Running could be just as effective at treating depression as medication - The Independent
- Running could be just as effective at treating depression as medication The Independent
- Running may work better than drugs for depression UPI News
- Antidepressants vs. Running: What Works Best to Beat Depression SciTechDaily
- New study shows running can be as effective as drugs in helping depression Runner's World UK
- New survey confirms the obvious: running helps us battle our demons SussexWorld
- View Full Coverage on Google News
2 years 4 weeks ago
Dominican Republic could have new occupational health and safety regulations
Santo Domingo.- The Dominican Republic is working on new occupational health and safety regulations, expected to be implemented before the end of 2023. Minister Luis Miguel De Camps revealed that these regulations will address various aspects, including psychosocial risks and advancements made in the workplace over the past two decades.
Santo Domingo.- The Dominican Republic is working on new occupational health and safety regulations, expected to be implemented before the end of 2023. Minister Luis Miguel De Camps revealed that these regulations will address various aspects, including psychosocial risks and advancements made in the workplace over the past two decades. The goal is to provide modern, updated occupational health and safety regulations that consider present realities, such as work through digital platforms.
The updates will also focus on certifying safety and security instruments to ensure quality and trust in workplace safety measures. Additionally, the new regulations aim to address psychosocial risks and mental health issues, particularly related to digital work arrangements and maintaining a balance between work and family life.
Celso Juan Marranzini, President of the National Council of Private Enterprise (Conep), emphasized the importance of employee safety, as it directly impacts productivity. Companies that prioritize employee safety experience increased motivation and effectiveness among their workforce.
This focus on occupational health and safety aligns with the efforts to promote comprehensive well-being and human development, reflecting the importance of creating a safe and healthy work environment for the benefit of both employees and society as a whole.
2 years 4 weeks ago
Health
Health – Demerara Waves Online News- Guyana
Guyana Cancer Society, in collaboration with GTT, others, hold specialist medical outreach in Bartica
The Guyana Cancer Society has partnered with GTT, Ministry of Health, the US Embassy and several cancer support organizations in holding a specialist medical outreach at the Bartica Regional Hospital in Cuyuni – Mazaruni (Region Seven). A contingent of 15 specialist doctors including two gynaecologists, one pediatrician, one urologist, five dentists, four ophthalmologists, and two ...
The Guyana Cancer Society has partnered with GTT, Ministry of Health, the US Embassy and several cancer support organizations in holding a specialist medical outreach at the Bartica Regional Hospital in Cuyuni – Mazaruni (Region Seven). A contingent of 15 specialist doctors including two gynaecologists, one pediatrician, one urologist, five dentists, four ophthalmologists, and two ...
2 years 4 weeks ago
Business, Health, News
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
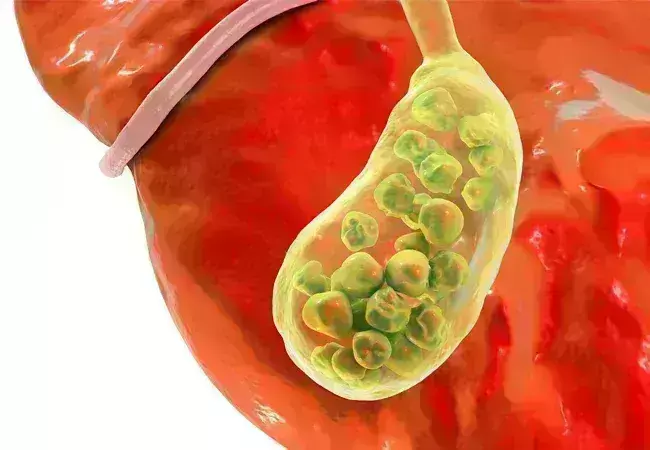
Laparoscopic choledocholithiasis superior to ERCP for common bile duct stones after cholecystectomy
Laparoscopic choledocholithiasis superior to ERCP for common bile duct stones after cholecystectomy suggests a new study published in the BMC Surgery.
A study was done to compare the overall efficacy of laparoscopic common bile duct exploration(LCBDE) with endoscopic retrograde cholangiopancreatography (ERCP ) after cholecystectomy.
Laparoscopic choledocholithiasis superior to ERCP for common bile duct stones after cholecystectomy suggests a new study published in the BMC Surgery.
A study was done to compare the overall efficacy of laparoscopic common bile duct exploration(LCBDE) with endoscopic retrograde cholangiopancreatography (ERCP ) after cholecystectomy.
From January 2017 to July 2021, Seventy patients with Choledocholithiasis after cholecystectomy who were admitted to our hospital were selected and divided into ERCP and LCBDE groups. comparison of baseline characteristics, clinical efficacy and postoperative complications between the ERCP and LCBDE.
The overall efficacy rate of LCBDE was 97.1%, while the overall efficacy rate in the ERCP group was 76.6%. The LCBDE group demonstrated a significantly higher overall effective rate compared to the ERCP group, with a statistically significant difference (p < 0.05). ②The preoperative and postoperative complications of the LCBDE group were visibly lower than the other group (P < 0.05). The postoperative time to oral intake, postoperative ventilation time, length of hospital stay, and hospital costs were higher in the ERCP group compared to the LCBDE group, with a statistically significant difference (P < 0.05).
In the treatment of common bile duct stones after cholecystectomy, LCBDE is a superior choice compared to ERCP in terms of stone diameter, quantity, clearance rate, and hospital costs.
The datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Calculus of the common bile duct in selected participants after cholecystectomy will be removed by using endoscopic retrograde cholangio-pancreatography(ERCP) combined with sphincter of Oddi. This treatment is of obvious therapeutic effect, with a success rate of 76–97%.
Reference:
Zhang, J., Li, L., Jiang, Y. et al. Comparative analysis of laparoscopic choledocholithiasis and ERCP treatment after cholecystectomy. BMC Surg 23, 304 (2023). https://doi.org/10.1186/s12893-023-02207-z
Keywords:
Zhang, J., Li, L., Jiang, Y, Comparative, analysis, laparoscopic, choledocholithiasis, ERCP, treatment, after, cholecystectomy, BMC Surgery
2 years 4 weeks ago
Surgery,Surgery News,Top Medical News
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
False positive pap smear may be early signal of genitourinary syndrome, suggests study
Florida: Recent data presented at the 2023 Menopause Meeting of the North American Menopause Society on September 27 reveals that a pap smear result indicating cervical dysplasia may actually be an early signal of genitourinary syndrome (vaginal atrophy) and can be treated effectively with local estrogen.
The study was led by Alberto Dominguez-Bali, MD, from the Miami Center for Obstetrics, Gynecology and Human Sexuality in Miami, Florida.
Starting in 2010, researchers in Antigua and Florida observed a rise in the number of perimenopausal women with no history of cervical abnormalities and low risk for sexually transmitted infections (STIs) presenting with abnormal Pap smears at their clinics.
The Papanicolaou test, also known as the Pap test or the Pap smear, was developed by Georgios Papanikolaou in the 1940s. It has been the mainstay of cervical cancer screening for the last 60+ years and involves exfoliating cells from the transformation zone of the cervix to enable the examination of these cells microscopically for the detection of cancerous or precancerous lesions.
They investigated 1500 women aged 30-70 from several clinics. The women had a low risk for sexually transmitted infections, a maximum of two sexual partners, and the presence of cervical dysplasia over 12 years.
The researchers reported the following findings:
- Nearly all (96.7%) of the women who received local estrogen treatment had a normal Pap smear following therapy.
- A high number of patients who initially presented with cervical dysplasia underwent interventions such as biopsies, colposcopies, cryotherapy, LEEP excisions, cone biopsies, and hysterectomies because of cervical atrophy.
- Local estrogen treatment could save patients money spent on treatments for cervical atrophy.
- Some women who underwent cone biopsies and hysterectomies and did not receive local estrogen still had vaginal dysplasia.
The researchers reported an early sign of genitourinary syndrome of menopause: false positive cervical dysplasia caused by cervicovaginal atrophy resulting from reduced estrogen levels during perimenopause.
"We also demonstrated how the use of local estrogen therapy can prevent a significant number of procedures and interventions, leading to significant cost savings," the researchers wrote. "This is particularly relevant as the number of Pap smears conducted in this population represents 50-60% of all Pap smears performed on women.
The authors of the study reported no limitations.
Reference:
The data were presented at the 2023 Menopause Meeting of the North American Menopause Society on September 27.
2 years 4 weeks ago
Medicine,Obstetrics and Gynaecology,Oncology,Medicine News,Obstetrics and Gynaecology News,Oncology News,Top Medical News,Laboratory Medicine,Laboratory Medicine News,Latest Medical News
Health – Demerara Waves Online News- Guyana
Guyana improving cancer screening, testing capacity
Guyana’s public health care system is now delivering cancer biopsy results in less than two weeks rather than waiting several months, says Health Minister Dr Frank Anthony. After visiting the doctor and biopsy specimens from suspicious lumps are taken, he said up to last month it took a long time before patients received results, resulting ...
Guyana’s public health care system is now delivering cancer biopsy results in less than two weeks rather than waiting several months, says Health Minister Dr Frank Anthony. After visiting the doctor and biopsy specimens from suspicious lumps are taken, he said up to last month it took a long time before patients received results, resulting ...
2 years 1 month ago
Business, Health, News
Health – Demerara Waves Online News- Guyana
GTT’s Pinktober targets GY$30 million to fight cancer
GTT is urging Guyanese to help that company raise GY$30 million to fight breast cancer and other cancers, amid staggering figures about that disease in this South American nation. GTT spokeswoman, Jasmin Harris says the money will be used raise awareness, screening and diagnosis. Key activities for the remainder of October/Pintokber are medical outreaches in ...
GTT is urging Guyanese to help that company raise GY$30 million to fight breast cancer and other cancers, amid staggering figures about that disease in this South American nation. GTT spokeswoman, Jasmin Harris says the money will be used raise awareness, screening and diagnosis. Key activities for the remainder of October/Pintokber are medical outreaches in ...
2 years 1 month ago
Business, Health, News
Food safety: A shared responsibility for all
FOOD-BORNE illnesses affect everyone. Every year approximately 600 million persons suffer from a food-borne illness and of that number an estimated 430,000 persons die. Children are especially affected as the global estimates demonstrates that 200 million of the reported cases are children.
Campylobacterosis, salmonellosis, coli infections, vibriosis, hepatitis as well as toxin-related illnesses such as those associated with seafood's and immature plant products are amongst the leading causes of food-related death and diseases reported each year .Contrary to popular opinion, many of these food-borne illnesses have been associated with long-term debilitating effects in humans.
Common food-borne pathogens and their effects on humans
There are about 250 food-borne pathogens as well as chemicals responsible for the annual incidence of food-borne illnesses reported. Clostridium botulinum often associated with canned food products produces a neurotoxin which can lead to long-term facial paralysis as well as paralysis of other muscles in the body; E coli 0157:H7 commonly affiliated with undercooked beef products causes hemolytic uremic syndrome and kidney failure; some strains of non-thyphoidal salmonella has been implicated in Reiter's syndrome and reactive arthritis; listeria monocytogenes, a bacterium affiliated with colds foods in particular deli meats and milk, has been a major cause of spontaneous abortion in pregnant women. Other organisms such as toxoplasma gondii and hepatitis E virus has also affected pregnant women in a similar manner. Nitrates and nitrites in cured meats has been implicated in oesophageal, thyroid cancers and other cancers. Staphylococcus aureus, an organism found on the skin of humans, has been associated with symptoms such as diarrhoea, vomiting and retching in humans within a few minutes after consuming a contaminated meal.
Whose responsibility is food safety?
While governments globally have a responsibility to ensure a safe food supply for the people of a nation, food safety, which is the act of safeguarding food for human consumption, is a multifaceted responsibility where the government, the food handler, the food producer, the food retailer, the food distributor, the farmer and the consumer is responsible along the food value chain.
Every food production system involves a series of complexed steps to ensure that food is kept safe from the "farm to the fork", associated with these steps are roles and responsibilities as well as practices which are necessary to ensure that food is protected to reduce the likelihood of contamination.
Government's responsibility for food safety
According to the United Nations Charter for Human Rights, each person has a right to safe food. Governments must, therefore, must implement laws and policies which are modern yet harmonised so that the health of the population can be protected. Government regulatory agencies must develop laws and enforce standards that govern the production, handling, storage and distribution of food. Regulatory inspections carried out by arms of government should not be cumbersome, as complicated food regulatory systems often lead to inefficiency. The establishment of systems for food borne disease surveillance, food recalls, food handler's certification as well as the provision of modern and efficient laboratory services for food testing are also the responsibility of governments.
Consumers responsibility for food safety
To determine the safety of food, consumers often use organoleptic skills such as the appearance or taste of food. In light of the many food production challenges and growing food safety concerns, consumers must become more vigilant of food safety requirements, by ensuring that, food safety standards along the value chain is not disregarded. Consumer responsibility for food safety includes awareness of the potential risks associated with certain food handling practices, as well as ensuring that the food they buy and consume is safe. Food labels are a contract between the food supplier and the consumer: Information such as expiry dates, used by dates, and allergen disclaimers must be given due attention by consumers. Foods that look good and smell good is not always safe, as the safety of the food being consumed depends also on the environment in which it was prepared, the ingredients used in the preparation, as well as the practices and attitude of the individual preparing the food. It is therefore the within the rights of the consumer to reject unsafe food and to become more vocal on food safety violation issues, whilst at the same time ensuring that their own practices do not contaminate food.
Food handlers responsibility for food safety
Just over 60 per cent of all food-borne illnesses are caused due to food handlers malpractices.
Hand washing with soap and water reduces incidence of infectious illness; the food handlers must understand their role in food protection by wearing proper protective clothing and keeping foods at the correct temperatures. For example, hot foods must be kept hot and cold foods must be kept cold. If food handlers are keen on their role in preventing food-borne illnesses, hot foods should never be allowed to become cold while on display to the point where reheating is necessary .
Throughout the food value chain much responsibility for food safety is with the food handler. Food handlers must therefore ensure they are free from communicable illnesses and any associated symptoms such as diarrhoea and vomiting whilst handling food.
Food business operators responsibilities for for food safety
Food handling and preparation must be carried out in a safe and hygienic manner to ensure that food is kept safe. Facilities for washing of hands, preparation of foods and proper storage of food are all important requirements to ensure that food is protected and kept safe. Pest such as rodents are known carriers of the leptospirosis bacteria which results in a global incidence of 60,000 deaths annually. Flies have also been implicated in cases of salmonellosis. Allergen management should be a part of food safety strategies implemented by food business operations; hence, policies that ensure the communication of risk from cross contact between food allergens such as nuts, wheat, soy, shellfish and gluten and non-allergen foods must be communicated to the consumer by food business operations.
The environment of food service establishments must also be kept sanitary to prevent the growth and spread of harmful microorganisms as well as pest infestation: the provision of facilities such as adequate and suitable toilets for staff, equipment for cleaning and sanitising, adequate and suitable equipment for food preparation and protection as well as hand washing are important responsibilities of food business operators. Food business operators must also ensure that employees are skilled in the area of work but even more important, food establishment employees must certified for handling food under the applicable regulations.
Food producers, supplier and distributors responsibility for food safety
Malpractices relating to the growing of agriculture crops as well as slaughtering of animals has been an increasing public health concern. Food producers, such as farmers in particular, have a crucial role in ensuring that pesticides and other chemical used in growing agricultural crops are those designed for such purposes and when used prudence is required to ensure that withdrawal periods are observed as not to adversely affect human health. Animal farmers must also adhere to good animal husbandry practices so that the risk of antimicrobial and growth enhancing agents used in livestock production does not adversely affect human health.
Food distributors are responsible for having suitably designed and maintained, equipment and vehicles to store, handle and protect food products during distribution and transportation. Food distributing vehicles should be used for such purposes only and should be and cleaned and disinfected accordingly. The role suppliers in ensuring a safe food supply is also paramount, as the safety of raw materials is a key factor in the production of safe foods. It is therefore the responsibility of food suppliers to ensure that raw materials and even finished goods are free from food safety hazards.
Next week we will explore who is responsible for food safety in Jamaica.
Dr Karlene Atkinson is a public health specialist and lecturer at the School of Public Health, University of Technology, Jamaica.
2 years 1 month ago
Help! I'm seeing spots
T'is
the season for…viral illnesses, the common cold, the bad flu, dengue. Among the many viral illnesses circulating this time of year is hand, foot and mouth disease (HFMDz). It affects mostly young children and causes fever and rash.
Transmission
T'is
the season for…viral illnesses, the common cold, the bad flu, dengue. Among the many viral illnesses circulating this time of year is hand, foot and mouth disease (HFMDz). It affects mostly young children and causes fever and rash.
Transmission
Hand, foot and mouth disease is caused primarily by the coxsackie virus, and spreads through close contact and it is very contagious especially within the first week. It is spread by contact with an infected person's nose drippings from a runny nose, air droplets from sneezing/coughing, contact with their spit/saliva and stool then touching another person's eyes, mouth or nose, by touching their blisters, kissing and hugging an infected person, through sharing utensils, and contact with infected toys and other surfaces (think counters, door knobs, switches, etc). Children are most infectious at the beginning of the illnesses; even before the rash develops. Even though the illness lasts only seven to 10 days, the virus can survive in stool for many weeks. It affects mainly young children, age five years and under, but it can affect older children and rarely adults. Children in basic school/pre-school/kindergarten are more susceptible to being infected.
Symptoms
First, there is a fever; usually a high fever (101-103 degrees Celsius) which lasts one to two days. The child will be fussy, appetite is little to none, and they will likely have a sore throat. Your child may tell you their throat is hurting, and not want to eat because it may be painful to swallow. They could also have a stomach ache, vomiting, and runny nose. After a day or two, these symptoms will subside.
Then, an itchy rash develops to the hands, feet, elbows, knees, palms (hand-middle) and soles (foot bottom), groin and buttocks. The rash can occur anywhere — I've even seen it on a patient's earlobe. It starts as tiny bumps, then turn into blisters that may burst/rupture and eventually a scab will form. The rash can be INCREDIBLY itchy causing significant discomfort to the little ones, and may be painful when they rupture.
They also develop painful sores in and around the mouth, so your child may not want to eat and prefer drinking.
For parents and caregivers, it's hard to watch your baby be so uncomfortable.
Treatment
As with most viral illnesses, there is no specific treatment to get rid of or cure the illness. It has to run its course and the body's immune system will do its work. The illness is usually mild, although uncomfortable and distressing for baby and parents, and will clear up in seven to 10 days on its own, We can treat the symptoms to alleviate pain and discomfort.
For fever and pain; give paracetamol/acetaminophen (that is Panadol or Tylenol). Follow the dosage chart on the side of the box or as directed by a doctor. Panadol should be given no more than every four hours. Tepid sponge baths can also help to reduce the fever. Ensure lots of hydration and rest. Even if they aren't eating, make sure they drink — water, fruit juices, coconut water, etc. Include foods/liquids rich in vitamin C and zinc which can help in boosting our immune system.
Of note, do NOT give any NSAIDS like Diclofenac (brand name Cataflam). During this time, any illness with fever could be dengue, and NSAIDs can lead to very severe dengue symptoms. Also, do not give aspirin as this may lead to Reye's syndrome.
For the mouth sores, if your child can swish and spit, let them do a warm salt water rinse. This can help to soothe the sores. Eating cold foods like popsicles, jello, yoghurt, etc can reduce their discomfort as well. Because the sores are usually painful, they may not eat, so ensure that they are at least drinking. Avoid salty, spicy and acidic foods. Those may irritate the mouth sores and cause more pain.
For the itchy rash, antihistamines (eg DPH, Histal, Aerius or Zyrtec) can alleviate itching. Calamine lotion may help as well. If you apply a cold object to the skin — like holding a bottle with frozen liquid to the foot bottom — it can ease the discomfort for a short while. Diaper cream with zinc oxide can help to "dry up" the rash as well. Oatmeal baths can soothe skin irritation. If the rash is extremely itchy, you can mix hydrocortisone cream with an antibiotic ointment and apply to the affected areas, but wait a few days after its onset. I have found good ol' aloe vera helps to soothe irritated skin.
Keep kids out of school and away from others for seven to 10 days, and until the rash is healed/dried up.
HFMDz is usually a mild illness, but there can be complications. Because of the painful mouth sores and decreased appetite, your child may not eat or drink much, which means they are at risk of becoming dehydrated. It is important that your child drinks enough fluids to prevent this.
There have been accounts of fingernails and toenails falling out after the virus, but they grow back. VERY rarely, a small number of people may develop an infection in the brain or spinal cord (meningitis and encephalitis).
If your child is severely dehydrated, lethargic or very droopy, or has a fever longer than three days, or having symptoms longer than 10 days, please seek medical attention.
It is important to remember that the virus that causes HFMDz is very contagious, and spreads at the very onset of the disease, even before you realise the children are sick. We can minimise the spread by ensuring effective and proper hygiene. Caregivers, including schools and daycares, should disinfect toys and frequently touched surfaces regularly, ensure hand washing for 20 seconds after taking care of babies — especially after diaper changes and cleaning up a runny nose or vomit, etc. Separate sick children from others and teach your children to cough and sneeze in their elbows, not their hands, followed by hand washing or using a hand sanitiser, encourage them not share food and drinks or utensils with others (this one will be hard, especially for toddlers), and teach them when and how to properly wash their hands.
Dr Tal's Tidbit
Hand, foot and mouth disease is a viral illness that brings fever and rash lasting about a week. The rash affects the hands and feet, including the palms and soles, but can affect the entire body. It is usually mild, but can cause lots of discomfort for your little one. It is very contagious so ensure good hygienic practices to limit and prevent its spread.
Dr Taleya Girvan has over a decade's experience treating children at the Bustamante Hospital for Children, working in the Accident and Emergency Department and Paediatric Cardiology Department. Her goal is to use the knowledge she has gained to improve the lives of patients by increasing knowledge about the health-care system in Jamaica. Dr Tal's Tidbits is a series in which she speaks to patients and caregivers providing practical advice that will improve health care for the general population. E-mail: dr.talstidbits@gmail.com IG @dr.tals_tidbits
2 years 1 month ago
1 in 10 babies worldwide are born early, with major impacts on health and survival
AN estimated 13.4 million babies were born early (before 37 full weeks of pregnancy) in 2020 — which is around one in 10 of all live births — according to a detailed study published in the Lancet today by authors from the World Health Organization (WHO), the United Nations Children's Fund (UNICEF) and the London School of Hygiene and Tropical Medicine.
Since prematurity is the leading cause of death in children's early years, there is an urgent need to strengthen both care for preterm babies as well as prevention efforts — particularly maternal health and nutrition — so as to improve childhood survival. For those who live, preterm birth also significantly increases the likelihood of suffering major illnesses, disability and developmental delays, and even chronic diseases as adults like diabetes and heart conditions.
As with other major trends relating to maternal health, no region of the world has significantly reduced rates of preterm births over the last decade. The annual global rate of reduction in preterm births between 2010 and 2020 was just 0.14 per cent.
"Preterm babies are especially vulnerable to life-threatening health complications and they need special care and attention," said Dr Anshu Banerjee, director of maternal, newborn, child and adolescent health and ageing at WHO. "These numbers show an urgent need for serious investment in services available to support them and their families as well as a greater focus on prevention — in particular, ensuring access to quality health care before and during every pregnancy."
The paper, 'National, regional, and global estimates of preterm birth in 2020, with trends from 2010: a systematic analysis', provides global, regional and country estimates and trends for preterm births between 2010 and 2020, revealing large disparities between regions and countries. Around 65 per cent of preterm births in 2020 occurred in sub-Saharan Africa and southern Asia, where over 13 per cent babies were born preterm. The rates in the worse affected countries — Bangladesh (16.2 per cent), Malawi (14.5 per cent) and Pakistan (14.3 per cent) — are three or four times higher than those in the least affected countries —Serbia (3.8 per cent), Moldova (4 per cent) and Kazakhstan (4.7 per cent).
Preterm birth is not just an issue in low- and middle-income countries, however, and the data shows clearly that it affects families in all parts of the world. Rates of 10 per cent or higher occur in some high-income countries such as Greece (11.6 per cent) and the United States of America (10 per cent).
Maternal health risks, such as adolescent pregnancy, infections, poor nutrition, and pre-eclampsia, are closely linked to preterm births. Quality antenatal care is critical to detect and manage complications, to ensure accurate pregnancy dating through early ultrasound scans and if needed, to delay labour through approved treatments.
2 years 1 month ago
HEART/NSTA, UNICEF inks partnership to target unattached youths
T
he
HEART/NSTA Trust and the United Nations Children's Fund (UNICEF) Jamaica signed a memorandum of understanding (MOU) to further strengthen human development in Jamaica.
T
he
HEART/NSTA Trust and the United Nations Children's Fund (UNICEF) Jamaica signed a memorandum of understanding (MOU) to further strengthen human development in Jamaica.
Speaking at the signing ceremony, the heads of both entities welcomed the partnership and signalled their commitment in providing yet another initiative to empower and provide meaningful opportunities for youths.
The partnership, under the banner of UNICEF's FunDoo initiative, seeks to equip young individuals with essential life and employability skills and facilitate their seamless transition into the workforce. The WhatsApp-based FunDoo will be accessible through UNICEF's technological innovation, U-Report, which is operated in 95 countries.
Dr Taneisha Ingleton, managing director of HEART/NSTA Trust, expressed that the partnership signifies an unwavering commitment to the youth of Jamaica.
"It is a beacon of hope, a promise of transformation, and a testament to the power of collaboration. Together, we will make a difference in the lives of thousands of young people, equipping them with the skills and opportunities they deserve," she said.
In welcoming the collaboration, country representative, UNICEF Jamaica, Olga Isaza stated that the initiative seeks to target youth who are not employed, neither are they in school, nor enrolled in any form of training programme to help them to transition into these opportunities.
"We are working to help teens develop the skills they need to adapt to the various challenges they may face in the future through our 21st-Century Skills Framework on which FunDoo is based. In addition to free career guidance, other skills include time management, critical thinking, resume writing and budgeting," she added.
The MOU articulates areas of collaboration, including:
1. Career Development: HEART/NSTA Trust will provide career profiles and road maps to UNICEF for career guidance and life skills.
2. Try-a-Skill Programmes: HEART/NSTA Trust will supply bite-size training contents for FunDoo and manuals for execution. UNICEF will develop mini-courses on FunDoo using
HEART's provided training content.
3. Capacity Building: UNICEF will provide master trainer training for HEART/NSTA Trust instructors, ensuring high-quality delivery. HEART/NSTA Trust will supply teachers to be trained as master trainers.
4. Trainees' Participation: HEART/NSTA Trust will actively promote FunDoo to both new and existing trainees. UNICEF, in addition to FunDoo, will provide HEART/NSTA Trust's participants with access to U-Report services, including the U-Matter mental health chatline. UNICEF will also encourage FunDoo users to enrol as new HEART trainees.
5. Monitoring: HEART will closely monitor the progress of trainees who transition into our training programmes or job opportunities.
Dr Ingleton noted that the partnership is perfectly aligned with Jamaica's national priorities, as it supports the Jamaica Country Office's education programme goal of transitioning 3,000 unattached young people into education, employment, or training.
Additionally, she stated that the initiative will engage at least 13,500 young individuals in the FunDoo programme, equipping them with the skills they need to thrive.
Both heads of entities welcomed the impact that the initiative will have on youths during the period of the partnership. "Today, we are holding hands and taking an important step together on behalf of the next generation to equip and empower them to fulfil their potential," declared UNICEF's Country Representative Isaza.
The MOU was signed at the HEART/NSTA Trust's corporate office located on Oxford Road in Kingston, on October 4, 2023.
2 years 1 month ago
Dengue outbreak in Barbados - Nation News
- Dengue outbreak in Barbados Nation News
- Barbados Ministry of Health confirms outbreak of dengue fever Jamaica Observer
- Ministry of Health declares dengue fever outbreak | Loop Barbados Loop News Barbados
- Bajans urged to take preventative measures against Dengue Nation News
- Dengue fever outbreak in Barbados, Health Ministry confirms Barbados Today
- View Full Coverage on Google News
2 years 1 month ago
Health Archives - Barbados Today
Dengue fever outbreak in Barbados, Health Ministry confirms
The Ministry of Health and Wellness has confirmed a dengue fever outbreak in Barbados.
Chief Medical Officer, Dr Kenneth George, disclosed that the threshold was reached at the end of September, where 518 cases were recorded compared to the same period in 2022, when there were 241 cases. The Ministry of Health and Wellness classifies a case of dengue fever as both suspected and confirmed.
Of the 40 confirmed cases of dengue for the year, 28 were recorded in September.
“These recent increases signal the start of a dengue fever outbreak in Barbados in September 2023. There were no confirmed cases in 2022,” the Chief Medical Officer stated.
The Pan American Health Organization (PAHO) has also advised that there have been outbreaks in Martinique and Guadeloupe in the Eastern Caribbean, with dengue virus serotype 2 resulting in some hospitalisations. There have also been recorded rising cases in the OECS, including Grenada. The World Health Organization recently indicated that increased cases of mosquito-borne disease were likely in Europe, the United States of America and Africa, as a result of climate change (warmer, wetter and less reliable climate).
Dengue fever is an acute mosquito-borne febrile illness caused by infection with one of the four known dengue serotypes. It is endemic in Barbados with occasional outbreaks.
The public is reminded of the symptoms, which include headaches, muscle and joint pains, vomiting and a characteristic skin rash. Most cases are self-limiting and recovery generally takes two to seven days.
In severe cases, haemorrhagic symptoms and organ failure can occur, which may, on occasion, result in shock and death. The likelihood of adverse outcomes occurs when there are multiple strains circulating. The Best-dos Santos Public Health Laboratory has advised that serotypes 1, 2 and 3 are circulating in Barbados.
Dr George urged members of the public to take immediate protective actions. These include:
- Source reduction – removal of sites and receptacles where stagnant water can collect. For example, the overflow dishes of plant pots in homes, plant cuttings and discarded tyres,
- using mosquito repellent on the skin,
- wearing light-coloured, long-sleeved shirts and long pants, particularly during peak biting times – dusk and dawn,
- using mosquito nets over infant beds, cribs, carriers and strollers,
- and installing window and door screens to keep out mosquitoes.
Additionally, Dr George advised persons who have an unexplained fever or exhibit any of the other symptoms mentioned above, to seek medical attention. A blood test will be required for confirmation of dengue fever.
The Chief Medical Officer said that the Ministry of Health and Wellness will use the location of reported suspected and confirmed dengue cases to inform its fogging campaign. He further advised that any unusual increases in mosquito sightings should be reported to the environmental health department of the nearest polyclinic. To date, there have been no deaths attributed to dengue fever.
(BGIS)
The post Dengue fever outbreak in Barbados, Health Ministry confirms appeared first on Barbados Today.
2 years 1 month ago
A Slider, Health, Local News
Skyrizi achieves consistent results in plaque psoriasis across racial, ethnic groups
NEW YORK — Skyrizi exhibited efficacy across racial and ethnic groups for the treatment of moderate to severe plaque psoriasis, according to a presentation at the Skin of Color Update 2023 meeting.“When we think about moderate to severe psoriasis, we have a lot of biologic options for treatment,” Raj Chovatiya, MD, PhD, assistant professor of dermatology at Northwestern University Feinberg Scho
ol of Medicine, told Healio. “And [Skyrizi (risankizumab, AbbVie)] is one of the most efficacious ones we have that has pretty infrequent dosing and really good short- and
2 years 1 month ago
Health Archives - Barbados Today
Use sugar and salt tax to fund healthcare, says BAMP head
President of the Barbados Association of Medical Practitioners (BAMP) Dr Lynda Williams is suggesting that the revenues collected from the 20 per cent sugar-sweetened beverage excise tax and the soon-to-be-implemented tax on products high in salt content be used specifically within the health sector.
She told Barbados TODAY she would prefer if the money collected by the government from those taxes be set aside specifically to boost the budget for healthcare, rather than be placed into the Consolidated Fund – the government account into which all revenues are paid and from which all spending is made.
“If we just put it in the general funds and hope that you can increase your health fund, that most likely will not happen,” the prominent doctor said.
“My feeling about all those things is that it works as long as the money that is collected from this goes towards health expenditure. If you are just putting on a tax and put it in the general fund as just another collection of taxation, and you hope that it pans out to be more expenditure for health, that is less significant than knowing that [based] on this revenue, this is how much to increase health expenditure by.”
Barbados has one of the highest rates of overweight and obese populations within Latin America and the Caribbean, with about 30 per cent of children considered overweight and 14 per cent obese.
About one in every three Barbadian adults is considered overweight, and a similar number is obese.
In an effort to help reduce the intake of sugar-sweetened beverages among Barbadians and control non-communicable diseases (NCDs) such as diabetes, the government introduced a 10 per cent excise tax on sugar-sweetened beverages in 2015. This was designed to generate in excess of $10 million in its first year.
Effective April 1, 2022, the Mia Mottley administration increased the excise tax on sweetened drinks to 20 per cent.
Dr Williams said she supported the tax measure but stressed that it was important for the government to know exactly how much was being collected and put that towards the development of the health sector.
The government is currently in the process of reviewing a draft policy for similar taxation on products high in salt content. This could be ready for implementation as early as the first quarter of next year.
“We have had the discussion about sugar taxes and we have implemented sugar-sweetened beverage taxes; now there is the discussion about salt…. Taxes have been shown in other countries to cause a reduction in spending when people are purchasing,” said Williams.
A joint University of the West Indies and Cambridge University study released in 2019 concluded that Barbadians were buying fewer sweet drinks and getting more bottled waters and non-sugar alternatives.
It showed that consumption dropped by some 10 per cent one year after the tax was implemented, when compared to two years before.
The post Use sugar and salt tax to fund healthcare, says BAMP head appeared first on Barbados Today.
2 years 1 month ago
A Slider, Education, Health, Local News
Demand for beds rises due to dengue fever in health centers
Dominican Republic.- Clinics and hospitals in the most dengue-affected areas of the country are still full of patients with symptoms of the viral disease.
Relatives of affected children go from one center to another, searching for beds and locating the best doctors. According to official data, there is a slight decrease in hospitals that have been more saturated with patients, but the population indicates that they cannot find beds.
“I will ask for discharge from this clinic, if my daughter does not improve, will take her to another center,” said the mother of a teenager diagnosed with dengue.
You can read: Gang of minors who committed armed robberies in SPM dismantled.
Situation
The Plaza de la Salud General Hospital had 29 patients admitted 12 hours ago; nine were waiting for beds in the emergency. This is the third hospital that has received the most patients with dengue fever. The Hugo Mendoza Pediatric Hospital has held first place. Yesterday afternoon, 82 minors were admitted; the emergency has a high demand. However, pediatricians insist that not everyone who comes to the emergency with a fever is dengue, as patients with influenza and other respiratory viruses have also increased.
The Robert Reid Cabral pediatric hospital had 58 minors admitted, while the Marcelino Velez Santana hospital reported 20. The Jaime Mota Hospital in Barahona had 20 admissions, and the Arturo Grullon Hospital had another 20 children. Dengue fever is also affected by the disease.
Warning signs
Firm and persistent abdominal pain; vomiting more than three in one hour, more than six in two hours; mucosal bleeding, mainly in the gums; edema; drowsy or irritable young children; hepatomegaly; hypotension (they stand up and get dizzy) and increased hematocrit, said Dr. Virgen Gomez, pediatric infectious disease specialist.
Symptoms
Dengue has symptoms that lead the family and the physician to think of dengue: the abrupt onset of fever, headache, body aches, vomiting and diarrhea, and rash.
Provinces
Some 25 provinces have presented more cases, with the municipality of Santo Domingo Norte having the highest incidence. This is why the Hugo Mendoza hospital authorities were forced to open more than 100 beds.
They have had up to 106 patients admitted. Santo Domingo, the National District, Barahona, La Vega, and San Cristobal have a high disease incidence.
The age groups that have been infected the most are 4 and 19 years old, but adults have also been infected, it has been proven.
It is an endemic disease. The virus is transmitted by the Aedes aegypti mosquito.
2 years 1 month ago
Health, Local
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Boehringer Ingelheim, Zealand Pharma announce initiation of 3 phase III trials investigating Survodutide for obesity
Ingelheim: Boehringer Ingelheim and Zealand Pharma A/S have announced the initiation of three Phase III trials investigating survodutide (also known as BI 456906) for people living with overweight or obesity. The trial design builds upon learnings from Phase II, in which people living with overweight or obesity achieved up to 19 percent weight loss.
The Phase III trials will soon open for recruitment.
Additional Phase II data, presented at the 59th Annual Meeting of the European Association for the Study of Diabetes (EASD), demonstrated reductions in absolute waist circumference (up to 16.0 cm), absolute body weight (up to 19.5 kg) and absolute systolic and diastolic blood pressure (up to 8.6 mmHg and 4.8 mmHg, respectively) over 46 weeks.
“As the prevalence of the disease of obesity continues to increase, it is imperative that we develop additional innovative approaches to address this serious, chronic disease,” said Carel le Roux, M.D., Ph.D., Professor at University College in Dublin, Ireland, and Principal Investigator of the trial. “Survodutide has a novel mechanism of action with the potential to reduce appetite while increasing liver energy expenditure. The promising Phase II data give us reason to be hopeful about the potential of survodutide as a treatment for people living with the disease of obesity.”
SYNCHRONIZE-1 (NCT06066515) and SYNCHRONIZE-2 (NCT06066528), now listed on clinicaltrials.gov, are Phase III studies investigating survodutide in people with obesity (BMI ≥30 kg/m2) or overweight (BMI ≥27 kg/m2) with comorbidities, including dyslipidemia, hypertension and obstructive sleep apnea. SYNCHRONIZE-1 will enrol people without type 2 diabetes (A1C <6.5%) and SYNCHRONIZE-2 will enrol people with type 2 diabetes (A1C ≥6.5%, <10%).
For both studies, the primary endpoints are percent change in body weight at week 76 and the proportion of people who achieve body weight loss of 5% or more at week 76. Secondary endpoints include body weight reductions of at least 10%, 15% and 20% at week 76. A total of 600 participants will be enroled in each of the two studies, randomized to receive weekly subcutaneous injections of either survodutide, reaching a maximum dose of 3.6 mg or 6.0 mg for maintenance treatment, or placebo.
The third study, SYNCHRONIZE-CVOT, is a Phase III trial that will enrol people with overweight or obesity with cardiovascular disease, chronic kidney disease, or risk factors for cardiovascular disease. In SYNCHRONIZE-CVOT, the primary endpoint is the time to first occurrence of any one of five major adverse cardiac events (5P-MACE): death, non-fatal stroke, non-fatal myocardial infarction, ischemia-related coronary revascularization and heart failure events.
“By implementing the valuable insights gained from the Phase II study, we are confident in the accelerated development of survodutide,” said Carinne Brouillon, Head of Human Pharma, Boehringer Ingelheim. “Obesity is a chronic disease associated with serious health complications that affects hundreds of millions worldwide. With these trial initiations, we continue to build on our heritage of bringing differentiated and innovative treatments to address cardiovascular, renal, and metabolic diseases.”
“We are excited that survodutide will shortly enter Phase III trials through the global SYNCHRONIZE program for people living with overweight or obesity,” said David Kendall, MD, Chief Medical Officer of Zealand Pharma. “With novel peptide therapeutics like survodutide, we are targeting key metabolic pathways, and these therapies have the potential to address one of the most significant healthcare challenges in medicine today.”
Read also: Boehringer unveils 81 percent discounted biosimilar of AbbVie Humira
2 years 1 month ago
News,Industry,Pharma News,Latest Industry News
Mother of three confident she has beaten breast cancer - Jamaica Star Online
- Mother of three confident she has beaten breast cancer Jamaica Star Online
- Summerville woman experiences firsthand how breast cancer treatment options have changed Medical University of South Carolina
- UAW Strike update coming • Young mom dies from aggressive cancer • Grosse Pointe Woods death investigation FOX 2 Detroit
- Hernando County mother and daughter spread positivity despite multiple cancer battles ABC Action News Tampa Bay
- Husband of Livonia mother of 3 who lost brave battle with cancer, shares her story FOX 2 Detroit
- View Full Coverage on Google News
2 years 1 month ago
News Archives - Healthy Caribbean Coalition
Open Letter to the National Standards Bodies of CARICOM
OPEN LETTER
to the National Standards Bodies of CARICOM
in reference to the
CARICOM Member State Voting on the Final Draft CARICOM Regional Standard for Specification for labeling of pre-packaged foods (FDCRS 5)
4 October, 2023
Dear CARICOM National Standards Bodies,
OPEN LETTER
to the National Standards Bodies of CARICOM
in reference to the
CARICOM Member State Voting on the Final Draft CARICOM Regional Standard for Specification for labeling of pre-packaged foods (FDCRS 5)
4 October, 2023
Dear CARICOM National Standards Bodies,
We are writing as leaders in health and nutrition across the Caribbean to urge your stakeholders representing diverse sectors of society and senior policymakers in Ministries of Trade, Commerce, Business, Finance, and Agriculture, to support the approval of the Final Draft CARICOM Regional Standard for Specification for labeling of pre-packaged foods (FDCRS 5), which includes the octagonal front-of-package warning label and the PAHO Nutrient Profile Model.
Caribbean people deserve the best nutritional labelling system to reduce malnutrition in all its forms—including undernutrition and overnutrition—and improve their health.
Among various nutritional labelling systems, scientific evidence, including from the Caribbean region, underscores the superior effectiveness of the octagonal warning label, which empowers consumers to quickly, correctly, and easily identify products with unhealthy nutritional profiles.
Caribbean countries have some of the world’s most alarming rates of non-communicable diseases (NCDs) and obesity. These conditions not only place immense strain on our healthcare systems, but also pose a significant threat to our economic stability, and, as underscored in the recent Bridgetown Declaration on NCDs and Mental Health, they jeopardize our regional development objectives and the attainment of the 2030 Sustainable Development Goals.
At the heart of these diet-related health challenges lies the overconsumption of foods high in sodium/salt, sugar, and fats – a situation which is in part due to the lack of awareness of the content of many foods. Current nutrition labels are difficult to read and understand and are often misleading.
Caribbean people deserve access to a labelling system that has proven its effectiveness in helping consumers make informed food choices.
Studies conducted globally, as well as regionally in Jamaica and in Barbados, show that the octagonal warning label outperforms all other labels in allowing consumers to quickly, easily, and correctly identify foods high in sodium/salt, sugar, and fats.[1] In Barbados, the introduction of octagonal warning labels has the potential to reduce NCD deaths by 16%, while saving the government in excess of 700 million US dollars in mortality costs annually.[2]
The impact of the octagonal warning labeling system extends far beyond the supermarket aisle. It has the capacity to easily identify those food products which should be regulated in various settings, including schools, and be subjected to taxation (unhealthy products) and subsidies (healthy products). The HCC and partners’ newly launched campaign, ‘Octagonal Warning Labels help consumers #ActOnFacts’ speaks to this and the other co-benefits of implementing this labelling standard.
The time to act is now.
The time to act is now, as we echo the commitment made by Caribbean Heads of State and Government in the 2007 Declaration of Port of Spain to address the “epidemic of chronic NCDs” by prioritising the prevention of NCDs through strong policies. Approval of this Final Draft CARICOM Regional Standard and the octagonal warning label not only honours this historic commitment, but also represents a significant step towards safeguarding the nutrition and health of our citizens, particularly those living with obesity and NCDs. The rising levels of childhood obesity in the region and the associated increased risk of NCDs, heighten the imperative for action; Caribbean people have a right to simple and easily understood information about the food they consume; right now, they do not.
Our collective voices build on the signatures of support from over 400 Caribbean public health professionals, academics, and ordinary citizens, and over 40 regional organisations.
We implore your stakeholders to consider the urgency of this matter and the profound impact that your decision will have on the immediate and future nutrition, health, and well-being of Caribbean people, and, by extension, national and regional development.
By approving the Final Draft CARICOM Regional Standard for Specification for labelling of pre-packaged foods and the octagonal warning label, through a fair and balanced vote including all key stakeholders, you will send a clear message of commitment to improve the lives of citizens across CARICOM and securing a healthier future for the region.
SIGNED
REGIONAL PARTNERS
Sir Trevor Hassell, President, Healthy Caribbean Coalition (HCC)
Mr. Dean Chambliss, Subregional Program Director for the Caribbean, Pan American Health Organization (PAHO)
Dr. Joy St. John, Executive Director, Caribbean Public Health Agency (CARPHA)
Dr. Didacus Jules, Director General, OECS Commission
Mr. Pieter Bult, Representative EC, UNICEF Eastern Caribbean
Mrs. Nicole Foster, Law Lecturer & Head, Law and Health Research Unit, Faculty of Law, University of the West Indies Cave Hill Campus.
Professor Simon Anderson, Director of the George Alleyne Chronic Disease Research Centre (GA-CDRC)
HCC PATRON
Sir George Alleyne, Director Emeritus, PAHO
NCD COMMISSION CHAIRS
Mr. Suleiman Bulbulia, Chair, Barbados National NCD Commission
Dr. Trevor Ferguson, Chair, Jamaica National NCD Commission
Dr. Jane Noel, Chair, Grenada National NCD Commission
CIVIL SOCIETY ORGANISATION PARTNERS
Dr. Vanessa White-Barrow, President, Caribbean Association of Nutritionist and Dieticians
Ms. Debbie Chen, Executive Director, Heart Foundation of Jamaica
Ms. Abi Begho, Founder and Programme Director, Lake Health and Wellbeing
Dr. Karen Sealey, Founder and Chair, Trinidad and Tobago NCD Alliance
Dr. Sonia Nixon, Chair, Grenada Cancer Society
Ms. Laura Tucker-Longsworth, Founder and Chair of the Belize Cancer Society, Former Speaker of the House of Assembly, Belize
Shannique Bowden, Executive Director, Jamaica Youth Advocacy Network
Ms. Janice Olliver-Creese, President, St Vincent and the Grenadines Diabetes & Hypertension Ass Inc
Ms. Juanita James, President, Antigua and Barbuda Diabetes Association
Dr. Nancy Charles Larco, Executive Director, Fondation Haïtienne de Diabète et de Maladies Cardiovasculaires, Haiti
Dr. Tamara Remy, President, St. Lucia Cancer Society
View/download the open letter here
[1] https://bmjopen.bmj.com/content/13/4/e065620
[2] https://iris.paho.org/bitstream/handle/10665.2/57989/PAHONMHRF230040_eng.pdf?sequence=1&isAllowed=y
The post Open Letter to the National Standards Bodies of CARICOM appeared first on Healthy Caribbean Coalition.
2 years 1 month ago
Front-of-Package Nutrition Warning Labels, News, Open Letters & Statements, OWL, Slider, Timeline
News Archives - Healthy Caribbean Coalition
What Is Happening With Food Labels in CARICOM?
On Wednesday 4 October, 2023 the HCC in partnership with PAHO, CARPHA, the OECS Commission, UNICEF and the Caribbean Public Health Law Forum, brought together key regional stakeholders providing an update on the status of front of package nutrition labels in CARICOM including: promoting the new campaign entitled
Octagonal warning labels help consumers #ActOnFacts and presenting science-based evidence in support of the octagonal warning label (OWL) contained within the Final Draft of the CARICOM Regional Standard for the Labelling of Pre-packaged Foods (FDCRS 5).
Read the press release for the webinar here.
The webinar was attended by over 200 participants from across the region.
Webinar Goal and Objectives
The goal of the webinar was to provide an update on the status of the Final Draft of the CARICOM Regional Standard for the Labelling of Pre-packaged Foods (FDCRS 5) which contains the octagonal front of package warning label and share evidence in support of octagonal warning labels as a key measure to catalyse the reshaping of food environments in the Caribbean.
The objectives of the webinar were:
- To promote the campaign “Octagonal Warning Labels help consumers #ACTONFACTS ” in support of the Final Draft of the CARICOM Regional Standard for the Labelling of Pre-packaged Foods (FDCRS 5) which contains the OWL as defined by the PAHO nutrient profile model.
- To increase public awareness of the detrimental impact of ultra-processed products high in sugars, fats and sodium and the role of the ‘high-in’ octagonal front of package warning labels (OWL) in promoting healthier food choices.
- To provide policymakers and policy influencers with a comprehensive understanding of FOPWL, specifically OWL, and to present robust scientific evidence underpinning the use of OWL and the Pan American Health Organisation (PAHO) Nutrient Profile Model (NPM) to guide OWL thresholds.
- To provide science-based evidence to correct misinformation about OWL including the false narrative that OWL negatively impacts trade and the economy.
- To encourage both the public and policymakers support for OWL and the FDCRS-5.
Overall Moderator
Ms. Maisha Hutton
Executive Director
HCC
Partners
Sir Trevor Hassell
President
HCC
Dr. Anselm Hennis
Director, Department of NCDs
and Mental Health
PAHO
Dr. Lisa Indar
Director, Surveillance, Disease
Prevention and Control Division
CARPHA
Dr. Didacus Jules
Director General
OECS Commission
Mr. Pieter Bult
UNICEF
Representative to the
Eastern Caribbean Area
Panellists
Ms. Tamie Marie
Communication Consultant
HCC
Ms. Samantha Moitt
Chief Nutrition Officer,
Nutrition Unit
Ministry of Health,Wellness
and the Environment
Antigua and Barbuda
Mr. Luis Galicia
PAHO International Consultant
Sodium Reduction
Dr. Fabio da Silva Gomes
Advisor Nutrition and Physical
Activity
PAHO
Ms. Nicole Foster
Lecturer, Faculty of Law
and Head of Law
and Health Research Unit
Ms. Isabel Barbosa
Senior Associate
Adjunct Professor of Law
O’Neill Institute for National
and Global Health Law
Georgetown University
Law Center
Ms. Xarriah Nicholls
Youth Advocate
Person living with an NCD
Healthy Caribbean Youth
The post What Is Happening With Food Labels in CARICOM? appeared first on Healthy Caribbean Coalition.
2 years 1 month ago
Front-of-Package Nutrition Warning Labels, Latest, News, OWL, Slider, Webinars, STT2