Eastern Caribbean launches regional project
4 months 1 week ago
Health, PRESS RELEASE, amalia del riego, coronavirus, COVID-19, fao, food and agriculture organization, lilia burunciuc, paho, pan american health organisation, Pandemic Fund, priya basu, renata clarke, who, world bank, world health organisation
Aspergillus fumigatus, lethal fungus spreading across US raises alarm — Florida, Texas, California & more states at risk - Mint
- Aspergillus fumigatus, lethal fungus spreading across US raises alarm — Florida, Texas, California & more states at risk Mint
- Deadly drug-resistant fungus spreading fast across US, WHO raises alarm financialexpress.com
- What is Aspergillus fumigatus spreading in the US: About the deadly fungus that 'eats you from the inside Times of India
- Deadly fungus in US threatens lives as infection rates rise in These seven states Hindustan Times
- Climate change leads to spread of infection-causing fungi, scientists say ABC News
4 months 1 week ago
Walking more may prevent cause of lower back pain: Study - NewsNation
- Walking more may prevent cause of lower back pain: Study NewsNation
- Getting in more steps may prevent the leading cause of disability in the US, study says CNN
- Longer walks linked to lower risk of chronic low back pain Medical Xpress
- How far you walk may be more important than speed to fix chronic back pain The Independent
- Back pain can be eased with walking - but there's a specific number of minutes to reach per day Daily Mail
4 months 1 week ago
Deadly fungus in US threatens lives as infection rates rise in These seven states | World News - Hindustan Times - Hindustan Times
- Deadly fungus in US threatens lives as infection rates rise in These seven states | World News - Hindustan Times Hindustan Times
- Climate change leads to spread of infection-causing fungi, scientists say ABC News
- Aspergillus fumigatus, lethal fungus spreading across US raises alarm — Florida, Texas, California & more states at risk Mint
- Deadly fungus that 'eats you from the inside out' invades US: 'Hundreds of thousands of lives at risk' Daily Mail
- Not a virus or bacteria, but this silent killer is spreading and climate change is helping it thrive The Economic Times
4 months 1 week ago
STAT+: Pharmalittle: We’re reading about a Sarepta setback with a DMD drug, FDA workload causes a delay, and more
4 months 1 week ago
Pharmalot, pharmalittle, STAT+
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Who were the 30 doctors? RTI sparks questions in Pharma Freebies case
4 months 1 week ago
MDTV,Top Videos MDTV,Channels - Medical Dialogues,Top Videos
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Health Bulletin 16/June/2025
4 months 1 week ago
MDTV,Channels - Medical Dialogues,Health News today MDTV,Health News Today
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Adopting healthy diet may have cardiometabolic benefits regardless of weight loss, suggests study
4 months 2 weeks ago
Cardiology-CTVS,Medicine,Diet and Nutrition,Cardiology & CTVS News,Diet and Nutrition News,Medicine News,Top Medical News,Latest Medical News
Kristopher Mohamed needs help to fund cancer fight - Trinidad and Tobago Newsday
Kristopher Mohamed needs help to fund cancer fight
Trinidad and Tobago Newsday
4 months 2 weeks ago
Advice for trying GLP-1 drugs for weight loss from a doctor who's been there - NPR
- Advice for trying GLP-1 drugs for weight loss from a doctor who's been there NPR
- Medical experts warn 'Big Food' is fighting back against Ozempic with addictive items for sale Fox News
- You need more than Ozempic to fight food addiction. Here's how The Detroit News
- Ozempic Disrupts Big Food’s ‘Bliss Point’ Addiction Model Dallas Express
- You need more than Ozempic to fight food addiction Havasu News
4 months 2 weeks ago
Intermittent fasting's surprising biblical roots revealed as diet trend grows
4 months 2 weeks ago
Health, diet-trends, weight-loss, religion, food-drink, lifestyle, Nutrition, healthy-living
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
USFDA approves expanded indication for AbbVie Mavyret for Acute Hepatitis C Virus
4 months 2 weeks ago
News,Industry,Pharma News,Latest Industry News
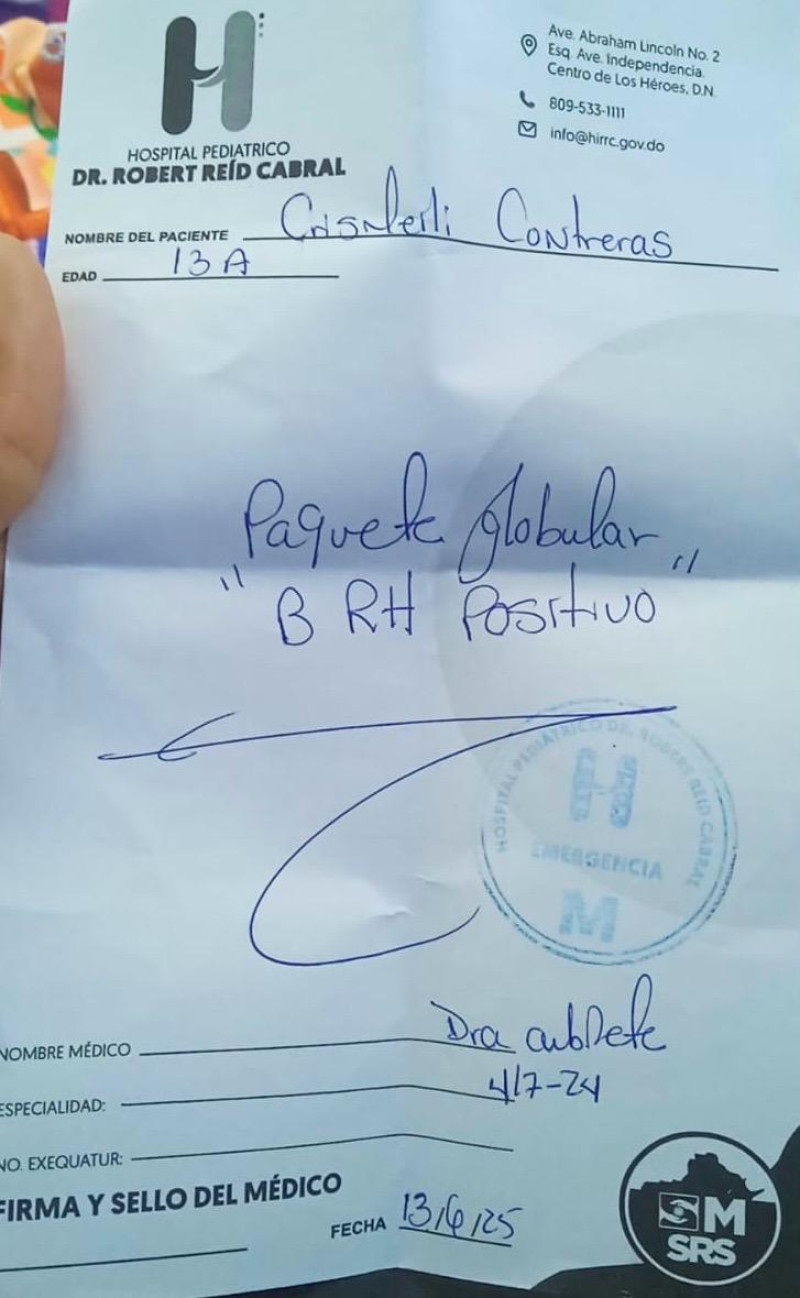
“B” positive blood urgently needed for a girl suffering from a rare disease
4 months 2 weeks ago
Health, Local
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Who were the 30 doctors? RTI sparks questions over secrecy in Pharma Freebies case
4 months 2 weeks ago
Editors pick,State News,News,Health news,Delhi,Doctor News,Latest Health News,Pharma News,NMC News,Notifications
Climate change leads to spread of infection-causing fungi, scientists say - ABC News
- Climate change leads to spread of infection-causing fungi, scientists say ABC News
- Deadly fungus that can "eat you from the inside out" is now in the U.S. and quickly spreading around the world Earth.com
- The deadly fungus spreading through Europe. Euro Weekly News
- Warning over hidden danger in compost that rots lungs and kills The Mirror
- Experts sound alarm over potentially lethal fungus that sounds straight out of 'The Last of Us': 'We're talking about hundreds of thousands of lives' The Cool Down
4 months 2 weeks ago