KFF Health News' 'What the Health?': Countdown to Shutdown
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
Health and other federal programs are at risk of shutting down, at least temporarily, as Congress races toward the Oct. 1 start of the fiscal year without having passed any of its 12 annual appropriations bills. A small band of conservative House Republicans are refusing to approve spending bills unless domestic spending is cut beyond levels agreed to in May.
Meanwhile, former President Donald Trump roils the GOP presidential primary field by vowing to please both sides in the divisive abortion debate.
This week’s panelists are Julie Rovner of KFF Health News, Alice Miranda Ollstein of Politico, Rachel Cohrs of Stat News, and Tami Luhby of CNN.
Panelists
Alice Miranda Ollstein
Politico
Rachel Cohrs
Stat News
Tami Luhby
CNN
Among the takeaways from this week’s episode:
- The odds of a government shutdown over spending levels are rising. While entitlement programs like Medicare would be largely spared, past shutdowns have shown that closing the federal government hobbles things Americans rely on, like food safety inspections and air travel.
- In Congress, the discord isn’t limited to spending bills. A House bill to increase price transparency in health care melted down before a vote this week, demonstrating again how hard it is to take on the hospital industry. Legislation on how pharmacy benefit managers operate is also in disarray, though its projected government savings means it could resurface as part of a spending deal before the end of the year.
- On the Senate side, legislation intended to strengthen primary care is teetering under Bernie Sanders’ stewardship — in large part over questions about how to pay for it. Also, this week Democrats broke Alabama Republican Sen. Tommy Tuberville’s abortion-related blockade of military promotions (kind of), going around him procedurally to confirm the new chair of the Joint Chiefs of Staff.
- And some Republicans are breaking with abortion opponents and mobilizing in support of legislation to renew the United States President’s Emergency Plan for AIDS Relief — including the former president who spearheaded the program, George W. Bush. Meanwhile, polling shows President Joe Biden is struggling to claim credit for the new Medicare drug negotiation program.
- And speaking of past presidents, former President Donald Trump gave NBC an interview over the weekend in which he offered a muddled stance on abortion. Vowing to settle the long, inflamed debate over the procedure — among other things — Trump’s comments were strikingly general election-focused for someone who has yet to win his party’s nomination.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: The Washington Post’s “Inside the Gold Rush to Sell Cheaper Imitations of Ozempic,” by Daniel Gilbert.
Alice Miranda Ollstein: Politico’s “The Anti-Vaccine Movement Is on the Rise. The White House Is at a Loss Over What to Do About It,” by Adam Cancryn.
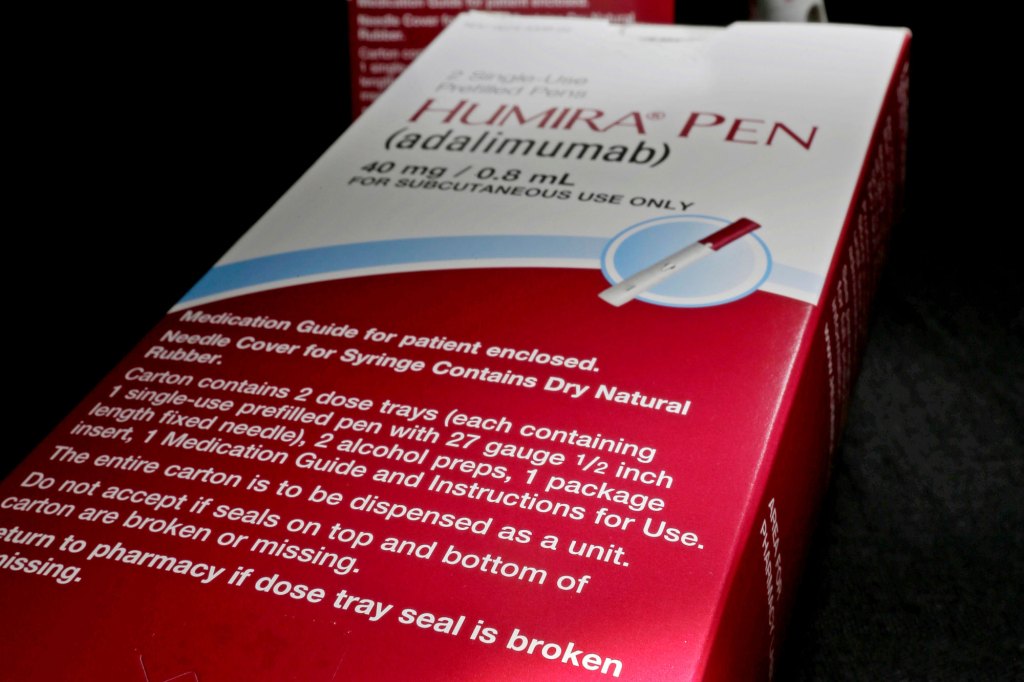
Rachel Cohrs: KFF Health News’ “Save Billions or Stick With Humira? Drug Brokers Steer Americans to the Costly Choice,” by Arthur Allen.
Tami Luhby: CNN’s “Supply and Insurance Issues Snarl Fall Covid-19 Vaccine Campaign for Some,” by Brenda Goodman.
Also mentioned in this week’s episode:
- The AP’s “Biden’s Medicare Price Negotiation Is Broadly Popular. But He’s Not Getting Much Credit,” by Seung Min Kim and Linley Sanders.
- Roll Call’s “Sanders, Marshall Reach Deal on Health Programs, but Challenges Remain,” by Jessie Hellmann and Lauren Clason.
CLICK TO EXPAND THE TRANSCRIPT
Transcript: Countdown to Shutdown
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News. And I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, Sept. 21, at 9 a.m. because, well, lots of news this week. And as always, news happens fast, and things might well have changed by the time you hear this. So here we go. We are joined today via video conference by Tami Luhby of CNN.
Tami Luhby: Good morning.
Rovner: Rachel Cohrs of Stat News.
Rachel Cohrs: Hi, everybody.
Rovner: And Alice Miranda Ollstein of Politico.
Alice Miranda Ollstein: Hello.
Rovner: Let’s get to some of that news. We will begin on Capitol Hill, where I might make a T-shirt from this tweet from Wednesday from longtime congressional reporter Jake Sherman: “I feel like this is not the orderly appropriations process that was promised after the debt ceiling deal passed.” For those of you who might’ve forgotten, many moons ago, actually it was May, Congress managed to avoid defaulting on the national debt, and as part of that debt ceiling deal agreed to a small reduction in annual domestic spending for the fiscal year that starts Oct. 1 (as in nine days from now). But some of the more conservative Republicans in the House want those cuts to go deeper, much deeper, in fact. And now they’re refusing to either vote for spending bills approved by the Republican-led appropriations committee or even for a short-term spending bill that would keep the government open after this year’s funding runs out. So how likely is a shutdown at this point? I would hazard a guess to say pretty likely. And anybody disagree with that?
Ollstein: It’s more likely than it was a week or two ago, for sure. The fact that we’re at the point where the House passing something that they know is dead on arrival in the Senate would be considered a victory for them. And so, if that’s the case, you really have to wonder what the end game is.
Rovner: Yeah, I mean it was notable, I think, that the House couldn’t even pass the rule for the Defense Appropriations Bill, which is the most Republican-backed spending bill, and the House couldn’t get that done. So I mean it does not bode well for the fate of some of these domestic programs that Republicans would, as I say, like to cut a lot deeper. Right?
Cohrs: Democrats are happy, I think, to watch Republicans flail for a while. I think we saw this during the speaker votes. Obviously, a CR [continuing resolution] could pass with wide bipartisan support, but I think there’s a political interest for Democrats going into an election year next year to lean into the idea of the House Republican chaos and blaming them for a shutdown. So I wouldn’t be too optimistic about Democrats billing them out anytime soon.
Rovner: But, bottom line, of course, is that a shutdown is not great for Democrats who support things that the government does. I mean, Tami, you’re watching, what does happen if there’s a shutdown? Not everything shuts down and not all the money stops flowing.
Luhby: No, and the important thing, unlike in the debt ceiling, potentially, was that Social Security will continue, Medicare will continue, but it’ll be very bothersome to a lot of people. There’ll be important things that … potentially chaos at airlines and food safety inspectors. I mean some of them are sometimes considered essential workers, but there’s still issues there. So people will be mad because they can’t go to their national parks potentially. I mean it’s different every time, so it’s a little hard to say exactly what the effects will be and we’ll see also whether this will be a full government shutdown, which will be much more serious than a partial government shutdown, although at this point it doesn’t look like they’re going to get any of the appropriation bills through.
Rovner: I was going to say, yeah, sometimes when they get some of the spending bills done, there’s a partial shutdown because they’ve gotten some of the spending bills done, but I’m pretty sure they’ve gotten zero done now. I think there’s one that managed to pass both the House and the Senate, but basically this would be a full shutdown of everything that’s funded through the appropriations process. Which as Tami points out, the big things are the Smithsonian and the National Zoo close, and national parks close, but also you can’t get an awful lot of government services. Meanwhile, the ill will among House Republicans is apparently rubbing off on other legislation. The House earlier this week was supposed to vote on a relatively noncontroversial package of bills aimed at making hospital insurance and drug prices more transparent, among other things. But even that couldn’t get through. Rachel, what happened to the transparency bill that everybody thought was going to be a slam-dunk?
Cohrs: Well, I don’t think everybody thought it was going to be a slam-dunk given the chaos that we saw, especially in the Democratic Caucus last week, where one out of three chairmen who work on health care in the House endorsed the package, but the other two would not. And they ran into a situation where, with the special rule that they were using to consider the House transparency package, they needed two-thirds vote to pass and they couldn’t get enough Democrats on board to pass it. And I think there were some process concerns from both sides that there was a compromise that came out right after August recess and it hadn’t been socialized properly and they didn’t have their ducks in a row in the Democratic side. But ultimately, I mean, the big picture for me I think was how hard it really is to take on the hospital industry. Because this was the first real effort I think from the House and it melted down before its first vote. That doesn’t mean it’s dead yet, but it was an embarrassment, I think, to everyone who worked on this that they couldn’t get this pretty noncontroversial package through. And when I tried to talk to people about what they actually oppose, it was these tiny little details about a privacy provision or one transparency provision and not with the big idea. It wasn’t ideological necessarily. So I think it was just a reflection on Congress has taken on pharma, they’re working on PBMs this year, but if they really do want to tackle hospital costs, which are a very big part of Medicare spending, it’s going to be a tough road ahead for them.
Rovner: As we like to point out, every single member of Congress has a hospital in their district, and they are quick to let their members of Congress know what they want and how they want them to vote on things. Before we move on, where are we on the PBM legislation? I know there was a whole raft of hearings this week on doing something about PBMs. And my inbox is full of people from both sides. “The PBMs are making drug prices higher.” “No, the PBMs are helping keep drug prices in check.” Where are we with the congressional effort to try and at least figure out what the PBMs do?
Cohrs: Yeah, I think there is still some disarray at this point. I would watch for action in December or whenever we actually have a conversation about government funding because some of these PBM bills do save money, which is the golden ticket in health care because there are a lot of programs that need to be paid for this year. So Congress will continue to debate those over the next couple of weeks, but I think everyone that I talk to is expecting potential passage in a larger package at the end of the year.
Rovner: So speaking of things that need to be paid for, the saga of Sen. Bernie Sanders and the reauthorization of some key primary care programs, including the popular community health center program, continues. When we left off last July, Sen. Sanders, who chairs the Senate Health, Education, Labor & Pensions Committee [HELP], tried to advance a bill to extend and greatly expand primary care programs without negotiating with his ranking Republican on the committee, Louisiana Sen. Bill Cassidy, who had his own bill to renew the programs. Cassidy protested and blocked the bill’s movement and the whole enterprise came to a screeching halt. Last week, Sanders announced he’d negotiated a bipartisan bill, but not with Cassidy, rather with Kansas Republican Roger Marshall, who chairs the relevant subcommittee. Cassidy, however, is still not pleased. Rachel, you’re following this. Sanders has scheduled a markup of the bill for later today. Is it really going to happen?
Cohrs: Well, I think things are on track and the thing to remember about a markup is it passes on a majority. So as long as Sen. Sanders can keep his Democratic members in line and gets Sen. Marshall, then it can pass committee. But I think there are some concerns that other Republicans will share with Sen. Cassidy about how the bill is paid for. There are a lot of ambitious programs to expand workforce training, have debt forgiveness, and address the primary care workforce crisis in a more meaningful way. But the list of pay-fors is a little undisciplined from what I’ve seen, I would say.
Rovner: That’s a good word.
Cohrs: Sen. Sanders is pulling some pay-fors from other committees, which he can’t necessarily do by himself, and they don’t actually have estimates from the Congressional Budget Office for some of the pay-fors that they’re planning to use. They’re just using internal committee math, which I don’t think is going to pass muster with Republicans in the full Senate, even if it gets through committee today. So I think we’ll see some of those concerns flare up. It could get ugly today compared with HELP markups of the past of community health center bills. And there are certainly some concerns about the application of the Hyde Amendment too, and how it would apply to some of this funding as it moves through the appropriations process.
Rovner: That’s the amendment that bans direct government funding of abortion, and there’s always a fight about the Hyde Amendment, which are reauthorizing these health programs. But I mean, we should point out, I mean this is one of the most bipartisanly popular programs, both the community health center program and these programs that basically give federal money to train more primary care doctors, which the country desperately needs. I mean, it’s something that pretty much everybody, or most of Congress, supports, but Cassidy has what, 60 amendments to this bill. I guess he’s really not happy. Cassidy who supports this in general just is unhappy with this process, right?
Cohrs: I think his concern is more that the legislation is half-baked, not that he’s against the idea of it. And Sen. Cassidy did sign on to a more limited House proposal as well, just saying, we need to fund the community health centers, we need to do something. This isn’t ready for prime time. We could see further negotiations, but the time is ticking for this funding to expire.
Rovner: Well, another program whose authorization expires at the end of the month is PEPFAR, the international AIDS/HIV program. It’s being blocked by anti-abortion activists among others, even though it doesn’t have anything to do with the abortion. And this is not just a bipartisan program, it’s a Republican-led program. Former President George W. Bush who signed it into law in 2003, had an op-ed this week pushing for the program in The Washington Post. Alice, you’ve been following this one. Is there any progress on PEPFAR?
Ollstein: Yes and no. There’s not a vote scheduled, there’s not a “Kumbaya” moment, but we are seeing some movement. I call it “Establishment Republican Strike Back.” You have some both on- and off-the-Hill Republicans really mobilizing to say, “Look, we need to reauthorize this program. This is ridiculous.” And they’re going against the anti-abortion groups and their allies on Capitol Hill who say, “No, let’s just extend this program just year by year through appropriations, not a reauthorization.” Which they say would rubber-stamp the Biden administration redirecting money towards abortion, which the Biden administration and everybody else denies is happening. And so we confirmed that Chairman Mike McCaul in the House and Lindsey Graham in the Senate are working with Democrats on some sort of reauthorization bill. It might not be the full five years, it might be three years, we don’t really know yet. But they think that at least a multiyear reauthorization will give the program some stability rather than the one-year funding patch that other House Republicans are mulling. So we’re going to see where this goes; obviously, it’s an interesting test for the influence of these anti-abortion groups on Capitol Hill. And my colleague and I also scooped that former President Bush, who oversaw the creation of this program, is quietly lobbying certain members, having meetings, and so we will see what kind of pull he still has in the party.
Rovner: Well, this was one of his signature achievements, literally. So it’s something that I know that … and we should point out, unlike the spending bills, the appropriation bills, if this doesn’t happen by Oct. 1, nothing stops, it’s just it becomes theoretically unauthorized, like many programs are, and it’s considered not a good sign for the program.
Luhby: One thing I also wanted to just bring up quickly, tangentially related to health care, but also showing how bipartisan programs are not getting the support that they did, is the WIC program, which is food assistance for women, infants and children, needs more money. Actually participation is up, but even before that, the House Republicans wanted to cut the funding for it, and that was going to be a big divide between them and the Senate. And now because participation is up, the Biden administration is actually asking for another $1.4 billion for the program. This is a program that, again, has always had support and has been fully funded, not had to turn people away. And now it’s looking that many women and small children may not be able to get the assistance if Congress isn’t able to actually fund the program fully.
Rovner: Yes, they’re definitely tied in knots. Well, Oct. 1 turns out to be a key date for a lot of health care issues. It’s also the day drugmakers are supposed to notify Medicare whether they will participate in negotiations for the 10 high-cost drugs Medicare has chosen for the first phase of the program that Congress approved last year. But that might all get blocked if a federal judge rules in favor of a suit brought by the U.S. Chamber of Commerce, among others. Rachel, there was a hearing on this last week, where does this lawsuit stand and when do we expect to hear something from the judge?
Cohrs: So the judge didn’t ask any questions of the attorneys, so they were essentially presenting arguments that we’ve already seen previewed in some of the briefing materials. We are expecting some action by Oct. 1, which is when the Chamber had requested a ruling on whether there’s going to be a preliminary injunction, just because drugmakers are supposed to sign paperwork and submit data to CMS by that Oct. 1 date. So I think we are just waiting to see what the ruling might be. Some of the key issues or whether the Chamber actually has standing to file this lawsuit, given it’s not an actual drug manufacturer. And there was some quibbling about what members they listed in the lawsuit. And then I think they only addressed the argument that the negotiation program violated drugmakers’ due process rights, which isn’t the full scope of the lawsuit. It’s not an indicator of success really anywhere else, but it is important because it is the very first test. And if a preliminary injunction is issued, then it brings everything to a halt. So I think it would be very impactful for other drugmakers as well.
Rovner: Nobody told me when I became a health reporter that I was going to have to learn every step of the civil judicial process, and yet here we are. Well, while we are still on the subject of drug prices, a new poll from the AP and the NORC finds that while the public, Republicans and Democrats, still strongly support Medicare being able to negotiate the price of prescription drugs, President [Joe] Biden is getting barely any credit for having accomplished something that Democrats have been pushing for for more than 20 years. Most respondents in the survey either don’t think the plan goes far enough, because, as we point out, it’s only the first 10 drugs, or they don’t realize that he’s the one that helped push it over the finish line. This should have been a huge win and it’s turning out to be a nothing. Is that going to change?
Ollstein: It’s kind of a “Groundhog Day” of the Obamacare experience in which they pass this big, huge reform that people had been fighting for so long, but they’re trying to campaign on it when people aren’t really feeling the effects of it yet. And so when people aren’t really feeling the benefit and they’re hearing, “Oh, we’re lowering your drug prices.” But they’re going to the pharmacy and they’re paying the same very high amount, it’s hard to get a political win from that. The long implementation timeline is against them there. So there are some provisions that kick in more quickly, so we’ll have to see if that makes any kind of difference. I think that’s why you hear them talk a lot about the insulin price cap because that is already in effect, but that hits fewer people than the bigger negotiation will theoretically hit eventually. So it’s tough, and I think it leaves a vacuum where the drug industry and conservatives can fearmonger or raise concerns and say, “This will make drugs inaccessible and they won’t submit new cures for approval.” And all this stuff. And because people aren’t feeling the benefits, but they’re hearing those downsides, yeah, that makes the landscape even tougher for Democrats.
Luhby: This is very much the pattern that the Biden administration has had with a lot of its achievements or successes because it’s also not getting any credit for anything in the economy. The job market is relatively strong still, the economy is relatively strong. Yes, we have high inflation and high prices, even though that’s moderated, prices are still high, and that’s what people are seeing. Gas prices are now up again, which is not good for the administration. But they’re touting their Bidenomics, which also includes lowering drug prices. But generally polling shows, including our CNN polling shows, that people do not think the economy is doing well and they’re not giving Biden any credit for anything.
Cohrs: I think part of the problem is that … it’s different from the Affordable Care Act where it was health care, health care, health care for a very long time. This is lumped into a bill called the Inflation Reduction Act. I think it got lumped in with climate, got looped in with tax. And the media, we did our best, but it was hard to explain everything that was in the bill. And Medicare negotiation is complicated, it’s wonky, and I don’t know that people fully understood everything that was in the Inflation Reduction Act when it passed and they capitulated to Sen. [Joe] Manchin for what he wanted to name it. And so I think some of that got muddled when it first passed and they’re kind of trying to do catch-up work to explain, again, like Alice said, something that hasn’t gone into effect, which is a really tough uphill climb.
Rovner: This has been a continuing frustration for Democrats, which is that actually getting legislation done in Washington always involves some kind of compromise, and it’s always going to be incremental. And the public doesn’t really respond to things that are incremental. It’s like, “Why isn’t it bigger? Why didn’t they do what they promised?” And so the Republicans get more credit for stopping things than the Democrats get for actually passing things. Right. Well, let us turn to abortion. The breaking news today is that the Senate is finally acting to bust the blockade Alabama Republican Sen. Tommy Tuberville has had on military promotion since February to protest a Defense Department policy allowing service people leave to travel to other states for abortions. And Tuberville himself is part of this breakage, right, Alice? And it’s not a full breakage.
Ollstein: Right. And there have also been some interesting interviews that maybe raise questions on how much Tuberville understands the mechanics of what he’s doing because he said in an interview, “Oh, well, the people who were in these jobs before, they’ll just stay in it and it’s fine.” And they had to explain, “Well, statutorily, they can’t after a certain date.” And he seemed surprised by that. And now you’re seeing these attempts to go around his own blockade, and Democrats to go around his blockade. In part, for a while, Democrats were really not wanting to do that, schedule these votes, until he fully relented because they thought that would increase the pressure.
Rovner: They didn’t want to do it nomination by nomination for the big-picture ones because they were afraid that would leave behind the smaller ones.
Ollstein: Exactly. But this is dragging on so long that I think you’re seeing some frustration and desire to do something, even if it’s not fully resolving the standoff.
Rovner: And I’m seeing frustration from other Republicans. Again, the idea of a Republican holding up military promotions for six months is something that was not on my Republican Bingo card five years ago or even two years ago. I’m sure he’s not making a lot of his colleagues very happy with this. So on the Republican presidential campaign trail, abortion continues to be a subject all the candidates are struggling with — all of them, it seems, except former President Donald Trump, who said in an interview with NBC on Sunday that he alone can solve this. Francis, you have the tape.
Donald Trump: We are going to agree to a number of weeks or months or however you want to define it, and both sides are going to come together, and both sides, and this is a big statement, both sides will come together and for the first time in 52 years, you’ll have an issue that we can put behind us.
Rovner: OK. Well, Trump — who actually seemed all over the place about where he is on the issue in a fairly bald attempt to both placate anti-abortion hardliners in the party’s base and those who support abortion rights, whose votes he might need if he wants to win another election — criticized his fellow Republicans, who he called, “inarticulate on the subject.” I imagine that’s not going over very well among all of the other Republican candidates, right?
Ollstein: We have a piece up on this this morning. One, Trump is clearly acting like he has already won the primary, so he is trying to speak to a general audience, as you noted, and go after those votes in the middle that he may need and so he’s pitching this compromise. And we have a piece that the anti-abortion groups are furious about this, but they don’t really know what to do about it because he probably is going to be the nominee and they’re probably going to spend tens of millions to help elect him if he is, even though they’re furious with these comments he’s making. And so it’s a really interesting moment for their influence. Of course, Trump is trying to have it both ways, he also is calling himself the most pro-life president of all time. He is continually taking credit for appointing the justices to the Supreme Court who overturned Roe v. Wade.
Rovner: Which he did.
Ollstein: Exactly.
Rovner: Which is true.
Ollstein: Which he definitely did. But he is not toeing the line anymore that these groups want. These groups want him to endorse some sort of federal ban on abortion and they want him to praise states like Florida that have passed even stricter bans. He is not doing that. And so there’s an interesting dynamic there. And now his primary opponents see this as an opening, they’re trailing him in the polls, and so they’re trying to capitalize on this. [Gov. Ron] DeSantis and a bunch of others came out blasting him for these abortion remarks. But again, he’s acting like he’s already won the primary, he’s brushing it off and ignoring them.
Rovner: I love how confident he is though, that there’s a way to settle this — really, that there is a compromise, it’s just nobody’s been smart enough to get to it.
Ollstein: Well, he also, in the same interview, he said he’ll solve the Ukraine-Russia war in a day. So I mean, I think we should consider it in that context. It was interesting when I talked to all these different anti-abortion groups, they all said the idea of cutting some sort of deal is ludicrous. There is no magic deal that everybody would be happy about. If anything …
Rovner: And those on the other side will say the same thing.
Ollstein: Exactly. How could you watch what’s happened over the past year or 30 years and think that’s remotely possible? However, they did acknowledge that him saying that does appeal to a certain kind of voter, who is like, “Yeah, let’s just compromise. Let’s just get past this. I’m sick of all the fighting.” So it’s another interesting tension.
Rovner: Yeah. And I love how Trump always says the quiet part out loud, which is that this is not a great issue for Republicans and they’re not talking about it right. It’s like Republicans know this is a not-great issue for Republicans, but they don’t usually say that in an interview on national television. That is Trump, and this will continue. Well, finally this week I wanted to talk about what I am calling the dark underbelly of the new weight loss drugs. This is my extra credit this week. It’s a Washington Post story by Daniel Gilbert called “Inside the Gold Rush to Sell Cheaper Imitations of Ozempic.” It’s about the huge swell of sometimes not-so-legitimate websites and wellness spas selling unapproved formulations of semaglutide and tirzepatide — better known by their brand names Ozempic, Wegovy, and Mounjaro — to unsuspecting consumers because the demand for these diabetes drugs is so high for people who want to lose weight. The FDA has declared semaglutide at least to be in shortage for the people it was originally approved for, those with Type 2 diabetes. But that designation legally allows compounding pharmacies to manufacture their own versions, at least in some cases, except to quote the piece, “Since then, a parallel marketplace with no modern precedent has sprung up attracting both licensed medical professionals and entrepreneurs with histories ranging from regulatory violations to armed robbery.” Meanwhile, and this is coming from a separate story, both Eli Lilly and Novo Nordisk, the manufacturers of the approved versions of the drugs, are suing companies they say are selling unapproved versions of their drug, including, in some cases, drugs that actually pretend to be the brand name drug that aren’t. This is becoming really a big messy buyer-beware market, right? Rachel, you guys have written about this.
Cohrs: It has. Yeah, my colleagues have done great coverage, including I think the lawsuit by manufacturers of these drugs who are seeing their profits slipping through their fingers as patients are turning to these alternatives that aren’t necessarily approved by the FDA. And I think there are also risks because we have seen some side effects from these medications; they range from some very serious GI symptoms to strange dreams. There’s just a whole lot going on there. And I think it is concerning that some patients are getting ahold of these medications, which are expensive if you’re buying them the traditional way. And again, for weight loss, I think some of these medications are still off-label, they’re not FDA-approved. So if they’re getting these without any supervision from a medical provider or somebody who they can ask when they have questions that come up and are monitoring for some of these other side effects, then I think it is a very dangerous game for these patients. And I think it’s just a symptom of this outpouring of interest and the regulators’, I think, failure to keep up with it. And there’s also some supply concerns. So I think it’s just this perfect storm of desperation from patients and the bureaucracy struggling to keep up.
Rovner: Yeah. One of the reasons I chose the story is I really feel like this is unprecedented. I mean, I suppose it could have been predicted because these drugs do seem to be very good at what they do and they are very expensive and very hard to get, so not such a surprise that not-so-honest people might spring up to try and fill the void. But it’s still a little bit scary to see people selling heaven only knows what to people who are very anxious to take things.
Luhby: And in related news, there are more doctors who are interested in obesity medicine now, so everyone is trying to cash in.
Rovner: Yeah, I mean, eventually I imagine this will sort itself out. It’s just that at the beginning when it’s so popular, although I will still … I keep thinking this, is the solution to really throw this much money at it or to try to figure out how to make these drugs cheaper? If it’s going to be such a societal good, maybe we should do something about the price. Anyway, that is my extra credit in this week’s news. Now we will take a quick break and then we’ll come back with the rest of our extra credits.
Hey, “What the Health?” listeners, you already know that few things in health care are ever simple. So, if you like our show, I recommend you also listen to “Tradeoffs,” a podcast that goes even deeper into our costly, complicated, and often counterintuitive health care system. Hosted by longtime health care journalist and friend Dan Gorenstein, “Tradeoffs” digs into the evidence and research data behind health care policies and tells the stories of real people impacted by decisions made in C-suites, doctors’ offices, and even Congress. Subscribe wherever you listen to your podcasts.
OK, we are back and it’s time for our extra-credit segment. That’s when we each recommend a story we read this week we think you should read, too. As always, don’t worry if you miss it; we will post the links on the podcast page at kffhealthnews.org and in our show notes on your phone or other mobile device. Tami, why don’t you go first this week?
Luhby: Sure. Well, this week I chose a good story by one of my colleagues, Brenda Goodman. It’s titled “Supply and Insurance Issues Snarl Fall Covid-19 Vaccine Campaign for Some.” And we’ve all been hearing this, I heard this from a friend of mine who’s a doctor, we know Cynthia Cox at KFF tweeted about this. And that even though the new vaccines are ready and the Biden administration has been pushing people to go get them, and many people are eager to get them, they’re not so easy to get. Either because drugstores are running out, that’s what happened to my friend. She went in and said there just wasn’t any supply available. Or for some other people, they’re supposed to be free for most Americans, but the insurance companies haven’t caught up with that yet. So they go in and either they’re denied or the pharmacy tells them that they have to pay potentially $200 for the vaccines. So the problem here is that there’s already an issue with getting vaccines and people getting vaccinated in this country and then putting up extra hurdles for them will only cause more problems and cause fewer people to get vaccinated because some people may not come back.
Rovner: Talk about something that should have been predictable. The distributors knew it was going to be available and pretty much when, and the insurance companies knew it was going to be available and pretty much when, and yet somehow they seem to have not gotten their act together when the predictable surge of people wanting to get the vaccine early came about. Alice, you wanted to add something?
Ollstein: Just anecdotally, the supply and the demand are completely out of whack. My partner is back home in Alabama right now and he was at a pharmacy where they were just wandering around asking random people, “Will you take the shot? Will you take the shot?” And a bunch of people were saying, “No.” And meanwhile, here in D.C., myself and everyone I know is just calling around wanting to get it and not able to. And so you think we’d have figured this out better after so many years of this.
Rovner: Well, I have an appointment for tomorrow. We’ll see if it happens. Rachel, why don’t you go next?
Cohrs: Sure. I chose a KFF Health News story by Arthur Allen, and the headline is “Save Billions or Stick With Humira? Drug Brokers Steer Americans to the Costly Choice.” And I just love a story where it’s off the news cycle a little bit and we see this big splashy announcement. And I think Arthur did a great job of following up here and seeing what actually was happening with formulary placement for Humira and the new biosimilars that just came on the market.
Rovner: Yep. Remind us what Humira is?
Cohrs: Oh, yeah. So it’s one of the most profitable drugs ever. The company that makes it, AbbVie, had created this big patent thicket to try to prevent it from competition for a very long time, but this year saw competition that had been on the market in Europe finally come online in the U.S. So again, a big change for AbbVie, for the market. But I think there was concern about whether people would actually switch to these new medications that have lower prices. But again, as it gets caught up and spit out of our drug supply chain, there are a whole lot of incentives that don’t necessarily result in the cheaper medication being prescribed. And Arthur found that Express Scripts and Optum, which are two of the three biggest pharmacy benefit managers, have the biosimilar versions of Humira at the same price as Humira. So that doesn’t really create a lot of incentive for people to switch. So I think it was just great follow-up reporting and we don’t really have a lot of visibility into these formularies sometimes. So I think it was a illuminating piece.
Rovner: Yeah. And the mess that is drug pricing. Alice.
Ollstein: So I also chose a great piece by my colleague Adam Cancryn and it’s called “The Anti-Vaccine Movement Is on the Rise. The White House Is at a Loss Over What to Do About It.” It’s part of a series we’re doing on anti-vax sentiment and its impacts. And this is just going into how the Biden administration really doesn’t have a plan for combating this, even as it’s posing a bigger and bigger public health threat. And some of their attempts to go after misinformation online were stymied in court and they also are struggling with not wanting to elevate it by debunking it — that that age-old tension of, is it better to just ignore it or is it better to combat it directly? A lot of this is also tying into RFK Jr.’s presidential bid and how much to acknowledge that or not. But the impact is that they’re not really taking this on, even as it’s getting worse and worse in the country.
Rovner: And I got a bunch of emails this week about the anti-vax movement spreading to pets — that people are now resisting getting their dogs and cats vaccinated. Seriously. I mean, it is a serious problem. Obviously, if people stop getting rabies vaccines, that could be a big deal. So something else to watch. All right. Well, I already did my extra credit. So that is it for this week. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left us a review; that helps other people find us, too. Special thanks as always to our indefatigable engineer, Francis Ying. Also, as always, you can email us your comments or questions. We’re at whatthehealth@kff.org. Or you can tweet me; I’m still @jrovner on X and on Bluesky. Tami?
Luhby: You can tweet me at @Luhby. I sometimes check it still.
Rovner: Rachel.
Cohrs: I’m on X @rachelcohrs.
Rovner: Alice.
Ollstein: I’m @AliceOllstein.
Rovner: We will be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
2 years 1 month ago
Elections, Health Care Costs, Health Industry, Medicaid, Medicare, Multimedia, Pharmaceuticals, Public Health, Abortion, Biden Administration, Drug Costs, HIV/AIDS, KFF Health News' 'What The Health?', Podcasts, U.S. Congress, Women's Health
Save Billions or Stick With Humira? Drug Brokers Steer Americans to the Costly Choice
Tennessee last year spent $48 million on a single drug, Humira — about $62,000 for each of the 775 patients who were covered by its employee health insurance program and receiving the treatment. So when nine Humira knockoffs, known as biosimilars, hit the market for as little as $995 a month, the opportunity for savings appeared ample and immediate.
But it isn’t here yet. Makers of biosimilars must still work within a health care system in which basic economics rarely seems to hold sway.
For real competition to take hold, the big pharmacy benefit managers, or PBMs, the companies that negotiate prices and set the prescription drug menu for 80% of insured patients in the United States, would have to position the new drugs favorably in health plans.
They haven’t, though the logic for doing so seems plain.
Humira has enjoyed high-priced U.S. exclusivity for 20 years. Its challengers could save the health care system $9 billion and herald savings from the whole class of drugs called biosimilars — a windfall akin to the hundreds of billions saved each year through the purchase of generic drugs.
The biosimilars work the same way as Humira, an injectable treatment for rheumatoid arthritis and other autoimmune diseases. And countries such as the United Kingdom, Denmark, and Poland have moved more than 90% of their Humira patients to the rival drugs since they launched in Europe in 2018. Kaiser Permanente, which oversees medical care for 12 million people in eight U.S. states, switched most of its patients to a biosimilar in February and expects to save $300 million this year alone.
Biologics — both the brand-name drugs and their imitators, or biosimilars — are made with living cells, such as yeast or bacteria. With dozens of biologics nearing the end of their patent protection in the next two decades, biosimilars could generate much higher savings than generics, said Paul Holmes, a partner at Williams Barber Morel who works with self-insured health plans. That’s because biologics are much more expensive than pills and other formulations made through simpler chemical processes.
For example, after the first generics for the blockbuster anti-reflux drug Nexium hit the market in 2015, they cost around $10 a month, compared with Nexium’s $100 price tag. Coherus BioSciences launched its Humira biosimilar, Yusimry, in July at $995 per two-syringe carton, compared with Humira’s $6,600 list price for a nearly identical product.
“The percentage savings might be similar, but the total dollar savings are much bigger,” Holmes said, “as long as the plan sponsors, the employers, realize the opportunity.”
That’s a big if.
While a manufacturer may need to spend a few million dollars to get a generic pill ready to market, makers of biosimilars say their development can require up to eight years and $200 million. The business won’t work unless they gain significant market share, they say.
The biggest hitch seems to be the PBMs. Express Scripts and Optum Rx, two of the three giant PBMs, have put biosimilars on their formularies, but at the same price as Humira. That gives doctors and patients little incentive to switch. So Humira remains dominant for now.
“We’re not seeing a lot of takeup of the biosimilar,” said Keith Athow, pharmacy director for Tennessee’s group insurance program, which covers 292,000 state and local employees and their dependents.
The ongoing saga of Humira — its peculiar appeal to drug middlemen and insurers, the patients who’ve benefited, the patients who’ve suffered as its list price jumped sixfold since 2003 — exemplifies the convoluted U.S. health care system, whose prescription drug coverage can be spotty and expenditures far more unequal than in other advanced economies.
Biologics like Humira occupy a growing share of U.S. health care spending, with their costs increasing 12.5% annually over the past five years. The drugs are increasingly important in treating cancers and autoimmune diseases, such as rheumatoid arthritis and inflammatory bowel disease, that afflict about 1 in 10 Americans.
Humira’s $200 billion in global sales make it the best-selling drug in history. Its manufacturer, AbbVie, has aggressively defended the drug, filing more than 240 patents and deploying legal threats and tweaks to the product to keep patent protections and competitors at bay.
The company’s fight for Humira didn’t stop when the biosimilars finally appeared. The drugmaker has told investors it doesn’t expect to lose much market share through 2024. “We are competing very effectively with the various biosimilar offerings,” AbbVie CEO Richard Gonzalez said during an earnings call.
How AbbVie Maintains Market Share
One of AbbVie’s strategies was to warn health plans that if they recommended biosimilars over Humira they would lose rebates on purchases of Skyrizi and Rinvoq, two drugs with no generic imitators that are each listed at about $120,000 a year, according to PBM officials. In other words, dropping one AbbVie drug would lead to higher costs for others.
Industry sources also say the PBMs persuaded AbbVie to increase its Humira rebates — the end-of-the-year payments, based on total use of the drug, which are mostly passed along by the PBMs to the health plan sponsors. Although rebate numbers are kept secret and vary widely, some reportedly jumped this year by 40% to 60% of the drug’s list price.
The leading PBMs — Express Scripts, Optum, and CVS Caremark — are powerful players, each part of a giant health conglomerate that includes a leading insurer, specialty pharmacies, doctors’ offices, and other businesses, some of them based overseas for tax advantages.
Yet challenges to PBM practices are mounting. The Federal Trade Commission began a major probe of the companies last year. Kroger canceled its pharmacy contract with Express Scripts last fall, saying it had no bargaining power in the arrangement, and, on Aug. 17, the insurer Blue Shield of California announced it was severing most of its business with CVS Caremark for similar reasons.
Critics of the top PBMs see the Humira biosimilars as a potential turning point for the secretive business processes that have contributed to stunningly high drug prices.
Although list prices for Humira are many times higher than those of the new biosimilars, discounts and rebates offered by AbbVie make its drug more competitive. But even if health plans were paying only, say, half of the net amount they pay for Humira now — and if several biosimilar makers charged as little as a sixth of the gross price — the costs could fall by around $30,000 a year per patient, said Greg Baker, CEO of AffirmedRx, a smaller PBM that is challenging the big companies.
Multiplied by the 313,000 patients currently prescribed Humira, that comes to about $9 billion in annual savings — a not inconsequential 1.4% of total national spending on pharmaceuticals in 2022.
The launch of the biosimilar Yusimry, which is being sold through Mark Cuban’s Cost Plus Drugs pharmacy and elsewhere, “should send off alarms to the employers,” said Juliana Reed, executive director of the Biosimilars Forum, an industry group. “They are going to ask, ‘Time out, why are you charging me 85% more, Mr. PBM, than what Mark Cuban is offering? What is going on in this system?’”
Cheaper drugs could make it easier for patients to pay for their drugs and presumably make them healthier. A KFF survey in 2022 found that nearly a fifth of adults reported not filling a prescription because of the cost. Reports of Humira patients quitting the drug for its cost are rife.
Convenience, Inertia, and Fear
When Sue Lee of suburban Louisville, Kentucky, retired as an insurance claims reviewer and went on Medicare in 2017, she learned that her monthly copay for Humira, which she took to treat painful plaque psoriasis, was rising from $60 to $8,000 a year.
It was a particularly bitter experience for Lee, now 81, because AbbVie had paid her for the previous three years to proselytize for the drug by chatting up dermatology nurses at fancy AbbVie-sponsored dinners. Casting about for a way to stay on the drug, Lee asked the company for help, but her income at the time was too high to qualify her for its assistance program.
“They were done with me,” she said. Lee went off the drug, and within a few weeks the psoriasis came back with a vengeance. Sores covered her calves, torso, and even the tips of her ears. Months later she got relief by entering a clinical trial for another drug.
Health plans are motivated to keep Humira as a preferred choice out of convenience, inertia, and fear. While such data is secret, one Midwestern firm with 2,500 employees told KFF Health News that AbbVie had effectively lowered Humira’s net cost to the company by 40% after July 1, the day most of the biosimilars launched.
One of the top three PBMs, CVS Caremark, announced in August that it was creating a partnership with drugmaker Sandoz to market its own cut-rate version of Humira, called Hyrimoz, in 2024. But Caremark didn’t appear to be fully embracing even its own biosimilar. Officials from the PBM notified customers that Hyrimoz will be on the same tier as Humira to “maximize rebates” from AbbVie, Tennessee’s Athow said.
Most of the rebates are passed along to health plans, the PBMs say. But if the state of Tennessee received a check for, say, $20 million at the end of last year, it was merely getting back some of the $48 million it already spent.
“It’s a devil’s bargain,” said Michael Thompson, president and CEO of the National Alliance of Healthcare Purchaser Coalitions. “The happiest day of a benefit executive’s year is walking into the CFO’s office with a several-million-dollar check and saying, ‘Look what I got you!’”
Executives from the leading PBMs have said their clients prefer high-priced, high-rebate drugs, but that’s not the whole story. Some of the fees and other payments that PBMs, distributors, consultants, and wholesalers earn are calculated based on a drug’s price, which gives them equally misplaced incentives, said Antonio Ciaccia, CEO of 46Brooklyn, a nonprofit that researches the drug supply chain.
“The large intermediaries are wedded to inflated sticker prices,” said Ciaccia.
AbbVie has warned some PBMs that if Humira isn’t offered on the same tier as biosimilars it will stop paying rebates for the drug, according to Alex Jung, a forensic accountant who consults with the Midwest Business Group on Health.
AbbVie did not respond to requests for comment.
One of the low-cost Humira biosimilars, Organon’s Hadlima, has made it onto several formularies, the ranked lists of drugs that health plans offer patients, since launching in February, but “access alone does not guarantee success” and doesn’t mean patients will get the product, Kevin Ali, Organon’s CEO, said in an earnings call in August.
If the biosimilars are priced no lower than Humira on health plan formularies, rheumatologists will lack an incentive to prescribe them. When PBMs put drugs on the same “tier” on a formulary, the patient’s copay is generally the same.
In an emailed statement, Optum Rx said that by adding several biosimilars to its formularies at the same price as Humira, “we are fostering competition while ensuring the broadest possible choice and access for those we serve.”
Switching a patient involves administrative costs for the patient, health plan, pharmacy, and doctor, said Marcus Snow, chair of the American College of Rheumatology’s Committee on Rheumatologic Care.
Doctors’ Inertia Is Powerful
Doctors seem reluctant to move patients off Humira. After years of struggling with insurance, the biggest concern of the patient and the rheumatologist, Snow said, is “forced switching by the insurer. If the patient is doing well, any change is concerning to them.” Still, the American College of Rheumatology recently distributed a video informing patients of the availability of biosimilars, and “the data is there that there’s virtually no difference,” Snow said. “We know the cost of health care is exploding. But at the same time, my job is to make my patient better. That trumps everything.”
“All things being equal, I like to keep the patient on the same drug,” said Madelaine Feldman, a New Orleans rheumatologist.
Gastrointestinal specialists, who often prescribe Humira for inflammatory bowel disease, seem similarly conflicted. American Gastroenterological Association spokesperson Rachel Shubert said the group’s policy guidance “opposes nonmedical switching” by an insurer, unless the decision is shared by provider and patient. But Siddharth Singh, chair of the group’s clinical guidelines committee, said he would not hesitate to switch a new patient to a biosimilar, although “these decisions are largely insurance-driven.”
HealthTrust, a company that procures drugs for about 2 million people, has had only five patients switch from Humira this year, said Cora Opsahl, director of the Service Employees International Union’s 32BJ Health Fund, a New York state plan that procures drugs through HealthTrust.
But the biosimilar companies hope to slowly gain market footholds. Companies like Coherus will have a niche and “they might be on the front end of a wave,” said Ciaccia, given employers’ growing demands for change in the system.
The $2,000 out-of-pocket cap on Medicare drug spending that goes into effect in 2025 under the Inflation Reduction Act could spur more interest in biosimilars. With insurers on the hook for more of a drug’s cost, they should be looking for cheaper options.
For Kaiser Permanente, the move to biosimilars was obvious once the company determined they were safe and effective, said Mary Beth Lang, KP’s chief pharmacy officer. The first Humira biosimilar, Amjevita, was 55% cheaper than the original drug, and she indicated that KP was paying even less since more drastically discounted biosimilars launched. Switched patients pay less for their medication than before, she said, and very few have tried to get back on Humira.
Prescryptive, a small PBM that promises transparent policies, switched 100% of its patients after most of the other biosimilars entered the market July 1 “with absolutely no interruption of therapy, no complaints, and no changes,” said Rich Lieblich, the company’s vice president for clinical services and industry relations.
AbbVie declined to respond to him with a competitive price, he said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
2 years 1 month ago
Health Care Costs, Health Industry, Pharmaceuticals, Drug Costs, Kentucky, New York, Prescription Drugs, Tennessee
KFF Health News' 'What the Health?': Underinsured Is the New Uninsured
The Host
Emmarie Huetteman
KFF Health News
Emmarie Huetteman, associate Washington editor, previously spent more than a decade reporting on the federal government, most recently covering surprise medical bills, drug pricing reform, and other health policy debates in Washington and on the campaign trail.
The Host
Emmarie Huetteman
KFF Health News
Emmarie Huetteman, associate Washington editor, previously spent more than a decade reporting on the federal government, most recently covering surprise medical bills, drug pricing reform, and other health policy debates in Washington and on the campaign trail.
The annual U.S. Census Bureau report this week revealed a drop in the uninsured rate last year as more working-age people obtained employer coverage. However, this year’s end of pandemic-era protections — which allowed many people to stay on Medicaid — is likely to have changed that picture quite a bit since. Meanwhile, reports show even many of those with insurance continue to struggle to afford their health care costs, and some providers are encouraging patients to take out loans that tack interest onto their medical debt.
Also, a mystery is unfolding in the federal budget: Why has recent Medicare spending per beneficiary leveled off? And the CDC recommends anyone who isat least 6 months old get the new covid booster.
This week’s panelists are Emmarie Huetteman of KFF Health News, Margot Sanger-Katz of The New York Times, Sarah Karlin-Smith of the Pink Sheet, and Joanne Kenen of the Johns Hopkins Bloomberg School of Public Health and Politico.
Panelists
Sarah Karlin-Smith
Pink Sheet
Joanne Kenen
Johns Hopkins Bloomberg School of Public Health and Politico
Margot Sanger-Katz
The New York Times
Among the takeaways from this week’s episode:
- The Census Bureau reported this week that the uninsured rate dropped to 10.8% in 2022, down from 11.6% in 2021, driven largely by a rise in employer-sponsored coverage. Since then, pandemic-era coverage protections have lapsed, though it remains to be seen exactly how many people could lose Medicaid coverage and stay uninsured.
- A concerning number of people who have insurance nonetheless struggle to afford their out-of-pocket costs. Medical debt is a common, escalating problem, exacerbated now as hospitals and other providers direct patients toward bank loans, credit cards, and other options that also saddle them with interest.
- Some state officials are worried that people who lose their Medicaid coverage could choose short-term health insurance plans with limited benefits — so-called junk plans — and find themselves owing more than they’d expect for future care.
- Meanwhile, a mystery is unfolding in the federal budget: After decades of warnings about runaway government spending, why has spending per Medicare beneficiary defied predictions and leveled off? At the same time, private insurance costs are increasing, with employer-sponsored plans expecting their largest increase in more than a decade.
- And the push for people to get the new covid booster is seeking to enshrine it in Americans’ annual preventive care regimen.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week that they think you should read, too:
Emmarie Huetteman: KFF Health News’ “The Shrinking Number of Primary Care Physicians Is Reaching a Tipping Point,” by Elisabeth Rosenthal.
Sarah Karlin-Smith: MedPage Today’s “Rural Hospital Turns to GoFundMe to Stay Afloat,” by Kristina Fiore.
Joanne Kenen: ProPublica’s “How Columbia Ignored Women, Undermined Prosecutors and Protected a Predator for More Than 20 Years,” by Bianca Fortis and Laura Beil.
Margot Sanger-Katz: Congressional Budget Office’s “Raising the Excise Tax on Cigarettes: Effects on Health and the Federal Budget.”
Also mentioned in this week’s episode:
- U.S. Census Bureau’s “Health Insurance Coverage of U.S. Workers Increased in 2022,” by Rachel Lindstrom, Katherine Keisler-Starkey, and Lisa Bunch.
- The Commonwealth Fund’s “Can Older Adults with Employer Coverage Afford Their Health Care?” by Lauren A. Haynes and Sara R. Collins.
- KFF Health News’ “What One Lending Company’s Hospital Contracts Reveal About Financing Patient Debt,” by Noam N. Levey.
- The New York Times’ “A Huge Threat to the U.S. Budget Has Receded. And No One Is Sure Why,” by Margot Sanger-Katz, Alicia Parlapiano, and Josh Katz.
- The Wall Street Journal’s “Health-Insurance Costs Are Taking Biggest Jumps in Years,” by Anna Wilde Mathews.
- The New York Times’ “The N.Y.C. Neighborhood That’s Getting Even Thinner on Ozempic,” by Joseph Goldstein.
click to open the transcript
Transcript: Underinsured Is the New Uninsured
KFF Health News’ ‘What the Health?’
Episode Title: Underinsured Is the New Uninsured
Episode Number: 314
Published: Sept. 14, 2023
[Editor’s note: This transcript, generated using transcription software, has been edited for style and clarity.]
Emmarie Huetteman: Hello and welcome back to “What the Health?” I’m Emmarie Huetteman, a Washington editor for KFF Health News. I’m filling in for Julie [Rovner] this week, who’s on vacation. And I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, Sept. 14, at 11 a.m. As always, news happens fast, and things might have changed by the time you hear this. So, here we go. We’re joined today by video conference by Margot Sanger-Katz of The New York Times.
Margot Sanger-Katz: Good morning, everybody.
Huetteman: Sarah Karlin-Smith of the Pink Sheet.
Sarah Karlin-Smith: Hi there.
Huetteman: And Joanne Kenen of the Johns Hopkins Bloomberg School of Public Health and Politico.
Joanne Kenen: Hi, everybody.
Huetteman: No interview this week, so let’s get right to the news. The percentage of working-age adults with health insurance went up last year, according to the annual Census report out this week. As a result, the uninsured rate dropped to 10.8% in 2022. But lower uninsured rates may be obscuring another problem: the number of people who are underinsured and facing high out-of-pocket costs. The Commonwealth Fund released a report last month on how difficult it is for many older adults with employer coverage to afford care. And recent reporting here at KFF Health News has probed how medical providers are steering patients toward bank loans and credit cards that saddled them with interest on top of their medical debt. So, the number of people without insurance is dropping. But that doesn’t mean that health care is becoming more affordable. So what does it mean to be underinsured? Are the policy conversations that focus on the uninsured rate missing the mark?
Sanger-Katz: So, two things I would say. One is that I even think that the Census report on what’s happening with the uninsured is obscuring a different issue, which is that there’s been this artificial increase in the number of people who are enrolled in Medicaid as a result of this pandemic policy. So the Congress said to the states, if you want to get extra money for your Medicaid program through the public health emergency, then you can’t kick anyone out of Medicaid regardless of whether they are no longer eligible for the program. And that provision expired this spring. And so this is one of the big stories in health policy that’s happening this year. States are trying to figure out how to reevaluate all of these people who have been in their Medicaid program for all these years and determine who’s eligible and who’s not eligible. And there’s been quite a lot of very good reporting on what’s going on. And I think there’s a combination of people who are losing their Medicaid coverage because they really genuinely are no longer eligible for Medicaid. And there also appears to be quite a large number of people who are losing their Medicaid coverage for administrative hiccup reasons — because there’s some paperwork error, or because they moved and they didn’t get a letter, or some other glitch in the system. And so when I looked at these numbers on the uninsured rate, in some ways what it told us is we gave a whole bunch of people insurance through these public programs during the pandemic and that depressed the uninsured rate. But we know right now that millions of people have lost insurance, even in the last few months, with more to come later this year. And so I’m very interested in the next installment of the Census report when we get back to more or less a normal Medicaid system, how many people will be without insurance. So that’s just one thing. And then just to get to your question, I think having insurance does not always mean that you can actually afford to pay for the health care that you need. We’ve seen over the last few decades a shift towards higher-deductible health care plans where people have to pay more money out-of-pocket before their insurance kicks in. We’ve also seen other kinds of cost sharing increase, where people have to pay higher copayments or a percentage of the cost of their care. And we’ve also seen, particularly in the Obamacare exchanges, but also in the employer market, that there’s a lot of insurance that doesn’t include any kind of out-of-network benefit. So it means, you know, if you can go to a provider who is covered by your insurance, your insurance will pay for it. But if you can’t find someone who’s covered by your insurance, you could still get hit with a big bill. The sort of surprise bills of old are banned. But, you know, the doctor can tell you in advance, and you can go and get all these medical services and then end up with some big bills. So whether or not just having an insurance card is really enough to ensure that people have access to health care remains an open question. And I think we have seen a lot of evidence over recent years that even people with insurance encounter a lot of financial difficulties when they get sick and often incur quite a lot of debt despite having insurance that protects them from the unlimited costs that they might face if they were uninsured.
Huetteman: Joanne.
Kenen: I would say two big things. The uninsurance rate, which we all think is going to go up because of this Medicaid unwinding, it’s worth stopping and thinking about. It’s what? 7.9[%]? Was that the number?
Huetteman: It was 10.8, was the uninsured rate last year.
Sanger-Katz: It depends if you look at any time of the year or all of the year.
Kenen: Back when the ACA [Affordable Care Act] was passed, it was closer to something like 18. So in terms of really changing the magnitude of the uninsurance problem in America, the work isn’t done. But this is a really significant change. Secondly, some aspects of care are better — or within reach because the ACA made so many preventive and primary care services free. That, too, is a gain. Obviously, through the medical debt, which KFF [Health News] now has done a great job — oh, and believe me, and other reporters, you’ve done an amazing job, story after story. You know, the “Bill of the Month” series that you edited, it’s … but they’re not isolated cases. It’s not like, oh, this person ran into this, you know, cost buzz saw. There’s insane pricing issues! And out-of-pocket and, you know, deductibles and extras, and incredibly hard to sort out even if you are a sophisticated, insured consumer of health care. Pricing is a mess. There have been changes to the health care market, in terms of consolidation of ownership, more private equity, bigger entities that just have created … added a new dimension to this problem. So have we made gains? We’ve made really important gains. Under the original ACA passed under the Obama administration and the changes, the access and generosity of subsidy changes that the Biden administration has made, even though they’re time-limited, they have to be renewed. But, you know, are people still being completely hit over the head and every other body part by really expensive costs? Yes. That is still a heartbreaking and really serious problem. I mean, I can just give one tiny incident where somebody … I needed a routine imaging thing in network. The doctor in that hospital wasn’t reachable. I had my primary care person send in the order because she’s not part of that health care system. She’s in network. The imaging center is in network. The doctor who told me I needed this test is in network. But because the actual order came from somebody not in their hospital and in … on the Maryland side of the line, instead of the D.C. side of the line, the hospital imaging center decided it was going to be out of network. And because she’s not ours and wanted to charge me an insane amount of money. I sorted it out. But it took me an insane amount of time and I shouldn’t have needed to do that.
Huetteman: Yeah, that’s absolutely true.
Kenen: I could have paid it, if I had to.
Huetteman: Absolutely. And as you noted, I do edit the “Bill of the Month” series. And we see that with all kinds of patients, even the most enterprising patients can’t get an answer to simple questions like, is this in network or out of network? Why did I get this bill? And it’s asking way too much of most people to try and fit that into the rest of the things that they do every day. You know, Margot brought up the Medicaid unwinding. Well, let’s speaking of insurance, let’s catch up there for a moment because there was a little news this week. We’re keeping an eye on those efforts to strip ineligible beneficiaries from state Medicaid rolls since the covid-19 public health emergency ended. Now, some state officials are worried that people who lose coverage could opt to replace it with short-term insurance plans. You might know them as “junk plans.” They often come with lower price tags, but these short-term plans do not have to follow the Affordable Care Act’s rules about what to cover. And people in the plans have found themselves owing for care they thought would be covered. The Trump administration expanded these plans, but this summer the Biden administration proposed limiting them once more. Remind us: What changes has Biden proposed for so-called junk plans and for people who lose their coverage during the Medicaid unwinding? What other options are available to them?
Sanger-Katz: So the Biden administration’s proposal was to basically return these short-term plans to actual short-term coverage, which is what they were designed to do. Part of what the Trump administration did is they kept this category of short-term plans. But then they said basically, well, you can just keep them for several years. And so they really became a more affordable but less comprehensive substitute for ACA-compliant insurance. So the Biden administration just wants to kind of squish ’em back down and say, OK, you can have them for like a couple of months, but you can’t keep them forever. I will say that a lot of people who are losing their Medicaid coverage as a result of the unwinding are probably pretty low on the income scale, just as a result of them having qualified for Medicaid in the first place. And so a very large share of them are eligible for free or close-to-free health plans on the Obamacare exchanges. Those enhanced subsidies that Joanne mentioned, they’re temporary, but they’re there for a few years. They really make a big difference for exactly this population that’s losing Medicaid coverage. If you’re just over the poverty line, you can often get a free plan that’s a — this is very technical, but — it’s a silver plan with these cost-sharing wraparound benefits. And so you end up with a plan where you really don’t have to pay very much at the point of care. You don’t have to pay anything in a premium. So I think, in general, that is the most obvious answer for most of these people who are losing their Medicaid. But I think it is a challenge to navigate that system, for states to help steer people towards these other options, and for them to get enrolled in a timely way. Because, of course, Obamacare markets are not open all the time. They’re open during an open enrollment period or for a short period after you lose another type of coverage.
Huetteman: Absolutely. And a lot of these states actually have efforts that are normally focused on open enrollment right now. And some officials say that they are redirecting those efforts toward helping these folks who are losing their Medicaid coverage to find the options, like those exchange plans that are available for zero-dollar premiums or low premiums under the subsidies available.
Kenen: I have seen some online ads from HHS [the Department of Health and Human Services], saying, you know, “Did you lose your Medicaid?” and it’s state-specific — “Did you lose your Medicaid in Virginia?” I don’t live in Virginia, so I’m not sure why I’m getting it. My phone is telling me the Virginia one. But there is an HHS [ad], and it is saying if you lost your Medicaid, go to healthcare.gov, we can help. You know, we may be able to help you. So they are outreaching, although I’m afraid that somebody who actually lost it in Virginia might be getting an ad about Nebraska or whatever. I live close to Virginia. It’s close enough. But there is some effort to reach people in a plain English, accessible pop-up on your phone, or your web browser, kind of way. So I have seen that over the last few weeks because the special enrollment period, I mean, most people who are no longer eligible for Medicaid are eligible for something, and something other than a junk plan. Some of them have insurance at work now because the job market is better than it was in 2020, obviously. Many people will be eligible for these highly subsidized plans that Margot just talked about. Very few people should be left out in the cold, but there’s a lot of work to be done to make those connections.
Huetteman: Absolutely. Absolutely. And going back to the Census report for a second, it had noted that a big part of the increase in coverage came from employer-sponsored coverage among working-age adults, although we have, of course, seen those reports that say … and then they try to afford their health care costs. And it’s really difficult for a lot of them, even when they have that insurance, as we talked about. All right. So let’s move on. The New York Times is reporting a mystery unfolding in the federal budget. And I’d like to call it “The Case of Flat Medicare Spending.” After decades of warnings about runaway government spending, a recent Times analysis shows that spending per Medicare beneficiary has actually leveled off over more than a decade. Meanwhile, The Wall Street Journal reports that private health insurance costs are climbing. Next year, employer-sponsored plans could see their biggest cost increase in more than a decade, and that trend could continue. So what’s going on with insurance costs? Let’s start with Medicare. Margot, you were the lead reporter on the Times analysis. What explains this Medicare spending slowdown?
Sanger-Katz: So part of the reason why I have found it to be a somewhat enjoyable story is that I think there is a bit of a mystery. I talked to lots of people who have studied and written about this phenomenon over the years, and I think there was no one I talked to who said “I 100% understand what is going on here. And I can tell you, here’s the thing.” But there are a bunch of factors that I think a lot of people think are contributing, and I’ll just run through them quickly. One of them is Medicare is getting a little younger. The baby boomers are retiring generally, like, 65-year-olds are a little cheaper to take care of than 85-year-olds. So as the age mix gets younger, we’ve seen the average cost of taking care of someone in Medicare get a little smaller. That’s like the easiest one. I think another one is that Obamacare and other legislative changes that Congress has passed during this period have just mechanically reduced the amount of money that Medicare is spending. So the two most obvious ways are, in the Affordable Care Act, Congress took money away from Medicare Advantage plans, paid them a smaller premium for taking care of patients, and they also reduced the amount that hospitals get every year, as what’s called a productivity adjustment. So hospitals get a little raise on their pay rates every year. And the legislation tamped that down. There was also, some listeners may remember, the budget sequester that happened in 2011, 2012, where there was kind of a haircut that Medicare had to take across the board. So there have been these kind of legislative changes. They explain like a little bit of what is going on. And now I think the rest of it really has to do with the health care system itself. And part of that seems to be that this has been a period of relatively limited technological improvement. So, you know, for years medicine just kept getting better and better. We had these miracle cures, we had these amazing surgeries. We, you know, especially like in the area of cardiovascular disease, just enormous advances in recent decades where, you know, first bypass surgery and then stents and then, you know, drugs that could prevent heart attacks. And so I think, you know, health care spending kept climbing and climbing in part because there was better stuff to spend it on. It was expensive, but it really improved people’s health. And in recent years, there’s just been a little less of that. There have clearly been medical advances, particularly in the pharmaceutical space. You know, we have better treatments for cancer, for certain types of cancers, than we had before and for other important diseases. But these expensive innovations tend to affect smaller percentages of people. We haven’t had a lot of really big blockbusters that everyone in Medicare is taking. And so that seems to explain some of the slowdown. And then I think the last piece is, like, kind of the piece that’s the hardest to really explain or pin down, but it seems like there’s just something different that doctors and hospitals are doing. They’re getting more efficient. They’re not always buying the latest and greatest thing, if there’s not evidence to support it. They’re reducing their medical errors. And, you know, I think Obamacare probably gets a share of the credit here. It really created a lot of changes in the way we pay for medical care and in the Medicare program itself. And it created this innovation center that’s supposed to test out all of these different things. But I think also over the same period, we’ve seen the private sector make many of the same moves. You know, private insurers have gotten a little bit more stingy about covering new technologies without evidence. They’ve tended to pay physicians and hospitals in bundles, or paying them incentives for quality, not paying them for certain types of care that involve errors. And so a lot of people I talked to said that they think the medical system is reacting to all of the payers crunching down on them. And so they’re just not being quite as aggressive and they’re trying to think more about value, which I feel like is like kind of a lame buzzword that often doesn’t mean anything. But I think, you know, it’s a way of thinking about this change. And, you know, that’s the kind of thing, if culturally that endures, you know, could continue into the future. Whereas some of these other factors, like the demographics, the lack of technological development, those — the Obamacare, which was kind of a one-time legislative change, you know — those things may not continue into the future, which is why the fact that we’ve had 15 years of flat Medicare spending is no guarantee that Medicare spending won’t spike again in the future. And I think you were right to point to what’s happening in the private sector, because private sector insurance premiums also have been like a little bit on the flat side through this period. And I think there is potential for them to take off again.
Huetteman: Absolutely. And that’s what The Wall Street Journal’s reporting had just said, that the health care costs for coming into next year are climbing. Let’s talk about that for a minute. Why are private insurance costs rising as Medicare spending levels off? One of the things that I noticed is we talked about technological innovation. Pharmaceutical innovation seems to be one of the things that’s contributing to rising private health insurance costs and elsewhere, in particular, those weight-loss drugs I know.
Kenen: And the Alzheimer’s drugs.
Huetteman: And the Alzheimer’s drugs.
Kenen: Eventually they’ll become more widely available. Sarah knows way more than the rest of us.
Karlin-Smith: The Alzheimer’s drugs will probably be less of an issue for the private health insurance population. But certainly weight-loss drugs are something that private insurers are worried about what percentage of the population they will cover with these drugs. And I think insurance companies, they have to balance that … difficult balance between what percentage of the drug cost rate you put on patients and what do you build into premiums. And sometimes there’s only so much flexibility they can have there. So I think that’s a big reason for what you’re seeing here.
Huetteman: Yeah, absolutely.
Sanger-Katz: I think the weight-loss drugs are interesting because they kind of are, potentially, an example of the kind of technology that is both expensive and good for public health, right? So, you know, when we have all these improvements in cardiac disease, like, that was great. People didn’t have heart attacks. They didn’t have disability in old age. They lived longer lives. That was great. But it cost a ton of money. And I think because we have been going through this period in which costs have been kind of level, and there hasn’t been a lot of expensive breakthrough technology, we haven’t had to weigh those things against each other in the way that we might now, where we might have to say, OK, well, like, this is really expensive, but also, like, it has a lot of benefits. and how do we decide what the right cost benefit is as a society, as an employer, as a public insurance program? And I think we’re going to see a lot of payers and economists and other analysts really thinking hard about these trade-offs in a way that they, I think, haven’t really been forced to do very much in the last few years with … I mean, maybe with the possible exception of those breakthrough therapies for hepatitis C —also expensive, huge public health benefit. And it was a struggle for our system to figure out what to do with them.
Kenen: But, like the statins, which, you know, revolutionized heart health, these drugs that are useful for both diabetes and … weight loss, the demand of people who just want them because they want to lose those 20 pounds, insurers are not — Medicare at least is not — covering it. Insurers have some rules about “Are you pre-diabetic?” and etc., etc., but they cost a lot of money and a lot of people want to take them. So I think they’re clearly great for diabetes. They clearly are a whole new class of drugs that are going to do good things. We still don’t. … There’s still questions about who should be using them for the rest of their lives, for weight control, etc., etc. Yes, there are going to be benefits, but this era of … what is the typical cost per month, Sarah?
Karlin-Smith: The list price of these drugs are thousands of dollars per month. But I think to your point, Joanne, though, the trouble for insurance companies who are figuring out how to cover this is they’re starting to get more research that there are these actual health benefits outside of just weight loss. And once you start to say, you know, that these drugs help prevent heart attacks and have hard evidence of that, it becomes harder for them to deny coverage. I think to Margot’s point of the long-term benefits, you might see to health because of it, we get back to another issue in the U.S. health system is, which is these private health insurance companies might essentially basically be footing the bill for benefits that Medicare is going to reap, not necessarily the insurance companies, right? So if somebody, you know, doesn’t have a heart attack at 50 because they’re on these drugs, that’s great. But if the savings is actually going to Medicare down the line, you know, the private health insurer doesn’t see the benefit of that. And that’s where some of the tensions you get into it in terms of, like, how we cover these products and who we give them to.
Kenen: Because that trade-off: quality of life and longevity of life. That’s what health is about, right? I mean, is having people live healthy, good lives, and it costs money. But there’s this issue of the drug prices have gotten very high, and hepatitis C is a perfect example. I mean, now it’s like we were freaked out about $84,000 in, you know, 2013, 2015, whenever that came out. You know, now that looks quaint. But that price was still so high that we didn’t get it to people. We could have wiped out hepatitis C or come damn close to wiping out hepatitis C, but the price the drug was an obstacle. So we’re still, I mean, there’s a big White House initiative now, you know, there’s creative … the Louisiana model of, you know, what they call the Netflix model where, you know, you have a contract to buy a whole ton of it for less per unit. I mean, these are still questions. Yes. I mean, we all know that certain drugs make a big difference. But if they’re priced at a point where people who need them the most can’t get them, then you’re not seeing what they’re really invented for.
Sanger-Katz: Oh, I was just going to say, I think that part of what interests me about this particular class of drugs and the debates that we are likely to have about them, and there are, you know, the way that they’re going to be adopted into our health care system is that setting aside the diabetes indication for a moment, the idea of drugs that effectively treat obesity, I think obesity is a very stigmatized disease in our country. And in fact, Medicare has statutory language that says that Medicare cannot cover drugs for weight loss. So it would actually require an act of Congress for these drugs to be approved for that purpose in Medicare. And in Medicaid, in general, states are required to cover FDA-approved drugs. You know, they can put some limitations, but they’re supposed to cover them. Again, there is a special statutory exclusion for weight-loss drugs where the states really have discretion they don’t have for a cancer drug, for a drug for diabetes, a drug for other common diseases. And so I do think that, you know, a lot of this debate is colored by people’s prejudices against people who have obesity, and the way that our medical care system has thought about them and the treatment for their disease over time. And I’m curious about that aspect of it as well. I mean, of course, I think that Joanne is absolutely right that we do not know long term how these drugs are going to help people with obesity, whether it’s really going to reduce the burden of disease down the road for them, whether it’s going to have other health consequences in an enduring way. You know, I think there are unknowns, but I think if you take the most optimistic possible look at these drugs, that there’s quite a lot of evidence that they really do improve people’s health. And if we treat these drugs differently than we would an expensive drug for an infectious disease like hepatitis C or different from an expensive drug for cancer diseases that are less stigmatized, I think that would maybe be a little bit sad.
Karlin-Smith: I mean certainly the reason why the initial restrictions in Medicare and other programs are baked in goes back to stigma to some degree. But also, I mean … because they were thinking of these as weight-loss drugs and sort of vanity treatments people would only be using for vanity. And at that time, the drugs that were available did not work quite as well and had a lot of dangers and certainly did not show any of these other health benefits that we’re starting to see with this new class of medicine. So I think that would be the hope that, you know, as the science and the products shift, as well as our medical understanding around what causes obesity, what doesn’t cause obesity, how much of it is … right, again, just as medical as any other condition and not all about a person’s behavior. And I think we will see that the benefits of some of these drugs for certain people, in particular, are probably a lot bigger than maybe the benefits of certain cancer treatments that we pay a lot more money for. The challenge is going to be the amount of people and the amount of time they are going to be on these drugs, right? You know, if you’re talking about these hepatitis C drugs, I think one reason they didn’t shock the budgets in the way people were expecting, besides the fact that, unfortunately, we didn’t get them to everybody, is they’re actually really short-term cures, right? I think it’s like 10 weeks or something.
Kenen: Some are like eight.
Karlin-Smith: Right. Ballpark. And with the obesity drugs, what we know … these new drugs so far is that you seem like you have to consistently take them. Once you get off them, the weight comes back. And then the assumption would be you lose all those health benefits. So we’re talking about a high-cost drug on a chronic basis that our system can’t afford.
Kenen: Margot, do you know? I mean, my guess is that the ban on covering weight-loss drugs was written into MMA [the Medicare Modernization Act] in 2003. That’s my guess. I don’t know if anyone …
Sanger-Katz: That’s right. Yeah. It was part of the creation of the drug benefit program.
Kenen: So I think that you’re totally right that it’s what both of you said. You know, we tended to say it was someone’s fault, like they didn’t have enough willpower. Or they, you know, didn’t do what they were supposed to do. And there was stigma and we thought about it diffrently. I also think the science, you know, Sarah alluded to this, I think the science of obesity has really changed, that we didn’t talk about it — even though obesity experts — really didn’t talk about it as a disease a generation ago. We thought of it as maybe as a risk factor, but we didn’t think of it as a disease in and of itself. And we now do know that. So I think that the coverage issues are going to change. But what are the criteria? How fast do they change, for who do they change? Do you really want to put somebody on a drug because they want to lose 10 or 15 punds, which is … versus someone who really has struggled with weight and has physical risk factors because of it, including, you know, heart disease, diabetes, all these other things we know about. I mean, I just think we don’t know. I mean, there was a piece in the Times about the Upper East Side of Manhattan is like this beehive of people taking these weight loss drugs because they can afford it, but they’re also thinner than the rest of the population. So it becomes, you know, a luxury good or another disparity.
Sanger-Katz: If insurance won’t cover these drugs ,of course, rich people are going to take them more than people of limited means. Right? Like, I think you can only really test the hypothesis of, like, who are these drugs meant to reach once … if you have coverage for them, right? I thought that story was very good, and it did reveal something that’s happening. But I also thought … it felt like it was focusing on the idea that that rich people were taking these drugs just for vanity. And I think …
Kenen: Some of them, not all clearly some of them.
Sanger-Katz: Some of them are, of course. But I thought the thing that was less explored in that story is all of the people in poor neighborhoods of New York who were not accessing those drugs. Was it because they couldn’t find any way to get them?
Kenen: Right, and some of them were pre-diabetic. Some of them. I mean, the other thing is people who are overweight are often pre-diabetic. And that is an indication. I mean, you can … it’s in flux. It’s going to change over the coming months, you know, but what a cost and how those benefits paid off and who’s going to end up paying and where the cost shifting is going to come, because there is always cost shifting. We just don’t know yet. But these drugs are here to stay. And there are questions. There are a lot of questions. The mounting evidence is that they are going to be a benefit. It’s just, you know, what do we pay for them? Who gets them? How long do the people stay on them, etc., etc., etc.
Sanger-Katz: And just to come back to Emmarie’s first question, like, what is this going to mean for our insurance premiums, right? With something like 40% of adults in the United States have obesity. If we start to see more and more people taking these drugs to treat this disease, all of us are going to have to pay for that in some way. And, you know, that affects overall health care.
Huetteman: Absolutely. Well, let’s move to the week’s big covid news now. This week, the FDA approved a new booster, which comes amid an uptick in cases and concerns about a surge this fall and winter. Before the CDC made its recommendations, though, there was debate over whether the booster should be recommended only for a couple of higher-risk groups. So who does the CDC say should get the shot? And what’s the response been like from the health care community so far?
Karlin-Smith: So the CDC decided their advisers and the CDC themselves to recommend the shot for everybody. That really didn’t surprise me because I think that was the direction FDA wanted to go as well. I think the majority came down to the fact that a broad recommendation would be the best for health equity and actually ensuring the people we really want to get the shots get them. If you start siphoning off the population and so forth, it actually might prevent people that really should get the shots from getting it. I think the booster debate has actually been really similar since we started approving covid boosters, which is that the companies that provided for the boosters is not the same as the original data they presented to get the vaccines approved. So we don’t have as much understanding with the type of rigorous research some people would like to know: OK, what is the added benefit you’re getting from these boosters? We know they provide some added benefit of protection for infection, but that’s very short-lived. And then I think there’s … people have differences of opinions of how much added protection it’s giving you from severe disease and death. And so there are factions who argue, and I think Paul Offit has become one of the most known and vocal cheerleaders of this mindset, which is that, well, actually, if you’ve already had, you know, two, three, four shots, you’ve already had covid, you’re probably really well protected against the worst outcomes. And these shots are not really going to do that much to protect you from an infection. “So why take them anymore?” — essentially, is sort of his mindset. And there are people that disagree. I think the thing that probably might help change mindsets is, at least in this country, probably not going to happen, which is, you know, more rigorous outcomes research here. But I think the sentiment of the CDC and its advice has been, well, these shots are extremely low risk and there’s at least some added benefit. So for most people, the risk-benefit balance is: Get it. And if you make it kind of simple, if you say, OK, you know, everybody, it’s time to get your next covid booster, the feeling is that will get the most people in the U.S. to go out and do it. Unfortunately, most covid booster recommendations have been fairly broad — the last, at least, and that hasn’t translated. But we’ll see. This is actually the first time that everyone, except for babies under 6 months — because you can’t start your covid vaccination until then —everybody is really included in the booster recommendation at the same time. In previous rounds, particularly for younger kids, it was more staggered. So this will be the simplest recommendation we have yet.
Kenen: And that’s part of the public health strategy, is to not talk about it so much as boosters, just as an annual shot. The way you get an annual flu shot. I mean, most people don’t get them. But the idea is that to normalize this, you know, you get an annual flu shot, you get an annual covid shot, for certain age groups you get annual RSV now that’ll be available. But that’s not for everybody. I mean, I think they really want to make this simple. OK, it’s fall, get your covid shot. We don’t think uptake is going to be real high. It hasn’t been for boosters. But in terms of trying to change, this is just, you know, this is one of those things to add to your to-do list this year and to, sort of, less “pandemicize” it. I don’t think that’s a word. But, you know, everyone will forgive me. And more just, you know, OK, you know, this is one of the things you got to do in the fall. Maybe “pandemicize” is a word or maybe it should be.
Sanger-Katz: I like it. Maybe we should use it.
Huetteman: Pandemicize your care.
Kenen: Right. You know, it’s part of your preventive care and just … I mean, good luck trying to de-politicize it. But that’s part of it. I mean, the CDC director, Mandy Cohen, she wrote an op-ed this week and it was all about, you know, I’m a doctor, I’m the CDC director, and I’m a mom. And, you know, my family is going to get it. You know, Ashish Jha was tweeting about how he’s going to get it, his elderly parents are going to get theirs as soon as possible, etc., etc. So it’s not going to be … the hard-core people who really don’t want these shots and haven’t taken the shots and believe the shots cause more harm than good, etc. It won’t change a lot of their minds. But there are a lot of people who are uncertain in the middle and their minds can be changed. And they have … they were changed in the initial round of shots. So that’s who the messaging is … it’s sort of a reminder to people who take the shots and an invitation to those who … haven’t been getting boosted that just start doing this every year.
Karlin-Smith: And it is important to emphasize when the boosters have been tweaked and, you know, updated to try to match as close as they possibly can the current version of the virus. The virus has evolved and shifted a lot over time to the point where even these boosters, you know, they can’t quite keep up with the virus. But the idea is that we’re helping broaden everybody’s protection by keeping it as up to date with the science. So I think that’s an important element of that, that people don’t appreciate. They’re not just giving you the exact same shot over and over again. They’re trying to, like we do with the flu vaccine every year, be as close to what is circulating as possible.
Kenen: And there’s a new, new, new, new variant that looked very — do I have enough “news” in there? — that looked, and I don’t remember the initials; I can’t keep track — that is really quite different than the other ones. And there was a lot of initial concern that this vaccine would not work or that we wouldn’t … that our protection would not work against that. The follow-up research is much more reassuring that the fall shot will work against that. But that one really is different, and it’s got a lot of mutations. And, you know, we don’t know yet how … some of these things come and go pretty quickly. I mean, who remembers Mu? That one people were very worried about and it seemed quite dangerous and luckily it didn’t take root. You know, people don’t even know there was a Greek letter called Mu. M-u, not m-o-o, in case anyone’s wondering. If relatives ask me if they should take it, the two things that struck me in reading about it are, yes, it works against this new variant, and we’re not really sure what are the new, new, new, new, new, new, new, new ones. And also, I mean, there’s some research that it does protect against long covid. And I think that’s a big selling point for people. I think there are people who still, with reason, worry about long covid, and that vaccination does provide some protection against that as well.
Huetteman: That’s a great point. I mean, anecdotally, you talk to your friends who’ve had covid, there’s going to be at least a few of them who say they haven’t quite felt like themselves ever since they had covid. And I think that is one of the things that really motivates people who aren’t in those higher-risk categories, to think about whether they need the booster or not.
Kenen: Yeah, and also the myocarditis … Sarah, correct … you follow this more closely than I do, so correct me if I’m wrong here, but I believe that they’re finding that the myocarditis risk in the newer formulations of the vaccine has dropped, that it is not as much of a concern for young men. And covid itself can cause myocarditis in some individuals. Did I get that right?
Karlin-Smith: Yeah, I think that that’s right. The general sense has been that the risk was more with the initial shots, and it seems to have gone down. I think that there are people that still worry about particular age groups of, like, young men in certain age groups, that maybe for them the benefit-risk balance with the myocarditis risk is, you know, might be a little bit different. And that’s where a lot of the pushback comes through. But right, like you said, there is a fairly high … there’s myocarditis risk from covid itself that needs to be balanced.
Huetteman: Well, OK. That’s this week’s news. Now we’ll take a quick break and then we’ll come back with extra credits.
Julie Rovner: Hey, “What the Health?” listeners, you already know that few things in health care are ever simple. So, if you like our show, I recommend you also listen to “Tradeoffs,” a podcast that goes even deeper into our costly, complicated, and often counterintuitive health care system. Hosted by longtime health care journalist and friend Dan Gorenstein, “Tradeoffs” digs into the evidence and research data behind health care policies and tells the stories of real people impacted by decisions made in C-suites, doctors’ offices, and even Congress. Subscribe wherever you listen to your podcasts.
Huetteman: OK, we’re back. And it’s time for our extra-credit segment. That’s when we each recommend a story we read this week that we think you should read, too. As always, don’t worry if you miss it; we’ll post the links on the podcast page at kffhealthnews.org and in our show notes on your phone or other mobile device. Sarah, why don’t you go first?
Karlin-Smith: Sure. So I looked at a MedPage Today page by Kristina Fiore that talks about a GoFundMe campaign that was started by a small rural hospital in Pennsylvania. They’re trying to raise $1.5 million to basically keep the hospital open. It’s the only hospital in the county. It’s a small critical-access hospital. And I think people who follow health care and health policy in the U.S. are probably used to seeing GoFundMe campaigns for individual health care, as we talked about earlier in the episode, right? The unaffordability that can happen even for people with good insurance if you … depending on your medical situation. But this situation, I thought, was really unique, a whole hospital, which is, I guess, community-owned, and they’re essentially turning to the internet to try and stay open. And it touches on some of the payment differences in how rural hospitals make their money, or the payment rates they get reimbursed versus more urban hospitals. Other issues it brings up is just, you know, how do you keep an institution open that’s serving a relatively small population of people? So, you don’t necessarily want to have people going to the hospital, but they’re basically arguing that if we don’t get this amount of people in our ER per day, we can’t stay open. But then that means you don’t have an ER for anybody. And I think it’s just worth looking at, looking at the facts they put on their GoFundMe page, just thinking about, you know, what this says about various policies in the U.S. health system. And, unfortunately for them right now, they’re well short of their $1.5 billion goal.
Huetteman: Yeah, it’s amazing to see this get translated into an institution-saving effort as opposed to an individual-saving effort. Joanne, you want to go next?
Kenen: Sure. This is a story that it was by Bianca Fortis from ProPublica, Laura Biel, who wrote this for ProPublica and New York Magazine, and also Laura, who’s a friend of mine, also has a fabulous podcast called “Exposed.” And in this case, I want to mention the photographer, too, because if you click on this, it’s quite extraordinary visuals. Hannah Whitaker from New York Magazine. And the title is “How Columbia …” — and this is the university, not the country — “How Columbia Ignored Women, Undermined Prosecutors and Protected a Predator for More Than 20 Years.” This is an OB-GYN who was abusing his patients, and it’s hundreds, hundreds that have been identified and known. We knew about him because some of the patients had come forward, including Evelyn Wang, who was Andrew Wang — is Andrew Wang’s wife, the presidential candidate last cycle. But we didn’t know this. You know, first of all, it’s even bigger than we knew three years ago, and he has been prosecuted — finally. But it took 20 years. And this is really more of a story about how the medical system, the health care system, had warning after warning after warning after warning, and they didn’t do anything. And also, many of the people who tried to give the warnings, some of the employees, including the medical assistants, and the nurses, and the receptionists, knew what was going on. And they thought that they, as lower-level women going up against a white male doctor, wouldn’t be believed. And they didn’t even try. They just felt like he’s the guy, he’s the doctor. I’m the, you know, I’m the nurse. They won’t listen to me. So that was another subtheme that came out to me. I had known vaguely about this. It’s really long, and I read every word. It’s a really horrifying saga of an abdication of responsibility to women who were really harmed. Vulnerable women who were really harmed.
Huetteman: Yeah, it’s a really troubling story, but it’s an important piece of journalism. And I advise that people give it a little time. Margot, would you like to go next?
Sanger-Katz: Yeah. So this is a very nerdy, deep cut. I wanted to talk about a CBO [Congressional Budget Office] report from 2012 called “Raising the Excise Tax on Cigarettes: Effects on Health and the Federal Budget.” So when I published this article about how Medicare spending has sort of flattened out, we got so many reader comments and emails and tweets and several people asked, “Could it be that the decline in smoking has led to lower costs for Medicare?” And that caused me to do some reporting and to read this paper. And I think the finding, the sort of counterintuitive finding that I will tell you about in a minute, from the CBO really speaks to some of the discussion that we were having earlier about these obesity drugs, which is that there are many beneficial preventive therapies in health care that are great for people’s health. They make them healthier, they have happier lives, they live longer, they have less burden of disease, but they are not cost-effective in the sense that they reduce our total spending on health care. And the simplest way to think about this is that if everyone in America just died at age 65, Medicare’s budget would look amazing. You know, it would be great. We would save so much money if we could just kill everyone at age 65. But that’s not what the goal of Medicare is. It’s not to save the maximum amount of money. It’s to get a good value, to improve people’s life and health as much as possible for a good value. And so this report was looking at what would happen if we had a really effective policy to reduce smoking in the United States. They looked at a tax that they estimated would reduce the smoking rate by a further 5 percentage points. And what they found is that it would cost the government more money, that people would be healthier, they would live longer lives, more of them would spend more years in Medicare, and they would end up having some other health problem that was expensive that they weren’t going to have before. And also they would collect a lot of Social Security payments because they would live a lot longer. And so I found it so stunning because the economics of it, I think, make a lot of sense. And when you think about it, it’s true. But it does go to show how, I think, that sometimes when we, and when politicians, talk about preventive health care, they always talk about it like it’s a win-win. You know, this is going to be great for people and it’s going to save money. And I think that in health care, many times things that are good and beneficial improve health and they cost money and we have to decide if it’s worth it.
Huetteman: Absolutely. That’s great. Thank you. My extra credit this week comes from KFF Health News. Dr. Elisabeth Rosenthal, our senior contributing editor, writes: “The Shrinking Number of Primary Care Physicians Is Reaching a Tipping Point.” And we’ve seen some great coverage lately on the disappearance of the primary care doctor in this country. And Dr. Rosenthal also offers some solutions to this yawning gap in our health care system. She reports that the percent of U.S. doctors that have moved into primary care is now at about 25%, which is much lower than in previous decades. And one point she makes, in particular, about a problem that’s leading to this is the payment structure that we have in our country favors surgeries and procedures, of course, not diagnostic tests, preventative care, when it comes to reimbursing doctors. And of course, this lack of primary care doctors has implications for our overall health, both individually and as a country. So I recommend that you give that article a little bit of your time this week.
All right. That’s our show for this week. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left a review; that helps other people find us, too. Special thanks, as always, to our amazing engineer, Francis Ying. And as always, you can email us your comments or questions. We’re at whatthehealth@kff.org. Or you can tweet me. I’m @emmarieDC. Sarah?
Karlin-Smith: I’m @SarahKarlin.
Huetteman: Joanne?
Kenen: @JoanneKenen on Twitter, @joannekenen1 on Threads.
Huetteman: And Margot.
Sanger-Katz: @sangerkatz in all the places.
Huetteman: We’ll be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Terry Byrne
Copy chief
Gabe Brison-Trezise
Deputy copy chief
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
2 years 1 month ago
COVID-19, Health Care Costs, Insurance, Medicaid, Medicare, Multimedia, Public Health, Uninsured, FDA, KFF Health News' 'What The Health?', Podcasts, vaccines
Un padre soñaba con una casa para su familia. La deuda médica casi los deja en la calle
DENVER. — A Kayce Atencio solía atormentarlo un pensamiento mientras trabajaba en un refugio para personas sin hogar en el centro de Denver. “Podría haber sido yo”, dijo Atencio, de 30 años, quien vive con su hijo y su hija en un pequeño apartamento, no muy lejos del refugio.
Casi lo fue. Atencio y sus hijos durmieron durante años en los sofás de amigos o en casa de familiares, sin poder alquilar un apartamento debido a su mal historial de crédito. Una de las principales razones, dijo, fue la deuda médica.
Atencio sufrió un ataque al corazón a los 19 años, desencadenado por una afección congénita no diagnosticada. Las deudas por su atención devastaron su crédito. “Siempre sentí que no podía salir adelante”, dijo, recordando una vida de trabajos sin futuro y préstamos con intereses altos mientras trataba de mantenerse al día con los cobradores de deudas.
A los 25 años, tuvo que declararse en quiebra.
En todo el país, la deuda médica obliga a legiones de estadounidenses a hacer sacrificios dolorosos. Muchos recortan gastos en alimentos, asumen trabajos adicionales o agotan sus ahorros para la jubilación. Para millones como Atencio, el sistema de atención médica amenaza sus propios hogares.
Esto ha resultado ser especialmente devastador en comunidades como Denver, donde los precios de las viviendas se han disparado, volviéndose inaccesibles para muchos residentes, alimentando una crisis que ha dejado a miles de personas sin hogar y durmiendo en las calles.
En Community Economic Defense Project, o CEDP, una organización sin fines de lucro de Denver que ayuda a las personas que enfrentan el desalojo o la ejecución hipotecaria de sus hogares, aproximadamente dos tercios de los clientes tienen deuda médica, según una encuesta informal realizada por KFF Health News y la organización.
Cerca de la mitad de las casi 70 personas encuestadas dijeron que la deuda médica desempeñó un papel en su problema de vivienda, y aproximadamente una de cada 6 dijo que fue un factor importante.
“Todo el día escucho sobre la deuda médica”, dijo Kaylee Mazza, defensora de inquilinos que trabaja en una clínica legal de CEDP en el tribunal de Denver que ofrece ayuda a los inquilinos que enfrentan procesos de desalojo. “Está en todas partes”.
A nivel nacional, alrededor de 100 millones de personas tienen alguna forma de deuda de atención médica. De ellos, aproximadamente una de cada 5 dijo que las deudas los obligaron a cambiar su situación de vida, incluyendo mudarse con amigos o familiares, según una encuesta de KFF de 2022.
Un creciente cuerpo de investigaciones muestra que la vivienda estable es fundamental para el bienestar físico y mental. Algunos sistemas médicos importantes, incluyendo varios en Colorado, incluso han comenzado a invertir en viviendas asequibles en sus comunidades, citando la necesidad de abordar los llamados determinantes sociales de salud.
Pero a medida que los hospitales y otros proveedores médicos dejan a millones en deuda, socavan inadvertidamente la salud de la comunidad, dijo Brian Klausner, médico en una clínica que atiende a pacientes sin hogar en Raleigh, Carolina del Norte.
“Muchos de los hospitales en todo el país que ahora públicamente se comprometen a abordar las inequidades en salud y eliminar las barreras para la salud están contribuyendo simultáneamente a crear estos mismos problemas”, dijo Klausner. “A nadie le gusta el elefante en la habitación, pero la realidad es que hay miles de estadounidenses enfermos que probablemente están sin hogar, y enfermos, debido a la deuda médica”.
Efecto dominó
La deuda médica puede socavar la seguridad de la vivienda de varias maneras. Para algunos, debilita su crédito, lo que dificulta alquilar o solicitar una hipoteca. El año pasado, aproximadamente uno de cada 8 consumidores estadounidenses con un informe de crédito tenía una deuda médica en él, según el Urban Institute, una organización sin fines de lucro.
Los pacientes con condiciones médicas crónicas pueden atrasarse en el pago del alquiler o de las cuotas de su hogar mientras luchan por mantener bajo control las deudas médicas para preservar el acceso a la atención médica. KFF Health News encontró que muchos hospitales y otros proveedores rechazan a pacientes con cuentas pendientes.
Denise Beasley, quien también ayuda a clientes en CEDP en Denver, dijo que muchas personas mayores, que normalmente dependen más de los médicos y los medicamentos, creen que deben pagar sus cuentas médicas y de farmacia antes que cualquier otra cosa. “Están aterrados”, dijo.
Para otros, esta deuda puede aumentar las dificultades financieras provocadas por un accidente o una enfermedad inesperada que los obliga a dejar de trabajar, poniendo en peligro su cobertura de salud o su capacidad para pagar la vivienda.
En Seattle, los investigadores encontraron una deuda médica generalizada entre los residentes de campamentos de personas sin hogar. Y aquellos con este tipo de deudas tendían a experimentar la falta de vivienda durante dos años más que los residentes de campamentos sin deuda.
En términos más generales, las personas con deuda médica tienen más probabilidades de decir que la deuda les ha impedido rentar o avanzar con una hipoteca, en comparación con las personas que tienen préstamos estudiantiles o de tarjetas de crédito, según una encuesta nacional de 2019 realizada por la empresa de bienes raíces Zillow entre inquilinos, compradores de viviendas y dueños de propiedades.
Para Atencio, quien dejó su hogar a los 16 años, sus problemas con la deuda médica comenzaron con el ataque al corazón. Estaba trabajando en una gasolinera y viviendo en Trinidad, una pequeña ciudad en el sur de Colorado cerca de la frontera con Nuevo México.
Fue llevado de urgencia a un hospital local, donde fue sometido a una cirugía. Las facturas, que superaban los $50,000, no estaban cubiertas por su plan de salud porque había acudido a un proveedor fuera de la red sin saberlo, contó. “Luché lo más que pude, pero no podía pagar un abogado. Estaba atrapado”.
Atencio, quien es transgénero, tiene el pelo oscuro corto y un gran tatuaje en su antebrazo derecho en memoria de dos amigos que murieron en un accidente automovilístico. Sentado en un sofá viejo en un apartamento con rejas en las ventanas, es filosófico acerca de su largo periplo desde esa crisis médica a través de años de deuda e inseguridad de vivienda. “Hemos salido adelante”, dijo. “Pero tuvo un costo”.
Cuando su crédito bajó a cerca de 300, la calificación más baja, había pocos lugares a los que recurrir en busca de ayuda. La relación de Atencio con sus padres, quienes se divorciaron cuando él tenía 2 años, había sido tensa durante años. Atencio se casó a los 18, pero él y su esposo rara vez tenían suficiente para llegar a fin de mes. “Recuerdo pensar, ‘¿Qué tipo de comienzo de mi vida adulta es este?'”.
Finalmente, fueron acogidos por la madre de su esposo. “Si no fuera por ella, habríamos estado sin hogar”, dijo. Pero salir de la deuda fue agonizante.
“Terminas en este ciclo”, dijo. “Te endeudas. Luego tomas préstamos para tratar de pagar parte de la deuda. Pero luego está todo ese interés”. Con un mal historial de crédito, Atencio en ocasiones dependía de prestamistas a los que hay que devolver el dinero pronto, cuyas altas tasas de interés pueden aumentar drásticamente lo que deben los prestatarios.
Además, muchos empleadores también verifican los puntajes de crédito, lo que dificultaba que Atencio encontrara algo más que trabajos mal remunerados.
El trabajo en el refugio fue un paso adelante, y este año Atencio obtuvo el apartamento, que está reservado para familias monoparentales en riesgo de quedarse sin hogar. (Atencio se separó de su esposo el año pasado).
Desafíos de vivienda en Colorado
Las luchas de vivienda de Atencio están lejos de ser únicas. Jim y Cindy Powers, quienes viven en Greeley, una pequeña ciudad al norte de Denver, vieron colapsar sus propios sueños de vivienda después de que a Cindy se le diagnosticara una afección potencialmente mortal que requirió múltiples cirugías y dejó a la pareja con más de $250,000 en deuda médica.
Cuando los Powers se declararon en quiebra, el acuerdo protegió su hogar. Pero su hipoteca fue vendida y el nuevo prestamista rechazó el plan de pago. Perdieron la casa.
Lindsey Vance, de 40 años, quien se mudó a Denver hace cinco años en busca de viviendas más asequibles que en el área de Washington, DC, de donde es originaria, aún no puede comprar una casa debido a deudas médicas. Ella y su esposo tienen un ingreso de seis cifras, pero las facturas médicas por incluso atención de rutina que ha luchado por pagar desde sus 20 años han afectado su crédito, dificultando la obtención de un préstamo. “Estamos atrapados en un punto muerto”, dijo.
En Denver y sus alrededores, funcionarios electos, líderes empresariales y otros se han mostrado cada vez más preocupados por la deuda médica mientras buscan formas de abordar lo que muchos ven como una crisis de vivienda.
“Son cosas profundamente conectadas”, dijo Sarah Parady, miembro del Concejo Municipal de Denver. “A medida que los precios de la vivienda han subido y subido, he visto a más y más personas, especialmente personas con problemas médicos y deudas, perder la seguridad en la vivienda”.
Parady, quien se postuló para el cargo el año pasado para abordar la asequibilidad de la vivienda, está liderando un esfuerzo para que la ciudad compre y cancele la deuda médica de los residentes de la ciudad.
Impulsado por los precios disparados y las tasas de interés en aumento, el costo de comprar una vivienda en Denver se más que duplicó desde 2015 hasta 2022, según un análisis reciente. Y con los alquileres también aumentando, los desalojos están en alza luego del paréntesis de los dos primeros años de la pandemia.
Tal vez en ningún lugar la crisis de Denver es más visible que en las calles. El centro de la ciudad está lleno de tiendas de campaña y campamentos, incluido uno que se extiende por varias cuadras cerca del refugio y la clínica donde Atencio solía trabajar. Según un conteo, la población sin hogar del área metropolitana de Denver aumentó casi un 50% desde 2020 hasta 2023.
CEDP, que fue fundado para ayudar a los residentes con desafíos de vivienda desencadenados por la pandemia, se unió este año a otros defensores de consumidores y pacientes de Colorado para presionar a la legislatura en busca de protecciones más sólidas para los pacientes con deuda médica.
Y en junio, Colorado promulgó una ley pionera que prohíbe que la deuda médica se incluya en los informes de crédito de los residentes o se tenga en cuenta en sus puntajes crediticios, una medida que colocó al estado a la vanguardia de los esfuerzos a nivel nacional para ampliar las protecciones contra las deuda para los pacientes.
Algunos otros estados están considerando medidas similares. Y en Washington, DC, defensores de consumidores y pacientes están presionando para que se tomen medidas federales para limitar las facturas médicas en los informes de crédito. En la mayoría de los estados, incluyendo muchos con las tasas más altas de deuda médica, los pacientes aún no tienen tales protecciones.
Por su parte, Atencio espera que el nuevo apartamento marque un punto de inflexión.
El hogar es modesto, una pequeña unidad en una vieja torre de concreto. Hay un guardia de seguridad en la puerta principal y pasillos largos pintados de azul y marrón institucional.
La familia de Atencio se está instalando, junto con cuatro ratas mascotas: Stitch, Cheese, Peach y Bubbles, que viven en una jaula grande en la sala de estar. “Esto se siente como libertad”, dijo Atencio.
Ha tratado de darles a sus hijos, de 5 y 11 años, una sensación de seguridad: comidas caseras y espacio para jugar o pasar el rato en sus propios dormitorios. Como todos los padres, se preocupa por el tiempo que pasan frente a las pantallas y frunce el ceño cuando critican lo que hay para cenar. (No les gustaron las papas que puso en un asado al horno).
Todos son estudiantes a tiempo completo: Atencio, que dejó su trabajo en el refugio, está cursando una maestría en trabajo social. Su hijo acaba de empezar el jardín de infantes y su hija está en la escuela media. “Tengo grandes planes y grandes objetivos”, dijo.
Y con varios miles de dólares de deuda médica aún por pagar, agregó que tiene cuidado de no llevar a sus hijos a un hospital o médico fuera de la red. “No cometeré ese error de nuevo”, dijo.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
2 years 1 month ago
Health Care Costs, Noticias En Español, States, Colorado, Cost of Living, Diagnosis: Debt, Homeless, Investigation
A Father Dreamed of a Home for His Family. Medical Debt Nearly Pushed Them Onto the Streets.
DENVER — Kayce Atencio used to be haunted by a thought while working at a homeless shelter in downtown Denver. “It could have been me,” said Atencio, 30, who lives in a small apartment with his son and daughter not far from the shelter.
It nearly was. Atencio and his children for years slept on friends’ couches or stayed with family, unable to rent an apartment because of poor credit. A big reason, he said, was medical debt.
Atencio had a heart attack at 19, triggered by an undiagnosed congenital condition. The debts from his care devastated his credit score. “It always felt like I just couldn’t get a leg up,” he said, recalling a life of dead-end jobs and high-interest loans as he tried to stay ahead of debt collectors. By 25, he’d declared bankruptcy.
Across the country, medical debt forces legions of Americans to make painful sacrifices. Many cut back on food, take on extra work, or drain retirement savings. For millions like Atencio, the health care system is threatening their very homes.
That’s proven particularly devastating in communities like Denver, where skyrocketing prices have put housing out of reach for many residents and fueled a crisis that’s left thousands homeless and sleeping on the streets.
At the Community Economic Defense Project, or CEDP, a Denver nonprofit that helps people facing eviction or home foreclosure, about two-thirds of clients have medical debt, an informal survey by KFF Health News and the organization suggests. Close to half of the nearly 70 people surveyed said medical debt played a role in their housing issue, with about 1 in 6 saying it was a major factor.
“All day long I hear about medical debt,” said Kaylee Mazza, a tenant advocate who staffs a CEDP legal clinic at the Denver courthouse that offers aid to tenants going through eviction proceedings. “It’s everywhere.”
Nationwide, about 100 million people have some form of health care debt. Of those, about 1 in 5 said the debts have forced them to change their living situation, including moving in with friends or family, according to a 2022 KFF poll.
A growing body of evidence shows that stable housing is critical to physical and mental well-being. Some major medical systems — including several in Colorado — have even begun investing in affordable housing in their communities, citing the need to address what are sometimes called social determinants of health.
But as hospitals and other medical providers leave millions in debt, they inadvertently undermine community health, said Brian Klausner, a physician at a clinic serving homeless patients in Raleigh, North Carolina.
“Many of the hospitals across the country that are now publicly vowing to address health inequities and break down barriers to health are simultaneously helping to create these very problems,” Klausner said. “Nobody likes the elephant in the room, but the reality is that there are thousands of sick Americans who are likely homeless — and sick — because of medical debt.”
A Downward Spiral
Medical debt can undermine housing security in several ways. For some, it depresses credit scores, making it difficult to get a lease or a mortgage. Last year, about 1 in 8 U.S. consumers with a credit report had a medical debt listed on it, according to the nonprofit Urban Institute.
Patients with chronic medical conditions may fall behind on rent or home payments as they scramble to keep medical debts in check to preserve access to health care. Many hospitals and other providers will turn away patients with outstanding bills, KFF Health News found.
Denise Beasley, who also assists clients at CEDP in Denver, said many older people, who typically depend most on physicians and medications, believe they must pay their medical and pharmacy bills before anything else. “The elderly are terrified,” she said.
For others, such debt can compound financial struggles brought on by an accident or unexpected illness that forces them to stop working, jeopardizing their health coverage or ability to pay for housing.
In Seattle, researchers found widespread medical debt among residents in homeless encampments. And those with such debt tended to experience homelessness two years longer than encampment residents without it.
More broadly, people with medical debt are more likely to say the debt has caused them to be turned down for a rental or a mortgage than people with student loans or credit card debt, according to a 2019 nationwide survey of renters, homebuyers, and property owners by real estate company Zillow.
For Atencio, who left home at 16, his struggles with medical debt began with the heart attack. He was working at a gas station and living in Trinidad, a small city in southern Colorado near the New Mexico border.
Rushed to a local hospital, he underwent surgery. The bills, which topped $50,000, weren’t covered by his health plan because he’d unknowingly gone to an out-of-network provider, he said. “I fought it as hard as I could, but I couldn’t afford a lawyer. I was stuck.”
Atencio, who is transgender, has close-cropped dark hair and a large tattoo on his right forearm memorializing two friends who died in a car accident. Sitting on an aging couch in an apartment with bars on the windows, he’s philosophical about his long journey from that medical crisis through years of debt and housing insecurity. “We’ve pulled ourselves out of this,” he said. “But it took a toll.”
When Atencio’s credit score dipped close to 300, the lowest rating, there were few places to turn for help. Atencio’s relationship with his parents, who divorced when he was 2, had been strained for years. Atencio got married at 18, but he and his husband rarely had enough to make ends meet. “I remember thinking, ‘What kind of a start to my adult life is this?’”
They were ultimately taken in by Atencio’s mother-in-law. “If it wasn’t for her, we would have been homeless,” he said. But getting out from the debt was agonizing.
“You end up in this cycle,” he said. “You get into debt. Then you take out loans to try to pay off some of the debt. But then there’s all this interest.” With poor credit, Atencio relied at times on payday lenders, whose high interest rates can dramatically increase what borrowers owe. Many employers also check credit scores, which made it difficult for Atencio to land anything but low-wage jobs.
The job at the shelter was a step up, and Atencio this year got the apartment, which is reserved for single-parent families at risk of being homeless. (Atencio separated from his husband last year.)
Colorado’s Housing Challenges
Atencio’s housing struggles are hardly unique. Jim and Cindy Powers, who live in Greeley, a small city north of Denver, saw their own housing dreams collapse after Cindy was diagnosed with a life-threatening condition that required multiple surgeries and left the couple with more than $250,000 in medical debt.
When the Powers declared bankruptcy, the settlement protected their home. But their mortgage was sold, and the new lender rejected the payment plan. They lost the house.
Lindsey Vance, 40, who moved to Denver five years ago seeking more affordable housing than the Washington, D.C., area where she was from, still can’t buy a house because of medical debts. She and her husband have a six-figure income, but medical bills for even routine care that she’s struggled to pay since her 20s have depressed her credit score, making it difficult to get a loan. “We’re stuck in a holding pattern,” she said.
In and around Denver, elected officials, business leaders, and others have become increasingly concerned about medical debt as they look for ways to tackle what many see as a housing crisis.
“These things are deeply connected,” Denver City Council member Sarah Parady said. “As housing prices have gone up and up, I’ve seen more and more people, especially people with a medical issues and debts, lose housing security.” Parady, who ran for office last year to address housing affordability, is helping lead an effort to get the city to buy and retire medical debt for city residents.
Fueled by skyrocketing prices and rising interest rates, the cost of buying a home more than doubled in Denver from 2015 to 2022, according to one recent analysis. And with rents also surging, evictions are rocketing upward after slowing during the first two years of the pandemic.
Perhaps nowhere is Denver’s crisis more visible than on the streets. The city’s downtown is dotted with tents and encampments, including one that stretches over several blocks near the shelter and clinic where Atencio used to work. By one count, metro Denver’s homeless population increased nearly 50% from 2020 to 2023.
CEDP, which was founded to help residents with housing challenges sparked by the pandemic, this year joined other Colorado consumer and patient advocates to push the legislature for stronger protections for patients with medical debt.
And in June, Colorado enacted a trailblazing bill that prohibits medical debt from being included on residents’ credit reports or factored into their credit scores, a move that put the state at the forefront of efforts nationally to expand debt protections for patients.
A few other states are considering similar steps. And in Washington, D.C., consumer and patient advocates are pushing for federal action to limit medical bills on credit reports. In most states — including many with the highest rates of medical debt — patients still have no such protections.
For his part, Atencio is hoping the new apartment marks a turning point.
The home is modest — a small unit in an aging concrete tower. There’s a security guard by the front door and long, linoleum corridors painted institutional blue and brown.
Atencio’s family is settling in, along with four pet rats — Stitch, Cheese, Peach, and Bubbles — who live in a large cage in the living room. “This feels like freedom,” said Atencio.
He’s tried to give his children, who are 5 and 11, a sense of security: home-cooked meals and the space to play or hang out in their own bedrooms. Like parents everywhere, he frets over their screen time and rolls his eyes when they critique what’s for dinner. (They didn’t like the potatoes he put in a pot roast.)
They are all full-time students: Atencio, who left his job at the shelter, is working on a master’s in social work. His son just started kindergarten, and his daughter is in middle school. “I have big plans and big goals,” he said.
And with several thousand dollars of medical debt still to pay off, Atencio said he’s careful not to take his kids to an out-of-network hospital or physician. “I won’t make that mistake again,” he said.
About This Project
“Diagnosis: Debt” is a reporting partnership between KFF Health News and NPR exploring the scale, impact, and causes of medical debt in America.
The series draws on original polling by KFF, court records, federal data on hospital finances, contracts obtained through public records requests, data on international health systems, and a yearlong investigation into the financial assistance and collection policies of more than 500 hospitals across the country.
Additional research was conducted by the Urban Institute, which analyzed credit bureau and other demographic data on poverty, race, and health status for KFF Health News to explore where medical debt is concentrated in the U.S. and what factors are associated with high debt levels.
The JPMorgan Chase Institute analyzed records from a sampling of Chase credit card holders to look at how customers’ balances may be affected by major medical expenses. And the CED Project, a Denver nonprofit, worked with KFF Health News on a survey of its clients to explore links between medical debt and housing instability.
KFF Health News journalists worked with KFF public opinion researchers to design and analyze the “KFF Health Care Debt Survey.” The survey was conducted Feb. 25 through March 20, 2022, online and via telephone, in English and Spanish, among a nationally representative sample of 2,375 U.S. adults, including 1,292 adults with current health care debt and 382 adults who had health care debt in the past five years. The margin of sampling error is plus or minus 3 percentage points for the full sample and 3 percentage points for those with current debt. For results based on subgroups, the margin of sampling error may be higher.
Reporters from KFF Health News and NPR also conducted hundreds of interviews with patients across the country; spoke with physicians, health industry leaders, consumer advocates, debt lawyers, and researchers; and reviewed scores of studies and surveys about medical debt.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
2 years 1 month ago
Health Care Costs, States, Colorado, Cost of Living, Diagnosis: Debt, Homeless, Investigation
A Peek at Big Pharma’s Playbook That Leaves Many Americans Unable to Afford Their Drugs
America’s pharmaceutical giants are suing this summer to block the federal government’s first effort at drug price regulation.
America’s pharmaceutical giants are suing this summer to block the federal government’s first effort at drug price regulation.
Last year’s Inflation Reduction Act included what on its face seems a modest proposal: The federal government would for the first time be empowered to negotiate prices Medicare pays for drugs — but only for 10 very expensive medicines beginning in 2026 (an additional 15 in 2027 and 2028, with more added in later years). Another provision would require manufacturers to pay rebates to Medicare for drug prices that increased faster than inflation.
Those provisions alone could reduce the federal deficit by $237 billion over 10 years, the Congressional Budget Office has calculated. That enormous savings would come from tamping down drug prices, which are costing an average of 3.44 times — sometimes 10 times — what the same brand-name drugs cost in other developed countries, where governments already negotiate prices.
These small steps were an attempt to rein in the only significant type of Medicare health spending — the cost of prescription drugs — that has not been controlled or limited by the government. But they were a call to arms for the pharmaceutical industry in a battle it assumed it had won: When Congress passed the Medicare prescription drug coverage benefit (Part D) in 2003, intense industry lobbying resulted in a last-minute insertion prohibiting Medicare from negotiating those prices.
Without any guardrails, prices for some existing drugs have soared, even as they have fallen sharply in other countries. New drugs — some with minimal benefit — have enormous price tags, buttressed by lobbying and marketing.
AZT, the first drug to successfully treat HIV/AIDS, was labeled “the most expensive drug in history” in the late 1980s. Its $8,000-a-year cost was derided as “inhuman” in a New York Times op-ed. Now, scores of drugs, many with much less benefit, cost more than $50,000 a year. Ten drugs, mostly used to treat rare diseases, cost over $700,000 annually.
Pharmaceutical manufacturers say high U.S. prices support research and development and point out that Americans tend to get new treatments first. But recent research has shown that the price of a drug is related neither to the amount of research and development required to bring it to market nor its therapeutic value.
And selling drugs first in the U.S. is a good business strategy. By introducing a drug in a developed country with limited scrutiny on price, manufacturers can set the bar high for negotiating with other nations.
Here are just a few of the many examples of drug pricing practices that have driven consumers to demand change.
Exhibit A is Humira, the best-selling drug in history, earning AbbVie $200 billion over two decades. Effective in the treatment of various autoimmune diseases, its core patent — the one on the biologic itself — expired in 2016. But for business purposes, the “controlling patent,” the last to expire, is far more important since it allows an ongoing monopoly.
AbbVie blanketed Humira with 165 peripheral patents, covering things like a manufacturing step or slightly new formulation, creating a so-called patent thicket, making it challenging for generics makers to make lower-cost copycats. (When they threatened to do so, AbbVie often offered them valuable deals not to enter the market.) Meanwhile, it continued to raise the price of the drug, most recently to $88,000 a year. This year, Humira-like generics (called biosimilars for its type of molecule) are entering the U.S. market; they have been available for a fraction of the price in Europe for five years.
Or take Revlimid, a drug by Celgene (now part of Bristol Myers Squibb), which treats multiple myeloma. It won FDA approval to treat that previously deadly disease in 2006 at about $4,500 a month; today it retails at triple that. Why? The company’s CEO explained price hikes were simply a “legitimate opportunity” to improve financial “performance.”
Since it must be taken for life to keep that cancer in check, patients who want to live (or their insurers) have had no choice but to pay. Though Revlimid’s patent protection ran out in 2022, Celgene avoided meaningful price-cutting competition by offering generic competitors “volume-limited licenses” to its patents so long as they agreed to initially produce a small share of the drug’s $12 billion monopoly market.
Par Pharmaceutical, another drugmaker, maneuvered to create a blockbuster market out of a centuries-old drug, isoproterenol, through a well-meaning FDA program that gave companies a three-year monopoly in exchange for performing formal testing on drugs in use before the agency was formed.
During those three years, Par wrapped its branded product, Vasostrict, used to maintain blood pressure in critically ill patients, with patents — including one on the compound’s pH level — extending its monopoly eight additional years. Par raised the price by 5,400% between 2010 and 2020. When the covid-19 pandemic filled intensive care units with severely ill patients, that hike cost Americans $600 million to $900 million in the first year.
And then there is AZT and its successors, which offer a full life to HIV-positive people. Pills today contain a combination of two or three medicines, the vast majority including one similar to AZT, tenofovir, made by Gilead Sciences. The individual medicines are old, off-patent. Why then do these combination pills, taken for life, sometimes cost $4,000 monthly?
It’s partly because many manufacturers of the combination pills have agreements with Gilead that they will use its expensive branded version of tenofovir in exchange for various business favors. Peter Staley, an activist with HIV, has been spearheading a class-action suit against Gilead, alleging “collusion.” The negotiated price for these pills is hundreds of dollars a month in the United Kingdom, not the thousands charged in the U.S.
Faced with such tactics, 8 in 10 Americans now support drug price negotiation, giving Congress and the Biden administration the impetus to act and to resist Big Pharma’s legal challenges, which many legal experts view as a desperate attempt to stave off the inevitable.
“I don’t think they have a good legal case,” said Aaron Kesselheim, who studies drug pricing at Harvard Medical School. “But it can delay things if they can find a judge to issue an injunction.” And even a year’s delay could translate into big money.
Yes, American patients are lucky to have first access to innovative drugs. And, sadly, patients in countries that refuse to pay up once in a while go without the latest treatment. But more sadly, polling shows, large numbers of Americans are forgoing prescribed medicines because they can’t afford them.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
2 years 2 months ago
Health Care Costs, Health Care Reform, Health Industry, Pharmaceuticals, Drug Costs, Legislation, Prescription Drugs
Your Exorbitant Medical Bill, Brought to You by the Latest Hospital Merger
When Mark Finney moved to southwestern Virginia with his young family a decade ago, there were different hospital systems and a range of independent doctors to choose from.
But when his knee started aching in late 2020, he discovered that Ballad Health was the only game in town: He went to his longtime primary care doctor, now employed by Ballad, who sent him to an orthopedist’s office owned by Ballad. That doctor sent him to get an X-ray at a Ballad-owned facility and then he was referred to a physical therapy center called Mountain States Rehab, which was now owned by Ballad as well.
When the price of his physical therapy doubled overnight — to nearly $200 for approximately 30 minutes — there was nowhere else to go, because Ballad Health effectively had a monopoly on care in 29 counties of the Appalachian Highlands in northeastern Tennessee, southwestern Virginia, northwestern North Carolina, and southeastern Kentucky.
“I was stuck,” said Finney, a college professor. “My wife now drives 50 miles to see a doctor that’s not part of Ballad, and I don’t have a doctor anymore.”
Biden administration regulators have unleashed a blizzard of antitrust activity and have broadened the definition of the types of unfair competition they can target. Regulators blocked a merger between publishing giants Penguin Random House and Simon & Schuster, saying it could have decreased author compensation and diminished the “diversity of our stories and ideas.” Regulators have filed suit to block JetBlue’s acquisition of Spirit Airlines on the grounds that the existence of the lower-cost Spirit kept fare increases by other carriers in check.
But while hospital mergers and creeping consolidation have arguably proved more traumatic and costly for countless Americans like Finney, they may prove harder to curtail.
After decades of unchecked mergers, health care is the land of giants, with one or two huge medical systems monopolizing care top to bottom in many cities, states, and even whole regions of the country. Reams of economic research show that the level of hospital consolidation today — 75% of markets are now considered highly consolidated — decreases patient choice, impedes innovation, erodes quality, and raises prices.
Ballad has generously contributed to performing arts and athletic centers as well as school bands. But, critics say, it has skimped on health care — closing intensive care units and reducing the number of nurses per ward — and demanded higher prices from insurers and patients. It has a habit of suing patients for unpaid bills. Its chief executive was paid about $4 million last year.
For many years in the past century the Federal Trade Commission made little effort to go to court to block hospital mergers because judges tended to rule that as nonprofit entities, hospitals were unlikely to use monopoly power to pursue abusive business practices. How wrong they were.
In 2021 President Joe Biden ordered the FTC to be more aggressive about hospital mergers and even to review those that had already occurred. But it is unclear if the agency has the tools to do much. “Regulators are 10 to 15 years behind and don’t have the resources — so that’s where we are,” said James Capretta, a senior fellow at the American Enterprise Institute.
The normal procedure for blocking proposed hospital mergers is cumbersome: often lengthy analysis to prove the effects on a particular market, warning letters, negotiations, and finally challenges in court.
With its staff of about 40 focused on hospitals, the FTC has prevented seven mergers in the past two years, said Rahul Rao, deputy director of the agency’s Bureau of Competition, who called the problem a “top priority.” But there were 53 hospital mergers and acquisitions in 2022 and have been more than 90 per year in recent years.
“It’s really hard to show that a prospective transaction is anti-competitive,” said Leemore Dafny, a Harvard economist who worked at the FTC about a decade ago. “I saw how hard it was for government to prove its case, even when it seemed obvious.”
In one market, two hospitals might be enough to ensure competition; in another, four. Even if the price goes up, that may not be considered anti-competitive if quality improves.
The FTC has an even harder time evaluating the vertical merger, which is far more common: when a big hospital system buys up a much smaller hospital or some doctors’ practices and independent surgery or radiology centers — or when it merges with a local insurer.
Many such mergers are never vetted at all, since transactions under $111 million do not have to be reported to the agency. “It’s a visibility problem,” Rao said. “We hear about it from news reports or from a state attorney general” who is more in touch with activity on the ground. Many of today’s behemoth systems — such as Northwell Health in New York, Sutter in California, and the University of Pittsburgh Medical Center in Pennsylvania — grew often by buying one small hospital, physician practice, or surgery center at a time, below the threshold where they would attract federal regulators’ scrutiny or merit use of their limited resources.
When hospitals buy doctors’ practices, research shows, rates for visits tend to go up as they did for Finney. Some purchases are essentially catch-and-kill operations: Buy a nearby independent outpatient cardiac center, for example, to eliminate cheaper competition.
As hospital systems have grown — and become major employers — their sway with state legislatures has created obstacles to curbing consolidation. Sympathetic state lawmakers have passed so-called Certificate of Public Advantage laws to shield hospitals from both federal and state antitrust action. Such certificates in Tennessee and Virginia allowed the formation of Ballad from two competing systems in 2018, over the FTC’s objections. The North Carolina Senate recently gave the UNC Health system the green light to expand, regardless of regulators’ thoughts.
The newest challenge is how to handle the growing number of cross-market mergers, where huge health systems in different parts of a state or of the country join forces. While the hospitals are not competing for the same patients, emerging research shows that these moves result in higher prices, in part because the increased negotiating clout of the enormous health system forces companies that cover employees in both markets to pay more in what previously was the cheaper region.
There are attempts and proposals to reinject a modicum of competition or restraint into the health system: The FTC has sought to ban noncompete clauses in job contracts that prevent doctors and nurses from moving from one hospital to another within a certain time, for example.
But many economists on both the left and the right have concluded that, at this point, meaningful competition may be difficult to restore in many markets. Barak Richman, a professor of law and business administration at Duke University, said, “It’s depressing for economists who live and breathe by competition to say maybe we just need price regulation.”
Indeed, a number of states — red and blue — are now gingerly floating moves to directly rein in prices. This year the Indiana Legislature, for example, banned hospitals from charging facility fees for visits outside of the hospital. The lawmakers even considered fining hospitals whose prices were more than 260% of the Medicare rate — though they deferred that move for two years in the hope that the threat would encourage better behavior.
With the FTC becoming more aggressive and legislatures considering such measures, perhaps hospital systems will heed the warnings and behave more like the care providers they’re meant to be and less like monopoly businesses.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
2 years 2 months ago
Cost and Quality, Health Care Costs, Health Industry, Hospitals, Legislation
The Real Costs of the New Alzheimer’s Drug, Most of Which Will Fall to Taxpayers
The first drug purporting to slow the advance of Alzheimer’s disease is likely to cost the U.S. health care system billions annually even as it remains out of reach for many of the lower-income seniors most likely to suffer from dementia.
Medicare and Medicaid patients will make up 92% of the market for lecanemab, according to Eisai Co., which sells the drug under the brand name Leqembi. In addition to the company’s $26,500 annual price tag for the drug, treatment could cost U.S. taxpayers $82,500 per patient per year, on average, for genetic tests and frequent brain scans, safety monitoring, and other care, according to estimates from the Institute for Clinical and Economic Review, or ICER. The FDA gave the drug full approval July 6. About 1 million Alzheimer’s patients in the U.S. could qualify to use it.
Patients with early Alzheimer’s disease who took lecanemab in a major clinical trial declined an average of five months slower than other subjects over an 18-month period, but many suffered brain swelling and bleeding. Although those side effects usually resolved without obvious harm, they apparently caused three deaths. The great expense of the drug and its treatment raises questions about how it will be paid for, and who will benefit.
“In the history of science, it’s a significant achievement to slightly slow down progression of dementia,” said John Mafi, a researcher and associate professor of medicine at the David Geffen School of Medicine at UCLA. “But the actual practical benefits to patients are very marginal, and there is a real risk and a real cost.”
To qualify for Leqembi, patients must undergo a PET scan that looks for amyloid plaques, the protein clumps that clog the brains of many Alzheimer’s patients. About 1 in 5 patients who took Leqembi in the major clinical test of the drug developed brain hemorrhaging or swelling, a risk that requires those taking the drug to undergo frequent medical checkups and brain scans called MRIs.
In anticipation of additional costs from the Leqembi drug class, the Centers for Medicare & Medicaid Services in 2021 increased monthly premiums for Medicare patients by 15%, and premiums may rise again in 2024 after a slight decline this year.
Such increases can be a significant burden for many of the 62 million Medicare subscribers who live on fixed incomes. “Real people will be affected,” Mafi said. He contributed to a study that estimated lecanemab and related care would cost Medicare $2 billion to $5 billion a year, making it one of the most expensive taxpayer-funded treatments.
In its analysis, ICER suggested that Leqembi could be cost-effective at an annual price of $8,900 to $21,500. In an interview, David Rind, ICER’s chief medical officer, said $10,000 to $15,000 a year would be reasonable. “Above that range doesn’t seem like a good place,” he said.
Whatever its price, patients may be delayed getting access to Leqembi because of the relative shortage of specialists capable of managing the drug, which will require genetic and neuropsychological testing as well as the PET scan to confirm a patient’s eligibility. A similar drug, Eli Lilly’s donanemab, is likely to win FDA approval this year.
Already there are long waits for the testing needed to assess dementia, Mafi said, noting that one of his patients with mild cognitive impairment had to wait eight months for an evaluation.
Such testing is not readily at hand because of the paucity of effective treatment for Alzheimer’s, which has helped to make geriatrics a relatively unappealing specialty. The United States has about a third as many dementia specialists per capita as Germany, and about half as many as Italy.
“Time is of the essence” for the neuropsychological testing, Mafi said, because once a patient’s cognitive ability declines below a certain threshold, they become ineligible for treatment with the drug, which was tested only in patients in the earliest stages of the disease.
Mafi’s study estimates that patients without supplemental Medicare coverage will have to pay about $6,600 out-of-pocket for each year of treatment. That could put it out of reach for many of the 1 in 7 “dual eligible” Medicare beneficiaries whose income is low enough to simultaneously qualify them for state Medicaid programs. Those programs are responsible for about 20% of physician bills for drug infusions, but they don’t always cover the full amount.
Some practitioners, such as cancer centers, cover their Medicaid losses by receiving higher rates for privately insured patients. But since almost all lecanemab patients are likely to be on government insurance, that “cross-subsidization” is less of an option, said Soeren Mattke, director of the Center for Improving Chronic Illness Care at the University of Southern California.
This poses a serious health equity issue because “dual eligibles are low-income patients with limited opportunities and education, and at higher risk of chronic illnesses including dementia,” Mattke said in an interview. Yet many doctors may not be willing to treat them, he said. “The idea of denying access to this group is just appalling.”
Eisai spokesperson Libby Holman said the company was reaching out to specialists and primary care physicians to make them aware of the drug, and that reimbursement options were improving. Eisai will provide the drug at no cost to patients in financial need, she said, and its “patient navigators” can help lock down insurance coverage.
“A lot of clinicians are excited about the drug, and patients are hearing about it,” said David Moss, chief financial officer of INmune Bio, a company that has another Alzheimer’s drug in development. “It’s a money center for infusion centers and MRI operators. It provides reasons for patients to come into the office, which is a billing thing.”
Outstanding doubts about Leqembi and related drugs have given urgency to efforts to monitor patient experiences. CMS is requiring Leqembi patients to be entered into a registry that tracks their outcomes. The agency has established a registry, but the Alzheimer’s Association, the leading advocacy group for dementia patients, is funding its own database to track those being treated, offering physician practices $2,500 to join it and up to $300 per patient visit.
In a letter to CMS on July 27, a group of policy experts said CMS should ensure that any and all Leqembi registries create and share data detailed enough for researchers and FDA safety teams to obtain a clear picture of the drug’s real-world profile.
The anti-amyloid drugs like lecanemab have created a polarized environment in medicine between those who think the drugs are a dangerous waste of money and those who believe they are a brilliant first step to a cure, said ICER’s Rind, who thinks lecanemab has modest benefits.
“People are as dug in on this as almost anything I’ve ever seen in medicine,” he said. “I don’t think it’s healthy.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
2 years 2 months ago
Aging, Health Care Costs, Health Industry, Medicaid, Medicare, Pharmaceuticals, Alzheimer's, CMS, Drug Costs
KFF Health News' 'What the Health?': Another Try for Mental Health ‘Parity’
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
The Biden administration continued a bipartisan, decades-long effort to ensure that health insurance treats mental illnesses the same as other ailments, with a new set of regulations aimed at ensuring that services are actually available without years-long waits or excessive out-of-pocket costs.
Meanwhile, two more committees in Congress approved bills this week aimed at reining in the power of pharmacy benefit managers, who are accused of keeping prescription drug prices high to increase their bottom lines.
This week’s panelists are Julie Rovner of KFF Health News, Anna Edney of Bloomberg, Joanne Kenen of the Johns Hopkins Bloomberg School of Public Health and Politico, and Sarah Karlin-Smith of the Pink Sheet.
Panelists
Anna Edney
Bloomberg
Joanne Kenen
Johns Hopkins Bloomberg School of Public Health and Politico
Sarah Karlin-Smith
Pink Sheet
Among the takeaways from this week’s episode:
- The Biden administration’s new rules to enforce federal mental health parity requirements include no threat of sanctions when health plans do not comply; noncompliance with even the most minimal federal rules has been a problem dating to the 1990s. Improving access to mental health care is not a new policy priority, nor a partisan one, yet it remains difficult to achieve.
- With the anniversary of the 988 Suicide & Crisis Lifeline, more people are becoming aware of how to access help and get it. Challenges remain, however, such as the hotline service’s inability to connect callers with local care. But the program seizes on the power of an initial connection for someone in a moment of crisis and offers a lifeline for a nation experiencing high rates of depression, anxiety, and suicide.
- In news about the so-called Medicaid unwinding, 12 states have paused disenrollment efforts amid concerns they are not following renewal requirements. A major consideration is that most people who are disenrolled would qualify to obtain inexpensive or even free coverage through the Affordable Care Act. But reenrollment can be challenging, particularly for those with language barriers or housing insecurity, for instance.
- With a flurry of committee activity, Congress is revving up to pass legislation by year’s end targeting the role of pharmacy benefit managers — and, based on the advertisements blanketing Washington, PBMs are nervous. It appears legislation would increase transparency and inform policymakers as they contemplate further, more substantive changes. That could be a tough sell to a public crying out for relief from high health care costs.
- Also on Capitol Hill, far-right lawmakers are pushing to insert abortion restrictions into annual government spending bills, threatening yet another government shutdown on Oct. 1. The issue is causing heartburn for less conservative Republicans who do not want more abortion votes ahead of their reelection campaigns.
- And the damage to a Pfizer storage facility by a tornado is amplifying concerns about drug shortages. After troubling problems with a factory in India caused shortages of critical cancer drugs, decision-makers in Washington have been keeping an eye on the growing issues, and a response may be brewing.
Also this week, Rovner interviews KFF Health News’ Céline Gounder about the new season of her “Epidemic” podcast. This season chronicles the successful public health effort to eradicate smallpox.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: The Nation’s “The Anti-Abortion Movement Gets a Dose of Post-Roe Reality,” by Amy Littlefield.
Joanne Kenen: Food & Environment Reporting Network’s “Can Biden’s Climate-Smart Agriculture Program Live Up to the Hype?” by Gabriel Popkin.
Anna Edney: Bloomberg’s “Mineral Sunscreens Have Potential Hidden Dangers, Too,” by Anna Edney.
Sarah Karlin-Smith: CNN’s “They Took Blockbuster Drugs for Weight Loss and Diabetes. Now Their Stomachs Are Paralyzed,” by Brenda Goodman.
Also mentioned in this week’s episode:
- CNN’s “Medicaid Disenrollments Paused in a Dozen States After Failure to Comply With Federal Rules,” by Tami Luhby.
- Abortion, Every Day’s “Why Are OBGYNs Being Forced to Go to Texas?” by Jessica Valenti.
- Politico’s “GOP Looks to Spending Fights for Wins on Abortion, Trans Care, Contraception,” by Alice Miranda Ollstein.
- KFF Health News’ “A Year With 988: What Worked? What Challenges Lie Ahead,” by Colleen DeGuzman.
click to open the transcript
Transcript: Another Try for Mental Health ‘Parity’
KFF Health News’ ‘What the Health?’Episode Title: Another Try for Mental Health ‘Parity’Episode Number: 307Published: July 27, 2023
[Editor’s note: This transcript, generated using transcription software, has been edited for style and clarity.]
Julie Rovner: Hello and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News, and I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, July 27, at 10 a.m. As always, news happens fast and things might have changed by the time you hear this. So, here we go. We are joined today via video conference by Joanne Kenen of the Johns Hopkins Bloomberg School of Public Health and Politico.
Joanne Kenen: Hi, everybody.
Rovner: Sarah Karlin-Smith, the Pink Sheet.
Sarah Karlin-Smith: Hi, Julie.
Rovner: And Anna Edney of Bloomberg News.
Edney: Hello.
Rovner: Later in this episode, we’ll have my interview with my KFF colleague Céline Gounder about the new season of her podcast “Epidemic,” which tracks one of the last great public health success stories, the eradication of smallpox. But first, this week’s news. I want to start this week with mental health, which we haven’t talked about in a while — specifically, mental health parity, which is both a law and a concept, that mental ailments should be covered and reimbursed by health insurance the same way as a broken bone or case of pneumonia or any other — air quotes — “physical ailment.” Policymakers, Republican and Democrat, and the mental health community have been fighting pretty much nonstop since the mid-1990s to require parity. And despite at least five separate acts of Congress over that time — I looked it up this week — we are still not there yet. To this day, patients with psychiatric illnesses find their care denied reimbursement, made difficult to access, or otherwise treated as lesser. This week, the Biden administration is taking another whack at the issue, putting out proposed rules it hopes will start to close the remaining parity gap, among other things by requiring health plans to analyze their networks and prior authorization rules and other potential barriers to care to ensure that members actually can get the care they need. What I didn’t see in the rules, though, was any new threat to sanction plans that don’t comply — because plans have been not complying for a couple of decades now. How much might these new rules help in the absence of a couple of multimillion-dollar fines?
Edney: I had that same question when I was considering this because I didn’t see like, OK, like, great, they’re going to do their self-policing, and then what? But I do think that there’s the possibility, and this has been used in health care before, of public shaming. If the administration gets to look over this data and in some way compile it and say, here’s the good guys, here’s the bad guys, maybe that gets us somewhere.
Rovner: You know, it strikes me, this has been going on for so very long. I mean, at first it was the employer community actually that did most of the negotiating, not the insurers. Now that it’s required, it’s the insurers who are in charge of it. But it has been just this incredible mountain to scale, and nobody has been able to do it yet.
Kenen: And it’s always been bipartisan.
Rovner: That’s right.
Kenen: And it really goes back to mostly, you know, the late Sen. [Paul] Wellstone [(D-Minn.)] and [Sen. Pete] Domenici [(R-N.M.)], both of whom had close relatives with serious mental illness. You know, Domenici was fairly conservative and traditional conservative, and Wellstone was extremely liberal. And they just said, I mean, this — the parity move began — the original parity legislation, at least the first one I’m aware of. And it was like, I think it was before I came to Washington. I think it was in the ’80s, certainly the early — by the ’90s.
Rovner: It was 1996 when when the first one actually passed. Yeah.
Kenen: I mean, they started talking about it before that because it took them seven or eight years. So this is not a new idea, and it’s not a partisan idea, and it’s still not done. It’s still not there.
Edney: I think there’s some societal shift too, possibly. I mean, we’re seeing it, and maybe we’re getting closer. I’ve seen a lot of billboards lately. I’ve done some work travel. When I’m on the road, I feel like I’m always seeing these billboards that are saying mental health care is health care. And trying to hammer that through has really taken a long time.
Rovner: So while we are on the subject of mental health, one of the good things I think the government has done in the last year is start the 988 Suicide & Crisis Lifeline, which turned 1 this month. Early data from shifting the hotline from a 10-digit number to a three-digit one that’s a lot easier to remember does suggest that more people are becoming aware of immediate help and more people are getting it. At the same time, it’s been able to keep up with the demand, even improving call answering times — I know that was a big concern — but there is still a long way to go, and this is hardly a panacea for what we know is an ongoing mental health crisis, right?
Karlin-Smith: This is a good first step to get people in crisis help without some of the risks that we’ve seen. If you go towards the 911 route, sometimes police are not well trained to handle these calls and they end in worse outcomes than necessary. But then you have to have that second part, which is what we were talking about before, which is the access to the longer-term mental health support to actually receive the treatment you need. There’s also some issues with this hotline going forward in terms of long-term funding and, you know, other tweaks they need to work out to make sure, again, that people who are not expecting to interact with law enforcement actually don’t end up indirectly getting there and things like that as well.
Kenen: Do any of you know whether there’s discussion of sort of making people who don’t remember it’s 988 and they call 911 — instead of dispatching cops, are the dispatchers being trained to just transfer it over to 988?
Rovner: That I don’t know.
Kenen: I’m not aware of that. But it just sort of seems common sense.
Rovner: One thing I know they’re working on is, right now I think there’s no geolocation. So when you call 988, you don’t necessarily get automatically referred to resources that are in your community because they don’t necessarily know where you’re calling from. And I know that’s an effort. But yeah, I’m sure there either is or is going to be some effort to interact between 988 and 911.
Kenen: It’s common sense to us. It doesn’t mean it’s actually happening. I mean, this is health care.
Rovner: As we point out, this is mental health care, too.
Kenen: Yeah, right.
Rovner: It’s a step.
Kenen: But I think that, you know, sort of the power of that initial connection is something that’s easy for people to underestimate. I mean, my son in college was doing a helpline during 2020-2021. You know, he was trained, and he was also trained, like, if you think this is beyond what a college-aged volunteer, that if you’re uncertain, you just switched immediately to a mental health professional. But sometimes it’s just, people feel really bad and just having a voice gets them through a crisis moment. And as we all know, there are a lot of people having a lot of crisis moments. I doubt any of us don’t know of a suicide in the last year, and maybe not in our immediate circle, but a friend of a friend, I mean, or, you know — I know several. You know, we are really at a moment of extreme crisis. And if a phone call can help some percentage of those people, then, you know, it needs to be publicized even more and improved so it can be more than a friendly voice, plus a connection to what, ending this repetition of crisis.
Rovner: I feel like the people who worked hard to get this implemented are pretty happy a year later at how, you know — obviously there’s further to go — but they’re happy with how far they’ve come. Well, so, probably the only thing worse than not getting care covered that should be is losing your health coverage altogether, which brings us to the Medicaid unwinding, as states redetermine who’s still eligible for Medicaid for the first time since the start of the pandemic. Our podcast colleague Tami Luhby over at CNN had a story Friday that I still haven’t seen anywhere else. Apparently 12 states have put their disenrollments on pause, says Tami. But we don’t know which 12, according to the KFF disenrollment tracker. As of Wednesday, July 26, at least 3.7 million people have been disenrolled from the 37 states that are reporting publicly, nearly three-quarters of those people for, quote, “procedural reasons,” meaning those people might still be eligible but for some reason didn’t complete the renewal process. The dozen states on pause are apparently ones that HHS [the Department of Health and Human Services] thinks are not following the renewal requirements and presumably ones whose disenrollments are out of line. The Centers for Medicare & Medicaid Services, which is overseeing this, is not naming those states, but this points up exactly what a lot of people predicted would happen when states started looking at eligibility again, that a lot of people who were quite likely still eligible were simply going to lose their insurance altogether, right?
Edney: Yeah, it seemed like there was a lot of preparation in some ways to anticipating this. And then, yeah, obviously you had the states that were just raring to go and try to get people off the rolls. And yeah, it would be very interesting to know what those 12 are. I think Tami’s reporting was stellar and she did a really good job. But that’s, like, one piece of the puzzle we’re missing. And I know CMS said that they’re not naming them because they are working well with them to try to fix it.
Rovner: The one thing we obviously do know is that there are several states that are doing this faster than is required — in fact, faster than is recommended. And what we know is that the faster they do it, the more likely they are going to have people sort of fall between the cracks. The people who are determined to be no longer eligible for Medicaid are supposed to be guided to programs for which they are eligible. And presumably most of them, unless they have, you know, gotten a really great job or hit the lottery, will still be eligible at least for subsidies under the Affordable Care Act. And they’re supposed to be guided to those programs. And it’s not clear yet whether that’s happening, although I know there are an awful lot of people who are watching this pretty closely. There were over 90 million people on Medicaid by the end of the pandemic, by the point at which states no longer had to keep people on. That’s a lot more people than Medicaid normally has. It’s usually more around 70 or even 80 million. So there’s excess people. And the question is what’s going to happen to those people and whether they’re going to have some sort of health insurance. And I guess it’s going to be more than a couple of months before we know that. Yes, Joanne.
Kenen: I think that it’s important to remember that there’s no open enrollment season for Medicaid the way there is for the ACA, so that if you’re disenrolled and you get sick and you go to a doctor or a hospital, they can requalify you and you can get it again. The problem is people who think that they’re disenrolled or are told that they’re disenrolled may not realize. They may not go to the doctor because they think they can’t afford it. They may not understand there’s a public education campaign there, too, that I haven’t seen. You know, if you get community health clinics, hospitals, they can do Medicare, Medicaid certification. But it’s dangerous, right? If you think, oh, I’m going to get a bill I can’t afford and I’m just going to see if I can tough this out, that’s not the way to take care of your health. So there’s that additional conundrum. And then, you know, I think that HHS can be flexible on special enrollment periods for those who are not Medicaid-eligible and are ACA-eligible, but most of them are still Medicaid-eligible.
Rovner: If you get kicked off of Medicaid, you get an automatic special enrollment for the ACA anyway.
Kenen: But not forever. If the issue is it’s in a language you don’t speak or at an address you don’t live in, or you just threw it out because you didn’t understand what it was — there is institutional failures in the health care system, and then there’s people have different addresses in three years, particularly poor people; they move around. There’s a communication gap. You know, I talked to a health care system a while ago in Indiana, a safety net, that was going through electronic health records and contacting people. And yet that’s Indiana and they, you know, I think it was Tami who pointed out a few weeks ago on the podcast, Indiana is not doing great, in spite of, you know, really more of a concerted effort than other states or at least other health systems, not that I talk to every single health system in the country. I was really impressed with how proactive they were being. And still people are falling, not just through the cracks. I mean, there’s just tons of cracks. It’s like, you know, this whole landscape of cracks.
Rovner: I think everybody knew this was going to be a big undertaking. And obviously the states that are trying to do it with some care are having problems because it’s a big undertaking. And the states that are doing it with a little bit less care are throwing a lot more people off of their health insurance. And we will continue to follow this. So it is the end of July. I’m still not sure how that happened.
Kenen: ’Cause after June, Julie.
Rovner: Yes. Thank you. July is often when committees in Congress rush to mark up bills that they hope to get to the floor and possibly to the president in that brief period when lawmakers return from the August recess before they go out for the year, usually around Thanksgiving. This year is obviously no exception. While Sen. Bernie Sanders [(I-Vt.)] at the Health, Education, Labor and Pensions Committee has delayed consideration of that primary care-community health center bill that we talked about last week until September, after Republicans rebelled against what was supposed to have been a bipartisan bill, committee action on pharmacy benefit managers and other Medicare issues did take place yesterday in the Senate Finance Committee and the House Ways and Means Committee. Sarah, you’re following this, right? What’s happening? And I mean, so we’ve now had basically all four of the committees that have some kind of jurisdiction over this who’ve acted. Is something going to happen on PBM regulation this year?
Karlin-Smith: Actually, five committees have acted because the House Ed[ucation] and Workforce Committee has also acted on the topic. So there’s a lot of committees with a stake in this. I think there’s certainly set up for something for the fall, end of the year, to happen in the pharmacy benefit manager space. And there’s a decent amount of bipartisanship around the issue, depending on exactly which committee you’re looking at. But even if the policies that haven’t gotten through haven’t been bipartisan, I think there’s general bipartisan interest among all the committees of tackling the issue. The question is how meaningful, I guess, the policies that we get done are. Right now it looks like what we’re going to end up with is some kind of transparency measure. It reminded me a little bit of our discussion of the mental health stuff [President Joe] Biden is doing going forward. Essentially what it’s going to end up doing is get the government a lot of detailed data about how PBMs operate, how this vertical integration of PBMs — so there’s a lot of common ownership between PBMs, health insurance plans, pharmacies and so forth — may be impacting the cost of our health care and perhaps in a negative way. And then from that point, the idea would be that later Congress could go back and actually do the sort of policy reforms that might be needed. So I know there are some people that are super excited about this transparency because it is such an opaque industry. But at the same point, you can’t kind of go to your constituents and say, “We’ve changed something,” right away or, you know, “We’re going to save you a ton of money with this kind of legislation.”
Rovner: You could tell how worried the PBMs are by how much advertising you see, if you still watch TV that has advertising, which I do, because I watch cable news. I mean, the PBMs are clearly anxious about what Congress might do. And given the fact that, as you point out and as we’ve been saying for years, drug prices are a very bipartisan issue — and it is kind of surprising, like mental health, it’s bipartisan, and they still haven’t been able to push this as far as I think both Democrats and Republicans would like for it to go. Is there anything in these bills that surprised you, that goes further than you expected or less far than expected?
Karlin-Smith: There’s been efforts to sort of delink PBM compensation from rebates. And in the past, when Congress has tried to look into doing this, it’s ended up being extremely costly to the government. And they figured out in this set of policies sort of how to do this without those costs, which is basically, they’re making sure that the PBMs don’t have this perverse incentive to make money off of higher-priced drugs. However, the health plans are still going to be able to do that. So it’s not clear how much of a benefit this will really be, because at this point, the health plans and the PBMs are essentially one and the same. They have the same ownership. But, you know, I do think there has been some kind of creativity and thoughtfulness on Congress’ part of, OK, how do we tackle this without also actually increasing how much the government spends? Because the government helps support a lot of the premiums in these health insurance programs.
Rovner: Yeah. So the government has quite a quite a financial stake in how this all turns out. All right. Well, we will definitely watch that space closely. Let us move on to abortion. In addition to it being markup season for bills like PBMs, it’s also appropriations season on Capitol Hill, with the Sept. 30 deadline looming for a completion of the 12 annual spending bills. Otherwise, large parts of the government shut down, which we have seen before in recent years. And even though Democrats and Republicans thought they had a spending detente with the approval earlier this spring of legislation to lift the nation’s debt ceiling, Republicans in the House have other ideas; they not only want to cut spending even further than the levels agreed to in the debt ceiling bill, but they want to add abortion and other social policy riders to a long list of spending bills, including not just the one for the Department of Health and Human Services but the one for the Food and Drug Administration, which is in the agriculture appropriations, for reasons I’ve never quite determined; the financial services bill, which includes funding for abortion in the federal health insurance plan for government workers; and the spending bill for Washington, D.C., which wants to use its own taxpayer money for abortion, and Congress has been making that illegal pretty much for decades. In addition to abortion bans, conservatives want riders to ban gender-affirming care and even bar the FDA from banning menthol cigarettes. So it’s not just abortion. It’s literally a long list of social issues. Now, this is nothing new. A half a dozen spending bills have carried a Hyde [Amendment] type of abortion ban language for decades, as neither Republicans nor Democrats have had the votes to either expand or take away the existing restrictions. On the other hand, these conservatives pushing all these new riders don’t seem to care if the government shuts down if these bills pass. And that’s something new, right?
Kenen: Over abortion it’s something new, but they haven’t cared. I mean, they’ve shut down the government before.
Rovner: That’s true. The last time was over Obamacare.
Kenen: Right. And, which, the great irony is the one thing they — when they shut down the government because Obamacare was mandatory, not just discretionary funding, Obamacare went ahead anyway. So, I mean, minor details, but I think this is probably going to be an annual battle from now on. It depends how hard they fight for how long. And with some of these very conservative, ultra-conservative lawmakers, we’ve seen them dig in on abortion, on other issues like the defense appointees. So I think it’s going to be a messy October.
Rovner: Yeah, I went back and pulled some of my old clips. In the early 1990s I used to literally keep a spreadsheet, and I think that’s before we had Excel, of which bill, which of the appropriations bills had abortion language and what the status was of the fights, because they were the same fights year after year after year. And as I said, they kind of reached a rapprochement at one point, or not even a rapprochement — neither side could move what was already there. At some point, they kind of stopped trying, although we have seen liberals the last few years try to make a run at the actual, the original Hyde Amendment that bans federal funding for most abortions — that’s in the HHS bill — and unsuccessfully. They have not had the votes to do that. Presumably, Republicans don’t have the votes now to get any of these — at least certainly not in the Senate — to get any of these new riders in. But as we point out, they could definitely keep the government closed for a while over it. I mean, in the Clinton administration, President [Bill] Clinton actually had to swallow a bunch of new riders because either it was that or keep the government closed. So that’s kind of how they’ve gotten in there, is that one side has sort of pushed the other to the brink. You know, everybody seems to assume at this point that we are cruising towards a shutdown on Oct. 1. Does anybody think that we’re not?
Kenen: I mean, I’m not on the Hill anymore, but I certainly expect a shutdown. I don’t know how long it lasts or how you resolve it. And I — even more certain we’ll have one next year, which, the same issues will be hot buttons five weeks before the elections. So whatever happens this year is likely to be even more intense next year, although, you know, next year’s far away and the news cycle’s about seven seconds. So, you know, I think this could be an annual fight and for some time to come, and some years will be more intense than others. And you can create a deal about something else. And, you know, the House moderates are — there are not many moderates — but they’re sort of more traditional conservatives. And there’s a split in the Republican Party in the House, and we don’t know who’s going to fold when, and we don’t — we haven’t had this kind of a showdown. So we don’t really know how long the House will hold out, because some of the more moderate lawmakers who are — they’re all up for reelection next year. I mean, some of them don’t agree. Some of are not as all or nothing on abortion as the —
Rovner: Well, there are what, a dozen and a half Republicans who are in districts that President Biden won who do not want to vote on any of these things and have made it fairly clear to their leadership that they do not want to vote on any of these things. But obviously the conservatives do.
Kenen: And they’ve been public about that. They’ve said it. I mean, we’re not guessing. Some of them spoke up and said, you know, leave it to the states. And that’s what the court decided. And they don’t want to nationalize this even further than it’s nationalized. And I think, you know, when you have the Freedom Caucus taking out Marjorie Taylor Greene, I mean, I have no idea what’s next.
Rovner: Yeah, things are odd. Well, I want to mention one more abortion story this week that I read in the newsletter “Abortion, Every Day,” by Jessica Valenti. And shoutout here: If you’re interested in this issue and you don’t subscribe, you’re missing out. I will include the link in the show notes. The story’s about Texas and the exam to become a board-certified obstetrician-gynecologist. The board that conducts the exam is based in Dallas and has been for decades, and Texas is traditionally where this test has been administered. During the pandemic, the exam was given virtually because nothing was really in person. But this year, if a doctor wants to become board-certified, he or she will have to travel to Texas this fall. And a lot of OB-GYNs don’t want to do that, for fairly obvious reasons, like they are afraid of getting arrested and sent to prison because of Texas’ extreme anti-abortion laws. And yikes, really, this does not seem to be an insignificant legal risk here for doctors who have been performing abortions in other states. This is quite the dilemma, isn’t it?
Karlin-Smith: Well, the other thing I thought was interesting about — read part of that piece — is just, she was pointing out that you might not just want to advertise in a state where a lot of people are anti-abortion that all of these people who perform abortions are all going to be at the same place at the same time. So it’s not just that they’re going to be in Texas. Like, if anybody wants to go after them, they know exactly where they are. So it can create, if nothing else, just like an opportunity for big demonstrations or interactions that might disrupt kind of the normal flow of the exam-taking.
Kenen: Or violence. Most people who are anti-abortion are obviously not violent, but we have seen political violence in this country before. And you just need one person, which, you know, we seem to have plenty of people who are willing to shoot at other people. I thought it was an excellent piece. I mean, I had not come across that before until you sent it around, and there’s a solution — you know, like, if you did it virtually before — and I wasn’t clear, or maybe I just didn’t pay attention: Was this certification or also recertification?
Rovner: No, this was just certification. Recertification’s separate. So these are these are young doctors who want to become board-certified for the first time.
Kenen: But the recertification issues will be similar. And this is a yearly — I mean, I don’t see why they just don’t give people the option of doing it virtual.
Rovner: But we’ll see if they back down. But you know, I had the same thought that Sarah did. It’s like, great, let’s advertise that everybody’s going to be in one place at one time, you know, taking this exam. Well, we’ll see how that one plays out. Well, finally this week, building on last week’s discussion on health and climate change and on drug shortages, a tornado in Rocky Mount, North Carolina, seriously damaged a giant Pfizer drug storage facility, potentially worsening several different drug shortages. Sarah, I remember when the hurricane in Puerto Rico seemed to light a fire under the FDA and the drug industry about the dangers of manufacturing being too centralized in one place. Now we have to worry about storage, too? Are we going to end up, like, burying everything underground in Fort Knox?
Karlin-Smith: I think there’s been a focus even since before [Hurricane] Maria, but that certainly brought up that there’s a lack of redundancy in U.S. medical supply chains and, really, global supply chains. It’s not so much that they need to be buried, you know, that we need bunkers. It’s just that — Pfizer had to revise the numbers, but I think the correct number was that that facility produces about 8% of the sterile kind of injectables used in the U.S. health system, 25% of all Pfizer’s — it’s more like each company or the different plants that produce these drugs, it needs to be done in more places so that if you have these severe weather events in one part of the country, there’s another facility that’s also producing these drugs or has storage. So I don’t know that these solutions need to be as extreme as you brought up. But I think the problem has been that when solutions to drug shortages have come up in Congress, they tend to focus on FDA authorities or things that kind of nibble around the edges of this issue, and no one’s ever really been able to address some of the underlying economic tensions here and the incentives that these companies have to invest in redundancy, invest in better manufacturing quality, and so forth. Because at the end of the day these are often some of the oldest and cheapest drugs we have, but they’re not necessarily actually the easiest to produce. While oftentimes we’re talking about very expensive, high-cost drugs here, this may be a case where we have to think about whether we’ve let the prices drop too low and that’s sort of keeping a market that works if everything’s going perfectly well but then leads to these shortages and other problems in health care.
Rovner: Yeah, the whole just-in-time supply chain. Well, before we leave this, Anna, since you’re our expert on this, particularly international manufacturing, I mean, has sort of what’s been happening domestically lit a fire under anybody who’s also worried about some of these, you know, overseas plants not living up to their safety requirements?
Edney: Well, I think there are these scary things happen like a tornado or hurricane and everybody is kind of suddenly paying attention. But I think that the decision-makers in the White House or on Capitol Hill have been paying attention a little bit longer. We’ve seen these cancer — I mean, for a long time not getting anything done, as Sarah mentioned — but recently, it’s sort of I think the initial spark there was these cancer drug shortages that, you know, people not being able to get their chemo. And that was from an overseas factory; that was from a factory in India that had a lot of issues, including shredding all of their quality testing documents and throwing them in a truck, trying to get it out of there before the FDA inspectors could even see it.
Kenen: That’s always very reassuring.
Edney: It is. Yeah. It makes you feel really good. And one bag did not make it out of the plant in time, so they just threw acid on it instead of letting FDA inspectors look at it. So it’s definitely building in this tornado. And what might come out of it if there are a lot of shortages, I haven’t seen huge concern yet from the FDA on that front. But I think that it’s something that just keeps happening. It’s not letting up. And, you know, my colleagues did a really good story yesterday. There’s a shortage of a certain type of penicillin you give to pregnant people who have syphilis. If you pass syphilis on to your baby, the baby can die or be born with a lot of issues — it’s not like if an adult gets syphilis — and they’re having to ration it, and adults aren’t getting treated fully for syphilis because the babies need it more so, and so this is like a steady march that just keeps going on. And there’s so many issues with the industry, sort of how it’s set up, what Sarah was talking about, that we haven’t seen anybody really be able to touch yet.
Rovner: We will continue to stay on top of it, even if nobody else does. Well, that is this week’s news. Now we will play my interview with KFF’s Céline Gounder, and then we will come back and do our extra credit. I am pleased to welcome back to the podcast Dr. Céline Gounder, KFF senior fellow and editor-at-large for public health, as well as an infectious disease specialist and epidemiologist in New York and elsewhere. Céline is here today to tell us about the second season of her podcast, “Epidemic,” which tells the story of the successful effort to eradicate smallpox and explores whether public health can accomplish such big things ever again. Céline, thank you for joining us.
Céline Gounder: It’s great to be here, Julie.
Rovner: So how did you learn about the last steps in the journey to end smallpox, and why did you think this was a story worth telling broadly now?
Gounder: Well, this is something I actually studied back when I was in college in the ’90s, and I did my senior thesis in college on polio eradication, and this was in the late ’90s, and we have yet to eradicate polio, which goes to show you how difficult it is to eradicate an infectious disease. And in the course of doing that research, I was an intern at the World Health Organization for a summer and then continued to do research on it during my senior year. I also learned a lot about smallpox eradication. I got to meet a lot of the old leaders of that effort, folks like D.A. Henderson and Ciro de Quadros. And fast-forward to the present day: I think coming out of covid we’re unfortunately not learning what at least I think are the lessons of that pandemic. And I think sometimes it’s easier to go back in time in history, and that helps to depoliticize things, when people’s emotions are not running as high about a particular topic. And my thought was to go back and look at smallpox: What are the lessons from that effort, a successful effort, and also to make sure to get that history while we still have some of those leaders with us today.
Rovner: Yes, you’re singing my song here. I noticed the first episode is called “The Goddess of Smallpox.” Is there really a goddess of smallpox?
Gounder: There is: Shitala Mata. And the point of this episode was really twofold. One was to communicate the importance of understanding local culture and beliefs, not to dismiss these as superstitions, but really as ways of adapting to what was, in this case, a very centuries-long reality of living with smallpox. And the way people thought about it was that in some ways it was a curse, but in some ways it was also a blessing. And understanding that dichotomy is also important, whether it’s with smallpox or other infectious diseases. It’s important to understand that when you’re trying to communicate about social and public health interventions.
Rovner: Yeah, because I think people don’t understand that public health is so unique to each place. I feel like in the last 50 years, even through HIV and other infectious diseases, the industrialized world still hasn’t learned very well how to deal with developing countries in terms of cultural sensitivity and the need for local trust. Why is this a lesson that governments keep having to relearn?
Gounder: Well, I would argue we don’t even do it well in our own country. And I think it’s because we think of health in terms of health care, not public health, in the United States. And that also implies a very biomedical approach to health issues. And I think the mindset here is very much, oh, well, once you have the biomedical tools — the vaccines, the diagnostics, the drugs — problem solved. And that’s not really solving the problem in a pandemic, where much of your challenge is really social and political and economic and cultural. And so if you don’t think about it in those terms, you’re really going to have a flat-footed response.
Rovner: So what should we have learned from the smallpox eradication effort that might have helped us deal with covid or might help us in the future deal with the next pandemic?
Gounder: Well, I think one side of this is really understanding what the local culture was, spending time with people in community to build trust. I think we came around to understanding it in part, in some ways, in some populations, in some geographies, but unfortunately, I think it was very much in the crisis and not necessarily a long-term concerted effort to do this. And that I think is concerning because we will face other epidemics and pandemics in the future. So, you know, how do you lose trust? How do you build trust? I think that’s a really key piece. Another big one is dreaming big. And Dr. Bill Foege — he was one of the leaders of smallpox eradication, went on to be the director of the CDC [Centers for Disease Control and Prevention] under President [Jimmy] Carter — one of the pieces of advice he’s given to me as a mentor over the years is you’ve got to be almost foolishly optimistic about getting things done, and don’t listen to the cynics and pessimists. Of course, you want to be pragmatic and understand what will or won’t work, but to take on such huge endeavors as eradicating smallpox, you do have to be very optimistic and remind yourself every day that this is something you can do if you put your mind to it.
Rovner: I noticed, at least in the first couple of episodes that I’ve listened to, the media doesn’t come out of this looking particularly good. You’re both a journalist and a medical expert. What advice do you have for journalists trying to cover big public health stories like this, like covid, like things that are really important in how you communicate this to the public?
Gounder: Well, I think one is try to be hyperlocal in at least some of your reporting. I think one mistake during the pandemic was having this very top-down perspective of “here is what the CDC says” or “here is what the FDA says” or whomever in D.C. is saying, and that doesn’t really resonate with people. They want to see their own experiences reflected in the reporting and they want to see people from their community, people they trust. And so I think that is something that we should do better at. And unfortunately, we’re also somewhat hampered in doing so because there’s been a real collapse of local journalism in most of the country. So it really does fall to places like KFF Health News, for example, to try to do some of that important reporting.
Rovner: We will all keep at it. Céline Gounder, thank you so much for joining us. You can find Season 2 of “Epidemic,” called “Eradicating Smallpox,” wherever you get your podcasts.
Gounder: Thanks, Julie.
Rovner: OK, we’re back. It’s time for our extra credit segment. That’s when we each recommend a story we read this week we think you should read too. As always, don’t worry if you miss it. We will post the links on the podcast page at kffhealthnews.org and in our show notes on your phone or other mobile device. Sarah, why don’t you go first this week?
Karlin-Smith: Sure. I took a look at a piece from Brenda Goodman at CNN called “They Took Blockbuster Drugs for Weight Loss and Diabetes. Now Their Stomachs Are Paralyzed,” and it’s a really good deep dive into — people probably have heard of Ozempic, Wegovy — these what are called GLP-1 drugs that have been used for diabetes. And we’ve realized in higher doses even for people without diabetes, they often are very helpful at losing weight, that that’s partially because they slow the passage of food through your stomach. And there are questions about whether for some people that is leading to stomach paralysis or other extreme side effects. And I think it’s a really interesting deep dive into the complicated world of figuring out, Is this caused by the drug? Is it caused by other conditions that people have? And then how should you counsel people about whether they should receive the drugs and the benefits outweighing the risks? So I think it’s like just a good thing for people to read when you sort of hear all this hype about a product and how great they must be, that it’s always a little bit more complicated than that. And it also brought up another aspect of it, which is how these drugs may impact people who are going to get surgery and anesthesia and just the importance of communicating this to your doctor so they know how to appropriately handle the drugs. Because if you still have food content in your stomach during a surgery, that can be extremely dangerous. And I thought just that aspect alone of this story is really interesting, because they talk about people maybe not wanting to even let their doctors know they’re on these drugs because of stigma surrounding weight loss. And just again, once you get a new medicine that might end up being taken by a lot of people, the complications or, you know, there’s the dynamics of how it impacts other parts of medicine, and we need to adjust.
Rovner: Yeah. And I think the other thing is, you know, we know these drugs are safe because people with diabetes have been taking them for, what, six or seven years. But inevitably, anytime you get a drug that lots more people take, then you start to see the outlier side effects, which, if it’s a lot of people, can affect a lot of people. Joanne.
Kenen: I have a piece from FERN, which is the Food & Environment Reporting Network and in partnership with Yale Environ 360, and it’s by Gabriel Popkin. And it’s called “Can Biden’s Climate-Smart Agriculture Program Live Up to the Hype?” And I knew nothing about smart agriculture, which is why I found this so interesting. So, this is an intersection of climate change and food, which is obviously also a factor in climate change. And there’s a lot of money from the Biden administration for farmers to use new techniques that are more green-friendly because as we all know, you know, beef and dairy, things that we thought were just good for us — maybe not beef so much — but, like, they’re really not so good for the planet we live on. So can you do things like, instead of using fertilizer, plant cover crops in the offseason? I mean, there’s a whole list of things that — none of us are farmers, but there’s also questions about are they going to work? Is it greenwashing? Is it stuff that will work but not in the time frame that this program is funding? How much of it’s going to go to big agribusiness, and how much of it is going to go to small farmers? So it’s one hand, it’s another. You know, there’s a lot of low-tech practices. We’re going to have to do absolutely everything we can on climate. We’re going to have to use a variety of — you know, very large toolkit. So it was interesting to me reading about these things that you can do that make agriculture, you know, still grow our food without hurting the planet, but also a lot of questions about, you know, is this really a solution or not? But, you know, I didn’t know anything about it. So it was a very interesting read.
Rovner: And boy, you think the drug companies are influential on Capitol Hill. Try going with big agriculture. Anna.
Edney: I’m going to toot my own horn for a second here —
Rovner: Please.
Edney: — and do one of my mini-investigations that I did, “Mineral Sunscreens Have Potential Hidden Dangers, Too.” So there’s been a lot of talk: Use mineral sunscreen to save the environment or, you know, for your own health potentially. But they’re white, they’re very thick. And, you know, people don’t want to look quite that ghostly. So what’s been happening lately is they’ve been getting better. But what I found out is a lot of that is due to a chemical — that is what people are trying to move away from, is chemical sunscreens — but the sunscreen-makers are using this chemical called butyloctyl salicylate. And you can read the article for kind of the issues with it. I guess the main one I would point out is, you know, I talked to the Environmental Working Group because they do these verifications of sunscreens based on their look at how good are they for your health, and a couple of their mineral ones had this ingredient in it. So when I asked them about it, they said, Oh, whoops; like, we do actually need to revisit this because it is a chemical that is not recommended for children under 4 to be using on their bodies. So there’s other issues with it, too — just the question of whether you’re really being reef-safe if it’s in there, and other things as well.
Rovner: It is hard to be safe and be good to the planet. My story this week is by Amy Littlefield of The Nation magazine, and it’s called “The Anti-Abortion Movement Gets a Dose of Post-Roe Reality.” It’s about her visit to the annual conference of the National Right to Life Committee, which for decades was the nation’s leading anti-abortion organization, although it’s been eclipsed by some others more recently. The story includes a couple of eye-opening observations, including that the anti-abortion movement is surprised that all those bans didn’t actually reduce the number of abortions by very much. As we know, women who are looking for abortions normally will find a way to get them, either in state or out of state or underground or whatever. And we also learned in this story that some in the movement are willing to allow rape and incest exceptions in abortion bills, which they have traditionally opposed, because they want to use those as sweeteners for bills that would make it easier to enforce bans, stronger bans, things like the idea in Texas of allowing individual citizens to use civil lawsuits and forbidding local prosecutors from declining to prosecute abortion cases. We’re seeing that in some sort of blue cities in red states. It’s a really interesting read and I really recommend it. OK. That is our show for this week. As always, if you enjoyed the podcast, you can subscribe where ever you get your podcasts. We’d appreciate it if you left us a review; that helps other people find us, too. Special thanks, as always, to our producer, Francis Ying. Also as always, you can email us your comments or questions. We’re at whatthehealth@kff.org. Or you can tweet me. I’m @jrovner, and I’m on Bluesky and Threads. Joanne.
Kenen: @joannekenen1 at Threads.
Rovner: Sarah.
Karlin-Smith: I’m @SarahKarlin or @sarah.karlinsmith, depending on which of these many social media platforms you’re looking at, though.
Rovner: Anna.
Edney: @annaedney on Twitter and @anna_edneyreports on Threads.
Rovner: You can always find us here next week where we will always be in your podcast feed. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Stitcher, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
2 years 3 months ago
Capitol Desk, Health Care Costs, Health Care Reform, Health Industry, Insurance, Medicaid, Medicare, Mental Health, Multimedia, Pharmaceuticals, Public Health, Abortion, KFF Health News' 'What The Health?', Legislation, Podcasts, Prescription Drugs, texas, vaccines, Women's Health
KFF Health News' 'What the Health?': The Long Road to Reining In Short-Term Plans
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
It took more than two years, but the Biden administration has finally kept a promise made by then-candidate Joe Biden to roll back the Trump administration’s expansion of short-term, limited-duration health plans. The plans have been controversial because, while they offer lower premiums than more comprehensive health plans, they offer far fewer benefits and are not subject to the consumer protections of the Affordable Care Act.
Also this week, the FDA for the first time approved the over-the-counter sale of a hormonal birth control pill. With more states imposing restrictions on abortion, backers of the move say making it easier to prevent pregnancy is necessary now more than ever.
This week’s panelists are Julie Rovner of KFF Health News, Alice Miranda Ollstein of Politico, Amy Goldstein of The Washington Post, and Rachel Cohrs of Stat.
Panelists
Alice Miranda Ollstein
Politico
Amy Goldstein
The Washington Post
Rachel Cohrs
Stat News
Among the takeaways from this week’s episode:
- The FDA’s much-anticipated approval of the first over-the-counter hormonal birth control pill followed the advice of its outside advisory committee. The pill, Opill, will be available on shelves without age restrictions.
- The Biden administration announced moves to limit so-called junk plans on insurance marketplaces. The Trump administration had dropped many restrictions on the plans, which were originally intended to be used for short-term coverage gaps.
- As the nation continues to settle into a post-Dobbs patchwork of abortion laws, the Iowa Legislature approved a six-week ban on the procedure. And an Idaho law offers a key test of cross-border policing of abortion seekers, as other states watch how it unfolds.
- In other news, Georgia’s Medicaid work requirements took effect July 1, implementing new restrictions on who is eligible for the state-federal program for people with low incomes or disabilities. And the Supreme Court’s decision on affirmative action has the potential to shape the health care workforce, which research shows could have implications for the quality of patient care and health outcomes.
Also this week, Rovner interviews KFF Health News’ Bram Sable-Smith, who reported and wrote the latest KFF Health News-NPR “Bill of the Month” feature, about a patient who lacked a permanent mailing address and never got the hospital bills from an emergency surgery — but did receive a summons after she was sued for the debt. If you have an outrageous or exorbitant medical bill you want to share with us, you can do that here.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: KFF Health News’ “Doctor Lands in the Doghouse After Giving Covid Vaccine Waivers Too Freely,” by Brett Kelman.
Rachel Cohrs: ProPublica’s “How Often Do Health Insurers Say No to Patients? No One Knows,” by Robin Fields, and Stat’s “How UnitedHealth’s Acquisition of a Popular Medicare Advantage Algorithm Sparked Internal Dissent Over Denied Care,” by Casey Ross and Bob Herman.
Amy Goldstein: The New York Times’ “Medicare Advantage Plans Offer Few Psychiatrists,” by Reed Abelson.
Alice Miranda Ollstein: The Wall Street Journal’s “America Is Wrapped in Miles of Toxic Lead Cables,” by Susan Pulliam, Shalini Ramachandran, John West, Coulter Jones, and Thomas Gryta.
Also mentioned in this week’s episode:
- Stat’s “How One Medical School Became Remarkably Diverse — Without Considering Race in Admissions,” by Usha Lee McFarling.
- The New York Times’ “With End of Affirmative Action, a Push for a New Tool: Adversity Scores, by Stephanie Saul.
click to open the transcript
Transcript: The Long Road to Reining In Short-Term Plans
KFF Health News’ ‘What the Health?’Episode Title: The Long Road to Reining In Short-Term PlansEpisode Number: 305Published: July 13, 2023
[Editor’s note: This transcript, generated using transcription software, has been edited for style and clarity.]
Julie Rovner: Hello and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News. And I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, July 13, at 10 a.m. As always, news happens fast and things might have changed by the time you hear this. So here we go. Today we are joined via video conference by Alice Miranda Ollstein of Politico.
Alice Miranda Ollstein: Good morning.
Rovner: Rachel Cohrs of Stat News.
Rachel Cohrs: Hi, everybody.
Rovner: And Amy Goldstein of The Washington Post.
Goldstein: Good to be with you.
Rovner: Later in this episode, we’ll have my interview with KFF Health News’ Bram Sable-Smith, who wrote the latest KFF Health News-NPR “Bill of the Month.” The hospital that provided care to this month’s patient couldn’t find her to send her a bill, but the debt collectors sure could. But first, this week’s news. Actually, it’s more like the last month’s news because we actually haven’t talked about news in a while. So we’re going to try to hit a bunch of items in sort of a lightning round. Let’s start with something we knew was coming. We just didn’t know exactly when. Last week, the Biden administration finally cracked down on short-term health plans. Those are the ones that are not subject to the strict rules of the Affordable Care Act. Amy, you wrote about this. What are short-term plans, and why have they been so controversial?
Goldstein: Well, short-term plans — they’re called short-term limited-duration plans, and really terrible argot, but that’s their name. They’ve been around as an alternative to plans that are meeting the rules of the Affordable Care Act. They were originally designed for people to use as small bridges between, say, when they lost a job and they were about to get a new job and they needed something in the interim to provide health coverage. Republicans, during the time that they were trying very hard several years ago to get rid of as much as the Affordable Care Act as they could — they didn’t succeed at a lot of that, but they did succeed during the Trump administration at lengthening the time that people could have these plans. So they extended them from what had been a three-month maximum during the latter part of the [Barack] Obama administration to 12 months, and then they were renewable for up to three years. And Democrats began calling these “junk plans,” saying that people didn’t exactly know what they were buying, that the premiums were low but the benefits were small and if people got sick and really needed a lot of care they could be stuck paying for a lot of it on their own.
Rovner: And these were the very plans that the ACA was kind of designed to get rid of, right, where people would say, I have this great health plan, it only costs me $50 a month — but by the way, it only provides $500 worth of care.
Goldstein: Well, there’s that. And the other thing that the ACA was designed to do is treat people with preexisting conditions equally. And these plans do not have to do that. Some do, but they’re not required to. So President [Joe] Biden, since he was candidate Biden running for the 2020 election, has been saying for quite a while that he was going to knock down the duration of these plans, and some of his fellow Democrats have been leaning on him: “Why haven’t you done it yet?” And last week, he finally did. He didn’t bring it exactly to where the Obama administration had it, but he brought them down to three months with a one-month extension, so a total of four months.
Rovner: And I guess the resistance here is that they’re still kind of popular, right, for people who think they would rather pay very low premiums for very few benefits?
Goldstein: Well, the catch is that we don’t really know how popular they are because there aren’t very reliable data on how many people have these. But the presumption is that some people like them.
Rovner: All right, well we will see what happens with this time they’re trying to crack down. Let us move on to abortion and reproductive rights. We will start with the breaking news. The Food and Drug Administration just this morning approved Opill, which is the first over-the-counter birth control pill. Alice, we’ve known this was coming, right?
Ollstein: Yes, we did. We thought it would be a little later in the summer. But the decision itself reflects what the FDA’s outside advisory panel strongly recommended, which is to make these pills available over the counter without a prescription and without an age restriction, which was one looming question over this process.
Rovner: Yeah, I guess, Rachel, I mean, the issue here has been can women be trusted enough to know when they shouldn’t take birth control pills because they are contraindicated for some people?
Rachel Cohrs: Right. And I think that certainly it’s important to read through the information. There’s a question as to whether women will do that. And one part of the release that stood out to me is that the specific type of pill that this is requires women to take it around the same time every day, which is not necessarily the case for all birth control pills. And I think there’s a little bit more flexibility than there used to be with this kind of pill. But it is just important that all of this communication happens. And if there’s not a doctor or pharmacist in the middle, I think it will be kind of interesting to see how this plays out in the real world.
Rovner: Well, while this could definitely help people prevent pregnancy who don’t want to get pregnant, there’s certainly a lot of action still in the states around abortion. We’re going to start in Iowa, which since the last time we spoke has done basically a 360 on abortion. Last month, the state Supreme Court deadlocked on whether to reinstate a 2018 ban on almost all abortions. That left a lower court order blocking the ban intact, so abortion remained legal in Iowa. But anti-abortion Gov. Kim Reynolds refused to take no for an answer. She called a special session of the state legislature, which on Tuesday essentially repassed the 2018 ban. It’s supposed to take effect as soon as the governor signs it, which could be as soon as Friday. But first it goes back to court, right, Alice?
Ollstein: Right. As with all of these things, there’s just a lot of back-and-forth before it’s final. Groups have already filed a lawsuit. And, you know, because the courts’ sort of mixed treatment of the previous version of this, we sort of don’t know what’s going to happen. But the law could go into effect and then be blocked by courts later or it could be blocked before it goes into effect. There’s a lot of different ways this could go, but this is one of several states where new restrictions are coming online. We’re more than a year out from the Dobbs decision now, and things are not settled at all. Things are still flipping back and forth in different states.
Rovner: Yeah, there’s a lot of states where old restrictions came into effect and then were blocked and now they’re putting new restrictions and they might be blocked. Well, turning to another “I” state, this time Idaho, where the legislature this spring passed a first-in-the-nation bill attempting to criminalize the act of helping a minor cross state lines for an abortion, even if the abortion is legal in the state the minor travels to. Now, abortion rights supporters have filed a first-in-the-nation lawsuit to block the first-in-the-nation law. This could have really big ramifications. This is different from a lot of what’s going on in a lot of the other states, right?
Ollstein: Yeah. Over the last year, there’s been a lot of fear on the left of states reaching across their borders to try to police abortion. And it hasn’t really happened yet that we have seen. And so this, I think, is a key test of whether more states will attempt to go in this direction. You know, a lot of blue states passed sort of shield laws for patients, for providers, for data, out of fear that more red states would attempt more cross-border policing. But that really hasn’t materialized broadly yet.
Rovner: I remember Missouri was the one that was talking about it, right, to make it a crime if —
Ollstein: Right.
Rovner: I know they didn’t do it, but they were talking about if women went particularly to Illinois, which is now one of these abortion havens, and came back, they would try to prosecute them, although that never really came to be.
Ollstein: Exactly. And so it’s interesting that even really conservative states with big Republican majorities, most have not gone down this road yet. And so I imagine a lot of them are watching how this case goes.
Rovner: Well, as long as we’re talking about states that start with “I,” let’s turn to Indiana, where Planned Parenthood reports that all of their appointments for abortions are taken between now and when that state’s near-total ban takes effect in a few weeks. This points out something I think often gets missed in these sort of score card maps of states that have bans and restrictions, which is there’s a lot of states where abortion is technically still legal but realistically not available, right?
Ollstein: The difference between being technically legal and available is nothing new. This was true prior to Dobbs as well. There were lots of states that only had one abortion clinic for the entire state. There were, like, six of those. And so, you know, you may have the right to have the procedure on paper, but if there’s only one place you could go and you’re not able to physically get there or they don’t have an appointment within the time window you need, you’re out of luck; that right isn’t, you know, meaningful for you. And so that’s becoming, you know, more true as abortion access is eliminated in a lot of the country and more and more people are depending on fewer and fewer states.
Rovner: And fewer and fewer clinics in fewer and fewer states. Well, finally, an update on the one-man nomination blockade by Alabama Republican Sen. Tommy Tuberville, who we talked about in March. He has stopped approval of basically all Defense Department personnel moves, including routine promotions, in protest of the Biden administration’s policy of providing leave and travel expenses for servicewomen to get abortions if they’re stationed in states where it’s illegal. Now, for the first time in more than 150 years, the Marine Corps has no approved commandant. Any idea which side’s going to back down here? Rachel, this is backing up the entire legislative calendar in the Senate, right?
Cohrs: It is. And I think some of the coverage this week has highlighted just how there hasn’t really been a willingness among Republican leadership to really put the pressure on Tuberville. But honestly, I don’t know when this stops for him. Having temporary leadership in all these positions isn’t kind of the impetus for him to say that he’s made his point. And I think there are also questions about — there may be more education required about exactly what the difference is between a temporary leader and a permanently installed leader. Obviously, the decisions that they’re making every day are life-and-death and are different than the leadership positions we see over at something like the NIH [National Institutes of Health], where, you know, I think it is —
Rovner: Which is also held up. But that’s another story.
Cohrs: Right, another story. But I just don’t see where this ends quite yet, unless there’s some will from Republican leadership to really bring him in line. And they just haven’t summoned that yet.
Rovner: I imagine there’ll be a vote on this when they get to the defense bill, right, which —the defense authorization, which is going to come up, I think, in both houses in the coming weeks. I mean, one would think that if there’s a vote and he loses, he might back down. I’m just guessing here. I guess we’ll have to wait and see what happens with that. All right. Well, it’s also been a busy couple of weeks in other social policy. On the one hand, a new federal law took effect that makes it easier for people to get accommodations to be able to do their jobs while pregnant. And Maine is going to start offering paid family and parental leave, although not until 2026. That makes it the 13th state to enact such a policy. On the other hand, Georgia is the first state to implement work requirements for Medicaid. Amy, the last time we discussed this, federal judges had tossed out Medicaid work requirements and Republicans in Congress were unsuccessful in getting those requirements back into the debt ceiling compromise. So how come Georgia gets to do this?
Goldstein: Well, I’ve begun to think of Medicaid work requirements as whack-a-mole, if you remember the arcade game in which you knock down an animal with a mallet only to have it pop up unexpectedly somewhere else. So, as you say, work requirements was something that Republicans were very eager to institute in 2017, 2018, when the Trump administration’s Center for Medicare & Medicaid Services encouraged states to adopt them. And there were basically plans to give people Medicaid at the time, mainly people in Medicaid expansion groups, if they worked or went to school or did community service for at least 80 hours a month. As you say, that was knocked down both by a district court and then a federal circuit court. And it looked like that was that, particularly when the Biden administration came along and undid the Trump administration’s regulation that had allowed states to submit proposals, the waivers for these kinds of plans. Well, lo and behold, Georgia said they wanted to do this. They said they wanted to do it in a little bit different way, because, for the first time ever, Georgia was going to be a partial expansion state for Medicaid, allowing people to get onto Medicaid if they had incomes up to the poverty level but not up to the full expansion poverty level that the ACA allows. And the Biden administration didn’t like that so much. And that partial expansion was to be twinned with work requirements. The Biden administration didn’t —
Rovner: For that expansion group, though, right? Not for everybody.
Goldstein: Just for that partial expansion group. The Biden administration didn’t like that so much. But last summer, a judge in Georgia said, no, she thinks this is OK. And the reason was that, unlike the other states, if this was pegged to a partial expansion, any expansion with work requirements would increase the number of people with Medicaid. So that was sort of in her judge judgment — I shouldn’t say the judge’s judgment — consistent with the purposes of the program. So Georgia has gone ahead, and the beginning of this month they allowed people to start enrolling in something called Georgia Pathways to Coverage. And we’ll have to see how it goes.
Rovner: Yeah. And just to be clear, I mean, Alice, you did some stellar work back a couple of years ago about Arkansas, about people losing coverage because of the work requirements, even if they were working, just because of how hard it was to report the work hours, right?
Ollstein: Absolutely. I mean, it’s kind of what we’re seeing now with the Medicaid unwinding, is that, you know, people just aren’t able to know what’s going on, aren’t able to be reached, fall through the cracks, can’t navigate the bureaucracy, and lose coverage that they should be entitled to. So we saw that happen, and I think to Amy’s point, the administration seems to be taking a very different stance on states like Arkansas, you know, which already had expanded Medicaid and then went to impose a work requirement, whereas Georgia didn’t have it before and this is kind of a compromise because it’s like, well, more people will be insured if we allow this to go forward total, you know, so maybe it’s better than nothing, although a lot of folks on the left are very opposed to the concept of work requirements, citing data that the people who are on Medicaid who can work are already working — the vast, vast, vast majority. And those who are not working, either they are caring for a child or someone with disability, or they themselves have a disability, or they’re a student. You know, there’s all these categories of why folks are unable to work.
Rovner: But in this expansion group, one would assume that if they’re earning up to the federal poverty line, they have some source of income. So one would assume that many of them are working. But I think it’ll be really interesting for researchers to watch to see, you know, a sort of a proof of concept in either direction with this.
Goldstein: And let me quickly mention a couple of things. Georgia’s rules are actually in some ways the same as what other states had tried to do previously. But in other ways, this is the strictest set of work requirements that anyone has tried in a couple of ways: People have to meet these work requirements up to age 64, which is older than other states had done for the most part. There’s also no exemption if you’re taking care of a child or taking care of an older family member. So how well people, in addition to the bureaucratic hoops that Alice was talking about, which are of grave concern to some of the people who oppose this in Georgia — there’s also a question of who’s going to actually be able to qualify for this.
Rovner: While we are on the subject of court decisions, one of the odd court decisions that I think has happened over the past few weeks is a federal district court decision out of Louisiana barring many officials in the Biden administration, including the surgeon general and the head of the CDC [Centers for Disease Control and Prevention], from talking to social media sites, particularly about things like medical misinformation. This feels like something I had not seen before in terms of actually trying to ban the administration from talking to private companies based on First Amendment concerns, which is what this is.
Cohrs: Right. Well, I mean, the First Amendment protects speech from interference from the government —
Rovner: Right
Cohrs: — which has always been, you know, this gray area with these independent platforms. And I think this issue, you know, has obviously become highly politicized. It came up several times when Rochelle Walensky, the former CDC director, was testifying on the Hill. So I think certainly we’ve seen this trend overall in these highly political court decisions and this strategy that certain litigants are taking where they’re trying to find defendants in a certain jurisdiction that’s going to be advantageous to them. So it will certainly be interesting to see how this plays out in the future and makes its way through the court system, but certainly is an eye-popping precedent. Like you mentioned, we don’t usually see something like this.
Rovner: And I wanted to mention, I think also because this is yet another of these judges that the right has found that are likely to agree with them. Like we’ve seen now: The judges in Texas, we now have one in Louisiana. Sort of kind of watch that docket. While we are still on the subject of courts, 2023 was the first year in the last decade or so that there was not a major health-related decision in the last big cases decided by the Supreme Court. But it seems like one of those non-health cases, the one essentially striking down affirmative action, might have some major implications for health care after all, particularly for medical education, right?
Cohrs: Yes. Some of my colleagues did some I think great follow-up reporting on this. And I think the idea is that there has been research that has shown that when patients are able to see a doctor of their same racial background, that it does have positive implications for their care. And there has also been studies of schools where there have been bans on race-conscious admissions showing that there is a decrease in medical school students from underrepresented backgrounds traditionally. And so I think that cause and effect is concerning for people, that if there are fewer medical students — there already aren’t a representative amount — from underrepresented groups, that could trickle down to, again, just exacerbating so many of these inequities that we see in health care provision. I know there was just a big study on the maternal mortality outcomes that came out recently as well. And I think all of these things are tied together. And I think Axios reported on one interesting potential loophole, was using proxy measures, like where someone went to school or their parents’ background, something like that, to try to ensure diversity from that lens. But I think it certainly is going to make these medical schools recalculate how they’re doing admissions and make some hard choices about how to maintain diversity that can be beneficial for patients.
Rovner: One thing that I think has come up in all of these discussions is the fact that the University of California-Davis has done an interesting job of creating a very diverse medical school class, even though race-conscious admissions have been banned in California for years. So I think a lot of schools are going to be looking sort of to see what UC Davis has done and perhaps emulate that. And I will put one of the UC Davis stories in the show notes for everybody. All right. Finally in this week’s news, the drug industry has filed a lawsuit challenging the Medicare drug price negotiation program that’s just now starting to get off the ground. Rachel, you wrote about this. How does pharma think it can block price-setting for Medicare that Medicare does for pretty much everything else that Medicare pays for? They set prices for hospitals and doctors and medical equipment. Why are drugmakers thinking that they’re special?
Cohrs: Right. So, again, this is four lawsuits as well, not just one: two from two trade groups and two drugmakers. And they’re each kind of using different arguments. But I think the big picture here is if the government called it price-setting, I don’t think pharma would have as much of an argument, but they’re calling it a negotiation. And I think one of the drugmakers’ key claims is that by signing these contracts to enter into this process, they’re tacitly admitting that this price that they come up with in this process is, quote-unquote, “fair.” And, you know, they don’t want to agree to that because then it makes the price that they’re charging everyone else look unfair on the other side of the coin. And I think there’s also these really high penalties for these companies who decide not to participate; I mean, tens of millions of dollars on the first day is the kind of number that we’re seeing for some of these companies that have filed lawsuits. And I think there’s also the option for them to take all of their drugs off of the market. But I think there’s a question with the timeline of whether they could have even done that before the law was passed. So the big picture from the drugmaker side of things is that the penalties are so high for them not to participate and that the government is framing this as a negotiation when it really is just price-setting, like Medicare does in so many other areas. So I think one interesting development that happened this week was that the [U.S.] Chamber of Commerce filed a motion for a preliminary injunction, which could make all of these lawsuits move much faster and really put a stop to the program. We hadn’t seen either of these lawsuits request a motion like that. And I think they requested a ruling by Oct. 1, which is when the first kind of round of 10 drugmakers would have had to sign their contracts with Medicare. So I think this certainly is picking up speed and urgency as we’re moving toward that Sept. 1 selection date.
Rovner: I didn’t even notice. Are these lawsuits all filed here in Washington, D.C., or —
Cohrs: No, they are not. As we’ve seen, the drugmakers are very strategic in where they filed. I think Merck did file in D.C., but the chamber filed in Ohio; it had some of their local chapters join in as well. I think we saw another company file in New Jersey. So I think they are kind of hedging their bets and trying to get rulings from as many different jurisdictions as they can.
Rovner: Find a judge who’s willing to slap an injunction on this whole thing.
Cohrs: Yes.
Rovner: Which we will talk about when and if it happens. All right. That is this week’s news, or at least as much as we have time to get to. Now, we will play my “Bill of the Month” interview with Bram Sable-Smith, and then we will be back with our extra credits. We are pleased to welcome back to the podcast Bram Sable-Smith, who reported and wrote the latest KFF Health News-NPR “Bill of the Month.” Bram, so nice to see you again.
Bram Sable-Smith: Always a pleasure to be here.
Rovner: So, this month’s patient was, like a lot of young people, an uninsured 23-year-old when she ended up in the emergency room. Tell us who she is and what kind of medical care she needed and got.
Sable-Smith: Yeah, that’s right. Her name was Bethany Birch. And, in addition to being uninsured, she was also unemployed at the time, and she had had pain in her diaphragm for eight months. It prevented her from eating. She lost about 25 pounds in that time. And when she went to the emergency room, she found out she needed her gallbladder removed.
Rovner: And got it, right?
Sable-Smith: And got it. Yeah, she got that surgery almost immediately. Because she hadn’t been eating food — her food resistance — it meant she could get in for surgery right away.
Rovner: And that cured her? Yes?
Sable-Smith: It did cure her. Yes, she felt a lot better.
Rovner: So now we’re talking about the bill. The hospital tried to send her the bill, but apparently it couldn’t find her. Is this a common thing, and why couldn’t they find her? One presumes she gave them an address when she presented at the emergency room.
Sable-Smith: She did give them an address, but by the time she was discharged, she had lost her housing. Her home situation was unstable. So just that brief visit to the hospital, by the time she left, she had no more house to live in. And she did end up crashing with her family for several months. And, eventually, she did update her address with the post office. But by the time she had done that, it was after the hospital had sent the three bills to her for her visit.
Rovner: So the hospital doesn’t get any response, and they do what we know hospitals do. They sued for nonpayment. And the debt collection firm did manage to find her. So then what happened?
Sable-Smith: Well, she went to court, and like so many people who end up in court with medical debt, she did not have a lawyer representing her. She met with a representative from the debt collection firm, and she worked out a payment plan to pay her bill, plus court costs, in $100 monthly installments. But at the time, Tennessee had a default interest rate on judgments like the one that Bethany had of 7%. So the judge tacked on a 7% interest rate to her bill.
Rovner: So, yeah, and that was presumably a lot for her to carry. What finally happened with the bill?
Sable-Smith: Well, she paid her $100 monthly payments for over four years. It totaled about $5,200 she paid in that time. But at the same time, the interest rate was accruing. And so she owed an additional $2,700 on top of the initial bill that she had gotten. From her perspective, it was just impossible. She wasn’t digging out of this debt. So she started getting help from a family friend, who’s a billing expert, who took on her case. They asked the hospital and the debt collection firm to settle her debt because she had already paid so much. But they were unsuccessful in doing so. They sent their bill to us. We started reporting the story. Then they asked again to settle her debt by paying an additional $100 on top of what she had already paid. And this time they agreed. And so she settled her debt and she got a balance-zero statement.
Rovner: Amazing how just one phone call from us can do some work. Now, as somebody who is unemployed and, as you pointed out, uninsured at the time she got the care, Bethany should have been eligible for the hospital’s financial assistance policy. Why didn’t she get help before the debt ballooned with court costs and all that interest?
Sable-Smith: Well, the simple answer is that she never applied. But, as we know, it’s much more complicated than that. So given her status as single, uninsured, unemployed, it’s very possible that she would have qualified for financial help, maybe even for free care altogether. But the onus was on her as a patient to apply. And we know her situation was unstable. You know, she went through a period of homelessness. She didn’t have a lot of expendable money at the time. It’s a long process to apply for these programs. There’s a lot of forms. It can be cumbersome. And that prevents a lot of people from applying to these programs. So advocates push for something called presumptive eligibility, where the hospital takes the onus of applying away from patients and they automatically put them through the process. And this hospital that Bethany went to, they actually have switched to that presumptive eligibility model, just not in time to help her case.
Rovner: So what’s the takeaway here? I guess everybody has to be a proactive patient, not just with your medical care, but especially with your bills. What happens to a patient who finds themselves in a similar situation?
Sable-Smith: Well, you know, from a consumer standpoint like that, one takeaway is to ask for financial help. A lot more people qualify than you might think. You might not think you qualify, but it’s very possible you could. And then from a policy perspective, hospitals switching to presumptive eligibility — that’s something that they’re able to do. And also, some states have pushed to ban or even limit interest payments on this kind of medical debt. So that’s something that other people are considering as well.
Rovner: Or you can write to us, and we will show you how in our show notes.
Sable-Smith: That’s always a possibility, too.
Rovner: Bram Sable-Smith, thank you so much.
Sable-Smith: Yeah, thanks for having me.
Rovner: OK, we’re back, and it’s time for our extra credit segment. That’s when we each recommend a story we read this week we think you should read too. As always, don’t worry if you miss it. We will post the links on the podcast page at kffhealthnews.org and in our show notes on your phone or other mobile device. Rachel, why don’t you go first?
Cohrs: OK, I’m cheating a little bit and I’m doing a double feature. So the first story for my extra credit is headlined “How Often Do Health Insurers Say No to Patients? No One Knows.” It’s in ProPublica by Robin Fields, and I think it’s just a great feature on the idea that Obamacare entitled the government and patients to more information about how often insurers deny care to patients. And the government hasn’t really pursued that information. And even, like, state health insurance commissions aren’t providing the information they’re collecting. And Robin just had such a difficult time getting any sort of information from anyone, even though we’re legally entitled to it. So I thought that was just kind of a great highlight of this next area of criticism of the health insurance industry, which, and I think that —
Rovner: I would say, all this focus on premiums and not as much focus on what you actually get for those premiums.
Cohrs: Exactly. So true. I think there’ve been some high-profile examples, great reporting. And I thought that meshed well with some reporting from my colleagues Casey Ross and Bob Herman, who wrote a follow-up to some of their prior reporting titled “How UnitedHealth’s Acquisition of a Popular Medicare Advantage Algorithm Sparked Internal Dissent Over Denied Care.” Again, looking at how algorithms in this one privatized Medicare program, which is growing in size and enrollment across the country, was actually overruling clinicians’ decisions about how long patients should be receiving care in facilities. And if the algorithm says they should be done, then they’re done. And I think it definitely sparked some concerns from people in the company who were willing to speak to them just because they were so concerned about this trend.
Rovner: Alice.
Ollstein: I have a very impressive investigation from The Wall Street Journal. There are five bylines, and we will post the link. This is about lead-covered telecom cables owned by AT&T, Verizon, other companies that have been left to decay and leach into the environment all around the country. This documents how the companies knew about them but have not moved to clean them up and get rid of them. They are impacting water sources. They are near playgrounds where children are, and it goes into the very disturbing health impacts of lead exposure. This is something the country has made a lot of progress on when it comes to paint and other sources, but obviously we still have a long way to go.
Rovner: Yeah, because there’s not enough things to be worried about environmentally, here is something else. It is very good reporting.
Rovner: Amy.
Goldstein: My extra credit this week is from The New York Times, by Reed Abelson, with the headline “Medicare Advantage Plans Offer Few Psychiatrists.” And this isn’t a giant story, but I think it is at the nexus of two very important questions: one, the long-standing question of whether privatized Medicare is better or worse for people who are older Americans on Medicare than the traditional version of Medicare; and the question of are people getting enough access to mental health care? And I guess what struck me is that there’s been so much attention lately to the question of access to mental health services for younger Americans, and this looked at the question of access to mental health services for older Americans. And what this story, based on a study, talks about is that the study found that more than half of the counties, the researchers who did this study found, is that those counties did not have a single psychiatrist participating in Medicare Advantage and that a lot of these plans have what’s called “narrow” or “skinny” networks, where a very small fraction of the available psychiatrists in a community were in that plan’s network. Now, [there are] people who are criticizing that study saying, well, you can’t look at just psychiatrists; there are other people who provide competent mental health care. But I think it just raises the question of who is getting what they need.
Rovner: Indeed. Well, my story this week is also about just plain good reporting. It’s called “Doctor Lands in the Doghouse After Giving Covid Vaccine Waivers Too Freely.” It’s by Brett Kelman of KFF Health News. But it’s about some old-fashioned reporting by another outlet, Nashville’s NewsChannel 5. It seemed that during the height of the covid vaccine rollout, when lots of places were requiring proof of vaccines and lots of people didn’t want to get them, the doctor in question, named Robert Coble, was providing waivers through a website without much —OK, any — oversight. How did they prove it? By obtaining a waiver for a reporter’s black Labrador retriever, Charlie. Earlier this spring, Coble quietly surrendered his medical license to the state Department of Health. Journalism works. OK, that is our show for this week. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left us a review; that helps other people find us too. Special thanks, as always, to our producer, Francis Ying. Also as always, you can email us your comments or questions. We’re at whatthehealth@kff.org. Or you can still tweet me. I’m @jrovner. I’m on Threads too, @julie.rovner.
Rovner: Amy.
Goldstein: I’m @goldsteinamy.
Rovner: Rachel.
Cohrs: I’m @rachelcohrs on Twitter and @rachelcohrsreporter on Threads.
Rovner: Alice.
Ollstein: @AliceOllstein.
Rovner: We will be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ ‘What the Health?’ on Spotify, Apple Podcasts, Stitcher, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
2 years 3 months ago
Courts, Health Care Costs, Health Industry, Insurance, Medicaid, Medicare, Multimedia, Biden Administration, Contraception, Drug Costs, FDA, KFF Health News' 'What The Health?', Podcasts, Pregnancy, Women's Health