KFF Health News' 'What the Health?': Trump’s Bill Reaches the Finish Line
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
Early Thursday afternoon, the House approved a budget reconciliation bill that not only would make permanent many of President Donald Trump’s 2017 tax cuts, but also impose deep cuts to Medicaid, the Affordable Care Act, and, indirectly, Medicare.
Meanwhile, those appointed by Health and Human Services Secretary Robert F. Kennedy Jr. to a key vaccine advisory panel used their first official meeting to cast doubt on a preservative that has been used in flu vaccines for decades — with studies showing no evidence of its harm in low doses.
This week’s panelists are Julie Rovner of KFF Health News, Alice Miranda Ollstein of Politico, Maya Goldman of Axios, and Sarah Karlin-Smith of the Pink Sheet.
Panelists
Maya Goldman
Axios
Sarah Karlin-Smith
Pink Sheet
@sarahkarlin-smith.bsky.social
Alice Miranda Ollstein
Politico
Among the takeaways from this week’s episode:
- This week the GOP steamrolled toward a major constriction of the nation’s social safety net, pushing through Trump’s tax and spending bill. The legislation contains significant changes to the way Medicaid is funded and delivered — in particular, through imposing the program’s first federal work requirement on many enrollees. Hospitals say the changes would be devastating, potentially resulting in the loss of services and facilities that could touch all patients, not only those on Medicaid.
- Some proposals in Trump’s bill were dropped during the Senate’s consideration, including a ban on Medicaid coverage for gender-affirming care and federal funding cuts for states that use their own Medicaid funds to cover immigrants without legal status. And for all the talk of not touching Medicare, the legislation’s repercussions for the deficit are expected to trigger spending cuts to the program that covers those over 65 and some with disabilities — potentially as soon as the next fiscal year.
- The newly reconstituted Advisory Committee on Immunization Practices met last week, and it looked pretty different from previous meetings: In addition to new members, there were fewer staffers on hand from the Centers for Disease Control and Prevention — and the notable presence of vaccine critics. The panel’s vote to reverse the recommendation of flu shots containing a mercury-based preservative — plus its plans to review the childhood vaccine schedule — hint at what’s to come.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: The Lancet’s “Evaluating the Impact of Two Decades of USAID Interventions and Projecting the Effects of Defunding on Mortality up to 2030: A Retrospective Impact Evaluation and Forecasting Analysis,” by Daniella Medeiros Cavalcanti, et al.
Alice Miranda Ollstein: The New York Times’ “‘I Feel Like I’ve Been Lied To’: When a Measles Outbreak Hits Home,” by Eli Saslow.
Maya Goldman: Axios’ “New Docs Get Schooled in Old Diseases as Vax Rates Fall,” by Tina Reed.
Sarah Karlin-Smith: Wired’s “Snake Venom, Urine, and a Quest to Live Forever: Inside a Biohacking Conference Emboldened by MAHA,” by Will Bahr.
Also mentioned in this week’s episode:
- NBC News’ “Crisis Pregnancy Centers Told To Avoid Ultrasounds for Suspected Ectopic Pregnancies,” by Abigail Brooks.
- ProPublica’s “A ‘Striking’ Trend: After Texas Banned Abortion, More Women Nearly Bled to Death During Miscarriage,” by Kavitha Surana, Lizzie Presser, and Andrea Suozzo.
- The Washington Post’s “DOGE Loses Control Over Government Grants Website, Freeing Up Billions,” by Dan Diamond and Hannah Natanson.
click to open the transcript
Transcript: Trump’s Bill Reaches the Finish Line
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello, and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News, and I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, July 3, at 10 a.m. As always, and particularly this week, news happens fast and things might have changed by the time you hear this. So, here we go.
Today we are joined via videoconference by Alice Miranda Ollstein of Politico.
Alice Miranda Ollstein: Hello.
Rovner: Sarah Karlin-Smith at the Pink Sheet.
Sarah Karlin-Smith: Hi, everybody.
Rovner: And Maya Goldman of Axios News.
Maya Goldman: Good to be here.
Rovner: No interview this week, but more than enough news, so we will get right to it. So as we sit down to tape, the House is on the cusp of passing the biggest constriction of the federal social safety net ever, part of President [Donald] Trump’s, quote, “One Big Beautiful Bill,” which is technically no longer called that, because the name was ruled out of order when it went through the Senate. In an effort to get the bill to the president’s desk by the July Fourth holiday, aka tomorrow, the House had to swallow without changes the bill that passed the Senate on Tuesday morning after Vice President JD Vance broke a 50-50 tie. And the House has been in session continuously since Wednesday morning working to do just that, with lots of arm-twisting and threatening and cajoling to walk back the complaints from both conservative Republicans, who are objecting to the trillions of dollars the bill would add to the national debt, as well as moderates objecting to the Medicaid and food stamp cuts.
There is a whole lot to unpack here, but let’s start with Medicaid, which would take the biggest hit of the health programs in this bill — ironically, just weeks before the program’s 60th anniversary. What does this bill do to Medicaid?
Goldman: This bill makes some huge changes to the way that Medicaid is funded and delivered in the United States. One of the biggest changes is the first federal work requirement for Medicaid, which we’ve talked about at length.
Rovner: Pretty much every week.
Goldman: Pretty much every week. It’s going to be — it’s sort of death by paperwork for many people. They’re not necessarily forced to lose their coverage, but there are so many paperwork hurdles and barriers to making sure that you are reporting things correctly, that CBO [the Congressional Budget Office] expects millions of people are going to lose coverage. And we know from limited experiments with work requirements in Arkansas that it does not increase employment. So, that’s the biggie.
Rovner: The House froze provider taxes, which is what most — all states but Alaska? — use to help pay their share of Medicaid. The Senate went even further, didn’t they?
Goldman: Yeah. Hospitals are saying that it’s going to be absolutely devastating to them. When you cut funding, cut reimbursement in that way, cut the amount of money that’s available in that way, it trickles down to the patient, ultimately.
Karlin-Smith: Especially things like the provider tax, but even just the loss to certain health systems of Medicaid patients end up having a spiral effect where it may impact people who are on other health insurance, because these facilities will no longer have that funding to operate the way they are. Particularly some facilities talked about how the Obamacare Medicaid expansion really allowed them to expand their services and beef up. And now if they lose that population, you actually end up with risks of facilities closing. The Senate tried to provide a little bit of money to alleviate that, but I think that’s generally seen as quite small compared to the long-term effects of this bill.
Rovner: Yeah, there’s a $50 billion rural hospital slush fund, if you will, but that’s not going to offset $930 billion in cuts to Medicaid. And it’s important — I know we keep saying this, but it’s important to say again: It’s not just the people who will lose Medicaid who will be impacted, because if these facilities close — we’re talking about hospitals and rural clinics and other facilities that depend on Medicaid — people with all kinds of insurance are going to lack access. I see lots of nods going around.
Goldman: Yeah. One salient example that somebody told me earlier this week was, think about ER wait times. It already takes so long to get seen if you go into the ER. And when people don’t have health insurance, they’re seeking care at the ER because it’s an emergency and they waited until it was an emergency, or that’s just where they feel they can go. But this is going to increase ER wait times for everybody.
Rovner: And also, if nursing homes or other facilities close, people get backed up in the ER because they can’t move into the hospital when they need hospital care, because the hospital can’t discharge the people who are already there. I had sort of forgotten how that the crowded ERs are often a result of things other than too many people in the ER.
Goldman: Right.
Rovner: They’re a result of other strains on sort of the supply chain for care.
Goldman: There’s so many ripple effects and dominoes that are going to fall, if you will.
Rovner: So, there were some things that were in the House bill that, as predicted, didn’t make it into the Senate bill, because the parliamentarian said they violated the budget rules for reconciliation. That included the proposed Medicaid ban on all transgender care for minors and adults, and most of the cuts to states that use their own funds to cover undocumented people. But the parliamentarian ended up kind of splitting the difference on cutting funding to Planned Parenthood, which she had ruled in 2017 Congress couldn’t do in reconciliation. Alice, what happened here?
Ollstein: She decided that one year of cuts was OK, when they had originally sought 10. And the only reason they originally sought 10 is that’s how these bills work. It’s a 10-year budget window. That’s how you calculate things. They sort of meant it to function like a permanent defund. So, the anti-abortion movement was really divided on this outcome, where some were declaring it a big victory and some were saying: Oh, only one year. This is such a disappointment and not what we were promised blah, blah, blah. And it’ll be really interesting to see if even one year does function like a sort of permanent defund.
On the one hand, the anti-abortion movement is worried that because it’s one year, that means they’ll have to vote on it again next year right before the midterms, when people might get more squirrelly because of the politics of it, which obviously still exist now but would be more potent then. But clinics can’t survive without funding for long. We’re already seeing Planned Parenthoods around the country close because of Title X cuts, because of other budget instability. And so once a clinic closes, even if the funding comes back later, it can’t flip a switch and turn it back on. When things close, they close, the staff moves away, etc.
Rovner: And we should emphasize Medicaid has not been used to pay for federal abortion funding ever.
Ollstein: Yes. Yes.
Rovner: That’s part of the Hyde Amendment. So we’re talking about non-abortion services here. We’re talking about contraception, and STD testing and treatment, and cancer screenings, and other types of primary care that almost every Planned Parenthood provides. They don’t all provide abortion, but they all provide these other ancillary services that lots of Medicaid patients use.
Ollstein: Right. And so this will shut down clinics in states where abortion is legal, and it’ll shut down clinics in states where abortion is illegal and these clinics only are providing those other reproductive health services, which are already in scant supply and hard to come by. There’s massive maternity care deserts, contraceptive deserts around the country, and this is set to make that worse.
Rovner: So, while this bill was not painted as a repeal of the Affordable Care Act, unlike the 2017 version, it does do a lot to scale that law back. This has kind of flown under the radar. Maya, you wrote about this. What does this bill do to the ACA?
Goldman: Yeah. Well, so, there were a lot of changes that Congress was seeking to codify from rule that the Trump administration has finalized that really create a lot of extra barriers to enrolling in the ACA. A lot of those did not make it into the final bill that is being voted on, but there’s still more paperwork — death by paperwork. I think there’s preenrollment verification of eligibility, things like that. And I think just in general, the ACA has created massive gains in the insurer population in the United States over the last decade and a half. And there’s estimates that show that this would wipe out three-fourths of that gain. And so that’s just staggering to see that.
Rovner: Yeah. I think people have underestimated the impact that this could have on the ACA. Of course, we’ve talked about this also a million times. This bill does not extend the additional subsidies that were created under the Biden administration, which has basically doubled the number of people who’ve been able to afford coverage and bought it on the marketplaces. But I’ve seen estimates that more than half of the people could actually end up dropping out of ACA coverage.
Goldman: Yeah. And I think it’s important to talk about the timelines here. A lot of the work requirements in Medicaid won’t take effect for a couple of years, but people are going to lose their enhanced subsidies in January. And so we are going to see pretty immediate effects of this.
Rovner: And they’re shortening the enrollment time.
Goldman: Yeah.
Rovner: And people won’t be able to be auto-reenrolled, which is how a lot of people continue on their ACA coverage. There are a lot of little things that I think together add up to a whole lot for the ACA.
Goldman: Right. And Trump administration ACA enrollment barriers that were finalized might not be codified in this law, but they’re still finalized.
Rovner: Yeah.
Goldman: And so they will take effect for 2026 coverage.
Rovner: And while President Trump has said repeatedly that he didn’t want to touch Medicare, this bill ironically is going to do exactly that, because the amount the tax cuts add to the deficit is likely to trigger a Medicare sequester under budget rules. That means there will be automatic cuts to Medicare, probably as soon as next year.
All right, well, that is the moving bill, the One Big Beautiful Bill. One thing that has at least stopped moving for now is the Supreme Court, at least for the moment. The justices wrapped up their formal 2024-2025 term with some pretty significant health-related cases that impact two topics we’re talking about elsewhere in this episode, abortion and vaccines.
First, abortion. The court ruled that Medicaid patients don’t have the right to sue to enforce the section of Medicaid law that ensures free choice of provider. In this case, it frees South Carolina to kick Planned Parenthood out of its Medicaid program. Now, this isn’t about abortion. This is about, as we said, other services that Planned Parenthood provides. But, Alice, what are the ramifications of this ruling?
Ollstein: They could be very big. A lot of states have already tried and are likely to try to cut Planned Parenthood out of their Medicaid programs. And given this federal defund, this is now going after some of their remaining supports, which is state Medicaid programs, which is a separate revenue stream. And so this will just lead to even more clinic closures. And already, this kind of sexual health care is very hard to come by in a lot of places in the country. And that is set to be even more true in the future. And this is sort of the culmination of something that the right has worked towards for a long time. And so they had just a bunch of different strategies and tactics to go after Planned Parenthood in so many ways in the courts, and there’s still more shoes to drop. There’s still court cases pending.
There’s one in Texas that’s accusing Planned Parenthood of defrauding the state, and so that judgment could wipe them out even more. This federal legislative effort, there’s the Supreme Court case — and they’ve really been effective at just throwing everything at the wall and seeing what sticks. And enough is sticking now that the organization is really — they were able to beat back a lot of these attempts before. They were able to rally in Congress. They were able to rally at the state level to push back on a lot of this. And that wasn’t true this time. And so I don’t know what conclusion to take from that. There’s, obviously, people are very overwhelmed. There’s a lot going on. There are organizations getting hit left and right, and maybe this just got lost in the noise this time.
Rovner: Yeah, I think that may be. Well, the other big Supreme Court decision was one we’d talked about quite a bit, the so-called Braidwood case that was challenging the ability of the CDC’s [Center for Disease Control and Prevention’s] Preventive Services Task Force from recommending services that would then be covered by health insurance. This was arguably a win for the Biden administration. The court ruled that the task force members do not need to be confirmed by the Senate. But, Sarah, this also gives Secretary [Robert F.] Kennedy [Jr.] more power to do what he will with other advisory committees, right?
Karlin-Smith: Right. By affirming the way the U.S. Preventive Services Task Force was set up, in that the HHS [Department of Health and Human Services] secretary is ultimately the authority for appointing the task force, which then makes recommendations around what coverage requirements under the ACA. It also sort of affirms the authority of the HHS secretary here. And I think people think it has implications for other bodies like CDC’s advisory committee on vaccines as well, where the secretary has a lot of authority.
So, I think people who really support the coverage advantages that have come through the USPSTF and Obamacare have always pushed for this outcome in this case. But given our current HHS secretary, there are some worries that it might lead to rollbacks or changes in areas of the health care paradigm that he does not support.
Rovner: Well, let us segue to that right now. That is, of course, as you mentioned, the other major CDC advisory committee, the one on immunization practices. When we left off, Secretary Kennedy had broken his promise to Senate health committee chairman Bill Cassidy and fired all 17 members of the committee, replacing them with vaccine skeptics and a couple of outright vaccine deniers. So last week, the newly reconstituted panel held its first meeting. How’d that go?
Karlin-Smith: It was definitely an interesting meeting, different, I think, for people who have watched ACIP [the Advisory Committee on Immunization Practices] in the past. Besides just getting rid of the members of the advisory panel, Kennedy also removed a lot of the CDC staff who work on that topic as well. So the CDC staffers who were there and doing their typical presentations were much smaller in number. And for the most part, I think they did a really good job of sticking to the tried-and-true science around these products and really having to grapple with extremely, I think, unusual questions from many of the panelists. But the agenda got shrunk quite a bit, and one of the topics was quite controversial. Basically, they decided to review the ingredient thimerosal, which was largely taken out of vaccines in the late ’90s, early 2000s, but remains in certain larger vials of flu vaccines.
Rovner: It’s a preservative, right? You need something in a multi-dose vaccine vial to keep it from getting contaminated.
Karlin-Smith: And they had a presentation from Lyn Redwood, who was a former leader of the Children’s Health Defense, which is a very anti-vax organization started by Robert Kennedy. The presentation was generally seen as not based in science and evidence, and there was no other presentations, and the committee voted to not really allow flu vaccines with that ingredient.
And the impact in the U.S. here is going to be pretty small because, I think, it’s about 4% of people get vaccines through those large-quantity vials, like if you’re in a nursing home or something like that. But what people are saying, and Scott Gottlieb [Food and Drug Administration commissioner in the first Trump administration] was talking a lot about this last week, was that this is really a hint of what is to come and the types of things they are going to take aim at. And he’s particularly concerned about another, what’s called an adjuvant, which is an ingredient added to vaccines to help make them work better, that’s in a lot of childhood vaccines, that Kennedy hinted at he wanted on the agenda for this meeting. It came off the agenda, but he presumes they will circle back to it. And if companies can’t use that ingredient in their vaccines, he’s not really clear they have anything else that is as good and as safe, and could force them out of the market.
So there were a bunch of hints of things concerning fights to come. The other big one was that they were saying they want to review the totality of the childhood vaccine schedule and the amount of vaccines kids get, which was really a red flag for people who followed the anti-vaccine movement, because anti-vaxxers have a lot of long-debunked claims that kids get too many vaccines, they get them too closer together. And scientists, again, have thoroughly debunked that, but they still push that.
Rovner: And that was something else that Kennedy promised Cassidy he wouldn’t mess with, if I recall correctly, right?
Karlin-Smith: You know, the nature of the agreement between Cassidy and Kennedy keeps getting more confusing to me. And I actually talked to both HHS’ secretary’s office and Cassidy’s office last week about that. And they both don’t actually agree on quite exactly what the terms were. But anyway, I looked at it in terms of the terms, like whether it’s to preserve the recommendations ACIP has made over time in the childhood schedule, whether it’s to preserve the committee members. I think it’s pretty clear that Kennedy has violated the sort of heart of the matter, which is he has gone after safe, effective vaccines and people’s access to vaccines in this country in ways that are likely to be problematic. And there are hints of more to come. He’s also cut off funding for vaccines globally. So, I don’t know. I almost just laugh thinking about what they actually agreed to, but there’s really no way Cassidy can say that Kennedy followed through on his promises.
Rovner: Well, meanwhile, even while ACIP was meeting last week, the HHS secretary was informing the members of Gavi, that’s the Global Alliance for Vaccines and Immunizations, that he was canceling the U.S.’ scheduled billion-dollar contribution because, he said, the public-private partnership that has vaccinated more than a billion children over the past two and a half decades doesn’t take vaccine safety seriously enough. Really?
Karlin-Smith: Yeah. Kennedy has these claims, again, that I think are, very clearly have been, debunked by experts, that Gavi is not thinking clearly about vaccine safety and offering vaccines they shouldn’t be, and the result is going to be huge gaps in what children can get around the globe to vaccines. And it comes on top of all the other cuts the U.S. has made recently to global health in terms of USAID [the U.S. Agency for International Development]. So I think these are going to be big impacts. And they may eventually trickle down to impact the U.S. in ways people don’t expect.
If you think about a virus like covid, which continues to evolve, one of the fears that people have always had is we get a variant that is, as it evolves, that is more dangerous to people and we’re less able to protect with the vaccines we have. If you allow the virus to kind of spread through unvaccinated communities because, say you weren’t providing these vaccines abroad, that increases the risk that we get a bad variant going on. So obviously, we should be concerned, I think, just about the millions of deaths people are saying this could cause globally, but there’s also impacts to our country as well and our health.
Rovner: I know there’s all this talk about soft-power humanitarian assistance and helping other countries, but as long as people can get on airplanes, it’s in our interest that people in other countries don’t get things that can be spread here, too, right?
Goldman: Yeah. One very small comment that was made during the ACIP meeting this week from CDC staff was an update on the measles outbreak, which I just thought was interesting. They said that the outbreak in the South from earlier this year is mostly under control, but people are still bringing in measles from foreign countries. And so that’s very much a real, real threat.
Rovner: Yeah.
Ollstein: It’s the lesson that we just keep not learning again and again, which is if you allow diseases to spread anywhere, it’ll inevitably impact us here. We don’t live on an island. We have a very interconnected world. You can’t have a Well we’re going to only protect our people and nobody else mentality, because that’s just not how it works. And we’re reducing resources to vaccinate people here as well.
Rovner: That’s right. Turning back to abortion, there was other news on that front this week. In Wisconsin, the state Supreme Court formally overturned that state’s 1849 abortion ban. That was the big issue in the Supreme Court election earlier this year. But a couple of other stories caught my eye. One is from NBC News about how crisis pregnancy centers, those anti-abortion facilities that draw women in by offering free pregnancy tests and ultrasounds, are actually advising clinics against offering ultrasounds in some cases after a clinic settled a lawsuit for misdiagnosing a woman’s ectopic pregnancy, thus endangering her life. Alice, if this is a big part of the centers’ draw with these ultrasounds, what’s going on here?
Ollstein: I think it’s a good example. I want to stress that there’s a big variety of quality of medical care at these centers. Some have actual doctors and nurses on staff. Some don’t at all. Some offer good evidence-based care. Some do not. And I have heard from a lot of doctors that patients will come to them with ultrasounds that were incorrectly done or interpreted by crisis pregnancy centers. They were given wrong information about the gestation of their pregnancy, about the viability of their pregnancy. And so this doesn’t surprise me at all, based on what I’ve heard anecdotally.
People should also remember that these centers are not regulated as much as health clinics are. And that goes for things like HIPAA [the Health Insurance Portability and Accountability Act] as well. They don’t have the same privacy protections for the information people share there. And so I think we should also keep in mind that women might be depending more and more on these going forward as Planned Parenthoods close, as other clinics close because of all the cuts we just talked about. These clinics are really proliferating and are trying to fill that vacuum. And so things like this should keep people questioning the quality of care they provide.
Rovner: Yeah. And of course, layer on top of that the Medicaid cuts. There’s going to be an increased inability to get care, particularly in far-flung areas. You can sort of see how this can sort of all pile onto itself.
Well, the other story that grabbed me this week comes from the Pulitzer Prize-winning team at ProPublica. It’s an analysis of hospital data from Texas that suggests that the state’s total abortion ban is making it more likely that women experiencing early miscarriages may not be getting timely care, and thus are more likely to need blood transfusions or experience other complications. Anti-abortion groups continue to maintain that these bans don’t impact women with pregnancy complications, which are super common, for those who don’t know, particularly early in pregnancy. But experience continues to suggest that that is not the case.
Ollstein: Yeah. This is a follow-up to a lot of really good reporting ProPublica has done. They also showed that sepsis rates in Texas have gone way up in the wake of the abortion ban. And so anti-abortion groups like to point to the state’s report showing how many abortions are still happening in the state because of the medical emergency exceptions, and saying: See? It’s working. People are using the exceptions. And it is true that some people are, but I think that this kind of data shows that a lot of people are not. And again, if it’s with what I hear anecdotally, there’s just a lot of variety on the ground from hospital to hospital, even in the same city, interpreting the law differently. Their legal teams interpret what they can and can’t provide. It could depend on what resources they have. It could depend on whether they’re a public or private hospital, and whether they’re afraid of the state coming after them and their funding.
And so I think this shows that one doctor could say, Yes, I do feel comfortable doing this procedure to save this woman’s life, and another doctor could say, I’m going to wait and see. And then you get the sepsis, the hemorrhage. These are very sensitive situations when even a short delay could really be life-and-death, or be long-term health consequences. People have lost the ability to have more children. We’ve seen stories about that. We’ve seen stories about people having to suffer a lot of health consequences while their doctors figure out what kind of care they can provide.
Rovner: In the case of early miscarriage, the standard of care is to empty the uterus basically to make sure that the bleeding stops, which is either a D&C [dilation and curettage], which of course can also be an early abortion, or using the abortion pill mifepristone and misoprostol, which now apparently doctors are loath to use even in cases of miscarriage. I think that’s sort of the take-home of this story, which is a little bit scary because early miscarriage is really, really, really common.
Ollstein: Absolutely. And this is about the hospital context, which is obviously very important, but I’m also hearing that this is an issue even for outpatient care. So if somebody is having a miscarriage, it’s not severe enough that they have to be hospitalized, but they do need this medication to help it along. And when they go to the pharmacy, their prescription says, “missed abortion” or “spontaneous abortion,” which are the technical terms for miscarriage. But a pharmacist who isn’t aware of that, isn’t used to it, it’s not something they see all the time, they see that and they freak out and they say, Oh, I don’t want to get sued, so they don’t dispense the medication. Or there are delays. They need to call and double-check. And that has been causing a lot of turmoil as well.
Rovner: All right. Well, finally this week, Elon Musk is fighting with President Trump again over the budget reconciliation bill, but the long shadow of DOGE [the Department of Government Efficiency] still lives on in federal agencies. On the one hand, The Washington Post scooped this week that DOGE no longer has control over the Grants.gov website, which controls access to more than half a trillion dollars in federal grant funding. On the other hand, I’m still hearing that money is barely getting out and still has to get multiple approvals from political appointees before it can basically get to where it’s supposed to be going. NPR has a story this week with the ominous headline “‘Where’s Our Money?’ CDC Grant Funding Is Moving So Slowly Layoffs Are Happening.”
I know there’s so much other news happening right now, it’s easy to overlook, but I feel like the public health and health research infrastructure are getting starved to death while the rest of us are looking at shinier objects.
Goldman: Yeah. This the whole flood-the-zone strategy, right? There’s so many things going on that we can’t possibly keep up with all of them, but this is extremely important. I think if you talk to any research scientist that gets federal funding, they would tell you that things have not gotten back to normal. And there’s so much litigation moving through the courts that it’s going to take a really long time before this is settled, period.
Rovner: Yeah. We did see yet another court decision this week warning that the layoffs at HHS were illegal. But a lot of these layoffs happened so long ago that these people have found other jobs or put their houses up for sale. You can’t quite put this toothpaste back in the tube.
Goldman: Right. And also, with this particular ruling, this came from a Rhode Island federal judge, a Biden appointee, so it wasn’t very surprising. But it said that the reorganization plan of HHS was illegal. Or, not illegal, it was a temporary injunction on the reorganization plan and said HHS cannot place anyone else on administrative leave. But it doesn’t require them to rehire the employees that have been laid off, which is also interesting.
Rovner: Yeah. Well, we will continue to monitor that. All right, that is as much as this week’s news as we have time for. Now it’s time for our extra-credit segment. That’s where we each recognize a story we read this week we think you should read, too. Don’t worry if you miss it. We will put the links in our show notes on your phone or other mobile device. Sarah, you were first to choose this week. Why don’t you go first?
Karlin-Smith: I took a look at a Wired piece from Will Bahr, “Snake Venom, Urine, and a Quest To Live Forever: Inside a Biohacking Conference Emboldened by MAHA.” And it is about a conference in Texas kind of designed to sell you products that they claim might help you live to 180 or more. A lot of what appears to be people essentially preying on people’s fears of mortality, aging, death to sell things that do not appear to be scientifically tested or validated by agencies like FDA. The founder even talks about using his own purified urine to treat his allergies. They’re microdosing snake venom. And it does seem like RFK is sort of emboldening this kind of way of thinking and behavior.
One of the things I felt was really interesting about the story is the author can’t quite pin down what unites all of these people in their interests in this space. In many cases, they claim there are sort of — there’s not a political element to it. But since I cover the pharma industry very closely, they all seem disappointed with mainstream medical systems and the pharma industry with the U.S., and they are seeking other avenues. But it’s quite an interesting look at the types of things they are willing to try to extend their lives.
Rovner: Yeah, it is quite the story. Maya, why don’t you go next?
Goldman: My extra credit this week is from my Axios colleague Tina Reed. It’s called “New Docs Get Schooled in Old Diseases as Vaxx Rates Fall.” And it’s all about how medical schools are adjusting their curriculum to teach students to spend more time on measles and things that we have considered to be wiped out in the United States. And I think it just — it really goes to show that this is something that is real and that’s actually happening. People are coming to emergency rooms and hospitals with these illnesses, and young doctors need to learn about them. We already have so many things to learn in medical school that there’s certainly a trade-off there.
Rovner: There is, indeed. And Alice, you have a related story.
Ollstein: Yes, I do. So, this is from The New York Times. It’s called “‘I Feel I’ve Been Lied To’: When a Measles Outbreak Hits Home,” by Eli Saslow. And it’s about the measles outbreak that originated in Texas. But what I think it does a really good job at is, we’ve talked a lot about how people have played up the dangers of vaccines and exaggerated them and, in some cases, outright lied about them, and how that’s influencing people, fear of autism, etc., fear of these adverse reactions. But I think this piece really shows that the other side of that coin is how much some of those same voices have downplayed measles and covid.
And so we have this situation where people are too afraid of the wrong things — vaccines — and not afraid enough of the right things — measles and these diseases. And so in the story people who are just, including people with some medical training, being shocked at how bad it is, at how healthy kids are really suffering and needing hospitalization and needing to be put on oxygen. And that really clashes with the message from this administration, which has really downplayed that and said it’s mainly hitting people who were already unhealthy or already had preexisting conditions, which is not true. It can hit other people. And so, yeah, I think it’s a very nuanced look at that.
Rovner: Yeah, it’s a really extraordinary story. My extra credit this week is from the medical journal The Lancet. And I won’t read the entire title or its multiple authors, because that would take the rest of the podcast. But I will summarize it by noting that it finds that funding provided by the U.S. Agency for International Development, which officially closed up shop this week after being basically illegally dissolved by the Trump administration, has saved more than 90 million lives over the past two decades. And if the cuts made this year are not restored, an additional 14 million people will die who might not have otherwise. Far from the Trump administration’s claims that USAID has little to show for its work, this study suggests that the agency has had an enormous impact in reducing deaths from HIV and AIDS, from malaria and other tropical diseases, as well as those other diseases afflicting less developed nations. We’ll have to see how much if any of those services will be maintained or restored.
OK. That’s this week’s show. Thanks to our editor, Emmarie Huetteman, and our producer-engineer, Francis Ying. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left us a review. That helps other people find us, too. Also, as always, you can email us your comments or questions. We’re at whatthehealth@kff.org. You can find me on X, @jrovner, or on Bluesky, @julierovner. Where are you guys these days? Sarah?
Karlin-Smith: I’m a little bit on X, mostly on Bluesky, at @SarahKarlin or @sarahkarlin-smith.
Rovner: Alice?
Ollstein: Mostly on Bluesky, @alicemiranda. Still a little bit on X, @AliceOllstein.
Rovner: Maya.
Goldman: I am on X, @mayagoldman_, and also on LinkedIn. You can just find me under my name.
Rovner: We will be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
3 weeks 22 hours ago
Courts, Health Care Costs, Health Care Reform, Health Industry, Insurance, Medicaid, Medicare, Multimedia, Public Health, States, Abortion, CDC, KFF Health News' 'What The Health?', Legislation, Podcasts, reproductive health, Trump Administration, vaccines, Women's Health
PAHO/WHO | Pan American Health Organization
Measles cases rise in the Americas in 2025
Measles cases rise in the Americas in 2025
Cristina Mitchell
3 Jul 2025
Measles cases rise in the Americas in 2025
Cristina Mitchell
3 Jul 2025
3 weeks 1 day ago
Grenada Hospitals Authority: RFP – Communication Specialist
The deadline to submit proposals for the position of Communication Specialist (individual or company) is 25 July 2025
View the full post Grenada Hospitals Authority: RFP – Communication Specialist on NOW Grenada.
The deadline to submit proposals for the position of Communication Specialist (individual or company) is 25 July 2025
View the full post Grenada Hospitals Authority: RFP – Communication Specialist on NOW Grenada.
3 weeks 1 day ago
ADVERTISEMENT, Business, Health, communication specialist, general hospital, gha, grenada hospitals authority, grenada hospitals authority act, hospital laundry, Ministry of Health, princess alice hospital, princess royal hospital, rfp, statutorisation transition team
PAHO/WHO | Pan American Health Organization
PAHO and CDRI Sign Agreement to Strengthen Health Infrastructure Resilience Against Disasters
PAHO and CDRI Sign Agreement to Strengthen Health Infrastructure Resilience Against Disasters
Cristina Mitchell
3 Jul 2025
PAHO and CDRI Sign Agreement to Strengthen Health Infrastructure Resilience Against Disasters
Cristina Mitchell
3 Jul 2025
3 weeks 1 day ago
Increased foreign medical demand fuels interest in Dominican Republic’s health sector
Santo Domingo.- The Dominican Republic is rapidly establishing itself as a leading regional destination for health tourism, driven by a rising demand for affordable, high-quality medical care outside the United States and other expensive markets. International patients—particularly Dominican expatriates in the U.S.
Santo Domingo.- The Dominican Republic is rapidly establishing itself as a leading regional destination for health tourism, driven by a rising demand for affordable, high-quality medical care outside the United States and other expensive markets. International patients—particularly Dominican expatriates in the U.S. and American citizens with limited insurance coverage—are attracted by the country’s excellent clinical standards, short wait times, and competitive pricing offered by private healthcare providers.
With over two million Dominicans living in the U.S. and a large population of underinsured Americans, the demand for medical services such as preventive check-ups, minimally invasive surgeries, advanced dental care, and fertility treatments continues to grow. According to data from The Commonwealth Fund, nearly 30 million Americans lack health insurance, and another 45 million have limited coverage, fueling the search for affordable, quality care alternatives.
For healthcare providers in the Dominican Republic, this trend presents a valuable opportunity to broaden their services for international patients, integrate telemedicine and remote post-surgery follow-up, build stronger partnerships with insurers and medical facilitators, and generate foreign exchange and specialized jobs—ultimately raising the national healthcare standard.
The Dominican Association of Health Tourism (ADTS) boasts a network of member institutions that adhere to international standards, employ bilingual staff, and maintain modern facilities with global certifications. Innovative programs like SENASA’s Larimar plan—which enables Dominicans abroad to access local medical services with insured coverage—and “health remittance” initiatives offering prepaid medical packages are expanding the market even further.
Thanks to its strong air connectivity, favorable investment environment, and renowned hospitality, the Dominican Republic is strengthening its role as a premier health and wellness destination in the Caribbean, providing a cost-effective, top-quality healthcare option for patients from around the world.
3 weeks 1 day ago
Health, tourism
Health Archives - Barbados Today
Violence against nurses sparks fresh safety calls
Three nurses at the Queen Elizabeth Hospital were attacked by a patient wielding a sharp object early on Wednesday, in the second violent incident targeting the nursing community in less than a month, prompting renewed calls for urgent action to protect healthcare staff.
The female patient had the object concealed before she attacked the nurses, who received immediate medical and psychological support, the hospital’s communications specialist Shane Sealy confirmed.
While the injuries were not life-threatening, the incident sparked renewed concerns over the safety of healthcare professionals both inside and outside medical facilities.
The Barbados Nurses Association (BNA) urged health authorities to install panic buttons on all hospital wards and conduct a comprehensive review of security protocols.
“And to the public,” BNA President Dr Fay Parris said in a strong appeal, “stop the violence against nurses. They care for you. Let’s care for them.”
“We also urge nurses to take proactive steps to protect themselves. Over the past two weeks, BNA has started facilitating the provision of self-defence sessions and ‘Safety First’ webinars—both eligible for continuing education credits. BNA invites all nurses, nursing personnel and nursing students to make use of this opportunity to learn the skills to protect themselves.”
The latest attack comes just weeks after a nurse was assaulted near the St Philip District Hospital. The BNA had raised serious concerns then—and is now intensifying its calls for stronger protections.
A BNA team visited QEH in the aftermath of Wednesday’s incident and spoke to injured nurses, according to Dr Parris, who said the BNA was assured the matter is under investigation, that immediate safety steps have been taken, and that counselling is being arranged.
In light of mounting concerns from nurses, the association has invited the permanent secretary in the Ministry of Health and officials to a virtual town hall this week to address safety challenges. It is awaiting confirmation of the meeting’s date and time.
After the latest incident, the QEH issued a statement saying that the staff who were attacked, and others present at the time were understandably shaken by the event.
“Immediate medical attention and psychological support were offered to all affected personnel. The matter is being reviewed by hospital management in collaboration with The Barbados Police Service, and QEH is providing full support to ensure all aspects of the incident are understood,” Sealy said.
QEH Chief Executive Officer Neil Clark added that the safety of staff, patients and visitors remains paramount.
He said: “We take this matter extremely seriously. The safety and well-being of our staff, patients, and visitors is always our top priority.”
Sealy added that as part of its routine commitment to continuous improvement, the hospital will use this incident “to reflect on and further refine existing safety procedures.”
Police Service spokesman Acting Inspector Ryan Brathwaite confirmed to Barbados TODAY that the incident had been reported to the police and investigations were under way.
(SB)
The post Violence against nurses sparks fresh safety calls appeared first on Barbados Today.
3 weeks 1 day ago
Health, Local News
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
INDIA bloc will bring Rajasthan Health Model to Bihar: Ashok Gehlot
Patna: Senior Congress leader Ashok Gehlot announced on Monday that the 'Rajasthan model of health care' will be replicated in Bihar if the INDIA bloc comes to power following the upcoming assembly polls this year.
Patna: Senior Congress leader Ashok Gehlot announced on Monday that the 'Rajasthan model of health care' will be replicated in Bihar if the INDIA bloc comes to power following the upcoming assembly polls this year.
The former Rajasthan chief minister came up with the promise at a press conference in Sadaqat Ashram, the BPCC headquarters, where AICC in-charge for Bihar Krishna Allavaru and state Congress president Rajesh Kumar were also present.
Gehlot claimed that under his rule, Rajasthan bore witness to an "unparalleled health model" wherein "cent per cent people" got the benefit of free medical insurance cover, unlike the Centre’s Ayushman Bharat scheme, which "caters to only a segment of the population", news agency PTI reported.
Also Read:Bihar Surgeon Threatened with Rs 20 lakh Extortion Call
"The Rajasthan Right to Health Act guaranteed free tests, treatment and medicines to each and every family. No other state has such a health model. If we come to power in Bihar, it will be replicated here," said the Congress leader, whose party is INDIA bloc's second largest constituent in the eastern state, where the coalition includes the RJD and the Left.
He also voiced concern over the “lack” of medical facilities in Bihar, pointing out that “60 per cent posts of doctors are vacant. The state government has not even been able to spend the budgetary allocation for health. Out of Rs 69,790 crore spent between 2016 and 2022, the state could utilise only Rs 21,743 crore. The will to ensure good governance is obviously lacking here”.
Speaking on the occasion, Allavaru alleged that "the so-called double engine government in Bihar is actually a trouble engine. It has brought here the Gujarat model of question paper leak, which is playing havoc with the future of the state’s youth".
Recalling the 17-month-long alliance with Chief Minister Nitish Kumar that ended last year, Allavaru claimed "more than three lakh people got government jobs during that period and there was not a single instance of paper leak".
"Therefore, Bihar is yearning for a change. Change will happen in the upcoming assembly elections," asserted the AICC in-charge of the state.
Also Read:Retired NMCH Nurse, Daughter shot dead outside home
3 weeks 1 day ago
State News,Bihar,Latest Health News,Recent Health News
PAHO/WHO | Pan American Health Organization
WHO launches bold push to raise health taxes and save millions of lives
WHO launches bold push to raise health taxes and save millions of lives
Cristina Mitchell
2 Jul 2025
WHO launches bold push to raise health taxes and save millions of lives
Cristina Mitchell
2 Jul 2025
3 weeks 2 days ago
Lifeguard and SGU students assist in saving elderly man
A Grenada lifeguard and SGU medical students responded to a medical emergency, saving the life of an elderly man at Grand Anse Beach on Monday, 30 June
View the full post Lifeguard and SGU students assist in saving elderly man on NOW Grenada.
A Grenada lifeguard and SGU medical students responded to a medical emergency, saving the life of an elderly man at Grand Anse Beach on Monday, 30 June
View the full post Lifeguard and SGU students assist in saving elderly man on NOW Grenada.
3 weeks 2 days ago
Health, PRESS RELEASE, Watersports, Youth, abhilash uddandam, aed, automated external defibrillator, deb eastwood, grenada lifeguards, tyrone jacob, zakariya dirie
PAHO/WHO | Pan American Health Organization
PAHO and Global Affairs Canada initiative strengthens the health of women and adolescents in situations of vulnerability in six countries of the Americas
PAHO and Global Affairs Canada initiative strengthens the health of women and adolescents in situations of vulnerability in six countries of the Americas
Cristina Mitchell
2 Jul 2025
PAHO and Global Affairs Canada initiative strengthens the health of women and adolescents in situations of vulnerability in six countries of the Americas
Cristina Mitchell
2 Jul 2025
3 weeks 2 days ago
PAHO/WHO | Pan American Health Organization
Noncommunicable disease deaths in the Americas have risen 43% since 2000, PAHO report shows
Noncommunicable disease deaths in the Americas have risen 43% since 2000, PAHO report shows
Cristina Mitchell
2 Jul 2025
Noncommunicable disease deaths in the Americas have risen 43% since 2000, PAHO report shows
Cristina Mitchell
2 Jul 2025
3 weeks 2 days ago
STAT+: Pharmalittle: We’re reading about Spain probing Novo weight loss ads, AstraZeneca stock listing, and more
Hello, everyone, and how are you today? We are doing just fine, thank you, especially since the middle of the week is already upon us. After all, we have made it this far so we have decided to hang on for another couple of days. And why not? Given the likely alternatives, this seems to be a reasonable decision.
To make the time fly, we are firing up the trusted coffee kettle and brewing another cup of stimulation. Our choice today is strawberry creme, which occupies a prominent spot in our pantry. But now, the time has come to get cracking. Here are a few items of interest to help you get started. We hope you have a lovely day, and do keep in touch. Feedback, tips, and suggestions are always welcome. …
Spain is investigating Novo Nordisk over concerns it may be illegally advertising its weight loss drugs Ozempic and Wegovy, EuroNews tells us. It is the latest in a string of inquiries into the company, with authorities in at least two other European countries accusing Novo Nordisk of unlawfully promoting its medications in recent years. Health officials worry drugmakers are seeking to boost already sky-high demand, possibly in violation of a European Union ban on consumer advertising for drugs that can only be obtained via prescription. The latest kerfuffle involves a campaign Novo Nordisk launched in Spain this month to raise public awareness about the health risks of obesity. The company also launched a website — which has since been taken down — on obesity’s health risks that cited endorsements from key scientific societies, recommended questions for people to ask their doctors, and offered weight loss tips. The tips included a healthy diet, exercise and sleep, and did not explicitly mention any medicines, but the Spanish health ministry said the campaign could serve as “covert advertising” for Novo Nordisk drugs.
AstraZeneca chief executive officer Pascal Soriot would like to move the drugmaker’s stock market listing to the U.S., The Times of London reports. Soriot has spoken privately of his preference to move the listing on a number of occasions and has even discussed moving AstraZeneca’s domicile. But he is likely to face resistance from parts of the board should he push for such a move, as well as the U.K. government, which is not believed to have been informed. Soriot, who has led AstraZeneca since 2012, has spoken publicly of his concerns about how Europe has fallen behind the U.S. and China, the company’s two largest markets, in innovating new medicines. He is known to be deeply frustrated with the U.K.’s operating environment, particularly restrictions on the approval of new medicines by the National Institute for Health and Care Excellence and the pricing of medicines under a National Health Service sales rebate scheme. Any attempt to move the listing would be highly controversial and a significant blow to the London stock market and the U.K. life sciences sector, which the Labor government set as a priority in its industrial strategy.
3 weeks 2 days ago
Pharma, Pharmalot, pharmalittle, STAT+
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Premarket approval application for Skinvive by Juvederm for neck lines reduction under USFDA review: Abbvie Allergan Aesthetics
Irvine: AbbVie's Allergan Aesthetics has announced that the U.S. Food and Drug Administration (FDA) has accepted for review the supplemental premarket approval (sPMA) application for SKINVIVE by JUVÉDERM to reduce neck lines for the improvement of neck appearance.
Irvine: AbbVie's Allergan Aesthetics has announced that the U.S. Food and Drug Administration (FDA) has accepted for review the supplemental premarket approval (sPMA) application for SKINVIVE by JUVÉDERM to reduce neck lines for the improvement of neck appearance.
SKINVIVE by JUVÉDERM is currently approved in the U.S. to improve skin smoothness of the cheeks in adults over the age of 21.
"SKINVIVE by JUVÉDERM is an injectable version of hyaluronic acid, a naturally occurring molecule found in the skin and important for skin hydration," said Darin Messina, Ph.D., senior vice president, aesthetics R&D, AbbVie. "The submission of SKINVIVE by JUVÉDERM to treat neck lines demonstrates our continued focus on developing new indications for comprehensive lower face and neck treatment as part of our market-leading portfolio of products, including BOTOX Cosmetic and SkinMedica."
Neck appearance is a top concern among people seeking aesthetic treatment, with millions of consumers considering professionally administered treatments to address their neck concerns. SKINVIVE by JUVÉDERM could offer hyaluronic acid injectable that aims to reduce neck lines to improve neck appearance.
The sPMA submission is supported by data from a multicenter, evaluator-blinded, randomized controlled study evaluating the safety and effectiveness of SKINVIVE by JUVÉDERM in adults with moderate to severe horizontal neck lines seeking improvement in neck appearance. All primary and secondary endpoints were met. Based on investigator assessment of horizontal neck lines, 80% of patients treated with SKINVIVE by JUVÉDERM achieved at least a 1-grade improvement at month 1. Nearly 90% of patients treated with SKINVIVE by JUVÉDERM reported improvement in neck appearance at month 1 as assessed by the Global Aesthetic Improvement Scale. Patients treated with SKINVIVE by JUVÉDERM reported being significantly less bothered with the overall appearance of their neck following treatment as measured by the FACE-Q questionnaire, while patients in the control group demonstrated no significant change. Treatment-emergent adverse events for SKINVIVE by JUVÉDERM were mild in severity and consistent with known safety profile. Additional data from the clinical study will be submitted for presentation at a future medical congress and for publication.
"Patients express frustration about the visible changes in their neck due to aging and sun exposure and seek non-surgical treatment options to address them," said Jeanine Downie, MD, FAAD, board-certified dermatologist and clinical investigator. "SKINVIVE by JUVÉDERM may offer another tool for patients exploring their aesthetics treatment journey beyond the face."
3 weeks 2 days ago
News,Dermatology,Dermatology News,Industry,Pharma News,Latest Industry News
‘MAHA Report’ Calls for Fighting Chronic Disease, but Trump and Kennedy Have Yanked Funding
The Trump administration has declared that it will aggressively combat chronic disease in America.
Yet in its feverish purge of federal health programs, it has proposed eliminating the National Center for Chronic Disease Prevention and Health Promotion and its annual funding of $1.4 billion.
The Trump administration has declared that it will aggressively combat chronic disease in America.
Yet in its feverish purge of federal health programs, it has proposed eliminating the National Center for Chronic Disease Prevention and Health Promotion and its annual funding of $1.4 billion.
That’s one of many disconnects between what the administration says about health — notably, in the “MAHA Report” that President Donald Trump recently presented at the White House — and what it’s actually doing, scientists and public health advocates say.
Among other contradictions:
- The report says more research is needed on health-related topics such as chronic diseases and the cumulative effects of chemicals in the environment. But the Trump administration’s mass cancellation of federal research grants to scientists at universities, including Harvard, has derailed studies on those subjects.
- The report denounces industry-funded research on chemicals and health as widespread and unreliable. But the administration is seeking to cut government funding that could serve as a counterweight.
- The report calls for “fearless gold-standard science.” But the administration has sowed widespread fear in the scientific world that it is out to stifle or skew research that challenges its desired conclusions.
“There are many inconsistencies between rhetoric and action,” said Alonzo Plough, chief science officer at the Robert Wood Johnson Foundation, a philanthropy focused on health.
The report, a cornerstone of President Donald Trump’s “Make America Healthy Again” agenda, was issued by a commission that includes Secretary of Health and Human Services Robert F. Kennedy Jr. and other top administration officials.
News organizations found that it footnoted nonexistent sources and contained signs that it was produced with help from artificial intelligence. White House Press Secretary Karoline Leavitt described the problems as “formatting issues,” and the administration revised the report.
Trump ordered the report to assess causes of a “childhood chronic disease crisis.” His commission is now working on a plan of action.
Spokespeople for the White House and Department of Health and Human Services did not respond to questions for this article.
Studies Derailed
The MAHA report says environmental chemicals may pose risks to children’s health. Citing the National Institutes of Health, it said there’s a “need for continued studies from the public and private sectors, especially the NIH, to better understand the cumulative load of multiple exposures and how it may impact children’s health.”
Meanwhile, the administration has cut funding for related studies.
For example, in 2020 the Environmental Protection Agency asked scientists to propose ways of researching children’s exposure to chemicals from soil and dust. It said that, for kids ages 6 months to 6 years, ingesting particulates — by putting their hands on the ground or floor then in their mouths — could be a significant means of exposure to contaminants such as herbicides, pesticides, and a group of chemicals known as PFAS.
One of the grants — for almost $1.4 million over several years — went to a team of scientists at Johns Hopkins University and the University of California-San Francisco. Researchers gained permission to collect samples from people’s homes, including dust and diapers.
But, beyond a small test run, they didn’t get to analyze the urine and stool samples because the grant was terminated this spring, said study leader Keeve Nachman, a professor of environmental health and engineering at Hopkins.
“The objectives of the award are no longer consistent with EPA funding priorities,” the agency said in a May 10 termination notice.
Another EPA solicitation from 2020 addressed many of the issues the MAHA report highlighted: cumulative exposures to chemicals and developmental problems such as attention-deficit/hyperactivity disorder, obesity, anxiety, and depression. One of the resulting grants funded the Center for Early Life Exposures and Neurotoxicity at the University of North Carolina-Chapel Hill. That grant was ended weeks early in May, said the center’s director, Stephanie Engel, a UNC professor of epidemiology.
In a statement, EPA press secretary Brigit Hirsch said the agency “is continuing to invest in research and labs to advance the mission of protecting human health and the environment.” Due to an agency reorganization, “the way these grants are administered will be different going forward,” said Hirsch, who did not otherwise answer questions about specific grants.
In its battle with Harvard, the Trump administration has stopped paying for research the NIH had commissioned on topics such as how autism might be related to paternal exposure to air pollution.
The loss of millions of dollars of NIH funding has also undermined data-gathering for long-term research on chronic diseases, Harvard researchers said. A series of projects with names like Nurses’ Health Study II and Nurses’ Health Study 3 have been tracking thousands of people for decades and aimed to keep tracking them as long as possible as well as enrolling new participants, even across generations.
The work has included periodically surveying participants — mainly nurses and other health professionals who enrolled to support science — and collecting biological samples such as blood, urine, stool, or toenail clippings.
Researchers studying health problems such as autism, ADHD, or cancer could tap the data and samples to trace potential contributing factors, said Francine Laden, an environmental epidemiologist at Harvard’s T.H. Chan School of Public Health. The information could retrospectively reveal exposures before people were born — when they were still in utero — and exposures their parents experienced before they were conceived.
Harvard expected that some of the grants wouldn’t be renewed, but the Trump administration brought ongoing funding to an abrupt end, said Walter Willett, a professor of epidemiology and nutrition at the Chan school.
As a result, researchers are scrambling to find money to keep following more than 200,000 people who enrolled in studies beginning in the 1980s — including children of participants who are now adults themselves — and to preserve about 2 million samples, Willett said.
“So now our ability to do exactly what the administration wants to do is jeopardized,” said Jorge Chavarro, a professor of nutrition and epidemiology at the Chan school. “And there’s not an equivalent resource. It’s not like you can magically recreate these resources without having to wait 20 or 30 years to be able to answer the questions” that the Trump administration “wants answered now.”
Over the past few months, the administration has fired or pushed out almost 5,000 NIH employees, blocked almost $3 billion in grant funding from being awarded, and terminated almost 2,500 grants totaling almost $5 billion, said Sen. Patty Murray (D-Wash.), vice chair of the Senate Appropriations Committee, at a June 10 hearing on the NIH budget.
In addition, research institutions have been waiting months to receive money under grants they’ve already been awarded, Murray said.
In canceling hundreds of grants with race, gender, or sexuality dimensions, the administration engaged in blatant discrimination, a federal judge ruled on June 16.
Cutting Funding
After issuing the MAHA report, the administration published budget proposals to cut funding for the NIH by $17.0 billion, or 38%, the Centers for Disease Control and Prevention by $550 million, or 12%, and the EPA by $5 billion, or 54%.
“This budget reflects the President’s vision of making Americans the healthiest in the world while achieving his goal of transforming the bureaucracy,” the HHS “Budget in Brief” document says. Elements of Trump’s proposed budget for the 2026 fiscal year clash with priorities laid out in the MAHA report.
Kennedy has cited diabetes as part of a crisis in children’s health. The $1.4 billion unit the White House has proposed to eliminate at the CDC — the National Center for Chronic Disease Prevention and Health Promotion — has housed a program to track diabetes in children, adolescents, and young adults.
“To say that you want to focus on chronic diseases” and then “to, for all practical purposes, eliminate the entity at the Centers for Disease Control and Prevention which does chronic diseases,” said Georges Benjamin, executive director of the American Public Health Association, “obviously doesn’t make a lot of sense.”
In a May letter, Office of Management and Budget Director Russell Vought listed the chronic disease center as “duplicative, DEI, or simply unnecessary,” using an abbreviation for diversity, equity, and inclusion programs.
Within the NIH, the White House has proposed cutting $320 million from the National Institute of Environmental Health Sciences, a reduction of 35%. That unit funds or conducts a wide array of research on issues such as chronic disease.
Trump’s budget proposes spending $500 million “to tackle priority activities to Make America Healthy Again,” including $260 million for his new Administration for a Healthy America to address the “chronic illness epidemic.”
Ceding Ground to Industry
The MAHA report argues that corporate influence has compromised government agencies and public health through “corporate capture.”
It alleges that most research on chronic childhood diseases is funded by the food, pharmaceutical, and chemical industries, as well as special interest organizations and professional associations. It says, for example, that a “significant portion of environmental toxicology and epidemiology studies are conducted by private corporations,” including pesticide manufacturers, and it cites “potential biases in industry-funded research.”
It’s “self-evident that cutbacks in federal funding leave the field open to the very corporate funding RFK has decried,” said Peter Lurie, president of the Center for Science in the Public Interest, a watchdog group focused on food and health.
Lurie shared the report’s concern about industry-funded research but said ceding ground to industry won’t help. “Industry will tend to fund those studies that look to them like they will yield results beneficial to industry,” he said.
In search of new funding sources, Harvard’s school of public health “is now ramping up targeted outreach to potential corporate partners, with careful review to ensure the science meets the highest standards of research integrity,” Andrea Baccarelli, dean of the school’s faculty, wrote in a June 11 letter to students, faculty, and others.
“It’s just simple math that if you devastate governmental funding by tens of billions of dollars, then the percentage of industry funding dollars will go up,” said Plough, who is also a clinical professor at the University of Washington School of Public Health.
“So therefore, what they claim to fear more,” he said, will “become even more influential.”
The MAHA report says “the U.S. government is committed to fostering radical transparency and gold-standard science.”
But many scientists and other scholars see the Trump administration waging a war on science that conflicts with its agenda.
In March, members of the National Academies of Sciences, Engineering, and Medicine accused the administration of “destroying” scientific independence, “engaging in censorship,” and “pressuring researchers to alter or abandon their work on ideological grounds.”
In May, NIH employees wrote that the administration was politicizing research — for example, by halting or censoring work on health disparities, health impacts of climate change, gender identity, and immunizations.
Recent comments by Kennedy pose another threat to transparency, researchers and health advocates say.
Kennedy said on a podcast that he would probably create in-house government journals and stop NIH scientists from publishing their research in The Lancet, The New England Journal of Medicine, The Journal of the American Medical Association, and others.
Creating new government outlets for research would be a plus, said Dariush Mozaffarian, director of the Food is Medicine Institute at the Friedman School of Nutrition Science and Policy at Tufts University.
But confining government scientists to government journals, he said, “would be a disaster” and “would basically amount to censorship.”
“That’s just not a good idea for science,” Mozaffarian said.
We’d like to speak with current and former personnel from the Department of Health and Human Services or its component agencies who believe the public should understand the impact of what’s happening within the federal health bureaucracy. Please message KFF Health News on Signal at (415) 519-8778 or get in touch here.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
3 weeks 2 days ago
Health Industry, Agency Watch, CDC, Chronic Disease Care, Environmental Health, HHS, NIH, Trump Administration
Con el verano hay más mosquitos y, temen oficiales, más casos de dengue
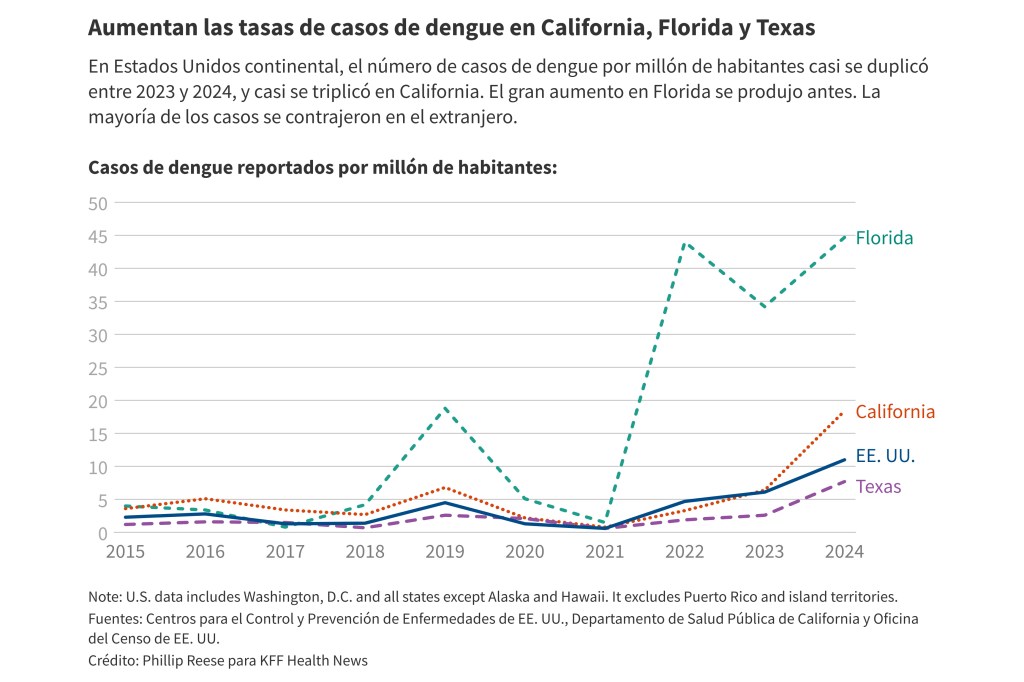
Con el verano marcando el comienzo de la temporada alta de mosquitos, autoridades sanitarias y de control de vectores se preparan para la posibilidad de otro año con tasas históricas de dengue.
Con el verano marcando el comienzo de la temporada alta de mosquitos, autoridades sanitarias y de control de vectores se preparan para la posibilidad de otro año con tasas históricas de dengue. Y con el cambio climático, la falta de una vacuna eficaz y los recortes federales en la investigación, les preocupa que la enfermedad se vuelva endémica en una franja más amplia de Norteamérica.
El año pasado se reportaron alrededor de 3.700 nuevas infecciones por dengue en Estados Unidos, frente a las 2.050 de 2023, según los Centros para el Control y Prevención de Enfermedades (CDC). Todos los casos de 2024 se adquirieron en el extranjero, excepto 105 contraídos en California, Florida o Texas. Los CDC emitieron una alerta sanitaria en marzo advirtiendo sobre el riesgo continuo de infección por dengue.
"Creo que el dengue ha llegado para quedarse", declaró Michael Ben-Aderet, especialista en enfermedades infecciosas y director médico asociado de epidemiología hospitalaria del Cedars-Sinai de Los Ángeles, sobre la posibilidad de que el dengue se convierta en la nueva normalidad en el país. "Estos mosquitos no se irán a ninguna parte".
El dengue es endémico —una etiqueta que las autoridades de salud pública asignan cuando las enfermedades aparecen de forma constante en una región— en muchas zonas más cálidas del mundo, como Latinoamérica, India y el sudeste asiático. Los casos de dengue aumentaron notablemente el año pasado en muchos de esos lugares, especialmente en Centro y Sur América.
La enfermedad, que puede propagarse por la picadura de mosquitos Aedes que portan el virus, no fue común en Estados Unidos continental durante gran parte del siglo pasado. Actualmente, la mayoría de los casos de dengue adquiridos localmente (es decir, no relacionados con viajes) en el país se registran en Puerto Rico, donde se registró un fuerte aumento en 2024, lo que desencadenó una emergencia de salud pública local.
La mayoría de las personas que desarrollan dengue no se enferman. Sin embargo, en algunas, los síntomas son graves: sangrado por la nariz o la boca, dolor de estómago intenso, vómitos e hinchazón. En ocasiones, el dengue causa la muerte.
California ofrece un caso centinela sobre la propagación del dengue en el país. Hace 25 años, no se conocía la presencia de los mosquitos Aedes aegypti y Aedes albopictus, que transmiten el dengue, en el estado. Actualmente, se encuentran en 25 condados y más de 400 ciudades y comunidades no incorporadas, principalmente en el sur de California y en el Valle Central.
La propagación de los mosquitos es preocupante porque su presencia aumenta la probabilidad de transmisión de enfermedades, afirmó Steve Abshier, presidente de la Mosquito and Vector Control Association of California.
Entre 2016 y 2022, se registró un promedio de 136 nuevos casos de dengue al año en California, cada uno de los cuales probablemente traído al estado por alguien que viajó y se infectó en otro lugar. En 2023, se registraron alrededor de 250 casos nuevos, incluyendo dos adquiridos localmente.
En 2024, California registró 725 nuevos casos de dengue, incluyendo 18 adquiridos localmente, según datos estatales.
El cambio climático podría contribuir al aumento de la población de mosquitos Aedes, afirmó Ben-Aderet. Estos mosquitos sobreviven mejor en zonas urbanas cálidas, y suelen picar durante el día. Las infecciones de transmisión local suelen ocurrir cuando alguien contrae dengue durante un viaje, regresa a casa y lo pica un mosquito Aedes que, a su vez, pica e infecta a otra persona.
"Se han propagado rápidamente por toda California", explicó Ben-Aderet.
El dengue representa un desafío para muchos médicos de atención primaria que nunca lo han visto. Ben-Aderet dijo que los médicos que sospechan dengue deben obtener un historial de viaje detallado de sus pacientes, pero confirmar el diagnóstico no siempre es rápido.
"No existe una prueba sencilla para detectarlo", afirmó. "La única prueba que tenemos para el dengue son las pruebas de anticuerpos". Agregó que "la mayoría de los laboratorios probablemente no lo estén comercializando, por lo que suele ser una prueba que se debe analizar en otra instalación. Por lo tanto, es fundamental sospechar que alguien tiene dengue".
Las mejores prácticas para evitar el dengue incluyen eliminar cualquier agua estancada en una propiedad, aunque sea poca, y usar repelente de mosquitos, dijo Abshier. Limitar la actividad al atardecer y al amanecer, cuando los mosquitos pican con mayor frecuencia, también puede ayudar.
Los esfuerzos para combatir el dengue en California se complicaron aún más este año después de que los incendios forestales arrasaran Los Ángeles.
Los incendios ocurrieron en una zona de alta incidencia de enfermedades transmitidas por mosquitos. Funcionarios del San Gabriel Valley Mosquito and Vector Control District han trabajado durante meses para tratar más de 1.400 piscinas sin mantenimiento que quedaron tras el incendio, eliminando así posibles criaderos de mosquitos.
Estos oficiales han utilizado recursos locales y estatales para tratar las piscinas, dijo Anais Medina Díaz, vocera del distrito. Han solicitado un reembolso a la Agencia Federal para el Manejo de Emergencias (FEMA), que históricamente no ha financiado las iniciativas de control de vectores luego de incendios forestales.
En California, las agencias de control de vectores suelen financiarse principalmente con impuestos y tasas locales que pagan los propietarios.
Algunos funcionarios están implementando el novedoso método de liberar mosquitos Aedes esterilizados para reducir el problema. Eso puede resultar eficaz, pero implementar el método en un gran número de áreas sería costoso y requeriría un esfuerzo masivo a nivel estatal, dijo Abshier.
Mientras tanto, el gobierno federal está reduciendo sus intervenciones: varios medios han informado que los Institutos Nacionales de Salud dejarán de financiar nuevas investigaciones relacionadas con el cambio climático, que podrían incluir trabajos sobre el dengue.
Este año, las tasas de dengue reportadas en gran parte del continente americano han disminuido significativamente desde 2024. Sin embargo, es probable que la tendencia en Estados Unidos no se esclarezca hasta finales de año, después que termine la temporada de mosquitos de verano.
Los investigadores de salud y control de vectores no están seguros de la gravedad de la situación en California.
Algunos afirman que podría haber brotes limitados, mientras que otros predicen que el dengue podría empeorar mucho. Sujan Shresta, profesor e investigador de enfermedades infecciosas en el Instituto de Inmunología de La Jolla, señaló que otros lugares, como Nepal, experimentaron relativamente pocos casos de dengue en el pasado reciente, pero ahora se registran brotes grandes con regularidad.
Existe una vacuna para niños, pero está siendo discontinuada debido a la falta de demanda mundial. Otras dos vacunas no están disponibles en Estados Unidos. El laboratorio de Shresta trabaja arduamente en una vacuna eficaz y segura contra el dengue. Espera publicar los resultados de las pruebas en animales en aproximadamente un año; si son positivos, los ensayos en humanos podrían ser posibles en unos dos años.
"Si no hay una buena vacuna ni buenos antivirales, este será un país endémico para dengue", afirmó.
Phillip Reese es especialista en reportaje de datos y profesor asociado de Periodismo en la Universidad Estatal de California-Sacramento.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
3 weeks 2 days ago
Global Health Watch, Noticias En Español, Public Health, States, california, Florida, Latinos, texas
As Mosquito Season Peaks, Officials Brace for New Normal of Dengue Cases
As summer ushers in peak mosquito season, health and vector control officials are bracing for the possibility of another year of historic rates of dengue.
As summer ushers in peak mosquito season, health and vector control officials are bracing for the possibility of another year of historic rates of dengue. And with climate change, the lack of an effective vaccine, and federal research cuts, they worry the disease will become endemic to a larger swath of North America.
About 3,700 new dengue infections were reported last year in the contiguous United States, up from about 2,050 in 2023, according to the Centers for Disease Control and Prevention. All of last year’s cases were acquired abroad, except for 105 cases contracted in California, Florida, or Texas. The CDC issued a health alert in March warning of the ongoing risk of dengue infection.
“I think dengue is here with us to stay,” said infectious disease specialist Michael Ben-Aderet, associate medical director of hospital epidemiology at Cedars-Sinai in Los Angeles, about dengue becoming a new normal in the U.S. “These mosquitoes aren't going anywhere.”
Dengue is endemic — a label health officials assign when diseases appear consistently in a region — in many warmer parts of the world, including Latin America, India, and Southeast Asia. Dengue cases increased markedly last year in many of those places, especially in Central and South America.
The disease, which can spread when people are bitten by infected Aedes mosquitoes, was not common in the contiguous United States for much of the last century. Today, most locally acquired (meaning unrelated to travel) dengue cases in the U.S. happen in Puerto Rico, which saw a sharp increase in 2024, triggering a local public health emergency.
Most people who contract dengue don’t get sick. But in some people symptoms are severe: bleeding from the nose or mouth, intense stomach pain, vomiting, and swelling. Occasionally, dengue causes death.
California offers a case study in how dengue is spreading in the U.S. The Aedes aegypti and Aedes albopictus mosquitoes that transmit dengue weren’t known to be in the state 25 years ago. They are now found in 25 counties and more than 400 cities and unincorporated communities, mostly in Southern California and the Central Valley.
The spread of the mosquitoes is concerning because their presence increases the likelihood of disease transmission, said Steve Abshier, president of the Mosquito and Vector Control Association of California.
From 2016 through 2022, there were an average of 136 new dengue cases a year in California, each case most likely brought to the state by someone who had traveled and been infected elsewhere. In 2023, there were about 250 new cases, including two acquired locally.
In 2024, California saw 725 new dengue cases, including 18 acquired locally, state data shows.
Climate change could contribute to growth in the Aedes mosquitoes’ population, Ben-Aderet said. These mosquitoes survive best in warm urban areas, often biting during the daytime. Locally acquired infections often occur when someone catches dengue during travel, then comes home and is bitten by an Aedes mosquito that bites and infects another person.
“They've just been spreading like wildfire throughout California,” Ben-Aderet said.
Dengue presents a challenge to the many primary care doctors who have never seen it. Ben-Aderet said doctors who suspect dengue should obtain a detailed travel history from their patients, but confirming the diagnosis is not always quick.
“There's no easy test for it,” he said. “The only test that we have for dengue is antibody tests.” He added that “most labs probably aren't doing it commercially, so it's usually like a send-out test from most labs. So you really have to suspect someone has dengue.”
Best practices for avoiding dengue include eliminating any standing pools of water on a property — even small pools — and using mosquito repellent, Abshier said. Limiting activity at dusk and dawn, when mosquitoes bite most often, can also help.
Efforts to combat dengue in California became even more complicated this year after wildfires ripped through Los Angeles. The fires occurred in a hot spot for mosquito-borne illnesses. San Gabriel Valley Mosquito and Vector Control District officials have worked for months to treat more than 1,400 unmaintained swimming pools left in the wake of fire, removing potential breeding grounds for mosquitoes.
San Gabriel vector control officials have used local and state resources to treat the pools, said district spokesperson Anais Medina Diaz. They have applied for reimbursement from the Federal Emergency Management Agency, which has not historically paid for vector control efforts following wildfires.
In California, vector control agencies are often primarily funded by local taxes and fees on property owners.
Some officials are pursuing the novel method of releasing sterilized Aedes mosquitoes to reduce the problem. That may prove effective, but deploying the method in a large number of areas would be costly and would require a massive effort at the state level, Abshier said. Meanwhile, the federal government is pulling back on interventions: Several outlets have reported that the National Institutes of Health will stop funding new climate change-related research, which could include work on dengue.
This year, reported rates of dengue in much of the Americas have declined significantly from 2024. But the trend in the United States likely won’t be clear until later in the year, after the summer mosquito season ends.
Health and vector control researchers aren't sure how bad it will get in California. Some say there may be limited outbreaks, while others predict dengue could get much worse. Sujan Shresta, a professor and infectious disease researcher at the La Jolla Institute for Immunology, said other places, like Nepal, experienced relatively few cases of dengue in the recent past but now regularly see large outbreaks.
There is a vaccine for children, but it faces discontinuation from a lack of global demand. Two other dengue vaccines are unavailable in the United States. Shresta’s lab is hard at work on an effective, safe vaccine for dengue. She hopes to release results from animal testing in a year or so; if the results are positive, human trials could be possible in about two years.
“If there's no good vaccine, no good antivirals, this will be a dengue-endemic country,” she said.
Phillip Reese is a data reporting specialist and an associate professor of journalism at California State University-Sacramento.
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
3 weeks 2 days ago
california, Multimedia, Public Health, States, Environmental Health, Florida, texas
Can you afford to get sick?
Take a moment and think of how many persons you know; family, friends, co-workers, who have been affected by cancer, heart disease, stroke, or another critical illness. For many Jamaicans, it’s more than just a statistic. It’s personal. When...
Take a moment and think of how many persons you know; family, friends, co-workers, who have been affected by cancer, heart disease, stroke, or another critical illness. For many Jamaicans, it’s more than just a statistic. It’s personal. When...
3 weeks 2 days ago
Could your gut health be why you are tired, moody and struggling to lose weight?
GUT HEALTH is crucial for overall well-being because it impacts digestion, immunity, mental health, and even heart health. A healthy gut ensures efficient nutrient absorption, strengthens the immune system, and may even influence mood and cognitive...
GUT HEALTH is crucial for overall well-being because it impacts digestion, immunity, mental health, and even heart health. A healthy gut ensures efficient nutrient absorption, strengthens the immune system, and may even influence mood and cognitive...
3 weeks 2 days ago
Foods, habits that can nourish or harm your gut health
GUT HEALTH is an easy thing to take for granted or to ignore completely, if everything is generally functioning well. However, poor gut health can impact your overall health in a variety of ways, from the obvious stomach discomfort to less obvious...
GUT HEALTH is an easy thing to take for granted or to ignore completely, if everything is generally functioning well. However, poor gut health can impact your overall health in a variety of ways, from the obvious stomach discomfort to less obvious...
3 weeks 2 days ago
The way forward for the Jamaican psilocybin industry
As awareness of psilocybin treating mental and behavioural conditions gathers steam in Jamaica, consultant psychiatrist Saphire Longmore is of the view that the positive turnarounds experienced by users of the ‘magic mushroom’ needs to be built...
As awareness of psilocybin treating mental and behavioural conditions gathers steam in Jamaica, consultant psychiatrist Saphire Longmore is of the view that the positive turnarounds experienced by users of the ‘magic mushroom’ needs to be built...
3 weeks 2 days ago