How to stay safe this Christmas
IT IS Christmas Day, and you want to enjoy yourself, that is only natural! The holiday period is commonly a time of overindulgence, with almost infinite food at our fingertips, it can be difficult not to go overboard. Studies have found that...
IT IS Christmas Day, and you want to enjoy yourself, that is only natural! The holiday period is commonly a time of overindulgence, with almost infinite food at our fingertips, it can be difficult not to go overboard. Studies have found that...
1 year 10 months ago
The Market for Biosimilars Is Funky. The Industry Thinks PBMs Are To Blame
Over the past year there’s been movement to rein in the three big PBMs, which face little regulation though they help set drug prices and drug choices for 80 percent of Americans and their doctors.
The House voted Dec. 11, 320-71, for legislation that would require the PBMs to change some of the ways they do business. The big three — CVS Health, Express Scripts, and OptumRx — have all announced their own reform measures in recent months.
The bill looks unlikely to pass the Senate, though some of its provisions might eventually become law. Meanwhile, some of the most baffling contradictions of PBM drug pricing are coming to a head.
Take AbbVie’s Humira, the highest-earning drug ever. Eight biosimilars — what ordinary people would call generics — came onto the market this year, raising hopes of big savings for patients and insurers. Some cost as little as $995 a month, compared to Humira’s wholesale price of $6,992.
The Pharmaceutical Care Management Association, which represents the big PBMs, told KFF Health News in a statement that its members are pushing to use more of the biosimilars. Why then, asks Juliana Reed, CEO of the Biosimilars Forum trade group, did Humira account for 98.5 percent of all sales of the drug and its biosimilars as recently as November?
I’ve been told that AbbVie has threatened to withhold rebates it pays PBMs for some of its other medicines unless they give Humira good placement on formularies, the all-important lists of drugs available to their customers. The PBMs say their formularies provide the best deal for employers, but these are “assertions impossible to verify,” says James Gelfand, president and CEO of The ERISA Industry Committee, which represents large employers.
The PBMs’ strategy is purposefully obscure. Negotiations with drugmakers constitute their special sauce and they aren’t sharing the ingredients. But given that it costs up to $300 million to develop a biosimilar, the Humira battle is key to the future of biosimilars in general, and to more competition to lower expensive drug prices.
“If you can’t break into anti-inflammatory drugs it will be hard to break into any model,” Gelfand said. “It’s the weather vane, the shape of things to come.”
There’s more weird stuff going on with biosimilars. To get Inflectra, its biosimilar to Johnson & Johnson’s blockbuster Remicade, onto formularies, Pfizer pays large rebates to insurers, I’ve been told.
That’s driven down average net prices for Inflectra as well as other versions of the drug.
Good, right? Not according to rheumatologists, the doctors who typically administer these complicated, infused drugs in their offices.
The doctors say they still have to pay much higher prices to obtain Inflectra from distributors. But their reimbursement from Medicare is reduced because of the rebates, they say. Several rheumatologists told me that the way the math works out — or rather, doesn’t — they could lose as much as $20,000 a year on each patient.
The choice is “lose money, or divert the patient to a hospital infusion center,” said Chris Phillips, a doctor in Paducah, Ky., who chairs the American College of Rheumatology’s insurance subcommittee. The latter is “more expensive and usually not as good an experience for the patient.”
Payment imbalances also have developed for Amgen’s Avsola, another Remicade biosimilar, and for biosimilar forms of Genentech’s Rituxan, a cancer drug also infused to treat autoimmune conditions, rheumatologists say.
“The whole point of biosimilars is to make these drugs more accessible, but they’re becoming unaffordable,” said Madelaine Feldman, immediate past president of the Coalition of State Rheumatology Organizations.
Spokespeople for Pfizer and for the Pharmaceutical Care Management Association acknowledged the rheumatologists’ dilemma. Each said it was up to the other to resolve the problem.
This article is not available for syndication due to republishing restrictions. If you have questions about the availability of this or other content for republication, please contact NewsWeb@kff.org.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 10 months ago
Health Care Costs, Health Industry, Pharmaceuticals, Prescription Drugs, The Health 202
STAT+: Pharmalittle: Weight loss drugs are being paired with bariatric surgery; Carl Icahn plans to oust Illumina directors
Top of the morning to you. And a fine one it is. Lots of sunshine and clear blue skies are enveloping the Pharmalot campus, where the official mascots are bounding about the grounds and the short person has departed for a challenging apprenticeship. As for us, we are as busy as ever hunting and gathering items of interest.
We trust you have your own busy agendas. So join us as we hoist the ever-present cup of stimulation — our choice today is gingerbread — and attack the fast-growing to-do list. We hope you have a smashing day and, of course, do stay in touch. Our settings are adjusted to accept postcards and telegrams. …
Activist investor Carl Icahn plans to oust directors at Illumina, laying the groundwork for a second board challenge at the gene-sequencing company months after shareholders elected one of his director candidates, Reuters writes. Icahn disclosed his plans without offering details in a letter to other shareholders less than 24 hours after Illumina said it will divest blood test maker Grail. In Monday’s letter, Icahn blamed the Grail acquisition, which has faced regulatory challenges since 2021, for a 75% drop in Illumina’s share price that he says wiped away $55 billion in value for shareholders. The stock was up more than 2% at $130.39 on Monday.
As more data emerge that obesity drugs like Wegovy can reduce complications from heart and kidney problems as well, scientists have been wondering whether these benefits are driven by weight loss alone or also by other mechanisms. A new study suggests that one possible contributor is the drugs’ ability to reduce inflammation independent of weight loss, STAT tells us. In mice experiments, scientists found that the treatments, known as GLP-1-based drugs, acted through the brain to reduce inflammation throughout the body. This was over a short period of time before the mice lost weight, according to the study, published Monday in Cell Metabolism.
1 year 10 months ago
Pharma, Pharmalot, pharmalittle, STAT+
When a Quick Telehealth Visit Yields Multiple Surprises Beyond a Big Bill
In September 2022, Elyse Greenblatt of Queens returned home from a trip to Rwanda with a rather unwelcome-back gift: persistent congestion.
She felt a pain in her sinuses and sought a quick resolution.
In September 2022, Elyse Greenblatt of Queens returned home from a trip to Rwanda with a rather unwelcome-back gift: persistent congestion.
She felt a pain in her sinuses and sought a quick resolution.
Covid-19 couldn’t be ruled out, so rather than risk passing on an unknown infection to others in a waiting room, the New Yorker booked a telehealth visit through her usual health system, Mount Sinai — a perennial on best-hospitals lists.
That proved an expensive decision. She remembers the visit as taking barely any time. The doctor decided it was likely a sinus infection, not covid, and prescribed her fluticasone, a nasal spray that relieves congestion, and an antibiotic, Keflex. (The Centers for Disease Control and Prevention says antibiotics “are not needed for many sinus infections, but your doctor can decide if you need” one.)
Then the bill came.
The Patient: Elyse Greenblatt, now 38, had insurance coverage through Empire BlueCross BlueShield, a New York-based insurer.
Medical Services: A telehealth urgent care visit through Mount Sinai’s personal record app. Greenblatt was connected with an urgent care doctor through the luck of the draw. She was diagnosed with sinusitis, prescribed an antibiotic and Flonase, and told to come back if there was no improvement.
All this meant a big bill. The insurer said the telehealth visit was deemed an out-of-network service — a charge Greenblatt said the digital service didn’t do a great job of warning her about. It came as a surprise. “In my mind, if all my doctors are ‘in-insurance,’ why would they pair me with someone who was ‘out-of-insurance’?” she asked. And the hospital system tried its best to make contesting the charge difficult, she said.
Service Provider: The doctor was affiliated with Mount Sinai’s health system, though where the bill came from was unclear: Was it from one of the system’s hospitals or another unit?
Total Bill: $660 for what was billed as a 45- to 59-minute visit. The insurer paid nothing, ruling it out of network.
What Gives: The bill was puzzling on multiple levels. Most notably: How could this be an out-of-network service? Generally, urgent care visits delivered via video are a competitive part of the health care economy, and they’re not typically terribly expensive.
Mount Sinai’s telehealth booking process is at pains to assure bookers they’re getting a low price. After receiving the bill, Greenblatt went back to the app to recreate her steps — and she took a screenshot of one particular part of the app: the details. She got an estimated wait time of 10 minutes, for a cost of $60. “Cost may be less based on insurance,” the app said; this information, Mount Sinai spokesperson Lucia Lee said, is “for the patient’s benefit,” and the “cost may differ depending on the patient’s insurance.”
A $60 fee would be in line with, if not a bit cheaper than, many other telehealth services. Doctor on Demand, for example, offers visits from a clinician for $79 for a 15-minute visit, assuming the customer’s insurance doesn’t cover it. Amazon’s new clinic service, offering telehealth care for a wide range of conditions, advertises that charges start at $30 for a sinus infection.
The Health Care Cost Institute, an organization that analyzes health care claims data, told KFF Health News its data shows an urgent care telehealth visit runs, on average, $120 in total costs — but only $14 in out-of-pocket charges.
So how did this visit end up costing astronomically so much more than the average? After all, one of the selling points of telemedicine is not only convenience but cost savings.
First, there was the length of the visit. The doctor’s bill described it as moderately lengthy. But Greenblatt recalled the visit as simple and straightforward; she described her symptoms and got an antibiotic prescription — not a moderately complex visit requiring the better part of an hour to resolve.
The choice of description is a somewhat wonky part of health care billing that plays a big part in how expensive care can get. The more complex the case, and the longer it takes to diagnose and treat, the more providers can charge patients and insurers.
Greenblatt’s doctor billed her at a moderate level of care — curious, given her memory of the visit as quick, almost perfunctory. “I think it was five minutes,” she recalled. “I said it was a sinus infection; she told me I was right. ‘Take some meds, you’ll be fine.’”
Ishani Ganguli, a doctor at Brigham and Women’s Hospital in Boston who studies telehealth, said she didn’t know the exact circumstances of care but was “a bit surprised that it was not billed at a lower level” if it was indeed a quick visit.
That leaves the out-of-network aspect of the bill, allowing the insurer to pay nothing for the care. (Stephanie DuBois, a spokesperson for Empire BlueCross BlueShield, Greenblatt’s insurer, said the payer covers virtual visits through two services, or through in-network doctors. The Mount Sinai doctor fit neither criteria.) Still, why did Mount Sinai, Greenblatt’s usual health care system, assign her an out-of-network doctor?
“If one gets their care from the Mount Sinai system and the care is within network, I don’t think it is reasonable for the patients to expect or understand that one of the Mount Sinai clinicians is suddenly going to be out of network,” said Ateev Mehrotra, a hospitalist and telehealth researcher at Beth Israel Deaconess Medical Center.
It struck the doctors specializing in telehealth research whom KFF Health News consulted as an unusual situation, especially since the doctor who provided the care was employed by the prestigious health system.
The doctor in question may have been in network for no insurers whatsoever: A review of the doctor’s Mount Sinai profile page — archived in November 2022 — does not list any accepted insurance. (That’s in contrast to other doctors in the system.)
Lee, Mount Sinai’s spokesperson, said the doctor did take at least some insurance. When asked about the doctor’s webpage not showing any accepted plans, she responded the site “instructs patients to contact her office for the most up-to-date information.”
Attempting to solve this billing puzzle turned into a major league headache for Greenblatt. Deepening the mystery: After calling Mount Sinai’s billing department, she was told the case had been routed to disputes and marked as “urgent.”
But the doctor’s office would seemingly not respond. “In most other professions, you can’t just ignore a message for a year,” she observed.
The bill would disappear on her patient portal, then come back again. Another call revealed a new twist: She was told by a staffer that she’d signed a form consenting to the out-of-network charge. But “when I asked to get a copy of the form I signed, she asked if she could fax it,” Greenblatt said. Greenblatt said no. The billing department then asked whether they could put the form in her patient portal, for which Greenblatt gave permission. No form materialized.
When KFF Health News asked Mount Sinai about the case in mid-October of this year, Lee, the system’s spokesperson, forwarded a copy of the three-page form — which Greenblatt didn’t remember signing. Lee said the forms are presented as part of the flow of the check-in process and “intended to be obvious to the patient as required by law.” Lee said on average, a patient signs two to four forms before checking into the visit.
But, according to the time stamp on the forms, Greenblatt’s visit concluded before she signed. Lee said it is “not standard” to sign forms after the visit has concluded, and said that once informed, patients “may contact the office and reschedule with an ‘in-network provider.’”
“If it was provided after the service was rendered, that is an exception and situational,” she concluded.
The business with the forms — their timing and their obviousness — is potentially a vital distinction. In December 2020, Congress enacted the No Surprises Act, designed to crack down on so-called surprise medical bills that arise when patients think their care is covered by insurance but actually isn’t. Allie Shalom, a lawyer with Foley & Lardner, said the law requires notice to be given to patients, and consent obtained in advance.
More from Bill of the Month
-
Out for Blood? For Routine Lab Work, the Hospital Billed Her $2,400
Nov 21, 2023
-
When That Supposedly Free Annual Physical Generates a Bill
Oct 30, 2023
-
She Received Chemo in Two States. Why Did It Cost So Much More in Alaska?
Sep 29, 2023
But the legislation provides an exception. It applies only to hospitals, hospital outpatient facilities, critical access hospitals, and ambulatory surgery centers. Greenblatt’s medical bill variously presents her visit as “Office/Outpatient” or “Episodic Telehealth,” making it hard to “tell the exact entity that provided the services,” Shalom said.
That, in turn, makes its status under the No Surprises Act unclear. The rules apply when an out-of-network provider charges a patient for care received at an in-network facility. But Shalom couldn’t be sure what entity charged Greenblatt, and, therefore, whether that entity was in network.
As for Mount Sinai, Lee said asking for consent post-visit does not comply with the No Surprises Act, though she said the system needed more time to research whether Greenblatt was billed by the hospital or another entity.
The Resolution: Greenblatt’s bill is unpaid and unresolved.
The Takeaway: Unfortunately, patients need to be on guard to protect their wallets.
If you want to be a smart shopper, consider timing the length of your visit. The “Bill of the Month” team regularly receives submissions from patients who were billed for a visit significantly longer than what took place. You shouldn’t, for example, be charged for time sitting in a virtual waiting room.
Most important, even when you seek care at an in-network hospital, whose doctors are typically in network, always ask if a particular physician you’ve not seen before is in your network. Many practices and hospitals offer providers in both categories (even if that logically feels unfair to patients). Providers are supposed to inform you that the care being rendered is out of network. But that “informed consent” is often buried in a pile of consent forms that you auto-sign, in rapid fire. And the language is often a blanket statement, such as “I understand that some of my care may be provided by caregivers not in my insurance network” or “I agree to pay for services not covered by my insurance.”
To a patient trying to quickly book care, that may not feel like “informed consent” at all.
“It’s problematic to expect patients to read the fine print, especially when they feel unwell,” Ganguli said.
Emily Siner reported the audio story.
Bill of the Month is a crowdsourced investigation by KFF Health News and NPR that dissects and explains medical bills. Do you have an interesting medical bill you want to share with us? Tell us about it!
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 10 months ago
Health Care Costs, Health Industry, Insurance, Multimedia, States, Audio, Bill Of The Month, Doctor Networks, Health IT, Insurers, Investigation, New York, Surprise Bills, Telemedicine
PAHO/WHO | Pan American Health Organization
Four Latin American countries use thermotherapy to treat cutaneous leishmaniasis in vulnerable populations
Four Latin American countries use thermotherapy to treat cutaneous leishmaniasis in vulnerable populations
Oscar Reyes
18 Dec 2023
Four Latin American countries use thermotherapy to treat cutaneous leishmaniasis in vulnerable populations
Oscar Reyes
18 Dec 2023
1 year 10 months ago
Fixed-duration pirtobrutinib plus venetoclax, rituximab promising in CLL
Fixed-duration pirtobrutinib plus venetoclax with or without rituximab was well tolerated and showed promising efficacy in patients with relapsed or refractory chronic lymphocytic leukemia, according to data presented at ASH Annual Meeting.Lindsey E.
Roeker, MD, of Memorial Sloan Kettering Cancer Center, and colleagues examined the safety and efficacy of fixed-duration pirtobrutinib (Jaypirca, Eli Lilly & Co. — a noncovalent Bruton tyrosine kinase inhibitor — combined with venetoclax (Venclexta; Genentech, AbbVie) with and without rituximab (Rituxan; Genentech, Biogen) in
1 year 10 months ago
Specialists have highlighted tips to ensure proper food handling and to recognize symptoms that require attention
SANTO DOMINGO.- In anticipation of the Christmas and New Year festivities, Elianet Castillo, an infectious disease specialist at the Medical Center for Diabetes, Obesity, and Specialties (CEMDOE), has urged people to maintain healthy habits to prevent food poisoning through safe practices for individuals and families.
“Food poisoning is a syndrome caused by consuming food contaminated with microorganisms, toxins, or chemicals. It is associated with more than 250 pathogens, particularly when food is mishandled,” the specialist explained.
The foods most commonly linked to food poisoning include undercooked or improperly reheated meats, eggs, creams, mayonnaise, unpasteurized milk, seafood, fruits, and vegetables.
She noted that symptoms of food poisoning, such as nausea, vomiting, diarrhea, abdominal cramps, general malaise, and sometimes fever, usually appear abruptly and can start within six hours after consuming contaminated food.
“A sign of food poisoning is that multiple people who consumed the same contaminated source are affected. Symptoms typically last a few days, and most people recover well without medical treatment. However, in immunocompromised individuals (like cancer patients, those on steroids, or other immunosuppressive medications), and patients with comorbidities like heart disease, chronic kidney disease, and diabetes, the illness can be more severe or prolonged, requiring specialized medical care,” stated the specialist from the center accredited by the Joint Commission International (JCI).
According to international food safety standards, Dr. Castillo recommends eight tips to reduce the risk of contracting foodborne illnesses: wash hands and surfaces where food will be handled; wash fruits and vegetables; separate foods to avoid cross-contamination between fruits, vegetables, meats, seafood, poultry, and eggs; wash utensils that have been in contact with these foods, especially if they were raw.
Additionally, she advises cooking food to the correct temperature; ensuring that reheated food is completely cooked or heated before consumption; not leaving perishable foods out of the refrigerator for more than an hour; and not marinating foods on the kitchen counter, instead marinating in the refrigerator.
About CEMDOE:
CEMDOE is an outpatient medical institution accredited by the Joint Commission International. It focuses on providing comprehensive, safe, and quality care centered on the patient and their family. The center offers over 45 specialties, a clinical laboratory, a state-of-the-art imaging center, endoscopy, a multipurpose operating room, hemodialysis, and a specialized diabetic foot area. CEMDOE is part of INTEGRA, a health asset manager.
1 year 10 months ago
Health
Morning Rounds: Why some doctors plan to quit their jobs
Understand how science, health policy, and medicine shape the world everyday. Sign up for our Morning Rounds newsletter here.
Understand how science, health policy, and medicine shape the world everyday. Sign up for our Morning Rounds newsletter here.
Good morning folks, we’re almost there! The shortest day of the year is this week. It’s also our last week of Morning Rounds before a break for the holidays, and the last Monday from me for 2023. See you next year!
1 year 10 months ago
Uncategorized
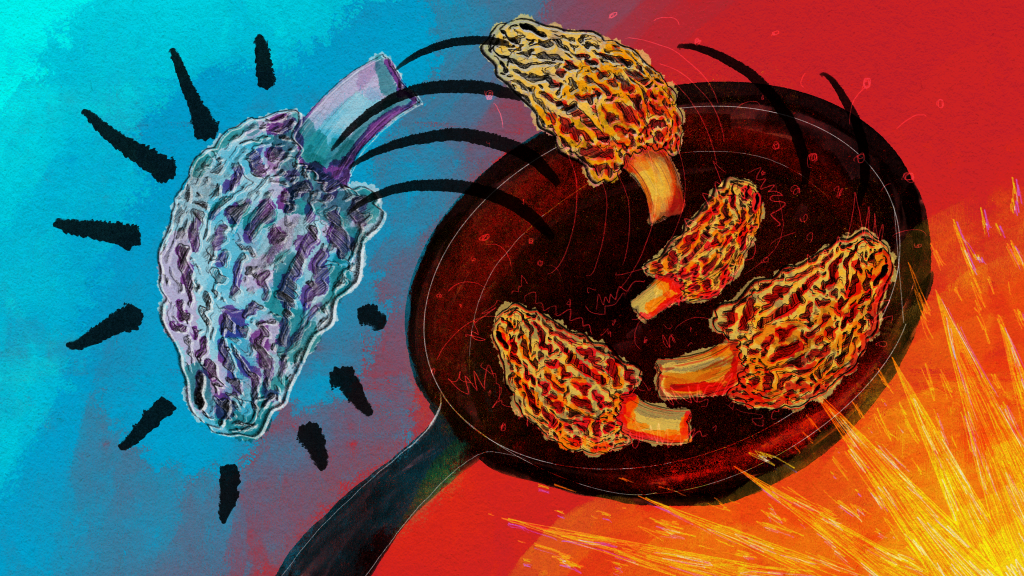
Mysterious Morel Mushrooms at Center of Food Poisoning Outbreak
A food poisoning outbreak that killed two people and sickened 51, stemming from a Montana restaurant, has highlighted just how little is known about morel mushrooms and the risks in preparing the popular and expensive delicacy.
The FDA conducted an investigation into morel mushrooms after the severe illness outbreak linked to Dave’s Sushi in Bozeman in late March and April. The investigation found that undercooked or raw morels were the likely culprit, and it led the agency to issue its first guidelines on preparing morels.
“The toxins in morel mushrooms that may cause illness are not fully understood; however, using proper preparation procedures, such as cooking, can help to reduce toxin levels,” according to the FDA guidance.
Even then, a risk remains, according to the FDA: “Properly preparing and cooking morel mushrooms can reduce risk of illness, however there is no guarantee of safety even if cooking steps are taken prior to consumption.”
Jon Ebelt, spokesperson for Montana’s health department, said there is limited public health information or medical literature on morels. And samples of the morels taken from Dave’s Sushi detected no specific toxin, pathogen, pesticide, or volatile or nonvolatile organic compound in the mushrooms.
Aaron Parker, the owner of Dave’s Sushi, said morels are a “boutique item.” In season, generally during the spring and fall, morels can cost him $40 per pound, while morels purchased out of season are close to $80 per pound, he said.
Many highly regarded recipe books describe sauteing morels to preserve the sought-after, earthy flavor. At Dave’s, a marinade, sometimes boiling, was poured over the raw mushrooms before they were served, Parker said. After his own investigation, Parker said he found boiling them between 10 and 30 minutes is the safest way to prepare morel mushrooms.
Parker said he reached out to chefs across the country and found that many, like him, were surprised to learn about the toxicity of morels.
“They had no idea that morel mushrooms had this sort of inherent risk factor regardless of preparation,” Parker said.
According to the FDA’s Food Code, the vast majority of the more than 5,000 fleshy mushroom species that grow naturally in North America have not been tested for toxicity. Of those that have, 15 species are deadly, 60 are toxic whether raw or cooked — including “false” morels, which look like spongy edible morels — and at least 40 are poisonous if eaten raw, but safer when cooked.
The North American Mycological Association, a national nonprofit whose members are mushroom experts, recorded 1,641 cases of mushroom poisonings and 17 deaths from 1985 to 2006. One hundred and twenty-nine of those poisonings were attributed to morels, but no deaths were reported.
Marian Maxwell, the outreach chairperson for the Puget Sound Mycological Society, based in Seattle, said cooking breaks down the chitin in mushrooms, the same compound found in the exoskeletons of shellfish, and helps destroy toxins. Maxwell said morels may naturally contain a type of hydrazine — a chemical often used in pesticides or rocket fuel that can cause cancer — which can affect people differently. Cooking does boil off the hydrazine, she said, “but some people still have reactions even though it’s cooked and most of that hydrazine is gone.”
Heather Hallen-Adams, chair of the toxicology committee of the North American Mycological Association, said hydrazine has been shown to exist in false morels, but it’s not as “clear-cut” in true morels, which were the mushrooms used at Dave’s Sushi.
Mushroom-caused food poisonings in restaurant settings are rare — the Montana outbreak is believed to be one of the first in the U.S. related to morels — but they have happened infrequently abroad. In 2019, a morel food poisoning outbreak at a Michelin-star-rated restaurant in Spain sickened about 30 customers. One woman who ate the morels died, but her death was determined to be from natural causes. Raw morels were served on a pasta salad in Vancouver, British Columbia, in 2019 and poisoned 77 consumers, though none died.
Before the new guidelines were issued, the FDA’s Food Code guidance to states was only that serving wild mushrooms must be approved by a “regulatory authority.”
The FDA’s Food Code bans the sale of wild-picked mushrooms in a restaurant or other food establishment unless it’s been approved to do so, though cultivated wild mushrooms can be sold if the cultivation operations are overseen by a regulatory agency, as was the case with the morels at Dave’s Sushi. States’ regulations vary, according to a 2021 study by the Georgia Department of Public Health and included in the Association of Food and Drug Officials’ regulatory guidelines. For example, Montana and a half-dozen other states allow restaurants to sell wild mushrooms if they come from a licensed seller, according to the study. Seventeen other states allow the sale of wild mushrooms that have been identified by a state-credentialed expert.
The study found that the varied resources states use to identify safe wild mushrooms — including mycological associations, academics, and the food service industry — may suggest a need for better communication.
The study recognized a “guidance document” as the “single most important step forward” given the variety in regulations and the demand for wild mushrooms.
Hallen-Adams said raw morels are known to be poisonous by “mushroom people,” but that’s not common knowledge among chefs.
In the Dave’s Sushi case, Hallen-Adams said, it was obvious that safety information didn’t get to the people who needed it. “And this could be something that could be addressed by labeling,” she said.
There hasn’t been much emphasis placed on making sure consumers know how to properly prepare the mushrooms, Hallen-Adams said, “and that’s something we need to start doing.”
Hallen-Adams, who trains people in Nebraska on mushroom identification, said the North American Mycological Association planned to update its website and include more prominent information about the need to cook mushrooms, with a specific mention of morels.
Montana’s health department intends to publish guidelines on morel safety in the spring, when morel season is approaching.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 10 months ago
Public Health, Rural Health, States, FDA, Food Safety, Montana
STAT+: Here are the best biopharma CEOs of 2023
It’s that time of the year again when I recognize the Best Biopharma CEO of the year.
This year’s selection is so deservingly obvious that I won’t fabricate suspense by starting with an honor roll of runners-up. More on those high-achieving folks later. Let’s get right to the main course: David Ricks of Eli Lilly is the runaway, rock star, who-else-could-it-be Best Biopharma CEO of 2023.
What an incredible year it’s been for Ricks and the Lilly executive team who helped him achieve so much. My colleague Matt Herper wrote earlier this year about the “dynamic duo” of Ricks and Chief Scientific Officer Dan Skovronsky.
1 year 10 months ago
Adam's Take, Biotech, biotechnology, Eli Lilly, Novo Nordisk, Pharmaceuticals, STAT+
STAT+: New Jersey’s telehealth restrictions cut off access to lifesaving care, lawsuit alleges
Since states started rolling back pandemic-inspired flexibilities that allowed physicians to easily practice telehealth across state lines, virtual health care providers have criticized state-based medical licensure rules as unnecessarily burdensome, expensive, and detrimental to patient care.
Now, two of them are arguing in a lawsuit that they can also be unconstitutional.
Since states started rolling back pandemic-inspired flexibilities that allowed physicians to easily practice telehealth across state lines, virtual health care providers have criticized state-based medical licensure rules as unnecessarily burdensome, expensive, and detrimental to patient care.
Now, two of them are arguing in a lawsuit that they can also be unconstitutional.
On Wednesday, a neurosurgeon, an oncologist, and two New Jersey-based patients sued the state’s medical board, alleging that the state’s licensure requirements for doctors practicing via telemedicine restrict livesaving access to specialty care. The case marks a newly aggressive strategy as health care systems and regulators continue to debate the role of state medical licensing in an increasingly virtual health care system.
1 year 10 months ago
Health Tech, Health Tech, patients, STAT+, telehealth
Health Archives - Barbados Today
Companies announce partnership to release dengue-fighting mosquitoes in the Caribbean
(AP) — Two private companies announced Friday a partnership to release mosquitoes across the Caribbean, including Jamaica, bred with a bacterium that blocks the dengue virus as the region fights a record number of cases.
Orbit Services Partners Inc., a company registered in Barbados, is partnering with Verily, a San Francisco-based health technology company, for the project.
The companies have been meeting with government officials in the region in hopes of launching the project early next year, said Orbit chairman Anthony Da Silva.
It would target nations including Barbados, Guyana, Jamaica, St Kitts & Nevis, St Maarten, St Martin, Suriname, Dominican Republic and Haiti.
Similar projects using the Wolbachia bacterium already have been implemented elsewhere in the world. Mosquitoes are infected with Wolbachia in a laboratory and then released into the wild, where they pass it on to their offspring.
The bacterium prevents the dengue virus from replicating inside a mosquito’s gut.
Da Silva said the partnership has been three years in the making and was delayed by the pandemic.
The proposal is still pending approval in individual Caribbean nations.
The Caribbean, along with the Americas, has reported more than four million dengue cases so far this year, the highest number since record-keeping began in 1980.
The post Companies announce partnership to release dengue-fighting mosquitoes in the Caribbean appeared first on Barbados Today.
1 year 10 months ago
A Slider, Health, Regional
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Even moderate alcohol drinking raises hyperuricemia risk in men, study claims
China: A large cross-sectional study in Chongqing, China, has shed light on the association between alcohol consumption and the risk of hyperuricaemia among adults.
The study findings published in BMJ Open have demonstrated the frequency and degree of alcohol consumption to be the risk factors for hyperuricemia (HUA), especially in males. Moderate drinking was also observed to be a risk factor for HUA among men in the study.
"Different from the benefits of moderate drinking found in other research, HUA risk among moderate drinkers is 1.23 times than that of never drinkers among those in males," the researchers reported. "HUA risk is higher for those who usually drink alcohol l than for those who never drink alcohol among the total population."
"The risk of HUA caused by harmful drinking is the highest, which is 1.81 times that of never-drinkers among the total population and 2.13 times than that of never-drinkers among males," they added, "However, among females, HUA risk was not found to change with drinking."
Hyperuricaemia is becoming a common chronic disease with a worldwide economic and health burden. Considering the widespread consumption of alcohol in the world, some clinicians' review of dietary advice for HUA and gout patients shows that the most general advice is complete avoidance or restriction of alcohol intake, in which this suggested frequency is usually beyond weight loss.
The influence of drinking frequency and degree on hyperuricaemia needs further exploration. Therefore, Siyu Chen, School of Public Health, Chongqing Medical University, Chongqing, China, and colleagues aimed to investigate the relationship between alcohol consumption and hyperuricaemia based on a large population.
The researchers enrolled 20,833 participants aged 30–79 years in the China Multi-Ethnic Cohort, Chongqing region. The serum levels of fasting blood glucose, uric acid, and blood lipids were tested. A standardised questionnaire was used to collect basic demographic statistics such as gender, age, education level, marital status, detailed information on alcohol consumption, and family annual income.
The study led to the following findings:
- After controlling for potential confounders, compared with participants who never consumed alcohol, participants who drank 3–5 days per week had the highest HUA risk (OR: 1.51) and those who drank alcohol harmfully had the highest risk of HUA (OR: 1.81).
- Those who drank moderately had no significant association with the risk of HUA. However, among men, compared with participants who never consumed alcohol, those who drank moderately were also a risk factor for HUA (OR: 1.23) and those who drank alcohol harmfully had the highest risk of HUA (OR: 2.13).
- Compared with participants who drank alcohol moderately, the OR for those who drank alcohol harmfully had the highest risk of HUA was 1.88, and the corresponding OR for each level increment in the degree of alcohol consumption was 1.22.
- Among men, compared with participants who drank alcohol moderately, those who drank alcohol harmfully had the highest risk of HUA (OR: 1.93), and the corresponding OR for each level increment in the degree of alcohol consumption was 1.24.
The study demonstrated a positive relation between the frequency and degree of alcohol consumption and the risk of hyperuricemia. This positive connection was obvious among men, but weak among women. Moderate drinking was also revealed to be a risk factor for HUA among men in the study.
"There is a need for further interventional and prospective research to verify the causal relationship and clarify the specific mechanism," they concluded.
Reference:
Chen S, Ding R, Tang X, et alAssociation between alcohol consumption and risk of hyperuricaemia among adults: a large cross-sectional study in Chongqing, ChinaBMJ Open 2023;13:e074697. doi: 10.1136/bmjopen-2023-074697
1 year 10 months ago
Medicine,Nephrology,Orthopaedics,Diet and Nutrition,Diet and Nutrition News,Medicine News,Nephrology News,Orthopaedics News,Top Medical News,Latest Medical News
Problems with dental implants
DENTAL implants are a groundbreaking modern solution to a tooth loss problem.
What problems are common with dental implants? What can I do about them myself, and what requires a professional?
We're here to address your most pressing questions and concerns around problems with dental implants.
DENTAL implants are a groundbreaking modern solution to a tooth loss problem.
What problems are common with dental implants? What can I do about them myself, and what requires a professional?
We're here to address your most pressing questions and concerns around problems with dental implants.
Dental implant overview
Dental implants are a high-tech solution used to replace your missing teeth; your natural tooth root is replaced with a titanium screw that fuses to your jawbone during the implant process. This titanium root acts as an anchor for a dental restoration, typically either a crown, bridge, or dentures.
These permanent solutions can improve your chewing and speaking ability, along with your look. Even better, they don't get cavities but still require proper care to avoid other problems.
Reasons your dental professional may recommend dental implants include:
• Cavities
• Fractured or broken teeth
• Excessive tooth wear from grinding your teeth (also known as bruxism)
• Injury
If you're considering implants it's a great idea to consult with your dental professional regarding your risk factors that impact your chance of complications.
Problems with implants
According to research, implants are considered safe and there's only a five per cent chance that you will reject your implant. Although these risks are usually slight and can be treated by your dental professional, various complications can arise.
Complications of dental implants can include:
• Infection around the implant
• Damage to blood vessels, teeth, or other tissue
• Nerve damage leading to pain, numbness, or a tingling sensation
• Issues with your sinuses (in cases where the implant is placed in the upper jaw).
The full process of getting dental implants can take several months as it can include tooth extraction, preparation, implantation, healing, and placement of the restoration. For this reason it's vital to give yourself the best chance of successful healing and integration of the implant with your natural bone.
Your risk for complications may be increased if you:
• Are in poor health, regardless of age
• Smoke or use tobacco products
• Have diabetes, leukaemia, or other chronic illness
•Received radiation therapy in the past
• Do not follow the aftercare instructions by your dental professional carefully
• Do not take medications as prescribed.
We recommend contacting your dental professional if you experience signs of infection, unusual swelling, pain, or have a difficult time chewing or speaking after your implant procedure.
Treatment and prevention
Implants can provide a solution for the remainder of life for some people while others experience complications or require additional treatment. Even though the implants and restoration are not natural teeth, your diet and oral care routine are still essential in maintaining their long-term success and your health.
Treatment for complications like loosening or infection typically includes removal and re-implantation by your dental professional. It may reassure you to know that even if your implant fails, re-implantation is successful about 90 per cenyt of the time.
You can reduce your chance of complications with dental implants by:
• Avoiding smoking and tobacco products
• Preventing gum disease through proper diet and oral care
• Brushing for two minutes twice daily
• Cleaning between your teeth using a flossing device once daily
• Scheduling regular visits with your dental professional
• Properly caring for your dental restorations
• Not grinding your teeth (consider a mouthguard at night to help reduce the damage).
Here are some steps to reduce discomfort following dental implantation:
• Rinse with a mix of three per cent hydrogen peroxide and equal parts water, or antibacterial mouth rinse
• Avoid hard, sticky, or chewy foods that could irritate your sensitive mouth.
• Take over-the-counter medications as instructed on the packaging.
• Use a cold compress or ice pack by applying it to the affected area outside your cheek for 20 minutes, three times a day.
Dental implants have positively affected the lives of many, thanks to the ability of titanium to integrate into your bone. Even though your restorations can't get cavities it's vital to maintain a proper diet and dental routine to avoid complications.
Dr Sharon Robinson, DDS, has offices at Dental Place Cosmetix Spa, located at shop #5, Winchester Business Centre, 15 Hope Road, Kingston 10. Dr Robinson is an adjunct lecturer at the University of Technology, Jamaica, School of Oral Health Sciences. She may be contacted at 876-630-4710 and 876-441-4872 (
WhatsApp
). Like their
Facebook
and
Instagram
pages, Dental Place Cosmetix Spa.
1 year 10 months ago
Environmental data — a primary tool for reducing mosquito-borne diseases
EARLY theories of health and medicine have posited mysterious origins for numerous diseases as scientists have tried various experiments and theories in order to curtail the spread of infectious illnesses.
In the 18th century mosquito-borne diseases such as malaria were thought to be caused by bad air ("mala aria") from marshlands, however in later years other scientists made new discoveries and realised that infectious illnesses were caused by a germ, giving rise to the germ theory. This theory of an infectious disease being caused by a germ was the construct for a new approach to managing infectious diseases globally. However, as time evolves, more empirical evidence has been found and used in various fields of medicine to reduce the public health burden through the implementation of evidence-based interventions and strategies.
Mosquito-borne diseases have continued to be a grave global public health issue, contributing to considerable economic cost in many countries. Diseases such as malaria, yellow fever and dengue are endemic in most of the tropical and subtropical parts of the world, and since January 2023 there have been more than 1,000 confirmed cases of dengue in Jamaica. Many Caribbean states have also experienced increased numbers of mosquito-borne diseases since the beginning of the year, despite the implementation of numerous mosquito-control strategies.
Strengthen entomological capacities through better use of environmental data
Many factors such as climate change, unplanned urbanisation, human behaviour, and globalisation are contributing to the emergence and re-emergence of mosquito-borne diseases in recent years. Using data captured from environmental surveillance is therefore necessary to combat these challenges and ensure the effective implementation of mosquito-control programmes. Mosquito-control programmes devoid of scientifically gathered data are often plagued with repeated problems and ineffective use of resources. Constant gathering and use of data, such as the mosquito index — in particular breteau and container indices), identification of potential and common sites for mosquito breeding, distribution of wetlands, levels of precipitation, atmospheric temperatures and wind speed — allow for implementation of effective strategies necessary to curtail incidents of mosquito-borne diseases. Dengue fever is a major public health problem throughout most tropical and some subtropical regions worldwide, and so is Zika fever and other arboviral infections such as chikungunya. Malaria is endemic to many Caribbean countries and remains a major killer of children, particularly in sub-Saharan Africa where it results in the death of a child every two minutes. Environmental data, if captured and used properly, can strengthen entomological capacities as the information provides an understanding of patterns, causes and effects of mosquito-borne diseases, as well as areas that require priority attention to avert possible outbreaks of mosquito-borne diseases.
Common failings of mosquito-control programmes:
1. Failure to capture and incorporate environmental data such as atmospheric temperatures, levels of precipitation, wind speed and land cover conditions when planning and implementing mosquito-control strategies.
The atmospheric temperature of an area and land cover conditions are useful pieces of information that can be used to predict the likelihood of mosquito proliferation atmospheric temperatures within particular ranges that encourage the reproduction of mosquitoes. Female mosquitoes cannot develop eggs at temperatures below 50°F (10°C). Atmospheric temperatures of 27-32 °C are favourable for the rapid completion of the mosquito life cycle. The condition of land cover also has a direct bearing on the effectiveness of mosquito-control strategies. In urban areas of Brazil, environmental surveillance data shows a positive relationship between environmental temperatures, land cover, and Aedes agypti mosquito breeding. In Brazil, roofs made of asbestos and concrete have also been proven to provide favourable sites for Aedes aeygptyi breeding. Mosquitoes are biting nuisances, resulting in cases of urticarial rashes and other dermatological infections. Effective programmes are therefore necessary for a multiplicity of reasons.
2. Failure to adequately incorporate and use technology when implementing mosquito-control strategies.
It is a proven fact that GIS (geographic information systems) technology has significantly transformed mosquito-control strategies in many countries worldwide. GIS enables the visualisation and analysis of geographical data, thereby providing valuable insights into mosquito population dynamics. GIS can be used to map mosquito larvae and adult habitats as well as human populations which are at a greater risk for mosquito exposure and mosquito-borne infections. Through GIS mapping, areas of priority that require ongoing entomological management can be easily identified. Using GIS technology permits the development and use of mosquito-control treatment area maps and leads to better schedules for mosquito-control activities — all of which are necessary to ensure proper management and use of programme resources.
3. Relaxing mosquito-control activities in dry months.
At no time should mosquito-control activities be relaxed. While it is a known fact that some species of female mosquitoes lay their eggs above the waterline in water-holding containers it is also proven scientifically that other species will lay their eggs on damp soil — even when there is no flooding. Water levels on land of 12.7 mm (1/2 inch) or above can cause mosquito eggs to hatch. GIS technology provides data that enables consistent monitoring for timely and proactive implementation of larviciding and adulticiding activities so as to avert increases in indices.
4. Failure to use evidenced-based data in conducting adultidicing (fogging) activities.
If desired mosquito-control targets, such as those set by the World Health Organization, are to be met then the natural behaviour of a particular mosquito specie must be considered. For example, research shows that the Aedes aegyptyi mosquito is diurnal and engages in peak biting activities in the environment approximately two hours after sunrise and several hours before sunset. It is therefore advisable that for rapid reduction in adult mosquito population, adulticiding activities should be done in the same area at dusk and at dawn; wind speed should also be less than 1.6 km/h. Wind speed directly impacts the proper dispersal and effectiveness of insecticides in the atmosphere.
What else is needed for effective mosquito control?
• Mosquito-control programmes require increased investment to strengthen programmatic capacity. The provision of tools and equipment that capture environmental data is mandatory for the success of any mosquito-control programme. Installation and monitoring of rain gauges throughout communities will provide data to identify when increased mosquito control activities are required. Installation and monitoring of light traps and Ovi traps provide useful data to guide mosquito-control activities in areas such as ports of entry. According to International Health Regulations (IHR), a minimum of 400-meter zones around seaports, airports, and ground crossings are to be maintained as a vector-free zone so that the transmission risk of pathogens imported with vectors or reservoirs can be minimised or nullified.
• The use of chemicals, including insecticides, is the first line control for mosquitoes all over the world, however many of these chemicals are known to have damaging effects on the environment. To minimise the need for the use of chemicals in mosquito control, consistent education strategies geared towards environmental sanitation are required. Capturing and using environmental data — such as the sanitary status of a particular community — will identify conditions which are likely to support mosquito-breeding activities in domestic and other settings so that strategies geared towards source reduction can be implemented in a timely manner. Strategies such as community clean-up days implemented ahead of expected seasons of rainfall can prove useful in reducing mosquito indices.
It is a proven fact that much has been done to curtail the incidence and prevalence of mosquito-borne diseases in Jamaica. Amidst these achievements, better use of environmental data as a tool for reducing mosquito-borne diseases can benefit the nation vastly by ensuring more efficient use of resources and reduction of many public health burdens associated with mosquito-borne diseases nationally.
Dr Karlene Atkinson is a public health specialist and lecturer at the School of Public Health, University of Technology, Jamaica.
1 year 10 months ago
Dengue cases decrease
Santo Domingo—Some 99 municipalities in the country reported a decrease in dengue cases this week compared to those reported the previous week, with the surveillance system capturing 983 new cases of the disease, which has maintained a high demand for medical attention in recent months.
Reduction of cases
Santo Domingo—Some 99 municipalities in the country reported a decrease in dengue cases this week compared to those reported the previous week, with the surveillance system capturing 983 new cases of the disease, which has maintained a high demand for medical attention in recent months.
Reduction of cases
According to reports from the Epidemiology Department of the Ministry of Public Health, during epidemiological week number 48, 983 new dengue cases were reported, showing a reduction in the last four weeks of registration, when the average number of weekly cases exceeded 1,000 reported.
This year, the country is experiencing a dengue epidemic, generating a demand for attention in the emergency and hospitalization areas of clinics and hospitals, especially in Greater Santo Domingo. Epidemic conditions of dengue are also registered in different counties of the region.
1 year 10 months ago
Health, Local
‘Financial Ruin Is Baked Into the System’: Readers on the Costs of Long-Term Care
Thousands of readers reacted to the articles in the “Dying Broke” series about the financial burden of long-term care in the United States. They offered their assessments for the government and market failures that have drained the lifetime savings of so many American families. And some offered possible solutions.
Thousands of readers reacted to the articles in the “Dying Broke” series about the financial burden of long-term care in the United States. They offered their assessments for the government and market failures that have drained the lifetime savings of so many American families. And some offered possible solutions.
In more than 4,200 comments, readers shared their struggles in caring for spouses, older parents, and grandparents. They expressed anxieties about getting older themselves and needing help to stay at home or in institutions like nursing homes or assisted living facilities.
Many suggested changes to U.S. policy, like expanding the government’s payments for care and allowing more immigrants to stay in the country to help meet the demand for workers. Some even said they would rather end their lives than become a financial burden to their children.
Many readers blamed the predominantly for-profit nature of American medicine and the long-term care industry for depleting the financial resources of older people, leaving the federal-state Medicaid programs to take care of them once they were destitute.
“It is incorrect to say the money isn’t there to pay for elder care,” Jim Castrone, 72, a retired financial controller in Placitas, New Mexico, commented. “It’s there, in the form of profits that accrue to the owners of these facilities.”
“It is a system of wealth transference from the middle class and the poor to the owners of for-profit medical care, including hospitals and the long-term care facilities outlined in this article, underwritten by the government,” he added.
Other readers pointed to insurance policies that, despite limitations, had helped them pay for services. And some relayed their concerns that Americans were not saving enough and were unprepared to take care of themselves as they aged.
What Other Nations Provide
Other countries’ treatment of their older citizens was repeatedly mentioned. Readers contrasted the care they observed older people receiving in foreign countries with the treatment in the United States, which spends less on long-term care as a portion of its gross domestic product than do most wealthy nations.
Marsha Moyer, 75, a retired teaching assistant in Memphis, Tennessee, said she spent 12 years as a caregiver for her parents in San Diego County and an additional six for her husband. While they had advantages many don’t, Moyer said, “it was a long, lonely job, a sad job, an uphill climb.”
By contrast, her sister-in-law’s mother lived to 103 in a “fully funded, lovely elder care home” in Denmark during her last five years. “My sister-in-law didn’t have to choose between her own life, her career, and helping her healthy but very old mother,” Moyer said. “She could have both. I had to choose.”
Birgit Rosenberg, 58, a software developer in Southampton, Pennsylvania, said her mother had end-stage dementia and had been in a nursing home in Germany for more than two years. “The cost for her absolutely excellent care in a cheerful, clean facility is her pittance of Social Security, about $180 a month,” she said. “A friend recently had to put her mother into a nursing home here in the U.S. Twice, when visiting, she has found her mother on the floor in her room, where she had been for who knows how long.”
Brad and Carol Burns moved from Fort Worth, Texas, in 2019 to Chapala, Jalisco, in Mexico, dumping their $650-a-month long-term care policy because care is so much more affordable south of the border. Brad, 63, a retired pharmaceutical researcher, said his mother lived just a few miles away in a memory care facility that costs $2,050 a month, which she can afford with her Social Security payments and an annuity. She is receiving “amazing” care, he said.
“As a reminder, most people in Mexico cannot afford the care we find affordable and that makes me sad,” he said. “But their care for us is amazing, all health care, here, actually. At her home, they address her as Mom or Barbarita, little Barbara.”
Insurance Policies Debated
Many, many readers said they could relate to problems with long-term care insurance policies, and their soaring costs. Some who hold such policies said they provided comfort for a possible worst-case scenario while others castigated insurers for making it difficult to access benefits.
“They really make you work for the money, and you’d better have someone available who can call them and work on the endless and ever-changing paperwork,” said Janet Blanding, 62, a technical writer in Fancy Gap, Virginia.
Derek Sippel, 47, a registered nurse in Naples, Florida, cited the $11,000 monthly cost of his mother’s nursing home care for dementia as the reason he bought a policy. He pays about $195 a month with a lifetime benefit of $350,000. “I may never need to use the benefit[s], but it makes me feel better knowing that I have it if I need it,” he said in his comment. He said he could not make that kind of money by investing on his own.
“It’s the risk you take with any kind of insurance,” he said. “I don’t want to be a burden on anyone.”
Pleas for More Immigrant Workers
One solution that readers proposed was to increase the number of immigrants allowed into the country to help address the chronic shortage of long-term care workers. Larry Cretan, 73, a retired bank executive in Woodside, California, said that over time, his parents had six caretakers who were immigrants. “There is no magic bullet,” he said, “but one obvious step — hello, people — we need more immigrants! Who do you think does most of this work?”
Victoria Raab, 67, a retired copy editor in New York, said that many older Americans must use paid help because their grown children live far away. Her parents and some of their peers rely on immigrants from the Philippines and Eritrea, she said, “working loosely within the margins of labor regulations.”
“These exemplary populations should be able to fill caretaker roles transparently in exchange for citizenship because they are an obvious and invaluable asset to a difficult profession that lacks American workers of their skill and positive cultural attitudes toward the elderly,” Raab said.
Federal Fixes Sought
Other readers called for the federal government to create a comprehensive, national long-term care system, as some other countries have. In the United States, federal and state programs that finance long-term care are mainly available only to the very poor. For middle-class families, sustained subsidies for home care, for example, are fairly nonexistent.
“I am a geriatric nurse practitioner in New York and have seen this story time and time again,” Sarah Romanelli, 31, said. “My patients are shocked when we review the options and its costs. Medicaid can’t be the only option to pay for long-term care. Congress needs to act to establish a better system for middle-class Americans to finance long-term care.”
John Reeder, 76, a retired federal economist in Arlington, Virginia, called for a federal single-payer system “from birth to senior care in which we all pay and profit-making [is] removed.”
Other readers, however, argued that people needed to take more responsibility by preparing for the expense of old age.
Mark Dennen, 69, in West Harwich, Massachusetts, said people should save more rather than expect taxpayers to bail them out. “For too many, the answer is, ‘How can we hide assets and make the government pay?’ That is just another way of saying, ‘How can I make somebody else pay my bills?’” he said, adding, “We don’t need the latest phone/car/clothes, but we will need long-term care. Choices.”
Questioning the Value of Life-Prolonging Procedures
A number of readers condemned the country’s medical culture for pushing expensive surgeries and other procedures that do little to improve the quality of people’s few remaining years.
Thomas Thuene, 60, a consultant in Boston’s Roslindale neighborhood, described how a friend’s mother who had heart failure was repeatedly sent from the elder care facility where she lived to the hospital and back, via ambulance. “There was no arguing with the care facility,” he said. “However, the moment all her money was gone, the facility gently nudged my friend to think of end-of-life care for his mother. It seems the financial ruin is baked into the system.”
Joan Chambers, 69, an architectural draftsperson in Southold, New York, said that during a hospitalization on a cardiac unit she observed many fellow patients “bedridden with empty eyes,” awaiting implants of stents and pacemakers.
“I realized then and there that we are not patients, we are commodities,” she said. “Most of us will die from heart failure. It will take courage for a family member to refuse a ‘simple’ procedure that will keep a loved one’s heart beating for a few more years, but we have to stop this cruelty.
“We have to remember that even though we are grateful to our health care professionals, they are not our friends. They are our employees and we can say no.”
One physician, James Sullivan, 64, in Cataumet, a neighborhood of Bourne, Massachusetts, said he planned to refuse hospitalization and other extraordinary measures if he suffered from dementia. “We spend billions of dollars, and a lot of heartache, treating demented people for pneumonia, urinary tract infections, cancers, things that are going to kill them sooner or later, for no meaningful benefit,” Sullivan said. “I would not want my son to spend his good years, and money, helping to maintain me alive if I don’t even know what’s going on,” he said.
Considering ‘Assisted Dying’
Others went further, declaring they would rather arrange for their own deaths than suffer in greatly diminished capacity. “My long-term care plan is simple,” said Karen Clodfelter, 65, a library assistant in St. Louis. “When the money runs out, I will take myself out of the picture.” Clodfelter said she helped care for her mother until her death at 101. “I’ve seen extreme old age,” she said, “and I’m not interested in going there.”
Some suggested that medically assisted death should be a more widely available option in a country that takes such poor care of its elderly. Meridee Wendell, 76, of Sunnyvale, California, said: “If we can’t manage to provide assisted living to our fellow Americans, could we at least offer assisted dying? At least some of us would see it as a desirable solution.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 10 months ago
Aging, Health Care Costs, Health Industry, Aid In Dying, california, Dying Broke, Florida, Legislation, Long-Term Care, Massachusetts, Missouri, New Mexico, New York, Pennsylvania, Tennessee, texas, Virginia
Millions of Dollars Flow From Pharma to Patient Advocacy Groups
Pharma money is all over the place — in universities, companies doing continuing medical education for doctors and in prominent patient advocacy organizations that are household names across America.
Public Citizen, a consumer advocacy nonprofit, reports today that between 2010 and 2022, the drug industry’s main lobbying group and member companies provided at least $6 billion in grants to more than 20,000 organizations. The analysis, provided exclusively to KFF Health News in advance of its release, focused on the Pharmaceutical Research and Manufacturers of America (PhRMA) and 31 drug companies that were members of the trade group as of March.
The money dwarfs industry spending over that time on federal lobbying and campaign contributions to lawmakers. With high drug prices a regular topic of debate in Washington, drug industry grants to patient advocacy groups in particular raises questions about conflicts of interest — including whether organizations that accept the industry’s money shy away from pushing policies the drugmakers oppose, even if patients may benefit.
“There’s a risk that those entanglements influence the work of those organizations,” said Matthew McCoy, an assistant professor of medical ethics and health policy at the University of Pennsylvania who has studied patient advocacy groups’ influence and transparency.
He said there’s another important dynamic likely at play, too. Companies aren’t blindly choosing which groups to fund but instead are “probably selecting organizations that are already inclined to see the world, see the policy issues, the way they see it.”
A couple examples you’ll recognize: The American Heart Association received $64.1 million over the 12-year period. The American Cancer Society and its advocacy affiliate, the American Cancer Society Cancer Action Network, together received $23.1 million.
The question is whether the money affects the heavyweight groups’ advocacy. After the House passed the Inflation Reduction Act in August 2022, the American Cancer Society Cancer Action Network’s statement hailed the bill’s cap on Medicare enrollees’ out-of-pocket costs for prescription drugs and additional tax credits for ACA insurance plans. But the group was silent on a contentious provision giving Medicare the ability to negotiate drug prices with manufacturers.
Lisa Lacasse, president of the American Cancer Society Cancer Action Network, said in an emailed statement that the organization didn’t take a formal position on Medicare drug negotiation because “the policy’s impact on patient access to and affordability of cancer treatments was unclear.” In contrast, the Part D out-of-pocket cap “has evidence-based patient benefit.”
- “ACS CAN’s only constituents are cancer patients, survivors, and their loved ones nationwide. ACS CAN’s policy agenda is driven entirely by evidence with the single purpose of achieving our mission to end cancer as we know it, for everyone,” she added. “Contributions to the organization do not influence policy decisions or positions.”
The American Heart Association similarly has touted its support of the three-year extension of enhanced Obamacare tax credits in the IRA, but was silent on drug price negotiation. “We have strict standards in place to monitor relationships with industry and protect against conflicts of interest,” Steve Weiss, a spokesperson for the group, said in an emailed statement. “These funds in no way influence our advocacy, programs or science.”
- “We engage with different organizations who have a wide array of health care opinions and priorities,” Alex Schriver, senior vice president of public affairs at PhRMA, said in an emailed statement. “We may not agree on every issue, but we believe engagement and dialogue is important to promoting a health care policy environment that supports innovation, a highly-skilled workforce and access to lifesaving medicines.”
While the patient groups’ primary mission is to advocate for people with particular diseases, including by boosting funding for research, their work in Washington often bolsters that of pharmaceutical companies whose drugs their patients rely upon. At the same time, the story isn’t always black and white, and just because a group gets money doesn’t automatically make them a “pharma lackey,” said Mike Tanglis, research director at Public Citizen. “It’s not so clean cut,” McCoy added.
The American Diabetes Association received $26.4 million from the drug industry — yet the group supported allowing Medicare to negotiate prescription drug prices. Multiple drug companies have sued to stop the program.
Francisco Prieto, chair of the American Diabetes Association’s national advocacy committee, said in a statement that support from its corporate and other partners allows the group to provide resources about diabetes to health care personnel as well as patients and their caregivers.
“Our partners do not influence our business or policy decisions, which are made solely based on our mission and what is in the best interest of patients around the world,” he said.
Many groups receiving grants do criticize high drug prices generally or highlight patients’ difficulties in affording care. But, “specifically calling out pharma companies doesn’t seem to be a huge priority for them,” Tanglis said.
It isn’t always obvious which groups drug companies are paying. Congress in 2010 enacted the Physician Payments Sunshine Act, a law that required payments to physicians from drug and medical device makers to be registered on a public website. But patient groups were not addressed in the bill. Drug companies’ payments to patient groups can be — but aren’t always — included in annual filings to the IRS or in charitable giving reports.
The American Heart Association in its 2022 annual report lists contributions from corporations, foundations and others. The American Diabetes Association in its latest annual report lists corporate sponsors and ranges for the amounts they give, but not precise dollar figures. Similarly, the American Cancer Society’s most recent report names corporate sponsors giving more than $1 million, but exact amounts aren’t disclosed.
McCoy believes there should be “some kind of mandated transparency across the board” for payments and that patient groups should openly answer questions about steps they take to make sure the funding doesn’t influence their decisions.
“Those are all great things that patient advocacy groups can and should be doing,” McCoy said.
This article is not available for syndication due to republishing restrictions. If you have questions about the availability of this or other content for republication, please contact NewsWeb@kff.org.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 10 months ago
Health Industry, Pharmaceuticals, The Health 202
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Dual ICMR Recognition: Amrita Hospital, Kochi, Bags now Centre of Excellence in Groundbreaking Snakebite and Paediatric Cardiac Research
Kochi: Amrita Hospital, Kochi, has earned dual recognition from the Indian Council of Medical Research (ICMR) for its groundbreaking contributions to venomous snakebite and pediatric cardiac research.
This significant acknowledgment establishes the hospital, as a Centre of Excellence in both domains, reinforcing its position as a leader in medical research and a frontrunner in addressing critical healthcare challenges.
The designation of the Centre of Excellence for snakebite treatment by ICMR signifies the creation of the first-of-its-kind centre in the entire country. This distinction is a testament to the team's exceptional work in therapeutic, preventative, capacity-building, awareness creation, and research aspects related to snakebite.
The distinguished team includes Dr. Jaideep Menon, Dr. Bipin Nair, V V Pillay, Gireesh Kumar, T P Sreekrishnan, Sabarish B. Nair, Muralidharan V, and Aravind MS.
Snakebite a Neglected Tropical Disease (NTD), is predominantly a rural issue affecting millions across the globe in the Tropics and sub-Tropics, most commonly occupational or accidental. India shares a significant burden, with an estimated 58,000 deaths annually, constituting over half of the global toll. WHO data reveals 4.5 to 5.4 million snakebites yearly, leading to 1.8 to 2.7 million envenomings, with 81,000 to 138,000 victims succumbing to complications and 400,000 developing permanent disabilities. In September 2022, the Union Ministry of Health and Family Welfare (MoHFW) initiated a national program for snakebite envenoming prevention and control.
Dr. Jaideep Menon, Professor, Adult Cardiology and Public Health, Amrita Hospital, Kochi, expressing gratitude for the ICMR recognition, stated, "Over 70% of snakebite cases impact males aged 20 to 60, causing severe socio-economic consequences, often resulting in the loss of the family's primary breadwinner. This distinction motivated our team to intensify our comprehensive approach, including awareness creation, capacity building, and essential research.
The Collaborative Centre of Excellence aims to address various aspects related to snakebite envenoming, including developing information, education, and communication (IEC) materials, conducting high-priority research, networking with stakeholders, and providing policy inputs to reduce mortality and morbidity associated with this neglected public health concern.’’
The Collaborative Centre of Excellence aims to research snakebites, build a comprehensive repository on snakes, venom, and treatment, identify mitigation hotspots, collaborate with institutions, conduct awareness-raising research, and contribute to the 2030 SDG target, with a focus on enhancing public health capacity and advocacy. The CCoE aims to generate evidence necessary for laying out the National Program on snakebite in India.
Simultaneously, Amrita Hospital's Pediatric Heart Program, Kochi also, received the prestigious Centre of Excellence award from ICMR, recognizing its exceptional contributions to pediatric cardiac research.
This accolade, granted through a rigorous nationwide application process for collaborating centers of excellence, highlights the program's outstanding track record in high-quality research, publications, innovations, and mentorship.
Established in 1998, Amrita Hospital's Pediatric Heart Program demonstrates enduring commitment through groundbreaking research, addressing vital questions in delivering pediatric cardiac care in resource-limited settings.
The program's legacy includes developing cost-effective strategies for managing congenital heart defects, publishing in leading international journals, and conducting impactful community-based studies on pediatric heart disease. Over the years, the program's dedicated research facility has overseen numerous grant-funded projects, resulting in a rich portfolio of over 200 published papers, fostering a culture of research among trainees who regularly contribute to esteemed international journals.
Dr. R. Krishna Kumar, Clinical Professor and Head of Pediatric Cardiology at Amrita Hospital, Kochi, along with Dr. Mahesh, Clinical Professor of Pediatric Cardiology, expressed, "Accepting the prestigious Centre of Excellence award from DG ICMR for our Pediatric Heart Program at Amrita Hospital fills us with great pride.
This recognition underscores our steadfast commitment to advancing pediatric cardiac research. Our dedicated team consistently engages in high-quality research, leading to innovations and impactful publications. This award stands as a testament to our continuous efforts and inspires us to persist in our journey of excellence in pediatric cardiac care."
The official ceremonies unfolded at the ICMR headquarters in New Delhi, where Director-General Rajeev Behl presented plaques to the distinguished teams. With these two awards, the Centres are actively working on developing pan-India solutions to address these critical health challenges.
Also Read:Amrita Hospital hosts India's 1st educational course of International Stereotactic Radiosurgery Society
1 year 10 months ago
State News,News,Health news,Kerala,Hospital & Diagnostics,Doctor News,Latest Health News,Recent Health News