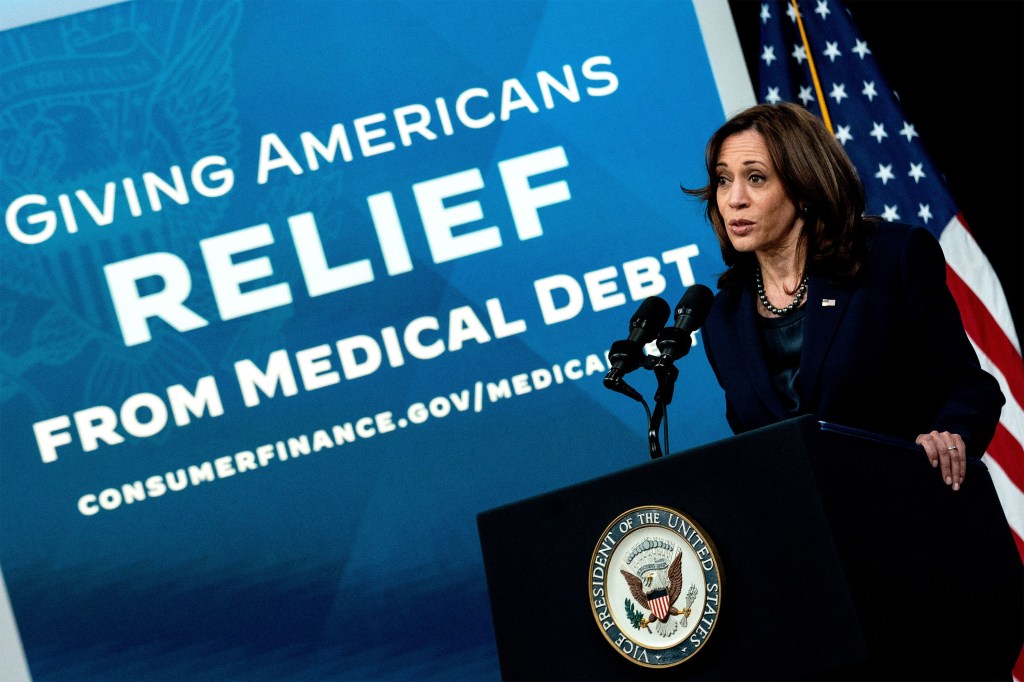
Harris apoya la reducción de la deuda médica. Los “conceptos” de Trump preocupan a defensores.
Defensores de pacientes y consumidores confían en que Kamala Harris acelere los esfuerzos federales para ayudar a las personas que luchan con deudas médicas, si gana en las elecciones presidenciales del próximo mes.
Y ven a la vicepresidenta y candidata demócrata como la mejor esperanza para preservar el acceso de los estadounidenses a seguros de salud. La cobertura integral que limita los costos directos de los pacientes es la mejor defensa contra el endeudamiento, dicen los expertos.
La administración Biden ha ampliado las protecciones financieras para los pacientes, incluyendo una propuesta histórica de la Oficina de Protección Financiera del Consumidor (CFPB) para eliminar la deuda médica de los informes de crédito de los consumidores.
En 2022, el presidente Joe Biden también firmó la Ley de Reducción de la Inflación, que limita cuánto deben pagar los afiliados de Medicare por medicamentos recetados, incluyendo un tope de $35 al mes para la insulina. Y en legislaturas de todo el país, demócratas y republicanos han trabajado juntos de manera discreta para promulgar leyes que frenen a los cobradores de deudas.
Sin embargo, defensores dicen que el gobierno federal podría hacer más para abordar un problema que afecta a 100 millones de estadounidenses, obligando a muchos a trabajar más, perder sus hogares y reducir el gasto en alimentos y otros artículos esenciales.
“Biden y Harris han hecho más para abordar la crisis de deuda médica en este país que cualquier otra administración”, dijo Mona Shah, directora senior de política y estrategia en Community Catalyst, una organización sin fines de lucro que ha liderado los esfuerzos nacionales para fortalecer las protecciones contra la deuda médica. “Pero hay más por hacer y debe ser una prioridad para el próximo Congreso y administración”.
Al mismo tiempo, los defensores de los pacientes temen que si el ex presidente Donald Trump gana un segundo mandato, debilitará las protecciones de los seguros permitiendo que los estados recorten sus programas de Medicaid o reduciendo la ayuda federal para que los estadounidenses compren cobertura médica. Eso pondría a millones de personas en mayor riesgo de endeudarse si enferman.
En su primer mandato, Trump y los republicanos del Congreso intentaron en 2017 derogar la Ley de Cuidado de Salud a Bajo Precio (ACA), un movimiento que, según analistas independientes, habría despojado de cobertura médica a millones de estadounidenses y habría aumentado los costos para las personas con afecciones preexistentes, como diabetes y cáncer.
Trump y sus aliados del Partido Republicano continúan atacando a ACA, y el ex presidente ha dicho que quiere revertir la Ley de Reducción de la Inflación, que también incluye ayuda para que los estadounidenses de bajos y medianos ingresos compren seguros de salud.
“Las personas enfrentarán una ola de deuda médica por pagar primas y precios de medicamentos recetados”, dijo Anthony Wright, director ejecutivo de Families USA, un grupo de consumidores que ha apoyado las protecciones federales de salud. “Los pacientes y el público deberían estar preocupados”.
La campaña de Trump no respondió a consultas sobre su agenda de salud. Y el ex presidente no suele hablar de atención médica o deuda médica en la campaña, aunque dijo en el debate del mes pasado que tenía “conceptos de un plan” para mejorar la ACA. Trump no ha ofrecido detalles.
Harris ha prometido repetidamente proteger ACA y renovar los subsidios ampliados para las primas mensuales del seguro creados por la Ley de Reducción de la Inflación. Esa ayuda está programada para expirar el próximo año.
La vicepresidenta también ha expresado su apoyo a un mayor gasto gubernamental para comprar y cancelar deudas médicas antiguas de los pacientes. En los últimos años, varios estados y ciudades han comprado deuda médica en nombre de sus residentes.
Estos esfuerzos han aliviado la deuda de cientos de miles de personas, aunque muchos defensores dicen que cancelar deudas antiguas es, en el mejor de los casos, una solución a corto plazo, ya que los pacientes seguirán acumulando facturas que no pueden pagar sin una acción más sustantiva.
“Es un bote con un agujero”, dijo Katie Berge, una cabildera de la Sociedad de Leucemia y Linfoma. Este grupo de pacientes fue una de más de 50 organizaciones que el año pasado enviaron cartas a la administración Biden instando a las agencias federales a tomar medidas más agresivas para proteger a los estadounidenses de la deuda médica.
“La deuda médica ya no es un problema de nicho”, dijo Kirsten Sloan, quien trabaja en política federal para la Red de Acción contra el Cáncer de la Sociedad Americana de Cáncer. “Es clave para el bienestar económico de millones de estadounidenses”.
La Oficina de Protección Financiera del Consumidor está desarrollando regulaciones que prohibirían que las facturas médicas aparezcan en los informes de crédito de los consumidores, lo que mejoraría los puntajes crediticios y facilitaría que millones de estadounidenses alquilen una vivienda, consigan un trabajo o consigan un préstamo para un automóvil.
Harris, quien ha calificado la deuda médica como “crítica para la salud financiera y el bienestar de millones de estadounidenses”, apoyó con entusiasmo la propuesta de regulación. “No se debería privar a nadie del acceso a oportunidades económicas simplemente porque experimentó una emergencia médica”, dijo en junio.
El compañero de fórmula de Harris, el gobernador de Minnesota, Tim Walz, quien ha dicho que su propia familia luchó con la deuda médica cuando era joven, firmó en junio una ley estatal que reprime el cobro de deudas.
Los funcionarios de la CFPB dijeron que las regulaciones se finalizarán a principios del próximo año. Trump no ha indicado si seguiría adelante con las protecciones contra la deuda médica. En su primer mandato, la CFPB hizo poco para abordarla, y los republicanos en el Congreso han criticado durante mucho tiempo a la agencia reguladora.
Si Harris gana, muchos grupos de consumidores quieren que la CFPB refuerce aún más las medidas, incluyendo una mayor supervisión de las tarjetas de crédito médicas y otros productos financieros que los hospitales y otros proveedores médicos han comenzado a ofrecer a los pacientes. Por estos préstamos, las personas están obligadas a pagar intereses adicionales sobre su deuda médica.
“Estamos viendo una variedad de nuevos productos financieros médicos”, dijo April Kuehnhoff, abogada senior del Centro Nacional de Derecho del Consumidor. “Estos pueden generar nuevas preocupaciones sobre las protecciones al consumidor, y es fundamental que la CFPB y otros reguladores supervisen a estas empresas”.
Algunos defensores quieren que otras agencias federales también se involucren.
Esto incluye al enorme Departamento de Salud y Servicios Humanos (HHS), que controla cientos de miles de millones de dólares a través de los programas de Medicare y Medicaid. Ese dinero otorga al gobierno federal una enorme influencia sobre los hospitales y otros proveedores médicos.
Hasta ahora, la administración Biden no ha utilizado esa influencia para abordar la deuda médica.
Pero en un posible anticipo de futuras acciones, los líderes estatales en Carolina del Norte recientemente obtuvieron la aprobación federal para una iniciativa de deuda médica que obligará a los hospitales a tomar medidas para aliviar las deudas de los pacientes a cambio de ayuda gubernamental. Harris elogió la iniciativa.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 1 week ago
Elections, Health Care Costs, Health Industry, Insurance, Noticias En Español, States, Biden Administration, Diagnosis: Debt, Investigation, Obamacare Plans, Trump Administration
Happening in Springfield: New Immigrants Offer Economic Promise, Health System Challenges
When Republican vice presidential candidate JD Vance claimed Haitian immigrants had caused infectious-disease rates to “skyrocket” in Springfield, Ohio, local health commissioner Chris Cook checked the records.
They showed that in 2023, for example, there were four active tuberculosis cases in Clark County, which includes Springfield, up from three in 2022. HIV cases had risen, but sexually transmitted illnesses overall were decreasing.
“I wouldn’t call it skyrocketing,” said Cook, noting that there were 190 active cases in 2023 in all of Ohio. “You hear the rhetoric. But as a whole, reportable infectious diseases to the health department are decreasing.”
Tensions are running high in this industrial town of about 58,000 people. Bomb threats closed schools and public buildings after GOP presidential nominee Donald Trump falsely claimed that Haitian immigrants — who he alleged were there illegally — were stealing and eating household pets. City and county officials disputed the claims the former president levied during his Sept. 10 debate with Vice President Kamala Harris, his Democratic opponent.
Trump was amplifying comments made by Vance that — along with his claims about the immigration status of this population — were broadly panned as false. When asked during a CNN interview about the debunked pet-eating rumor, Vance, a U.S. senator from Ohio, acknowledged that the image he created was based not on facts but on “firsthand accounts from my constituents.” He said he was willing “to create” stories to focus attention on how immigration can overrun communities.
But Ohio Gov. Mike DeWine, also a Republican, has said immigrants have been an economic boon to Springfield. Many began arriving because businesses in the town, which had seen its population decrease, needed labor.
Largely lost in the political rancor is the way Springfield and the surrounding area responded to the influx of Haitian immigrants. Local health institutions tried to address the needs of this new population, which had lacked basic public health care such as immunization and often didn’t understand the U.S. health system.
The town is a microcosm of how immigration is reshaping communities throughout the United States. In the Springfield area, Catholic charities, other philanthropies, volunteers, and county agencies have banded together over the past three to four years to tackle the challenge and connect immigrants who have critical health needs with providers and care.
For instance, a community health center added Haitian Creole interpreters. The county health department opened a refugee health testing clinic to provide immunizations and basic health screenings, operating on such a shoestring budget that it’s open only two days a week.
And a coalition of groups to aid the Haitian community was created about two years ago to identify and respond to immigrant community needs. The group meets once a month with about 55 or 60 participants. On Sept. 18, about a week after Trump ramped up the furor at the debate, a record 138 participants joined in.
“We have all learned the necessity of collaboration,” said Casey Rollins, director of Springfield’s St. Vincent de Paul, a nonprofit Catholic social services organization that has become a lifeline for many of the town’s Haitian immigrants. “There’s a lot of medical need. Many of the people have high blood pressure, or they frequently have diabetes.”
Several factors have led Haitians to leave their Caribbean country for the United States, including a devastating earthquake in 2010, political unrest after the 2021 assassination of Haiti’s president, and ongoing gang violence. Even when health facilities in the country are open, it can be too treacherous for Haitians to travel for treatment.
“The gangs typically leave us alone, but it’s not a guarantee,” said Paul Glover, who helps oversee the St. Vincent’s Center for children with disabilities in Haiti. “We had a 3,000-square-foot clinic. It was destroyed. So was the X-ray machine. People have been putting off health care.”
An estimated 12,000 to 15,000 Haitian immigrants live in Clark County, officials said. About 700,000 Haitian immigrants lived in the United States in 2022, according to U.S. Census data.
Those who have settled in the Springfield area are generally in the country legally under a federal program that lets noncitizens temporarily enter and stay in the United States under certain circumstances, such as for urgent humanitarian reasons, according to city officials.
The influx of immigrants created a learning curve for hospitals and primary care providers in Springfield, as well as for the newcomers themselves. In Haiti, people often go directly to a hospital to receive care for all sorts of maladies, and county officials and advocacy groups said many of the immigrants were unfamiliar with the U.S. system of seeing primary care doctors first or making appointments for treatment.
Many sought care at Rocking Horse Community Health Center, a nonprofit, federally qualified health center that provides mental health, primary, and preventive care to people regardless of their insurance status or ability to pay. Federally qualified health centers serve medically underserved areas and populations.
The center treated 410 patients from Haiti in 2022, up more than 250% from 115 in 2021, according to Nettie Carter-Smith, the center’s director of community relations. Because the patients required interpreters, visits often stretched twice as long.
Rocking Horse hired patient navigators fluent in Haitian Creole, one of the two official languages of Haiti. Its roving purple bus provides on-site health screenings, vaccinations, and management of chronic conditions. And this school year, it’s operating a $2 million health clinic at Springfield High.
Many Haitians in Springfield have reported threats since Trump and Vance made their town a focus of the campaign. Community organizations were unable to identify any immigrants willing to be interviewed for this story.
Hospitals have also felt the impact. Mercy Health’s Springfield Regional Medical Center also saw a rapid influx of patients, spokesperson Jennifer Robinson said, with high utilization of emergency, primary care, and women’s health services.
This year, hospitals also have seen several readmissions for newborns struggling to thrive as some new mothers have trouble breastfeeding or getting supplemental formula, county officials said. One reason: New Haitian immigrants must wait six to eight weeks to get into a program that provides supplemental food for low-income pregnant, breastfeeding, or non-breastfeeding postpartum women, as well as for children and infants.
At Kettering Health Springfield, Haitian immigrants come to the emergency department for nonemergency care. Nurses are working on two related projects, one focusing on cultural awareness for staff and another exploring ways to improve communication with Haitian immigrants during discharge and in scheduling follow-up appointments.
Many of the immigrants are able to get health insurance. Haitian entrants generally qualify for Medicaid, the state-federal program for the low-income and disabled. For hospitals, that means lower reimbursement rates than with traditional insurance.
During 2023, 60,494 people in Clark County were enrolled in Medicaid, about 25% of whom were Black, according to state data. That’s up from 50,112 in 2017, when 17% of the enrollees were Black. That increase coincides with the rise of the Haitian population.
In September, DeWine pledged $2.5 million to help health centers and the county health department meet the Haitian and broader community’s needs. The Republican governor has pushed back on the recent national focus on the town, saying the spread of false rumors has been hurtful for the community.
Ken Gordon, a spokesperson for the Ohio Department of Health, acknowledged the difficulties Springfield’s health systems have faced and said the department is monitoring to avert potential outbreaks of measles, whooping cough, and even polio.
People diagnosed with HIV in the county increased from 142 residents in 2018 to 178 to 2022, according to state health department data. Cook, the Clark County health commissioner, said the data lags by about 1.5 years.
But Cook said, “as a whole, all reportable infections to the health department are not increasing.” Last year, he said, no one died of tuberculosis. “But 42 people died of covid.”
Healthbeat is a nonprofit newsroom covering public health published by Civic News Company and KFF Health News. Sign up for its newsletters here.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 2 weeks ago
Elections, Health Industry, Public Health, Race and Health, States, Healthbeat, Immigrants, Ohio
Employers Haven’t a Clue How Their Drug Benefits Are Managed
Most employers have little idea what the pharmacy benefit managers they hire do with the money they exchange for the medications used by their employees, according to a KFF survey released Wednesday morning.
Most employers have little idea what the pharmacy benefit managers they hire do with the money they exchange for the medications used by their employees, according to a KFF survey released Wednesday morning.
In KFF’s latest employer health benefits survey, company officials were asked how much of the rebates collected from drugmakers by pharmacy benefit managers, or PBMs, is returned to them. In recent years, the pharmaceutical industry has tried to deflect criticism of high drug prices by saying much of that income is siphoned off by the PBMs, companies that manage patients’ drug benefits on behalf of employers and health plans.
PBM leaders say they save companies and patients billions of dollars annually by obtaining rebates from drugmakers that they pass along to employers. Drugmakers, meanwhile, say they raise their list prices so high in order to afford the rebates that PBMs demand in exchange for placing the drugs on formularies that make them available to patients.
Leaders of the three largest PBMs — CVS Caremark, Optum RX and Express Scripts — all testified in Congress in July that 95% to 98% of the rebates they collect from drugmakers flow to employers.
For KFF’s survey of 2,142 randomly selected companies, officials from those with 500 or more employees were asked how much of the rebates negotiated by PBMs returned to the company as savings. About 19% said they received most of the rebates, 27% said some, and 16% said little. Thirty-seven percent of the respondents didn’t know.
While a larger percentage of officials from the largest companies said they got most or some of the rebates, the answers — and their contrast with the testimony of PBM leaders — reflect the confusion or ignorance of employers about what their drug benefit managers do, said survey leader Gary Claxton, a senior vice president at KFF, a health information nonprofit that includes KFF Health News.
“I don’t think they can ever know all the ways the money moves around because there are so many layers, between the wholesalers and the pharmacies and the manufacturers,” he said.
Critics say big PBMs — which are parts of conglomerates that include pharmacies, providers, and insurers — may conceal the size of their rebates by conducting negotiations through corporate-controlled rebate aggregators, or group purchasers, mostly based overseas in tax havens, that siphon off a percentage of the cash before it goes on the PBMs’ books.
PBMs also make money by encouraging or requiring patients to use affiliated specialty pharmacies, by skimping on payments to other pharmacies, and by collecting extra cash from drug companies through the federal 340B drug pricing program, which is aimed at lowering drug costs for low-income patients, said Antonio Ciaccia, CEO of 46brooklyn Research.
The KFF survey indicates how little employers understand the PBMs and their pricing policies. “Employers are generally frustrated by the lack of transparency into all the prices out there,” Claxton said. “They can’t actually know what’s true.”
Billionaire Mark Cuban started a company to undercut the PBMs by selling pharmaceuticals with transparent pricing policies. He tells Fortune 500 executives he meets, “You’re getting ripped off, you’re losing money because it’s not your core competency to understand how your PBM and health insurance contracts work,” Cuban told KFF Health News in an interview Tuesday.
Ciaccia, who has conducted PBM investigations for several states, said employers are not equipped to understand the behavior of the PBMs and often are surprised at how unregulated the PBM business is.
“You’d assume that employers want to pay less, that they would want to pay more attention,” he said. “But what I’ve learned is they are often underequipped, underresourced, and oftentimes not understanding the severity of the lack of oversight and accountability.”
Employers may assume the PBMs are acting in their best interest, but they don’t have a legal obligation to do so.
Prices can be all over the map, even those charged by the same PBM, Ciaccia said. In a Medicaid study he recently conducted, a PBM was billing employers anywhere from $2,000 to $8,000 for a month’s worth of imatinib, a cancer drug that can be bought as a generic for as little as $30.
PBM contracts often guarantee discounts of certain percentage points for generics and brand-name drugs. But the contracts then contain five pages of exclusions, and “no employer will know what they mean,” Ciaccia said. “That person doesn’t have enough information to have an informed opinion.”
The KFF survey found that companies’ annual premiums for coverage of individual employees had increased from an average of $7,739 in 2021 to $8,951 this year, and $22,221 to $25,572 for families. Among employers’ greatest concerns was how to cover increasingly popular weight loss drugs that list at $2,000 a month or more.
Only 18% of respondents said their companies covered drugs such as Wegovy for weight loss. The largest group of employers offering such coverage — 28% — was those with 5,000 or more employees.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 2 weeks ago
Health Care Costs, Health Industry, Insurance, Pharmaceuticals, Drug Costs, Prescription Drugs
Calif. Ballot Measure Targets Drug Discount Program Spending
Californians in November will weigh in on a ballot initiative to increase scrutiny over the use of health-care dollars — particularly money from a federal drug discount program — meant to support patient care largely for low-income or indigent people.
Californians in November will weigh in on a ballot initiative to increase scrutiny over the use of health-care dollars — particularly money from a federal drug discount program — meant to support patient care largely for low-income or indigent people. The revenue is sometimes used to address housing instability and homelessness among vulnerable patient populations.
Voters are being asked whether California should increase accountability in the 340B drug discount program, which provides money for community clinics, safety net hospitals and other nonprofit health-care providers.
The program requires pharmaceutical companies to give drug discounts to these clinics and nonprofit entities, which can bank revenue by charging higher reimbursement rates.
Advocates pushing the measure, Proposition 34, say some entities are using the drug discount program as a slush fund, plowing money into housing and homelessness initiatives that don’t meet basic patient safety standards. Researchers and advocates have called for greater oversight.
“There are 340B entities that are misusing these public dollars,” said Nathan Click, a spokesperson for the pro-Proposition 34 campaign. “The whole point of this program is to use this money to get more low-income people health-care services.”
The initiative wouldn’t bar 340B providers from using health-care funds for housing or homelessness programs. Instead, it targets providers that spend more than $100 million on purposes other than direct patient care over 10 years. It would mandate that 98 percentof 340B revenues go to direct patient care. It also targets 340B providers with health insurer contracts and pharmacy licenses and those serving low-income Medicaid or Medicare patients that have been dinged with at least 500 high-severity housing violations for substandard or unsafe conditions.
That has placed a bull’s eye on the Los Angeles-based AIDS Healthcare Foundation, a nonprofit that provides direct patient care via clinics and pharmacies in California and other states, including Illinois, Texas and New York. It also owns housing for low-income and homeless people.
A Los Angeles Times investigation found that many residents of AIDS Healthcare Foundation properties are living in deplorable, unhealthy conditions.
Michael Weinstein, the foundation’s president, disputes those claims and argues that Proposition 34 proponents, including real estate interests, are going after him for another ballot initiative that seeks to implement rent control in more communities across California.
“It’s a revenge initiative,” Weinstein said, arguing that the deep-pocketed California Apartment Association is targeting his foundation — and its health and housing operations — because it has backed ballot measures pushing rent control across California. “This is a two-pronged attack against us to defeat rent control.”
Weinstein is locked in a feud with the apartment association, the chief sponsor of the initiative, which has contributed handsomely to pass Proposition 34. Opponents argue that the initiative is “a wolf in sheep’s clothing.”
Weinstein acknowledged to KFF Health News that his nonprofit uses money from 340B drug discounts to support its housing initiatives but argued they are helping treat and house some of the most vulnerable people, who would otherwise be homeless.
The apartment association declined several requests for comment. But Proposition 34 backers say they aren’t going after rent control — or Weinstein and his nonprofit.
Supporters argue that “rising health care costs are squeezing millions of Californians” and say that the initiative would “give California patients and taxpayers much needed relief, and lowers state drug costs, while saving California taxpayers billions.”
If the initiative passes and 340B providers do not spend 98 percent of the revenue on direct patient care, they could lose their license to practice health care and their nonprofit status.
This article is not available for syndication due to republishing restrictions. If you have questions about the availability of this or other content for republication, please contact NewsWeb@kff.org.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 2 weeks ago
california, Elections, Health Care Costs, Health Industry, Pharmaceuticals, States, Drug Costs, Health Brief
An Arm and a Leg: Don’t Get ‘Bullied’ Into Paying What You Don’t Owe
Caitlyn Mai thought she did everything right. She called ahead to make sure her insurer would cover her cochlear implant surgery. She thought everything went according to plan but she still got a bill for the full cost of the surgery: more than $139,000.
What Caitlyn did next is a reminder of why a beloved former guest once said you should “never pay the first bill.” This episode of “An Arm and a Leg” is an extended version of the July installment of the “Bill of the Month” series, created in partnership with NPR.
Dan Weissmann
Host and producer of "An Arm and a Leg." Previously, Dan was a staff reporter for Marketplace and Chicago's WBEZ. His work also appears on All Things Considered, Marketplace, the BBC, 99 Percent Invisible, and Reveal, from the Center for Investigative Reporting.
Credits
Emily Pisacreta
Producer
Claire Davenport
Producer
Adam Raymonda
Audio wizard
Ellen Weiss
Editor
click to open the transcript
Don’t Get ‘Bullied’ Into Paying What You Don’t Owe
Dan: Hey there —
One morning when she was in eighth grade, Caitlin Mai did what she always did when she woke up.
Caitlyn Mai: Music has always been a big part of my life. And so I immediately put in my headphones and started putting on music as I was about to get out of bed and get ready. And I noticed my earbud in my right ear wasn’t working.
Dan: It was obvious, because on this Beatles tune she’d cued up, Eleanor Rigby, the vocals are almost all on the right-hand side, and she couldn’t hear them.
Caitlyn: I was like, that’s kind of weird. So I switched the earbuds and it worked fine. But then it was, the other one wasn’t working in my right ear. And I was like, what?
Dan: Yeah, confusing. And then she tried getting out of bed.
Caitlyn: I was so dizzy. It was my first time experiencing vertigo, and it was so severe, I couldn’t walk across the room without getting severely motion sick.
Dan: With that vertigo, Caitlin could barely walk at all. She had no sense of balance — that actually relies on a mechanism inside our ears. Later, doctors found she had lost 87 percent of her hearing on the right side.
Caitlyn: They think I just had some sort of virus that settled in my ear, and it damaged my ear. But I went to bed completely healthy the night before. Woke up, couldn’t hear out of my ear.
Dan: She had to learn how to walk all over again.
Caitlyn: I have to rely on my eyes. My friends still find it hilarious if I close my eyes, I fall over.
Dan: That was eighth grade. Caitlyn made it through high school, in Tulsa where she grew up without a lot of accommodations.
Caitlyn: Cause in middle school, early high school, you don’t want to bring attention to your disability. At least I really didn’t want to at the time. I was super anxious about that.
Dan: Catilyn’s 27 now, she works as a legal assistant in Oklahoma City. Her husband’s a lawyer. And for the longest time, she couldn’t access a tool that helps restore hearing for lots of people: Cochlear implants — small devices that stimulate nerves inside the ear.
The FDA didn’t approve them for just one ear until a couple of years ago. Last year, Caitlin got her insurance to approve one for her. She had surgery in December to insert the implant. And in January, an audiologist attached an external component to switch on Caitlin’s right-side hearing.
Caitlyn: She said, okay, at some point, you’re gonna start hearing some beeps, just say yes when you can hear them. And my husband said my face just, out of nowhere, lit up, and I go, yes! It was streaming directly to my cochlear implant. And I definitely started tearing up.
Dan: Then, two weeks later, Caitlin got an alert from the hospital on her phone.
Caitlyn: And I open it up, and I immediately started having a panic attack.
Dan: It was a bill for a hundred and thirty-nine thousand dollars. The full amount for Caitlin’s surgery.
Which, given that Caitlyn had gotten her insurance company’s OK for the procedure in advance, was a pretty big surprise. NPR featured Caitlyn’s story recently for a series they do with our pals at KFF Health News.
NPR HOST: Time now for the latest installment in our bill of the month series, where we dissect and explain confusing or outrageous medical bills.
Dan: I interviewed Caitlyn for that story. And we’re bringing you an expanded version here because Caitlin’s situation — well, it was a good story. And it made me curious about a couple things.
It also reminded me of some good advice we’ve heard here before — and it reminded me of an important colleague and teacher. And the bottom line to Caitlyn’s story? Stand up for yourself. Don’t cave. Make the next call.
This is An Arm and a Leg — a show about why health care costs so freaking much, and what we can maybe do about it. I’m Dan Weissmann. I’m a reporter, and I like a challenge — so our job on this show is to take one of the most enraging, terrifying, depressing parts of American life, and bring you something entertaining, empowering, and useful.
To get her insurance company’s approval, Caitlyn had already spent a lot of time — and a lot of money — in the months before surgery. For instance …
Caitlyn: To prove to insurance that a hearing aid wouldn’t work had to be fitted for a hearing aid and then do a couple hours of testing to prove, yep, it doesn’t help.
Dan: There were reviews with audiologists, with her surgeon, and an MRI to make sure there wasn’t too much scar tissue for an implant to take.
Caitlyn: That took a long time to get scheduled, get insurance to approve, pay for, then get back for another appointment. I counted up at one point — it’s like around eight or ten appointments that I had before the final, okay, let’s schedule surgery.
Dan: And — you caught that, right? Where she mentioned she had to get her insurance to approve paying for the MRI? Every one of these preliminary steps cost money, and she had to wrangle with her insurance to get their OK.
But of course even with her insurance saying yes, there were still copays, and deductibles, and what’s called co-insurance — where you pay a percentage of any bill from a hospital.
Which meant Caitlyn was chipping away at what’s called her out-of-pocket maximum: The most she could be on the hook for in a given calendar year. The surgery got scheduled for December — the same calendar year as all those tests — and she checked to see what she might have to pay.
Caitlyn: I looked at my little portal for insurance, I’m showing what’s left on my out-of-pocket max for the year is around 2,000, give or take, 200 dollars.
Dan: She called the insurance company to confirm that estimate. And then she cranked up her due diligence.
Caitlyn: I called the hospital, and I asked for the names of the anesthesiologist, the radiologist. I asked for all of the details of who is possibly going to be on my case. And then I turned around and I called insurance and I said, I want to make sure all of these physicians are going to be in network on this date.
Dan: Caitlyn had done her homework. Probably more than a lot of us would have thought to do. I asked her: How’d you get so diligent? And first, like a lot of folks I’ve talked with, she said: Having a major health issue as a kid — losing her hearing — gave her an early heads-up to watch out.
Caitlyn: A little bit was, uh, experience of my mom dealing with insurance battles with me growing up. I remember her running into issues with that.
Can: And she’s got some experts in her life now. Her brother and her sister in law work in health care. One of her best friends is a healthcare lawyer and had some tips.
Caitlyn: But honestly, I think a lot of it is I have anxiety, and so I was just really paranoid.
Dan: The surgery went great. And a few weeks later, Caitlyn was in the audiologist’s office, getting that external component attached, and hearing on her right side for the first time in 15 years. Caitlyn says it all took some getting used to.
Caitlyn: I remember those, like, first few days especially, it wasn’t really like I was hearing full sounds. It was kind of just different pitches. I wasn’t hearing the words and everything, it was just the breakdown of the different pitches. And they also were just so much higher than they should be.
Dan: So interesting. Radiolab may have already done this story — [but] I’m just like, let’s find out what that’s about.
Caitlyn: I love Radiolab.
Dan: Me too! Anyway, two weeks after she starts getting used to her new hearing situation, Caitlyn gets that alert on her phone.
Caitlyn: And it tells me I have a new invoice. And I was like, oh, awesome! I’m not stressed at all, I did my due diligence. I know it’s gonna be expensive, but affordable.
Dan: Except, right: It’s a hundred and thirty-nine thousand dollars! Six figures. The full amount for her surgery. You might remember, Caitlyn said she had a panic attack. That was literal: Heart palpitations, hyperventilating.
It took her 20 or 30 minutes to get calm enough to start making calls. And she says her insurance told her they hadn’t paid because the hospital had neglected to send something important.
Caitlyn: The itemized bill. Which has all the codes and everything,
Dan: Caitlyn says she immediately asked the hospital, in writing to send her insurance the itemized bill, and she says sent a follow-up a week later. But her phone kept pinging with alerts about owing the hospital a hundred and thirty-nine thousand dollars.
Caitlyn: The app so conveniently told me that I could sign up for monthly payments of 11,000 dollars a month, which is just so absurd.
Dan: After two weeks, she asked her insurance: Do you have that itemized bill yet? They didn’t. So she called the hospital again.
Caitlyn: The girl I spoke with said she was putting in a request to have it faxed to my insurance and that would take two to three weeks. And I said, hold on, it takes you two to three weeks to fax a document?
Dan: Answer: Apparently yes? And Caitlyn says even three weeks later, her insurance company still hadn’t gotten that itemized bill the hospital promised to fax.
And all this time Caitlyn was still getting notices from the hospital billing department. And the latest one said, “past due.” She tried something new: So she called the hospital and demanded they send the itemized bill directly to her, immediately. Which they did.
Caitlyn: So I turned around and faxed it to my insurance.
Dan: Yeah but, this did not end things, not yet. Caitlyn says she got more notices labeled past due. She fought her way to a direct conversation with a supervisor.
Caitlyn: They kept saying,‘well, a supervisor’s not available right now.’ I said, No, you’re finding a supervisor. I don’t care if they’re cutting their lunch short. I’m talking to a supervisor right now. I don’t care if I sound like a Karen. It’s been a long, long year already.
Dan: Eventually, Caitlyn got a supervisor on the line and got the supervisor to get permission from a manager to stop sending her bills while the hospital waited for insurance to pay.
By this time, it was late March, almost two months after that first bill gave Caitlyn that panic attack. Also by this time, Caitlyn had sent her bill to the folks at NPR and KFF Health News for that Bill of the Month feature they do.
Caitlyn: I was like, I just need to vent. And so I submitted it just to vent it out. Never expecting anyone to reach out.
Dan: But they did. And on April 9th, Caitlyn got a call from a regional Patient Service Center manager.
Caitlyn: And she was super nice and tried to be really apologetic, but never actually accepting any blame. Or outright saying,‘we’re so sorry.’ Just said, ‘I’m sorry for your frustration, that sounds awful.’
Dan: She DID tell Caitlyn that the hospital had received payment from her insurance. And that Caitlyn could expect a final bill within a week. And that instead of a hundred thirty nine thousand, it was gonna be one thousand, nine hundred eighty-two dollars and twenty-five cents.
Caitlyn: I said,‘yep, that actually matches what my insurance said,’ and she said,‘oh, you know what was left on your out-of-pocket, most people don’t,’ and I said,‘I’m very well versed in every dollar sign at this point in this entire case.’
Dan: Caitlyn says she got that bill four days later and paid it immediately.
Caitlyn: And I saved the receipt of that, I have saved everything. It feels like it’s resolved, but there’s part of me that’s still waiting for the other shoe to drop
Dan: So, Caitlyn’s story brings up a LOT. Of course, I loved the way she kept fighting, and ultimately took control of the situation. And I hated how she got trapped between these two big entities and how much time and stress the whole thing cost her.
Because, you know, the hospital could’ve resolved this so quickly by just sending that itemized bill to Caitlyn’s insurance company.
Caitlyn: And the hospital did not do that. They just turned around and billed me. Which was a stupid idea, since the insurance company is more likely to have the money. Not the legal assistant in Oklahoma.
Dan: Caitlyn’s story raised a few questions, and brought back a lot of themes we’ve touched on before. We dug in also found some new tips, and some memories I want to share. That’s coming right up.
This episode of An Arm and a Leg is a co-production of Public Road Productions and KFF Health News, a nonprofit newsroom covering healthcare in America. Their senior contributing editor, Elisabeth Rosenthal, reported Caitlyn’s story for KFF and NPR. She wrote a book about U.S. healthcare. It’s called “An American Sickness,” and it was an inspiration for this show.
One question we ask sometimes on this show when we see a bill that’s so wildly ridiculous and unfair is: Can they freaking DO that?!? Like, is that even legal?
Like in this instance, can they just keep billing you while they’re apparently not even playing ball with your insurance? And: Do we have any legal weapons to fight back with?
We asked a bunch of legal experts, and they pretty much all said: Yes, they probably can do that, and no, we probably don’t have any easy legal weapons we can fight with. But then I talked with Berneta Haynes. She’s a senior attorney with the National Consumer Law Center.
And she had some practical thoughts that are super-worth sharing. She used to work for a nonprofit called Georgia Watch — that’s a state-level consumer protection group. They operated a hotline people could call for help.
Berneta Haynes: Consumers and patients would call us with all kinds of hospital billing issues and medical debt issues. And we’ve had these kinds of weird questions where really, there wasn’t a particular lever at the legal level to actually help them. But if they feel like they’re experiencing what could be considered potentially an unfair business practice, it is totally within their right to file a complaint within their state A. G.’s office.
Dan: The A.G. The state attorney general. Whoever’s doing you wrong, you can file a complaint.
Berneta: Whether or not there’s any real hook that your AG could use to hold them accountable is always a question that’s up in the air. But even just the act of filing a complaint is very likely to get that entity, that company, to behave correctly.
Dan: Basically, go up the chain. Whether to a government watchdog, or in the organization that’s bugging you. We’ve heard this before, but I loved the specifics that Berneta Haynes shared with me about her own experiences.
Berneta: I will tell you, one of the mechanisms my husband and I have had to utilize repeatedly, not in a hospital context, but in various other service contexts is to reach out or threaten to reach out to the CEO or president. And it gets results every time. It gets results every time!
Dan: Oh, and here’s the pro tip.
Berneta: My husband has repeatedly, when he’s had to do it, set up a LinkedIn premium account just to find the CEO and message them directly.
Dan: Ooh, that’s good!
Berneta: That has been the way we’ve gotten resolution on all kinds of issues related to insurance companies not wanting to do right by us. And so forth.
Dan: So that was fun. Now, I do want to talk a little bit about what Caitlyn did, and what allowed her to do it. Caitlyn figures she made at least a dozen phone calls. And she says she’s lucky — privileged — to have a job where she could do that. Here’s the first thing she says she did once she got over that panic attack when the bill arrived.
Caitlyn: I just went to my boss’s office and I said, I’m going to have to make some phone calls. There’s a problem with my hospital bill. She’s like, don’t worry about it. Do what you need to.
Dan: And she had people in her corner, like the friend who’s a healthcare lawyer. And legal advice wasn’t the big thing that friend gave Caitlyn.
Caitlyn: Most of the time I was just venting to her, and she was like,‘you need to keep pushing, like, keep going at them. Don’t let them win. Don’t roll over. Just keep pushing. They should be paying.’
Dan: And at that point, I told Caitlyn, she and her story were really reminding me of someone.
Dan: There’s a reporter named Marshall Allen. He worked for ProPublica for a long time. He wrote on healthcare, and he wrote on stuff like this. And eventually he wrote a book, giving advice to people. And the title of the book was, Never Pay the First Bill.
Caitlyn: Oh!
Dan: And I told Caitlyn, Marshall was on my mind at the time because when Caitlyn and I talked in May, Marshall had just died, like less than two weeks before. And he was young — 52. He had three kids.
Caitlyn: So sad.
Dan: Super, super, super sad.
Dan: And of course the title of Marshall’s book — Never Pay the First Bill — that’s exactly how Caitlyn played things. She wasn’t going to think about paying anything until she got her questions answered. And it is worth remembering.
When we were talking with legal experts, one thing a few of them said was: If you pay something that insurance was supposed to cover, and then insurance comes through, you’re supposed to get a refund. But who wants to chase that?
Yeah. Don’t pay that first bill until you’ve made sure this is money you really owe. So, this seems like a good time to memorialize Marshall Allen a little bit. He liked to compare the healthcare system to a schoolyard bully. Here’s what he told me when he was on this show in 2021 when his book had just come out.
Marshall Allen: What I think we need to do is stand up to the bully. We need to stop being afraid. We need to stop thinking someone else is going to stick up for us. And I wrote the book to equip and empower people to stand up to the bullies.
And I think it’s tremendously empowering, but it’s hard, and standing up to a bully takes incredible courage. It takes fortitude. It takes persistence. You might get beat up in the process. There’s no guarantee of victory. It’s risky, right? But if we don’t try, we don’t have a chance.
Dan: Marshall was a Christian minister before he became a reporter. He wrote a thoughtful essay about how his work as an investigative reporter fit with his faith. The gist was: The Bible is pretty clear that cheating people and exploiting them is wrong.
And to me, it seems like there was an element of ministry– not just evangelism — to what he did after his book came out. Here’s what he told me in 2021:
Marshall: I’ve started taking calls, and I’m responding to emails that I get from people and I’m saying,‘call me, let’s talk it through, let me help you with this. Let’s work through this together.’ And now I’m helping people work through their bills, work through these situations where they’re being cheated. It’s super satisfying and gratifying, so it’s my new hobby.
Dan: He kept at it. He left ProPublica and took a job with the Office of the Inspector General at the federal department of Health and Human Services. And he published a newsletter — it was free, but he encouraged people to pay if they could, and he used the money to hire medical-bill advocates to help people with especially tricky cases.
And Marshall was funny. I want to close out this episode with a story he told me the first time we talked, in 2019. It’s kind of an origin story.
Marshall: So when I was 16 years old, um, I worked for this dinner theater in Golden, Colorado, where I grew up. One day I show up for work, and they’ve closed down the business. They owed me like three weeks of pay.
The guy had closed the place without paying us and said,‘there’s no money. We shut down the business. We can’t afford to pay you. You’re out of luck.’ Well, we were all pretty angry about that. We were really angry because they had opened a sister dinner theater under the same company umbrella across town. And we all knew that. And we were like, well, if you can afford to keep your other place open, you can afford to pay us. And they said,‘sorry, kids, you’re out of luck.’
Dan: Marshall goes home, tells his mom what’s going on.
Marshall: And my mom tells me you should sue him. I’m like, mom, what do you mean? I can barely drive. How can I sue the guy? She goes,‘you should take him to small claims court.’ So lo and behold, I go down, I fill out the paperwork.
It’s a few paragraphs. It’s easy to fill out the paperwork in small claims court. I fill out the paperwork and turn in like 10 bucks at the time or whatever it costs. It’s not that expensive to file one of these cases. And I get a notice in the mail like six weeks later. And I have a court date, and I’m like geared up for this big Perry Mason moment.
Dan: Perry Mason was a lawyer on this super old TV show — courtroom drama. But this wasn’t a courtroom.
Marshall: It’s more like a conference room and there’s some administrative hearing judge in there. And lo and behold, the owner of the company and his attorney had to show up in court there with me.
And I thought we’d have a big argument all the administrative judge did is he read my few paragraphs on the little thing I’d written up and he looks over at the owner and he goes,‘is what this kid saying true?’And the owner’s like, ‘well, yeah.’ And the judge is like,‘give this kid his money.’ And I was like, This is amazing. You know what? Maybe the court system does actually work every now and then maybe every now and then the little guy can win.
Dan: Marshall and I both stayed interested in how people can use the legal system to get our rights. I learned a lot from Marshall, and like a lot of people, I just loved his spirit. Marshall Allen, thank you. And here’s the end of my conversation with Caitlyn.
Dan: Marshall Allen would have been extremely proud of you.
Caitlyn: Yeah.
Dan: Caitlyn has the final word here.
Caitlyn: I got to the point where I was like, it’s my fight. I’ve got gasoline in the fire. I’m, I’m going for it.
Dan: We’ll be back with a new episode in a few weeks. Till then, take care of yourself.
This episode of An Arm and a Leg was produced by me, Dan Weissmann, with help from Emily Pisacreta and Claire Davenport — and edited by Ellen Weiss.
KFF senior contributing editor Elisabeth Rosenthal reported Caitlyn’s story for KFF and NPR. She was editor in chief there when she invited me to collaborate with KFF to make this show’s second season, and we’ve been colleagues ever since. I’ve never felt so lucky or so thankful.
Special thanks to Christopher Robertson at Boston University’s School of Law, Wendy Epstein of the College of Law at DePaul University, Sabrina Corlette at Georgetown University’s Center on Health Insurance Reforms, and Elisabeth Benjamin from the Community Service Society of New York for pitching in with legal expertise here.
Adam Raymonda is our audio wizard. Our music is by Dave Weiner and Blue Dot Sessions. Gabrielle Healy is our managing editor for audience. Bea Bosco is our consulting director of operations. Sarah Ballama is our operations manager.
An Arm and a Leg is produced in partnership with KFF Health News. That’s a national newsroom producing in-depth journalism about healthcare in America and a core program at KFF, an independent source of health policy research, polling, and journalism.
Zach Dyer is senior audio producer at KFF Health News. He’s editorial liaison to this show. And thanks to the Institute for Nonprofit News for serving as our fiscal sponsor. They allow us to accept tax-exempt donations. You can learn more about INN at INN.org. Finally, thank you to everybody who supports this show financially. You can join in any time at https://armandalegshow.com/support/. Thank you so much for pitching in if you can — and, thanks for listening.
“An Arm and a Leg” is a co-production of KFF Health News and Public Road Productions.
To keep in touch with “An Arm and a Leg,” subscribe to its newsletters. You can also follow the show on Facebook and the social platform X. And if you’ve got stories to tell about the health care system, the producers would love to hear from you.
To hear all KFF Health News podcasts, click here.
And subscribe to “An Arm and a Leg” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 2 months ago
Health Care Costs, Health Industry, Insurance, Multimedia, An Arm and a Leg, Oklahoma, Out-Of-Pocket Costs, Podcasts, Surprise Bills
Readers Weigh In on Abortion and Ways To Tackle the Opioid Crisis
Letters to the Editor is a periodic feature. We welcome all comments and will publish a selection. We edit for length and clarity and require full names.
Debunking Abortion Myths
Letters to the Editor is a periodic feature. We welcome all comments and will publish a selection. We edit for length and clarity and require full names.
Debunking Abortion Myths
I want to send a big THANK YOU to Matt Volz for writing a fact-checking article on the nonsense rhetoric around “abortion up until and after birth” that has run wild and unchallenged in the media (“GOP’s Tim Sheehy Revives Discredited Abortion Claims in Pivotal Senate Race,” July 9). Thanks for putting abortion later in pregnancy in context and debunking false assumptions.
I am a near-third-trimester abortion patient (nonviable pregnancy, terminated at 26 weeks), and I am so sick of hearing politicians like Tim Sheehy talk about something they have never experienced or bothered to learn about. It is as though I am watching the entire nation maliciously gossip about me and other parents like me. Those of us in the termination for medical reasons (TFMR) community have walked through hell only to have our voices, at best, be ignored or, more commonly, be insulted and threatened.
And I imagine watching this political circus is just as hurtful for parents who lost an infant shortly after birth and had to provide palliative care. That is who they are talking about with “abortion after birth”; they are talking about comfort care for infants who will not survive.
Thank you again for bringing a dose of reality to a conversation that never should have become political. These are impossible decisions that only parents should make. It was really refreshing to read Volz’s article and know that some journalists are still willing to fact-check the absurd claims floating around. It was encouraging to know that someone does see us.
— Anne Angus, Bozeman, Montana
A physician and Yale professor of radiology and biomedical imaging took to the social platform X to share feedback:
.@SenatorTester is a great Senator. And his opponent is a great liar. Both the GOP presidential candidate and Tim Sheehy have perpetuated this lie. Please push back every time you hear it. https://t.co/1LBGPgOA2u
— (((Howard Forman))) (@thehowie) July 9, 2024
— Howard Forman, New Haven, Connecticut
I just read your article at PolitiFact on Republican Senate candidate Tim Sheehy’s statement about abortion, and I would like to point out (what I believe) are a couple of errors.
1. In paragraph 10, you quote KFF’s Alina Salganicoff saying that “in the good-faith medical judgment of the treating health care provider, continuation of the pregnancy would pose a risk to the pregnant patient’s life or health.” Now, you may know that almost at the same time that the Roe v. Wade decision was released, there was a decision called Doe v. Bolton that interpreted “health” to mean almost anything. That broad interpretation of health is found in your article in paragraph 24: “Women have abortions later in pregnancy either because they find out new information or because of economic or political barriers,” [Katrina] Kimport said.
When a woman can have an abortion after viability because she offers any reason that can be interpreted as “health,” then abortion would be legal throughout all nine months of pregnancy. I believe that you are wrong in your interpretation. Democrats do not want to name any restriction on abortion during all nine months, and every mention of “health” is a fig leaf that does not restrict abortion at all. Every abortion advocate knows that.
2. Whether late-term abortions are rare or not is logically irrelevant to whether late-term abortions should be restricted.
Why don’t you know these things?
— Darryl A. Linde, Tahlequah, Oklahoma
An Air Force veteran added his two cents on X:
Dems have the facts. Republicans spread fear and lies.https://t.co/6CWfKhqxJZ
— James Knight (@jamesUSAF_vet) July 12, 2024
— James Knight, Reno, Nevada
Making a Healthy Difference for the Homeless
Thank you for printing this story (“A California Medical Group Treats Only Homeless Patients — And Makes Money Doing It,” July 19). It really piqued my interest and portrayed a positive solution for getting care to the people.
Up here in the Bay Area, I believe there are a couple of groups who go out and find what needs doing instead of waiting for people to come to them — but nothing like this. Makes me curious about what we actually have going on here.
— Laurie Lippe, El Cerrito, California
A self-described “nurse turned health tech nerd” commended the effort on X:
"They distribute GPS devices so they can track their homeless patients. They keep company credit cards on hand in case a patient needs emergency food or water, or an Uber ride to the doctor"This is healthcare at its best 💕https://t.co/UhM1dgTPH7
— Rik Renard (@rikrenard) July 22, 2024
— Rik Renard, New York City
A senior policy director at the National Health Care for the Homeless Council shared the post on X — while stressing that her tweets reflected her own opinions and not those of her organization:
I’m with @DrJimWithers: “I do worry about the corporatization of street medicine and capitalism invading what we’ve been building, largely as a social justice mission outside of the traditional health care system.” https://t.co/IOjazvrvqP
— Barbara DiPietro (@BarbaraDiPietro) July 19, 2024
— Barbara DiPietro, Baltimore
On X, a physician who says she champions “physicians, patients, public health, and the patient-physician relationship” reacted to our coverage surrounding the Federal Trade Commission’s rule banning the use of noncompete agreements in employment contracts:
FTC #noncompete crackdown may not protect doctors and nurses at ~64% of US community hospitals that are tax-exempt nonprofits or government-owned.But, @FTC said some nonprofits could be bound by the rule if they do not operate as true charities. https://t.co/9fDbfVflTH
— Marilyn Heine (@MarilynHeineMD) May 28, 2024
— Marilyn Heine, Langhorne, Pennsylvania
Without a Noncompete Ban on All Employers, Rural Access to Care Suffers
When news broke that the Federal Trade Commission would be banning noncompete agreements in employment contracts, many of us in the medical profession celebrated. However, until nonprofit hospitals and health care facilities benefit from the same ban, access to care — particularly in rural regions — will suffer.
As reported in “Health Worker for a Nonprofit? The New Ban on Noncompete Contracts May Not Help You” (June 5), about two-thirds of U.S. community hospitals are nonprofit or government-owned. This means that most hospitals nationwide may continue to enforce noncompete agreements among their employees, a practice that will have an outsize impact on rural medical professionals.
As a rheumatologist in a rural area, I’ve seen how detrimental limited access to care is for patients. Noncompete agreements serve only to further limit access to much-needed care. Due to the physician shortage being particularly acute in rural America, there are oftentimes only a few specialty physicians servicing a large region. Suppose one of these specialists is employed by a large health system and wants to transition to a private practice. It reduces the number of accessible specialists in the area when their noncompete agreement prohibits them from practicing near any of the health care facilities associated with the system. And increasing consolidation across health care means many rural regions may have only a single health system that operates across the entire state and surrounding areas. A geographically limiting noncompete agreement essentially stops a physician or medical professional from practicing entirely in the area, or they must uproot their life and move away from the major health system.
I hope the FTC takes further action to include nonprofit health care employers in its noncompete ban. I also urge nonprofit employers to consider their rural patients’ access to care when requiring providers to sign noncompete agreements. It’s in the best interest of our patient’s health to get rid of these agreements entirely.
— Chris Phillips, chair of the American College of Rheumatology’s Committee on Rheumatologic Care, Paducah, Kentucky
The president of the Texas Medical Board also posted on X with feedback:
Is it a coincidence that this affects everyone, except those who work for nonprofit hospitals and health care facilities, which employs the largest number of medical professionals?The FTC and it's selective enforcement and rules is blatantly obvious! https://t.co/RzXInqiJ8D
— Sherif Zaafran, MD (@szaafran) June 16, 2024
— Sherif Zaafran, Houston
Repurposing Newspaper Boxes for Public Health
I recently read your article by Mara Silvers regarding the state’s intended use of public health vending machines (PHVMs) to help fight the opioid overdose epidemic (“Montana’s Plan To Curb Opioid Overdoses Includes Vending Machines,” July 18). Working on the covid-19 response for almost four years now, and with our American Rescue Plan Act funding coming to an end, we recently used a byline in our equipment budget to purchase and place “resource kiosks” in the community.
In 2022, after researching the use of vending machines for test distribution, we discovered vending machines have high barrier-to-entry costs and high maintenance costs. And even if purchasing isn’t possible, rental contracts come with high fees. We decided it was better to use a lower-cost resource that could be purchased in greater quantity, easily placed with community partners, and required no maintenance: the refurbished newspaper kiosk.
We decided to purchase double-decker boxes, which have a secondary door, creating another shelf, for roughly $410 apiece and stocked them with covid tests, nasal naloxone, injectable naloxone, fentanyl test strips, xylazine test strips, various types of condoms, and lubrication packets. We are in the process of securing a supply of gun locks and adding links to our pilot landing page for individual free gun lock deliveries, as well as links for free sexually transmitted infection test kits. We have investigated providing dental supplies and other items, but long-term funding is a constant concern. Grant money for most programs (likely all ARPA dollars) is running out, so the viability of these types of pilot programs is tentative without a buy-in from state or federal agencies.
Mara’s article hinted at criteria for possible placements and, similarly, we didn’t use locational overdose data, which can be “othering” to communities, but instead placed these kiosks with community partners that have been accomplished supporters of their at-risk populations throughout the covid response. Each community partner helped protect the communities they served through increased access to resources and provided information as trusted messengers. Truly meeting people where they are.
While money quickly appeared to fight the covid pandemic, and states spirited away dollars for pet projects, that sea of funding has dried up, and there doesn’t seem to be a plan for any continued funding. Covid-related functions have all been folded back into communicable disease epidemiology programs, which were already underfunded; in our state, the money funding the naloxone bulk fund is also drying up. Covid deaths might be down, but there is always a new bug (H5N1), STI infections are up, and gun-related deaths grow year over year. Funding population-level health interventions is our next pandemic.
With enough funding, kiosk-sized PHVMs could be swiftly added to any public health agency’s or community program’s quiver of tools to help increase access to resources and information for the most vulnerable residents.
Thank you for publishing a great article about the emerging opportunities to respond to changing public health needs!
— Christopher Howk, Arapahoe County Public Health’s covid-19 testing and logistics coordinator, Greenwood Village, Colorado
A retiree with a PhD in quantum chemistry tweeted his surprise over the news:
Montana’s Plan To Curb Opioid Overdoses Includes Vending Machineshttps://t.co/kNxYjnIOEO(What???!! Vending machines for opioids?)
— John Lounsbury (@jlounsbury59) July 18, 2024
— John Lounsbury, Lake Frederick, Virginia
Misappropriation of Opioid Settlement Funds
OK, so I see how all these states got all these lump sums of money for people like us who became addicted and whose lives were devastated by Purdue Pharma, Vicodin, and all the pharmacies (“Lifesaving Drugs and Police Projects Mark First Use of Opioid Settlement Cash in California,” July 12). How come all these states got all the money but those of us who have suffered have to wait, hire lawyers, and wait years for the money that was just handed over to these states? We’re the ones whose lives were devastated. My son was hooked, I was hooked, and my wife, and yet we must sit here penniless after the addiction, while all these states take the money — and they don’t do what they’re supposed to with it, and everyone knows it.
— Michael Stewart, Des Moines, Iowa
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 2 months ago
Health Industry, Public Health, Rural Health, Abortion, Homeless, Letter To The Editor, Misinformation, Opioids, Substance Misuse, Women's Health
Why Many Nonprofit (Wink, Wink) Hospitals Are Rolling in Money
One owns a for-profit insurer, a venture capital company, and for-profit hospitals in Italy and Kazakhstan; it has just acquired its fourth
One owns a for-profit insurer, a venture capital company, and for-profit hospitals in Italy and Kazakhstan; it has just acquired its fourth for-profit hospital in Ireland. Another owns one of the largest for-profit hospitals in London, is partnering to build a massive training facility for a professional basketball team, and has launched and financed 80 for-profit start-ups. Another partners with a wellness spa where rooms cost $4,000 a night and co-invests with “leading private equity firms.”
Do these sound like charities?
These diversified businesses are, in fact, some of the country’s largest nonprofit hospital systems. And they have somehow managed to keep myriad for-profit enterprises under their nonprofit umbrella — a status that means they pay little or no taxes, float bonds at preferred rates, and gain numerous other financial advantages.
Through legal maneuvering, regulatory neglect, and a large dollop of lobbying, they have remained tax-exempt charities, classified as 501(c)(3)s.
“Hospitals are some of the biggest businesses in the U.S. — nonprofit in name only,” said Martin Gaynor, an economics and public policy professor at Carnegie Mellon University. “They realized they could own for-profit businesses and keep their not-for-profit status. So the parking lot is for-profit; the laundry service is for-profit; they open up for-profit entities in other countries that are expressly for making money. Great work if you can get it.”
Many universities’ most robust income streams come from their technically nonprofit hospitals. At Stanford University, 62% of operating revenue in fiscal 2023 was from health services; at the University of Chicago, patient services brought in 49% of operating revenue in fiscal 2022.
To be sure, many hospitals’ major source of income is still likely to be pricey patient care. Because they are nonprofit and therefore, by definition, can’t show that thing called “profit,” excess earnings are called “operating surpluses.” Meanwhile, some nonprofit hospitals, particularly in rural areas and inner cities, struggle to stay afloat because they depend heavily on lower payments from Medicaid and Medicare and have no alternative income streams.
But investments are making “a bigger and bigger difference” in the bottom line of many big systems, said Ge Bai, a professor of health care accounting at the Johns Hopkins University Bloomberg School of Public Health. Investment income helped Cleveland Clinic overcome the deficit incurred during the pandemic.
When many U.S. hospitals were founded over the past two centuries, mostly by religious groups, they were accorded nonprofit status for doling out free care during an era in which fewer people had insurance and bills were modest. The institutions operated on razor-thin margins. But as more Americans gained insurance and medical treatments became more effective — and more expensive — there was money to be made.
Not-for-profit hospitals merged with one another, pursuing economies of scale, like joint purchasing of linens and surgical supplies. Then, in this century, they also began acquiring parts of the health care systems that had long been for-profit, such as doctors’ groups, as well as imaging and surgery centers. That raised some legal eyebrows — how could a nonprofit simply acquire a for-profit? — but regulators and the IRS let it ride.
And in recent years, partnerships with, and ownership of, profit-making ventures have strayed further and further afield from the purported charitable health care mission in their community.
“When I first encountered it, I was dumbfounded — I said, ‘This not charitable,’” said Michael West, an attorney and senior vice president of the New York Council of Nonprofits. “I’ve long questioned why these institutions get away with it. I just don’t see how it’s compliant with the IRS tax code.” West also pointed out that they don’t act like charities: “I mean, everyone knows someone with an outstanding $15,000 bill they can’t pay.”
Hospitals get their tax breaks for providing “charity care and community benefit.” But how much charity care is enough and, more important, what sort of activities count as “community benefit” and how to value them? IRS guidance released this year remains fuzzy on the issue.
Academics who study the subject have consistently found the value of many hospitals’ good work pales in comparison with the value of their tax breaks. Studies have shown that generally nonprofit and for-profit hospitals spend about the same portion of their expenses on the charity care component.
Here are some things listed as “community benefit” on hospital systems’ 990 tax forms: creating jobs; building energy-efficient facilities; hiring minority- or women-owned contractors; upgrading parks with lighting and comfortable seating; creating healing gardens and spas for patients.
All good works, to be sure, but health care?
What’s more, to justify engaging in for-profit business while maintaining their not-for-profit status, hospitals must connect the business revenue to that mission. Otherwise, they pay an unrelated business income tax.
“Their CEOs — many from the corporate world — spout drivel and turn somersaults to make the case,” said Lawton Burns, a management professor at the University of Pennsylvania’s Wharton School. “They do a lot of profitable stuff — they’re very clever and entrepreneurial.”
The truth is that a number of not-for-profit hospitals have become wealthy diversified business organizations. The most visible manifestation of that is outsize executive compensation at many of the country’s big health systems. Seven of the 10 most highly paid nonprofit CEOs in the United States run hospitals and are paid millions, sometimes tens of millions, of dollars annually. The CEOs of the Gates and Ford foundations make far less, just a bit over $1 million.
When challenged about the generous pay packages — as they often are — hospitals respond that running a hospital is a complicated business, that pharmaceutical and insurance execs make much more. Also, board compensation committees determine the payout, considering salaries at comparable institutions as well as the hospital’s financial performance.
One obvious reason for the regulatory tolerance is that hospital systems are major employers — the largest in many states (including Massachusetts, Pennsylvania, Minnesota, Arizona, and Delaware). They are big-time lobbying forces and major donors in Washington and in state capitals.
But some patients have had enough: In a suit brought by a local school board, a judge last year declared that four Pennsylvania hospitals in the Tower Health system had to pay property taxes because its executive pay was “eye popping” and it demonstrated “profit motives through actions such as charging management fees from its hospitals.”
A 2020 Government Accountability Office report chided the IRS for its lack of vigilance in reviewing nonprofit hospitals’ community benefit and recommended ways to “improve IRS oversight.” A follow-up GAO report to Congress in 2023 said, “IRS officials told us that the agency had not revoked a hospital’s tax-exempt status for failing to provide sufficient community benefits in the previous 10 years” and recommended that Congress lay out more specific standards. The IRS declined to comment for this column.
Attorneys general, who regulate charity at the state level, could also get involved. But, in practice, “there is zero accountability,” West said. “Most nonprofits live in fear of the AG. Not hospitals.”
Today’s big hospital systems do miraculous, lifesaving stuff. But they are not channeling Mother Teresa. Maybe it’s time to end the community benefit charade for those that exploit it, and have these big businesses pay at least some tax. Communities could then use those dollars in ways that directly benefit residents’ health.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 2 months ago
Health Care Costs, Health Care Reform, Health Industry, Hospitals
KFF Health News' 'What the Health?': At GOP Convention, Health Policy Is Mostly MIA
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
The Republican National Convention highlighted a number of policy issues this week, but health care was not among them. That was not much of a surprise, as it is not a top priority for former President Donald Trump or most GOP voters. The nomination of Sen. J.D. Vance of Ohio adds an outspoken abortion opponent to the Republican ticket, though he brings no particular background or expertise in health care.
Meanwhile, abortion opponents are busy trying to block state ballot questions from reaching voters in November. Legal battles over potential proposals continue in several states, including Florida, Arkansas, and Arizona.
This week’s panelists are Julie Rovner of KFF Health News, Alice Miranda Ollstein of Politico, Sarah Karlin-Smith of the Pink Sheet, and Joanne Kenen of the Johns Hopkins schools of public health and nursing and Politico Magazine.
Panelists
Alice Miranda Ollstein
Politico
Joanne Kenen
Johns Hopkins University and Politico
Sarah Karlin-Smith
Pink Sheet
Among the takeaways from this week’s episode:
- Sen. J.D. Vance of Ohio has cast few votes on health policy since joining Congress last year. He has taken a doctrinaire approach to abortion restrictions, though, including expressing support for prohibiting abortion-related interstate travel and invoking the Comstock Act to block use of the mail for abortion medications. He also speaks openly about his mother’s struggles with addiction, framing it as a health rather than criminal issue in a way that resonates with many Americans.
- Although Republicans have largely abandoned calls to repeal and replace the Affordable Care Act, it would be easy for former President Donald Trump to undermine the program in a second term; expanded subsidies for coverage are due to expire next year, and there’s always the option to cut spending on marketing the program, as Trump did during his first term.
- Trump’s recent comments to Robert F. Kennedy Jr. about childhood vaccinations echoed tropes linked to the anti-vaccination movement — particularly the false claim that while one vaccine may be safe, it is perhaps dangerous to receive several at once. The federal vaccination schedule has been rigorously evaluated and found to be safe and effective.
- Covid is surging once again, with President Joe Biden among those testing positive this week. The virus is proving a year-round concern and has peaked regularly in summertime; covid spreads best indoors, and lately millions of Americans have taken refuge inside from extremely high temperatures. Meanwhile, the virology community is concerned that the nation isn’t testing enough animals or humans to understand the risk posed by bird flu.
Also this week, Rovner interviews KFF Health News’ Renuka Rayasam, who wrote the June installment of KFF Health News-NPR’s “Bill of the Month,” about a patient who walked into what he thought was an urgent care center and walked out with an emergency room bill. If you have an exorbitant or baffling medical bill, you can send it to us here.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: Time magazine’s “‘We’re Living in a Nightmare:’ Inside the Health Crisis of a Texas Bitcoin Town,” by Andrew R Chow.
Joanne Kenen: The Washington Post’s “A Mom Struggles To Feed Her Kids After GOP States Reject Federal Funds,” by Annie Gowen.
Alice Miranda Ollstein: ProPublica’s “Texas Sends Millions to Crisis Pregnancy Centers. It’s Meant To Help Needy Families, but No One Knows if It Works,” by Cassandra Jaramillo, Jeremy Kohler, and Sophie Chou, ProPublica, and Jessica Kegu, CBS News.
Sarah Karlin-Smith: The New York Times’ “Promised Cures, Tainted Cells: How Cord Blood Banks Mislead Patients,” by Sarah Kliff and Azeen Ghorayshi.
Also mentioned on this week’s podcast:
The Wall Street Journal’s “Mail-Order Drugs Were Supposed To Keep Costs Down. It’s Doing the Opposite,” by Jared S. Hopkins.
Click to open the transcript
Transcript: At GOP Convention, Health Policy Is Mostly MIA
KFF Health News’ ‘What the Health?’Episode Title: ‘At GOP Convention, Health Policy Is Mostly MIA’Episode Number: 356Published: July 18, 2024
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello, and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News, and I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, July 18, at 10 a.m. As always, news happens fast and things might’ve changed by the time you hear this. So, here we go.
We are joined today via video conference by Alice Miranda Ollstein, of Politico.
Alice Miranda Ollstein: Good morning.
Rovner: Sarah Karlin-Smith at the Pink Sheet.
Sarah Karlin-Smith: Hi, everybody.
Rovner: And Joanne Kenen of the Johns Hopkins Schools of public health and nursing, and Politico Magazine.
Joanne Kenen: Hi, everybody.
Rovner: Later in this episode, we’ll have my interview with KFF Health News’ Renuka Rayasam, about the latest “Bill of the Month.” This month’s patient went to a facility with urgent care in its name but then got charged emergency room prices. But first, this week’s news.
So as of this morning, we are most of the way through the Republican National Convention, which obviously has a somewhat different tone than was expected, following last weekend’s assassination attempt on former President Donald Trump. The big news of the week is Trump’s selection of Ohio Republican Sen. JD Vance as his running mate. Vance has only been in the Senate since 2023, had not served previously in public office, and he doesn’t have much of a record on much of anything in health care. So, what do we know about what he thinks?
Ollstein: Well, I have been most focused on his abortion record, which is somewhat more extensive than his record on other health policy. Obviously, Congress has not done very much on abortion, but he’s been loud and proud about his anti-abortion views, including calling for national restrictions. He calls it a national minimum standard, but the idea is that he does not want people in conservative states where abortion is banned to be able to travel to progressive states where it is allowed. He has given interviews to that effect. He has signed letters to that effect. He has called for enforcement of the Comstock Act, which, as we’ve talked about before, is this long dormant statute that prohibits the mailing of abortion drugs or medical instruments that could be used to terminate a pregnancy. And so this is a very interesting moment to pick Vance.
The Republican Party is attempting to reach out to more moderate voters and convince them that they are hoping to leave this issue to the states. Vance’s record somewhat says otherwise. He also opposed efforts in his own state of Ohio to hold a referendum that ended up striking down that state’s abortion ban. So, definitely a lot for Democrats to go after in his record and they are not wasting any time; they are already doing it.
Rovner: Yeah, I’m kind of surprised because Vance, very much like Trump, has been kind of everywhere, or at least he has said that he’s kind of everywhere on abortion. But as you mentioned, Alice, you don’t have to look very hard to see that he’s pretty doctrinaire on the issue. Do you think people are going to buy this newer, softer Republicanism on abortion?
Ollstein: Well, abortion rights groups that I’ve spoken to are worried that people are buying it. They’re worried as they campaign around the country that the Republican Party’s attempt to walk away from their past calls for national restrictions on abortion are breaking through to people. And so they are trying really hard to counter that message and to stress that Republicans can and would pursue national restrictions, if elected.
I think both Democratic candidates and abortion rights groups are working to say even the leave-it-to-states position is too extreme and is harming people. And so they’re lifting up the stories of people in Texas and other states with bans who have experienced severe medical harm as a result of being denied an abortion. And so they’re lifting up those stories to say, “Hey, even saying let’s leave it to the states, let’s not do a national ban — even that is unacceptable in the eyes of the left.”
Kenen: The other issue obviously with his life story is opioids. His mother was addicted. Originally it began with being prescribed a legal painkiller. It’s a familiar story: became addicted, he was raised by his grandmother. His mother, who he showed on TV last night and she was either in tears or really close to tears, she’s 10 years sober now. He had a tough life and opioids was part of the reason he had a tough life. And whatever you think of his politics, that particular element of his life story resonates with people because it may explain some of his political views. But that experience is not a partisan experience and he was a kid. So I think he clearly does see opioids as a medical problem, not just, oh, let’s throw them in jail. I mean, the country and the Republican Party, that has been a change. It’s not a change that’s completed, but that shift is across party lines as well. That’s part of him that — it’s something you listen to when he tells that story.
I mean also, he told a story about his grandmother late in life, the grandmother who raised him, having, when she died, they found 19 handguns in the house all over the place. And he told sort of a funny story that she was old and frail and she always wanted to have one within reach. And all I could think of is, all these unlocked handguns with kids in the house! I mean, which is not a regulatory issue, but there’s a gun safety issue there. I’m just thinking, oh my God, 19 guns in drawers all over the house. But he’s obviously a very, the Republican Party is … I mean, after the assassination attempt, you have not heard Donald Trump say, “Maybe I need to rethink my position on gun control.” I mean, that’s not part of the dialogue right now.
I think having someone with that experience, talking about it the way he does, is a positive thing, really. Saying, “Here’s what we went through. Here’s why. Here’s how awful it was. Here’s how difficult it was to get out of it. And this is what these families need.” I mean, that is …
Rovner: Although it’s a little bit ironic because he’s very anti-social programs, in general.
Karlin-Smith: And he’s had a bad track record of trying to address the opioid crisis. He had a charity he started that he ended I guess about when he was running for Senate that really was deemed nonsuccessful. It also had questionable ties to Purdue Pharma, that’s sort of responsible for the opioid crisis. And the other thing that you sometimes hear in both him and Trump’s rhetoric is the blaming of immigrants and the drug cartels and all of that stuff for the opioid crisis. So, there’s a little bit of use of the topic, I think, to drop anti-immigrant sentiment and not really think about how to address the actual health struggles.
Kenen: When he talks about his family, he’s not saying China sent my mother fentanyl. I think it is good for people to hear stories from the perspective of a family who had this, as it is a health problem, reminding people that this is not thugs on the street shooting heroin. It’s a substance abuse disorder, it’s a disease. And so I think the country has come a long way, but it isn’t where it needs to be in terms of understanding that it’s a behavioral health problem. So I think in that sense he will probably be a reminder of that. But he doesn’t have a health record. I mean, he wasn’t there during the Obamacare wars. We don’t really know what he thinks about. I’m not aware of anything he’s really said about entitlements and Medicare. He does come from the state … I mean, Trump is saying he won’t touch it. But I mean if he said Medicare stuff, I missed it. I mean, if one of you knows, correct …
Karlin-Smith: Well, he has actually said that he supports Medicare drug price negotiation at times, which is interesting and unique for a Republican. And I mean Trump, as well, has been a bit different from the traditional Republican, I think, when it comes to the pharma industry and stuff, but I think that maybe is even a bridge too far in some ways.
Rovner: Yeah, he’s generally pretty anti-social program, so it’ll be interesting to see how he walks that line.
Well, this is all good segue into my next question, which is, health in general has been mostly MIA during this convention, including any update on Trump’s ear injury from the attempted assassination. Are we finally post-repeal-and-replace in the Republican Party? Or is this just one of those things that they don’t want to talk about but might yet take up if they get into office?
Kenen: We don’t know what the balance of power is in the Senate and the House, right? I mean, that’s probably going to be part of it. I mean, if they have huge … if they capture both chambers with huge majorities, it’s a new ballgame. Whether they actually try to repeal it, versus there’s all sorts of ways they can undermine it. Trump did not succeed in repealing it. Trump and the House Republicans did not, the Republicans in general did not succeed in repealing it, despite a lot of effort. But they did undermine it in all sorts of ways and coverage actually fell during the Trump administration. ACA [Affordable Care Act] coverage did drop; it didn’t vanish completely, but it dropped. And under Biden it continued to grow. Now, the Republicans get their health care through the ACA, so it’s become much more normalized, but we don’t know what they will do. Trump is not a predictable politician, right? I mean, he often made a big deal about trying to lower drug prices early in his term, and then nothing. And then he even released huge, long list of things …
I remember one of our reporters — Sarah and I were both … Sarah, Alice, and I were all at Politico — and I think it was David who counted the number of question marks in that report. And at the end of the day, nothing much happened. I don’t think the ACA is untouchable; it may or may not be unrepealable in its entirety, but it’s certainly not untouchable.
Rovner: Well, he also changes positions on a whim, as we’ve seen. Most politicians you can at least count on to, when they take a position, to keep it at least for a matter of days or weeks, and Trump sometimes in the same interview can sort of contradict himself, as we know. But I mean, obviously a quick way to undermine the ACA, as you say, would just be to let the extended subsidies expire because they would need to be re-upped if that’s going to continue and there are many millions of people that are now …
Kenen: And they expire next year.
Rovner: … Yes, that are …
Kenen: And there are also two other things. You cut the navigating budget. You cut advertising. You don’t try to sell it. I don’t mean literally sell it, but you don’t try to go out and urge … I mean, that was their playbook last time, and that’s why — it’s one reason enrollment dropped. And that was, the subsidies were under Biden, the extended subsidies. So that’s one year away.
Ollstein: But it’s no surprise that this hasn’t been a big topic of discussion at the RNC [Republican National Convention]. I mean, polling shows that voters trust Democrats more on health care; it’s one of their best issues. It’s not a good issue for Republicans. And so it was fully expected that they would stick to things that are more favorable to them: crime, inflation, whatnot. So, I do expect to hear a lot about health care at the DNC [Democratic National Convention] in a few weeks. But beyond that, we do not know what’s going to happen at the DNC.
Rovner: Yeah.
Karlin-Smith: I was going to say, the one health issue we haven’t really touched on, which the Republicans have been hammering on, is transgender health care and pushing limits on it, especially for people transitioning, children, and adolescents. And I think that’s clearly been a strategic move, particularly as they’ve gotten into more political trouble with abortion and women in the party. They clearly seem to think that the transgender issue, in general, appeals more to their base and it’s less risky for them.
Rovner: Their culture warrior base, as you will. Yeah, and we have in fact seen a fair bit of that. Well, before we leave the convention, one more item: It seems that Trump and RFK Jr. [independent presidential candidate Robert F. Kennedy Jr.] had a phone conversation, which of course leaked to the public, during which they talked about vaccine resistance. Now we know that RFK Jr. is a longtime anti-vaxxer. What, if anything, does the recounting of this conversation suggest about former President Trump’s vaccine views? And we’ve talked about this a little bit before, he’s been very antimandate for the covid vaccine, but it’s been a little bit of a blank on basic childhood vaccines.
Karlin-Smith: And I mean, his remarks are, they’re almost a little bit difficult to parse, they don’t quite make sense, but they seem to be essentially repeating anti-vax tropes around, well, maybe one vaccine on their own isn’t dangerous, but we give kids too many vaccines at a time or too close together. And all of that stuff has been debunked over the years as incorrect. The vaccine schedule has been rigorously evaluated for safety and efficacy and so forth.
That said, Trump obviously was in office when we spearheaded the development of covid vaccines, which ended up being wildly successful, and he didn’t really undermine that process, I guess, for the most part when he was in office. So it’s hard to know. Again, there’s a lot of difficulty in predicting what Trump will actually do and it may depend a lot who he surrounds himself with and who he appoints to key positions in his health department and what their views are. Because he seems like he can be easily persuaded and right now he may just be in, again, campaign mode, very much trying to appeal to a certain population. And you could easily see him — because he doesn’t seem to care about switching positions — just pivoting and being slightly less anti-vax. But it’s certainly concerning to people who have been even more about the U.S. anti-vax sentiments since covid and decreases in vaccination rates.
Rovner: It did feel like he was trying to say what he thought RFK Jr. wanted to hear, so as to win his endorsement, which we know that Trump is very good at doing. He channels what he says depending on who he’s talking to, which is what a lot of politicians do. He just tends to do it more obviously than many others.
Kenen: Julie, we heard this at the tail end of the 2016 campaign. He made a few comments, exactly, very, very similar to this, the size of a horse vaccine and you see the changes — there’s too many, too many vaccines, too large doses. We heard this briefly in the late 2016, and we heard it at the very — I no longer remember whether it was during transition in 2016 or whether it was early in 2017 when he was in the White House — but we heard a little bit of this then, too. And he had a meeting with RFK then. And RFK said that Trump was talking about maybe setting up a commission and RFK at one point said that Trump had asked him to head the commission. We don’t think that was necessarily the case.
First of all, there was no commission. The White House never confirmed that they had asked RFK to lead it. Who knows who said what in a closed room, or who heard what or what they wanted to hear; we don’t know. But we heard this whole episode, including Trump and RFK, at approximately the beginning of 2017, and it did go away. Covid didn’t happen right away; covid was later. There was no anti-vax commission. There was no vax commission. There was no change in vaccination policy in those early years prepandemic. And as Sarah just pointed out, Trump was incredibly pro-vaccine during the pandemic. I mean, the Operation Warp Speed was hailed by even people who didn’t like anything else about Trump. When public health liked Operation Warp Speed, he got vaccines into arms fast, faster than many of us thought, right?
The difference — there were anti-vaxxers then; there have been since smallpox — but it is much more politicized and much more prominent, and in some ways it has almost replaced the ACA as your identifying health issue. If you talk to somebody about the ACA, you know what party they are, you even know where within the party they are, what wing. And that’s not 100% true of anti-vaxxers. There are anti-vaxxers on both sides, but the politicization has been on the Republican-medical-libertarian side, that you-can’t-tell-me-what-to-do-it’s-my-body side. It is much more part of his base and a more intense, visible, and vocal part of his base. So, it’s the same comments, or very similar comments, to the same person in a different political context.
Rovner: Well, I think it’s safe to say that abortion does remain the most potent political health issue of the year, and there was lots of state-based abortion election news this week. As we’ve been discussing all year, as many as a dozen states will have abortion questions on the ballot for voters this November, but not without a fight. Florida has just added an addendum to its ballot measures, suggesting that if passed, it could cost the state money. And in Arkansas and Montana, there are now legal fights over which signatures should or shouldn’t be counted in getting some of those questions to the ballot.
Alice, in every state that’s voted on abortion since Dobbs [v. Jackson Women’s Health Organization], the abortion-right side has prevailed. Is the strategy here to try to prevent people from voting in the first place?
Ollstein: Oh, yes. I wrote a story about this in January. It’s been true for a while, and it’s been true in the states that already had their votes, too. There were efforts in Ohio to make a vote harder or to block it entirely. There were efforts in Michigan to do so. And even the same tactics are being repeated. And so the fight over the cost estimate in Florida, which is usually just a very boring, bureaucratic, routine thing, has become this political fight. And that also happened in Missouri. So, we’re seeing these trends and patterns and basically any aspect of this process that can be mobilized to become a fight between conservative state officials and these groups that are attempting to get these measures on the ballot, it has been. And so Arizona is also having a fight over the language that is going to go in the voter guide that goes out to everybody. So there’s a fight going on there that’s going to go to court next week about whether it says fetus or unborn child. So, all of these little aspects of it, there’s going to be more lawsuits over signature, validation, and so it’s going to be a knockdown, drag-out fight to the end.
It’s been really interesting to see that conservative efforts to mount these so-called decline-to-sign campaigns, where they go out and try to just convince people not to sign the petition — those have completely failed, even in states that haven’t gotten the kind of national support and funding that Florida and Nevada and some of these states have. Even those places have met their signature goals and so they’re now moving to this next phase of the fight, which is these legal and bureaucratic challenges.
Rovner: This is going to play out, I suspect, right, almost until the last minute, in terms of getting some of these on the ballot.
Meanwhile, here on Capitol Hill, there’s an effort underway by some abortion rights backers to repeal the 1873 Comstock Act, which some anti-abortion activists say could be used to establish a national abortion ban. On the one hand, repealing the law would take away that possibility. On the other hand, suggesting that it needs to be repealed undercuts the Biden administration’s contention that the law is currently unenforceable. This seemed to be a pretty risky proposition for abortion rights forces no matter which way they go, right?
Ollstein: Well, for a while, the theory on the abortion rights side was, oh, we shouldn’t draw attention to Comstock because we don’t want to give the right the idea of using it to make a backdoor abortion ban. But that doesn’t really hold water anymore because they clearly know about it and they clearly have the idea already and are open about their desire to use it in documents like Project 2025, in letters from lawmakers urging enforcement of the Comstock Act. And so the whole …
Rovner: In concurring opinions in Supreme Court cases.
Ollstein: … Exactly, exactly. In legal filings in Supreme Court cases from the plaintiffs. So clearly, the whole “don’t give the right the idea thing” is not really the strategy anymore; the right already has the idea. And so now I think it’s more like you said, about undercutting the legal argument that it is not enforceable anyway. But those who do advocate for its repeal say, “Why wouldn’t we take this tool out of contention?” But this is sort of a philosophical fight because they don’t have the votes to repeal it anyway.
Rovner: Yeah, though I think the idea is if you bring it up you put Republicans on the record, as …
Ollstein: Sure, but they’ve been doing that on so many things. I mean, they’ve been doing that on IVF [in vitro fertilization], they’ve been doing that on contraception, they’ve been doing that on abortion, they’ve been doing it on the right to travel for an abortion. They’ve been doing it over and over and over and I don’t see a lot of evidence that it’s making a big impact in the election. I could be wrong, but I think that’s the current state of things.
Rovner: Yeah, I’m with you on that one.
All right, well, while we are all busy living our lives and talking about politics, covid is making its now annual summer comeback. President Biden is currently quarantining at his beach house in Rehoboth after testing positive. HHS [Department of Health and Human Services] Secretary Xavier Becerra was diagnosed earlier this week. And wastewater testing shows covid levels are “very high” in seven states, including big ones like Florida, Texas, and California. Sarah, do we just not care anymore? Is this just not news?
Karlin-Smith: Probably, it depends on who you ask, right? But I think obviously with Biden getting covid, it’s going to get more attention again. I think that a lot of health officials, including in the Biden administration, spent a lot of time trying to maybe optimistically hope that covid was going to become a seasonal struggle, much like flu, where we really sort of know a more defined risk period in the winter and that helps us manage it a bit. And always sort of seemed a little bit more optimistic than reality. And I think recently I’ve listened to some CDC [Centers for Disease Control and Prevention] meetings and stuff where — it’s not really, it’s a little bit subtle — but I think they’re finally kind of coming around to, oh wait, actually this is something where we probably are going to have these two peaks every year. They’re sort of year-round risk. But there hasn’t been a ton done to actually think through, OK, what does that mean for how we handle it?
In this country, every year they have been approving a second vaccine for the people most at risk, although uptake of that is incredibly low. So it does seem like it’s become a little bit of a neglected public health crisis. And certainly in the news sometimes when something kind of stays at this sort of constant level of problem, but nothing changes, it can sometimes, I think, be harder for news outlets to figure out how to draw attention to it.
Rovner: It does seem like, I mean, most of the prominent people who have been getting it have been getting mild cases. I imagine that that sort of has something to do … We’re not seeing … even Biden, who’s as we all know, 81, is quarantining at his beach house, so.
Karlin-Smith: Right, I mean, if you kind of stay up to date, as the terminology is, on your vaccinations, you don’t have a lot of high-risk conditions, if you are in certain at-risk groups you get Paxlovid. For the most part a lot of people are doing well. But that said, I think, I’m afraid to say the numbers, but if you look up the amount of deaths per week and so forth, it’s still quite high. We’re still losing — again, more people are still dying from covid every year, quite a few more than from the flu. I mean, one thing I think people have also pointed out is when new babies are born, you can’t get vaccinated until you’re 6 months. The under-6-month population has been impacted quite a bit again. So, it is that tension. And we saw it with the flu before covid, which is every year flu is actually a very big issue in the U.S. and the public health world for hospitals and stuff but the U.S. never quite put enough maybe attention or pressure to figure out how to actually change that dynamic and get better flu vaccine uptake and so forth.
Kenen: And the intense heat makes it, I mean — covid is much, much, much, much more transmissible inside than outside. And the intense heat — we’re not sitting around enjoying warm weather, we’re inside hiding from sweltering weather. We’re all in Washington or the Washington area, and it’s been hot with a capital H for weeks here, weeks. So people are inside. They can’t even be outside in the evening, it’s still hot. So we think of winter as being the indoors time in most of the country, and summer sort of the indoors time in only certain states. But right now we are in more transmissible environments for covid and …
Rovner: Meanwhile, while we’re all trying to ignore covid, we have bird flu that seems to be getting more and more serious, although people seem to just not want to think about it. We’re looking at obviously in many states bird flu spreading to dairy cows and therefore spreading to dairy workers. Sarah, we don’t really even know how big this problem is, right? Because we’re not really looking for it?
Karlin-Smith: That seems to be one of the biggest concerns of people in the public health-virology community who are criticizing the current response right now, is just we’re not testing enough, both in terms of animal populations that could be impacted and then the people that work or live closely by these animal populations, to figure out how this virus is spreading, how many people are actually impacted. Is the genetics of the virus changing? And the problem of course then is, if you don’t do this tracking, there’s a sense that we can get ourselves in a situation where it’s too late. By the time we realize something is wrong, it’s going to already be a very dangerous situation.
Rovner: Yeah, I mean, before covid, the big concern about a pandemic was bird flu. And was bird flu jumping from birds to other animals to humans, which is exactly what we’re seeing even though we’re not seeing a ton of it yet.
Kenen: We’re not seeing a ton of it, and in its current form, to the best of our knowledge, it’s not that dangerous. The fear is the more species it’s in and the more people it’s in, the more opportunities it has to become more dangerous. So, just because people have not become seriously ill, which is great, but it doesn’t mean it stays great, we just don’t — Sarah knows more about this than I do, but the flu virus mutates very easily. It combines with other flu viruses. That’s why you hear about Type A and Type B and all that. I mean, it’s not a stable virus and that is not, I’m not sure if stable is the right …
Rovner: It’s why we need a different flu shot every year.
Kenen: Right, and the flu shots we have, bird flu is different.
Rovner: Well, we will continue to watch that.
Kenen: Sarah can correct anything I just got wrong. But I think the gist was right, right?
Rovner: Sarah is nodding.
All right, well finally, one follow up from last week in the wake of the report from the Federal Trade Commission on self-dealing by pharmacy benefits managers: We get a piece from The Wall Street Journal this week [“Mail-Order Drugs Were Supposed To Keep Costs Down. It’s Doing the Opposite.”] documenting how much more mail-order pharmacies, particularly mail-order pharmacies owned by said PBMs [pharmacy benefit managers] are charging. Quoting from the story, “Branded drugs filled by mail were marked up on average three to six times higher than the cost of medicines dispensed by chain and grocery-store pharmacies, and roughly 35 times higher than those filled by independent pharmacies.” That’s according to the study commissioned by the Washington State Pharmacy Association. It’s not been a great month for the PBM industry. Sarah, I’m going to ask you what I asked the panel last week: Is Congress finally ready to do something?
Karlin-Smith: It seemed like Congress has finally been ready to do something for a while. Certainly, both sides have passed legislation and committees and so forth, and it’s been pretty bipartisan. So we’ll see. I think some of it costs — I forget if some of it costs a little money — but some of it does save. And that’s always an issue. And we know that Congress is just not very good at passing stand-alone bills on particular topics, so I think the key times will be to look at when we get to any big end-of-year funding deals and that sort of thing, depending on all the dynamics with the election and the lame duck, but …
Rovner: I mean, this has been so bipartisan. I mean, there’s bipartisan irritation in both houses, in both parties.
Karlin-Smith: Right, and I think the antitrust sort of element of this with PBMs kind of appeals to the Republican side of the aisle quite a bit. And that’s why there’s always been a bit of bipartisan interest. And the question becomes: PBMs sort of fill the role that in other countries government price negotiators fill. And that’s not particularly popular in the U.S., particularly on the Republican side of the aisle. And so most of the legislation that is pending, I think, will maybe hopefully get us to some transparency solutions, tweak some things around the edges, but it’s not really going to solve the crisis. It’s going to be, I mean, a very [Washington,] D.C. health policy move, which is kind of, take some incremental steps that might eventually move us down to later reforms, but it’s going to be slow-moving, whatever happens. So, PBMs are going to be in the spotlight for probably a while longer.
Rovner: Yes, which popular issue moves slower: drug prices or gun control?
All right, well finally this week the health policy community has lost another giant. Gail Wilensky, who ran Medicare and Medicaid under the first President Bush, and the advisory group MedPAC for many years after that, died of cancer last week at age 81. Gail managed to be both polite and outspoken at the same time. A Republican economist who worked with and disagreed with both Democrats and Republicans, and who, I think it’s fair to say, was respected by just about everyone who ever dealt with her. She taught me, and lots of others, a large chunk of what I know about health policy. She will be very much missed. Joanne, I guess you worked with her probably as long as I did.
Kenen: Yeah, I’m the one who told you she had died, right?
Rovner: That’s true.
Kenen: I think that when I heard her speak in a professional setting in the last few years, she talked to her about herself not as a Republican health economist, but as a free market health economist. She was very well respected and very well liked, but she also ended up being a person without a party. But she was a fixture and she was a nice person.
Rovner: And she wasn’t afraid to say when she was the head of MedPAC she made a lot of people angry. She made a lot of Republicans angry in some of those sort of positions that she took. She basically called it as she saw it and let the chips fall.
Kenen: And Julie, she went to Michigan, right?
Rovner: Yes, and she went to Michigan. That’s true. A fellow Michigan Wolverine. All right, well, that is the news for this week. Now we will play my interview with Renuka Rayasam, and then we will come back and do our extra credits.
I am pleased to welcome to the podcast my KFF Health News colleague Renuka Rayasam, who reported and wrote the latest KFF Health News-NPR “Bill of the Month.” It’s about what should have been a simple visit to an urgent care center but of course turned out to be anything but. Renu, thanks for joining us.
Renuka Rayasam: Thanks for having me.
Rovner: So, tell us about this month’s patient, who he is, and what kind of medical problem he had.
Rayasam: Sure, let me tell you about the patient in this month’s “Bill of the Month.” His name is Tim Chong. He’s a Dallas man, and last December he felt severe stomach pain and he didn’t know what it was from. And he thought at first maybe he’d had some food poisoning. But the pain didn’t subside and he thought, OK, I don’t want to have to pay an ER bill, so let me go to an urgent care. And he opted to visit Parkland Health’s Urgent Care Emergency Center, where he learned he had a kidney stone and was told to go home and that it would pass on its own.
Rovner: Now, we’re told all the time exactly what he was told, that if we have a health problem that needs immediate attention but probably not a hospital-level emergency, we should go to an urgent care center rather than a hospital emergency room. And most insurers encourage you to do this; they give you a big incentive by charging a far smaller copay for urgent care. So, that’s what he tried to do, right?
Rayasam: That’s what he tried to do, at least that’s what he thought he was doing. Like I said, this is a facility, it’s called Urgent Care Emergency Center. He told me that he walked in, he thought he was at an urgent care, he got checked out, was told it was a kidney stone. He actually went back five days later because his stomach pain worsened and didn’t get better. And it wasn’t until he got the bills the following month that he realized he was actually at an emergency center and not an urgent care center. His bill was $500 for each visit, not $50 for each visit as he had anticipated.
Rovner: And no one told him when he went there?
Rayasam: He said no one told him. And we reached out to Parkland Health and they said, “Well, we have notices all over the place. We label it very clearly: This is an emergency care center, you may be charged emergency care fees,” but they also sent me a picture of some of those notices and those are notices that are buried among a lot of different notices on walls. Plus, this is a person who is suffering from severe stomach pain. He was really not in a position to read those disclosures. He went by what the front desk staff did or didn’t tell him and what the name of the facility was.
Rovner: I was going to say, there was a sign that said “Urgent Care,” right?
Rayasam: Right, absolutely. Urgent Care Emergency Center, right? And so when we reached out to Parkland, they said, “Hey, we are clearly labeled as an emergency center. We’re an extension of the main emergency room.” And that’s the other thing you have to remember about this case, which is that this is the person who knew Parkland’s facility. He knew they had a separate emergency room center and he said, “I didn’t go into that building. I didn’t go into the building that’s labeled emergency room. I run into this building labeled Urgent Care Emergency Center.” Parkland says, hey, this is an extension of their main emergency room. This is where they send lower-level emergency cases, but obviously it’s a really confusing name and a really confusing setup.
Rovner: Yeah, absolutely. So, how did this all turn out? Medically, he was OK eventually, right?
Rayasam: Medically he was OK eventually. Eventually the stone did pass. And it wasn’t until he got these bills that he kind of knew what happened. When he first got the bills, he thought, well, obviously there’s some mistake. He talked to his insurer. His insurer, BlueCross and BlueShield of Texas, told him that Parkland had billed these visits using emergency room codes and he thought, wait a second, why are they using emergency room codes? I didn’t go into the emergency room. And that’s when Parkland told him, “Hey, you actually did go into an emergency room. Sorry for your confusion. You still owe us $1,000 total.” He paid part of the bills. He was trying to challenge the bills and he reached out to us at “Bill of the Month,” but eventually his bill got sent to collection and Parkland’s sort of standing by their decision to charge him $500 for each visit.
Rovner: So he basically still owes $1,000?
Rayasam: Yes, that’s right.
Rovner: So what’s the takeaway here? This feels like the ultimate bait and switch. How do you possibly make sure that a facility that says urgent care on the door isn’t actually a hospital emergency room?
Rayasam: That’s a great question. When it comes to the American medical system, unfortunately patients still have to do a lot of self-triage. One expert I’ve talked to said it’s still up to the patients to walk through the right door. Regulators have done a little bit, in Texas in particular, of making sure these facilities, these freestanding emergency room centers, as they’re called — and this one is hospital-owned, so the name is confusin, but it’s technically a freestanding emergency center, so it did have the name emergency in the name of the facility, and I think that that’s required in Texas — but I’ve talked to others who’ve said, you should ban the term urgent care from a facility that’s not urgent care. Because this is a concept that’s very familiar to most Americans. Urgent care has been around for decades; you have an idea of what an urgent care is.
And when you look at this place on its website, it’s called Urgent Care Emergency Center, it’s sort of advertised as a separate clinic within Parkland structure. It’s closed on nights, it’s closed on Sundays. The list of things they say they treat very much resembles an urgent care. So, this patient’s confusion I think is very, very understandable and he’s certainly not the only one that’s had that confusion at this facility. Regulators could ban the term urgent care for facilities that bill like emergency rooms. But until that happens it’s up to the patients to call, to check, and to ask about billing when they show up, which isn’t always easy to do when you’re suffering from severe stomach pain.
Rovner: Another thing for patients to watch out for.
Rayasam: Yes, absolutely, and worry about.
Rovner: Yes, Renuka Rayasam, thank you so much for joining.
Rayasam: Thank you, Julie.
Rovner: OK, we are back. It’s time for our extra credit segment. That’s when we each recommend a story we read this week we think you should read, too. As always, don’t worry if you miss it. We will post the links on the podcast page at kffhealthnews.org and in our show notes on your phone or other mobile device.
Sarah, why don’t you go first this week?
Karlin-Smith: Sure, I looked at a New York Times piece called “Promised Cures, Tainted Cells: How Cord Blood Banks Mislead Patients.” And it’s about the often very aggressive sort of tactics of these banks to convince women to save some of the cord blood after they give birth with the promise that it may be able to help treat your child’s illness down the road. And the investigation into this found that there’s a number of problems. One is that, for the most part, the science has progressed in a way that some of what people used to maybe use some of these cells for, they now use adult stem cells. The other is these banks are just not actually storing the products properly and much of it gets contaminated so it couldn’t even be used. Or sometimes you just don’t even collect enough, I guess, of the tissue to even be able to use it.
In one instance, they documented a family that — the bank knew that the cells were contaminated and were still charging them for quite a long time. And the other thing that I actually personally found fascinated by this — because my OB-GYN actually did kind of, I feel like, push one of these companies — was that they can pay the OB-GYNs quite a hefty fee for what seems like a very small amount of work. And it’s not subject to the same sort of kickback type of regulation that there may be for other pharmaceutical/medical device interactions between doctors and parts of the biotech industry. So I found that quite fascinating as well, what the economic incentives are to push this on people.
Rovner: Yeah. One more example of capitalism and health care being uncomfortable bedfellows, Chapter 1 Million. Joanne?
Kenen: There was a fantastic piece in The Washington Post by Annie Gowan: “A Mom Struggles To Feed Her Kids After GOP States Reject Federal Funds,” which was a long headline, but it was also a long story. But it was one of those wonderful narrative stories that really put a human face on a policy decision.
The federal government has created some extra funds for childhood nutrition, childhood food, and some of the Republican governors, including in this particular family’s case, the Republican Gov. Kevin Stitt in Oklahoma, have turned down these funds. And families … So this is a single, full-time working mom. She is employed. She’s got three teenagers. They’re all athletic and active and hungry and she doesn’t have enough food for them. And particularly in the summer when they don’t get meals in school, the struggle to get enough food, she goes without meals. Her kids — one of the kids actually works in the food pantry where they get their food from. The amount of time and energy this mom spends just making sure her children get fed when there is a source of revenue that her state chose not to us: It’s a really, really good story. It’s long, but I read it all even before Julie sent it to me. I said, “I already read that one.” It’s really very good and it’s very human. And, why?
Rovner: Policy affects real people.
Kenen: This is hungry teenagers.
Rovner: It’s one of things that journalism is for.
Kenen: Right, right, and they’re also not eating real healthy food because they’re not living on grapefruits and vegetables. They’re living on starchy stuff.
Rovner: Alice?
Ollstein: I chose a good piece from ProPublica called “Texas Sends Millions to Crisis Pregnancy Centers. It’s Meant To Help Needy Families, but No One Knows if It Works.” And it is about just how little oversight there is of the budgets of taxpayer dollars that are going to these anti-abortion centers that in many cases use the majority of funding not for providing services. A lot of it goes to overhead. And so there’s a lot of fascinating details in there. These centers can bill the state a lot of money just for handing out pamphlets, for handing out supplies that were donated that they got for free. They get to charge the state for handing those out. And there’s just not a lot of evaluation of, is this serving people? Is this improving health outcomes? And I think it’s a good critical look at this as other states are moving towards adopting similar programs to what’s going on in Texas.
Rovner: Yeah, we’re seeing a lot of states put a lot of money towards some of these centers.
Well, my extra credit this week is from Time magazine. It’s called, “‘We’re Living in a Nightmare:’ Inside the Health Crisis of a Texas Bitcoin Town,” by Andrew Chow. And in case we didn’t already have enough to worry about, it seems that the noise that comes from the giant server farms used to mine bitcoin can cause all manner of health problems for those in the surrounding areasm from headaches to nausea and vomiting to hypertension. At a local meeting, one resident reported that “her 8-year-old daughter was losing her hearing and fluids were leaking from her ears.”
The company that operates the bitcoin plant says it’s in the process of moving to a quieter cooling system. That’s what makes all the noise. But as cryptocurrency mining continues to grow and spread, it’s likely that other communities will be affected in the way the people of Granbury, Texas, have been.
All right. That is our show for this week. As always, if you enjoy the podcast, you can subscribe wherever you get your podcast. We’d appreciate it if you left us a review; that helps other people find us, too. Special thanks as always to our technical guru, Francis Ying, and our editor, Emmarie Huetteman. As always, you can email us your comments or questions. We’re at whatthehealth@kff.org, or you can still find me at X, I’m @jrovner. Sarah, where are you these days?
Karlin-Smith: I’m mostly on X @SarahKarlin or on some other platforms like Bluesky, at @sarahkarlin-smith.
Rovner: Alice?
Ollstein: I’m on X @AliceOllstein and on Bluesky @alicemiranda.
Rovner: Joanne?
Kenen: A little bit on X @JoanneKenen and a little bit on Threads @joannekenen1.
Rovner: We will be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 3 months ago
Courts, COVID-19, Health Industry, Multimedia, Public Health, Abortion, Audio, Biden Administration, Drug Costs, KFF Health News' 'What The Health?', Obamacare Plans, Podcasts, reproductive health, Trump Administration, vaccines, Women's Health
California Health Care Pioneer Goes National, Girds for Partisan Skirmishes
SACRAMENTO — When then-Gov. Arnold Schwarzenegger called for nearly all Californians to buy health insurance or face a penalty, Anthony Wright slammed the 2007 proposal as “unwarranted, unworkable, and unwise” — one that would punish those who could least afford coverage.
The head of Health Access California, one of the state’s most influential consumer groups, changed course only after he and his allies extracted a deal to increase subsidies for people in need.
The plan was ultimately blocked by Democrats who wanted the state to adopt a single-payer health care system instead. Yet the moment encapsulates classic Anthony Wright: independent-minded and willing to compromise if it could help Californians live healthier lives without going broke.
This summer, Wright will assume the helm of the health consumer group Families USA, taking his campaign for more affordable and accessible health care to the national level and a deeply divided Congress. In his 23 years in Sacramento, Wright has successfully lobbied to outlaw surprise medical billing, require companies to report drug price increases, and cap hospital bills for uninsured patients — policies that have spread nationwide.
“He pushed the envelope and gave people aspirational leadership,” said Jennifer Kent, who served as Schwarzenegger’s head of the Department of Health Care Services, which administers the state Medicaid program. The two were often on opposing sides on health policy issues. “There was always, like, one more thing, one more goal, one more thing to achieve.”
Recently, Wright co-led a coalition of labor and immigrant rights activists to provide comprehensive Medicaid benefits to all eligible California residents regardless of immigration status. The state funds this coverage because the federal government doesn’t allow it.
His wins have come mostly under Democratic governors and legislatures and when Republican support hasn’t been needed. That will not be the case in Washington, D.C., where Republicans currently control the House and the Senate Democratic Caucus has a razor-thin majority, which has made it extremely difficult to pass substantive legislation. November’s elections are not expected to ease the partisan impasse.
Though both Health Access and Families USA are technically nonpartisan, they tend to align with Democrats and lobby for Democratic policies, including abortion rights. But “Anthony doesn’t just talk to his own people,” said David Panush, a veteran Sacramento health policy consultant. “He has an ability to connect with people who don’t agree with you on everything.”
Wright, who interned for Vice President Al Gore and worked as a consumer advocate at the Federal Communications Commission in his 20s, acknowledges his job will be tougher in the nation’s capital, and said he is “wide-eyed about the dysfunction” there. He said he also plans to work directly with state lawmakers, including encouraging those in the 10, mostly Republican states that have not yet expanded Medicaid under the Affordable Care Act to do so.
In an interview with California Healthline senior correspondent Samantha Young, Wright, 53, discussed his accomplishments in Sacramento and the challenges he will face leading a national consumer advocacy group. His remarks have been edited for length and clarity.
Q: Is there something California has done that you’d like to see other states or the federal government adopt?
Just saying “We did this in California” is not going to get me very far in 49 other states. But stuff that has already gone national, like the additional assistance to buy health care coverage with state subsidies, that became something that was a model for what the federal government did in the American Rescue Plan [Act] and the Inflation Reduction Act. Those additional tax credits have had a huge impact. About 5 million Americans have coverage because of them. Yet, those additional tax credits expire in 2025. If those tax credits expire, the average premium will spike $400 a month.
Q: You said you will find yourself playing defense if former President Donald Trump is elected in November. What do you mean?
Our health is on the ballot. I worry about the Affordable Care Act and the protections for preexisting conditions, the help for people to afford coverage, and all the other consumer patient protections. I think reproductive health is obviously front and center, but that’s not the only thing that could be taken away. It could also be something like Medicare’s authority to negotiate prices on prescription drugs.
Q: But Trump has said he doesn’t want to repeal the ACA this time, rather “make it better.”
We just need to look at the record of what was proposed during his first term, which would have left millions more people uninsured, which would have spiked premiums, which would have gotten rid of key patient protections.
Q: What’s on your agenda if President Joe Biden wins reelection?
It partially depends on the makeup of Congress and other elected officials. Do you extend this guarantee that nobody has to spend more than 8.5% of their income on coverage? Are there benefits that we can actually improve in Medicare and Medicaid with regard to vision and dental? What are the cost drivers in our health system?
There is a lot we can do at both the state and the federal level to get people both access to health care and also financial security, so that their health emergency doesn’t become a financial emergency as well.
Q: Will it be harder to get things done in a polarized Washington?
The dysfunction of D.C. is a real thing. I don’t have delusions that I have any special powers, but we will try to do our best to make progress. There are still very stark differences, whether it’s about the Affordable Care Act or, more broadly, about the social safety net. But there’s always opportunities for advancing an agenda.
There could be a lot of common ground on areas like health care costs and having greater oversight and accountability for quality in cost and quality in value, for fixing market failures in our health system.
Q: What would happen in California if the ACA were repealed?
When there was the big threat to the ACA, a lot of people thought, “Can’t California just do its own thing?” Without the tens of billions of dollars that the Affordable Care Act provides, it would have been very hard to sustain. If you get rid of those subsidies, and 5 million Californians lose their coverage, it becomes a smaller and sicker risk pool. Then premiums spike up for everybody, and, basically, the market becomes a death spiral that will cover nobody, healthy or sick.
Q: California expanded Medicaid to qualified immigrants living in the state without authorization. Do you think that could happen at the federal level?
Not at the moment. I would probably be more focused on the states that are not providing Medicaid to American citizens [who] just happen to be low-income. They are turning away precious dollars that are available for them.
Q: What do you take away from your time at Health Access that will help you in Washington?
It’s very rare that anything of consequence is done in a year. In many cases, we’ve had to run a bill or pursue a policy for multiple years or sessions. So, the power of persistence is that if you never give up, you’re never defeated, only delayed. Prescription drug price transparency took three years, surprise medical bills took three years, the hospital fair-pricing act took five years.
Having a coalition of consumer voices is important. Patients and the public are not just another stakeholder. Patients and the public are the point of the health care system.
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 3 months ago
california, Health Care Costs, Health Industry, Insurance, Medicaid, Medicare, Spotlight, States, Obamacare Plans, U.S. Congress
Pain Doesn’t Belong on a Scale of Zero to 10
Over the past two years, a simple but baffling request has preceded most of my encounters with medical professionals: “Rate your pain on a scale of zero to 10.”
I trained as a physician and have asked patients the very same question thousands of times, so I think hard about how to quantify the sum of the sore hips, the prickly thighs, and the numbing, itchy pain near my left shoulder blade. I pause and then, mostly arbitrarily, choose a number. “Three or four?” I venture, knowing the real answer is long, complicated, and not measurable in this one-dimensional way.
Pain is a squirrely thing. It’s sometimes burning, sometimes drilling, sometimes a deep-in-the-muscles clenching ache. Mine can depend on my mood or how much attention I afford it and can recede nearly entirely if I’m engrossed in a film or a task. Pain can also be disabling enough to cancel vacations, or so overwhelming that it leads people to opioid addiction. Even 10+ pain can be bearable when it’s endured for good reason, like giving birth to a child. But what’s the purpose of the pains I have now, the lingering effects of a head injury?
The concept of reducing these shades of pain to a single number dates to the 1970s. But the zero-to-10 scale is ubiquitous today because of what was called a “pain revolution” in the ’90s, when intense new attention to addressing pain — primarily with opioids — was framed as progress. Doctors today have a fuller understanding of treating pain, as well as the terrible consequences of prescribing opioids so readily. What they are learning only now is how to better measure pain and treat its many forms.
About 30 years ago, physicians who championed the use of opioids gave robust new life to what had been a niche specialty: pain management. They started pushing the idea that pain should be measured at every appointment as a “fifth vital sign.” The American Pain Society went as far as copyrighting the phrase. But unlike the other vital signs — blood pressure, temperature, heart rate, and breathing rate — pain had no objective scale. How to measure the unmeasurable? The society encouraged doctors and nurses to use the zero-to-10 rating system. Around that time, the FDA approved OxyContin, a slow-release opioid painkiller made by Purdue Pharma. The drugmaker itself encouraged doctors to routinely record and treat pain, and aggressively marketed opioids as an obvious solution.
To be fair, in an era when pain was too often ignored or undertreated, the zero-to-10 rating system could be regarded as an advance. Morphine pumps were not available for those cancer patients I saw in the ’80s, even those in agonizing pain from cancer in their bones; doctors regarded pain as an inevitable part of disease. In the emergency room where I practiced in the early ’90s, prescribing even a few opioid pills was a hassle: It required asking the head nurse to unlock a special prescription pad and making a copy for the state agency that tracked prescribing patterns. Regulators (rightly) worried that handing out narcotics would lead to addiction. As a result, some patients in need of relief likely went without.
After pain doctors and opioid manufacturers campaigned for broader use of opioids — claiming that newer forms were not addictive, or much less so than previous incarnations — prescribing the drugs became far easier and were promoted for all kinds of pain, whether from knee arthritis or back problems. As a young doctor joining the “pain revolution,” I probably asked patients thousands of times to rate their pain on a scale of zero to 10 and wrote many scripts each week for pain medication, as monitoring “the fifth vital sign” quickly became routine in the medical system. In time, a zero-to-10 pain measurement became a necessary box to fill in electronic medical records. The Joint Commission on the Accreditation of Healthcare Organizations made regularly assessing pain a prerequisite for medical centers receiving federal health care dollars. Medical groups added treatment of pain to their list of patient rights, and satisfaction with pain treatment became a component of post-visit patient surveys. (A poor showing could mean lower reimbursement from some insurers.)
But this approach to pain management had clear drawbacks. Studies accumulated showing that measuring patients’ pain didn’t result in better pain control. Doctors showed little interest in or didn’t know how to respond to the recorded answer. And patients’ satisfaction with their doctors’ discussion of pain didn’t necessarily mean they got adequate treatment. At the same time, the drugs were fueling the growing opioid epidemic. Research showed that an estimated 3% to 19% of people who received a prescription for pain medication from a doctor developed an addiction.
Doctors who wanted to treat pain had few other options, though. “We had a good sense that these drugs weren’t the only way to manage pain,” Linda Porter, director of the National Institutes of Health’s Office of Pain Policy and Planning, told me. “But we didn’t have a good understanding of the complexity or alternatives.” The enthusiasm for narcotics left many varietals of pain underexplored and undertreated for years. Only in 2018, a year when nearly 50,000 Americans died of an overdose, did Congress start funding a program — the Early Phase Pain Investigation Clinical Network, or EPPIC-Net — designed to explore types of pain and find better solutions. The network connects specialists at 12 academic specialized clinical centers and is meant to jump-start new research in the field and find bespoke solutions for different kinds of pain.
A zero-to-10 scale may make sense in certain situations, such as when a nurse uses it to adjust a medication dose for a patient hospitalized after surgery or an accident. And researchers and pain specialists have tried to create better rating tools — dozens, in fact, none of which was adequate to capture pain’s complexity, a European panel of experts concluded. The Veterans Health Administration, for instance, created one that had supplemental questions and visual prompts: A rating of 5 correlated with a frown and a pain level that “interrupts some activities.” The survey took much longer to administer and produced results that were no better than the zero-to-10 system. By the 2010s, many medical organizations, including the American Medical Association and the American Academy of Family Physicians, were rejecting not just the zero-to-10 scale but the entire notion that pain could be meaningfully self-reported numerically by a patient.
In the years that opioids had dominated pain remedies, a few drugs — such as gabapentin and pregabalin for neuropathy, and lidocaine patches and creams for musculoskeletal aches — had become available. “There was a growing awareness of the incredible complexity of pain — that you would have to find the right drugs for the right patients,” Rebecca Hommer, EPPIC-Net’s interim director, told me. Researchers are now looking for biomarkers associated with different kinds of pain so that drug studies can use more objective measures to assess the medications’ effect. A better understanding of the neural pathways and neurotransmitters that create different types of pain could also help researchers design drugs to interrupt and tame them.
Any treatments that come out of this research are unlikely to be blockbusters like opioids; by design, they will be useful to fewer people. That also makes them less appealing prospects to drug companies. So EPPIC-Net is helping small drug companies, academics, and even individual doctors design and conduct early-stage trials to test the safety and efficacy of promising pain-taming molecules. That information will be handed over to drug manufacturers for late-stage trials, all with the aim of getting new drugs approved by the FDA more quickly.
The first EPPIC-Net trials are just getting underway. Finding better treatments will be no easy task, because the nervous system is a largely unexplored universe of molecules, cells, and electronic connections that interact in countless ways. The 2021 Nobel Prize in Physiology or Medicine went to scientists who discovered the mechanisms that allow us to feel the most basic sensations: cold and hot. In comparison, pain is a hydra. A simple number might feel definitive. But it’s not helping anyone make the pain go away.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 3 months ago
Health Care Reform, Health Industry, Opioids