness, geriatric-health, family-and-friends, alzheimers, mental-health
Health Archives - Barbados Today
Teachers’ union pleads with landowners to clear lots near schools of vines
By Anesta Henry
Cow-itch vines growing on empty lots have been creating major headaches for some schools across the island and President of the Barbados Union of Teachers (BUT) Rudy Lovell wants landowners to have the offending lots cleared and maintained.
He has complained that cow-itch is becoming a “nuisance” as several schools have been affected already for this school term. One teacher who had a serious allergic reaction, was ordered by her doctor not to return to the school to which she was assigned.
Lovell charged that some of the offensive lands may even be owned by the State.
“This is a serious matter. The Barbados Union of Teachers is imploring, begging, beseeching, whatever word you want to use, landowners who have lands adjacent to schools that are harbouring cow-itch to clear the lands. This is becoming a nuisance and several schools have been affected. This term alone, Daryl Jordan Secondary, Grantley Adams Secondary, Gordon Greenidge Primary have been affected.
“Now I am getting complaints from Mount Tabor Primary, I am getting complaints from Blackman and Gollop Primary, from Thelma Berry Nursery, and this is just to name a few,” Lovell said.
He said that the Ministry of Education has been working to address the vexing issue, but admitted that they could only do “so much”.
When contacted, Minister of Environment and National Beautification, Adrian Forde, told Barbados TODAY he would be contacting the Ministry of Education and the Ministry of Health and Wellness to investigate the environmental concern being reported by the BUT.
“I would talk to the Minister of Education and find out what the concerns are. I know the Environmental Health offices under the Ministry of Health can also activate certain legislation under the Health Services Regulations as it relates to properties. So it would be a collective effort,” Forde said.
Meanwhile, Lovell said the union believes that landowners have a social responsibility to ensure that their lands do not pose any threat to persons in surrounding areas. The president said this is why the BUT is encouraging landowners who know that their properties are overgrown with bush, to clear the lots.
He said it is unfair to students, teachers and ancillary staff who occupy school plants, to have to be exposed to “this nuisance called cow-itch”.
“And even though we may ask the Ministry of Education to intervene at times, the Ministry of Education can only close the schools. And even after the schools are reopened, in some cases, the lands are not really cleared to the extent that the cow-itch has been totally removed. So we are asking the landowners to do what they are supposed to do by maintaining their properties.
“I know in some cases, schools have been reaching out to the landowners. But the thing is that this is an annual problem. We know that around this time of the year cow-itch grows. Why wait until it impacts or affects the occupants of the schools to then come and clear the fields? Why not be proactive as a landowner and seek to remove the cow-itch from the properties? I received calls on a daily basis with regards to cow-itch, it is a total nuisance,” Lovell said.
The BUT president also indicated that he has been getting multiple complaints from teachers that they have been experiencing allergic reactions as a result of the hazard.
Forde said he agreed 100 per cent with Lovell’s plea, and revealed that the Government was currently working on legislation that would address landowners being forced to either clear their lots or be subjected to penalties if they refuse to do so.
“The school of thought is that landowners who are not complying to have those persons be given a period of time to do the remedial work.”
He said if this fails, the Government would do the cleaning and bill the charges to the landowner whether it is through the land tax bill or by some other means.
“The legislation hasn’t been drafted yet but there are definitely plans to deal with this issue. Really and truly this is not how we should be operating as Barbadians, this is not who we are as a people,” Minister Forde said.
The post Teachers’ union pleads with landowners to clear lots near schools of vines appeared first on Barbados Today.
2 years 5 months ago
A Slider, Environment, Health, Local News
California requiere que hospitales recurran a familiares cercanos de pacientes para decisiones médicas, cerrando un vacío de larga data
Hace unos cuatro años, el doctor Gene Dorio formó parte del comité de ética de un hospital del sur de California cuyos administradores insistían en que ellos podían decidir si desconectaban el respirador de un paciente inconsciente, a pesar de que la esposa y los hijos querían seguir manteniendo al hombre con vida.
El año pasado, Dorio le explicó a legisladores estatales que el problema era que el hospital tenía derecho a invalidar los deseos de la familia porque el paciente no había hecho un documento de directiva avanzada, ni había designado a alguien con poder notarial. El hospital optó por escuchar a la familia, pero según la ley del estado, los deseos de la familia no tenían peso.
Eso ya no es así. Desde el 1 de enero, California se sumó a otros 45 estados y al Distrito de Columbia con leyes que permiten a una persona tomar decisiones en nombre de un paciente, incluso si no estaba autorizada por el paciente antes de que ocurriera la situación médica.
La lista incluye cónyuges o parejas de hecho, hermanos, hijos y nietos adultos, padres y un pariente adulto o amigo íntimo; y en muchos casos, a las personas que llevaron al paciente para que lo atendieran en un primer momento.
“Los hospitales y las HMO podían usurpar los derechos de las familias y tomar decisiones médicas críticas en virtud de la ley vigente en aquel momento, incluidas las decisiones de desconectar al paciente”, explicó a KHN Dorio, especialista en geriatría de Santa Clarita y miembro de la organización no partidista California Senior Legislature. “Sabíamos que necesitábamos una ley como la que tienen la mayoría de los otros estados”.
Según datos analizados por investigadores de Penn Medicine, solo un tercio de los adultos estadounidenses tiene o bien instrucciones previas, que detallan lo que quieren sobre su atención médica, o bien un poder médico, que autoriza a otra persona a tomar esas decisiones.
Según sus partidarios, la finalidad detrás de la ley de parentesco es darles facultad a los representantes para que aboguen por los pacientes en lugar de permitir que un hospital tome las decisiones médicas, que pueden estar influenciadas por el costo, las camas disponibles o las presiones de los seguros.
“Esta ley libera de presión a los hospitales, a los que se pide que presten asistencia, salven vidas, se ocupen de Medicare, de los seguros… de muchas cosas a la vez”, afirmó Michele Mann, abogada de Valencia, California, especializada en planificación patrimonial, incluidas las directivas avanzadas.
Los derechos médicos de los pacientes han evolucionado a lo largo de los años, pero es un misterio por qué el estado ha tardado tanto tiempo en aprobar una ley de parentesco. Cuando la California Senior Legislature, que patrocina y promueve leyes destinadas a ayudar a la población de edad avanzada, pidió ayuda a la Oficina del Asesor Legislativo del Estado con el proyecto de ley algunos abogados se sorprendieron de ya no hubiera una ley vigente, dijo Dorio.
Los pacientes que no disponen de un documento de directivas avanzadas o de un poder notarial pueden designar a un sustituto, aunque solo sea declarándolo verbalmente en el hospital, pero, obviamente, es necesario que el paciente esté consciente.
Si un paciente llega a un hospital o centro médico incapacitado o lo está posteriormente, los proveedores deben hacer un esfuerzo de buena fe para encontrar a una persona autorizada a tomar decisiones médicas, según una ley de California en vigor desde 2005.
Los pasos incluyen revisar las pertenencias del paciente y ponerse en contacto con cualquier persona que el hospital “crea razonablemente que tiene autoridad” para tomar decisiones a través de directivas o de un poder notarial. El hospital debe demostrar que se ha puesto en contacto con el secretario de estado para preguntar si el paciente tenía instrucciones anticipadas.
Con la nueva ley vigente, los proveedores de atención médica deben comprobar si el paciente tiene directivas avanzadas o un poder notarial. Pero una vez que los funcionarios han determinado que no existe ninguno, pueden recurrir a la lista de parientes más próximos, todos los cuales están legalmente autorizados a hablar en nombre del paciente.
“Es innovador”, afirmó Mann, que toma decisiones por su hermana, que tiene esclerosis múltiple y vive en un centro de cuidados de largo plazo. “Con la lista de parientes cercanos, a menudo la persona que trae al paciente es un familiar o un amigo íntimo que conoce claramente los deseos del paciente. En esos casos, se acabó la búsqueda del hospital: hay un representante legalmente autorizado”.
El proyecto de ley AB 2338, presentado por el asambleísta Mike Gipson, agregó una sección al código de sucesiones, y se asemeja a la forma en que la mayoría de los estados maneja la división de los bienes de una persona después de su muerte.
En California, cuando una persona muere sin dejar testamento, sus bienes y propiedades se distribuyen siguiendo un orden de prioridad fijo y descendiente: primero el cónyuge, después los hijos, los padres, los hermanos, etc. Ahora, las decisiones médicas de una persona se decidirán de la misma manera, pero no necesariamente en el mismo orden.
California otorga a los hospitales y a los proveedores médicos la discreción de decidir qué familiar o amigo íntimo puede tomar decisiones médicas, una disposición introducida en el proyecto de ley después de que la influyente Asociación de Hospitales de California y otros grupos médicos se opusieran a una jerarquía pre establecida.
Algunos expertos se preguntan hasta qué punto será eficaz la nueva ley, ya que los hospitales conservan la facultad de elegir al representante del paciente, sobre todo si hay opiniones encontradas entre los miembros de la familia.
“Aunque no tengo motivos para creer que vayan a abusar del poder, los hospitales pueden decidir quién sería una buena persona para tomar decisiones”, dijo Alexander Capron, experto en derecho médico y ética, y profesor emérito de la Universidad del Sur de California.
Lois Richardson, vicepresidenta y asesora jurídica de la asociación de hospitales, dijo que un orden estricto de sustitutos a menudo no refleja lo que un paciente desearía. “La preocupación siempre ha sido que, en muchos casos, una jerarquía estatutaria estricta no refleja las relaciones familiares reales”, agregó.
El cabildeo de los hospitales abandonó su oposición después de que Gipson accediera a dar flexibilidad al sector, y la medida se aprobó en la legislatura prácticamente sin oposición.
Lo ideal sería que las personas dispusieran de un documento de directivas avanzadas para garantizar el cumplimiento de sus deseos, según Gipson. Pero para las personas mayores, las que viven solas y cualquiera que no tenga este documento, la ley abre el abanico de personas que pueden actuar en su nombre, incluido un amigo íntimo que bien podría ser de familia.
“Al menos así, tienes a alguien que sabe lo que quieres tomando esas decisiones”, indicó Gipson, “en lugar de dejarlo en manos de un hospital”.
Esta historia fue producida por KHN, que publica California Healthline, un servicio editorialmente independiente de la California Health Care Foundation.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
USE OUR CONTENT
This story can be republished for free (details).
2 years 5 months ago
Noticias En Español, States, California Legislature, End Of Life, Hospitals, Legislation
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
MCh Paediatric Surgery: Admissions, medical colleges, fees, eligibility criteria details
MCh Paediatric
Surgery or Master of Chirurgiae in Paediatric Surgery also known as MCh in Paediatric
Surgery is a super specialty level course for doctors in India that they do after completion of their postgraduate medical degree course. The duration
of this super specialty course is 3 years, and it focuses on the study of
MCh Paediatric
Surgery or Master of Chirurgiae in Paediatric Surgery also known as MCh in Paediatric
Surgery is a super specialty level course for doctors in India that they do after completion of their postgraduate medical degree course. The duration
of this super specialty course is 3 years, and it focuses on the study of
various concepts involving the surgical care of fetuses, infants, children,
adolescents, and young adults.
The course is a full-time course pursued at various recognized medical
colleges across the country. Some of the top medical colleges offering this
course include All India Institute of Medical Sciences, New Delhi, Maulana Azad Medical College, New Delhi, G.B. Pant Institute of PG medical education and research, New
Delhi, and more.
Admission to this course is done through the NEET-SS Entrance exam
conducted by the National Board of Examinations, followed by counseling based
on the scores of the exam that is conducted by DGHS/MCC/State Authorities.
The fee for pursuing MCh (Paediatric Surgery)
varies from college to college and may range from Rs.1,000
to Rs 6,04,000/- in government colleges and from Rs.1,10,000 to Rs.29,00,000 per year for private colleges.
After completion of their respective course, doctors can either join the
job market or can pursue certificate courses and Fellowship programs recognized by
NMC and NBE. Candidates can take reputed jobs at positions as Senior residents,
Consultants, etc. with an approximate salary range of Rs 9 lakhs to Rs. 23
lakhs per annum.
What is MCh in Paediatric Surgery?
Master
of Chirurgiae in Paediatric Surgery, also known as MCh (Paediatric Surgery) or MCh in (Paediatric Surgery) is a three-year super specialty
programme that candidates can pursue after completing a postgraduate degree.
Pediatric Surgery is the branch of medical
science dealing with the study of those who specialize in treating children. They're
trained to do surgery of infants, children, and young adults.
National
Medical Commission (NMC), the apex medical regulator, has released a Guidelines
for Competency-Based Postgraduate Training Programme for MCh in Paediatric
Surgery.
The Competency-Based
Postgraduate Training Programme governs the education and training of MChs in Paediatric
Surgery.
The postgraduate students must gain ample knowledge and
experience in the diagnosis, and treatment of patients with acute, serious, and
life-threatening medical and surgical diseases.
PG education intends to create specialists who can
contribute to high-quality health care and advances in science through research
and training.
The required training done by a postgraduate specialist in
the field of Paediatric
Surgery would help the specialist to recognize the health needs of
the community. The student should be competent to handle medical problems
effectively and should be aware of the recent advances in their specialty.
The candidate is also expected to know the principles of
research methodology and modes of the consulting library. The candidate should regularly
attend conferences, workshops, and CMEs to upgrade her/ his knowledge.
Course Highlights
Here are some of the course highlights of MCh in Paediatric Surgery
Name of Course
MCh in Paediatric Surgery
Level
Doctorate
Duration of Course
Three years
Course Mode
Full Time
Minimum Academic
Requirement
Candidates must have a postgraduate medical Degree in MS/DNB General Surgery from any college/university recognized by the Medical Council of India (Now NMC)/NBE, this feeder qualification mentioned here is as of 2022. For any further changes to the prerequisite requirement please refer to the DNB website.
Admission Process /
Entrance Process / Entrance Modalities
Entrance Exam (NEET-SS)
INI CET for various
AIIMS, PGIMER Chandigarh, JIPMER Puducherry, NIMHANS Bengaluru
Counseling by DGHS/MCC/State
Authorities
Course Fees
In government
colleges from Rs.1,000 to
Rs 6,04,000 per year
In Private
colleges from Rs.1,10,000
to Rs.29,00,000 per year
Average Salary
Rs 9 lakhs to Rs. 23
lakhs per annum
Eligibility Criteria
The eligibility criteria for MCh in Paediatric Surgery are defined as the set of rules or
minimum prerequisites that aspirants must meet to be eligible for
admission, which includes:
Name of Super Specialty course
Course Type
Prior Eligibility Requirement
Pediatric Surgery
MCh
MS/DNB (General Surgery)
Note:
·
The feeder qualification
for MCh Pediatric Surgery is defined by the NBE and is subject to changes by
the NBE.
·
The feeder qualification
mentioned here is as of 2022.
·
For any changes, please
refer to the NBE website.
- The prior entry qualifications
shall be strictly by Post Graduate Medical Education
Regulations, 2000, and its amendments notified by the NMC and any
clarification issued from NMC in this regard. - The candidate must have
obtained permanent registration with any State Medical Council to be
eligible for admission. - The medical college's
recognition cut-off dates for the Postgraduate Degree courses shall be as
prescribed by the medical council of India (now NMC).
Admission Process
The admission process contains a few steps to
be followed in order by the candidates for admission to MCh in Paediatric
Surgery. Candidates can view the complete
admission process for MCh in Paediatric Surgery mentioned below:
- The NEET-SS or
National Eligibility Entrance Test for Super specialty courses is a national-level
master's level examination conducted by the NBE for admission to DM/MCh/DrNB Courses. - Qualifying Criteria-Candidates placed at the
50th percentile or above shall be declared as qualified in the NEET-SS in their
respective specialty. - The following Medical institutions are not
covered under centralized admissions for DM/MCh courses through NEET-SS:
1.
AIIMS, New Delhi, and other AIIMS
2.
PGIMER, Chandigarh
3.
JIPMER, Puducherry
4.
NIMHANS, Bengaluru
- Candidates from all eligible feeder specialty
subjects shall be required to appear in the question paper of the respective group if they are willing to opt for a super specialty course in any of the super
specialty courses covered in that group. - A candidate can opt for appearing in the
question papers of as many groups for which his/her Postgraduate specialty
qualification is an eligible feeder qualification. - By appearing in the question paper of a group
and on qualifying for the examination, a candidate shall be eligible to exercise
his/her choices in the counseling only for those super specialty subjects
covered in the said group for which his/ her broad specialty is an eligible feeder
qualification.
Fees Structure
The fee structure for MCh in Paediatric Surgery varies from college to college. The fee is generally
less for Government Institutes and more for private institutes. The average fee structure for MCh in Paediatric Surgery is around may range from Rs.1,000 to Rs 6,04,000 in government colleges and from for private
colleges Rs.1,10,000 to Rs.29,00,000 per year.
Colleges offering MCh in Paediatric Surgery
Various medical colleges across India offer courses for
pursuing MCh in (Paediatric
Surgery).
As per National Medical Commission (NMC) website, the following medical
colleges are offering MCh in (Paediatric Surgery) courses
for the academic year 2022-23.
Sl.No.
Course Name
State
Name and Address of
Medical College / Medical Institution
Annual Intake (Seats)
1
M.Ch - Paediatric Surgery
Andhra Pradesh
Kurnool Medical College, Kurnool
2
2
M.Ch - Paediatric Surgery
Andhra Pradesh
Narayana Medical College, Nellore
2
3
M.Ch - Paediatric Surgery
Andhra Pradesh
Andhra Medical College, Visakhapatnam
1
4
M.Ch - Paediatric Surgery
Andhra Pradesh
Guntur Medical College, Guntur
2
5
M.Ch - Paediatric Surgery
Assam
Assam Medial College, Dibrugarh
2
6
M.Ch - Paediatric Surgery
Assam
Gauhati Medical College, Guwahati
2
7
M.Ch - Paediatric Surgery
Bihar
Indira Gandhi Institute of Medical
Sciences, Sheikhpura, Patna
2
8
M.Ch - Paediatric Surgery
Chandigarh
Postgraduate Institute of Medical Education &
Research, Chandigarh
8
9
M.Ch - Paediatric Surgery
Chattisgarh
All India Institute of Medical Sciences, Raipur
2
10
M.Ch - Paediatric Surgery
Chattisgarh
Pt. J N M Medical College, Raipur
3
11
M.Ch - Paediatric Surgery
Delhi
G.B. Pant Institute of Postgraduate Medical
Education and Research, New Delhi
4
12
M.Ch - Paediatric Surgery
Delhi
Atal Bihari Vajpayee Institute of Medical
Sciences and Dr. RML Hospital, New Delhi
5
13
M.Ch - Paediatric Surgery
Delhi
Maulana Azad Medical College, New Delhi
4
14
M.Ch - Paediatric Surgery
Delhi
All India Institute of Medical Sciences, New
Delhi
9
15
M.Ch - Paediatric Surgery
Delhi
Chacha Nehru Bal Chikitsalaya
2
16
M.Ch - Paediatric Surgery
Delhi
Vardhman Mahavir Medical College & Safdarjung
Hospital, Delhi
4
17
M.Ch - Paediatric Surgery
Delhi
Lady Hardinge Medical College, New Delhi
4
18
M.Ch - Paediatric Surgery
Gujarat
B J Medical College, Ahmedabad
3
19
M.Ch - Paediatric Surgery
Gujarat
Smt. N.H.L.Municipal Medical College, Ahmedabad
2
20
M.Ch - Paediatric Surgery
Haryana
Pt. B D Sharma Postgraduate Institute of Medical
Sciences, Rohtak (Haryana)
2
21
M.Ch - Paediatric Surgery
Jammu & Kashmir
Sher-I-Kashmir Instt. Of Medical Sciences,
Srinagar
2
22
M.Ch - Paediatric Surgery
Jharkhand
Rajendra Institute of Medical Sciences, Ranchi
3
23
M.Ch - Paediatric Surgery
Karnataka
Rajarajeswari Medical College & Hospital,
Bangalore
1
24
M.Ch - Paediatric Surgery
Karnataka
Kasturba Medical College, Manipal
1
25
M.Ch - Paediatric Surgery
Karnataka
St. Johns Medical College, Bangalore
2
26
M.Ch - Paediatric Surgery
Karnataka
Bangalore Medical College and Research Institute,
Bangalore
3
27
M.Ch - Paediatric Surgery
Karnataka
JJM Medical College, Davangere
1
28
M.Ch - Paediatric Surgery
Karnataka
Indira Gandhi Institute of Child Health,
Bangalore
8
29
M.Ch - Paediatric Surgery
Karnataka
M S Ramaiah Medical College, Bangalore
3
30
M.Ch - Paediatric Surgery
Karnataka
Jawaharlal Nehru Medical College, Belgaum
1
31
M.Ch - Paediatric Surgery
Kerala
Government Medical College, Kozhikode, Calicut
4
32
M.Ch - Paediatric Surgery
Kerala
Medical College, Thiruvananthapuram
6
33
M.Ch - Paediatric Surgery
Kerala
Government Medical College, Kottayam
1
34
M.Ch - Paediatric Surgery
Kerala
Amrita School of Medicine, Elamkara, Kochi
3
35
M.Ch - Paediatric Surgery
Madhya Pradesh
Gandhi Medical College, Bhopal
1
36
M.Ch - Paediatric Surgery
Madhya Pradesh
All India Institute of Medical Sciences, Bhopal
2
37
M.Ch - Paediatric Surgery
Madhya Pradesh
Index Medical College Hospital & Research
Centre, Indore
2
38
M.Ch - Paediatric Surgery
Madhya Pradesh
M G M Medical College, Indore
2
39
M.Ch - Paediatric Surgery
Madhya Pradesh
Sri Aurobindo Medical College and Post Graduate
Institute, Indore
1
40
M.Ch - Paediatric Surgery
Maharashtra
Grant Medical College, Mumbai
1
41
M.Ch - Paediatric Surgery
Maharashtra
N. K. P. Salve Instt. of Medical Sciences and
Research Centre and Lata Mangeshkar Hospital, Nagpur
1
42
M.Ch - Paediatric Surgery
Maharashtra
Lokmanya Tilak Municipal Medical College, Sion,
Mumbai
4
43
M.Ch - Paediatric Surgery
Maharashtra
Topiwala National Medical College, Mumbai
2
44
M.Ch - Paediatric Surgery
Maharashtra
Seth GS Medical College, and KEM Hospital, Mumbai
8
45
M.Ch - Paediatric Surgery
Maharashtra
Armed Forces Medical College, Pune
46
M.Ch - Paediatric Surgery
Maharashtra
Dr. D Y Patil Medical College, Hospital and
Research Centre, Pimpri, Pune
2
47
M.Ch - Paediatric Surgery
Maharashtra
B. J. Govt. Medical College, Pune
2
48
M.Ch - Paediatric Surgery
Maharashtra
Government Medical College, Nagpur
2
49
M.Ch - Paediatric Surgery
Maharashtra
Padmashree Dr. D.Y.Patil Medical College, Navi
Mumbai
1
50
M.Ch - Paediatric Surgery
Orissa
All India Institute of Medical Sciences,
Bhubaneswar
4
51
M.Ch - Paediatric Surgery
Orissa
SCB Medical College, Cuttack
6
52
M.Ch - Paediatric Surgery
Pondicherry
Jawaharlal Institute of Postgraduate Medical
Education & Research, Puducherry
2
53
M.Ch - Paediatric Surgery
Punjab
Christian Medical College, Ludhiana
1
54
M.Ch - Paediatric Surgery
Rajasthan
SMS Medical College, Jaipur
10
55
M.Ch - Paediatric Surgery
Rajasthan
All India Institute of Medical Sciences, Jodhpur
2
56
M.Ch - Paediatric Surgery
Tamil Nadu
Christian Medical College, Vellore
4
57
M.Ch - Paediatric Surgery
Tamil Nadu
Coimbatore Medical College, Coimbatore
4
58
M.Ch - Paediatric Surgery
Tamil Nadu
Sri Ramachandra Medical College & Research
Institute, Chennai
1
59
M.Ch - Paediatric Surgery
Tamil Nadu
Madras Medical College, Chennai
9
60
M.Ch - Paediatric Surgery
Tamil Nadu
Madurai Medical College, Madurai
2
61
M.Ch - Paediatric Surgery
Tamil Nadu
Govt. Mohan Kumaramangalam Medical College,
Salem- 30
2
62
M.Ch - Paediatric Surgery
Tamil Nadu
Stanley Medical College, Chennai
2
63
M.Ch - Paediatric Surgery
Tamil Nadu
Tirunelveli Medical College,Tirunelveli
2
64
M.Ch - Paediatric Surgery
Tamil Nadu
SRM Medical College Hospital & Research
Centre, Chengalpattu
1
65
M.Ch - Paediatric Surgery
Tamil Nadu
PSG Institute of Medical Sciences, Coimbatore
1
66
M.Ch - Paediatric Surgery
Tamil Nadu
Thanjavur Medical College,Thanjavur
1
67
M.Ch - Paediatric Surgery
Telangana
Gandhi Medical College, Secunderabad
1
68
M.Ch - Paediatric Surgery
Telangana
Osmania Medical College, Hyderabad
8
69
M.Ch - Paediatric Surgery
Uttarakhand
All India Institute of Medical Sciences,
Rishikesh
14
70
M.Ch - Paediatric Surgery
Uttar Pradesh
King George Medical University, Lucknow
2
71
M.Ch - Paediatric Surgery
Uttar Pradesh
Institute of Medical Sciences, BHU, Varanasi
4
72
M.Ch - Paediatric Surgery
Uttar Pradesh
Sanjay Gandhi Postgraduate Institute of Medical
Sciences, Lucknow
2
73
M.Ch - Paediatric Surgery
Uttar Pradesh
Super Speciality Paediatric Hospital & Post
Graduate Teaching Institute, Noida
1
74
M.Ch - Paediatric Surgery
West Bengal
Nilratan Sircar Medical College, Kolkata
6
75
M.Ch - Paediatric Surgery
West Bengal
Institute of Postgraduate Medical Education &
Research, Kolkata
5
76
M.Ch - Paediatric Surgery
West Bengal
Govt. Medical College, Kolkata
2
SyllabusAn MCh in Paediatric Surgery
is a three years specialization course that provides training in the stream of
Surgery.
The course
content for MCh in Paediatric Surgery is
given in the Competency-Based Postgraduate Training Programme released
by National Medical Commission, which can be assessed through the link
mentioned below:
NMC Guidelines For Competency-Based Training Programme For MCh Pediatric Surgery
A. Cognitive domain
The following is a broad outline of the
syllabus:
Basic sciences
as applied to Pediatric Surgery
- Medical genetics and gene therapy.
- Antenatal diagnosis and fetal intervention
- Developmental and transitional physiology of the
respiratory, cardiovascular, and renal systems - Neonatal physiology and assessment of the surgical
neonate. - Neonatal sepsis
- Nutrition – enteral, parenteral
- Vascular access
- Principles of imaging (radiodiagnosis, nuclear)
in Pediatric practice - Pharmacology and use of common drugs,
antibiotics, and policy - Pediatric analgesia and anesthesia, critical
care, mechanical ventilation - General principles of Endoscopy and Minimal
Access Surgery – fetoscopy, genitourinary endoscopy, trachea-bronchoscopy,
laparoscopy, thoracoscopy, robotic surgery - Biomedical ethics and legal issues in Pediatric
surgical practice. - The organization of a Pediatric Surgical unit
- HIV/AIDS in children
- National health policy programs pertinent to
Pediatric practice - Telemedicine and telesurgery - principles,
practice, and limitations
Trauma
- Birth trauma
- Pediatric trauma – general principles.
- Thoracic, abdominal, genitourinary, and central
nervous system trauma - Soft tissue and envenomation injuries
- Musculoskeletal and vascular trauma
- Burns
- Child abuse.
Pediatric
Oncology
- General principles of oncology, radiotherapy, and
chemotherapy - Wilms' tumor
- Neuroblastoma
- Liver tumors
- Rhabdomyosarcoma
- Germ cell tumors
- Other tumors of childhood (outline)-Leukemias,
Lymphomas, Bone tumors, CNS - tumors.
- Retinoblastoma
Transplantation
- General principles
- Kidney and liver transplantation
- Outline of other solid organ and bone marrow
transplantation.
Head and Neck
Disorders
- Craniofacial anomalies
- Cleft lip and palate
- Disorders of the upper airway and oral cavity.
- Salivary glands
- Disorders of lymph nodes.
- Thyroid and parathyroid gland
- Cysts and sinuses of the neck
- Torticollis
Thoracic
Disorders
- Congenital chest wall deformities.
- Disorders of the breast.
- Diaphragmatic hernia and eventration
- Mediastinal mass lesions.
- Endoscopy of the upper aerodigestive tract.
- Congenital tracheal and Bronchopulmonary/
foregut malformations - Infective pleuro-pulmonary condition.
- Congenital esophageal anomalies
- Esophageal motility disorders , achalasia cardia, gastro-oesophagal reflux
- Oesophageal rupture, injury, stricture,
perforation. - Esophageal replacement.
Abdominal
Disorders
- Umbilical disorders and abdominal wall defects.
- Inguinal hernias and hydroceles
- Testicular maldescent, torsion
- Hypertrophic pyloric stenosis.
- Duodenal atresia, annular pancreas.
- Jejunoileal atresia and stenosis
- Meconium ileus
- Meckel's diverticulum
- Intussusception.
- Disorder of midgut rotation.
- Short bowel syndrome
- Gastrointestinal endoscopy and laparoscopy.
- Gastrointestinal bleeding
- Gastrointestinal duplications.
- Mesenteric and omental cysts
- Ascites
- The polypoid disease of the GIT
- Necrotising enterocolitis.
- Intestinal stomas
- Primary peritonitis.
- Inflammatory bowel disease in children.
- Colonic atresia and functional obstruction.
- Appendicitis
- Hirschsprung disease, neuromuscular disorders of
intestines - Anorectal malformations.
- Congenital short colon /pouch colon
- Colonic and rectal tumors
- Neonatal/Infantile obstructive cholangiopathy
- Congenital biliary dilatation.
- Infective and inflammatory hepatobiliary
disorders - Benign liver tumors
- Portal hypertension
- Disorders of the pancreas
- Splenectomy and post-splenectomy sepsis.
- Adrenal gland.
Genitourinary
and related disorders
- Renal agenesis, dysplasia, cystic disease,
ectopia - Pelvic ureteral junction obstruction
- Vesicoureteric reflux
- Infective and inflammatory renal disorder.
- Pediatric urolithiasis
- Congenital ureteric anomalies.
- Prune belly syndrome
- Urinary diversion and undiversion, bladder
augmentation - Disorders of bladder function.
- Structural bladder disorders
- Exstrophy – epispadias complex
- Hypospadias.
- Anomalies of the external genitalia
- Disorders of Sex Differentiation
- Abnormalities of the female genital tract.
Miscellaneous
Pediatric Surgical Disorders
- Spina bifida
- Hydrocephalus
- Congenital heart disease
- Congenital orthopedic deformities
- Amputation, bone, and joint infections
- Conjoined twins
- Hemangiomas & vascular malformations.
Career Options
After completing an MCh in Paediatric Surgery, candidates will get employment opportunities
in Government as well as in the Private sector.
In the
Government sector, candidates have various options to choose from which include
Registrar, Senior Resident, Demonstrator, Tutor, etc.
While in the Private sector, the options include Resident Doctor,
Consultant, Visiting Consultant (Paediatric Surgeon), Junior
Consultant, Senior Consultant (Paediatric Surgeon), Assistant Professor,
Associate Professor (Paediatric Surgeon).
Courses After MCh in Paediatric Surgery Course
MCh in Paediatric
Surgery is a specialization
course that can be pursued after finishing a Postgraduate medical course.
After pursuing specialization in MCh in Paediatric
Surgery, a candidate could also
pursue certificate courses and Fellowship programs recognized by NMC and NBE,
where MCh in Paediatric
Surgery is a feeder
qualification.
These include:
- Post-Doctoral
Fellowship in Pediatric Gastrointestinal Surgery - Fellowship
Programme In Pediatric Minimally Invasive Surgery
Frequently Asked Questions (FAQs) –MCh in Paediatric Surgery Course
·
Question: What is the full
form of an MCh?
Answer: The full form of an MCh is Master of
Chirurgiae.
·
Question: What is an MCh in Paediatric
Surgery?
Answer: MCh Paediatric Surgery
or Master of
Chirurgiae in Paediatric Surgery also known as MCh in Paediatric
Surgery is a super specialty level
course for doctors in India that they do after completion of their postgraduate
medical degree course.
·
Question: What is the
duration of an MCh in Paediatric Surgery?
Answer: MCh in Paediatric Surgery is a super
specialty programme of three years.
·
Question: What
is the eligibility of an MCh in Paediatric
Surgery?
Answer: Candidates must have a postgraduate medical Degree in MS/DNB General Surgery from any college/university recognized by the Medical Council of India (Now NMC)/NBE., this feeder qualification mentioned here is as of 2022. For any further changes to the prerequisite requirement please refer to the DNB website.
- Question: What
is the scope of an MCh in Paediatric
Surgery?
Answer:
MCh in Paediatric Surgery offers
candidates various employment opportunities and career prospects.
- Question: What
is the average salary for an MCh in Paediatric Surgery
candidate?
Answer:
The MCh in Paediatric Surgery candidate's average salary is between Rs. 9 lakhs to Rs. 23 lakhs per annum depending on the experience.
•Question: Can you teach after
completing an MCh Course?
Answer: Yes, the candidate
can teach in a medical college/hospital after completing an MCh course.
- What is the most common Pediatric Surgery?
The most common
Pediatric Surgery is Hernia Surgery.
2 years 5 months ago
News,Health news,NMC News,Medical Education,Medical Colleges News,Medical Courses News,Medical Universities News,Medical Admission News,Latest Medical Education News,Medical Courses
Health Minister says hospitalization for cholera “remains well controlled and low”
The Minister of Public Health, Daniel Rivera, called on Thursday to continue cholera vaccination, improve hygiene conditions, and avoid consuming food from places of sale that appear insufficient to prevent the spread of this bacterium, which has so far affected 71 people in the Dominican Republic.
The official assured that the ministry’s and the community’s joint interventions, vaccination, house-to-house visits, and the epidemiological fence will be maintained.
“Thank God, many of these cases that appear are mild, which is why hospitalization remains well controlled and low,” he said, adding that this does not mean that the disease’s overall situation has been resolved. “We’re not going to say it’s under control; that’s impossible,” the minister declared. Rivera stated that “it depends on people washing their hands before and after going to the bathroom, and before each meal, cooking food well because many of the people we have detected with cholera consumed poorly cooked food or in inadequate outlets in order to achieve control levels”.
“We’re doing well, the population is cooperating with vaccination,” he said. The goal is to have 24 thousand doses applied by the end of this week. The official reiterated that it is “an individual decision” and praised those who “take care of cleanliness and hygiene in their homes.”
2 years 5 months ago
Health, Local
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Tears sampled by ocular swab can help detect the COVID-19 virus
Brazil: A recent study in the Journal of Clinical Medicine has suggested an alternative method to nasopharyngeal swabbing, which is unpleasant for detecting the coronavirus that causes COVID-19. The study found that tears collected by swabbing can detect the coronavirus.
A swab is an absorbent cotton pad on a flexible rod used to clean wounds, apply medication and take specimens.
Brazil: A recent study in the Journal of Clinical Medicine has suggested an alternative method to nasopharyngeal swabbing, which is unpleasant for detecting the coronavirus that causes COVID-19. The study found that tears collected by swabbing can detect the coronavirus.
A swab is an absorbent cotton pad on a flexible rod used to clean wounds, apply medication and take specimens.
The researchers analyzed samples from patients diagnosed with the disease by conventional methods. They were admitted to the Hospital for Rehabilitation of Craniofacial Anomalies (HRAC), run by the Bauru Dental School (FOB-USP). SARS-CoV-2 was detected in 18.2% of the samples, suggesting this method could be an alternative to nasopharyngeal swabbing, which is unpleasant, and that health workers should take steps to protect themselves against infection via patients’ tears, although the risk is admittedly low.
Moreover, a combination of two factors-more, comorbidities and a higher mortality rate-among patients whose tear samples tested positive, suggests that this virus detection method could be a prognosis predictor.
“Initially, we set out to develop a diagnostic test based on an easier collection of material without causing patient discomfort. Nasal and nasopharyngeal swabbing is not only unpleasant but also often performed incorrectly. For people with a nasal septum deviation, it can be a problem. We believed that tear sampling would be easy to execute and more tolerable. We succeeded in showing this to be feasible. Among the limitations of the study was not knowing whether the amount of liquid collected for the test influences its result,” Luiz Fernando Manzoni Lourençone, professor of medicine at HRAC and last author of the article, told Agência FAPESP.
The findings suggest that the probability of detecting the virus in tears is greater when the patient has a high viral load, which can lead to viremia in body fluids, he added.
FAPESP supported the study via a scientific initiation scholarship awarded to Luís Expedito Sabage, an undergraduate student supervised by Lourençone.
Technique
The study cohort comprised 61 hospitalized patients, with 28 testing negative and 33 positive for COVID-19 by RT-qPCR via nasopharyngeal swab. Tears were analyzed from all 33 positives and from 14 of the 28 negatives. The tears were collected in the first half of 2021 when the main viral variants circulating in São Paulo state were gamma and delta.
In addition to collection by conjunctival swab, the scientists also used a technique known as the Schirmer strip test, in which a strip of filter paper is placed for five minutes inside the lower eyelid (normally used to determine whether the eye produces enough tears). The samples were analyzed between July and November 2021.
SARS-CoV-2 was detected in 18.2% of the samples collected by conjunctival swab and 12.1% of those collected by Schirmer strip. As expected, none of the patients who tested negative for the virus via nasopharyngeal swab had tears that tested positive.
The Charlson Comorbidity Index (CCI) was used to predict risk of death within a year of hospitalization for patients with 20 specific conditions. Patients with SARS-CoV-2 particles in tear samples had an almost sevenfold chance of dying compared to patients with a negative result. Those patients also had other factors that could contribute to death, such as a poor ten-year survival rate based on CCI.
Most of the patients had low tear production and eye discomfort regardless of their COVID-19 diagnosis, possibly pointing to the need for artificial tear use during hospitalization, according to the authors.
The study also included demographic, clinical and ocular symptom data. The main diagnostic test used was real-time quantitative PCR (polymerase chain reaction), which can detect a single copy of viral RNA in a sample and is considered the gold standard for diagnosing COVID-19 by clinical analysis laboratories worldwide.
Innovating in comparison with previous research, in this study, viral RNA positivity was determined much more precisely by analyzing the nucleocapsid (N), envelope (E) and RNA-dependent RNA polymerase (RdRp).
An article published in July 2021 in Experimental Biology and Medicine by a group of researchers at the State University of Campinas’s School of Medical Sciences (FCM-UNICAMP), also in São Paulo state, reported the results of a study conducted at its teaching hospital where SARS-CoV-2 was detected in tear samples from 8.43% of the 83 patients enrolled in the study.
“When we started, in early 2021, we lacked the technology to cross-reference certain types of data as a route out of basic science and into clinical practice. Since then, Sabage has worked as a research intern at Stanford University’s Byers Eye Institute [in the United States], a leading centre for advanced studies of ocular fluids. Their technology enabled us to detect several correlations and confirm the presence of SARS-CoV-2 in our tear samples. Partnering with another team brought results for our campus and opened up a new research line,” Lourençone said.
Reference:
Sabage, L.E.; Sun, Y.J.; Wolf, J.; Sabage, J.; Mazzo, A.; Santos, C.F.; Mahajan, V.B.; Manzoni Lourençone, L.F. Conjunctival Swabs Reveal Higher Detection Rate Compared to Schirmer Strips for SARS-CoV-2 RNA Detection in Tears of Hospitalized COVID-19 Patients. J. Clin. Med. 2022, 11, 6929. https://doi.org/10.3390/jcm11236929
2 years 5 months ago
ENT,Medicine,ENT News,Medicine News,Top Medical News
PAHO provides guidance to countries as chikungunya cases increase | Loop Caribbean News - Loop News Caribbean
- PAHO provides guidance to countries as chikungunya cases increase | Loop Caribbean News Loop News Caribbean
- PAHO provides guidance to countries in response to increased chikungunya cases Jamaica Gleaner
- View Full Coverage on Google News
2 years 5 months ago
The Kids Are Not OK
The Host
Julie Rovner
KHN
Julie Rovner is chief Washington correspondent and host of KHN’s weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
Teen girls “are experiencing record high levels of violence, sadness, and suicide risk,” according to a new survey from the Centers for Disease Control and Prevention. In 2021, according to the survey, nearly 3 in 5 U.S. teen girls reported feeling “persistently sad or hopeless.”
Meanwhile, a conservative judge in Texas has delayed his ruling in a case that could ban a key drug used in medication abortion. A group of anti-abortion doctors is suing to challenge the FDA’s approval decades ago of the abortion pill mifepristone.
This week’s panelists are Julie Rovner of KHN, Alice Miranda Ollstein of Politico, Joanne Kenen of the Johns Hopkins Bloomberg School of Public Health and Politico, and Sandhya Raman of CQ Roll Call.
Panelists
Alice Miranda Ollstein
Politico
Joanne Kenen
Johns Hopkins Bloomberg School of Public Health and Politico
Sandhya Raman
CQ Roll Call
Among the takeaways from this week’s episode:
- American teenagers reported record rates of sadness in 2021, with especially high levels of depression in girls and teens identifying as LGBTQ+, according to a startling CDC report. Sexual violence, mass shootings, cyberbullying, and climate change are among the intensifying problems plaguing young people.
- New polling shows more Americans are dissatisfied with abortion policy than ever before, as a U.S. district court judge in Texas makes a last call for arguments on the fate of mifepristone. The case is undermining confidence in continued access to the drug, and many providers are discussing using only misoprostol for medication abortions. Misoprostol is used with mifepristone in the current two-drug regimen but is safe and effective, though slightly less so, when used on its own.
- There are big holes in federal health privacy protections, and some companies that provide health care, like mental health services, exploit those loopholes to sell personal, identifying information about their customers. And this week, Republican Gov. Glenn Youngkin of Virginia blocked a state law that would have banned search warrants for data collected by menstrual tracking apps.
- California plans to manufacture insulin, directly taking on high prices for the diabetes drug. While other states have expressed interest in following suit, it will likely be up to wealthy, populous California to prove the concept.
Plus, for “extra credit” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: NPR’s “Is the Deadly Fungi Pandemic in ‘The Last of Us’ Actually Possible?” by Michaeleen Doucleff
Alice Ollstein: The New York Times’ “Childbirth Is Deadlier for Black Families Even When They’re Rich, Expansive Study Finds,” by Claire Cain Miller, Sarah Kliff, and Larry Buchanan; interactive produced by Larry Buchanan and Shannon Lin
Joanne Kenen: NPR’s “In Tennessee, a Medicaid Mix-Up Could Land You on a ‘Most Wanted’ List,” by Blake Farmer
Sandhya Raman: Bloomberg Businessweek’s “Zantac’s Maker Kept Quiet About Cancer Risks for 40 Years,” by Anna Edney, Susan Berfield, and Jef Feeley
Also mentioned in this week’s podcast:
- The CDC’s “U.S. Teen Girls Experiencing Increased Sadness and Violence”
- The Fun Violence Archive’s “Mass Shootings in 2023”
- The Washington Post’s “Now for Sale: Data on Your Mental Health,” by Drew Harwell
Click to open the transcript
Transcript: The Kids Are Not OK
KHN’s ‘What the Health?’Episode Title: The Kids Are Not OKEpisode Number: 285Published: Feb. 16, 2023
Julie Rovner: Hello and welcome back to KHN’s “What the Health?” I’m Julie Rovner, chief Washington correspondent at Kaiser Health News. And I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, Feb. 16, at 10 a.m. As always, news happens fast, and things might have changed by the time you hear this. So here we go. Today we are joined via video conference by Alice Miranda Ollstein of Politico.
Alice Miranda Ollstein: Good morning.
Rovner: Sandhya Raman of CQ Roll Call.
Sandhya Raman: Good morning.
Rovner: And Joanne Kenen of the Johns Hopkins Bloomberg School of Public Health and Politico.
Joanne Kenen: Hi, everybody.
Rovner: Later in this episode we’ll have the winner of KHN’s health policy valentines contest. I hope everyone had a pleasant Valentine’s Day with someone that you love. But first, this week’s health news. I’m calling our lede segment this week “The Kids Are Not OK,” and we’ll get to the gun violence stuff in a minute. First is news from the Centers for Disease Control and Prevention’s Youth Risk Behavior Survey. And let me just read from the press release, quote, “Nearly 3 in 5 — 57% — of U.S. teen girls felt persistently sad or hopeless in 2021, double that of boys representing a nearly 60% increase, and the highest level reported over the past decade.” According to the survey, teens who identify as LGBTQ+ have, quote, “ongoing and extreme distress. More than 1 in 5 of that group said they had attempted suicide in the year before the survey.” Now, clearly, 2021 was a bad year for most of us. The pandemic was still raging, but the political fights over things like vaccines and masking were raging, too. But these rates of mental health problems found by the biannual survey of high school students has gone up in every report since 2001. Why is this happening? What is wrong with our young people and what can we do to help?
Kenen: Well, whatever’s wrong with our young people is going to also be wrong with our old people. I mean, we create the world in which … I mean, I’m a mother and I’m an aunt and I’m an extended-family motherly person. There’s something about the world that we have created for our young people. Julie, we grew up in the Cold War. We grew up … we don’t remember the missile crisis and things like that. But we did grow up in an era of anxiety, existential threats. And yet, for our generation, it wasn’t as bad as it is for this generation. And in this generation, you look at kids who seem to be on top of the world, and they feel like the world is on top of them.
Rovner: Well, at least in my case, you couldn’t be bullied unless you were in person … which is not true anymore.
Kenen: But even 2000, 2001, it wasn’t. That’s not the only thing going on here. And it’s not only the pandemic. I mean, it’s lots of things.
Ollstein: What really jumped out to me in this data was the really high rates of rape and sexual violence. You know, the CDC has said that 1 in 5 teen girls have experienced sexual violence just in the past year, and more than 1 in 10 say they’ve been forced to have sex. This was grouped together with the mental health, depression, suicidal ideation data, indicating that these things are related. And so I think in order to pinpoint some factors, it really seems like … people don’t know how to relate to each other in a sexual way that’s healthy. I think a lot about the efforts to restrict education about sex and sexuality in schools and how that could potentially make this even worse.
Rovner: And remember, this is a survey of high school students. So these are younger young people, or at least early in their, you know, sexual awareness.
Kenen: Yeah, but there was assault and unwanted … there was ugly stuff in prior generations, tons of it. And it wasn’t … and in some ways it was more secretive and more shameful. I mean, I’m not saying it’s not a problem. It’s obviously a huge problem. Alice is right. But it’s not unique to this generation. It’s hard to measure because we weren’t looking for it. But it certainly wasn’t something that didn’t happen. But I think it was even more secretive in the past. So I agree with Alice, but I don’t think that’s all of it.
Rovner: Sandhya.
Ollstein: And you’re right that it’s hard to know for past generations.
Kenen: But they didn’t ask that question.
Ollstein: Since they’ve been asking, it’s gotten worse. They say it’s … sexual violence is up 20% since 2017. Rape is up 27% since 2019. So since they’ve been investigating this, it’s getting worse.
Raman: I would also add the cyberbullying element is a huge piece. You know, if we were looking at this maybe 20 years ago, that was not the same case. The amount of time that teens and young people spend online is much greater now, even within the data they looked at it — that cyberbullying was a lot higher for teens, for LGBTQ youth. And that has been a broad issue that, even this week in Congress, the Senate Judiciary Committee was looking at protecting kids online. And a huge element of that was cyberbullying. You heard from different parents who had lost a child due to excessive cyberbullying on a lot of these social media apps and due to suicide or other mental health issues. And I think that’s a huge piece of now versus, you know, several years ago.
Rovner: Yeah, I agree. Well, clearly, one factor in the declining mental well-being of high school students is the threat of being swept up in a mass shooting event. As if this week’s shooting at Michigan State University wasn’t awful enough, some of the students who had to shelter in place for hours in East Lansing were also survivors of the Oxford, Michigan, high school shooting in 2021. And there was even one student that we know of who was at Sandy Hook Elementary in 2012. Now, in college, there have been 71 mass shootings, defined as an incident in which four or more people are shot or killed, so far in 2023, according to the Gun Violence Archive, and it’s only the middle of February. And just in time, Gallup reports that 63% of Americans are dissatisfied with the nation’s gun laws. Up 7 percentage points from last year and the highest level in 23 years. Is there any way to get this any closer to the top of the issues for lawmakers to address? I mean, they got something tiny done last year, but it feels like the problem is just exploding.
Raman: No, I was going to say, even last year with the incremental stuff was really difficult to get across the board. And, even going back to the CDC data, there were survey results about how many kids are afraid to go to school right now. And that was one of the factors that was rising. And gun violence is obviously a factor in safety, especially for kids now. But I think on a federal level, getting something additional across the line, especially with this split Congress, is going to be really difficult. It might be more of a state-level thing. I think Michigan is already talking about doing something, but it might have to be more on that end than federal.
Ollstein: Yeah, absolutely. And not only with the divided Congress, but I think a lot of the champions of gun reform on the Republican side have since retired. I’m thinking of Sen. [Pat] Toomey, in particular. And so not only do you have a House-Senate divide, but you don’t have some of the voices on the right calling for this that you’re used to.
Rovner: Yeah, the sides seem to be retreating to the poles, as usual, and the public is not happy about it.
Kenen: Well, one last thing, Julie, really quickly. I mean, I think young people today are very aware of climate as an existential threat, which was not true of prior generations.
Rovner: Yes.
Kenen: And I think kids have this real profound fear. And I think that feeds into the anxiety part of it. At least, you know, they just …
Rovner: Yeah, I think that’s absolutely true. And that’s something that’s been ratcheting up over the past several years as we’ve seen this mental well-being …
Kenen: The pace of damage to the Earth is faster than the scientists had projected.
Rovner: All right. Well, now we’re going to turn to abortion, which is another place where the public is not happy with how it’s being regulated. Yet a different Gallup poll finds Americans more dissatisfied with U.S. abortion policy than any time in 23 years, with a record 69% of adults reporting dissatisfaction. That includes 46% who want less strict laws and only 14% who say they want more restrictions. Yet the political energy seems like it’s with the anti-abortion side, or am I misreading that?
Ollstein: I think there’s a lot of activity on both sides. I mean, Sandhya mentioned Michigan, and I think that’s a spot — along with Minnesota, where Democrats really won big in this past election and want to use their new state-level power to advance some abortion rights measures. But I think you’re seeing a lot more on the “anti-” side, and you’re seeing a lot more splits within the anti-abortion side over how to restrict abortion, how far to go, what kind of exemptions to include, if any. And so you’re seeing a lot more debate, whereas the left, who wants to protect abortion rights, seems a little bit more unified on what they want to do right now. And then, like guns, the federal level is pretty stalemate, roadblock. Nothing much is going to happen there.
Rovner: But also, I think it’s that, you know — and I’m as guilty of this as anybody — that the journalists would rather cover squabbles than people who are actually together. So maybe it’s getting a little more ink. Well, it continues to look like a single federal judge in Texas might well try to ban the abortion pill. mifepristone nationwide. Trump appointee Matthew Kaczmarek did not rule as expected last week in a case charging FDA with wrongly approving the drug 22 years ago. Rather, the judge gave the parties two more weeks to submit briefs, which seems to have prompted every party with the least bit of interest in this case to file amicus briefs. I have never seen anything like this at the federal district court level. It looks like a major Supreme Court case, but it’s not. Has anybody else seen anything like this? I mean, this case seems to be taking on as much importance as your average big Supreme Court case.
Ollstein: It very well could be a Supreme Court case in the future. And I think that’s reflected there, too. And I also want to note that part of the reason for the couple of weeks of delay the judge ordered was to allow the drugmaker to have time to submit arguments because the drugmaker, Danco [Laboratories], says that the different parties in the suit, even the FDA, aren’t really representing their interests and they want to argue for the right to market their product. So that’s pretty interesting. But then, yeah, you have the attorneys general, Democrats, and Republicans lining up on either side of the case. The Republican attorneys general saying, “We support banning this medication nationwide” and the Democratic attorneys general saying, “No, let’s trust the FDA and their scientific process to approve this drug.”
Kenen: I mean, I think there’s sort of a significance in how it’s described because you can say, well, Congress gave the FDA the power to approve drugs. But the anti-abortion movement does not call this a medication abortion. They call it chemical abortion. And therefore, they’re treating this not as a drug but as a lethal chemical. You know, whether the judge goes along with that thinking … we know he’s a strongly anti-abortion judge. There’s no question. And there’s a widespread anticipation that he is going to rule with the anti-abortion side. But we never know what a judge is going to do until a judge does it. And Alice has covered this much more closely than I have, so she’ll probably want to weigh in more. But the issue is, is he going to think that the court should overrule the FDA or is he going to think this is a, quote, “chemical,” not a, quote “medication,” and therefore that the FDA is irrelevant? And I mean, Alice, you can give a better restatement of what I just said since you’ve written about it.
Rovner: I want to respond to Alice’s earlier point about the drug company wanting to get involved, because the big question here, not to get into too much legal minutiae, is why did the people who are suing have standing to sue? They have not been injured by the ability to sell this drug for 22 years. No one’s making them buy it. Arguably, the only party that has standing is the drug company, because if it was cut off, they would lose money. They have an obvious injury here. So the legal niceties of this may not go together either. Alice, do you want to do a follow-up?
Ollstein: Yeah, I mean, to go to the standing issue, the people challenging the FDA approval here are conservative doctors who say that they’ve had to do follow-up treatment for patients who’ve taken the abortion pill and then need follow-up treatment, and that takes their time and attention away from treating other patients. I mean, doctors treating a patient, that’s kind of their job. So I think there’s definitely a question on harm and standing there. Just a couple of thoughts on the case. Abortion rights groups both say that this could be an absolute crisis, disaster across the country. But then they also point out that people will still be able to have medication abortions because the two-pill regimen that’s been used for 20 years, it can still work with just the second pill. So this case is about banning the first pill. The different providers who have spoken out say we’re preparing to just provide abortions via the second pill, if needed.
Rovner: And that second pill, misoprostol, is not going to be pulled off the market. It’s used for many, many things. It just happens it also can end a pregnancy.
Ollstein: Exactly. Way harder to ban. And that’s one thing. Medication abortions will still continue if the judge rules how people expect him to. You know, another thing with all the amicus briefs and the drug company intervening as people are bringing up, if we allow someone to come in 20 years after the fact and challenge FDA approval of something, doesn’t that open Pandora’s box to people challenging all kinds of things, I mean, vaccines and whatnot? And won’t that cause chaos and not make drug companies feel like they can trust the process and have confidence in bringing drugs to market in the U.S.? So that’s another piece of the puzzle as well.
Raman: I would add that there’s already a little bit of chaos because, you know, whatever ruling we have, likely later this month, is almost definitely going to be appealed and then probably appeals again. So it’s going … we could have a back-and-forth process where providers might go one way and then the other. And then, in the contingency stuff they’ve been doing, piggybacking on what Alice was saying, is that if they do this misoprostol regimen, it’s not as straightforward as the two-dose that you’re used to in that there are different amounts of dosage, you might have to do repeated dosages. It’s not as simple, even if that’s done in a lot of other parts of the world. And then some providers have said that they would also just switch to doing all surgical abortions. But that also is more timely. You’d have to do the whole thing in clinic rather than send someone home with the pill. And then that is going to take longer. You’re going to schedule fewer patients. There’s already that many different contingency plans that these clinics are going to have to do regardless of what we hear down the line and through the appeals process.
Rovner: We already know that clinics are backed up from women coming from other states. So patients are having to wait longer to get abortions. And, you know, as … it gets further along, you have to do different procedures that are more expensive. It’s already piling up in different places. Well, speaking of some other different places, we’re seeing a lot of national pro- and anti-abortion groups getting involved in a Wisconsin Supreme Court election, of all things. What is up with that?
Ollstein: Well, that could decide the fate of abortion access in that state. You know, you have the split of a Democratic governor and a Republican legislature. So things really could come down. You know, the state had a pre-Roe ban that went into effect. So things are expected to come down to the makeup of the Supreme Court. And so you’re having just tons of outside money being poured into this race for that reason and really putting a spotlight on how much power are these state supreme courts have. And it’s true in other states as well. And there are many cases pending in different states. You know, I’ve been following the Kentucky one, in particular, but there are a bunch of different cases pending before a state supreme court that could really re-legalize or maintain the ban on abortion.
Kenen: There are also election issues and, on abortion, in the state of Wisconsin, election rules, election certification issues that it’s one of the three or four states where that’s really a hot potato. And that’s another reason this race is getting so much attention. I mean, it’s the state Supreme Court race that’s getting a huge amount of national attention and national money. So there are several issues I would agree with Alice on. The No. 1 is probably abortion. But it’s not only abortion.
Raman: And it’s interesting because this is the first time that EMILY’s List has endorsed ever a state Supreme Court race. And I think another thing to consider is that, you know, this is still considered a nonpartisan race since it’s a court seat. I mean …
Rovner: In theory.
Raman: In theory, yes. Even though all of these groups are looking at the histories of how people have ruled in the past. But I think that’s another thing that makes it a little bit more interesting given it’s not strictly a Democrat or Republican endorsement, like a lot of the other things that we’ve been following.
Rovner: Yes. And I saw on the other side the Susan B Anthony List, the anti-abortion group, said … put out a press release this week saying they’re going to have six-figure spending in Wisconsin on this race. So …
Kenen: It’ll be very good for the Wisconsin economy.
Rovner: It will be very good for the Wisconsin economy. Well, anti-abortion lawmakers are busy in a bunch of states pursuing another new trend, giving tax breaks to so-called crisis pregnancy centers that, at least when abortion was legal, lured pregnant women in by pretending to be an abortion clinic and then trying to convince them not to terminate their pregnancies. Missouri has already allowed donors to these crisis pregnancy centers to write off contributions on their state taxes. Now, Kansas, Arkansas, and Oklahoma are considering similar programs, but Kansas is the only one of those states where abortion is still legal. What are CPCs going to do now that they can’t pose as abortion facilities?
Raman: I think there’s still a lot of confusion for folks. I mean, given how a lot of these laws have been changing back and forth. I mean, even as folks that follow this very closely, there’s so many different things where someone … I think we’ve looked at polling before where people don’t always know: Is abortion illegal or not legal in our state? Or at what point? It’s difficult to keep track of, with so many changes going back and forth. So I think that there could feasibly still be people who might be looking for an abortion that don’t understand or — we’ve seen that a lot of these clinics have also bought a lot of ads so that you might be searching for an abortion and you get redirected to one of these clinics. So I think there’s still overlap in folks that might be searching for one and end up at another.
Kenen: I don’t know how much online presence they have, because that could be across state lines. You know, if someone’s on or near a border, there’s all sorts of … people might think that surgical abortions are legal, but medication is not, or that they can or someone could help them order pills. You can never underestimate how confused Americans are about any number of things. So … but they also might …
Rovner: This is confusing, to be fair.
Kenen: Yes. But they also might concentrate their efforts less on the no-abortion states and move more to the abortion states. Or they may advertise in ways that captures or attempts to capture people who are looking to go out of state or to get a cross-state-line prescription, whatever. They can promote themselves in different ways. Or they may also just decide to not do as much in Texas and do a lot more in upstate New York. I mean, I don’t know how they’re going to totally respond to the legal landscape either.
Ollstein: Yeah. And they’ve also become sort of a legal force of their own. I know they’re involved in challenging some of California’s pro-abortion rights policies. The CDC is specifically. So they also have … are trying to play a role on that front, in addition to direct patients’ interface or however we want to phrase it.
Rovner: All right. Well, while we’re talking about patients’ privacy, I want to talk about data. First, a kind of terrifying story from The Washington Post this week details how data brokers have been selling the names and addresses of people with depression, anxiety, and other mental health disorders so they can be advertised to. A lot of this has come from people using mental health apps or websites that are not covered by the HIPAA privacy rules because they are not technically covered health entities. A separate story this week notes how Virginia Gov. Glenn Youngkin helped defeat a bill in the Virginia legislature to provide legal protections to women’s menstrual data contained in period tracking apps. A Virginia official who was opposing the bill said it would put limits on search warrants, which could lead to other problems down the road. One researcher described the privacy practices of the vast majority of mental health apps as, quote, “exceptionally creepy.” How concerned should we be about all of this?
Kenen: I found that really horrifying. And a family friend who had been looking for a therapist and I said, well, maybe — and they were having trouble finding somebody in network and it’s very expensive — and I said, “Well, maybe you should look into some of the online ones that do take insurance.” And after reading that, I told that person, “I’m not so sure that it’s a good idea.” And we do have a shortage of mental health providers in this country. We have an even greater shortage of mental health providers that take insurance. There’s been a lot of talk about how telemedicine for mental health is at least part of the answer. But this should really raise … because they’re not just selling de-identified data. Some of them in that article were selling people’s names, address, diagnosis, and medical history. If it was truly, truly, truly de-identified, it’s different then. And that can be used for research. But a lot of what’s so-called de-identified isn’t de-identified. And this doesn’t even pretend to be. This is, like, search, and you can find out who the person is, an awful lot of intimate detail about their lives. So unless there’s some real safeguards, would you want any of your medical data with your name on it being sold? No. It is. It is being. But …
Rovner: When the HIPAA rules first went into effect, which was around the year 2000, actually it took a few years — researchers came to Capitol Hill screaming because they were afraid they weren’t going to be able to get any of this de-identified data and they weren’t going to be able to continue to do research. Now, we seem to have gone far in the other direction. And I know that there are efforts on Capitol Hill to do things to update the women’s reproductive information, keeping that private. Anybody think that they might get into an expansion of HIPAA? I mean, that’s really all it would take would be to create more covered entities.
Raman: Yeah, it isn’t as much about the expansion of HIPAA, but there have definitely been pretty concerted efforts to get … the U.S. doesn’t have a comprehensive data privacy law. You know, in contrast to, like, the EU or something. And that has been a big effort for the lawmakers that are focused on tech policy for a while. Even the hearing earlier this week with Senate Judiciary, they brought up several bills. And the issue has been that all of these issues are bipartisan, folks are on board. It’s just not enough people are on board, and little things that have been getting in the way there. And so that has been an issue. And I think even during that hearing, we had one researcher bring up different sites — like NEDA, which is mentioned in some of these lawsuits by some of the hospitals — have been collecting all of this data. But then they, as researchers, are not able to get access to that data, and that would be extremely beneficial for them to be able to say this is what the impact of some of these things are on kids. So it’s a Catch-22 where it’s, like, OK a) we’re not having the research be able to get the data, b) we’re having it sold in a malicious way and c) we haven’t been able to find a solution to mitigate all of this.
Kenen: Yeah, I don’t know about the prospects for a gigantic tech bill because it has many components and they’re controversial and hard to get 60 votes for. But I think there’s a difference between selling stuff about who bought shoes versus someone who is on an anti-psychotic or an antidepressant or whatever, or getting marital counseling, whatever. I mean, these are not the same issue as the whole constellation of tech issues. I can see this being something bipartisan. HIPAA has been updated a little bit, but the fundamental HIPAA law dates back to what, ’96, Julie? … I think that’s when it was.
Rovner: Yeah, although …
Kenen: It has been updated, but it hasn’t been overhauled to really fit the cyber universe we live in.
Rovner: But also Congress never really did HIPAA. People don’t remember this: The 1996 law basically had a provision that said Congress needs to fundamentally address privacy if we’re going to move more towards digital health records, which at the time was starting to happen. And if they don’t, then the secretary of Health and Human Services is authorized to put out regs. And guess what? Congress didn’t do it. So the HIPAA regs that we have now were put out at the end of the Clinton administration. Congress was never able to come together on this. So now things have obviously gotten worse.
Kenen: Yes. And since the Supreme Court now doesn’t like agencies regulating that, that seems to create an entire new existential question. But do I think that medical privacy is something that you could find some kind of bipartisan lanes on? I don’t think a lot of bipartisan things are going to happen in the next two years. This does seem to be one of the few areas that is not a red-blue ideological issue. And I can see Republicans and Democrats being horrified by some of this and maybe not totally sealing it up, but putting … better guardrails on what can be brokered.
Raman: One of the issues has been, I think even in the past, was that California is the one state that has implemented a few layers of very intense data privacy laws. And so, you know, when you have people in leadership that are in from California and it’s hard to get some of those compromises across when it might be more watered down than something California has and take precedent being federal. So it’s one of the many layers of why it’s been difficult over the past year to get any of this stuff done.
Rovner: Well, we should note that the Biden administration is actually working on some enforcement. Earlier this month, the Federal Trade Commission fined the prescription drug discounter GoodRx $1.5 million for illegally sharing customer’s personal health information. It was the very first enforcement action under a 2009 law that applies to health record vendors and others not covered by HIPAA. So at least there’s one avenue where this could be pursued. I imagine we’ll be seeing more of that if not, you know, whether or not they can reach all of these things seems unlikely.
Kenen: Yeah, doing it piecemeal does not seem to be the approach, and I’m not even sure how much $1.5 million is for GoodRx. I don’t think that’s a lot of money for any major pharmaceutical entity.
Rovner: No. And there are a lot of people who use it. All right. Well, finally this week, while we’re talking about drugs, I’ve been trying to get to this for a while. California has — speaking of California, things that other states haven’t done — California has decided to try to limit the cost of insulin for people with diabetes by manufacturing it itself. Could this set a precedent to really disrupt the insulin market, or is California just so big and wealthy that it’s basically the only state that could do something like this — or only state they would do something like this?
Ollstein: So I will note that Gov. [Gretchen] Whitmer in Michigan has also proposed state manufacturing of insulin. So California might not be the only one. I think the idea is that insulin is pretty cheap to manufacture. It’s become the poster child for out-of-control drug prices for that reason — the disparity between what it costs for patients and what it costs to make is so vast. And so I think you are likely to have a few states. But I think it will take a state doing it successfully to get a significant number of others to follow.
Rovner: I think there might be a thought that because California is so big, it could disrupt the market elsewhere — I mean, in the country. That strikes me as a reach. But it’s, you know, Congress, again — talking about things that Congress can’t do — they managed to limit insulin prices for people on Medicare, but not even for everybody else.
Kenen: There was also a good piece in The Atlantic, maybe two or three months ago, that some of these new diabetic drugs, which are injectables and very expensive, mean you don’t need insulin. So … but by addressing making insulin really cheap, which is a good … I mean so people who are on insulin and need insulin … but there are some people who actually could take one of these other drugs and then they wouldn’t be able to afford these other drugs, which might be better for them. And then they’ll end up on cheap insulin. So it’s always more complicated than it sounds. And I also think there’s different kinds of insulin. Someone else on the panel might, you know, that I’m not sure that …
Rovner: There are lots of different formulations.
Kenen: There are two major kinds of diabetes, obviously, Type 1 and Type 2. And then there’s different patients with different degrees of … you know, how far their other health conditions is advanced, etc., etc. So cheap insulin is not even a solution for diabetes. It’s one part of a solution for one of many chronic diseases in America.
Rovner: Well, we will never not have enough things to talk about. That is the news for this week. Now it is time for our extra-credit segment. That’s when we each recommend a story we read this week we think you should read, too. As always, don’t worry if you miss it. We will post the links on the podcast page at khn.org and in our show notes on your phone or other mobile device. Joanne, why don’t you kick us off this week?
Kenen: Yes. This was a collaboration between NPR, Nashville Public Radio, and Kaiser Health News, aired on NPR by Blake Farmer. “In Tennessee, a Medicaid Mix-Up Could Land You on a ‘Most Wanted’ List.” And basically, Tennessee is cracking down on Medicaid fraud. Most Medicaid fraud is actually from doctors and other health care providers — there have been a bunch of home health scandals and so forth. The amount of fraud and the amount of money involved in patient fraud is small, and yet they’re spending a huge amount of money to try to capture a small amount of fraud. And there are huge mistakes. Like the person in this article was just … she was entitled to Medicaid. She did nothing wrong. But they publicly … like, they don’t even wait for you to be convicted. They’re publishing … they’re making public the charge. This woman turned out to be … it had to do with an old address on … an expired driver’s license that got the system confused. She was doing nothing wrong, and yet she was completely blacklisted, employment and everything else because she was accused of being a felon in publicly available databases. So, a) are they looking in the right place for fraud? And b) are they protecting people’s rights? Clearly the latter they are not because they were publishing … people were accused but not convicted, and then they weren’t removing it in a timely, effective way. So this woman is, like, unemployable. She can’t rent an apartment, and she did nothing wrong. So there’s a whole series of abuses in this story. Not that Medicaid fraud is a good thing. Medicaid fraud is a bad thing, but this is not the way to go after it.
Rovner: This was one in a series of horrifying stories this week. Alice, you have another horrifying story.
Ollstein: Yes. Although this is under the banner of more evidence to bolster the upsetting things that we sort of already knew. This is a really good piece from The New York Times, laying out a lot of data to show that there is these differences in maternal mortality between Black and white women that can’t be attributed to income, showing that even wealthier Black women still face much worse outcomes. And so they say, you know, even when you account for income, even when you account for education and a lot of other factors, there are still these impacts of structural racism in the health system that continue to put Black mothers more in danger. And so this is coming at a time when there’s a lot of focus on this. But there has been sort of a lot of focus on the income, socioeconomic side and people recommending that states expand postpartum coverage of Medicaid. And that certainly is recommended, and experts think that would help. But this shows that it won’t completely solve the problem and there are other factors to address.
Kenen: And it’s not just in maternal mortality. I mean, the racial disparities in health care are not just income-related.
Rovner: And finally, Sandhya, you have a story from one of our fellow podcast panelists.
Raman: Yeah, the story I picked is “Zantac’s Maker Kept Quiet About Cancer Risks for 40 Years,” and that’s at Bloomberg News from Anna Edney, Susan Berfield, and Jef Feeley. And this was a really great story about Zantac, the heartburn and reflux drug that was once one of the world’s best-selling prescription medications. And then in 2020, it was pulled off the U.S. market over cancer risks. And the article goes through how since its beginnings, Glaxo’s own scientists, the drugmaker, had warned that it could be dangerous, but proving some of this has been a little difficult. … But the story goes through some of the documents that show that Glaxo chose not to look into this, even though the leading health agencies — EPA, FDA, WHO — all say NDMA is a carcinogen.
Rovner: Yeah, it’s quite the investigation. Well worth reading. Well, my story is a little less horrifying than everybody else’s. It’s from my former NPR Science Desk colleague Michaeleen Doucleff and it’s called “Is the Deadly Fungi Pandemic in ‘The Last of Us’ Actually Possible?” And I will cut to the chase. The answer is most almost certainly no. But that’s not to say we shouldn’t be worried about fungi and fungal diseases, particularly as the Earth continues to warm, which is what touches off the pandemic in the video game/HBO miniseries that’s airing now. There are new fungal diseases that can be pretty nasty, too, but zombies, almost certainly not. Well, maybe, certainly not. Anyway, listen to or read Michaeleen’s story. Before we go, this week was Valentine’s Day and, as promised, we have the winner of KHN’s best health policy valentine, as chosen by our editors and social media staff. This year’s winner is Jennifer Goldberg, and it goes as follows: “Roses are red, candy is sweet. Adding #Dental to #Medicare makes it more complete!” Congrats to Jennifer and thanks everyone for your creative health policy valentines.
OK, that’s our show for this week. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left us a review — that helps other people find us, too. Special thanks, as always, to our ever-patient producer, Francis Ying. As always, you can email us your comments or questions. We’re at whatthehealth — all one word — @kff.org. Or you can tweet me. I’m @jrovner. Joanne?
Kenen: @JoanneKenen
Rovner: Sandhya?
Raman: @SandhyaWrites
Rovner: Alice.
Ollstein: @AliceOllstein
Rovner: We will be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KHN’s What the Health? on Spotify, Apple Podcasts, Stitcher, Pocket Casts, or wherever you listen to podcasts.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
USE OUR CONTENT
This story can be republished for free (details).
2 years 5 months ago
Mental Health, Multimedia, Pharmaceuticals, Abortion, Children's Health, Drug Costs, Health IT, KHN's 'What The Health?', Podcasts
Ingestible Sensor Reveals Gastric Motility
Researchers at MIT have developed an ingestible sensor that can reveal gastrointestinal motility issues, such as gastroparesis and gastroesophageal reflux disease. The technology is intended for use as an easy at-home method to diagnose such issues, which typically require more invasive and inconvenient procedures, such as endoscopy or X-ray imaging. This new technology is based on the concept that a magnetic field produced by an electromagnetic coil becomes weaker the further away you move from the coil. This change in field signal is predictable, allowing researchers to calculate the distance accurately by measuring the magnetic field. The ingestible sensor measures the surrounding magnetic field and uses this to calculate its distance from an electromagnetic coil that is located outside the body. This allows the sensor to calculate where in the gastrointestinal tract it is, and this information can reveal to clinicians which parts of the tract are responsible for slow motility.
Gastrointestinal motility disorders occur when a part of the GI tract fails to move food through as it should. This can happen in any part of the GI tract, and obviously a first step in treating these conditions is to figure out which part of the gut is causing the problem. However, current approaches are a little cumbersome or invasive, requiring patient exposure to radiation in the form of X-ray imaging or endoscopic techniques involving the insertion of pressure sensing catheters that can measure the contractions of the gut.
“Many people around the world suffer from GI dysmotility or poor motility, and having the ability to monitor GI motility without having to go into a hospital is important to really understand what is happening to a patient,” said Giovanni Traverso, a researcher involved in the study.
To address this, these researchers focused on developing a simple capsule that can be swallowed and then reveal its location as it travels down through the GI tract. The technology achieves this by referencing an electromagnetic coil that remains outside the body. This second device is envisaged as being taped to the skin of the patient, or perhaps being integrated into their clothes or a backpack.
“Because the magnetic field gradient uniquely encodes the spatial positions, these small devices can be designed in a way that they can sense the magnetic field at their respective locations,” said Saransh Sharma, another researcher involved in the study. “After the device measures the field, we can back-calculate what the location of the device is.”
So far, in a large animal study in which the researchers used X-ray imaging to determine the position of the sensor and then compared this with the sensor’s own readings, the system correctly calculated its location in the gut within 5-10 millimeters.
Study in journal Nature Electronics: Location-aware ingestible microdevices for wireless monitoring of gastrointestinal dynamics
Via: MIT
2 years 5 months ago
GI, mit
Is it worth removing your fallopian tubes if you're not at an obvious risk of ovarian cancer? A top advocacy group recommends it - Yahoo! Voices
- Is it worth removing your fallopian tubes if you're not at an obvious risk of ovarian cancer? A top advocacy group recommends it Yahoo! Voices
- Is it worth removing your fallopian tubes if you're not at an obvious risk of ovarian cancer? A top advocacy group recommends it Yahoo News
2 years 5 months ago
Is it worth removing your fallopian tubes if you're not at an obvious risk of ovarian cancer? A top advocacy group recommends it - Yahoo! Voices
- Is it worth removing your fallopian tubes if you're not at an obvious risk of ovarian cancer? A top advocacy group recommends it Yahoo! Voices
- Is it worth removing your fallopian tubes if you're not at an obvious risk of ovarian cancer? A top advocacy group recommends it Yahoo News
- Fallopian Tubes: Is Pregnancy Possible With Only One? News18
- View Full Coverage on Google News
2 years 5 months ago
Specialist warns that causing abortion is always dangerous
On a daily basis, the country’s health centers receive cases of patients of all ages who have medical complications as a result of induced abortions performed under unsafe conditions that endanger their health and lives.
The consequences of having an unsafe abortion, whether because the woman ingested pills or another substance or because it was induced by another person, can range from emotional consequences to permanent anemia, mutilations, irreversible damage to the uterus, and even death.
This is how Dr. César López, president of the Dominican Society of Obstetrics and Gynecology, explains it, noting that in cases like this, where a woman’s life is put in danger, especially if she is an adolescent, no one is innocent, and there are responsibilities from all sectors, including a lack of sexual education in schools and the family itself. “Provoking or inducing an abortion will always be dangerous, and even more so if all the conditions that must be met, such as asepsis, correct anesthesia, and the expertise of the doctor who performs it, are not met,” he explained.
However, recent studies have shown that abortions are safe if performed between 70 days of gestation. Abortions are considered safe when they are “performed using a method recommended by WHO that is appropriate to the pregnancy duration and the person providing or supporting the abortion is trained,” according to experts such as Fathalla. “The WHO definition recognizes that the people, skills, and medical standards considered safe in the provision of induced abortions are different for medical abortion (which is performed with drugs alone), and surgical abortion (which is performed with a manual or electric aspirator), and that skills and medical standards required for safe abortion also vary depending upon the duration of the pregnancy and evolving scientific advances”.
The same studies state that abortions are considered less safe if they meet either the method or the provider criterion but not both. As a result, abortion is considered less safe when performed using outdated methods such as sharp curettage, even if the provider is trained, or when women using tablets lack access to proper information or a trained person if they require assistance.
2 years 5 months ago
Health, Local
Relaxation of COVID-19 restrictions coincided with increase in asthma exacerbations
Adults with asthma experienced more exacerbations and acute respiratory infections after COVID-19 restrictions were relaxed, according to study results published in Thorax.“The findings highlight the potential importance of public health measures like mask wearing/reduced social mixing for cutting risk of respiratory infections, which are the main triggers of asthma attacks,” Adrian Martineau,
MRCP, PhD, clinical professor of respiratory infection and immunity at Barts and the London School of Medicine and Dentistry, Queen Mary University of London, told Healio. “Obviously
2 years 5 months ago
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
GMC Jammu Begins 3 Years BSc Paramedical Courses In 8 Departments
Jammu: Government Medical College (GMC), Jammu, has begun 3 years of BSc Paramedical courses in 8 departments.
The courses included are –
1. BSc MLT
2. BSc Cardiac Care
3. BSc Renal Dialysis
4. BSc Respiratory Care
5. BSc Anesthesia
6. BSc Operation Theatre Technology
7. BSc Radiography
8. BSc Neuroscience Technology
Jammu: Government Medical College (GMC), Jammu, has begun 3 years of BSc Paramedical courses in 8 departments.
The courses included are –
1. BSc MLT
2. BSc Cardiac Care
3. BSc Renal Dialysis
4. BSc Respiratory Care
5. BSc Anesthesia
6. BSc Operation Theatre Technology
7. BSc Radiography
8. BSc Neuroscience Technology
The 1st batch was started in the year 2021 in the college. More than 100 students were admitted in all 8 streams. At present, four such batches are running smoothly in GMC Jammu.
As per the reports from Rising Kashmir, the meeting was chaired by Principal and Dean Dr Shashi Sudhan Sharma in which Dr Rachna Sabarwal, Professor, presented a brief presentation regarding the regulation and curriculum of BSc Paramedical courses, Department of Biochemistry and In-charge academics BSc paramedical course.
Also Read:CPS Mumbai Issues Instructions For Students For Convocation Ceremony
The admission to paramedical courses is based on parameters set by JK BOPEE. The following are the eligibility criteria –
1. The candidates must be a domicile of UT of J&K/UT of Ladakh.
2. The candidates must be 17 years of age as of 31st December of the admitting year.
3. The candidates must have passed 10+2 or equivalent examination with Science (PCB) and English through a recognized Board / University securing minimum qualifying marks.
Government Medical College, Jammu, a premier institute of J&K (Union Territory), was started in 1973 in a temporary building to provide quality education and deliver healthcare services to the people of this region. This institution is located in the heart of Temple City, Jammu. The institution started with a total of nine hundred beds. With the inauguration of the Medical College Hospital building in 1993, it has now increased to 1700 beds, including associated hospitals, including Sir. Col. R.N.Chopra Nursing Home. The courses offered are MBBS, PG, Degree in Physiotherapy, Ancillary Medical Training, and Paramedical.
Also Read:MUHS issues notice on No Objection Certificate Required For Migration, Transfer Of 1st Year MBBS Students
2 years 5 months ago
State News,News,Jammu & Kashmir,Medical Education,Paramedical Education News,Latest Medical Education News
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
DM Neurology: Admissions, Medical Colleges, fees, eligibility criteria details
DM Neurology or Doctorate of Medicine in Neurology also known as DM in Neurology
is a super speciality level course for doctors in India that is done by them
after completion of their postgraduate medical degree course. The duration of
this super speciality course is 3 years, and it deals
with the nervous system and its functional disorders.
DM Neurology or Doctorate of Medicine in Neurology also known as DM in Neurology
is a super speciality level course for doctors in India that is done by them
after completion of their postgraduate medical degree course. The duration of
this super speciality course is 3 years, and it deals
with the nervous system and its functional disorders.
Neurologists diagnose and treat diseases of the brain, spinal
cord, and nerves.
The course is a full-time course pursued at various recognized medical
colleges across the country. Some top medical colleges offering this
course include All India Institute of Medical Sciences, New Delhi, Sree Chitra Thirunal Institute for Medical Science
and Technology, Thiruvananthapuram,
Jawaharlal Institute of Postgraduate Medical Education & Research,
Puducherry (JIPMER), and more.
Admission to this course is done through the NEET-SS Entrance exam
conducted by the National Board of Examinations, followed by counseling based
on the scores of the exam that is conducted by DGHS/MCC/State Authorities.
The fee for pursuing DM (Neurology) varies from college to college and
may range from Rs. 5000 to Rs. 30 lakhs per year.
After completion of their respective course, doctors can either join the
job market or can pursue certificate courses and Fellowship programmes
recognized by NMC and NBE. Candidates can take reputed jobs at positions as
Senior residents, Consultants, etc. with an approximate salary range of Rs.30
lakhs to Rs. 60 lakhs per year depending upon their expertise.
What is DM in Neurology?
Doctorate of Medicine in Neurology, also known as DM (Neurology) or DM
in (Neurology) is a three-year super speciality programme that candidates can
pursue after completing a postgraduate medical degree.
Neurology is the branch of medical science dealing with the nervous system and its functional disorders. Neurologists diagnose and treat diseases and disorders of the brain, spinal cord, and nerves.
The postgraduate students must gain ample knowledge and experience in
the diagnosis, and treatment of patients with acute, serious, and life-threatening
medical and surgical diseases.
PG education intends to create specialists who can contribute to
high-quality health care and advances in science through research and training.
The required training done by a postgraduate specialist in the field of Neurology
would help the specialist to recognize the health needs of the community. The
student should be competent to handle medical problems effectively and should
be aware of the recent advances in their specialty.
The candidate is also expected to know the principles of research
methodology and modes of the consulting library. The candidate should regularly
attend conferences, workshops and CMEs to upgrade her/ his knowledge.
Course Highlights
Here are some of the course highlights of DM in Neurology
Name of Course
DM in Neurology
Level
Doctorate
Duration of Course
Three years
Course Mode
Full Time
Minimum Academic
Requirement
Candidates must have a postgraduate medical Degree in MD/DNB
(General Medicine) or MD/DNB (Paediatrics) obtained from any
college/university recognized by the Medical Council of India (Now NMC)/NBE,
this feeder qualification mentioned here is as of 2022. For any further
changes to the prerequisite requirement please refer to the NBE website.
Admission Process /
Entrance Process / Entrance Modalities
Entrance Exam
(NEET-SS)
INI CET for various
AIIMS, PGIMER Chandigarh, JIPMER Puducherry, NIMHANS Bengaluru
Counselling by DGHS/MCC/State
Authorities
Course Fees
Rs.5000 to
Rs. 20 lakhs per year
Average Salary
Rs.30 lakhs to Rs. 60
lakhs per year
Eligibility Criteria
The eligibility criteria for DM in Neurology are defined as the set of
rules or minimum prerequisites that aspirants must meet to be eligible
for admission, which includes:
Name of DM course
Course Type
Prior Eligibility Requirement
Neurology
DM
MD/DNB (General Medicine)
MD/DNB (Paediatrics)
Note:
· The feeder qualification for DM in Neurology is
defined by the NBE and is subject to changes by the NBE.
· The feeder qualification mentioned here is as of
2022.
· For any changes, please refer to the NBE website.
· The candidate must have obtained permanent
registration with any State Medical Council to be eligible for admission.
· The medical college's recognition cut-off dates for
the Postgraduate Degree courses shall be as prescribed by the Medical Council
of India (now NMC).
Admission Process
- The admission process
contains a few steps to be followed in order by the candidates for
admission to DM in Neurology. Candidates can view the complete admission
process for DM in Neurology mentioned below:
- The NEET-SS or National
Eligibility Entrance Test for Super speciality courses is a national-level
master's level examination conducted by the NBE for admission to
DM/MCh/DrNB Courses.
- Qualifying
Criteria-Candidates placed at the 50th percentile or above shall be
declared as qualified in the NEET-SS in their respective speciality.
- The following Medical
institutions are not covered under centralized admissions for DM/ MCh
courses through NEET-SS:
- AIIMS,
New Delhi and other AIIMS - PGIMER,
Chandigarh - JIPMER,
Puducherry - NIMHANS,
Bengaluru
- Candidates from all eligible
feeder speciality subjects shall be required to appear in the question
paper of the respective group if they are willing to opt for a super
speciality course in any of the super speciality courses covered in that
group.
- A candidate can opt for
appearing in the question papers of as many groups for which his/her
Postgraduate speciality qualification is an eligible feeder qualification.
- By appearing in the question
paper of a group and on qualifying for the examination, a candidate shall be eligible
to exercise his/her choices in the counselling only for those super speciality subjects covered in the said group for which his/ her broad
speciality is an eligible feeder qualification.
Fees Structure
The fee structure for DM in Neurology varies from college to college.
The fee is generally less for Government Institutes and more for private
institutes. The average fee structure for DM in Neurology is around Rs.5000 to Rs. 30 lakhs per year.
Colleges offering DM in Neurology
There are various medical colleges across India that offer courses for
pursuing DM in (Neurology).
As per National Medical Commission (NMC) website, the following medical
colleges are offering DM in (Neurology) courses for the academic year 2022-23.
Sl.No.
Course Name
State
Name and Address of
Medical College / Medical Institution
Management of College
1
DM - Neurology
Andhra Pradesh
Andhra Medical College, Visakhapatnam
Govt.
2
DM - Neurology
Andhra Pradesh
Sri Venkateswara Institute of Medical Sciences
(SVIMS) , Tirupati
Govt.
3
DM - Neurology
Andhra Pradesh
Guntur Medical College, Guntur
Govt.
4
DM - Neurology
Andhra Pradesh
NRI Medical College, Guntur
Trust
5
DM - Neurology
Andhra Pradesh
Narayana Medical College, Nellore
Trust
6
DM - Neurology
Assam
Gauhati Medical College, Guwahati
Govt.
7
DM - Neurology
Bihar
Indira Gandhi Institute of Medical
Sciences, Sheikhpura, Patna
Govt.
8
DM - Neurology
Chandigarh
Postgraduate Institute of Medical Education &
Research, Chandigarh
Govt.
9
DM - Neurology
Delhi
All India Institute of Medical Sciences, New
Delhi
Govt.
10
DM - Neurology
Delhi
Atal Bihari Vajpayee Institute of Medical
Sciences and Dr RML Hospital, New Delhi
Govt.
11
DM - Neurology
Delhi
G.B. Pant Institute of Postgraduate Medical
Education and Research, New Delhi
Govt.
12
DM - Neurology
Delhi
Vardhman Mahavir Medical College & Safdarjung
Hospital, Delhi
Govt.
13
DM - Neurology
Delhi
Institute of Human Behaviour and Allied Sciences,
Delhi
Govt.
14
DM - Neurology
Gujarat
SBKS Medical Instt. & Research Centre,
Vadodra
Trust
15
DM - Neurology
Gujarat
Smt. N.H.L.Municipal Medical College, Ahmedabad
Govt.
16
DM - Neurology
Jammu & Kashmir
Sher-I-Kashmir Instt. Of Medical Sciences,
Srinagar
Govt.
17
DM - Neurology
Karnataka
National Institute of Mental Health & Neuro
Sciences, Bangalore
Govt.
18
DM - Neurology
Karnataka
Jawaharlal Nehru Medical College, Belgaum
Trust
19
DM - Neurology
Karnataka
S S Institute of Medical Sciences& Research
Centre, Davangere
Trust
20
DM - Neurology
Karnataka
Kasturba Medical College, Manipal
Trust
21
DM - Neurology
Karnataka
Father Mullers Medical College, Mangalore
Trust
22
DM - Neurology
Karnataka
JSS Medical College, Mysore
Trust
23
DM - Neurology
Karnataka
Vydehi Institute Of Medical Sciences &
Research Centre, Bangalore
Trust
24
DM - Neurology
Karnataka
St. Johns Medical College, Bangalore
Trust
25
DM - Neurology
Karnataka
Bangalore Medical College and Research Institute,
Bangalore
Govt.
26
DM - Neurology
Karnataka
M S Ramaiah Medical College, Bangalore
Trust
27
DM - Neurology
Kerala
Government Medical College, Kottayam
Govt.
28
DM - Neurology
Kerala
Sree Chitra Thirunal Institute for Medical
Science and Technology, Thiruvananthapura
Govt.
29
DM - Neurology
Kerala
Government Medical College, Kozhikode, Calicut
Govt.
30
DM - Neurology
Kerala
Medical College, Thiruvananthapuram
Govt.
31
DM - Neurology
Kerala
Pushpagiri Institute Of Medical Sciences and
Research Centre, Tiruvalla
Trust
32
DM - Neurology
Kerala
M E S Medical College , Perintalmanna Malappuram
Distt.Kerala
Trust
33
DM - Neurology
Kerala
Jubilee Mission Medical College & Research
Institute, Thrissur
Trust
34
DM - Neurology
Kerala
T D Medical College, Alleppey (Allappuzha)
Govt.
35
DM - Neurology
Kerala
Amrita School of Medicine, Elamkara, Kochi
Trust
36
DM - Neurology
Madhya Pradesh
All India Institute of Medical Sciences, Bhopal
Govt.
37
DM - Neurology
Madhya Pradesh
Sri Aurobindo Medical College and Post Graduate
Institute, Indore
Trust
38
DM - Neurology
Maharashtra
Seth GS Medical College, and KEM Hospital, Mumbai
Govt.
39
DM - Neurology
Maharashtra
Bombay Hospital Institute of Medical Sciences,
Mumbai
Govt.
40
DM - Neurology
Maharashtra
Topiwala National Medical College, Mumbai
Govt.
41
DM - Neurology
Maharashtra
Grant Medical College, Mumbai
Govt.
42
DM - Neurology
Maharashtra
Jawaharlal Nehru Medical College, Sawangi
(Meghe), Wardha
Trust
43
DM - Neurology
Maharashtra
Bharati Vidyapeeth University Medical College,
Pune
Trust
44
DM - Neurology
Maharashtra
Dr D Y Patil Medical College, Hospital and
Research Centre, Pimpri, Pune
Trust
45
DM - Neurology
Meghalaya
North Eastern Indira Gandhi Regional Instt. of
Health and Medical Sciences, Shillong
Govt.
46
DM - Neurology
Orissa
All India Institute of Medical Sciences,
Bhubaneswar
Govt.
47
DM - Neurology
Orissa
Kalinga Institute of Medical Sciences,
Bhubaneswar
Trust
48
DM - Neurology
Orissa
Instt. Of Medical Sciences & SUM Hospital,
Bhubaneswar
Trust
49
DM - Neurology
Orissa
SCB Medical College, Cuttack
Govt.
50
DM - Neurology
Pondicherry
Jawaharlal Institute of Postgraduate Medical
Education & Research, Pondicherry
Govt.
51
DM - Neurology
Punjab
Christian Medical College, Ludhiana
Trust
52
DM - Neurology
Punjab
Dayanand Medical College & Hospital, Ludhiana
Trust
53
DM - Neurology
Rajasthan
SMS Medical College, Jaipur
Govt.
54
DM - Neurology
Rajasthan
All India Institute of Medical Sciences, Jodhpur
Govt.
55
DM - Neurology
Rajasthan
Geetanjali Medical College & Hospital, Udaipur
Trust
56
DM - Neurology
Rajasthan
Mahatma Gandhi Medical College and Hospital,
Sitapur, Jaipur
Trust
57
DM - Neurology
Rajasthan
Government Medical College, Kota
Govt.
58
DM - Neurology
Rajasthan
Dr SN Medical College, Jodhpur
Govt.
59
DM - Neurology
Tamil Nadu
Sri Ramachandra Medical College & Research
Institute, Chennai
Trust
60
DM - Neurology
Tamil Nadu
Tirunelveli Medical College,Tirunelveli
Govt.
61
DM - Neurology
Tamil Nadu
Madurai Medical College, Madurai
Govt.
62
DM - Neurology
Tamil Nadu
Saveetha Medical College and Hospital,
Kanchipuram
Trust
63
DM - Neurology
Tamil Nadu
Stanley Medical College, Chennai
Govt.
64
DM - Neurology
Tamil Nadu
Madras Medical College, Chennai
Govt.
65
DM - Neurology
Tamil Nadu
Christian Medical College, Vellore
Trust
66
DM - Neurology
Tamil Nadu
Dhanalakshmi Srinivasan Medical College and
Hospital,Perambalur
Trust
67
DM - Neurology
Tamil Nadu
KanyaKumari Government Medical College,
Asaripallam
Govt.
68
DM - Neurology
Tamil Nadu
Govt. Mohan Kumaramangalam Medical College,
Salem- 30
Govt.
69
DM - Neurology
Tamil Nadu
K A P Viswanathan Government Medical College,
Trichy
Govt.
70
DM - Neurology
Tamil Nadu
Thoothukudi Medical College, Thoothukudi
Govt.
71
DM - Neurology
Tamil Nadu
Chengalpattu Medical College, Chengalpattu
Govt.
72
DM - Neurology
Tamil Nadu
Coimbatore Medical College, Coimbatore
Govt.
73
DM - Neurology
Tamil Nadu
Thanjavur Medical College,Thanjavur
Govt.
74
DM - Neurology
Tamil Nadu
Chettinad Hospital & Research Institute,
Kanchipuram
Trust
75
DM - Neurology
Tamil Nadu
Sree Balaji Medical College and Hospital, Chennai
Trust
76
DM - Neurology
Tamil Nadu
SRM Medical College Hospital & Research
Centre, Chengalpattu
Trust
77
DM - Neurology
Tamil Nadu
Meenakshi Medical College and Research Institute,
Enathur
Trust
78
DM - Neurology
Tamil Nadu
PSG Institute of Medical Sciences, Coimbatore
Trust
79
DM - Neurology
Telangana
Osmania Medical College, Hyderabad
Govt.
80
DM - Neurology
Telangana
Nizams Institute of Medical Sciences, Hyderabad
Govt.
81
DM - Neurology
Telangana
Gandhi Medical College, Secunderabad
Govt.
82
DM - Neurology
Telangana
Chalmeda Anand Rao Insttitute Of Medical
Sciences, Karimnagar
Trust
83
DM - Neurology
Telangana
Deccan College of Medical Sciences, Hyderabad
Trust
84
DM - Neurology
Uttarakhand
All India Institute of Medical Sciences,
Rishikesh
Govt.
85
DM - Neurology
Uttarakhand
Himalayan Institute of Medical Sciences, Dehradun
Trust
86
DM - Neurology
Uttar Pradesh
Institute of Medical Sciences, BHU, Varansi
Govt.
87
DM - Neurology
Uttar Pradesh
Sanjay Gandhi Postgraduate Institute of Medical
Sciences, Lucknow
Govt.
88
DM - Neurology
Uttar Pradesh
King George Medical University, Lucknow
Govt.
89
DM - Neurology
Uttar Pradesh
Dr. Ram Manohar Lohia Institute of Medical
Sciences,Lucknow
Govt.
90
DM - Neurology
West Bengal
Institute of Postgraduate Medical Education &
Research, Kolkata
Govt.
91
DM - Neurology
West Bengal
Calcutta National Medical College, Kolkata
Govt.
92
DM - Neurology
West Bengal
Burdwan Medical College, Burdwan
Govt.
93
DM - Neurology
West Bengal
Nilratan Sircar Medical College, Kolkata
Govt.
94
DM - Neurology
West Bengal
Govt. Medical College, Kolkata
Govt.
Syllabus
A DM in Neurology is a three years specialization course that provides
training in the stream of Neurology.
The course content for DM in Neurology is given in the Competency-Based Postgraduate Training Programme released by National Medical Commission, which can be assessed through the link mentioned below:
NMC Guidelines For Competency Based Training Programme For DM Neurology
SYLLABUS
Course contents
AIM:
To produce specialists with necessary skills, judgement and sense of dedication to tackle all major and minor cardiac problems. The candidates will be trained in all aspects of Neurology starting from Basic Sciences to recent advances.
PAPER I: BASIC SCIENCES RELATED TO NEUROLOGY
NEUROANATOMY
The Neuroanatomy with special emphasis on development of:
· Neuroaxis (brain, spinal cord and neurons and glia),
· Autonomic nervous system and their maturation process in the post-natal, childhood and adolescent states;
· Location and significance of stem cells,
· CSF pathways,
· Blood supply and sino venous drainage of brain and spinal cord, the meninges,
· Skull and vertebral column, the cranial nerves, spinal roots, plexuses, and their relation to neighboring structures;
· Anatomy of peripheral nerves,
· Neuromuscular junction and muscles;
· Histology of cerebrum, cerebellum, pituitary gland, brain stem and
spinal cord, nerves and neuromuscular junction and muscle.
· Functional anatomy of lobes of cerebrum and white matter tracts of brain and spinal cord, craniovertebral junction, conus and epiconus and cauda equina, brachial and lumbosacral plexuses, cavernous and other venous sinuses;
· New developments in understanding of:
o Ultrastructural anatomy of neurons,
o axonal transport,
o neural networks and synapses and nerve cell function at molecular level.
NEUROPHYSIOLOGY
- Neurophysiology will cover all the physiological changes in the nervous system during its normal function with special reference to nerve impulse transmission along myelinated fibers,
- neuromuscular junction and synaptic transmission,
· muscle contraction;
· visual, auditory and somatosensory and cognitive evoked potentials;
· Regulation of secretions by glands, neural control of viscera such as heart, respiration, GI tract, bladder and sexual function; sleep-wake cycles;
· Maintenance of consciousness,
· special senses,
· control of functions of (a) pituitary, (b) autonomic system (c) cerebellum, (d) and extrapyramidal functions,
· reflexes,
· upper and lower motor neuron concepts and sensory system.
MOLECULAR BIOLOGY
Brain is the one structure where maximum genes are expressed in the human
body. The topics include:
· Principles of molecular biology including Gene Structure, Expression and regulation;
· Recombinant DNA Technology;
· PCR Techniques,
· Molecular basis for neuronal and glial function,
· Molecular and cellular biology of the membranes and ion-channels,
· Mitochondrial genome,
· Role of RNA in normal neuronal growth and functional expression,
· Receptors of neurotransmitters,
· Molecular and cellular biology of muscles and neuromuscular junction, etc.
· The Human Genome and its future implications for Neurology including
developmental and neurogenetic disorders,
· bioethical implications and genetic counselling,
· Nerve growth and other trophic factors and neuroprotectors,
· Neural Tissue modification by genetic approaches including Gene Transfer, stem cell therapy etc.
· Molecular Development of neural tissue in peripheral nerve repair
NEUROCHEMISTRY
· All aspects of normal and abnormal patterns of neurochemistry including:
· Neurotransmitters associated with different anatomical and functional areas of brain and spinal cord, especially with respect to dopaminergic, serotoninergic, adrenergic and cholinergic systems,
· Opioids,
· Excitatory and inhibitory amino acids and their role in pathogenesis of Parkinsonism, depression, migraine, dementia, epilepsy,
· Neuromuscular junction and muscle contractions,
· Carbohydrate, amino acid and lipid metabolism,
· Neural expression of disorders of their metabolism,
· Electrolytes and their effect on encephalopathies,
· Muscle membrane function, storage disorders,
· Porphyria.
NEUROPHARMACOLOGY
- Application of neuropharmacology in medical therapy of epilepsy, Parkinsonism, movement disorders, neuropsychiatric syndromes, spasticity, pain syndromes, disorders of sleep and dysautonomia syndromes.
- Antiepileptic drugs, usage during disorders of renal, hepatic function and in dementia.
- Adverse drug reactions of common drugs used in Neurological disorders including antiepileptic drugs, antiplatelets, anticoagulants etc.
NEUROPATHOLOGY
- Pathological changes in various neurological diseases with special reference to vascular, immune-mediated, demyelinating and dysmyelinating, metabolic and nutritional, genetic and developmental, infectious and iatrogenic and neoplastic etiologies and clinical correlation.
- Pathological changes in nerve and muscle in neuropathies and myopathies.
- Ultrastructural pathology such as apoptosis, ubiquitinopathies, mitochondrial diseases, channelopathies, peroxisomal disorders, inclusion bodies, prion diseases, disorders mediated by antibodies against various cell and nuclear components, paraneoplastic disorders etc.
NEUROMICROBIOLOGY
Microbiological aspects of infectious neurologic diseases including:
- Encephalitis, meningitis, brain abscess, granulomas, myelitis, cold abscess, cerebral malaria, parasitic cysts of nervous system, rhino cerebral mycoses, leprous neuritis, neuro leptospirosis, primary and secondary Neuro HIV infections, congenital TORCH infections of brain, slow virus infections such as CJD and SSPE.
- Neurological complications of viral infections such as Polio, EBV, Chickenpox, Rabies, Herpes, Japanese encephalitis and other epidemic viral infections.
NEUROTOXICOLOGY
Diagnosis and effective therapy of:
· Organophosphorus poisoning,
· hydrocarbon poisoning,
· lead, arsenic, botulinum toxin and tetanus toxicity,
· snake, scorpion, spider, wasp and beestings.
NEUROGENETICS AND PROTEOMICS:
· Autosomal dominant and recessive and X-linked inheritance patterns,
· disorders of chromosomal anomalies,
· Gene mutations, trinucleotide repeats, dysregulation of gene expressions,
· Enzyme deficiency syndromes,
· Storage disorders,
· Disorders of polygenic inheritance,
· Proteomics in health and disease.
NEUROEPIDEMIOLOGY:
- Basic methodology in community and hospital based neuro-epidemiological studies such as systematic data collection, analysis, derivation of logical conclusions,
· Concepts of case-control and cohort studies, correlations,
· Regressions and survival analysis,
· Basic principles of clinical trials.
PAPER II: CLINICAL NEUROLOGY INCLUDING PEDIATRIC NEUROLOGY and NEUROPSYCHIATRY.
GENERAL EVALUATION OF THE PATIENT
- The science and art of history taking,
- Physical examination including elements of accurate history taking, symptoms associated with neurological disease,
- Physical examination of adults, children, infants and neonates, syndromes
associated with congenital and acquired neurological disease, cutaneous
markers,
· Examination of unconscious patients,
· Examination of higher mental functions, cranial nerves, the ocular fundus,
· Examination of tone, power of muscles,
· Proper elicitation of superficial and deep reflexes including alternate techniques,
· Neonatal and released reflexes,
- Neurodevelopmental assessment of children, sensory system, peripheral nerves, signs of Meningeal irritation, skull and spine examination including measurement of head circumference, shortness of neck and carotid pulsations .and vertebral bruits.
DISTURBANCES OF SENSORIUM
- Pathophysiology and diagnosis of COMA,
- Diagnosis and management of coma, delirium and acute confusional states, reversible and irreversible causes,
- Persistent vegetative states and brain death,
- Neurophysiological evaluation and confirmation of these states,
- Mechanical ventilation and other supportive measures of comatose patient,
- Prevention of complications of prolonged coma,
· The significance of timely brain death in organ donation and ICU resource utilization.
SEIZURES and EPILEPSY and SYNCOPE
· Diagnosis of seizures, epilepsy and epileptic syndromes,
- Recognition, clinical assessment and management of seizures especially their electrodiagnosis, video monitoring with emphasize on phenomenology and their correlation with EEG,
- Structural and functional brain imaging such as CT and MRI and fMRI and SPECT scan,
- Special situations such as epilepsy in pregnant and nursing mothers, driving, risky occupations, its social stigmas differentiation from pseudo seizures,
- Use of conventional and newer antiepileptic drugs, their drug interactions and adverse effects etc.,
- Modern lines of management of intractable epilepsies, such as ketogenic diet, vagal nerve stimulation, epilepsy surgery,
- Pre-surgical evaluation of patients,
- Management of status epilepticus and refractory status epilepticus,
- Differentiation of seizures from syncope, drop attacks, cataplexy, startles etc.
HEADACHES and OTHER CRANIAL NEURALGIAS
· Acquisition of skills in the analysis of headaches of various causes such as those from raised intracranial pressures, migraines, cranial neuralgias, vascular malformations,
· Meningeal irritation, Psychogenic etc. and their proper pharmacologic management.
CEREBROVASCULAR DISEASES
· Vascular anatomy of the brain and spinal cord,
- Various causes and types of cerebrovascular syndromes, ischemic and hemorrhagic types, arterial and venous types, anterior and posterior circulation strokes,
· OCSP and TOAST classifications,
· Investigation of strokes including neuroimaging using Dopplers,
- CT and MR imaging and angiography, acute stroke therapy including
thrombolytic therapy,
· Interventional therapy of cerebrovascular diseases,
· Principles of management of subarachnoid haemorrhage etc.
- Special situations like strokes in the young, strategies for primary and secondary prevention of stroke.
DEMENTIAS
· Concept of minimal cognitive impairment,
- Reversible and irreversible dementias causes such as Alzheimer’s and other neurodegenerative diseases and vascular and nutritional and infectious dementias, their impact on individuals, families and in society.
- Genetic and familial syndromes.
- Pharmacotherapy of dementias, the potential role of cognitive rehabilitation and special care of the disabled.
PARKINSONISM AND MOVEMENT DISORDERS
· Disorders of the extrapyramidal system such as Parkinsonism, chorea, dystonia, athetosis, tics, their diagnosis and management,
· Pharmacotherapy of Parkinsonism and its complications,
- management of complications of Parkinsonism therapy, including principles of deep brain stimulation and lesion surgeries.
· Use of EMG-guided botulinum toxin therapy,
· Management of spasticity using intrathecal baclofen and TENS.
ATAXIC SYNDROMES:
· Para infectious demyelination, cerebellar tumours, hereditary ataxias, vestibular disorders,
· Diagnosis and management of brainstem disorders,
· Axial and extra-axial differentiation.
CRANIAL NEUROPATHIES:
- Disorders of smell, vision, visual pathways, pupillary pathways and reflexes,
- Internuclear and supranuclear ophthalmoplegia,
- Other oculomotor disorders,
- Trigeminal nerve testing,
- Bell’s palsy,
- Differentiation from UMN facial lesions,
- Brain stem reflexes,
- Investigations of vertigo and dizziness,
- Differentiation between central and peripheral vertigo,
· Differential diagnosis of nystagmus,
· Investigations of deafness, bulbar and pseudobulbar syndromes.
CNS INFECTIONS:
- Diagnosis and management of viral encephalitides, meningitis bacterial, tuberculous, fungal, parasitic infections such as cysticercosis, cerebral malaria, SSPE, Neuro HIV primary and secondary infections with exposure to gram stain and cultures, bac tec, QBC, ELISA and PCR technologies.
NEUROIMMUNOLOGY DISEASES
- Diagnosis and management of CNS conditions such as Multiple Sclerosis, PNS conditions such as GBS, CIDP, Myasthenia gravis, polymyositis.
NEUROGENETIC DISORDERS
· Various chromosomal diseases,
- Single gene mutations such as enzyme deficiencies,
- Autosomal dominant and recessive conditions and X-linked disorders,
trinucleotide repeats,
- Disorders of DNA repair. Genetics of Huntington’s disease, familial dementias, other storage disorders, hereditary ataxias,
- Hereditary spastic paraplegias, HMSN, muscular dystrophies, mitochondrial inheritance disorders.
DEVELOPMENTAL DISORDERS OF NERVOUS SYSTEM
· Neuronal migration disorders,
· Craniovertebral junction diseases,
· Spinal dysraphism,
- Phacomatoses and other neurocutaneous syndromes- their recognition and management.
MYELOPATHIES
- Clinical diagnosis of distinction between compressive and non-compressive myelopathies,
· Spinal syndromes such as anterior cord, subacute combined degeneration,
· Central cord syndrome,
· Brown-Sequard syndrome,
· Tabetic syndrome,
· Ellsberg phenomenon.
· Diagnosis of spinal cord and root compression syndromes,
· CV junction lesions,
· Syringomyelia, conus cauda lesions,
· Spinal AVMs,
· tropical and hereditary spastic paraplegias,
· Fluorosis.
PERIPHERAL NEUROPATHIES
- Immune mediated, hereditary, toxic, nutritional and infectious type peripheral neuropathies; their clinical and electrophysiological diagnosis.
MYOPATHIES AND NEUROMUSCULAR JUNCTION DISORDERS
· Clinical evaluation of patients with known or suspected muscle diseases aided by EMG,
- Muscle pathology, histochemistry, immunopathology and genetic studies,
- Dystrophies, polymyositis, channnelopathies, congenital and mitochondrial myopathies,
· Neuromuscular junction disorders such as myasthenia, botulism, Eaton-lambert syndrome,
- Snake and organophosphorus poisoning, their electrophysiological diagnosis and management.
· Myotonia, stiff person syndrome.
PAEDITRIC NEUROLOGY:
· Normal development of motor and mental milestones in a child, Cerebral palsy,
· Attention deficit disorder,
· Autism,
· Developmental dyslexia,
· Intrauterine TORCH infections,
· Storage disorders,
· Inborn errors of metabolism affecting nervous system,
· Developmental malformations,
· Child hood seizures and epilepsies,
· Neurodegenerative diseases.
COGNITIVE NEUROLOGY AND NEUROPSYCHIATRY:
· Detailed techniques of higher mental functions evaluation,
- Basics of primary and secondary neuropsychiatric conditions such as anxiety, depression, schizophrenia, acute psychosis, acute confusional reactions (delirium), organic brain syndrome,
· Primary and secondary dementias, differentiation from pseudodementia.
TROPICAL NEUROLOGY
Conditions which are specifically found in the tropics like to be taught in detail;
· Neuro-cysticercosis,
· Cerebral malaria,
· Tropical spastic paraplegia,
· Snake/scorpion/ Chandipura
· Encephalitis,
· Madras Motor Neuron disease etc.
PAPER III: DIAGNOSTIC and INTERVENTIONAL NEUROLOGY INCLUDING NEUROLOGICAL INSTRUMENTATION, DIAGNOSTIC
NEUROLOGY
· Performing and interpreting Digital Electroneurogram, Electromyogram,
· Evoked potentials, Electroencephalography,
· Interpretation of skull and spine X-rays,
· Computerized tomography of brain and spine,
- Magnetic resonance images of brain including correct identification of various sequences, angiograms, MR spectroscopy,
· Basics of functional MRI,
- Interpretation of digital subtraction imaging, SPECT scans of brain, subdural EEG recording, transphenoidal electrode EEG techniques for temporal lobe seizures,
- video EEG interpretation of phenomenology and EEG-phenomenology correlations,
- EEG telemetry,
- Transcranial Doppler diagnosis and monitoring of acute ischemic stroke,
- Subarachnoid haemorrhage,
- Detection of right-to-left shunts etc;
- Colour duplex scanning in Carotid and vertebral extracranial segment screening.
NEUROINSTRUMENTATIONS
Acquire skills in procedures like:
· Intrathecal administration of antispasticity drugs, beta interferons in demyelination, opiates in intractable pain etc.,
· EMG-guided Botox therapy for dystonia,
· Subcutaneous administration of antimigraine and antiparkinsonian drugs,
- Intraarterial thrombolysis in extended windows of thrombolysis in ischemic strokes,
- Transcranial Ultrasound clot-bust intervention in a registry in acute stroke care unit,
- Planning in deep brain stimulation therapy in uncontrolled dyskinesias and on-off phenomena in long standing Parkinsonism,
· Planning in vagal nerve stimulation in intractable epilepsy.
PAPER IV:
RECENT ADVANCES IN NEUROLOGY:
ADVANCES IN NEUROIMAGING TECHNIQUES, BIONICS IN NEURAL PROSTHESIS and REHABILITATION, NEUROPROTEOMICS and NEUROGENETICS, STEM CELL and GENE THERAPY
ADVANCES IN NEUROIMAGING TECHNIQUES:
· Integration of CT, MR, SPECT, and PET images with each other and with EEG.
- EVOKED potentials-based brain maps in structural and functional localization in neurological phenomena and diseases.
- DSA interpretation and diagnosis.
BIONICS IN NEURAL PROSTHESIS AND REHABILITATION:
· Advanced techniques in neuro-rehabilitation such as TENS, principles of man-machine interphase devices in cord, nerve and plexus injuries, cochlear implants, artificial vision.
NEUROPROTEOMICS AND NEUROGENETICS:
Brain functions are regulated by proteomics and genomics linked to various proteins and genes relevant to the brain, the body’s maximum number of proteins and genes being expressed in brain as neurotransmitters or channel proteins and predisposing the brain to a number of disorders of abnormal functioning of these proteins.
STEM CELL AND GENE THERAPY:
· Principles of ongoing experiments on stem cell therapy for nervous system disorders such as foetal brain tissue transplants in parkinsonism; intrathecal marrow transplants in MND,MS, and Spinal trauma; myoblasts infusion therapy in dystrophies.
NEUROEPIDEMIOLOGICAL STUDIES AND CLINICAL TRIALS:
The students of the DM course will be trained in conducting sound Neuro-epidemiology studies on regionally and nationally important neurological conditions as well as on diseases of scientific and research interest to the department. They will also be trained in the principles of clinical trials.
Essential Practical Knowledge
1. Online certification in Research Methodology Course
- 2. Certification of NIHSS, MRS, mBI, EDSS
- 3. Interpretation of acute stroke imaging
- 4. Performance of cerebral angiography and interpretation of DSA
- 5. Performance of TCD
- 6. Performance and interpretation of electrophysiological tests
Career Options
After completing a DM in Neurology, candidates will get employment
opportunities in Government and the Private sector.
In the Government sector, candidates have various options to choose from
which include Registrar, Senior Resident, Demonstrator, Tutor, etc.
While in the Private sector, the options include Resident Doctor,
Consultant, Visiting Consultant (Neurology), Junior Consultant, Senior
Consultant (Neurology), and Neurology Specialist.
Courses After DM in Neurology Course
DM in Neurology is a specialization course that can be pursued after
finishing a Postgraduate medical course. After pursuing a specialization in DM in
Neurology, a candidate could also pursue certificate courses and Fellowship
programmes recognized by NMC and NBE, where DM in Neurology is a feeder
qualification.
Frequently Asked Questions (FAQs) –DM in Neurology Course
- Question: What is the
full form of DM?
Answer: The full form
of DM is a Doctorate of Medicine.
- Question: What is a DM
in Neurology?
Answer: DM Neurology
or Doctorate of Medicine in Neurology also known as DM in Neurology is a super
specialty level course for doctors in India that they do after
completion of their postgraduate medical
degree course.
- Question: What is the
duration of a DM in Neurology?
Answer: DM in Neurology
is a super speciality programme of three years.
- Question: What is the
eligibility of a DM in Neurology?
Answer:
The candidate must have a postgraduate medical Degree in MD/DNB (General Medicine) or MD/DNB
(Paediatrics) obtained from any college/university recognized
by the Medical Council of India (Now NMC)/NBE, this feeder qualification
mentioned here is as of 2022. For any further changes to the prerequisite
requirement please refer to the NBE website.
- Question: What is the
scope of a DM in Neurology?
Answer: DM in Neurology
offers candidates various employment opportunities and career prospects.
- Question: What is the
average salary for a DM in Neurology candidate?
Answer: The DM in Neurology
candidate's average salary is between Rs. 30 lakhs to Rs. 60 lakhs per year
depending on the experience.
- Question: Can you
teach after completing DM Course?
Answer: Yes, the candidate
can teach in a medical college/hospital after completing the DM course.
2 years 5 months ago
News,Health news,NMC News,Medical Education,Medical Colleges News,Medical Courses News,Medical Universities News,Medical Admission News,Latest Medical Education News,Medical Courses
Jamaican fruit bat's response to SARS-CoV-2 adapted to human
In a recent study posted to the bioRxiv* server, researchers examined the vulnerability of Jamaican fruit bats (Artibeus jamaicensis) to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
In a recent study posted to the bioRxiv* server, researchers examined the vulnerability of Jamaican fruit bats (Artibeus jamaicensis) to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
2 years 5 months ago