Two hospitals participate in landmark bariatric surgery
The Metropolitan Hospital of Santiago (HOMS) and the Centers for Diagnostics, Advanced Medicine, and Telemedicine (Cedimat) made history by introducing the MagDI System for bariatric surgery against obesity. It is a milestone in bariatric and metabolic surgery in the Dominican Republic.
The Metropolitan Hospital of Santiago (HOMS) and the Centers for Diagnostics, Advanced Medicine, and Telemedicine (Cedimat) made history by introducing the MagDI System for bariatric surgery against obesity. It is a milestone in bariatric and metabolic surgery in the Dominican Republic.
HOMS, together with its Digestive, Bariatric, and Precision Surgery Institute, and in collaboration with Jenner Dominicana, performed the first Magnetic Bariatric Surgery in the Dominican Republic, Central America, and the Caribbean, consolidating its position as a regional benchmark in surgical innovation.
For the first time
Magnetic bariatric surgery, performed at Homs and Cedimat, is a hybrid procedure that creates a partial bypass of the small intestine (between the duodenum and ileum) by placing a magnet endoscopically in the duodenum and another laparoscopically in the ileum.
These magnets attract each other to form an anastomosis, which allows for a faster recovery with less pain, no blood loss, and a lower risk.
In Santiago, the procedure was attended by Rafael Sánchez Español, General Director and bariatric surgeon; Héctor Sánchez Navarro, Head of Robotic and Bariatric Surgery; and James Hamilton, Director of Innovation and Quality.
This team had the honor of welcoming Michel Gagner, a Canadian pioneer in bariatric surgery and creator of the MagDI technique used in this procedure. Also present were Brígida Navarro, gastroenterologist and director of the Center for Digestive Studies, and Luis Peralta.
From Cedimat
In its press release, the company states that it has consolidated its leadership in the treatment of obesity and type 2 diabetes with the introduction of the revolutionary MagDI system, a minimally invasive bariatric and metabolic technique that marks a significant milestone in Dominican medicine. This advancement was presented by Dr. Luis Alfredo Betances, director of the Bariatric and Metabolic Surgery Program at CEDIMAT, along with Dr. Michel Garnier (creator of the technology) at the Bariatric Institute.
1 month 3 weeks ago
Health, Local
The Dominican Republic launches a campaign against dengue fever. How is the country doing?
Las Caobas, Santo Domingo Oeste. – Health Minister Víctor Atallah reported that the Dominican Republic has seen a reduction of more than 85% in dengue cases nationwide, a result of the impact of preventive and educational efforts deployed throughout the country.
During the nationwide relaunch of the “Let’s Beat Dengue” campaign, under the slogan “Eliminate, Clean, and Cover,” the Minister of Health emphasized that prevention efforts have allowed the country to be recognized as a leader in disease control.
He also affirmed that the achievements in the fight against dengue are the result of coordinated efforts with the Provincial Directorates and Health Areas (DPS/DAS), as well as the active participation of communities. He specified that the campaign will have a renewed focus on education and the control of mosquito breeding sites.
“We have demonstrated that prevention works. The country today shows encouraging figures that reflect the dedication of our personnel and the commitment to protecting the health of the Dominican people. Now we will redouble our efforts to sustain and expand this success, and continue winning the battle against dengue,” Atallah stated.
The campaign was launched simultaneously in all DPS/DAS (Dental Health Departments).
According to data from the Epidemiology Directorate, between epidemiological weeks 1 and 32 of this year, 171 confirmed cases were reported, compared to the 1,110 cases recorded in the same period in 2024, reflecting a reduction of more than 85%.
The trend in dengue fever over the past four weeks has also shown a downward trend, with EW 32 having the lowest number of cases, with only one confirmed report.
Juan Manuel Méndez García, executive director of the Emergency Operations Center (COE), stated that the campaign has a positive impact, emphasizing that prevention is a fundamental pillar in the effort to protect the population.
He also stated that the COE is joining these actions, reinforcing its commitment to working together to ensure the well-being of citizens.
Speaking at the opening ceremony, Ancell Shecker, Vice Minister of Technical and Pedagogical Affairs of the Dominican Republic’s Ministry of Education (MINERD), emphasized that health and education are national causes and that it is everyone’s responsibility to work on disease prevention. Therefore, today, the Ministry of Education is joining the “Let’s Beat Dengue” campaign.
The Dominican Republic was recognized by the Pan American Health Organization (PAHO) for its effective management of dengue fever, particularly in 2024, when the country was named a regional leader in disease control amid a rise in cases in other nations.
As part of the campaign, educational workshops, community operations to eliminate breeding sites, targeted fumigations, junk removal, distribution of informational materials, and distribution of abate (larvicide), in addition to providing guidance to the population, will continue to be carried out with the goal of keeping the disease under control.
Among the complementary initiatives is the National Plan for the Prevention and Control of Dengue, developed with the support of PAHO, which has prioritized social interventions.
Also present at the “Anti-Dengue Family” strategy, developed in coordination with the Ministry of Education and PAHO, is the “Anti-Dengue Family” strategy, which trains students and teachers to multiply preventive efforts in their communities.
The Ministry of Health reiterated that the key to defeating dengue lies in joint action between authorities and the population, urging continued implementation of preventive measures in homes and communities.
Present at the campaign relaunch were Edisson Feliz Feliz, director of the Metropolitan Regional Health Service, and Alba María Ropero Álvarez, representative of the Pan American Health Organization (PAHO).
1 month 3 weeks ago
Health, Local
Debate on the effectiveness of dengue control
While the Ministry of Health maintains that dengue fever is under control in the Dominican Republic, the former director of the National Health Service (SNS), Dr. Nelson Rodríguez Monegro, asserts that no such strategy exists to combat the viral disease.
This year, 2025, is not an epidemic year, and if the country receives an award for control, it should be given to other countries on the continent that have better indicators. Rodríguez Monegro referred to the statements of the Minister of Public Health, Víctor Atallah, who stated that the Dominican Republic has recorded a 78% reduction in dengue cases, thanks to the work carried out by provincial and regional health departments. For the pediatrician and former director of the SNS, the reduction in dengue cases is not due to any implemented strategy; rather, 2025 is a non-epidemic year with a low incidence of the disease. “The decline in dengue cannot be attributed to official campaigns, since when there is a dengue prevention and control campaign, it is felt in the community,” he said.
What is happening in all countries of the Americas is that there is a significant reduction in the incidence of dengue, because this is a year of low incidence and possibly the next one as well, unlike 2022 and 2023, he explained.
Under the criteria used by the Dominican authorities, all of America should be declared champions in the fight against dengue.
Official position
The Ministry of Health called on citizens to join efforts to reduce dengue transmission. The Ministry of Health continues to strengthen vector control efforts to reduce dengue transmission in the country. It stated that mosquito breeding site elimination campaigns, community education on hygiene habits, and fumigation efforts have been intensified.
The Ministry also stated that it has implemented various actions as part of the National Dengue Plan, intending to reduce the incidence of this disease. It also said it has relaunched the “eliminate, clean, and cover” campaign. This week, data for week 33 were released.
Preventive measures against dengue include eliminating mosquito breeding sites (such as stagnant water in containers and tires), protecting against mosquito bites with repellent, and using mosquito nets over beds, doors, and windows.
Public Health urges people to visit the nearest health center if they experience symptoms such as a sudden high fever, severe headache (especially behind the eyes), muscle and joint pain (“breakbone fever”), nausea, vomiting, and a skin rash.
A confirmed case of dengue was reported this week, bringing the total number of cases to 174.
1 month 3 weeks ago
Health, Local
Rising respiratory illnesses in Grenada demand immediate action
“Recent surveillance data indicate a significant increase in cases of acute respiratory infections, including a resurgence of Covid-19”
View the full post Rising respiratory illnesses in Grenada demand immediate action on NOW Grenada.
“Recent surveillance data indicate a significant increase in cases of acute respiratory infections, including a resurgence of Covid-19”
View the full post Rising respiratory illnesses in Grenada demand immediate action on NOW Grenada.
1 month 3 weeks ago
Health, Notice, PRESS RELEASE, coronavirus, COVID-19, gis, Ministry of Health, respiratory infection, shawn charles
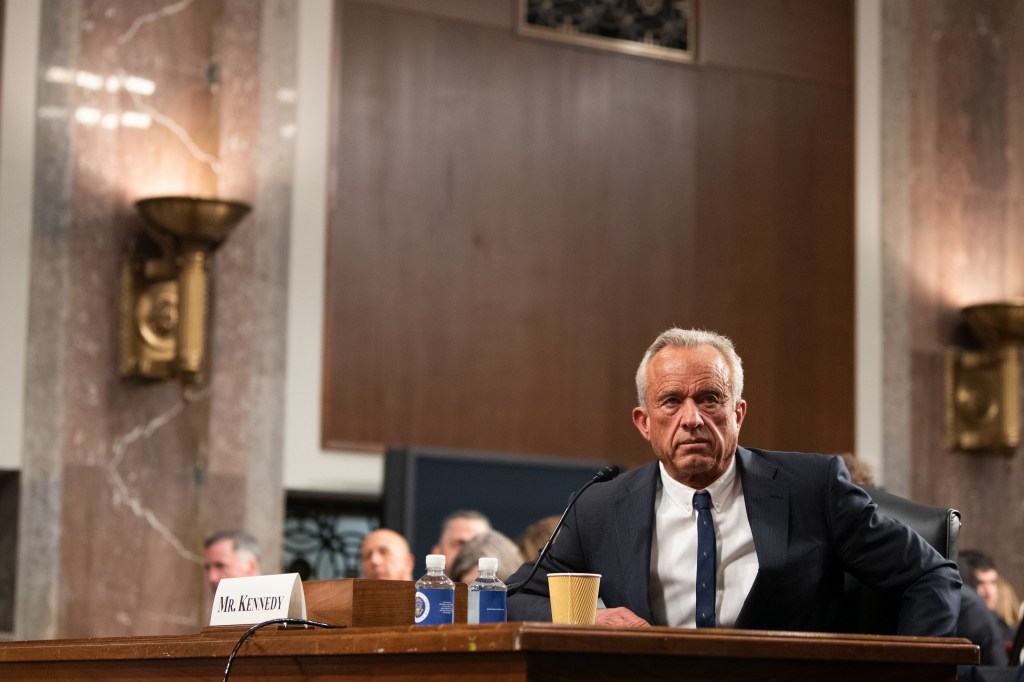
Estrategia antivacunas de Kennedy podría forzar el retiro de vacunas del mercado, advierten fabricantes
Durante una cena bajo palmeras en la terraza de Mar-a-Lago en diciembre, el presidente electo Donald Trump tranquilizó a los directores ejecutivos de las farmacéuticas Eli Lilly y
Durante una cena bajo palmeras en la terraza de Mar-a-Lago en diciembre, el presidente electo Donald Trump tranquilizó a los directores ejecutivos de las farmacéuticas Eli Lilly y Pfizer diciéndoles que el activista antivacunas Robert F. Kennedy Jr. no sería una elección radical para dirigir el Departamento de Salud y Servicios Humanos (HHS).
“Creo que va a ser mucho menos radical de lo que imaginan”, aseguró Trump ese mismo mes durante una conferencia de prensa en su complejo turístico en Palm Beach, Florida.
Ocho meses después, Kennedy ha intensificado sus ataques contra el sistema de vacunación.
Uno de sus principales objetivos es un programa federal de compensación que resuelve reclamos de daños por vacunas.
Según algunos expertos legales y líderes en salud pública, su estrategia podría llevar a la quiebra o al debilitamiento del fondo, obligando a las farmacéuticas a asumir riesgos legales y costos que las llevarían a dejar de fabricar vacunas por completo.
“Es una agenda radical”, dijo Angela Rasmussen, viróloga de la Organización de Vacunas y Enfermedades Infecciosas de la Universidad de Saskatchewan en Canadá. “Está usando varios mecanismos distintos y realmente no hay límites. La gente va a empezar a darse cuenta, pero no será suficiente para detener la ola de muertes, incluidas las de niños”.
Kennedy ha dicho que es necesario reformar el sistema de vacunación en el país porque, según él —sin ofrecer evidencia—, las vacunas están relacionadas con el autismo, la neurotoxicidad, las alergias y la muerte. Es una de las figuras líderes del movimiento “Make America Healthy Again” (“Hagamos a Estados Unidos Saludable Otra Vez”), una campaña informal que rechaza la medicina tradicional y promueve la llamada “libertad médica”.
Muchos de sus seguidores se oponen a las vacunas y creen que son peligrosas, a pesar de la evidencia científica que demuestra lo contrario.
Kennedy ha reconocido que quiere reformar el fondo de vacunas, conocido como el Programa de Compensación por Lesiones Causadas por Vacunas (VICP, por sus siglas en inglés). El 28 de julio escribió en la red social X que “el VICP está roto, y pienso arreglarlo”. El Departamento de Salud y Servicios Humanos (HHS) está trabajando con el Departamento de Justicia para reformar el programa, que protege a las farmacéuticas de la mayoría de las demandas por lesiones.
El HHS no respondió a la solicitud de entrevista con Kennedy, pero funcionarios de la agencia dijeron que él no está en contra de las vacunas. “El secretario Kennedy no es antivacunas: está a favor de la seguridad, la transparencia y la rendición de cuentas”, dijo por correo electrónico Vianca Rodríguez Feliciano, vocera del HHS.
Sin embargo, según personas familiarizadas con las discusiones internas —que pidieron no ser identificadas porque no están autorizadas para hablar sobre el tema—, Kennedy ha estado trabajando en silencio para restringir la disponibilidad de vacunas ampliamente utilizadas.
Una estrategia con varios frentes
La estrategia comenzó a tomar forma en la primavera. El primer paso fue sembrar dudas infundadas sobre la seguridad de las vacunas. En una reunión de gabinete en abril, Kennedy le dijo a Trump que el HHS estaba realizando un estudio masivo para identificar la causa del aumento de diagnósticos de autismo para septiembre.
Según informes de prensa, Kennedy asignó la tarea a David Geier, un investigador que ha repetido la afirmación —ya desacreditada— de que las vacunas causan autismo.
Luego, Kennedy redobló la apuesta cuestionando el uso de aluminio, que se agrega a muchas vacunas para reforzar la respuesta inmunitaria. En una reunión de gobernadores en julio, lo vinculó con las alergias, a pesar de que un estudio reciente en la revista Annals of Internal Medicine no encontró ninguna conexión. Se espera ampliamente que pida a un comité asesor federal que revise el uso del aluminio.
La investigación sobre el autismo y las dudas sobre el aluminio fueron los primeros pasos en su ofensiva contra el fondo de compensación, según dos fuentes.
Ese fondo ofrece compensaciones a personas con lesiones causadas por vacunas y ha pagado más de $5.000 millones desde su creación en 1988, según la Administración de Recursos y Servicios de Salud (HRSA, por sus siglas en inglés).
Antes de presentar una demanda en un tribunal, las personas afectadas presentan sus reclamos ante el “tribunal de vacunas”, que no tiene jurado y evalúa la evidencia. El dinero proviene de un pequeño impuesto especial sobre cada vacuna.
La compensación se determina en parte por una tabla que mantiene la HRSA y supervisa el secretario del HHS. Esta lista enumera las vacunas y sus posibles efectos secundarios, y abarca las inmunizaciones de rutina recomendadas por los Centros para el Control y Prevención de Enfermedades (CDC), que están sujetas al impuesto. Las lesiones incluyen anafilaxia y encefalitis. Quienes sufran esas condiciones dentro de cierto tiempo después de vacunarse pueden recibir una indemnización.
Kennedy quiere que se incluyan el autismo o las alergias en esa tabla, según dos personas familiarizadas con las discusiones internas y con preocupaciones expresadas públicamente por farmacéuticas y ex funcionarios. Podría lograrlo, por ejemplo, si una investigación dirigida por el HHS vinculara las vacunas con el autismo, o si un comité asesor recomendara eliminar el aluminio de las vacunas.
“Dado el índice de autismo, si se presentan muchos casos, eso podría llevar a la quiebra del programa”, dijo Dorit Reiss, profesora de la Universidad de California en San Francisco.
Si eso ocurriera, algunas farmacéuticas podrían dejar de fabricar vacunas —que no suelen ser productos muy rentables— para evitar demandas largas y costosas de personas que no puedan ser compensadas porque el fondo federal se haya agotado, dijeron expertos en estas leyes y fabricantes.
“El fondo de compensación, si desaparece, afectaría la decisión de seguir adelante o no con las vacunas”, dijo David Dodd, presidente y director ejecutivo de GeoVax Labs, una empresa biotecnológica que desarrolla vacunas e inmunoterapias.
Kennedy ha puesto a personas de su confianza para llevar adelante esta estrategia. Ha presionado para que escépticos de las vacunas ocupen puestos clave en los CDC, que recomiendan las vacunas, y en la Administración de Alimentos y Medicamentos (FDA), que las aprueba.
También seleccionó a líderes del movimiento antivacunas para que evaluaran candidatos para su equipo.
El resultado ha sido una serie de decisiones regulatorias y políticas que han limitado el acceso a las vacunas y el desarrollo de nuevas.
Este mes, el HHS anunció que suspendía $500 millones en subvenciones y contratos para el desarrollo de vacunas de ARNm, incluidas versiones más duraderas contra covid.
El gobierno federal dejó de recomendar las vacunas contra covid para mujeres embarazadas sanas y para niños, sin consultar al comité asesor de vacunas que tradicionalmente participaba en esas decisiones.
Además, Kennedy reorganizó ese comité con miembros elegidos por él, incluidos escépticos de las vacunas, y eliminó como enlaces a grupos como la Asociación Médica Estadounidense, la Asociación Nacional de Enfermeras y otras organizaciones. El comité modificado recomendó no aplicar vacunas contra la gripe que contienen un conservante que erróneamente se ha vinculado con el autismo.
Las llamadas de la Casa Blanca
La intención de Kennedy de mantener a escépticos de las vacunas en puestos de supervisión se evidenció en un acuerdo que hizo recientemente con Trump y su equipo, según dos fuentes. El acuerdo se concretó un domingo de julio por la noche, cuando Kennedy recibió una llamada de la Casa Blanca.
El tema era Vinay Prasad, un alto regulador de vacunas de la FDA. Recientemente había provocado una oleada de críticas en la industria por haber participado en la decisión de la agencia de pedir a la empresa Sarepta Therapeutics que suspendiera la distribución de una terapia génica, por razones de seguridad.
Las redes sociales y comentaristas conservadores encendieron la polémica. Laura Loomer, una provocadora de extrema derecha, dijo el 21 de julio en X que Prasad debía ser despedido y lo llamó “liberal progresista autoproclamado y fanático de Bernie Sanders”, en referencia al senador Bernie Sanders (independiente por Vermont). Varios legisladores comenzaron a presionar a la Casa Blanca con preguntas.
La controversia llegó a Trump, quien quería que Prasad se fuera, según las fuentes. Pero Kennedy no quería perderlo. Consideraba que necesitaba a alguien crítico de las vacunas al frente de la supervisión en la agencia.
Así que Kennedy negoció. A Prasad se le pediría que renunciara como director del Centro de Evaluación e Investigación de Productos Biológicos de la FDA, que regula vacunas y productos biológicos como las terapias génicas. Y el centro se dividiría en dos operaciones, lo que le permitiría a Kennedy elegir quién estaría a cargo del área de vacunas.
Algunos líderes en salud pública compartieron públicamente detalles del acuerdo y expresaron su preocupación. Scott Gottlieb, ex comisionado de la FDA, dijo el 1 de agosto en CNBC que pensaba que “sería muy destructivo para la agencia”.
Después de dejar la agencia en julio, Prasad ahora regresa, aunque no está claro si en el mismo cargo.
Recientemente, Kennedy fue demandado por Ray Flores, abogado externo principal de Children’s Health Defense, una organización antivacunas fundada por el propio Kennedy.
La demanda —financiada por esa organización— alega que Kennedy no lanzó un grupo de trabajo para estudiar la seguridad de las vacunas, como supuestamente se exige. Sin embargo, según una fuente, Kennedy y sus aliados consideran que se trata de una demanda “amigable” porque busca un resultado que él mismo desea.
El 14 de agosto, el HHS anunció que reactivaría un panel federal —disuelto en 1998— para supervisar las vacunas pediátricas.
Las acciones de Kennedy contra las vacunas también han generado demandas en su contra, incluida una presentada por la Academia Americana de Pediatría y otros grupos de salud pública. Su decisión de detener el financiamiento para el desarrollo de vacunas de ARNm provocó una oleada de críticas en redes sociales.
“Esto es irresponsable. Es peligroso. Va a costar vidas. Debemos contraatacar”, escribió el 5 de agosto el senador Edward Markey (demócrata por Massachusetts) en X.
“Intenté mantenerme objetivo y sin alarmismo frente a las acciones del HHS, pero sinceramente, esta medida va a costar vidas”, dijo ese mismo día Jerome Adams, ex cirujano general de Estados Unidos durante el anterior gobierno de Trump.
Kennedy y sus seguidores siguen decididos. En respuesta, sus aliados lanzaron una campaña de relaciones públicas sin precedentes para promover la figura del secretario de Salud, alimentando la especulación de que podría estar considerando una candidatura presidencial en 2028.
La organización sin fines de lucro MAHA Action organizó una llamada en julio para movilizar a los seguidores de Kennedy e inició una campaña publicitaria de seis cifras elogiando a Kennedy y a las iniciativas de salud del gobierno de Trump.
“Que no quepa duda: esta es una revolución que cambiará el rostro de las políticas de salud pública”, dijo Tony Lyons, presidente de MAHA Action, en un comunicado. “Los estadounidenses están exigiendo una transparencia radical y ciencia de primer nivel”.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 month 3 weeks ago
Noticias En Español, Public Health, Misinformation, Trump Administration, vaccines
PAHO/WHO | Pan American Health Organization
Antigen bank for foot-and-mouth disease opens in the Americas to facilitate quick access to emergency vaccines
Antigen bank for foot-and-mouth disease opens in the Americas to facilitate quick access to emergency vaccines
Oscar Reyes
29 Aug 2025
Antigen bank for foot-and-mouth disease opens in the Americas to facilitate quick access to emergency vaccines
Oscar Reyes
29 Aug 2025
1 month 4 weeks ago
GHTA launches free prostate cancer screenings
“Beginning in September, men aged 40 years and older are urged to take advantage of this free screening opportunity at convenient Allied Medical Laboratory clinics located across the island”
View the full post GHTA launches free prostate cancer screenings on NOW Grenada.
1 month 4 weeks ago
Business, Health, PRESS RELEASE, allied medical services, arlene friday, ghta, grenada hotel and tourism association, prostate cancer, tourism enhancement fund
PAHO/WHO | Pan American Health Organization
Ante brotes localizados de chikunguña y circulación sostenida de Oropouche, OPS pide fortalecer vigilancia y control vectorial en las Américas
Amid localized chikungunya outbreaks and ongoing Oropouche cases, PAHO urges strengthened surveillance and vector control across the Americas
Oscar Reyes
29 Aug 2025
Amid localized chikungunya outbreaks and ongoing Oropouche cases, PAHO urges strengthened surveillance and vector control across the Americas
Oscar Reyes
29 Aug 2025
1 month 4 weeks ago
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
AbbVie to buy Gilgamesh Pharma Bretisilocin for Major Depressive Disorder
North Chicago: AbbVie and Gilgamesh Pharmaceuticals Inc.
North Chicago: AbbVie and Gilgamesh Pharmaceuticals Inc. have announced a definitive agreement under which AbbVie will acquire Gilgamesh's lead investigational candidate, currently in clinical development for the treatment of patients with moderate-to-severe major depressive disorder (MDD).
Psychedelic compounds, including 5-HT2A receptor agonists, have gained recognition as potential treatments for mental health disorders, such as MDD, because of their demonstrated rapid, robust and durable antidepressant effects. However, existing agents in this class are hampered by their long duration of psychoactive experience.
Bretisilocin, a 5-HT2A receptor agonist and 5-HT releaser, is a novel, next-generation psychedelic compound designed to address development challenges observed within this class of compounds. Bretisilocin has been shown to exert a shorter duration of psychoactive experience, while retaining an extended therapeutic benefit.
Positive topline results from a Phase 2a study of bretisilocin in MDD were recently announced, demonstrating a clinically impactful and statistically significant reduction in severity of depressive symptoms versus low dose active comparator, as measured by the Montgomery-Åsberg Depression Rating Scale (MADRS) total score. At Day 14, a single dose (10mg) of bretisilocin demonstrated robust antidepressant effect with a -21.6 point change from baseline in MADRS total score compared to a -12.1 point change from baseline for the low dose (1mg) active comparator (p = 0.003). Bretisilocin was well tolerated with no serious adverse events.
"The field of psychiatry represents one of the most challenging areas in medicine, with a significant need for innovative solutions," said Roopal Thakkar, M.D., executive vice president, research and development and chief scientific officer, AbbVie. "This acquisition underscores our commitment to broadening and enhancing psychiatric care by investing in novel treatment approaches with the potential to reach patients for whom other treatments have been ineffective. We look forward to advancing bretisilocin to late-stage clinical development."
"AbbVie's leadership in neuroscience and commitment to advancing innovative treatments make them the ideal partner to advance bretisilocin rapidly forward while enabling Gilgamesh to continue pursuing our broader mission of developing novel, transformative therapies for complex mental health and neurological conditions," said Jonathan Sporn, M.D., chief executive officer at Gilgamesh Pharmaceuticals.
Under the terms of the agreement, AbbVie will acquire Gilgamesh's bretisilocin program for up to $1.2 billion, inclusive of an upfront payment and development milestones. Additionally, as part of the transaction, Gilgamesh will spin off a new entity that will operate under the name Gilgamesh Pharma Inc. to hold its employees and other programs, including its oral NMDA receptor antagonist blixeprodil (GM-1020), cardio-safe ibogaine analog, M1/M4 agonist program and existing collaboration with AbbVie. The transaction is subject to customary closing conditions.
This transaction builds upon AbbVie and Gilgamesh's 2024 collaboration and option-to-license agreement to advance the development of next-generation therapies for the treatment of psychiatric disorders. This option-to-license remains in effect and will be transferred to Gilgamesh Pharma Inc. in connection with the spin-out.
For AbbVie, Covington & Burling LLP is acting as legal counsel. For Gilgamesh, Centerview Partners LLC is acting as exclusive financial advisor and Ropes & Gray LLP is acting as legal counsel.
1 month 4 weeks ago
News,Industry,Pharma News,Latest Industry News
Health & Wellness | Toronto Caribbean Newspaper
Doctor banned from using real name builds 50-year medical legacy empire
"In 1967, the College of Physicians and Surgeons of Ontario prevented him from publishing under his own name.”
The post Doctor banned from using real name builds 50-year medical legacy empire first appeared on Toronto Caribbean Newspaper.
1 month 4 weeks ago
Health & Wellness, #communitynews, #health, doctor, medical, writer
Grenada continues to strengthen healthcare ties with US partners
The Ministry of Health met with US Principal Officer Cindy Diouf, hospital administrators, and 2 US military doctors to explore opportunities for training and enhancing medical infrastructure across the state
View the full post Grenada continues to strengthen healthcare ties with US partners on NOW Grenada.
1 month 4 weeks ago
Health, PRESS RELEASE, and st george’s university, andrew shue, cindy diouf, hannah st paul, hospital, nadma, rgpf, ricardo castaneda, royal grenada police force, sgu
PAHO/WHO | Pan American Health Organization
PAHO launches tool to monitor early child development in Latin America
PAHO launches tool to monitor early child development in Latin America
Cristina Mitchell
28 Aug 2025
PAHO launches tool to monitor early child development in Latin America
Cristina Mitchell
28 Aug 2025
1 month 4 weeks ago
Health Archives - Barbados Today
Isolation driving surge in self-harm, anxiety among youth, says doc
A sharp increase in self-harm and attempted suicide among young girls marks a deepening mental health emergency, with a government expert sounding the alarm that the true scope of the problem remains hidden.
Dr Joy Sue, consultant psychiatrist at the Ministry of Health and based at the Psychiatric Hospital in Black Rock, warned on Wednesday that these issues may represent only the surface of a much wider crisis affecting the nation’s young people, as males remain largely absent from those seeking assistance.
She explained that one of the main reasons for this troubling mental health trend is the fallout from the COVID-19 pandemic, which is only now becoming apparent.
“To tell you the truth, we have always seen a fair amount of cuttings, but it has increased. We had an increase in depressive anxiety [during COVID] for sure. And with that, we had an increase in persons who presented with cuttings and other forms of parasuicide or what we called self-harm, that is not necessarily meant to cause death.
“During COVID and post-COVID, those conditions increased. And the whole pandemic, and what came with the pandemic…meaning, the isolation, the online schooling, the lack of socialisation…we are only now seeing the fallout from that. Young people now have changed drastically from the way they behaved previously. I think a lot of it stems from that,” she said.
Addicted to devices
Dr Sue also addressed the addiction to mobile devices as a pressing mental health issue requiring intervention.
She said: “There is a lot more of the digital world… It’s much more a part of their lives now. They are addicted to social media, and that can affect your self-esteem…. They are doing this social comparison thing…. For most people, it is something they put on, but social media is not real life. Or, they are getting bullied on social media. All of that is a part of it. They were isolated all of that time during COVID, they did not have the social support necessary, so they weren’t adapting.”
Extending her concern about social media’s pervasive influence, Dr Sue added: “Even lying down next to each other, people are on their devices.”
Silent struggle
Dr Sue revealed that the majority of new clients she now sees are young people ranging from their early teens to age 35, further underlining how social and emotional challenges are affecting an entire generation.
She highlighted the importance of the home environment: “They didn’t just get depressed overnight. A lot of them have a lot of trauma dating back from childhood.”
Eating disorders and gender disparities
Eating disorders were flagged by Dr Sue as another disturbing trend, especially among young females seeking help. “You are going to have poor health outcomes later on. With all of these NCDs [non-communicable diseases] that we are talking about, it is going to put them at risk.”
The psychiatrist clarified that eating disorders are rarely the primary concern brought to her by clients, but emerge as a secondary diagnosis discovered during consultations: “They are not seeing me for eating on its own. So they usually are seeing me because of some kind of depressive anxiety. Eating habits is something that is a secondary diagnosis that is discovered when I speak to them, but not necessarily the reason why they are presenting.”
Asked about males turning up with eating disorders, Dr Sue noted: “You don’t get as many males presenting for depressive anxiety. That is from most females.
“There are a variety of reasons. The fact is that it is more common [for females] because of hormonal reasons. But that’s not the only reason. It could be cultural too. It is not that males aren’t experiencing that…but culturally, how ready females are to come forward and access services for something like that…which is not what the act says about males culturally. So, if males are going through something like that, culture says: ‘Suck it up, I am man, be strong;’ and perhaps because the males aren’t coming forward, we are not getting complaints from the males because they simply aren’t talking about it.”
This, she suggested, means the nation may be unaware of the true picture of mental health in Barbados, with women always more likely to seek help: “We are always trying to get to be the ones to come forward. A lot of emphasis is placed on males.”
Dr Sue emphasised the risks of men not seeking support: “The eating disorders in the men are associated with the other things that females also have. Don’t forget the males are the ones that are disproportionate by suicide as well. All those factors could contribute to increased risks, not only for NCDs, but for more severe mental health outcomes.”
Troubled home environments, missing girls
Touching on the possible link between mental health issues originating at home and the phenomenon of girls going missing, Dr Sue reflected on her work at the Government Industrial School (GIS) female section.
“The persons who were the perpetrators were [getting away] scot-free, while these girls were locked up. I always used to think this was foolishness. They are punishing them when they are victims and their rebellious behaviour is because of something that happened to them and those persons who did these things, they aren’t punished.
“When they are finished with [the Government Industrial School], they got to go back into the same household because they don’t have anywhere else to go. They are back into the same problems that were never resolved. A vicious cycle.”
emmanueljoseph@barbadostoday.bb
The post Isolation driving surge in self-harm, anxiety among youth, says doc appeared first on Barbados Today.
1 month 4 weeks ago
Health, Local News
Health Archives - Barbados Today
Barbados can shape the future of tobacco control
By Michael Landl, Director of the World Vapers’ Alliance
Barbados has made impressive progress in reducing smoking rates—the lowest in the Caribbean region—but there is still work to do. The stark difference between men’s and women’s smoking rates shows that targeted, practical solutions could push smoking down even further. As the global tobacco control community prepares for COP11, Barbados has a unique chance to push for smarter policies that reflect real-world success and science.
Harm reduction offers an alternative to the traditional all-or-nothing approach. Instead of demanding everyone quit nicotine altogether, which many struggle to do, harm reduction provides safer options like vaping, nicotine pouches and heat-not-burn products. These alternatives avoid burning tobacco, which produces the harmful smoke that leads to cancer, heart disease, and other deadly illnesses. The science is clear: remove the smoke, reduce the harm.
Worldwide, places that have embraced harm reduction—like Sweden, the UK, New Zealand and Japan—have rapidly cut smoking rates. Millions of smokers have successfully switched to these safer choices. Yet, despite this evidence, global tobacco control institutions often dismiss harm reduction as unproven or risky, ignoring the voices of consumers and smaller countries whose needs differ from those of wealthier nations. Instead, large donors and entrenched interests dominate the agenda.
Barbados should not accept being overlooked. The country’s experience and perspective are vital. COP11 presents the chance to lead, demanding a working group focused on tobacco harm reduction, mirroring Barbados’s recent global leadership on biodiversity. This group would ensure ongoing, evidence-based discussions, allow like-minded countries to collaborate, and prevent one-size-fits-all policies that ignore science and real lives.
Supporting harm reduction means rejecting blanket bans on less harmful products, tailoring rules to reflect true risk, and insisting on transparent negotiations where consumers who have benefited from these tools are heard. Tobacco control must evolve to put outcomes over ideology.
Barbados already has strong tobacco control laws and a balanced approach to vaping regulation. Promoting cessation support and harm reduction will build on this foundation, saving lives and accelerating progress. With an already low smoking rate of 6.4%, Barbados can follow Sweden and become the next smoke-free nation.
Speaking up at COP11 will set Barbados apart as a leader among smaller countries demanding science, fairness, and inclusion in global policy. The world needs voices like Barbados’s that prioritise people over politics.
The global health community faces a crucial choice: resist change and prolong suffering, or embrace proven, compassionate strategies that reduce harm. Barbados can help tip the scale toward progress. This moment calls for courage and clarity. Barbados can show leadership by backing harm reduction and making sure its people have access to safer choices. The world is watching. Now is the time for Barbados to act.
The post Barbados can shape the future of tobacco control appeared first on Barbados Today.
1 month 4 weeks ago
Health, Local News
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
ATTAIN-2 Trial: Oral GLP-1 Orforglipron Lowers Weight and HbA1c among diabetics with obesity
Topline results from the ATTAIN-2 trial have demonstrated that adults taking 36 mg orforglipron lost an average of 10.5% body weight at 72 weeks, with over half of participants on any dose achieving an HbA1c of 6.5% or lower.
Topline results from the ATTAIN-2 trial have demonstrated that adults taking 36 mg orforglipron lost an average of 10.5% body weight at 72 weeks, with over half of participants on any dose achieving an HbA1c of 6.5% or lower. The oral GLP-1 demonstrated significant benefits for adults with obesity and type 2 diabetes.
In the trial, all three doses of orforglipron met the primary and all key secondary endpoints, delivering significant weight loss, meaningful A1C reductions, and improvements in cardiometabolic risk factors at 72 weeks. For the primary endpoint, orforglipron 36 mg, taken once per day without food and water restrictions, lowered weight by an average of 10.5% (22.9 lbs) compared to 2.2% (5.1 lbs) with placebo using the efficacy estimand.1 With the completion of ATTAIN-2, Lilly now has the full clinical data package required to initiate global regulatory submissions for orforglipron.
"Based on my experience leading clinical trials in obesity and diabetes, these data show the potential for orforglipron to offer an efficacy, safety, and tolerability profile consistent with the injectable GLP-1 class," said Louis J. Aronne, MD, FACP, DABOM, founder and Chair Emeritus of the American Board of Obesity Medicine, former president of The Obesity Society, Fellow of the American College of Physicians, and world-renowned obesity specialist. "Orforglipron could help health care providers expand treatment options for patients who prefer oral therapies without compromising clinical results."
In the ATTAIN-2 trial, orforglipron met the primary endpoint of superior body weight reduction compared to placebo. Participants taking the highest dose of orforglipron lost an average of 22.9 lbs (10.5%) at 72 weeks using the efficacy estimand. In a key secondary endpoint, orforglipron lowered A1C by 1.3% to 1.8% from a baseline of 8.1% across doses. In another key secondary endpoint, 75% of participants taking the highest dose of orforglipron achieved an A1C ≤6.5%, which is at or below the American Diabetes Association's definition of diabetes. Additionally, orforglipron showed clinically meaningful benefits across key cardiovascular risk factors, including non-HDL cholesterol, systolic blood pressure and triglycerides. In a pre-specified exploratory analysis, the highest dose of orforglipron reduced high-sensitivity C-reactive protein (hsCRP) levels, a marker of inflammation, by 50.6%.
iSuperiority test was adjusted for multiplicity with all three doses.
iiSuperiority test was adjusted for multiplicity with the 12 mg and 36 mg doses.
For the treatment-regimen estimand, each dose of orforglipron led to statistically significant improvements across the primary and all key secondary endpoints, including:
• Percent weight reduction: -5.1% (-5.3 kg; -11.7 lbs; 6 mg), -7.0% (-7.2 kg; -15.9 lbs; 12 mg), -9.6% (-9.6 kg; -21.2 lbs; 36 mg), -2.5% (-2.7 kg; -6.0 lbs; placebo)
• Percentage of participants achieving body weight reductions of ≥10%: 22.6% (6 mg), 31.2% (12 mg), 45.6% (36 mg), 9.0% (placebo)
• Percentage of participants achieving body weight reductions of ≥15%: 6.8% (6 mg), 14.4% (12 mg), 26.0% (36 mg), 3.0% (placebo)
• A1C reduction: -1.2% (6 mg), -1.5% (12 mg), -1.7% (36 mg), -0.5% (placebo)
• Percentage of participants achieving A1C <7%: 64.6% (6 mg), 75.9% (12 mg), 75.5% (36 mg), 30.5% (placebo)
• Percentage of participants achieving A1C ≤6.5%: 52.5% (6 mg), 57.6% (12 mg), 66.6% (36 mg), 15.4% (placebo)
"The ATTAIN-2 results reinforce the potential for orforglipron, as a once-daily oral, to deliver meaningful weight loss and A1C reduction, consistent with similar landmark trials for injectable GLP-1s," said Kenneth Custer, Ph.D., Lilly executive vice president and president of Lilly Cardiometabolic Health. "With these positive data in hand, we are moving with urgency toward global regulatory submissions to potentially meet the needs of patients who are waiting. If approved, we are ready to offer a convenient, once-daily pill that can be scaled globally-removing barriers and redefining how obesity is treated around the world."
The overall safety profile of orforglipron in ATTAIN-2 was consistent with the established GLP-1 receptor agonist class. The most commonly reported adverse events were gastrointestinal-related and generally mild-to-moderate in severity. The most common adverse events for participants treated with orforglipron (6 mg, 12 mg and 36 mg, respectively) were nausea (20.1%, 31.1% and 36.4%) vs. 8.4% with placebo, vomiting (12.8%, 20.2% and 23.1%) vs. 3.8% with placebo, diarrhea (21.3%, 24.8% and 27.4%) vs. 15.0% with placebo, constipation (17.7%, 21.1% and 22.4%) vs. 7.8% with placebo, and dyspepsia (9.1%, 15.4% and 10.9%) vs. 3.5% with placebo. Treatment discontinuation rates due to adverse events were 6.1% (6 mg), 10.6% (12 mg) and 10.6% (36 mg) for orforglipron vs. 4.6% with placebo. Overall treatment discontinuation rates were balanced across the treatment groups with 19.1% (6 mg), 22.3% (12 mg) and 20.5% (36 mg) for orforglipron vs. 20.0% with placebo. No hepatic safety signal was observed.
Detailed ATTAIN-2 results will be presented at a future medical meeting and published in a peer-reviewed journal.
About orforglipron
Orforglipron (or-for-GLIP-ron) is an investigational, once-daily small molecule (non-peptide) oral glucagon-like peptide-1 receptor agonist that can be taken any time of the day without restrictions on food and water intake.5 Orforglipron was discovered by Chugai Pharmaceutical Co., Ltd. and licensed by Lilly in 2018. Chugai and Lilly published the preclinical pharmacology data of this molecule together. Lilly is running Phase 3 studies on orforglipron for the treatment of type 2 diabetes and for weight management in adults with obesity or overweight with at least one weight-related medical problem. It is also being studied as a potential treatment for obstructive sleep apnea and hypertension in adults with obesity.
About ATTAIN-2 and ATTAIN clinical trial program
ATTAIN-2 (NCT05872620) is a Phase 3, 72-week, randomized, double-blind, placebo-controlled trial comparing the efficacy and safety of orforglipron 6 mg, 12 mg and 36 mg as monotherapy with placebo in adults with obesity or overweight and type 2 diabetes. The trial randomized over 1,600 participants across the U.S., Argentina, Australia, Brazil, China, Czechia, Germany, Greece, India, South Korea and Puerto Rico in a 1:1:1:2 ratio to receive either 6 mg, 12 mg or 36 mg orforglipron or placebo. The primary objective of the study was to demonstrate that orforglipron (6 mg, 12 mg, 36 mg) is superior to placebo in mean body weight change from baseline at 72 weeks in people with a BMI ≥27.0 kg/m² and type 2 diabetes who are on stable treatment with either diet/exercise alone or up to three oral antihyperglycemic medications. All participants receiving orforglipron started the study at a dose of 1 mg once-daily and then increased the dose in a step-wise approach at four-week intervals to their final randomized maintenance dose of 6 mg (via steps at 1 mg and 3 mg), 12 mg (via steps at 1 mg, 3 mg and 6 mg) or 36 mg (via steps at 1 mg, 3 mg, 6 mg, 12 mg and 24 mg). Dose reduction was only allowed for GI tolerability if other mitigations failed.
The ATTAIN Phase 3 global clinical development program for orforglipron has enrolled more than 4,500 people with obesity or overweight across two global registration trials.
1 month 4 weeks ago
Diabetes and Endocrinology,Medicine,Diabetes and Endocrinology News,Medicine News,Top Medical News,Latest Medical News
Ah-choo and you: Beating the post-carnival cold
The GFNC shares simple post-Carnival nutrition tips: good nutrition, proper hydration, and rest are key to a speedy recovery
View the full post Ah-choo and you: Beating the post-carnival cold on NOW Grenada.
The GFNC shares simple post-Carnival nutrition tips: good nutrition, proper hydration, and rest are key to a speedy recovery
View the full post Ah-choo and you: Beating the post-carnival cold on NOW Grenada.
2 months 2 hours ago
Health, PRESS RELEASE, carnival, cold, flu, gfnc, grenada food and nutrition council, hydration
Grenada shines at Caribbean Association of Pharmacists Conference
Kelvin Dragon, RPh, received 2 prestigious awards for his outstanding service to the profession and the wider Caribbean community, while Lydia Andrews-Duncan, RPh, was elected as a council member of the Caribbean Association of Pharmacists
View the full post Grenada shines at Caribbean Association of Pharmacists Conference on NOW Grenada.
2 months 3 hours ago
Business, Health, PRESS RELEASE, cap, caribbean association of pharmacists, gap, grenada association of pharmacists, kelvin dragon, lydia andrews-duncan, t a marryshow community college, tamcc
Facing reality: Why our Age of Civil Responsibility Bill matters
”If we had perfect families, we would not need the ACR Bill… Let us disagree on the merits of the bill and how we can make it stronger to protect the nation’s adolescents, but please, let us rise above sensationalism and misinformation”
View the full post Facing reality: Why our Age of Civil Responsibility Bill matters on NOW Grenada.
2 months 3 hours ago
Health, Law, PRESS RELEASE, Youth, acr, advocates for safe parenthood improving reproductive equity, age of civil legal responsibility, age of civil responsibility, aspire, fred nunes, gppa, grenada planned parenthood association, Healthcare, incest, reproductive healthcare, sexual and reproductive health, sexual and reproductive health and rights, srh, srhr, teen, tonia frame
Health Archives - Barbados Today
Caribbean urged to strengthen health data to combat rise in vector-borne disease
Caribbean health authorities have been warned that unless the region urgently overhauls how health data is collected and applied, efforts to prevent and control outbreaks of diseases such as dengue, chikungunya, and Zika will be undermined, a top public health expert said Tuesday.
Director of Surveillance, Disease Prevention and Control at the Caribbean Public Health Agency (CARPHA), Dr Horace Cox, spoke to Barbados TODAY on the sidelines of a regional workshop being hosted at Blue Horizon Hotel. The training session, attended by health professionals from across the region, is focused on boosting the Caribbean’s collective capacity to predict, detect and respond to vector-borne diseases (VBDs).
He noted that although much has been done in recent years to improve data use in drafting public health policies, strengthening data quality and improving how it is applied in decision-making should be seen as the critical point in the region’s preparedness strategy.
Dr Cox said: “We are coming up with innovative tools at the Caribbean Public Health Agency in conversation with key stakeholders such as those in Barbados, that these tools can help to give us an early signal that something is about to happen. Once that’s the case, we trust that this can advance our preparedness not only as a nation in Barbados but also as a region and, by extension, our level of resilience to the public health threats that we continue to face.”
Much of the workshop, he noted, is about ensuring participants understand both the technical and practical value of high-quality information in safeguarding public health.
“Here we’re teaching the different participants about the importance of improving data quality, because we can come up with all of these fancy tools, but it’s what’s fed into them [that’s] important,” he said.
“Then also we’re building capacity on the use of risk assessment tools because we want them to be able to appreciate the level of risk and also to understand how the public health actions will be commensurate with that level of risk that’s assessed.”
According to Dr Cox, CARPHA and its partners are working on new models that will give health authorities more accurate early warning systems. However, these can only be successful if regional countries have the right infrastructure and ensure that the data being reported is both consistent and reliable.
“There’s been a lot of advancement in terms of the Caribbean getting better quality data using standardised tools that would harmonise the data sets across the board and ensure that they can speak to one another at the time when we’re attempting to do different analyses,” he said.
“Even though we’ve had these successes, it’s important for us to think about the next step. How could we ensure that these changes are institutionalised and that they become part of the culture?”
He stressed that the ultimate goal is not simply about producing large datasets or building new databases, but about ensuring that the data is properly analysed and used to guide real-world public health decisions.
“It’s not just about collecting data and having the best data package available to us, but it’s how to extract the information from it and to use it to inform public health action, and that’s the essence of it,” Dr Cox explained. “We want it to be a process that is smooth, that not only reflects very robust data systems, but also the translation of that evidence and the use of the evidence to inform public health action.”
At the most practical level, he added, the importance of good data must resonate beyond health professionals and policymakers, reaching right down to communities and families.
“When the data is collected, we want to ensure that you, at the very level of the community, understand how you’re using that data to ensure that you do the necessary preventive measures to protect not only you but your family and by extension the broader community,” he said. (SB)
The post Caribbean urged to strengthen health data to combat rise in vector-borne disease appeared first on Barbados Today.
2 months 7 hours ago
Health, Local News