PAHO/WHO | Pan American Health Organization
Countries of the Americas should strengthen Mpox surveillance in light of potential spread of new variant detected in African region, PAHO says
Countries of the Americas should strengthen Mpox surveillance in light of potential spread of new variant detected in African region, PAHO says
Cristina Mitchell
9 Aug 2024
Countries of the Americas should strengthen Mpox surveillance in light of potential spread of new variant detected in African region, PAHO says
Cristina Mitchell
9 Aug 2024
1 year 2 months ago
Swine flu detected in Michigan resident - MLive.com
- Swine flu detected in Michigan resident MLive.com
- Ingham County resident has H3N2 swine flu virus Detroit Free Press
- Colorado, Michigan report H3N2v flu infections University of Minnesota Twin Cities
- Michigan reports human case of swine flu Reuters.com
- Michigan resident infected with mutant virus that triggered global panic Daily Mail
1 year 2 months ago
New medical graduates from Cuba
Grenada’s healthcare system is on track to improve with the appointment of 6 Grenadian doctors, graduates of the University of Medical Sciences of Granma, Cuba
View the full post New medical graduates from Cuba on NOW Grenada.
Grenada’s healthcare system is on track to improve with the appointment of 6 Grenadian doctors, graduates of the University of Medical Sciences of Granma, Cuba
View the full post New medical graduates from Cuba on NOW Grenada.
1 year 2 months ago
Health, PRESS RELEASE, cuba, glen noel, ministry of foreign affairs, university of medical sciences of granma, yanet silveria
Health Archives - Barbados Today
Closing the Gap Breasfeeding for all
Message from Minister of Labour, Social Security and Third Sector Colin Jordan to mark World Breast Feeding Week 2024
A country’s economy grows and the standard of living of its residents is determined, in large measure, by the involvement, engagement and productivity of its workers. Workers who are engaged and producing at their optimum are workers who are healthy – emotionally and physically.
During this World Breastfeeding Week 2024, the Ministry of Labour, Social Security and Third Sector is happy to come alongside the Breastfeeding and Child Nutrition Foundation to remind us all of the importance of breastfeeding to workers, and to enterprise and national development.
Mothers who are able to breastfeed their children and are provided adequate facilities at work to express and store breast milk are generally more engaged, satisfied and committed workers. They are more inclined to get into and remain in formal employment. They are more likely to be advocates for the organisation.
Children who are breastfed are shown to be generally healthier and better-adjusted children. As adults, they have lower incidences of chronic, non-communicable diseases than other segments of the population. They are able to engage better, think more clearly, and therefore be more productive.
Let us join together to close the gap and support mothers who are able to breastfeed their children. Mothers benefit. Children benefit. Our communities benefit. Our nation benefits.
(Ministry of Labour, Social Security and Third Sector)
The post Closing the Gap Breasfeeding for all appeared first on Barbados Today.
1 year 2 months ago
Health, Local News
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
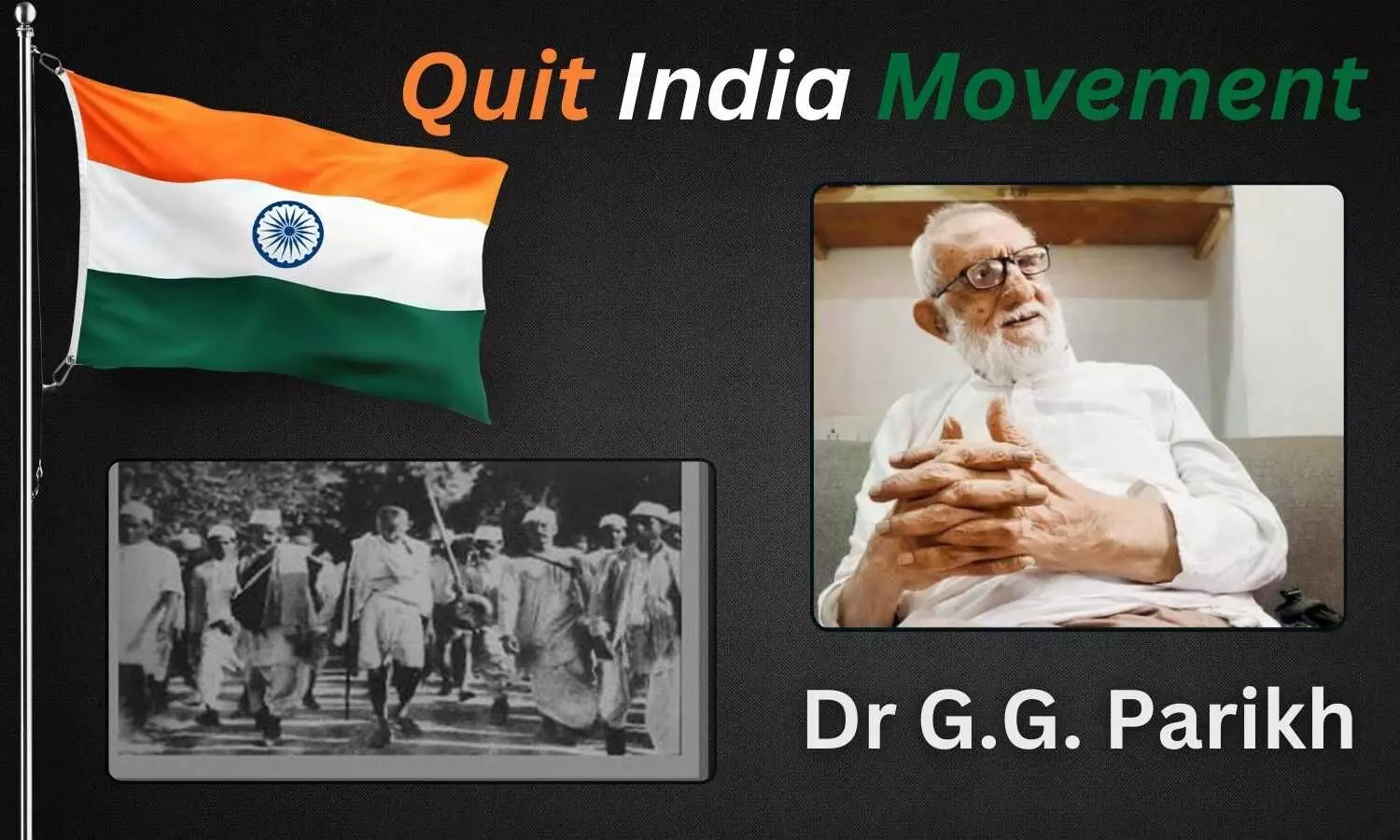
Dr. G.G. Parikh: Centenarian Doctor taking part in Quit India movement
After 82 years of the Quit India movement, we need to revisit the freedom fighters taking part in it. It was the first time police used tear gas when Aruna Asaf Ali hoisted the tricolour in Mumbai. Since the inception of this August, I have exchanged the views with one of its still surviving heroes Dr. G.G. Parikh on how to deal with dementia in the ripe age?
He shared how they had covered their faces with a handkerchief on that rainy day in the Gowalia Tank Maidan aka August Kranti Maidan, next to Fashion Street. A new phrase, the 42 Augusters came to be a part of modern history due to these freedom fighters. Last year, the Mumbai Press Club invited him to the Red Ink awards ceremony, where he delivered an excellent address sharing certain experiences from days of freedom struggle. One evening he repeated about himself as the product of the circumstances and elaborated it to some extent. In fact, the 42 Augusters are the imprisoned freedom fighters of Quit India Movement. Today, they are the rarest of the rare gems among public figures. The centenarian doctor is one of them with the fine memory. His commitment to the social causes had remained unwavering throughout the last many decades. Dr. GG Parikh recollected that the leadership of the independent India had betrayed the Mahatma. He said, “We were told that after independence, the rulers would be the servants of the public. But they started imitating the British, and that was the first betrayal. It’s not that we turned anti-Nehru, but we felt bad that Gandhi was forgotten so soon.” Dr. Gunvantrai Ganpatlal Parikh is better known as G.G. He was born on the bank of Bhogavo River, one of tributaries of the Sabarmati in Wadhwan, only 3 kms. Apart from the district headquarters of Surendranagar in Gujarat on 30th December 1924. He graduated in medical science from the G.S. Medical College, Parel (Mumbai) in 1950 and started practice to continue the tradition of Dr. Bidhan Chandra Roy. On every working day, he has continued to attend patients as a duty or a ritual of the clinic. Almost 75 years of practice is enough to make him one of the oldest practitioners of the medical science in the 21st century. Before earning the doctor’s degree, he was the founding member of All India Students Congress (AISC) known today as NSUI (National Students Union of India). He used to be fully active between 1943 and 1947. During the Quit India days, since most of Congress leaders were in jail, and the Bombay Pradesh Congress Committee (BPCC) went into coma, the AISC played like a mature political party, and GG offered services in its activities including collection of funds and to support the Royal Indian Navy mutiny. He used to be the president of the Bombay unit of the Student’s Congress in 1947. And further contributed to trade union movement and promotion of the consumer cooperatives. GG recollected how he ran away to the Prarthana Samaj before moving into the safe zone of his hostel on 9 August 1942. He was arrested on Churchgate Station during another incident of picketing with a group of student volunteers, and was sent to the Worli Temporary Prison (WTP). The best lessons in protests were his fondest memory from the ten months long first imprisonment before the end of his teenage. The arresting was repeated during the Emergency on 23rd October 1975 with George Fernandes. As such, he is one of those rare individuals to be at the receiving end of the two extreme acts of authoritarianism in Indian history. Last year, G.G. was making news during the annual ritual of the Quit India march to Chaupati beach and August Kranti Maidan. Dr. Parikh had joined Congress Socialist Party along with the members of the 42 Augusters club. He never tried to gain the political powers and remained all focused on the values and creative works that Gandhi ji tried hard to promote in the previous century. He believed the real social reform cannot be achieved through political power, it can only come through the moral authority, the kind that Mahatma Gandhi, Nelson Mandela and Martin Luther King possessed. Here he refers to the moral authority that arises out of the action on ground. His own long life is an embodiment of the Gandhian lifestyle. Yusuf Meharalli, his top source of inspiration, coined most powerful slogans of previous century i.e. Simon! Go Back, and Quit India. He used to be the most popular leader among students in Mumbai. GG is one of the founders of Yusuf Meharalli Centre that was started informally in 1961, and confirmed later with formal inauguration by Dr. Zakir Husain, the Vice-President of India in 1966. GG represents the spirit of certain socialist leaders like Yusuf Meharalli, Acharya Narendra Dev, Ram Manohar Lohia, J.P., Ram Nandan Mishra, Usha Mehta, etc. His thoughts and works on pertaining to the questions on social harmony can remind the sacrifices of Ganesh Shankar Vidyarthi. Defining the meaning of his name in life and works is one of virtues that he is known for. The three terms of Gunvantrai Ganpatlal Parikh are defined as the leader among the virtuous, son of the group’s leader, and an assayer or an examiner, respectively. At last, I want to say; Long live GG.Disclaimer: The views expressed in this article are of the author and not of Medical Dialogues. The Editorial/Content team of Medical Dialogues has not contributed to the writing/editing/packaging of this article.
1 year 2 months ago
Blog,News,Blog
STAT+: Pharmalittle: We’re reading about a California bill to restrain PBMs, a U.K. trade group scolding Novo, and more
And so, another working week will soon draw to a close. Not a moment too soon, yes? This is, you may recall, our treasured signal to daydream about weekend plans. Our agenda is fairly modest. We hope to catch up on our reading, spend time with our Pharmalot ancestor, and promenade with the official mascots.
We also hope to hold another listening party, where the rotation will likely feature this, this, this, and this. And what about you? This is a grand time to enjoy the great outdoors. Beaches and lakes are beckoning. City streets want to be strolled. And woods are inviting the adventurous for long mysterious walks. Take your pick. Or you could simply hide indoors and binge-watch something on the telly. Well, whatever you do, have a grand time. But be safe. Enjoy, and see you soon. …
A U.S. court tossed a U.S. Chamber of Commerce lawsuit challenging the Medicare Drug Price Negotiation Program established through the Inflation Reduction Act, with a judge finding that several plaintiffs in the suit lacked standing, STAT reports. U.S. District Judge Michael Newman for the Southern District of Ohio found that the Chamber’s argument it could sue on behalf of its members through associational standing was incorrect. The plaintiffs argued they could sue on behalf of pharmaceutical companies that are members of the organization — in this case, AbbVie and its subsidiary Pharmacyclics. Pharmacyclics is based in California, and AbbVie operates in Illinois, California, Massachusetts, and Washington, D.C., but the suit was filed with a local Chamber chapter in Dayton, Ohio.
California lawmakers are making a last-minute push before adjourning to restrain pharmacy benefit managers against the background of a national effort to rein in prescription drug prices, Bloomberg Law writes. Proponents of the bill, led by pharmacists, argue SB 966 would help place needed safeguards on the middlemen who negotiate with drug manufacturers and manage prescription benefits for employers. The bill would require PBMs to be licensed. Supporters say the companies have undermined competition and are financially squeezing smaller pharmacies. The effort comes as lawmakers in 41 states have filed more than 170 related bills this year to regulate PBMs.
1 year 2 months ago
Pharma, Pharmalot, pharmalittle, STAT+
Oropouche fever, the mysterious threat - The Lancet
- Oropouche fever, the mysterious threat The Lancet
- 'Sloth virus' reported in Europe for 1st time — but what is it? Livescience.com
- Oropouche Virus Outbreak Hits Europe as First Deaths Confirmed in Brazil ScienceAlert
- Travellers urged to stay ‘vigilant’ after Oropouche virus brought back to Europe The Telegraph
1 year 2 months ago
Health – Demerara Waves Online News- Guyana
Guyana closer to eliminating filariasis or ‘big foot’ disease
Guyana has almost eliminated filariasis, widely known locally as ‘big foot’, with remaining work to be done in only two of the ten administrative regions, Health Minister Dr Frank Anthony said, even as the United States Agency for International Development (USAID) and the Pan-American Health Organisation (PAHO) announced a new package of assistance to fight ...
Guyana has almost eliminated filariasis, widely known locally as ‘big foot’, with remaining work to be done in only two of the ten administrative regions, Health Minister Dr Frank Anthony said, even as the United States Agency for International Development (USAID) and the Pan-American Health Organisation (PAHO) announced a new package of assistance to fight ...
1 year 2 months ago
Health, News, 'big foot' disease, filaria parasite, lymphatic filariasis (LF), mass drug administration, Ministry of Health (Guyana), mosquito-borne disease, Pan American Health Organisation (PAHO), United States Agency for International Development (USAID)
Health Ministry: 666 dengue cases, 6 deaths - TT Newsday
- Health Ministry: 666 dengue cases, 6 deaths TT Newsday
- Dengue claims pharmacist Trinidad & Tobago Express Newspapers
- Bangladesh reports two more dengue deaths newagebd.net
- Trinidad & Tobago: Dengue deaths increase to eight teleSUR English
- Dengue fever: Two more deaths, 204 patients hospitalized in 24 Hours United News of Bangladesh - UNB
1 year 2 months ago
KFF Health News' 'What the Health?': The Walz Record
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
Minnesota Gov. Tim Walz is Vice President Kamala Harris’ choice of running mate. Walz — also a former U.S. congressman, high school teacher, and member of the National Guard — has a folksy, Midwestern affect and a liberal record. He has signed bills expanding abortion rights and medical care for transgender people as governor and represented a swing district in the House of Representatives.
Meanwhile, the number of abortions taking place in the U.S. since the overturn of Roe v. Wade continued to rise into early this year, according to a new study. That is frustrating abortion opponents, who are seeking more ways to bring the numbers down, even if it means barring pregnant women from traveling to other states.
This week’s panelists are Julie Rovner of KFF Health News, Sandhya Raman of CQ Roll Call, and Shefali Luthra of The 19th.
Panelists
Shefali Luthra
The 19th
Sandhya Raman
CQ Roll Call
Among the takeaways from this week’s episode:
- Walz has been active on health issues, including capping insulin prices, codifying access to abortion and gender-affirming care, and supporting veterans’ health, as well as challenging hospital consolidation efforts. In fact, the similarities between him and Harris highlight unity among Democrats on key health issues.
- Meanwhile, the GOP vice presidential nominee, Sen. JD Vance of Ohio, said in an interview that reforming the Affordable Care Act would still be on the table if Trump were reelected, though he did not elaborate. The lack of specificity in the GOP’s plans leaves a lot unknown about what a second Trump administration would do with health policy.
- A recent report shows the number of abortions continued to rise amid restrictions. How? Telehealth is a major reason for the trend. And a separate report shows hundreds of millions in taxpayer dollars have been funneled to crisis pregnancy centers since the overturn of Roe v. Wade, reflecting an effort in conservative state legislatures to steer funding to centers that discourage abortion.
- And Congress has departed for its August recess without funding the federal government, again. Those eyeing other must-pass legislation, such as extended telehealth flexibilities and pharmacy benefit manager reform, are banking on the lame-duck session after the election.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: JAMA Internal Medicine’s “Health, Access to Care, and Financial Barriers to Care Among People Incarcerated in US Prisons,” by Emily Lupton Lupez; Steffie Woolhandler; David U. Himmelstein; et al.
Shefali Luthra: KFF Health News’ “Inside Project 2025: Former Trump Official Outlines Hard Right Turn Against Abortion,” by Stephanie Armour.
Sandhya Raman: The War Horse’s “‘I Had a Body Part Repossessed’: Post-9/11 Amputee Vets Say VA Care Is Failing Them,” by Hope Hodge Seck.
Also mentioned on this week’s podcast:
- ProPublica’s “Texas Sends Millions to Crisis Pregnancy Centers. It’s Meant To Help Needy Families, But No One Knows if It Works,” by Cassandra Jaramillo, Jeremy Kohler, and Sophie Chou, ProPublica, and Jessica Kegu, CBS News.
- Vox’s “Free Medical School Won’t Solve the Doctor Shortage,” by Dylan Scott.
- Stat’s “How UnitedHealth Turned a Questionable Artery-Screening Program Into a Gold Mine,” by Casey Ross, Lizzy Lawrence, Bob Herman, and Tara Bannow.
- The Wall Street Journal’s “The One-Hour Nurse Visits That Let Insurers Collect $15 Billion From Medicare,” by Anna Wilde Mathews, Christopher Weaver, Tom McGinty, and Mark Maremont.
click to open the transcript
Transcript: The Walz Record
KFF Health News’ ‘What the Health?’ Episode Title: ‘The Walz Record’Episode Number: 359Published: Aug. 8, 2024
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello, and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News, and I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, Aug. 8, at 10 a.m. As always, news happens fast and things might’ve changed by the time you hear this, so here we go.
We are joined today via videoconference by Sandhya Raman of CQ Roll Call.
Sandhya Raman: Good morning.
Rovner: And Shefali Luthra of The 19th.
Shefali Luthra: Hello.
Rovner: No interview this week, but plenty of news for a hot summer week so we will get right to it. So for the second time in three weeks, we have a new vice-presidential nominee to talk about. Newly minted Democratic nominee Vice President Kamala Harris has chosen former congressman and current Minnesota Gov. Tim Walz to be her running mate. What do we know about Walz’s record on health care?
Raman: We know a lot. I think it’s easier to draw from his record compared to JD Vance, who was only elected for the first time in 2022. Tim Walz has had six terms in the House. He’s on his second term as governor. And from that you can see what his priorities are, how he’s drawn from his personal experience and the things that he’s been doing that are very in line with what either Biden and Harris or just Harris have done. When we had Biden, we hear a lot of talk about capping insulin costs, and that’s something that Walz signed a Minnesota bill for a few years ago. And he’s also been very active in reproductive health issues. He signed a couple abortion-related laws last year. That’s been a key focus of the Harris and Biden-Harris campaigns. He’s been active in talking about IVF and how his family has used that, also pretty in line with that.
Rovner: I love that he had a daughter using IVF, whose name is Hope.
Raman: Yeah, yeah.
Rovner: Very Midwestern.
Raman: Yes, and I think he’s also been pretty active on some of the veterans’ issues as a former member of the Army National Guard for several years. And just some of the education and health issues as a former teacher. And he signed legislation related to gender-affirming care as governor. So I think we have a pretty good idea of the types of things that he’d be interested in if they were elected.
Luthra: And I think what’s striking as well is how in line he seems to be on so many policy fronts to what we know the vice president and, frankly, what we know about the other people who were in contention for the vice-presidential nomination. And what I think that tells us is how unified a lot of the party is right now on health care and health policy issues in general. I was pretty struck by how quickly we got reactions from both pro-abortion rights groups and anti-abortion rights groups. As soon as the news came, SBA [Susan B. Anthony] Pro-Life America, one of the biggest anti-abortion groups, is quick to say this is the most pro-abortion ticket in history. They might be right.
Rovner: I was going to say it’s probably true.
Luthra: Yeah. And they could have said that about any Harris, et cetera, ticket, whether that was Walz, whether that was [Pennsylvania Gov. Josh] Shapiro, whether that was someone else from her reported list of finalists. And at the same time, what we saw from abortion rights advocates is they’re equally thrilled about this because they look at Walz as an ally. They look at the work that was done in Minnesota around getting rid of abortion bans; codifying abortion rights in the state constitution; limiting requirements like the 24-hour waiting period: That is gone in the state. And passing a shield law.
All of that underscores that he’s very in line with the vice president. I think what’s worth asking ourselves is how much does that matter when we have someone like Kamala Harris who is very interested in these issues. And in a way, we know far less about JD Vance. But whatever we could find out about him probably matters a lot more because Donald Trump has never shown much interest in health care or health policy. So if we did get a Trump-Vance ticket, it feels like there is a real possibility we’d have a lot more Vance influence in this area as opposed to Walz in a Harris-Walz administration.
Rovner: Which we’ll get to in a second. Just something that jumped out at me when I was researching this is that there’d been much made about the fact that Harris is the first presidential candidate who’s actually visited an abortion clinic. Well, so has Walz. So we’ve now got a presidential candidate and a vice-presidential candidate who have visited an abortion clinic. And I’m thinking even 15, 20 years ago on a Democratic ticket, how much the world has changed since the fall of Roe [v. Wade], that that never would’ve been something that anybody would’ve wanted to advertise. I think it speaks volumes as to really how big reproductive health is going to be going forward in this campaign.
Raman: They went together when they visited a clinic together in St. Paul [Minnesota] earlier. So I think that speaks to it, too, that it is a very important issue for both of them and that it is definitely going to be something the other side is going to really seize on and a point of distinction.
Rovner: Meanwhile, as Shefali alluded to, the Republicans continue to bob and weave on health care issues. Republican vice presidential nominee JD Vance told the news site Notice earlier this week that the ACA [Affordable Care Act] is indeed on the agenda for a second Trump administration, although he didn’t say exactly how. “I think we’re definitely going to have to fix the health care problem in this country,” was his exact quote. Any hints to what that might entail?
Raman: Honestly, no. I think that everything that we’ve heard so far has really just put multiple things up on the table without giving any specifics. Is the ACA repeal-and-replace still on the table? It depends on do we have a majority, do we have a minority, in Congress? And what would that even entail given that we had the whole thing in 2017 where it didn’t work out for them? And Trump has hinted back and forth and not been very clear, so we’re still not sure without more clarity from them.
Rovner: The rest of what JD Vance said was “Obamacare is still too expensive and a lot of people can’t afford it, and if they can’t afford it, they don’t get high-quality care, and we’re going to give them high-quality care.” And my thought was, that would be great. How on earth do you plan to make Obamacare less expensive and care higher quality? That seems like a rather tall order, but a great goal.
Luthra: And realistically, right? We don’t have, as Sandhya pointed out, a real record for JD Vance to look at. We do have a record for Donald Trump, but we don’t have statements of principle or value that we can really attribute to him. We don’t know what he really would do because we don’t know what he believes in. And that, I think, is why we put so much attention in the press. And why we’ve seen Democrats put so much attention on what Republican think tanks are talking about. And what the people who would staff those administrations would say. That is why something like Project 2025 merits so much scrutiny because those are the people who will be in power in institutions of government and potentially interpreting these kinds of vague sentences into actual policy that touches our lives.
Rovner: We don’t know very much of what Donald Trump really thinks about health care because he wants it that way. He wants to keep all of his options open. But one of the things that we do know is that he’s repeatedly promised not to touch Social Security or Medicare, the so-called third rails of American politics. He has specifically declined, however, to include Medicaid on that list of things that he won’t touch. And now we’re reading various proposals — as you mentioned, from Project 2025 to the Paragon Institute, which is run by a former Trump official — that are proposing various ways to scale back Medicaid, particularly federal Medicaid spending, possibly dramatically. Did they not learn from the 2017 repeal-and-replace fight that Medicaid, now that it covers like 90 million people, is kind of pretty popular?
Raman: I think that even after that, we’ve had so many times that we’ve seen in that administration trying to modify the ways that they can with Medicaid. We had the try to push for block grant proposals multiple times. We’ve had the work requirements try to come to fruition in multiple states before being struck down by the courts. And those things are still pretty popular if you look at the documents put out by a lot of these think tanks as something that could be brought up again. Including pulling back on expansion as a way that they see as really reducing federal spending, especially as they’re trying to reduce the national debt and just bring down costs in general.
Rovner: Pulling back on the federal match for expansion, more to the point.
Raman: Because Medicaid expansion is largely funded by the federal government. And so I think those are things that we could see given the history and the people that are working in those places and their connections to the former administration.
Luthra: And I do think it’s worth noting that Trump has said right now that he would not want to touch Social Security or Medicare. I think we can also put a few grains of salt, maybe some more salt, in there, because that is also what he said when he ran for president in 2016. And again, that isn’t really what he was as committed to as president. It was: What does [House Speaker] Paul Ryan want to do? What will I be willing to negotiate on? And with Trump in particular, there is such a distinction between knowing what is politically pragmatic to say in a campaign versus what is on the table as an administration, that I just think that it is incumbent on all of us to not take that with too much credibility, just in this very specific case.
Rovner: And also Social Security and Medicare sometimes need touching, saying that you’re not going to touch, leaving them on autopilot, is not a very responsible public policy. You actually do have to get under the hood occasionally and do things to these programs. But before we get to that, I want to talk a little bit more about abortion. This week, the Society of Family Planning, which is tracking the number of abortions around the U.S. in the wake of the Dobbs [v. Jackson Women’s Health Organization] ruling, reported that the volume of abortions continues to increase despite complete bans in 14 states and near-bans in several others. Shefali, how is this happening? Why is the number of abortions going up? One would think it would be going down.
Luthra: I think these numbers are really striking. They show a continuation of a trend, which is largely this increase in telehealth. More people getting abortion through, in some cases, shield law provision, living in states like Texas and getting pills mailed to them from doctors in New York. Or the fact that it is simply easier to get an abortion if you live in a state with abortion protections because telehealth is much more available right now. The numbers also do show more in-clinic care because people are traveling and overcoming great distances to get abortion.
One thing that I think is really important and that the authors had noted when this came out was these go through March. And on May 1, Florida’s abortion ban took effect, and that is one of the biggest abortion bans that we have seen since the Dobbs decision. And I think it will be really interesting to see whether the trend that we have been observing for quite some time — this steady increase and, in particular, growth of telehealth and continued travel — if that remains possible and viable when you lose a state with as many clinics and as many people as Florida had had.
Rovner: I saw Stephen Miller, the Trump adviser, on TV last night talking about “There will be no national abortion ban under Donald Trump,” which is a whole other discussion. But these numbers, and continuing to go up, must be making the anti-abortion movement crazy.
Luthra: They are losing their minds. They are deeply frustrated on two levels. They’re very concerned that people are finding ways to travel. That is not something they hoped for. And they are very concerned about telehealth in particular. And what they keep saying is they want to find some kind of legal strategy to challenge the shield law provision, but they haven’t quite figured out how. There is real talk in Texas among some of the anti-abortion activists. They’re trying to see is there a way we could pass legislation in a future session to perhaps ban internet providers from showing the websites that allow you to order medication abortion.
Something like that. All of this would be fought through the courts. All of this would be heavily litigated. But it is their No. 1 priority because it is an existential threat to abortion bans. Obviously, they are waiting to see what happens in the presidential election because if you do have an administration that is willing to restrict the ability to mail mifepristone through rehabilitating the Comstock Act — not passing a national abortion ban, but using older laws on the books — then that does some of the job for them and could very significantly put a dent in or even halt this trend.
Rovner: Well, speaking of the abortion pill, we’re seeing pressure campaigns from both sides now aimed at some of the big corporations, including Costco and Walmart, that could start selling the abortion pill in their brick-and-mortar pharmacies. This is something that the Food and Drug Administration, at least, started to make easier earlier in the Biden administration. Now we have institutional investors from blue states pushing companies to carry the drug to make it more available, or else they will divest their very large stock holdings. While we have institutional investors that represent anti-abortion groups, like the American Family Association, who are threatening to divest if the companies do start selling the abortion pills, I would not like to be on the board of any one of these big corporations right now. This seems like a rather uncomfortable place for them to be.
Luthra: Yeah, and none of this is surprising. Alice Ollstein, regular contributor to this podcast, broke a really great story, gosh, a year and a half ago now, when we saw that even CVS and Walgreens, for a time, didn’t want to distribute mifepristone in states where abortion was legal, but there were threats of litigation from attorneys general. And that has changed. The story points out that we have CVS and Walgreens carrying these pills and distributing them. But a lot of people do get medication from Costco. A lot of people do get medication from Walmart. What we’ll see is that this is just another way in which the fight over abortion, which has real meaning for so many people, just continues to play out in the corporate sector. It is something that has been true since Dobbs happened. It is just another sign of how much people care about this and the money behind it and the chaotic nature of banning a procedure in some states and heavily stigmatizing it even in others.
Rovner: The ripple effect of the Dobbs decision. I really do think the Supreme Court had no great appreciation for just how far into other facets of American life this was going to spread, which it definitely is. Well, even as abortions are going up, states with abortion bans are spending increasing amounts of taxpayer money on anti-abortion crisis pregnancy centers that try to talk pregnant people out of terminating their pregnancies. This is flying under the radar, I feel like. We’ve seen these crisis pregnancy centers have been around for a very long time, but what we haven’t seen is the amount of money that states are now saying, “Well see, we care about pregnant women, even though we’re banning abortion, because we’re giving all this money to these crisis pregnancy centers.”
Luthra: And I was pretty struck by just how much money we have seen states put into these centers since the Dobbs decision. The report that you highlight, Julie, found that it was almost $500 million across all these states has gone in since 2022. That’s almost half a billion dollars going into these centers. And you’re right that they do fly, in some ways, under the radar. And part of that is because it is very hard to know how they spend that money. They have very, very little accountability built in place. They are not regulated the way that health care systems are. That also means if you’re a patient and you go there for seeking health care, you are not protected by HIPAA necessarily. And you often will get “care” that can be inaccurate or misleading because, fundamentally, these institutions exist to try and deter people from getting abortions, from … staying pregnant and having children.
I do think that we will see more and more of this happen, and in some ways Republicans have been very overt about that. This was the focus of the March for Life. We saw a bunch of bills in Congress that Republicans put forth talking very specifically about federal funding for anti-abortion centers. This was the biggest trend we saw in statehouses this year when it came to abortion, was passing bills that would add more funding to anti-abortion centers. It’s one area where they feel like the political consequences are far less than bans because bans are unpopular and people don’t fully understand and know what these are. And so they’re not going to get as upset with you when they hear, “Oh, you put more money into these places that are supposed to help pregnant people.” Even though the reality is we don’t actually have any metrics or data that show that they do, and we do have a lot of journalism that shows that they mislead people.
Rovner: Yeah. I will put the link back to the good investigation that ProPublica did that we talked about a couple of weeks ago about how all the money in Texas is impossible to track, basically. All right, well, the Senate last week followed the House’s lead and recessed until early September, which leaves them just a few legislative days when they get back to either finish up all 12 of the regular spending bills — spoiler, that is not going to happen — or else pass some sort-of continuing resolution to keep the government open after the Oct. 1 start of fiscal 2025. Sandhya, they went into this — we’ve said this before — with so much optimism from the Republicans: “We’re going to get these all done before Oct. 1.” Where are we?
Raman: So, at this point, we’ve gotten some work done, but it’s very unlikely we would have things done before the end of September. So the House was on track initially to vote on the House floor on their Labor HHS [Health and Human Services] spending bill, but it got derailed after there were some issues with another bill, the energy-water bill, and after they’d fallen short on their legislative branch spending bill, they recessed early.
Rovner: We should point out that while “Labor-H” is always hard to pass, those other ones tend not to be … those are ones that usually go through.
Raman: Yeah, Labor H generally is done near the end of the whole slate just because it is notoriously one of the trickier ones to get all the agreement on. And it is the biggest nondefense spending bill. So it takes longer, and so less far along on the progress with that, and we’re in August recess, both chambers are out. We won’t see any progress until September. Before the Senate left, they did advance their spending bill on the committee level. That went a lot differently than the House’s markup. So we had three people opposed, but everyone else was pretty much in agreement. A lot less eventful. It wasn’t focused on amendment debate and it was bipartisan, which is a big thing.
So we will see it when they come back, if they gravitate a little bit more towards this, if they’re shifting a little bit in between the two bills. But I think another thing to keep in mind is they have so little time this year to get so much done. They have so much recess this year for the election that it really puts a crunch on their timeline. And then there are certain people advocating that if this person wins, if that person wins, should we do a shorter-term plan spending bill so that we can get our priorities in if this party’s in control, this party has more control. So it’s a difficult situation.
Rovner: Yeah. Here we are basically heading into the home stretch for the spending bills with a gigantic question mark. As usual. Every year they say, “This won’t happen next year.” Every year this happens next year. Well, meanwhile, this is our midyear reminder that Congress also has to pass a bunch of other bills to do things like preventing some pretty big cuts to Medicare physician pay, to keep community health centers and safety-net hospitals up and running, and they have to do all this by the end of the year. I assume we’re still looking at a postelection, lame-duck session to try to wrap everything together.
Raman: I think that’s what we’re looking at. The big priority is going to be to get the government funded. And I think. as with previous years, will we get some of these other things tacked onto there? Will we get extension of telehealth flexibilities or some of the PBM [pharmacy benefit manager] reform or some of the other things that we’ve been discussing at the committee level and hoping to get across the finish line? But it’s really difficult, I think, to get some of those things done until we have this broader package. And I think it’s important that some of the times when we get the broader package, it can help pay for other of the programs that we’ve been considering at the committee level.
Rovner: That was just what I was going to say. The PBM reform, in particular, saves money. Gee, you can prevent the physician pay cut and fund community health centers.
Raman: Yeah. So I think a lot of it will depend on how quickly they’re able to get to an agreement. And if you look at the differences between the House and the Senate bills, it’s billions of dollars. I think just on health spending, it was like almost a $16 billion difference in the top line number between the bills. So getting to some sort of middle ground is going to take some time to get there.
Rovner: Well, before we leave the Hill for the rest of the summer, the Senate Health, Education, Labor, and Pensions Committee, where Democrats and Republicans have not always seen eye to eye under Chairman Bernie Sanders, actually came together last month to open an investigation into, and issue a subpoena to, the CEO of Steward Health Care. You may remember we talked about Steward back in May. It’s a Dallas-based, physician-owned hospital group that was sold to a private equity firm, which promptly sold the real estate the hospitals were sitting on, forcing them to then pay rent. Then the private equity group basically cashed out. And now the hospitals are floundering financially, which is threatening patient care in several states. This is the first time the committee has issued a subpoena since 1981. I did not know that before this week. And it’s kind of a big deal. This is the first, I think, I feel like, big investigation, at least among this committee, about the consequences of private equity in health care.
Raman: Yeah, I would say that, and especially because this is bipartisan. And I think there have been so many bipartisan issues over the past couple of years that it has been difficult to get the chairman and the ranking member to see eye to eye on or to prioritize in the same order. And so I really do think it is a big deal to be able to issue that subpoena and have the CEO come in in September.
Rovner: Yeah, this will be interesting. [Sen.] Bernie Sanders made a big point of dragging up some of the drug company CEOs who said pretty much what we expected them to say. But this is a little bit of a different situation and there’s a bunch of senators from both parties who have hospitals in their states that are now being threatened by the bankruptcy of Steward Health Care, so we’ll see how that goes. Speaking of profiteering in health care, we have two really excellent stories this week on pretty much the same subject: Stat News as part of its continuing investigation into the way UnitedHealthcare is squeezing extra money out of the Medicare program, particularly the Medicare Advantage program, has a piece on the use of a questionable test that’s used to diagnose peripheral artery disease, which can dramatically increase the Medicare Advantage payment for a patient who has it, just kind of coincidentally.
Along similar lines, The Wall Street Journal has a story looking at how not just United, but other major Medicare Advantage insurers, including Humana and Aetna, are using the same test, often provided during a “free home visit” by a nurse practitioner, and scoring those very same extra Medicare Advantage payments. Now, I’m old enough to remember when the biggest knock on Medicare Advantage was that, because it had fixed payments, it gave insurers an incentive to skimp on care. So we had lots of patients who couldn’t get care that they needed. Now that the payments are risk-adjusted, there’s an incentive for insurers to give too much care, or at least to suggest that patients need more care than they do; like that maybe they have peripheral artery disease when they don’t, really. Are there any suggestions floating around how to fix this? Shefali, you were alluding to this, that Medicare Advantage, in particular, can be a little bit of a sinkhole for federal funds.
Luthra: I think this is something that we have struggled with for a long time, right. And I think I was always thrilled to see a Bob Herman byline and we get another one on this Stat story. And one thing that he has written about so compellingly is that the sheer power that health care providers have. And I think we just can’t really ignore the role that they play then in being able to get all of this federal money into their system for things that we don’t necessarily need. And that’s not an easy thing to address politically because people like their hospitals. And even when you hear from lawmakers who want to talk about better regulation of hospitals, they really only talk about for-profit hospitals. Even though if you were to go to a for-profit or not-for-profit, you might see some similarities in how they approach what they bill for. And this is something that we haven’t figured out a good solution to because of how our politics work. But I’m really grateful that we get more reporting like this that helps remind us just how skewed the incentives are in our system.
Rovner: Yeah, it’s hard to blame them. These are for-profit companies that have shareholders, and their job is to figure out how to make money for their shareholders. And they do it extremely well. But the money that they’re making is coming from U.S. taxpayers, and there are patients who are caught in the middle. It’s been a thorny issue. This has been what we’ve been fighting about with Medicare for Medicare’s entire 59 years of its existence. So that will continue while we try to figure out everything else, like making this year’s budget work. Finally this week, we reported in July how Michael Bloomberg gave his alma mater, Johns Hopkins University, another billion dollars that will, among other things, eliminate medical school tuition for most of its student body. We pointed out at the time that the schools that have gone tuition-free have not actually succeeded either in getting more students to go into primary care.
There’s the concern that if you have a lot of debt, you’re going to want to go into a specialty to pay it off. Nor has it enabled more students of color to become doctors. So now Bloomberg is making his philanthropy a little bit more direct. He’s giving a combined $600 million to the four historically Black colleges and universities that have their own medical schools, including Howard [University] here in D.C., in hopes of more directly addressing equity issues that go along with patients not being able to get culturally sensitive care. HBCUs educate the vast majority of the nation’s Black doctors, so is this finally a step in the right direction with the medical education and health equity?
Raman: I would argue it is. Like you said, if you look at the data, the American Association of Medical Colleges [Association of American Medical Colleges] said half of Black doctors graduate from one of these schools. And that could really increase some of the uptake of preventative care and trust in medicine in the Black community who, I think they’ve done some polling, that are more comfortable a lot of times with other Black doctors. And I think that another point was the money is also starting another medical school to increase that pipeline as well. And that is another big thing where it’s broadening the pipeline, but also just really feeding into these goals, should be big over time.
Rovner: A continuing effort, I think there. All right, well, that is the news for this week. It’s time for our extra-credit segment. That’s when we each recommend a story we read this week we think you should read, too. As always, don’t worry if you miss it. We will post the links on the podcast page at kffhealthnews.org and in our show notes on your phone or other mobile device. Sandhya, you got yours picked first this week. Why don’t you tell us about your extra credit?
Raman: So I chose, “‘I Had a Body Part Repossessed’: Post-9/11 Amputee Vets Say VA Care Is Failing Them.” And it’s by Hope Hodge Seck at The War Horse. And it is just a really excellent piece looking at some of the concerns that amputee vets have been having and what the shortcomings are in the care from the VA [U.S. Department of Veterans Affairs], not having bills paid for some of the prosthetics or just delays in receiving them. And one interesting issue that was brought up there is that VA care for post-9/11 amputee veterans doesn’t take into account some of the needs for that population. They’re very different from maybe the needs of senior veterans. And it goes into more about how Capitol Hill is hearing some of these concerns. But read the story and learn more.
Rovner: Shefali?
Luthra: This is from KFF Health News. It is by Stephanie Armour. It is on a topic we discussed earlier on this podcast. The headline is “Inside Project 2025: Former Trump Official Outlines Hard Right Turn Against Abortion.” And what I love about this piece is it does a great job going into detail about the reproductive health ideas and agenda that is outlined in Project 2025. But I also really love that it ties that to the people who are involved in Trump World. Right? And it talks about who are the people who wrote this. Roger Severino, obviously a huge name, very anti-abortion, was involved in Trump’s HHS when he was president last time, and …
Rovner: Did the Office for Civil Rights.
Luthra: Exactly, which has huge implications for abortion policy and reproductive health policy. And I think that Stephanie does a really great job of getting into the political back and forth that has emerged over Project 2025, in which Trump himself has tried to distance himself from the document, from what it outlines and what it says. But that doesn’t really stand up to scrutiny when we look at the authors because it is largely people who have worked for Trump, have advised him, and are likely to have influential roles coming forward. There’s also some ties between JD Vance and the folks at [The] Heritage [Foundation] and Project 2025 that really solidifies the notion that this is something that could be very influential in dictating what our country would look like under a Trump-Vance presidency. And I appreciate Stephanie’s work in clarifying what it says.
Rovner: Yeah, it’s a really good story. Well, my extra credit this week is a study in JAMA Internal Medicine. It’s from the Cambridge [Health] Alliance at Harvard and is called “Health, Access to Care, and Financial Barriers to Care Among People Incarcerated in US Prisons.” And it looks at something that I didn’t even know existed: copays required in prisons for prison inmates in order to obtain medical care. The study found, not surprisingly, that copays can be equal to more than a week’s wage for some inmates, who often make just pennies an hour for the work that they do behind bars. And that many inmates end up going without needed care because they can’t afford said copays.
It’s pretty eye-opening and I hope it gets some attention. OK, that is our show. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left us a review; that helps other people find us, too. Special thanks as always to our technical guru, Francis Ying, and our editor, Emmarie Huetteman. As always, you can email us your comments or questions; we’re at whatthehealth@kff.org. Or you can still find me at X, I’m @jrovner. Sandhya?
Raman: @SandhyaWrites.
Rovner: Shefali?
Luthra: @shefalil.
Rovner: We will be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 2 months ago
Elections, Multimedia, States, The Health Law, Abortion, KFF Health News' 'What The Health?', Minnesota, Podcasts, reproductive health, Telemedicine, U.S. Congress, Women's Health
New species of bug known for carrying 'Yellow Fever' found in Colorado - The Denver Gazette
- New species of bug known for carrying 'Yellow Fever' found in Colorado The Denver Gazette
- New mosquito species found in Grand Junction FOX 31 Denver
- New mosquito species detected in Mesa County WesternSlopeNow
- New mosquito species identified in Mesa County, systems in place to monitor and protect community Mesa County Public Health
- No reason for alarm with new mosquito found in Mesa County Grand Junction Daily Sentinel
1 year 2 months ago
PAHO/WHO | Pan American Health Organization
PAHO intensifies support to Central America to control dengue
PAHO intensifies support to Central America to control dengue
Cristina Mitchell
8 Aug 2024
PAHO intensifies support to Central America to control dengue
Cristina Mitchell
8 Aug 2024
1 year 2 months ago
Health Archives - Barbados Today
Return to mask-wearing, officials urge as new COVID variant spreads
Medical experts are calling on people to resume wearing masks as a new, more transmissible variant of COVID-19 gains dominance on the island.
No mask mandate has been issued.
Medical experts are calling on people to resume wearing masks as a new, more transmissible variant of COVID-19 gains dominance on the island.
No mask mandate has been issued.
The Barbados Association of Medical Practitioners (BAMP) has stressed that whilst caution is necessary, there is no cause for alarm. While the variant has been here for several months, this strain is a more dominant one.
BAMP President Dr Lynda Williams told Barbados TODAY: “It has greater transmission . . . it doesn’t have any greater mortality, but anything that can spread faster will affect the vulnerable people most quickly, so we have to go back to the usual hand-washing and wearing of masks around people who are vulnerable and especially if they are working with them.”
The variant, known as JN1, is a sub-variant of Omicron. Its presence was first confirmed by the Ministry of Health in January, alongside a rise in respiratory illnesses including Influenza A and B and COVID-19.
Dr Williams advised that individuals vaccinated in 2020/2021 and who did not receive any boosters since then, the extent of their protection would have waned.
She said: “We will watch and see what happens; there is no need to panic, we just need to remember it’s still out there and those who are elderly or have uncontrolled comorbidities such as diabetes, they are at risk.”
Chief Medical Officer Dr Kenneth George clarified that the mask mandate has not been reintroduced. But he urged vulnerable people, including the elderly, pregnant women, and those with chronic non-communicable diseases, to take precautionary measures against respiratory illnesses.
According to the US Centres for Disease Control and Prevention (CDC), JN1’s symptoms are similar to those of other strains, including sore throat, congestion, runny nose, cough, fatigue, headache, muscle aches, fever or chills, loss of sense of taste or smell, and shortness of breath or difficulty breathing.
The CDC notes that symptom type and severity usually depend more on an individual’s underlying health and immunity than on the specific variant causing the infection.
Despite COVID-19 no longer being classified as a disease of international public health concern, the Ministry of Health continues to test and monitor for COVID-19 strains, acknowledging that transmission of the virus has not ceased.
As the situation develops, health officials are advising people to exercise caution in crowded spaces and to prioritise protective measures, particularly for those at higher risk. (EJ)
The post Return to mask-wearing, officials urge as new COVID variant spreads appeared first on Barbados Today.
1 year 2 months ago
COVID-19, Health, Local News
U.S. Selected Practice Recommendations for Contraceptive Use, 2024 - CDC
- U.S. Selected Practice Recommendations for Contraceptive Use, 2024 CDC
- Health Officials Urge Doctors to Address IUD Insertion Pain The New York Times
- As IUD Horror Stories Go Viral, the CDC Is Finally Offering Pain Management Guidance Vogue
- Many Doctors Underestimate the Pain of IUD Insertion for Women. The CDC Wants to Change That The Elkhart Truth
- CDC provides updated contraception guidelines Contemporary Obgyn
1 year 2 months ago
Soups And Shakes Diet Can Put Type 2 Diabetes Into Remission, Study Finds - ScienceAlert
- Soups And Shakes Diet Can Put Type 2 Diabetes Into Remission, Study Finds ScienceAlert
- U.K. Type 2 Diabetes Program Puts 32% Of Patients Into Remission Forbes
- Why the soup and shake diet really works (if you can stick to it) The Telegraph
- NHS ‘soup and shake’ diet puts almost a third of type 2 diabetes cases in remission The Guardian
- Remission of type 2 diabetes feasible with soup and shake diet intervention Medical Xpress
1 year 2 months ago
Health – Demerara Waves Online News- Guyana
Guyana takes steps for US to lift catfish ban
Guyana continues to take numerous steps to convince the United States Department of Agriculture (USDA) that the now six-year-old ban on catfish exports should be lifted, officials said Wednesday. Chief Fisheries Officer of the Ministry of Agriculture, Denzil Roberts said Guyana’s relevant fisheries regulations and inspection manuals have been updated. US Ambassador to Guyana, Nicole ...
Guyana continues to take numerous steps to convince the United States Department of Agriculture (USDA) that the now six-year-old ban on catfish exports should be lifted, officials said Wednesday. Chief Fisheries Officer of the Ministry of Agriculture, Denzil Roberts said Guyana’s relevant fisheries regulations and inspection manuals have been updated. US Ambassador to Guyana, Nicole ...
1 year 2 months ago
Agriculture, Business, Food, Health, News, Politics, Ministry of Agriculture (Guyana), United States catfish ban, United States Department of Agriculture (USDA)
PAHO/WHO | Pan American Health Organization
La OPS fortalece el acceso a datos de salud a través de su Portal de Indicadores Básicos
PAHO strengthens access to health data through its Core Indicators Portal
Cristina Mitchell
7 Aug 2024
PAHO strengthens access to health data through its Core Indicators Portal
Cristina Mitchell
7 Aug 2024
1 year 2 months ago
Health – Demerara Waves Online News- Guyana
Dengue vaccination won’t be totally effective -Health Minister
Guyana is hesitant to vaccinate people against dengue because of the efficacy of the jab against all of the four sub-types of the mosquito-borne virus, cost and availability of the vaccines, Health Minister Dr Frank Anthony said Wednesday. With ten people already killed by dengue in 2023 and four this year, he said government would ...
Guyana is hesitant to vaccinate people against dengue because of the efficacy of the jab against all of the four sub-types of the mosquito-borne virus, cost and availability of the vaccines, Health Minister Dr Frank Anthony said Wednesday. With ten people already killed by dengue in 2023 and four this year, he said government would ...
1 year 2 months ago
Health, News, cost, dengue, dengue vaccines, Pan American Health Organisation (PAHO)
Q&A: Susvimo delivers immediate durability after implantation in wet AMD
Nearly 2 years after it voluntarily recalled Susvimo, Genentech recently announced plans to reintroduce the implant.In July, the FDA approved a post-approval supplement to the biologics license application for Susvimo (ranibizumab injection 100 mg/mL), which continuously delivers a customized formulation of ranibizumab through the port delivery platform for the treatment of wet age-related macu
lar degeneration. Susvimo is inserted during a one-time outpatient procedure and refilled every 6 months.Healio spoke with Chris Brittain, senior vice president and global head of ophthalmology product
1 year 2 months ago