Alarmante desafío de salud: venden opioides mezclados con tranquizilantes para animales en barrio de Philadelphia
Muchas personas del barrio de Kensington, en Philadelphia —el mayor mercado abierto de drogas al aire libre de la costa este— son adictas y aspiran, fuman o se inyectan al aire libre, encorvadas sobre cajas o en los escalones de las casas. A veces es difícil saber si están vivos o muertos. Las jeringuillas ensucian las aceras y el hedor de la orina inunda el aire.
Las aflicciones del barrio se remontan a principios de los años 70, cuando la industria desapareció y el tráfico de drogas se afianzó. Con cada nueva oleada de drogas, la situación se agrava. Ahora está peor que nunca. Ahora, con la llegada de la xilacina, un tranquilizante de uso veterinario, nuevas complicaciones están sobrecargando un sistema ya desbordado.
“Hay que poner manos a la obra”, dijo Dave Malloy, un veterano trabajador social de Philadelphia que trabaja en Kensington y otros lugares de la ciudad.
Los traficantes utilizan xilacina, un sedante barato no autorizado, para cortar el fentanilo, un opioide sintético 50 veces más potente que la heroína. El nombre callejero de la xilacina es “tranq”, y el fentanilo cortado con xilacina se llama “tranq dope”.
La xilacina lleva una década diseminándose por el país, según la Agencia Antidroga (DEA). Su aparición ha seguido la ruta del fentanilo: empezando en los mercados de heroína en polvo blanco del noreste y desplazándose después hacia el sur y el oeste.
Además, ha demostrado ser fácil de fabricar, vender y transportar en grandes cantidades para los narcotraficantes extranjeros, que acaban introduciéndola en Estados Unidos, donde circula a menudo en paquetes de correo exprés.
La xilacina se detectó por primera vez en Philadelphia en 2006. En 2021 se encontró en el 90% de las muestras de opioides callejeros. En ese año, el 44% de todas las muertes por sobredosis no intencionales relacionadas con el fentanilo incluyeron xilacina, según estadísticas de la ciudad. Dado que los procedimientos de análisis durante las autopsias varían mucho de un estado a otro, no hay datos exhaustivos sobre las muertes por sobredosis con xilacina a nivel nacional, según la DEA.
Aquí en Kensington, los resultados están a la vista. Usuarios demacrados caminan por las calles con heridas necróticas en piernas, brazos y manos, que a veces llegan al hueso.
La vasoconstricción que provoca la xilacina y las condiciones antihigiénicas dificultan la cicatrización de cualquier herida, y mucho más de las úlceras graves provocadas por la xilacina, explicó Silvana Mazzella, directora ejecutiva de Prevention Point Philadelphia, un grupo que ofrece servicios conocidos como “reducción del daño”.
Stephanie Klipp, enfermera que se dedica al cuidado de heridas y a la reducción de daños en Kensington, dijo que ha visto a personas “viviendo literalmente con lo que les queda de sus extremidades, con lo que obviamente debería ser amputado”.
El papel que desempeña la xilacina en las sobredosis mortales pone de relieve uno de sus atributos más complicados. Al ser un depresor del sistema nervioso central, la naloxona no funciona cuando se trata de un sedante.
Aunque la naloxona puede revertir el opioide de una sobredosis de “tranq dope”, alguien debe iniciar la respiración artificial hasta que lleguen los servicios de emergencia o la persona consiga llegar a un hospital, cosa que a menudo no ocurre. “Tenemos que mantener a las personas con vida el tiempo suficiente para tratarlas, y eso aquí es diferente cada día”, explicó Klipp.
Si un paciente llega al hospital, el siguiente paso es tratar el síndrome de abstinencia agudo de “tranq dope”, que es algo delicado. Apenas existen estudios sobre cómo actúa la xilacina en humanos.
Melanie Beddis vivió con su adicción dentro y fuera de las calles de Kensington durante unos cinco años. Recuerda el ciclo de desintoxicación de la heroína. Fue horrible, pero después de unos tres días de dolores, escalofríos y vómitos, podía “retener la comida y posiblemente dormir”. Con la “tranq dope” fue peor. Cuando intentó dejar esa mezcla en la cárcel, no pudo comer ni dormir durante unas tres semanas.
Las personas que se desintoxican de la “tranq dope” necesitan más medicamentos, explicó Beddis, ahora en recuperación, quien ahora es directora de programas de Savage Sisters Recovery, que ofrece alojamiento, asistencia y reducción de daños en Kensington.
“Necesitamos una receta que sea eficaz”, señaló Jeanmarie Perrone, médica y directora fundadora del Centro de Medicina de Adicciones de Penn Medicine.
Perrone dijo que primero trata la abstinencia de opioides, y luego, si un paciente sigue experimentando malestar, a menudo utiliza clonidina, un medicamento para la presión arterial que también funciona para la ansiedad. Otros médicos han probado distintos fármacos, como la gabapentina, un medicamento anticonvulsivo, o la metadona.
“Es necesario que haya más diálogo sobre lo que funciona y lo que no, y que se ajuste en tiempo real”, afirmó Malloy.
Philadelphia ha anunciado recientemente que va a poner en marcha un servicio móvil de atención de heridas como parte de su plan de gastos de los fondos del acuerdo sobre opioides, con la esperanza de que esto ayude al problema de la xilacina.
Lo mejor que pueden hacer los especialistas en las calles es limpiar y vendar las úlceras, proporcionar suministros, aconsejar a la gente que no se inyecte en las heridas y recomendar tratamiento en centros médicos, explicó Klipp, que no cree que un hospital pueda ofrecer a sus pacientes un tratamiento adecuado contra el dolor. Muchas personas no pueden quebrar el ciclo de la adicción y no hacen seguimiento.
Mientras que la heroína solía dar un margen de 6-8 horas antes de necesitar otra dosis, la “tranq dope” solo da 3-4 horas, estimó Malloy. “Es la principal causa de que la gente no reciba la atención médica adecuada”, añadió. “No pueden estar el tiempo suficiente en urgencias”.
Además, aunque las úlceras resultantes suelen ser muy dolorosas, los médicos son reacios a dar a los usuarios analgésicos fuertes. “Muchos médicos ven eso como que buscan medicación en lugar de lo que está pasando la gente”, dijo Beddis.
Por su parte, Jerry Daley, director ejecutivo de la sección local de un programa de subvenciones gestionado por la Oficina de Política Nacional de Control de Drogas (ONDCP), dijo que los funcionarios de salud y las fuerzas del orden deben comenzar a tomar medidas enérgicas contra la cadena de suministro de xilacina y transmitir el mensaje de que las empresas deshonestas que la fabrican están “literalmente beneficiándose de la vida y las extremidades de las personas”.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
USE OUR CONTENT
This story can be republished for free (details).
2 years 5 months ago
Noticias En Español, Pharmaceuticals, Public Health, Disparities, Homeless, Opioids, Pennsylvania, Prescription Drugs
PAHO/WHO | Pan American Health Organization
La OPS brinda orientaciones a los países de las Américas ante el aumento de casos de chikunguña
PAHO provides guidance to countries in response to increased chikungunya cases
Cristina Mitchell
15 Feb 2023
PAHO provides guidance to countries in response to increased chikungunya cases
Cristina Mitchell
15 Feb 2023
2 years 5 months ago
PAHO/WHO | Pan American Health Organization
Fourth meeting of the International Health Regulations (2005) (IHR) Emergency Committee on the Multi-Country Outbreak of monkeypox (mpox)
Fourth meeting of the International Health Regulations (2005) (IHR) Emergency Committee on the Multi-Country Outbreak of monkeypox (mpox)
Cristina Mitchell
15 Feb 2023
Fourth meeting of the International Health Regulations (2005) (IHR) Emergency Committee on the Multi-Country Outbreak of monkeypox (mpox)
Cristina Mitchell
15 Feb 2023
2 years 5 months ago
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Achieving very low LDL-C tied to lower risk of MI, stroke, and death with no safety concerns: FOURIER-OLE analysis
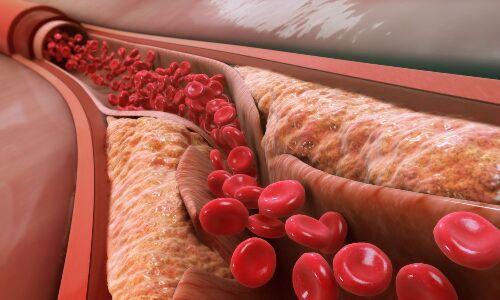
USA: Long-term achievement of lower LDL-C levels, down to <20 mg/dL, is associated with a reduced risk of cardiovascular (CV) outcomes and no safety concerns in patients with atherosclerotic cardiovascular disease, according to an analysis of FOURIER-OLE. The study appeared in the journal Circulation on Feb 13 2023.
USA: Long-term achievement of lower LDL-C levels, down to <20 mg/dL, is associated with a reduced risk of cardiovascular (CV) outcomes and no safety concerns in patients with atherosclerotic cardiovascular disease, according to an analysis of FOURIER-OLE. The study appeared in the journal Circulation on Feb 13 2023.
LDL-C (low-density lipoprotein cholesterol) is a well-known risk factor for atherosclerotic cardiovascular disease. However, there is no information on the optimal achieved LDL-C level concerning safety and efficacy in the long term.
FOURIER (Further Cardiovascular Outcomes Research With PCSK9 Inhibition in Subjects With Elevated Risk) comprised 27 564 patients with stable atherosclerotic cardiovascular disease. They were randomized to evolocumab or placebo and followed for a median of 2.2 years. In FOURIER-OLE, the open-label extension, 6635 patients transitioned to open-label evolocumab irrespective of initial treatment allocation in the parent trial and were followed for an additional five years.
Prakriti Gaba from Brigham and Women's Hospital and Harvard Medical School in Boston, MA, and colleagues examined the relationship between achieved LDL-C levels, defined as an average of the first two measured LDL-C levels, in FOURIER-OLE (in 6559 patients) and the incidence of subsequent CV and safety outcomes. Sensitivity analyses were also performed to evaluate cardiovascular and safety effects in the whole FOURIER-OLE and FOURIER patient population.
The study led to the following findings:
· In FOURIER-OLE, 40%, 24%, 16%, 12%, and 7% patients achieved LDL-cholesterol levels of 20 to <40, <20, 40 to <55, ≥70, and 55 to <70 mg/dL, respectively.
· The team observed a monotonic relationship between lower achieved LDL-C levels—down to very low levels <20 mg/dL—and a lower risk of the primary efficacy endpoint (composite of myocardial infarction, cardiovascular death, stroke, or hospitalization for unstable angina or coronary revascularization) and the key secondary efficacy endpoint (composite of myocardial infarction, cardiovascular death, or stroke) that persisted after multivariable adjustment.
· No statistically significant associations were found between lower achieved levels of LDL-C and increased risk of the safety outcomes (new or recurrent cancer, serious adverse events, hemorrhagic stroke, cataract-related adverse events, neurocognitive adverse events, new-onset diabetes, muscle-related events, or noncardiovascular death) in the primary analyses.
· Similar findings were seen in the whole FOURIER-OLE and FOURIER cohort up to a maximum follow-up of 8.6 years.
To conclude, long-term achievement of lower LDL-cholesterol levels down to <20 mg/dL was linked with a lower risk of CV outcomes and no notable safety concerns in patients with cardiovascular disease.
Reference:
Gaba P, O'Donoghue ML, Park JG, Wiviott SD, Atar D, Kuder JF, Im K, Murphy SA, De Ferrari GM, Gaciong ZA, Toth K, Gouni-Berthold I, Lopez-Miranda J, Schiele F, Mach F, Flores-Arredondo JH, López JAG, Elliott-Davey M, Wang B, Monsalvo ML, Abbasi S, Giugliano RP, Sabatine MS. Association Between Achieved Low-Density Lipoprotein Cholesterol Levels and Long-Term Cardiovascular and Safety Outcomes: An Analysis of FOURIER-OLE. Circulation. 2023 Feb 13. doi: 10.1161/CIRCULATIONAHA.122.063399. Epub ahead of print. PMID: 36779348.
2 years 5 months ago
Cardiology-CTVS,Cardiology & CTVS News,Top Medical News
Isolation of Burkholderia thailandensis from the environment
A new study in Emerging Infectious Diseases aimed to detect and isolate B. thailandensis from water and soil samples collected from Puerto Rico between December 2018 and March 2020 as well as Texas between November 2019 to November 2020.
A new study in Emerging Infectious Diseases aimed to detect and isolate B. thailandensis from water and soil samples collected from Puerto Rico between December 2018 and March 2020 as well as Texas between November 2019 to November 2020.
2 years 5 months ago
AAP's new childhood obesity guidance worries eating disorder specialists - NPR
- AAP's new childhood obesity guidance worries eating disorder specialists NPR
- Wellness Watch: Understanding The New Guidelines For Treating Childhood Obesity News On 6/KOTV
- New childhood obesity guidance raises worries over the risk of eating disorders Wisconsin Public Radio
- Dr. Amin offers recommendations to tackle obesity in kids KGET News
- View Full Coverage on Google News
2 years 5 months ago
AAP's new childhood obesity guidance worries eating disorder specialists - NPR
- AAP's new childhood obesity guidance worries eating disorder specialists NPR
- Dr. Amin offers recommendations to tackle obesity in kids KGET News
- New childhood obesity guidance raises worries over the risk of eating disorders Wisconsin Public Radio
- Wellness Watch: Understanding The New Guidelines For Treating Childhood Obesity News On 6/KOTV
- New U.S. childhood obesity guidelines recommend surgery, drugs CBC News: The National
2 years 5 months ago
As Opioids Mixed With Animal Tranquilizers Arrive in Kensington, So Do Alarming Health Challenges
Many people living on the streets in Philadelphia’s Kensington neighborhood — the largest open-air drug market on the East Coast — are in full-blown addiction, openly snorting, smoking, or injecting illicit drugs, hunched over crates or on stoops. Syringes litter sidewalks, and the stench of urine fouls the air.
The neighborhood’s afflictions date to the early 1970s, when industry left and the drug trade took hold. With each new wave of drugs, the situation grows grimmer. Now, with the arrival of xylazine, a veterinary tranquilizer, new complications are burdening an already overtaxed system.
“It’s all hands on deck,” said Dave Malloy, a longtime Philadelphia social worker who does mobile outreach in Kensington and around the city.
Dealers are using xylazine, which is uncontrolled by the federal government and cheap, to cut fentanyl, a synthetic opioid up to 50 times stronger than heroin. The street name for xylazine is “tranq,” and fentanyl cut with xylazine is “tranq dope.” Mixed with the narcotic, xylazine amplifies and extends the high of fentanyl or heroin.
But it also has dire health effects: It leaves users with unhealing necrotic ulcers, because xylazine restricts blood flow through skin tissue. Also, since xylazine is a sedative rather than a narcotic, overdoses of tranq dope do not respond as well to the usual antidote — naloxone — which reverses the effects of only the latter.
Xylazine has been spreading across the country for at least a decade, according to the Drug Enforcement Administration, starting in the Northeast and then moving south and west. Plus, it has proven to be easy for offshore bad actors to manufacture, sell, and ship in large quantities, eventually getting it into the U.S., where it often circulates by express delivery.
First detected in Philadelphia in 2006, xylazine was found in 90% of street opioid samples in the city by 2021. That year, 44% of all unintentional fentanyl-related overdose deaths involved xylazine, city statistics show. Since testing procedures during postmortems vary widely from state to state, no comprehensive data for xylazine-positive overdose deaths nationally exists, according to the DEA.
Here in Kensington, the results are on display. Emaciated users walk the streets with necrotic wounds on their legs, arms, and hands, sometimes reaching the bone.
Efforts to treat these ulcers are complicated by the narrowing of blood vessels that xylazine causes as well as dehydration and the unhygienic living conditions that many users experience while living homeless, said Silvana Mazzella, associate executive officer of the public health nonprofit Prevention Point Philadelphia, a group that provides services known as harm reduction.
Stephanie Klipp, a nurse who does wound care and is active in harm reduction efforts in Kensington, said she has seen people “literally living with what’s left of their limbs — with what obviously should be amputated.”
Fatal overdoses are rising because of xylazine’s resistance to naloxone. When breathing is suppressed by a sedative, the treatment is CPR and transfer to a hospital to be put on a ventilator. “We have to keep people alive long enough to treat them, and that looks different every day here,” Klipp said.
If a patient reaches the hospital, the focus becomes managing acute withdrawal from tranq dope, which is dicey. Little to no research exists on how xylazine acts in humans.
Melanie Beddis lived with her addiction on and off the streets in Kensington for about five years. She remembers the cycle of detoxing from heroin cold turkey. It was awful, but usually, after about three days of aches, chills, and vomiting, she could “hold down food and possibly sleep.” Tranq dope upped that ante, said Beddis, now director of programs for Savage Sisters Recovery, which offers housing, outreach, and harm reduction in Kensington.
She recalled that when she tried to kick this mix in jail, she couldn’t eat or sleep for about three weeks.
There is no clear formula for what works to aid detoxing from opiates mixed with xylazine.
“We do need a recipe that’s effective,” said Dr. Jeanmarie Perrone, founding director of the Penn Medicine Center for Addiction Medicine and Policy.
Perrone said she treats opioid withdrawal first, and then, if a patient is still uncomfortable, she often uses clonidine, a blood pressure medication that also lessens anxiety. Other doctors have tried gabapentin, an anticonvulsant medication sometimes used for anxiety.
Methadone, a medication for opioid use disorder, which blunts the effects of opioids and can be used for pain management, seems to help people in tranq dope withdrawal, too.
In the hospital, after stabilizing a patient, caring for xylazine wounds may take priority. This can range from cleaning, or debridement, to antibiotic treatment — sometimes intravenously for periods as long as weeks — to amputation.
Philadelphia recently announced it is launching mobile wound care as part of its spending plan for opioid settlement funds, hopeful that this will help the xylazine problem.
The best wound care that specialists on the street can do is clean and bandage ulcers, provide supplies, advise people not to inject into wounds, and recommend treatment in medical settings, said Klipp. But many people are lost in the cycle of addiction and don’t follow through.
While heroin has a six- to eight-hour window before the user needs another hit, tranq dope wanes in just three or four, Malloy estimated. “It’s the main driver why people don’t get the proper medical care,” he said. “They can’t sit long enough in the ER.”
Also, while the resulting ulcers are typically severely painful, doctors are reluctant to give users strong pain meds. “A lot of docs see that as med-seeking rather than what people are going through,” Beddis said.
In the meantime, Jerry Daley, executive director of the local chapter of a grant program run by the Office of National Drug Control Policy, said health officials and law enforcement need to start cracking down on the xylazine supply chain and driving home the message that rogue companies that make xylazine are “literally profiting off of people’s life and limb.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
USE OUR CONTENT
This story can be republished for free (details).
2 years 5 months ago
Pharmaceuticals, Public Health, Disparities, Homeless, Opioids, Pennsylvania, Prescription Drugs
Major advances in brain surgery
When you hear about advancements in brain surgery, it’s often a report of a new technology, surgical approach, or technique. But just as important are new ways of thinking that lead to shifts in how patients are cared for. Neurosurgery is the...
When you hear about advancements in brain surgery, it’s often a report of a new technology, surgical approach, or technique. But just as important are new ways of thinking that lead to shifts in how patients are cared for. Neurosurgery is the...
2 years 5 months ago
Health & Wellness | Toronto Caribbean Newspaper
Choosing to prioritize pleasure and play is a form of taking your power back and realigning with your inner child
BY AKUA GARCIA Greetings Gems! I pray this cosmic conversation finds you well. We are currently lingering in the Full Moon in Leo energy. As we have discussed before Full Moon’s show us the fullness of our intentions and provides the opportunity to release what no longer serves us. Under the illumination of this Full […]
2 years 5 months ago
Spirituality, #LatestPost
When do you need a neurosurgeon?
Most people think of neurosurgery as brain surgery, but it is much more. It is the medical specialty concerned with the diagnosis and treatment of patients with injury to, or diseases and disorders of, the brain, spinal cord and spinal column, and...
Most people think of neurosurgery as brain surgery, but it is much more. It is the medical specialty concerned with the diagnosis and treatment of patients with injury to, or diseases and disorders of, the brain, spinal cord and spinal column, and...
2 years 5 months ago
PAHO/WHO | Pan American Health Organization
PAHO launches campaign to raise awareness of childhood cancer in Latin America and the Caribbean
PAHO launches campaign to raise awareness of childhood cancer in Latin America and the Caribbean
Cristina Mitchell
14 Feb 2023
PAHO launches campaign to raise awareness of childhood cancer in Latin America and the Caribbean
Cristina Mitchell
14 Feb 2023
2 years 5 months ago
Automated Feeding Platform to Study Mosquito Disease Transmission
A team at Rice University has developed an automated feeding platform for mosquitoes that allows researchers to test different types of repellent and investigate mosquito-borne disease transmission. Traditionally, such mosquito research would require human volunteers or animal subjects for the mosquitos to feed on, but this is obviously inconvenient and a little distasteful. This new system dispenses with the need for human volunteers and associated laborious data collection and analysis. The technology consists of 3D printed synthetic skin with real blood that flows through small vessels. Mosquitos can feed through the skin and are kept in place in a surrounding box, which also contains mounted cameras that record the whole process. Machine learning algorithms then interpret the resulting video footage, providing a variety of data including bite number and duration.
Dengue, yellow fever, and malaria: what do they all have in common? The pesky mosquito. However, while this flying culprit is well known, studying the process of disease transmission in detail and developing new ways to deter mosquitos from biting in the first place can be difficult. At present, many researchers are forced to use animal subjects or human volunteers who are willing to sit for long periods while mosquitoes feast on their blood. This is clearly not ideal, and requires long periods of observation and data analysis.
To address these limitations, these researchers have created a synthetic and automated alternative. This consists of 3D printed hydrogel constructs that act as synthetic skin. These structures contain artificial blood vessels through which the researchers can circulate real human blood. A transparent box around the hydrogel patches keeps live mosquitos in place above, allowing them to land and feed. Cameras mounted in the box record the activity, and then the researchers use machine learning algorithms to analyze the footage.
“It provides a consistent and controlled method of observation,” said Omid Veiseh, a researcher involved in the study. “The hope is researchers will be able to use that to identify ways to prevent the spread of disease in the future.”
So far, the researchers have used the device to test various mosquito repellents, but the technology could also let researchers to investigate mosquito-mediated disease transmission in more detail. “We are using the system to examine virus transmission during blood feeding,” said Dawn Wesson, another researcher involved in the study. “We are interested both in how viruses get taken up by uninfected mosquitoes and how viruses get deposited, along with saliva, by infected mosquitoes. If we had a better understanding of the fine mechanics and proteins and other molecules that are involved, we might be able to develop some means of interfering in those processes.”
See a video about the device below:
Study in journal Frontiers in Bioengineering and Biotechnology: Development of an automated biomaterial platform to study mosquito feeding behavior
Via: Rice University
2 years 5 months ago
Medicine, Public Health, riceuniversity
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Indian Immunologicals launches its first set of virtual medical representatives
Hyderabad: The healthcare sector in India is leaping forward with digital innovations at an accelerated pace. Government of India's initiatives like the National Digital Health Mission, integration of artificial intelligence, data governance, and 5G services fuelling a rapid paradigm shift in the healthcare industry which is already on the threshold of a new era of digital transformation.
The Covid-19 pandemic primed the evolution of healthcare business models by channelizing novel digital concepts and strategies. Indian Immunologicals Limited (IIL) the Hyderabad-based subsidiary of the National Dairy Development Board (NDDB) has been at the forefront of business process innovation. Propelling the digital ecosystem, IIL, through its division Human Biologicals Institute, launched its first set of virtual medical representatives, a pioneering alternative to facilitate physician's interface in form of eMOz i.e. A virtual realm where e-reps can connect with doctors and foster digital relationships.
Traditional sales models in the pharma industry have been primarily indexed on engagement between sales representatives and physicians which has led to volume-based formulae, more sales representatives equal more visits to doctors, assuming incremental business. However, long have the industry embraced the challenge that the average time spent by physicians with a sales rep has seen a drastic downturn owing to various intersecting factors. The COVID-19 pandemic caused further restrictions that significantly curtailed reps' access to physicians.eMOZ is a cutting-edge and promising tool for information sharing. eMOz has inbuilt capabilities to provide constant updates on the specific needs of the physicians, thus fostering meaningful, tangible, and enduring gains. eMOz will enable complete stakeholder management on a virtual platform by providing detailed access to products and services. This will reduce several entry barriers while enhancing cost efficiency. eMOz will eventually be acquiring AI avatars of sales representatives to interact and assist physicians in one of its kind experiences. eMOz will provide credible solutions digitally for better patient care by offering greater convenience to physicians and saving their precious time.Speaking on the launch of eMOz, Dr K. Anand Kumar, Managing Director of IIL said "This generation of healthcare professionals are quite open for digital channels of communication, and we envision providing an engaging digital experience to our customers while focussing foremost on covering untapped markets".On the ground level, unveiling eMOz has witnessed significant interest from doctors. Dr Santosh Kumar Mishra, Senior Obstetric & Gynaecologist from Sanjita Maternity Care & Hospital, Bhubaneswar (Odisha) who interacted through eMOz and placed an order as well, said "There has been a huge emergence of various digital channels in our life post-pandemic, experiencing something like eMOz from Indian Immunologicals Limited is unique & interesting. It is more convenient than some of the usual drop-in interactions."While in-person rep visits still hold value, eMOz avatars will accentuate digital value perception among all stakeholders", Vice President, Human Health business, Shakul Srivastava said.
2 years 5 months ago
News,Industry,Pharma News,Latest Industry News
Health & Wellness | Toronto Caribbean Newspaper
Best vegan restaurants to try in Toronto for spring and summer 2023
BY RACHEL MARY RILEY Some of us know that life is short. But what is life without time-to-time enjoyment. Before you know we arrive at spring and summer. You shouldn’t even wait until spring and summer to grab a special meal as a treat, especially if you are on the way to losing weight and […]
The post Best vegan restaurants to try in Toronto for spring and summer 2023 first appeared on Toronto Caribbean Newspaper.
2 years 5 months ago
Fitness, #LatestPost
3D Bioengineered Skin Grafts Fit Complex Anatomy
Researchers at Columbia University’s Irving Medical Center have developed a method to create three-dimensional bioengineered skin grafts. To date, bioengineered skin is typically created in flat sheets. However, these are difficult to fit to complex anatomy, such as the hand, and so these researchers have designed a more sophisticated technique that combines laser scanning, 3D printing, and cell culture to create seamless three dimensional skin grafts. For instance, the researchers have already created a skin “glove” that could be useful in replacing skin on the hands by simply slipping it over the hand (just like a glove).
Replacing skin that has been damaged is a challenge. Traditional skin grafts require skin to be harvested elsewhere before application to the damaged area, which obviously isn’t ideal. Researchers have been developing bioengineered skin by combining human cells with biomaterials, but so far these constructs tended to be simple sheets which are not easy to cut and firmly affix to our undulating anatomy.
To address this, the Columbia researchers have developed a technique that can create three dimensional constructs that more closely resemble clothing that can simply be pulled on over damaged tissue. Aside from ease of application, the method requires the constructs to be designed for each situation, enabling personalized constructs that are perfectly tailored for each patient.
“Three-dimensional skin constructs that can be transplanted as ‘biological clothing’ would have many advantages,” said Hasan Erbil Abaci, a researcher involved in the study. “They would dramatically minimize the need for suturing, reduce the length of surgeries, and improve aesthetic outcomes.”
The approach involves laser scanning the area of the body onto which the graft will be applied – for instance, a burn injury that has damaged most of the skin on the hand. In this case, the patient’s hand would be scanned and then the researchers can use computer-aided design to create a template for a hollow glove-like construct. The next step involves 3D printing a biomaterial substrate in the required shape and then seeding it with connective tissue proteins, such as collagen, and skin fibroblasts that can secrete connective tissue components. The researchers then seed keratinocytes on the outside of the graft to form an epidermis layer.
After a culture period, the graft can be slipped onto the injured hand just like a glove. “We hypothesized that a 3D fully enclosed shape would more closely mimic our natural skin and be stronger mechanically, and that’s what we found,” said Abaci. “Simply remaining faithful to the continuous geometry of human skin significantly improves the composition, structure, and strength of the graft.”
Study in journal Science Advances: Engineering edgeless human skin with enhanced biomechanical properties
2 years 5 months ago
Materials, Plastic Surgery, Surgery, columbia, columbiauniversity, skin graft
FDA grants priority review to Linzess for functional constipation in children, teens
The FDA has granted priority review to a supplemental new drug application for Linzess for the treatment of functional constipation in patients aged 6 to17 years old, according to an Ironwood Pharmaceuticals press release.The company noted that the FDA has assigned the Linzess (linaclotide 72 mcg, AbbVie/Ironwood) application a Prescription Drug User Fee Act date of June 14, 2023 — approximatel
y 4 months earlier than the standard review cycle.“Pediatric functional constipation has a significant impact on young patients and their families, yet there are no FDA-approved prescription
2 years 5 months ago
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
DM Medical Gastroenterology: Admissions, Medical colleges, fees, eligibility criteria details
DM Medical Gastroenterology or Doctorate of Medicine in Medical
Gastroenterology also known as DM in Medical Gastroenterology is a super
specialty level course for doctors in India that is done by them after
completion of their postgraduate medical degree course. The duration of this
DM Medical Gastroenterology or Doctorate of Medicine in Medical
Gastroenterology also known as DM in Medical Gastroenterology is a super
specialty level course for doctors in India that is done by them after
completion of their postgraduate medical degree course. The duration of this
super specialty course is 3 years, and it deals with the diagnosis and treatment of human digestive system-related diseases and problems.
The course is a full-time course pursued at various recognized medical
colleges across the country. Some of the top medical colleges offering this
course include All India Institute of Medical Sciences, New Delhi, Jawaharlal
Institute of Postgraduate Medical Education & Research, Puducherry
(JIPMER), Postgraduate Institute of Medical Education & Research,
Chandigarh and more.
Admission to this course is done through the NEET-SS Entrance exam
conducted by the National Board of Examinations, followed by counselling based
on the scores of the exam that is conducted by DGHS/MCC/State Authorities.
The fee for pursuing DM (Medical Gastroenterology) varies from college
to college and may range from Rs. 10000 to Rs. 20 lakhs per year.
After completion of their respective course, doctors can either join the
job market or can pursue certificate courses and Fellowship programmes
recognized by NMC and NBE. Candidates can take reputed jobs at positions as
Senior residents, Consultants, etc. with an approximate salary range of Rs.6 lakhs to Rs. 60 lakhs per year depending upon their expertise.
What is DM in Medical Gastroenterology?
Doctorate of Medicine in Medical Gastroenterology, also known as DM (Medical
Gastroenterology) or DM in (Medical Gastroenterology) is a three-year super
speciality programme that candidates can pursue after completing the post-graduate
degree.
Medical Gastroenterology is the branch of medical science dealing with the diagnosis and treatment of human digestive system-related diseases and
problems.
Gastroenterology is the study of the normal function and diseases of the
oesophagus, stomach, small intestine, colon and rectum, pancreas, gallbladder,
bile ducts and liver.
The postgraduate students must gain ample knowledge and experience in
the diagnosis, and treatment of patients with acute, serious, and life-threatening
medical and surgical diseases.
PG education intends to create specialists who can contribute to
high-quality health care and advances in science through research and training.
The required training done by a postgraduate specialist in the field of Medical
Gastroenterology would help the specialist to recognize the health needs of the
community. The student should be competent to handle medical problems
effectively and should be aware of the recent advances in their speciality.
The candidate is also expected to know the principles of research
methodology and modes of the consulting library. The candidate should regularly
attend conferences, workshops and CMEs to upgrade her/ his knowledge.
Course Highlights
Here are some of the course highlights of DM in Medical Gastroenterology
Name of Course
DM in Medical
Gastroenterology
Level
Doctorate
Duration of Course
Three years
Course Mode
Full Time
Minimum Academic
Requirement
Candidates must have a postgraduate medical Degree in MD/DNB
(General Medicine) obtained from any college/university
recognized by the Medical Council of India (Now NMC)/NBE, this feeder
qualification mentioned here is as of 2022. For any further changes to the
prerequisite requirement please refer to the NBE website
Admission Process /
Entrance Process / Entrance Modalities
Entrance Exam
(NEET-SS)
INI CET for various
AIIMS, PGIMER Chandigarh, JIPMER Puducherry, NIMHANS Bengaluru
Counselling by
DGHS/MCC/State Authorities
Course Fees
Rs.10,000 to
Rs. 20 lakhs per year
Average Salary
Rs.6 lakhs to Rs. 60
lakhs per year
Eligibility Criteria
The eligibility criteria for DM in Medical Gastroenterology are defined
as the set of rules or minimum prerequisites that aspirants must meet in order
to be eligible for admission, which include:
Name of DM course
Course Type
Prior Eligibility Requirement
Medical
Gastroenterology
DM
MD/DNB (General Medicine)
Note:
· The feeder qualification for DM in Medical
Gastroenterology is defined by the NBE and is subject to
changes by the NBE.
· The feeder qualification mentioned here is as of
2022.
· For any changes, please refer to the NBE website.
· The candidate must have obtained permanent
registration of any State Medical Council to be eligible for admission.
· The medical college's recognition cut-off dates for
the Postgraduate Degree courses shall be as prescribed by the Medical Council
of India (now NMC).
Admission Process
- The admission process
contains a few steps to be followed in order by the candidates for
admission to DM in Medical Gastroenterology. Candidates can view the
complete admission process for DM in Medical Gastroenterology mentioned
below:
- The NEET-SS or National
Eligibility Entrance Test for Super speciality courses is a national-level
master's level examination conducted by the NBE for admission to
DM/MCh/DrNB Courses.
- Qualifying
Criteria-Candidates placed at the 50th percentile or above shall be
declared as qualified in the NEET-SS in their respective speciality.
- The following Medical
institutions are not covered under centralized admissions for DM/ MCh
courses through NEET-SS:
- AIIMS,
New Delhi and other AIIMS - PGIMER,
Chandigarh - JIPMER,
Puducherry - NIMHANS,
Bengaluru
- Candidates from all eligible
feeder speciality subjects shall be required to appear in the question
paper of the respective group if they are willing to opt for a super
speciality course in any of the super speciality courses covered in that
group.
- A candidate can opt for
appearing in the question papers of as many groups for which his/her
Postgraduate speciality qualification is an eligible feeder qualification.
- By appearing in the question
paper of a group and on qualifying for the examination, a candidate shall be
eligible to exercise his/her choices in the counselling only for those super speciality subjects covered in the said group for which his/ her broad
speciality is an eligible feeder qualification.
Fees Structure
The fee structure for DM in Medical Gastroenterology varies from college
to college. The fee is generally less for Government Institutes and more for
private institutes. The average fee structure for DM in Medical
Gastroenterology is around Rs. 10,000 to Rs. 20 lakhs per year.
Colleges offering DM in Medical Gastroenterology
There are various medical colleges across India that offer courses for
pursuing DM in (Medical Gastroenterology).
As per National Medical Commission (NMC) website, the following medical
colleges are offering DM in (Medical Gastroenterology) courses for the academic
year 2022-23.
Sl.No.
Course Name
State
Name and Address of
Medical College / Medical Institution
Management of College
1
DM - Medical Gastroenterology
Andhra Pradesh
Andhra Medical College, Visakhapatnam
Govt.
2
DM - Medical Gastroenterology
Andhra Pradesh
Guntur Medical College, Guntur
Govt.
3
DM - Medical Gastroenterology
Andhra Pradesh
Kurnool Medical College, Kurnool
Govt.
4
DM - Medical Gastroenterology
Andhra Pradesh
Narayana Medical College, Nellore
Trust
5
DM - Medical Gastroenterology
Assam
Gauhati Medical College, Guwahati
Govt.
6
DM - Medical Gastroenterology
Bihar
All India Institute of Medical Sciences, Patna
Govt.
7
DM - Medical Gastroenterology
Bihar
Indira Gandhi Institute of Medical
Sciences,Sheikhpura, Patna
Govt.
8
DM - Medical Gastroenterology
Chandigarh
Postgraduate Institute of Medical Education &
Research, Chandigarh
Govt.
9
DM - Medical Gastroenterology
Delhi
All India Institute of Medical Sciences, New
Delhi
Govt.
10
DM - Medical Gastroenterology
Delhi
G.B. Pant Institute of Postgraduate Medical
Education and Research, New Delhi
Govt.
11
DM - Medical Gastroenterology
Gujarat
Smt. N.H.L.Municipal Medical College, Ahmedabad
Govt.
12
DM - Medical Gastroenterology
Haryana
Maharishi Markandeshwar Institute Of Medical
Sciences & Research, Mullana, Ambala
Trust
13
DM - Medical Gastroenterology
Himachal Pradesh
Indira Gandhi Medical College, Shimla
Govt.
14
DM - Medical Gastroenterology
Jammu & Kashmir
Sher-I-Kashmir Instt. Of Medical Sciences,
Srinagar
Govt.
15
DM - Medical Gastroenterology
Karnataka
Jawaharlal Nehru Medical College, Belgaum
Trust
16
DM - Medical Gastroenterology
Karnataka
JSS Medical College, Mysore
Trust
17
DM - Medical Gastroenterology
Karnataka
M S Ramaiah Medical College, Bangalore
Trust
18
DM - Medical Gastroenterology
Karnataka
St. Johns Medical College, Bangalore
Trust
19
DM - Medical Gastroenterology
Karnataka
Kasturba Medical College, Manipal
Trust
20
DM - Medical Gastroenterology
Karnataka
Vydehi Institute Of Medical Sciences &
Research Centre, Bangalore
Trust
21
DM - Medical Gastroenterology
Kerala
Government Medical College, Kozhikode, Calicut
Govt.
22
DM - Medical Gastroenterology
Kerala
Medical College, Thiruvananthapuram
Govt.
23
DM - Medical Gastroenterology
Kerala
Government Medical College, Kottayam
Govt.
24
DM - Medical Gastroenterology
Kerala
Amrita School of Medicine, Elamkara, Kochi
Trust
25
DM - Medical Gastroenterology
Madhya Pradesh
Sri Aurobindo Medical College and Post Graduate
Institute, Indore
Trust
26
DM - Medical Gastroenterology
Maharashtra
Lokmanya Tilak Municipal Medical College, Sion,
Mumbai
Govt.
27
DM - Medical Gastroenterology
Maharashtra
Topiwala National Medical College, Mumbai
Govt.
28
DM - Medical Gastroenterology
Maharashtra
Seth GS Medical College, and KEM Hospital, Mumbai
Govt.
29
DM - Medical Gastroenterology
Maharashtra
Jawaharlal Nehru Medical College, Sawangi
(Meghe), Wardha
Trust
30
DM - Medical Gastroenterology
Maharashtra
Bharati Vidyapeeth University Medical College,
Pune
Trust
31
DM - Medical Gastroenterology
Maharashtra
Government Medical College, Nagpur
Govt.
32
DM - Medical Gastroenterology
Maharashtra
Tata Memorial Centre, Mumbai
Govt.
33
DM - Medical Gastroenterology
Orissa
All India Institute of Medical Sciences,
Bhubaneswar
Govt.
34
DM - Medical Gastroenterology
Orissa
Kalinga Institute of Medical Sciences,
Bhubaneswar
Trust
35
DM - Medical Gastroenterology
Orissa
Instt. Of Medical Sciences & SUM Hospital,
Bhubaneswar
Trust
36
DM - Medical Gastroenterology
Orissa
SCB Medical College, Cuttack
Govt.
37
DM - Medical Gastroenterology
Pondicherry
Jawaharlal Institute of Postgraduate Medical
Education & Research, Puducherry
Govt.
38
DM - Medical Gastroenterology
Punjab
Dayanand Medical College & Hospital, Ludhiana
Trust
39
DM - Medical Gastroenterology
Rajasthan
SMS Medical College, Jaipur
Govt.
40
DM - Medical Gastroenterology
Rajasthan
Jawaharlal Nehru Medical College, Ajmer
Govt.
41
DM - Medical Gastroenterology
Rajasthan
Mahatma Gandhi Medical College and Hospital,
Sitapur, Jaipur
Trust
42
DM - Medical Gastroenterology
Rajasthan
National Institute of Medical Science &
Research, Jaipur
Trust
43
DM - Medical Gastroenterology
Rajasthan
Mahatma Gandhi Medical College and Hospital,
Sitapur, Jaipur
Trust
44
DM - Medical Gastroenterology
Rajasthan
Dr SN Medical College, Jodhpur
Govt.
45
DM - Medical Gastroenterology
Tamil Nadu
Kilpauk Medical College, Chennai
Govt.
46
DM - Medical Gastroenterology
Tamil Nadu
Christian Medical College, Vellore
Trust
47
DM - Medical Gastroenterology
Tamil Nadu
Sri Ramachandra Medical College & Research
Institute, Chennai
Trust
48
DM - Medical Gastroenterology
Tamil Nadu
Madras Medical College, Chennai
Govt.
49
DM - Medical Gastroenterology
Tamil Nadu
Chettinad Hospital & Research Institute,
Kanchipuram
Trust
50
DM - Medical Gastroenterology
Tamil Nadu
Stanley Medical College, Chennai
Govt.
51
DM - Medical Gastroenterology
Tamil Nadu
Govt. Mohan Kumaramangalam Medical College,
Salem- 30
Govt.
52
DM - Medical Gastroenterology
Tamil Nadu
Thoothukudi Medical College, Thoothukudi
Govt.
53
DM - Medical Gastroenterology
Tamil Nadu
Tirunelveli Medical College,Tirunelveli
Govt.
54
DM - Medical Gastroenterology
Tamil Nadu
Madurai Medical College, Madurai
Govt.
55
DM - Medical Gastroenterology
Tamil Nadu
Coimbatore Medical College, Coimbatore
Govt.
56
DM - Medical Gastroenterology
Tamil Nadu
Meenakshi Medical College and Research Institute,
Enathur
Trust
57
DM - Medical Gastroenterology
Tamil Nadu
PSG Institute of Medical Sciences, Coimbatore
Trust
58
DM - Medical Gastroenterology
Telangana
Gandhi Medical College, Secunderabad
Govt.
59
DM - Medical Gastroenterology
Telangana
Osmania Medical College, Hyderabad
Govt.
60
DM - Medical Gastroenterology
Uttarakhand
All India Institute of Medical Sciences,
Rishikesh
Govt.
61
DM - Medical Gastroenterology
Uttar Pradesh
Sanjay Gandhi Postgraduate Institute of Medical
Sciences, Lucknow
Govt.
62
DM - Medical Gastroenterology
Uttar Pradesh
Institute of Medical Sciences, BHU, Varanasi
Govt.
63
DM - Medical Gastroenterology
Uttar Pradesh
King George Medical University, Lucknow
Govt.
64
DM - Medical Gastroenterology
Uttar Pradesh
Moti Lal Nehru Medical College, Allahabad
Govt.
65
DM - Medical Gastroenterology
West Bengal
Institute of Postgraduate Medical Education &
Research, Kolkata
Govt.
66
DM - Medical Gastroenterology
West Bengal
Govt. Medical College, Kolkata
Govt.
67
DM - Medical Gastroenterology
West Bengal
RG Kar Medical College, Kolkata
Govt.
Syllabus
DM in Medical Gastroenterology is a three years specialization course
that provides training in the stream of Medical Gastroenterology.
NMC till date as of (12/02/2023) has not defined a Competency-based
curriculum for DM Medical Gastroenterology. The syllabus of AIIMS below
provides a basic outline of what a DM Medical Gastroenterology
candidate has to undergo while training:
At this level of training, the insistence on a syllabus may not be
appropriate. Trainees should acquire an overall knowledge of Gastroenterology
by reading standard textbooks, monographs and peer-reviewed journals dealing
with Gastroenterology, Hepatology, Pancreatology and related Basic Sciences and
Epidemiology. A core syllabus is given below, but it does not purport to be either
comprehensive or restrictive. Furthermore, it is likely to change from time to
time.
Recommended Core Syllabus:
Basic Sciences
1. Immune system of the gastrointestinal tract (GIT) and its importance
in various GI disorders
2. Molecular biology in relation to GIT
3. Genetic diseases of the GIT and the liver
4. Gene therapy
5. GI tumours and tumour biology
6. Gastrointestinal hormones in health and diseases
7. Embryology of the gut, liver, pancreas and congenital anomalies
Miscellaneous
1. Upper and lower gastrointestinal bleeding
2. Gastrointestinal tuberculosis
3. HIV and the GIT, hepatobiliary and pancreatic systems
4. GIT and liver in systemic diseases
5. Cutaneous manifestations of GI diseases
6. Vascular diseases of the GIT
7. Gastrointestinal side effects of drugs especially NSAIDs
8. Gastro-intestinal symptoms physiology and interpretation
Nausea, vomiting
Pain abdomen
Diarrhoea
Constipation
Dysphagia
Jaundice
Esophagus
1. Basic anatomy, histology and physiology
2. Congenital anomalies
3. Motility of the oesophagus and motor disorders
4. Mechanism of deglutition and dysphasia
5. Approach to a patient with dysphasia
6. Gastro-esophageal reflux disease
7. Tumors of the oesophagus
8. Esophageal webs, membranes and diverticulum
9. Management of benign and malignant oesophagal strictures
10. Esophagus and systemic diseases
11. Infectious diseases of the oesophagus
12. Foreign bodies in the oesophagus and stomach
13. Esophageal perforation
14. Drug-induced esophagitis
Stomach
1. Anatomy, histology, functions
2. Physiology of acid and bicarbonate secretion in health and diseases
3. Defence mechanisms against acid and pepsin
4. Gastroduodenal motor function in health and diseases.
5. Gastritis (nonspecific and specific)
6. Helicobacter pylori infection
7. Peptic ulcer
8. Dyspepsia
9. Stress and stomach
10. Gastric hypersecretory states including Zollinger-Ellison syndrome
11. Ulcer complications and their management
12. Surgery for peptic ulcer
13. Post-gastrectomy complication
14. Bezoars
15. Tumors of the stomach
16. Diverticuli and hernia of the stomach
Small Intestine
1. Anatomy, blood supply, histology
2. Motility of the small intestine
3. Congenital anomalies
4. Normal absorption of the nutrients
5. Intestinal electrolyte absorption and secretion
6. Malabsorption syndromes
Pathophysiology, manifestations and approach
7. Celiac sprue
8. Infection-related diseases
a. Intestinal microflora in health and diseases
b. Tropical sprue
c. Whipple’s disease. Infectious diarrhoea and food poisoning
e. Parasitic diseases
9. Small intestinal ulcers
10. Short bowel syndrome and intestinal transplantation.
11. Eosinophilic gastroenteritis
12. Food allergies
13. Intestinal obstruction and pseudo-obstruction
14. Short bowel syndrome
15. Acute appendicitis
16. Malrotation of the gut
17. Bezoars
18. Management of diarrhoea
19. GI lymphomas
20. Small intestinal tumours
21. Small intestinal transplantation
Colon
1. Basic anatomy blood supply, histology and functions
2. Motility of the colon and disorders of motility
3. Congenital anomalies
4. Megacolon
5. Constipation
6. Colonic pseudo-obstruction
7. Fecal incontinence
8. Antibiotic-associated diarrhoea
9. Inflammatory bowel disease
a. Ulcerative colitis
b. Crohn’s disease
c. Indeterminate colitis
d. Ileostomies and its management
10. Diverticular disease of the colon
11. Radiation entero-colitis
12. Colonic polyps and polyposis syndromes
13. Malignant diseases of the colon
14. Other inflammatory diseases of the colon including
a. Solitary rectal ulcer syndrome
b. Diversion colitis
c. Collagenous and microscopic colitis
d. Non-specific ulcerations of the colon
e. Malakoplakia
f. Pneumatoses cystoids intestinalis
15. Hemorrhoids
16. Diseases of the anorectum
Pancreas
1. Anatomy, physiology, blood supply, developmental anomalies
2. Physiology of the pancreatic secretion
3. Pancreatic function tests
4. Acute pancreatitis
5. Recurrent acute pancreatitis
6. Chronic pancreatitis
7. Malignancies of the pancreas(Exocrine and endocrine)
8. Cystic fibrosis and other childhood disorders of the pancreas
9. Hereditary pancreatitis
10. Pancreatic transplantation
Biliary Tree
1. Anatomy, Physiology
2. Physiology of bile formation and excretion
3. Enterohepatic circulation
4. Bilirubin metabolism.
5. Approach to patients with jaundice
6. Gallstones, their complications, and management
7. Acute acalculous cholecystitis
8. Miscellaneous disorders of the gallbladder
9. Acute cholangitis
10. Benign biliary structure
11. Benign and malignant neoplasms of the biliary system.
12. Endoscopic management of biliary obstruction.
13. Motility and dysmotility of the biliary system and sphincter of Oddi
dysfunction
14. Congenital diseases of the biliary systems Liver
1. Anatomy, physiology, blood supply
2. Functions of the liver
3. Microcirculation of liver
4. Liver function tests
5. Portal hypertension
i. Extrahepatic portosplenic vein obstruction
ii. Non-cirrhotic portal fibrosis
iii. Cirrhosis
6. Acute viral hepatitis
7. Chronic hepatitis
8. Fulminant hepatic failure
9. Subacute hepatic failure
10. Cirrhosis of the liver
11. Ascites
12. Hepatorenal syndrome
13. Autoimmune liver disease
14. Metabolic liver disease
15. Sclerosing cholangitis- primary and secondary
16. Primary biliary cirrhosis
17. Hepatic venous outflow tract obstruction
18. Fibrocystic diseases of the liver
19. Wilson’s disease
20. Hemochromatosis
21. Liver in porphyria
22. Hepatic tumours
23. Infections of the liver
24. Liver in pregnancy
25. Liver in congestive heart failure
26. Liver biopsy
27. Liver transplantation and artificial liver support
Peritorium and Retroperitoneum
1. Ascites
2. Chronic peritonitis
3. Budd-Chiari syndrome
4. Malignant ascites
5. Diseases of the retroperitoneum Nutrition
1. Normal nutritional requirements
2. Assessment of nutritional status
3. Protein-energy malnutrition
4. Manifestations and management of nutritional deficiency and excess
5. Nutritional support in various GI disorders (malabsorption, acute and
chronic pancreatitis, inflammatory bowel disease)
Vascular Diseases of the GI Tract
GI Radiology
Reading and interpreting the common x-ray films including
X-ray films of the abdomen Barium studies, ultrasound
examination CT scans, MR scans and
angiography and ERCP films
GI Pathology
Reading and interpreting histological slides of common gastrointestinal
and liver diseases.
Endoscopic Training
Endoscopic training is an integral part of training in the super speciality
of gastroenterology. A trainee is supposed to have knowledge of instruments and
their application.
i. Endoscopes
ii. Accessories
iii. Sterilization of endoscopes and accessories
iv. Electrosurgical instrument
v. Keeping of endoscopes and accessories
Career Options
After completing a DM in Medical Gastroenterology, candidates will get
employment opportunities in Government as well as in the Private sector.
In the Government sector, candidates have various options to choose from
which include Registrar, Senior Resident, Demonstrator, Tutor, etc.
While in the Private sector, the options include Resident Doctor,
Consultant, Visiting Consultant (Medical Gastroenterology), Junior Consultant,
Senior Consultant (Medical Gastroenterology), and Medical Gastroenterology Specialist.
Courses After DM in Medical Gastroenterology Course
DM in Medical Gastroenterology is a specialization course that can be
pursued after finishing a Postgraduate medical course. After pursuing
specialization in DM in Medical Gastroenterology, a candidate could also pursue
certificate courses and Fellowship programmes recognized by NMC and NBE, where DM
in Medical Gastroenterology is a feeder qualification.
Frequently Asked Questions (FAQs) –DM in Medical Gastroenterology Course
- Question: What is the full form of DM?
Answer: The full form
of DM is a Doctorate of Medicine.
- Question: What is a DM in Medical Gastroenterology?
Answer: DM Medical
Gastroenterology or Doctorate of Medicine in Medical Gastroenterology also
known as DM in Medical Gastroenterology is a super specialty level course for
doctors in India that is done by them after completion of their postgraduate
medical degree course.
- Question: What is the duration of a DM in Medical Gastroenterology?
Answer: DM in Medical
Gastroenterology is a super-speciality programme of three years.
- Question: What is the eligibility of a DM in Medical Gastroenterology?
Answer: The
candidate must have a postgraduate medical Degree in MD/DNB (General Medicine)
obtained from any college/university recognized by the Medical Council of India
(Now NMC)/NBE, this feeder qualification mentioned here is as of 2022. For any further
changes to the prerequisite requirement please refer to the NBE website.
- Question: What is the scope of a DM in Medical Gastroenterology?
Answer: DM in Medical
Gastroenterology offers candidates various employment opportunities and career
prospects.
- Question: What is the average salary for a DM in Medical
Gastroenterology candidate?
Answer: The DM in Medical
Gastroenterology candidate's average salary is between Rs. 6 lakhs to Rs. 60
lakhs per year depending on the experience.
- Question: Can you teach after completing DM Course?
Answer: Yes, the candidate
can teach in a medical college/hospital after completing the DM course.
2 years 5 months ago
News,Health news,NMC News,Medical Education,Medical Colleges News,Medical Courses News,Medical Universities News,Medical Admission News,Latest Medical Education News,Medical Courses
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Weekly BIF as efficacious as degludec with lower incident hypoglycaemia in type 2 diabetes patients: Lancet
USA: Weekly basal insulin Fc (BIF) provided similar efficacy to degludec despite higher fasting glucose targets in the BIF groups, according to findings from a phase 2 study. Lower glucose variability and higher fasting glucose targets contribute to lower rates of hypoglycemia for BIF versus degludec.
The study's findings, published in The Lancet Diabetes & Endocrinology, support continued BIF development as a once-weekly insulin treatment for patients with diabetes.
The burden of daily basal insulin causes delays and hesitancy in initiating insulin therapy. Insulin efsitora alfa, or basal insulin Fc, designed for once-weekly administration, is a human IgG (immunoglobulin G) Fc domain. Juan Frias, Velocity Clinical Research, Los Angeles, CA, USA, and colleagues aimed to explore the efficacy and safety of BIF in type 2 diabetes patients treated previously with basal insulin in an open-label, randomized, phase 2, 32-week study.
The study was conducted across 44 sites in Puerto Rico, Mexico, and the USA, enrolling patients with type 2 diabetes. Adults aged ≥18 years treated with basal insulin and up to three oral antidiabetic medications were eligible. Patients were randomly assigned in the ratio of 1:1:1 to subcutaneous BIF -- BIF treatment group 1 (BIF-A1) or 2 (BIF-A2) or insulin degludec. Different fasting glucose targets were selected for the BIF-A1, BIF-A2, and degludec groups. Patients assigned to BIF received a one-time loading dose of 1·5–3 times their calculated weekly dose. The first weekly dose was administered one week after the loading dose.
The efficacy analysis set comprised data from all randomized study participants who received at least one dose of the study medication. Participants were analyzed as per the treatment they were assigned. Changes in HbA1c from baseline to week 32 were the primary measure of glycemic control for BIF. Also, BIF was compared with degludec.
The authors reported the following findings:
· 399 participants were enrolled between 2018 to 2020 and randomized; 135 to BIF-A1, 132 to BIF-A2, or 132 degludec; 51% were female, and 49% were male.
· 379 were analysed for the primary outcome (130 in BIF-A1; 125 in BIF-A2: n=125; 124 in degludec).
· Mean change in HbA1c from baseline to week 32 (primary outcome) was –0·6% for BIF-A1 and BIF-A2. Degludec achieved a change from a baseline of –0·7%.
· The pooled BIF analysis showed non-inferiority compared to degludec for the treatment difference in HbA1c (0·1%).
· In the BIF groups, the hypoglycaemia (≤3·9 mmol/L) event rates defined as hypoglycaemia events per patient per year were 25% lower versus the degludec group (treatment ratio BIF-A1 versus degludec was 0·75, and BIF-A2 versus degludec was 0·74).
· Basal insulin Fc was well tolerated; treatment-emergent adverse events were comparable across groups.
"Our findings support continued BIF development as a once-weekly insulin treatment for patients with diabetes," the researchers concluded.
Reference:
The study, "Safety and efficacy of once-weekly basal insulin Fc in people with type 2 diabetes previously treated with basal insulin: a multicentre, open-label, randomized, phase 2 study", was published in The Lancet Diabetes & Endocrinology. DOI: https://doi.org/10.1016/S2213-8587(22)00388-6
2 years 5 months ago
Diabetes and Endocrinology,Medicine,Diabetes and Endocrinology News,Medicine News,Top Medical News
Watch: Blockbuster drug Humira has new competition. Here’s why that matters
Humira has been the world’s best-selling medicine since it arrived on the market in 2002. Now, it is finally getting competition with the release of Amgen’s biosimilar drug, Amjevita.
Humira has been the world’s best-selling medicine since it arrived on the market in 2002. Now, it is finally getting competition with the release of Amgen’s biosimilar drug, Amjevita. Humira’s main patent expired in 2016, but a byzantine patent saga has kept other drugmakers from offering their own version of the monoclonal antibody used to treat conditions such as rheumatoid arthritis and Crohn’s disease.
In this video, STAT senior writer and Pharmalot columnist Ed Silverman breaks down the convoluted world of pharmacy benefit managers, formularies, and a legal maneuver called “patent thicketing” that controls how much patients pay for this beneficial treatment.
2 years 5 months ago
Pharma, Pharmalot, bioisimilars