KFF Health News' 'What the Health?': Alabama’s IVF Ruling Still Making Waves
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
Reverberations from the Alabama Supreme Court’s first-in-the-nation ruling that embryos are legally children continued this week, both in the states and in Washington. As Alabama lawmakers scrambled to find a way to protect in vitro fertilization services without directly denying the “personhood” of embryos, lawmakers in Florida postponed a vote on the state’s own “personhood” law. And in Washington, Republicans worked to find a way to satisfy two factions of their base: those who support IVF and those who believe embryos deserve full legal rights.
Meanwhile, Congress may finally be nearing a funding deal for the fiscal year that began Oct. 1. And while a few bipartisan health bills may catch a ride on the overall spending bill, several other priorities, including an overhaul of the pharmacy benefit manager industry, failed to make the cut.
This week’s panelists are Julie Rovner of KFF Health News, Rachel Cohrs of Stat, Riley Griffin of Bloomberg News, and Joanne Kenen of Johns Hopkins University’s schools of nursing and public health and Politico Magazine.
Panelists
Rachel Cohrs
Stat News
Riley Griffin
Bloomberg
Joanne Kenen
Johns Hopkins Bloomberg School of Public Health and Politico
Among the takeaways from this week’s episode:
- Lawmakers are readying short-term deals to keep the government funded and running for at least a few more weeks, though some health priorities like preparing for a future pandemic and keeping down prescription drug prices may not make the cut.
- After the Alabama Supreme Court’s decision that frozen embryos are people, Republicans find themselves divided over the future of IVF. The emotionally charged debate over the procedure — which many conservatives, including former Vice President Mike Pence, believe should remain available — is causing turmoil for the party. And Democrats will no doubt keep reminding voters about it, highlighting the repercussions of the conservative push into reproductive health care.
- A significant number of physicians in Idaho are leaving the state or the field of reproductive care entirely because of its strict abortion ban. With many hospitals struggling with the cost of labor and delivery services, the ban is only making it harder for women in some areas to get care before, during, and after childbirth — whether they need abortion care or not.
- A major cyberattack targeting the personal information of patients enrolled in a health plan owned by UnitedHealth Group is drawing attention to the heightened risks of consolidation in health care. Meanwhile, the Justice Department is separately investigating UnitedHealth for possible antitrust violations.
- “This Week in Health misinformation”: Panelist Joanne Kenen explains how efforts to prevent wrong information about a new vaccine for RSV have been less than successful.
Also this week, Rovner interviews Greer Donley, an associate professor at the University of Pittsburgh School of Law, about how a 150-year-old anti-vice law that’s still on the books could be used to ban abortion nationwide.
Plus, for “extra credit” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: ProPublica’s “Their States Banned Abortion. Doctors Now Say They Can’t Give Women Potential Lifesaving Care,” by Kavitha Surana.
Rachel Cohrs: The New York Times’ “$1 Billion Donation Will Provide Free Tuition at a Bronx Medical School,” by Joseph Goldstein.
Joanne Kenen: Axios’ “An Unexpected Finding Suggests Full Moons May Actually Be Tough on Hospitals,” by Tina Reed.
Riley Griffin: Bloomberg News’ “US Seeks to Limit China’s Access to Americans’ Personal Data,” by Riley Griffin and Mackenzie Hawkins.
Also mentioned on this week’s podcast:
- The Washington Post’s “Florida Lawmakers Postpone ‘Fetal Personhood’ Bill After Alabama IVF Ruling,” by Lori Rozsa.
- Stat’s “Congress Punts on PBM Reform Efforts,” by Rachel Cohrs and John Wilkerson.
- Politico Magazine’s “There’s a New Life-Saving Vaccine. Why Won’t People Take It?” by Joanne Kenen.
- Stat’s “Experts Say Scale of Change Cyberattack Shows Risks of Centralized Claims Processing,” by Brittany Trang, Tara Bannow, and Bob Herman.
- The Wall Street Journal’s “U.S. Opens UnitedHealth Antitrust Probe,” by Anna Wilde Mathews and Dave Michaels.
- CNN’s “Opinion: It’s Too Dangerous to Allow This Antiquated Law to Exist Any Longer,” by David S. Cohen, Greer Donley, and Rachel Rebouché.
click to open the transcript
Transcript: Alabama’s IVF Ruling Still Making Waves
KFF Health News’ ‘What the Health?’Episode Title: Alabama’s IVF Ruling Still Making WavesEpisode Number: 336Published: Feb. 29, 2024
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello, and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News, and I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, Feb. 29, at 10 a.m. Happy leap day, everyone. As always, news happens fast and things might’ve changed by the time you hear this, so here we go.
We are joined today via video conference by Rachel Cohrs of Stat News.
Rachel Cohrs: Hi, everybody.
Rovner: Riley Ray Griffin of Bloomberg News.
Riley Griffin: Hello, hello.
Rovner: And Joanne Kenen of the Johns Hopkins University schools of nursing and public health and Politico Magazine.
Joanne Kenen: Hi, everybody.
Rovner: Later in this episode we’ll have my interview with University of Pittsburgh law professor Greer Donley about that 150-year-old Comstock Act we’ve talked about so much lately. But first, this week’s news.
So as we tape this morning, the latest in a series of short-term spending bills for the fiscal year that began almost five months ago, is a day and a half away from expiring, and the short-term bill for the rest of the government is 15 days from expiring. And apparently the House and Senate are in the process of preparing yet another pair of short-term bills to keep the government open for another week each, making the new deadlines March 8 and March 22. I should point out that the Food and Drug Administration is included in the first set of spending bills that would expire, and the rest of HHS [Department of Health and Human Services] is in the second batch.
So what are the chances that this time Congress can finish up the spending bills for fiscal 2024? Rachel, I call this Groundhog Day, except February’s about to be over.
Cohrs: Yeah, it’s definitely looking better. I think this is the CR [continuing resolution] where, as I’m thinking about it, the adults are in the room and the negotiations are actually happening. Because we had a couple of fake-outs there, where nobody was really taking it seriously, but I think we are finally at a place where they do have some agreement on some spending bills. The House hopefully will be passing some of them, and I’m optimistic that they’ll get it at least close within that March 8-March 22 time frame to extend us out a few more months until we get to do this all over again in September.
At least right now, which it could change, they do have a couple of weeks, but it’s looking like the main kind of health care provisions that we were looking at are going to be more of an end-of-year conversation than happening this spring.
Rovner: Which is anticipating my next question, which is a bunch of smaller bipartisan bills that were expected to catch a ride on the spending bill train seemed to have been jettisoned because lawmakers couldn’t reach agreement. Although it does look like a handful will make it to the president’s desk in this next round, and its last round, of fiscal spending bills for fiscal 2024.
Let’s start with the bills that are expected to be included when we finally get to these spending bills, presumably in March.
Cohrs: So, from my reporting, it sounds like that there’s going to be an extension of funding for the really truly urgent programs that are expiring. We’re talking community health center funding, funding for some public health programs. It’s funding for safety-net hospitals through Medicaid. Those policies might be extended. There’s a chance that there could be some bump in Medicare payments for doctors. I haven’t seen a final number on that yet, but that’s at least in the conversation for this round.
Again, there’s going to be more cuts at the end of this year. So, I think we’ll be continuing to have this conversation, but those look like they’re in for now. Again, we don’t have final numbers, but that’s kind of what we’re expecting the package to look like.
Kenen: And the opioids is under what you described as public health, right, or is that still up in the air?
Cohrs: I think we’re talking SUPPORT Act; I think that is up in the air, from my understanding. With public health programs talking, like, special diabetes reauthorization — there are a couple more small-ball things, but I think SUPPORT Act, PAHPA [Pandemic and All Hazards Preparedness Act], to my understanding, are still up in the air. We’ll just have to wait for text. That hopefully comes soon.
Rovner: Riley, I see you nodding too. Is that what you’re hearing?
Griffin: Yeah. Questions about PAHPA, the authorizations for pandemic and emergency response activities, have been front of mind for folks for months and months, particularly given the timing, right? We are seeing this expire at a time when we’ve left the biggest health crisis of our generation, and seeing that punted further down the road I think will come as a big disappointment to the world of pandemic preparedness and biodefense, but perhaps not altogether unexpected.
Rovner: So Rachel, I know there were some sort of bigger things that clearly got left on the cutting room floor, like legislation to do something about pharmacy benefit managers and site-neutral payments in Medicare. Those are, at least for the moment, shelved, right?
Cohrs: Yes. That’s from my understanding. Again, I will say now they bought themselves a couple more weeks, so who knows? Sometimes a near-death experience is what it takes to get people moving in this town. But the most recent information I have is that site-neutral payments for administering drugs in physicians’ offices, that has been shelved until the end of the year and then also reforms to how PBMs [pharmacy benefit managers] operate. There’s just a lot of different policies floating around and a lot of different committees and they just didn’t come to the table and hash it out in time. And I think leadership just lost patience with them.
They do see that there’s another bite at the apple at the end of the year. We do have a lot of members retiring, Cathy McMorris Rodgers on the House side, maybe [Sen.] Bernie Sanders. He has not announced he’s running for reelection yet. So I think that’s something to keep in mind for the end of the year. And there also is a big telehealth reauthorization coming up, so I think they view that as a wildly popular policy that’s going to be really expensive and it’s going to be another … give them some more time to just hash out these differences.
Kenen: I would also point out that this annual fight about Medicare doctor payments was something that was supposedly permanently fixed. Julie and I spent, and many other reporters, spent countless hours staking out hallways in Congress about this obscure thing that was called SGR, the sustainable growth rate, but everyone called it the “doc fix.” It was this fight every year that went on and on and on about Medicare rates and then they replaced it and it was supposed to be, “We will never have to deal with this again.”
I decided I would never write another story about it after the best headline I ever wrote, which was, “What’s up, doc fix?” But here we are again. Every single year, there’s a fight about …
Rovner: Although this isn’t the SGR, it’s just …
Kenen: They got rid of SGR, that era was over. But what we’ve learned is that era will probably never be over. Every single year, there will be a lobbying blitz and a fight about Medicare Advantage and about Medicare physician pay. It’s like leap year, but it happens every year instead of every four.
Rovner: Because lobbyists need to get paid too.
All right, well, I want to turn to abortion where the fallout continues from that Alabama Supreme Court ruling earlier this month that found frozen embryos are legally children. Republicans, in particular, are caught in an almost impossible position between portions of their base who genuinely believe that a fertilized egg is a unique new person deserving of full legal rights and protections, and those who oppose abortion but believe that discarding unused embryos as part of the in vitro fertilization process is a morally acceptable way for couples to have babies.
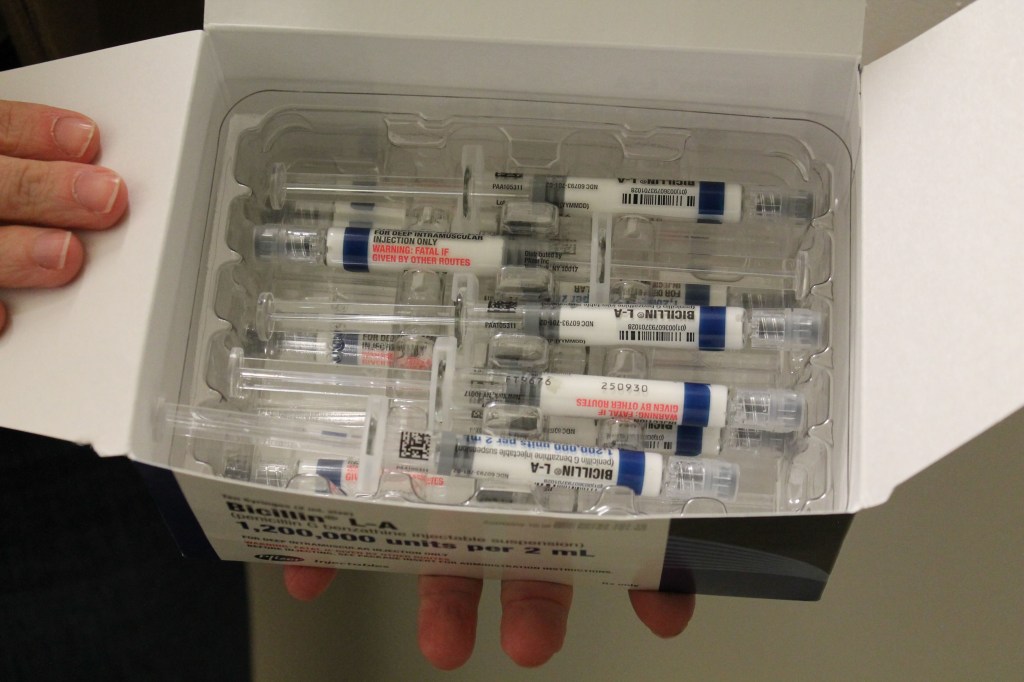
In Alabama, where the ruling has not just stopped IVF clinics from operating in the state, but has also made it impossible for those in the midst of an IVF cycle to take their embryos elsewhere because the companies that would transport them are also worried about liability, the Republican-dominated legislature is scrambling to find a way to allow IVF to resume in the state without directly contradicting the court’s ruling that “personhood” starts at fertilization.
This seems to be quite a tightrope. I mean, Riley, I see you nodding. Can they actually do this? Is there a solution on the table yet?
Griffin: No, I don’t think there’s a solution on the table yet, and there are eight clinics in Alabama that do this work, according to the CDC [Centers for Disease Control and Prevention]. Three of them have paused IVF treatment across the board. We’ve been in touch with these clinics as days go by as we see some of these developments, and they’re not changing their policies yet. Some of these efforts by Republicans to assure that there won’t be criminal penalties, they’re not reassuring them enough.
So, it certainly is a tightrope for providers and patients. It’s also a tightrope, as you mentioned, Julie, for the Republican Party, which is divided on this matter, and for Republican voters, who are also divided on this matter. But ultimately, this whole conversation comes back to what constitutes a human being? What constitutes a person? And the strategy of giving rights to an embryo allows abortion laws to be even more restrictive across this country.
Rovner: Yeah, I can’t tell you how many stories I’ve written about “When does life begin?” over the last 30 years, because that’s really what this comes down to. Does life begin at fertilization? Does it begin … I mean, doctors, I have learned this over the years, that conception is actually not fertilization. Conception is when basically a fertilized egg implants in a woman’s uterus. That’s when pregnancy begins. So there’s this continuing religious and scientific and ethical and kind of a quagmire that now is front and center again.
Joanne, you wanted to add something?
Kenen: No. I mean, I thought [Sen.] Lindsey Graham had one of the best quotes I’ve seen, which is, “Nobody’s ever been born in a freezer.” So this is a theological question that is turning into a political question. And even the proposed legislation in Alabama, which would give the clinics immunity or a pardon, I mean, pardon means you committed a crime. In this case, a murder, but you were pardoned for it. I mean, I don’t think that’s necessarily … and it’s only good for this was a stopgap that would, if it passes, I believe it would be just till early 2025.
So it might get these clinics open for a while. They may come up with some way of getting families that are in the middle of fertility treatments to be able to complete it, but other states could actually go the way Alabama went. We have no guarantee. There are people pushing for that in some of the more conservative states, so this may spread. The attempt in Congress, in the Senate, to bring up a bill that would address it …
Rovner: We’ll get to that in a second.
Kenen: I mean, Alabama’s a conservative state, but the governor, who was a conservative anti-abortion governor, has said she wants to reopen the clinics and protect them, but they haven’t come up with the formula to do that yet.
Rovner: So speaking of other states, when this decision came down in Alabama, Florida was preparing to pass its own personhood bill, but now that vote has been delayed at the request of the bill’s sponsor. The, I think, initial reaction to the Alabama decision was that it would spur similar action in other states, as you were just saying, Joanne, but is it possible that the opposite will happen, that it will stop action in other states because those who are pushing it are going to see that there’s a huge divide here?
Griffin: That hesitation certainly signals that that’s a possibility. The pause in pushing forward that path in Florida is a real signal that there is going to be more debate within the Republican Party.
One thing I do want to mention is a lot of focus has been on whether clinics in Alabama or otherwise would stop IVF treatment altogether. But I think equally important is how the clinics that are continuing to offer IVF treatment, what changes they’re making. The ones that we’re seeing, are speaking with in Alabama that are continuing to offer IVF, are changing their consent forms. They are fertilizing fewer eggs, they’re freezing eggs, but they’re not fertilizing them because they don’t want to have excess wastage, in their perspective, that could lead them to a place of liability.
So all these things ultimately have ramifications for patients. That is more costly. It means a longer timeline. It also means fewer shots on goal. It means that it is potentially harder for you to get pregnant, at the end of the day. So I want to center the fact that clinics that are continuing to offer IVF are facing real changes here too.
Rovner: We know from Texas that when states try to indemnify, saying, “Well, we won’t prosecute you,” that that’s really not good enough because doctors don’t want to run the chance of ending up in court, having to hire lawyers. I mean, even if they’re unlikely to be convicted and have their licenses taken away, just being charged is hard enough. And I think that’s what’s happening with doctors with some of these abortion exceptions, and that’s what’s happening with these IVF clinics in places where there’s personhood.
Sorry, Joanne. Go ahead.
Kenen: Egg-freezing technology has gotten better than it was just a few years ago, but egg-freezing technology, to the best of my knowledge, egg-freezing technology, though improved, is nowhere near as good as freezing an embryo. Particularly now they can bring embryos out to what they call the blastocyst stage. It’s about five days. They have a better chance of successful implantation.
In addition to the expense of IVF, and it’s expensive and most people don’t have insurance cover[age] for it, it means you’re going through drugs and treatment and all of us have had friends, I think, who’ve gone through it or relatives. It is just an incredibly stressful, emotionally painful process.
Rovner: Well, you’re pumping yourself full of hormones to create more eggs, so yeah.
Kenen: And you’re also trying to get pregnant. If you’re spending $20,000 a cycle or whatever it is, and pumping yourself full of hormones, doing all this, it means that having a child is of utmost importance to you.
And the emotional trauma of this, if you listen to the … we’ve heard interviews in the last few days of women who were about to have a transfer and things like that, the heartbreak is intense, and fertility is not like catching a cold. It’s really stressful and sad, and this is just causing anguish to families trying to have a child, trying to have a first child, trying to have a second child, whatever, or trying to have a child because there’s a health issue and they want to do the pre-implantation genetic testing so that they don’t have another child die. I mean, it’s really complicated and terrible costs on all kinds of costs, physical, emotional, and financial.
Rovner: Yeah, there are lots of layers to this.
Well, meanwhile, this decision has begun to have repercussions here on Capitol Hill. In the Senate, the Democrats are, again, while it’s in the news, trying to force Republicans into taking a stand on this issue by bringing up a bill that would guarantee nationwide access to IVF. This is a bill that they tried to bring up before and was blocked by Republicans. On Wednesday, a half a dozen senators led by Illinois’ Tammy Duckworth, a veteran who used IVF to have her two children, chided Republicans on the floor who failed again to let them bring up the IVF bill. This time, as last time, it was blocked by Republican Sen. Cindy Hyde-Smith of Mississippi.
I imagine the Democrats aren’t going to let this go anytime soon though. They certainly indicated that this is not their last attempt at this.
Kenen: No. Why should they? If anyone thought that the politics of abortion were going to subside by November, this has just given it … I don’t even have a word for how much it’s been reinvigorated. This is going to stick in people’s minds, and Republicans are divided on IVF, but there’s no path forward. Democrats are going to be trying again and again, if they can, and they’re going to remind voters of it again and again.
Rovner: And in the Republican House, they’re scrambling to figure out again, as in Alabama, how to demonstrate support for IVF without running afoul of their voters who are fetal personhood supporters.
Just to underline how delicate this all is, the personhood supporting anti-abortion group, Susan B. Anthony [Pro-Life America], put out a statement this week, not just thrashing the Democrats’ bill, which one would expect, but also the work going on by Republicans in Alabama and in the U.S. House for not going far enough. They point out that Louisiana has a law that allows for IVF, but not for the destruction of leftover embryos. Although that means, as Riley was saying before, those embryos have to be stored out of state, which adds to the already high cost of IVF.
It is really hard to imagine how Republicans at both the state and federal level are going to find their way out of this thicket.
Kenen: It’s a reproductive pretzel.
Griffin: It’s a reproductive pretzel where two-thirds of Americans say frozen embryos shouldn’t be considered people. So I mean, there is data to suggest that this isn’t a winning selling point for the Republican Party, and we saw that play out with presidential candidate Donald Trump immediately distancing himself from the Alabama Supreme Court decision. So, what a pretzel it is.
It’s going to be interesting to see how this pans out as the logistical hurdles continue to arise. And some are basic. I mean, I spoke last week with one clinic in Alabama that said that they had had dozens, I think they said 30 to 40, embryos that had been abandoned over decades going back as 2008, and they had tried to reach people by phone, by mail, by email. They had just been left behind. What do you do in that situation? They had been prepared to dispose of those embryos and now they’re sitting on shelves. Is that the answer? Is the only answer to have shelves and shelves of frozen embryos?
Rovner: Yeah, I mean, it is. It is definitely a pretzel.
Kenen: There was a move at one point to allow them to be adopted. I think …
Rovner: It’s still there. It’s still there.
Kenen: Right, but I don’t know what kind of consent you need. I mean, if the situations where someone left the frozen embryo and doesn’t respond or their email, they’ve changed their email or whatever, there may be some kind of way out for this mess that involves the possibility of adopting them at some point down the road, and they may not be biologically viable by that point. But when I was thinking of what are the political outs, what is the exit ramp, I haven’t heard any politicians talk about this yet, but that occurred to me as something that might end up figuring into this.
And the other thing, just to the point as to how deeply divided, I think many listeners know this, but for the handful who don’t, the illustration of how deeply divided even very anti-abortion Republicans are, is [former Vice President] Mike Pence, his family was created through IVF, and he’s clearly, he’s come out this week. I mean, there’s no question that Mike Pence is anti-abortion, there’s not a lot of doubt about that, but he has come forth and endorsed IVF as a life-affirming rather, as a good thing.
Rovner: And I actually went and checked when this all broke because Joanne probably remembers in the mid-2000s when they were talking about stem cell research that President George W. Bush had a big event with what were called “snowflake children,” which were children who were born because they were adopted leftover embryos that someone else basically gestated, and that …
Kenen: But I don’t think they’ll call them “snowflake” anymore.
Rovner: Yeah. Well, that adoption agency is still around and still working and still accepting leftover embryos to be adopted out. That does still exist. I imagine that’s probably of use in Louisiana too, where you’re not allowed to destroy leftover embryos.
Well, meanwhile, we have some new numbers on something else we’ve been talking about since Dobbs [v. Jackson Women’s Health Organization]. Doctors who deliver babies in states with abortion bans are choosing to leave rather than to risk arrest or fines for providing what they consider evidence-based care. In Idaho, according to a new report, 22% of practicing obstetricians stopped practicing or left the state from August 2022 to November 2023. And, at the same time, two hospitals’ obstetric programs in the state closed, while two others report having trouble recruiting enough doctors to keep their doors open.
I would think this is going to particularly impact more sparsely populated states like Idaho, which also, coincidentally or not, are the states that tend to have the strictest abortion bans. I mean, it’s going to be … this seems to be another case where it’s going to be harder, where abortion bans are going to make it harder to have babies.
Cohrs: Yeah. I mean, we’re already seeing a trend of hospital systems being reluctant to keep OB-GYN delivery units open anyway. We’ve seen care deserts. It’s really not a profitable endeavor unless you have a NICU [neonatal intensive care unit] attached. So I think this just really compounds the problems that we’ve been hearing about staffing, about rural health in general, recruiting, and just makes it one step harder for those departments that are really important for women to get the care they need as they’re giving birth, and just making sure that they’re safe and well-staffed for those appointments leading up to and following the birth as well.
Kenen: Right. And at a time we’re supposedly making maternal mortality a national health priority, right? So you can’t really protect women at risk, and, as Rachel said, it’s during childbirth, but it’s for months after. And without proper care, we are not going to be able to either bring down the overall maternal mortality rates nor close the racial disparities.
Griffin: I was just going to say, I highly recommend a story the New Yorker did this past January, “Did an Abortion Ban Cost a Young Texas Woman Her Life?” It’s a view into many of these different themes and will show you a real human story, a tragic one at that, about what these deserts, how they have consequential impact on people’s lives for both mother and baby.
Rovner: Yeah, and we talked about that when it came out. So if you go back, if you scroll back, you’ll find a link to it in the show notes.
I was going to say March is when we get “Match Day,” which is when graduating medical students find out where they’re going to be completing their training. And we saw just sort of the beginnings last year of kind of a dip in graduating medical students who want to become OB-GYNs who are applying to programs in states with abortion bans. I’ll be really curious this year to see whether that was a statistical anomaly or whether really people who want to train to be OB-GYNs don’t want to train in states where they’re really worried about changing laws.
We have to move on. I want to talk about something I’m calling the most under-covered health story of the month, a huge cyberattack on a company called Change Healthcare, which is owned by health industry giant UnitedHealth [Group]. Change processes insurance claims and pharmacy requests for more than 300,000 physicians and 60,000 pharmacies. And as of Wednesday, its systems were still down a week after the attack.
Rachel, I feel like this is a giant flashing red light of what’s at risk with gigantic consolidation in the health care industry. Am I wrong?
Cohrs: You’re right, which is why a couple of my colleagues did cover it as just this important red flag. And there are new SEC [Securities and Exchange Commission] reporting rules as well that require more disclosure around these kind of events. So I think that will …
Rovner: Around the cyberattacks?
Cohrs: Yes, around the cyberattacks, yes. But I think just the idea that, we’ll talk about this later too, but that Change is owned by UnitedHealth and just so much is consolidated that it really does create risks when there are vulnerabilities in these very essential processes. And I think a lot of people just don’t understand how many health care companies, they don’t provide any actual care. They’re just helping with the backroom kind of operations. And when you get these huge conglomerates or services that are bundled together under one umbrella, then it really does show you how a very small company maybe not everyone had heard of before this week could take down operations when you go to your pharmacy, when you go to your doctor’s office.
Rovner: Yeah, and there are doctors who aren’t getting paid. I mean, there’s bills that aren’t getting processed. Everything was done through the mail and it was slow and everybody said, “When we digitize it, it’s all going to be better and it’s all going to happen instantly.” And mostly what it’s done is it’s created all these other companies who are now making money off the health care system, and it’s why health care is a fifth of the U.S. economy.
But anticipating what you were about to say, Rachel, speaking of the giant consolidation in the health industry by UnitedHealth, I am not the only one, we are not the only ones who have noticed. The Wall Street Journal reported this week that the Justice Department has begun an antitrust investigation of said UnitedHealthcare, which provides not only health insurance and claims processing services like those from Change Healthcare, but also through its subsidiary Optum, owns a network of physician groups, one of the largest pharmacy benefit managers, and provides a variety of other health services. Apparently one question investigators are pursuing is whether United favors Optum-owned groups to the detriment of competing doctors and providers.
I think my question here is what took so long? I know that the Justice Department looked at it when United was buying Change Healthcare, but then they said that was OK.
Cohrs: Yeah. I will say I think this is a great piece of reporting here, and these are excellent questions about what happens when the vertical integration gets to this level, which we just really haven’t seen with UnitedHealthcare, where they’re aggressively acquiring provider clinics. I think it was a home health care company that they were trying to buy as well.
So I think it is interesting because now that the acquisitions have happened on some of these, there will be evidence and more material for investigators to look at. It won’t be a theoretical anymore. So I will be interested to see just how this plays out, but it does seem like the questions they’re asking are pretty wide-ranging, certainly related to providers, but also related to an MLR [medical loss ratio]. What if you own a provider that’s charging your insurance company? How does that even work and what are the competitive effects of that for other practices? So I think …
Rovner: And MLRs, for those who are not jargonists, it’s minimum loss ratios [also known as medical loss ratio], and it’s the Affordable Care Act requirement that insurers spend a certain amount of each dollar on actual care rather than overhead and profit and whatnot. So yeah, when you’re both the provider and the insurer, it’s kind of hard to figure out how that’s going.
I am sort of amazed that it’s taken this long because United has been sort of expanding geometrically for the last decade or so.
Kenen: It’s sort of like the term vertical integration, which is the correct term that Rachel used, but as she said that, I sort of had this image of a really tall, skinny, vertical octopus. There’s more and more and more things getting lumped into these big, consolidating, enormous companies that have so much control over so much of health care and concentrated in so few hands now. It’s not just United. I mean, they’re big, but the other big insurers are big too.
Cohrs: Right. I did want to also mention just that we’re kind of seeing this play out in other places too, like Eli Lilly creating telehealth clinics to prescribe their obesity medications. Again, there’s no evidence that they’re connected to this in any way, but I think it is going to be a cautionary tale for other health care companies who are looking into this model and asking themselves, “If UnitedHealthcare can do it, why can’t we do it?” It will be interesting to see how this plays out for the rest of the industry as well.
Rovner: Yeah, when I started covering health policy, I never thought I was going to become a business reporter, but here we are.
Moving on to “This Week in Health Misinformation,” we have Joanne, or rather an interesting, and as it turns out, extremely timely story about vaccines that Joanne wrote for Politico Magazine. Joanne, tell us your thesis here with this story.
Kenen: I wanted to look at how much the public health and clinician community had learned about combating misinformation, sort of a real-life, real-time unfolding before our eyes, which was the rollout of the RSV vaccine.
And I think the two big takeaways, I mean, it’s a fairly … I guess there were sort of three takeaways from that article. One, is they’ve learned stuff but not enough.
Two, is that it’s not that there was this huge campaign against the RSV vaccine, there is misinformation about the RSV vaccine, but basically it just got subsumed into this nonstop, ever-growing anti-vaccine movement that you didn’t have to target RSV. Vaccines is a dirty word for a section of the population.
And the third thing I learned is that the learning about fighting disinformation, the tools we have, you can learn about those tools and deploy those tools, but they don’t work great. There’ve been some studies that have found that what they call debunking or fact-checking, teaching people that what they believe is untrue, that they say, “Ah, that’s not right,” and then a week later they’re back to their original, as little as one week in some studies. One week, you’re back to what you originally thought. So we just don’t know how to do this yet. There are more and more tools, but we are not there.
Rovner: Well, and I say this story is timely because we’re looking at a pretty scary measles outbreak in Florida and a Florida surgeon general who has rejected all established public health advice by telling parents it’s up to them whether to send their exposed-but-unvaccinated children to school rather than keep them home for the full 21 days that measles can take to incubate.
The surgeon general has been publicly taken to task by, among others, Florida’s former surgeon general. I can remember several measles outbreaks over the years, often in less-than-fully-vaccinated communities, but I can’t remember any public health officials so obviously flouting standard public health advice.
Joanne, have you ever seen anything like this?
Kenen: No. It’s like his public stance is like, “Measles, schmeasles.” It’s like a parent has the right to decide whether they’re potentially contagious, goes to school and infects other children, some of whom may be vulnerable and have health problems. It is this complete elevation of medical liberty or medical freedom completely disconnected to the fact that we are connected to one another. We live in communities. We supposedly care about one another. We don’t do a very good job of that, and this is sort of the apotheosis of that.
Rovner: And one of the main reasons that public schools require vaccines is not just for the kids themselves, but for kids who may have younger siblings at home who are not yet fully vaccinated. That’s the whole idea behind herd immunity, is that if enough people are vaccinated then those who are still not fully vaccinated will be protected because it won’t be floating around. And obviously in Florida, measles, which is, according to many doctors, one of the most contagious diseases on the planet, is making a bit of a comeback. So it is sort of, as you point out, kind of the end result of this demonization of all vaccines.
Kenen: And our overall vaccination rate for childhood immunization has dropped and it’s dropped, I’d have to fact-check myself, I think what you need for herd immunity is 95% and it’s …
Rovner: I think it’s over 95.
Kenen: And that we’re down to maybe 93[%]. I mean, this number was in that article that I wrote, but I wrote it a few weeks ago and I may be off by a percentage point, so I want to sort of clarify that nobody should quote me without double-checking that. But basically, we’re not where we need to be and we’re not where we were just a few years ago.
Rovner: Another space we will continue to watch.
Well, that is this week’s news. Now we will play my interview with law professor Greer Donley, and then we will come back and do our extra credits.
I am thrilled to welcome to the podcast, Greer Donley, associate dean for research and faculty development and associate professor of law at the University of Pittsburgh Law School. She’s an expert in legal issues surrounding reproductive health in general and abortion in particular, and someone whose work I have regularly relied on over the past several years, so thank you so much for joining us.
Greer Donley: I’m so happy to be here. Thanks for having me.
Rovner: So I’ve asked you here to talk about how an anti-abortion president could use an 1873 law called the Comstock Act to basically ban abortion nationwide. But first, because it is still so in the news, I have to ask you about the controversy surrounding the Alabama Supreme Court’s ruling that frozen embryos for in vitro fertilization are legally children. Do you think this is a one-off, or is this the beginning of states really, fully embracing the idea of personhood from the moment of fertilization?
Donley: Man, I have a lot to say about that. So I’ll start by saying that first of all, this is the logical extension of what people have been saying for a long time about, “If life starts at conception, this is what that means.” So in some sense, this is one of those things where people say, “Believe people when they tell you something.” Folks have been saying forever, “Life starts at conception.” This is a logical outgrowth of that. So in some sense, it’s not particularly surprising.
It’s also worth noting that states have been moving towards personhood for decades, often through these kind of state laws, like wrongful death, which is exactly what happened here. So this is the first case that found that an embryo outside of a uterus was a children for this purpose of wrongful death, but many states had been moving in the direction of finding a fetus or even an embryo that’s within a pregnant person to be a child for the purpose of wrongful death for a while now. And that has always been viewed as the anti-abortion movement towards personhood. In some sense, this is just kind of the logical outgrowth, the logical extension, of the personhood movement and the permission that Dobbs essentially gave to states to go as far as they wanted to on this question.
So whether or not this is going to be the beginning of a new trend is, I think, in my mind, going to be really shaped by public backlash to the Alabama decision, particularly. I think that many folks within the anti-abortion movement, again, they mean what they say. They do believe that this is a life and it should be treated as any other life, but whether or not they are going to perceive this as the ideal political climate in which to push that agenda is another question.
And my personal view is that, given the backlash to the Alabama Supreme Court, you might see folks retreating a little bit from this. I think we’re starting to see a little bit of that, where more moderate people within the Republican Party are going to say, “This is not the moment to go this far,” or maybe even, “I’m not sure I actually support this logical outgrowth of my own opinion,” and so we’re going to have to kind of …
Rovner: “I co-sponsored this bill, but I didn’t realize that’s what it would do.”
Donley: Exactly. Right? So we’re going to, I think, really have to see how people’s views change in response to the backlash.
Rovner: Let us go back to Comstock. Who was this person, Anthony Comstock? What does this law do and why is it still on the books 151 years after it was passed?
Donley: Ugh, yes, OK. So Anthony Comstock, he is what people often call, “The anti-vice crusader.” This law passed in 1873. It’s actually a series of laws, but we often compile them and call them the Comstock Act.
The late 1800s were a moment of change, where many people in this country were for the first time being exposed to the idea that abortion is immoral for religious reasons. Before that for a long time, in the early 1800s, people regularly purchased products to try to what they call, “Bring on the menses,” or menstrual regulation. So it was not uncommon. It was a fairly commonly held view up until late 1800s that the pregnancy was nothing until it was a quickening, there was a quickening where the pregnant person felt movement.
So Comstock was one of the people who was really kind of a part of changing that culture in the late 1800s, and he had the power as the post office inspector of investigating the mail throughout our country. So he was influential not only in helping to pass a law that made it illegal to ship through interstate commerce all sorts of things that he considered immoral, which explicitly included abortion and contraception, but also used vague terms like “anything immoral.” And he was the person that was then in charge of enforcing those laws by actually investigating the mail. His investigations led to pretty horrible outcomes, including many people killing themselves after he started investigating them for a variety of Comstock-related crimes at the time.
So obviously, this law was passed before women had the right to vote, in a completely different time period than we exist today, and it really remained on the books by an accident of history, in my mind.
So in the early 1900s, there was a series of cases. This was the moment where we particularly saw a huge movement towards birth control. So as that movement was going on, you saw a lot of litigation in the courts that were interpreting the Comstock laws related to contraception, finding that it had to be narrowly limited to only unlawful contraception or unlawful abortion. Because the Comstock laws, by its terms, which this should shock everybody who’s hearing me, has literally no exceptions, not even for the life of the pregnant person. And it is so broad that it would ban abortion nationwide from the beginning of a pregnancy without exception. Procedural abortion, pills, everything.
Rovner: And people think of this as the U.S. mail, but it’s not just the U.S. mail. It’s basically any way you move things across state lines, right?
Donley: Right. Because we live in a national economy now, so there’s nothing in medicine that exists in a purely intrastate environment. So every abortion provider in the country is dependent on them and their state mail to get things that they need for procedural abortion and pills.
In the early to mid-1900s, right around the 1930s, there was a series of cases that said this law only applied for unlawful contraception and abortion because they had to read that term into the law. Eventually in the late 1930s, you saw the federal government stop enforcing it completely. And then you had the constitutional cases came out that found a right to contraception and abortion, and so the law was presumed unconstitutional for half a century. No one was repealing it because everyone assumed that it was never going to come back to life. In comes Dobbs, in come the modern anti-abortion movement, and now we are here.
Rovner: Yeah. So how could a President Trump, if he returns to the White House, use this to ban abortion nationwide?
Donley: Yes, because this law was never repealed, and because the case that presumptively made it unconstitutional, Roe v. Wade, and the cases that came after that, are now no longer good law, presumptively the law, like a zombie, comes back to life.
And so the anti-abortion movement is now trying to reinterpret the law, right? We’re talking about such a long period of time and all those 1930s cases, since that time period, you have the rise of what we call textualism, which is a theory of statutory interpretation that really likes to stick to the text. That was something that’s been around for a while, but in modern jurisprudence, that has become increasingly important, and the anti-abortion movement sees, “Well, all these judges are now textualists, and we can say this law is still good. By its clear terms, it bans shipping through interstate commerce anything that could be used for an abortion. Voila. We have our national abortion ban without having to get a single vote in Congress. All we need is a Republican president that will enforce the law as it’s written and on the books today,” and that is their theory.
Rovner: And that’s included, I think, in one of the briefs that was filed today in the abortion pill case, right?
Donley: Absolutely. In that case, that’s a case concerning the regulation of mifepristone, one of the abortion pills, that’s before the Supreme Court this summer. You had parties saying, “The law is clear and it is as broad as it’s written,” essentially.
Rovner: Well, this doesn’t apply to contraception anymore, right?
Donley: Right. So right after the Supreme Court case Griswold [v. Connecticut], which found a constitutional right to contraception, but before Roe, you had the Congress actually repealed the portion of Comstock related to contraception. But again, it was before Roe, so they didn’t repeal the part related to abortion, and then Roe came in and made that part presumptively unconstitutional.
Of course, going back in time, we would say, “You got to repeal that law. You have no idea what the future may be,” but I don’t think people really saw this moment coming. They should have. We should have all been preparing for this more. But, yeah.
Rovner: One of the things that I don’t think I had appreciated until I read the op-ed that you co-wrote, thank you very much, is that there could be a reach-back here. It’s not even just abortions going forward, right?
Donley: Right. So the idea here is that, generally, laws have a statute of limitations, right? So you could potentially have a President Trump come in, say that he’s going to start enforcing this law immediately, and even if the second Jan. 1 comes, people stop shipping anything through interstate commerce, he could still go back and say, “Well, the statute of limitations is five years.” So you go back in time for five years and potentially bring charges against someone.
So one of the important pieces of advocacy that we might have in this moment is to really encourage President Biden, if he were to not win the election, to preemptively essentially pardon anybody for any Comstock-related crimes to make sure that that can’t be used against them. That’s a power he actually has and will be a very important power for him to use in that instance. But it’s quite alarming how Comstock could be used in this period, but also retrospectively.
Rovner: Last question, and I know the answer to this, but I think I need to remind listeners, if Congress doesn’t have to pass anything to implement a nationwide ban, why haven’t previous anti-abortion Republican presidents tried to do this?
Donley: While Roe and [Planned Parenthood of Southeastern Pennsylvania v.] Casey were good law, there was no way that they could possibly do that. It would’ve been unconstitutional for them to try to criminalize people for exercising their constitutional right to reproductive health care for abortion. So we’re really in a new moment where essentially the Supreme Court overturned those cases while President Biden was in office, and so the real question is whether a Republican administration could come in and change everything.
Rovner: We shall see. Greer Donley, thank you so much for coming to explain this.
Donley: Thank you for having me.
Rovner: OK, we are back. It’s time for our extra-credit segment. That’s when we each recommend a story we read this week we think you should read, too. As always, don’t worry if you miss it. We will post the links on the podcast page at kffhealthnews.org and in our show notes on your phone or other mobile device.
Rachel, you were the first to choose this week. Why don’t you go first?
Cohrs: The article I chose is in The New York Times. The headline is “$1 Billion Donation Will Provide Free Tuition at a Bronx Medical School” by Joseph Goldstein. And it’s about how this 93-year-old widow of an early investor in Berkshire Hathaway has given $1 billion to a medical school in the Bronx to pay for students’ tuition. And I think her idea behind it is that it will open up the pool of students who might be able to go to medical school. I imagine applications might increase to this school as well. And she was a professor at the school during her career as well.
To me, it’s not a scalable solution necessarily for the cost of medical education, but I think it does highlight how broke everything is. When we’re talking about Medicare payment to doctors, I think one of the arguments they always use is doctors have debt and there’s inflation and costs have gone up so much, and I think the cost of education in this country certainly is one factor in that, that it’s really hard to address from a simply health care policy standpoint.
So I think not necessarily a scalable solution, but will definitely make a difference in a lot of students’ lives and just give them more freedom to practice in the specialty that they might want to, which we all know we need more primary care doctors and doctors in a variety of different settings. So I think it’s a rare piece of good news.
Rovner: Yeah, it might not be scalable, but it’s not the first, which is kind of … I remember, in fact, NYU is now having a no-tuition medical school. UCLA, although I think UCLA is only for students who can demonstrate financial need. But in doing those earlier stories, and I have not updated this, at the time, which is a couple of years ago, the average medical student debt graduating is over $250,000. So you can see why they feel like they need to be in more lucrative specialties because they’re going to be paying their student loans back until they’re in their 40s, most of them. This is clearly a step in that direction.
Riley, why don’t you go next?
Griffin: Yeah. I wanted to share a story that I’ve been fairly obsessed with over the last month. It’s one of my own. It’s “US Seeks to Limit China’s Access to Americans’ Personal Data.” This week, the Biden administration announced that it is issuing, or has at this point issued, an executive order to secure Americans’ sensitive personal data, and we broke this story about a month ago.
Why it is so interesting to the health world is, one of the key parts that was a motivating factor in putting together this executive order, is DNA, genomic data. The U.S., the National Security Council, our national security apparatus is really concerned about what China and other foreign adversaries are doing with our genetic information. And we can get more into that in the story itself, but it is fascinating, and now we’re seeing real action to regulate and protect and ensure that that bulk data doesn’t get into the hands of people who want to use it for blackmail and espionage.
Rovner: Yeah, it was super scary, I will say. Joanne?
Kenen: I couldn’t resist this one. It’s in Axios. It’s by Tina Reed, and the headline is “An Unexpected Finding Suggests Full Moons May Actually Be Tough on Hospitals.” Caveat, before I go on, there is research out there that proves what I’m about to say is wrong.
But anyway, a company that makes panic buttons, so a hospital security company that one of the things they do is provide panic buttons, they did a study of how and when these panic buttons are used, and they found they go up during full moons. And they also found that other things rise during full moons. GI [gastro-intestinal] disorders go up, ambulance rides connected to motor vehicle accidents go up, and psychiatric admissions go up. So maybe that research that I cited at the beginning saying this is hogwash needs to be reevaluated in some subcategories.
Rovner: There’s always new things to find out in science.
My extra credit this week is from ProPublica. It’s called “Their States Banned Abortion. Doctors Now Say They Can’t Give Women Potential Lifesaving Care,” by Kavitha Surana. It’s another in a series of stories we’ve seen about women with serious pregnancy complications that are not immediately life-threatening, but who nevertheless can’t get care that their doctors think they need.
This story, however, is written from the point of view of the doctors, specifically members of an abortion committee at Vanderbilt Hospital in Nashville who are dealing with the Tennessee ban that’s one of the strictest in the nation. It’s really putting doctors in an almost impossible position in some cases, feeling that they can’t even tell patients what the risks are of continuing their pregnancies for fear of violating that Tennessee law. It’s a whole new window into this story that we keep hearing about and a really good read.
OK. That is our show. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left us a review. That helps other people find us too. Special thanks as always to our very patient technical guru, Francis Ying, and our editor, Emmarie Huetteman.
As always, you can email us your comments or questions. We’re at whatthehealth@kff.org, or you can still find me hanging around at Twitter, @jrovner, or @julierovner at Bluesky and @julie.rovner at Threads.
Joanne, where are you hanging these days?
Kenen: Mostly at Threads, @joannekenen1. I still occasionally use X, and that’s @JoanneKenen.
Rovner: Riley, where can we find you on social media?
Griffin: You can find me at X @rileyraygriffin.
Rovner: And Rachel?
Cohrs: I’m at X @rachelcohrs and on LinkedIn more these days, so feel free to follow me there.
Rovner: There you go. We’ll be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 8 months ago
Courts, Multimedia, States, Abortion, Alabama, Florida, Health IT, Idaho, KFF Health News' 'What The Health?', Misinformation, Podcasts, U.S. Congress, Women's Health
Opinion: A new Louisiana capital-punishment bill would fundamentally alter physician licensing
After the recent nitrogen gas execution in Alabama of Kenneth Smith, state Attorney General Steve Marshall said that nitrogen gas “was intended to be — and has now proved to be — an effective and humane method of execution.”
After the recent nitrogen gas execution in Alabama of Kenneth Smith, state Attorney General Steve Marshall said that nitrogen gas “was intended to be — and has now proved to be — an effective and humane method of execution.”
It is hard to imagine a statement so obviously disconnected from facts. Eyewitness accounts described Smith’s death as a harrowing experience of dry heaving, thrashing, straining against leather straps, seizures, and terror. It took about a half-hour for Smith to die, although the state had previously predicted it would be over in minutes.
1 year 8 months ago
First Opinion, ethics, physicians, States
Pregnancy Care Was Always Lacking in Jails. It Could Get Worse.
It was about midnight in June 2022 when police officers showed up at Angela Collier’s door and told her that someone anonymously requested a welfare check because they thought she might have had a miscarriage.
Standing in front of the concrete steps of her home in Midway, Texas, Collier, initially barefoot and wearing a baggy gray T-shirt, told officers she planned to see a doctor in the morning because she had been bleeding.
Police body camera footage obtained by KFF Health News through an open records request shows that the officers then told Collier — who was 29 at the time and enrolled in online classes to study psychology — to turn around.
Instead of taking her to get medical care, they handcuffed and arrested her because she had outstanding warrants in a neighboring county for failing to appear in court to face misdemeanor drug charges three weeks earlier. She had missed that court date, medical records show, because she was at a hospital receiving treatment for pregnancy complications.
Despite her symptoms and being about 13 weeks pregnant, Collier spent the next day and a half in the Walker County Jail, about 80 miles north of Houston. She said her bleeding worsened there and she begged repeatedly for medical attention that she didn’t receive, according to a formal complaint she filed with the Texas Commission on Jail Standards.
“There wasn’t anything I could do,” she said, but “just lay there and be scared and not know what was going to happen.”
Collier’s experience highlights the limited oversight and absence of federal standards for reproductive care for pregnant women in the criminal justice system. Incarcerated people have a constitutional right to health care, yet only a half-dozen states have passed laws guaranteeing access to prenatal or postpartum medical care for people in custody, according to a review of reproductive health care legislation for incarcerated people by a research group at Johns Hopkins School of Medicine. And now abortion restrictions might be putting care further out of reach.
Collier’s arrest was “shocking and disturbing” because officers “blithely” took her to jail despite her miscarriage concerns, said Wanda Bertram, a spokesperson for the Prison Policy Initiative, a nonprofit organization that studies incarceration. Bertram reviewed the body cam footage and Collier’s complaint.
“Police arrest people who are in medical emergencies all the time,” she said. “And they do that regardless of the fact that the jail is often not equipped to care for those people in the way an emergency room might be.”
After a decline during the first year of the pandemic, the number of women in U.S. jails is once again rising, hitting nearly 93,000 in June 2022, a 33% increase over 2020, according to the Department of Justice. Tens of thousands of pregnant women enter U.S. jails each year, according to estimates by Carolyn Sufrin, an associate professor of gynecology and obstetrics at Johns Hopkins School of Medicine, who researches pregnancy care in jails and prisons.
The health care needs of incarcerated women have “always been an afterthought,” said Dana Sussman, deputy executive director at Pregnancy Justice, an organization that defends women who have been charged with crimes related to their pregnancy, such as substance use. For example, about half of states don’t provide free menstrual products in jails and prisons. “And then the needs of pregnant women are an afterthought beyond that,” Sussman said.
Researchers and advocates worry that confusion over recent abortion restrictions may further complicate the situation. A nurse cited Texas’ abortion laws as one reason Collier didn’t need care, according to her statement to the standards commission.
Texas law allows treatment of miscarriage and ectopic pregnancies, a life-threatening condition in which a fertilized egg implants outside the uterus. However, different interpretations of the law can create confusion.
A nurse told Collier that “hospitals no longer did dilation and curettage,” Collier told the commission. “Since I wasn’t hemorrhaging to the point of completely soaking my pants, there wasn’t anything that could be done for me,” she said.
Collier testified that she saw a nurse only once during her stay in jail, even after she repeatedly asked jail staffers for help. The nurse checked her temperature and blood pressure and told her to put in a formal request for Tylenol. Collier said she completed her miscarriage shortly after being released.
Collier’s case is a “canary in a coal mine” for what is happening in jails; abortion restrictions are “going to have a huge ripple effect on a system already unequipped to handle obstetric emergencies,” Sufrin said.
‘There Are No Consequences’
Jail and prison health policies vary widely around the country and often fall far short of the American College of Obstetricians and Gynecologists’ guidelines for reproductive health care for incarcerated people. ACOG and other groups recommend that incarcerated women have access to unscheduled or emergency obstetric visits on a 24-hour basis and that on-site health care providers should be better trained to recognize pregnancy problems.
In Alabama, where women have been jailed for substance use during pregnancy, the state offers pregnancy tests in jail. But it doesn’t guarantee a minimum standard of prenatal care, such as access to extra food and medical visits, according to Johns Hopkins’ review.
Policies for pregnant women at federal facilities also don’t align with national standards for nutrition, safe housing, and access to medical care, according to a 2021 report from the Government Accountability Office.
Even when laws exist to ensure that incarcerated pregnant women have access to care, the language is often vague, leaving discretion to jail personnel.
Since 2020, Tennessee law has required that jails and prisons provide pregnant women “regular prenatal and postpartum care, as necessary.” But last August a woman gave birth in a jail cell after seeking medical attention for more than an hour, according to the Montgomery County Sheriff’s Office.
Pregnancy complications can quickly escalate into life-threatening situations, requiring more timely and specialized care than jails can often provide, said Sufrin. And when jails fail to comply with laws on the books, little oversight or enforcement may exist.
In Louisiana, many jails didn’t consistently follow laws that aimed to improve access to reproductive health care, such as providing free menstrual items, according to a May 2023 report commissioned by state lawmakers. The report also said jails weren’t transparent about whether they followed other laws, such as prohibiting the use of solitary confinement for pregnant women.
Krishnaveni Gundu, as co-founder of the Texas Jail Project, which advocates for people held in county jails, has lobbied for more than a decade to strengthen state protections for pregnant incarcerated people.
In 2019, Texas became one of the few states to require that jails’ health policies include obstetrical and gynecological care. The law requires jails to promptly transport a pregnant person in labor to a hospital, and additional regulations mandate access to medical and mental health care for miscarriages and other pregnancy complications.
But Gundu said lack of oversight and meaningful enforcement mechanisms, along with “apathy” among jail employees, have undermined regulatory protections.
“All those reforms feel futile,” said Gundu, who helped Collier prepare for her testimony. “There are no consequences.”
Before her arrest, Collier had been to the hospital twice that month experiencing pregnancy complications, including a bladder infection, her medical records show. Yet the commission found that Walker County Jail didn’t violate minimum standards. The commission did not consider the police body cam footage or Collier’s personal medical records, which support her assertions of pregnancy complications, according to investigation documents obtained by KFF Health News via an open records request.
In making its determination, the commission relied mainly on the jail’s medical records, which note that Collier asked for medical attention for a miscarriage once, in the morning on the day she was released, and refused Tylenol.
“Your complaint of no medical care is unfounded,” the commission concluded, “and no further action will be taken.”
Collier’s miscarriage had ended before she entered the jail, argued Lt. Keith DeHart, jail lieutenant for the Walker County Sheriff’s Office. “I believe there was some misunderstanding,” he said.
Brandon Wood, executive director of the commission, wouldn’t comment on Collier’s case but defends the group’s investigation as thorough. Jails “have a duty to ensure that those records are accurate and truthful,” he said. And most Texas jails are complying with heightened standards, he said.
Bertram disagrees, saying the fact that care was denied to someone who was begging for it speaks volumes. “That should tell you something about what these standards are worth,” she said.
Last year, Chiree Harley spent six weeks in a Comal County, Texas, jail shortly after discovering she was pregnant and before she could get prenatal care, she said.
I was “thinking that I was going to be well taken care of,” said Harley, 37, who also struggled with substance use.
Jail officials put her in the infirmary, Harley said, but she saw only a jail doctor and never visited an OB-GYN, even though she had previous pregnancy complications including losing multiple pregnancies at around 21 weeks. This time she had no idea how far along she was.
She said that she started leaking amniotic fluid and having contractions on Nov. 1, but that jail officials waited nearly two days to take her to a hospital. Harley said officers forced her to sign papers releasing her from jail custody while she was having contractions in the hospital. Harley delivered at 23 weeks; the baby boy died less than a day later in her arms.
The whole experience was “very scary,” Harley said. “Afterwards we were all very, very devastated.”
Comal County declined to send Harley’s medical and other records in response to an open records request. Michael Shaunessy, a partner at McGinnis Lochridge who represents Comal County, said in a statement that, “at all times, the Comal County Jail provided Chiree Harley with all appropriate and necessary medical treatment for her and her unborn child.” He did not respond to questions about whether Harley was provided specialized obstetric care.
‘I Trusted Those People’
In states like Idaho, Mississippi, and Louisiana that installed near-total abortion bans after the Supreme Court eliminated the constitutional right to abortion in 2022, some patients might have to wait until no fetal cardiac activity is detected before they can get care, said Kari White, the executive and scientific director of Resound Research for Reproductive Health.
White co-authored a recent study that documented 50 cases in which pregnancy care deviated from the standard because of abortion restrictions even outside of jails and prisons. Health care providers who worry about running afoul of strict laws might tell patients to go home and wait until their situations worsen.
“Obviously, it’s much trickier for people who are in jail or in prison, because they are not going to necessarily be able to leave again,” she said.
Advocates argue that boosting oversight and standards is a start, but that states need to find other ways to manage pregnant women who get caught in the justice system.
For many pregnant people, even a short stay in jail can cause lasting trauma and interrupt crucial prenatal care.
Collier remembers being in “disbelief” when she was first arrested but said she was not “distraught.”
“I figured I would be taken care of, that nothing bad was gonna happen to me,” she said. As it became clear that she wouldn’t get care, she grew distressed.
After her miscarriage, Collier saw a mental health specialist and started medication to treat depression. She hasn’t returned to her studies, she said.
“I trusted those people,” Collier said about the jail staff. “The whole experience really messed my head up.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 8 months ago
States, Alabama, Idaho, Louisiana, Mississippi, Pregnancy, Prison Health Care, Tennessee, texas, Women's Health
KFF Health News' 'What the Health?': Alabama Court Rules Embryos Are Children. What Now?
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
The Alabama Supreme Court’s groundbreaking ruling last week that frozen embryos have legal rights as people has touched off a national debate about the potential fallout of the “personhood” movement. Already the University of Alabama-Birmingham has paused its in vitro fertilization program while it determines the ongoing legality of a process that has become increasingly common for those wishing to start a family.
Meanwhile, former President Donald Trump is reportedly leaning toward endorsing a national, 16-week abortion ban. At the same time, former aides are planning a long agenda of reproductive health restrictions should Trump win a second term.
This week’s panelists are Julie Rovner of KFF Health News, Lauren Weber of The Washington Post, Rachana Pradhan of KFF Health News, and Victoria Knight of Axios.
Panelists
Victoria Knight
Axios
Rachana Pradhan
KFF Health News
Lauren Weber
The Washington Post
Among the takeaways from this week’s episode:
- The Alabama Supreme Court’s decision on embryonic personhood could have wide-ranging implications beyond reproductive health care, with potential implications for tax deductions, child support payments, criminal law, and much more.
- Donald Trump is considering a national abortion ban at 16 weeks of gestation, according to recent reports. It is unclear whether such a ban would go far enough to please his conservative supporters, but it would be far enough to give Democrats ammunition to campaign on it. And some are looking into using a 19th-century anti-smut law, the Comstock Act, to implement a national ban under a new Trump presidency — no action from Congress necessary.
- New reporting from KFF Health News draws on many interviews with clinicians at Catholic hospitals about how the Roman Catholic Church’s directives dictate the care they may offer patients, especially in reproductive health. It also draws attention to the vast number of religiously affiliated hospitals and the fact that, for many women, a Catholic hospital may be their only option.
- Questions about President Joe Biden’s cognitive health are drawing attention to ageism in politics — as well as in American life, with fewer people taking precautions against the covid-19 virus even as it remains a serious threat to vulnerable people, especially the elderly. The mental fitness of the nation’s leaders is a valid, relevant question for many voters, though the questions are also fueled by frustration with a political system in which many offices are held by older people who have been around a long time.
Plus, for “extra credit” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: Stat’s “New CMS Rules Will Throttle Access Researchers Need to Medicare, Medicaid Data,” by Rachel M. Werner.
Lauren Weber: The Washington Post’s “They Take Kratom to Ease Pain or Anxiety. Sometimes, Death Follows,” by David Ovalle.
Rachana Pradhan: Politico’s “Red States Hopeful for a 2nd Trump Term Prepare to Curtail Medicaid,” by Megan Messerly.
Victoria Knight: ProPublica’s “The Year After a Denied Abortion,” by Stacy Kranitz and Kavitha Surana.
Also mentioned on this week’s podcast:
- The New York Times’ “Trump Privately Expresses Support for a 16-Week Abortion Ban,” by Maggie Haberman, Jonathan Swan, and Lisa Lerer.
- The New York Times’ “Trump Allies Plan New Sweeping Abortion Restrictions,” by Lisa Lerer and Elizabeth Dias.
- Politico’s “Trump Allies Prepare to Infuse ‘Christian Nationalism’ in Second Administration,” by Alexander Ward and Heidi Przybyla.
- KFF Health News’ “The Powerful Constraints on Medical Care in Catholic Hospitals Across America,” by Rachana Pradhan and Hannah Recht.
- The Washington Post’s “Tax Records Reveal the Lucrative World of Covid Misinformation,” by Lauren Weber.
- KFF Health News’ “Do We Simply Not Care About Old People?” by Judith Graham.
- Stat’s “A Neuropsychologist Clarifies Science on Aging and Memory in Wake of Biden Special Counsel Report,” by Annalisa Merelli.
click to open the transcript
Transcript: Alabama Court Rules Embryos Are Children. What Now?
KFF Health News’ ‘What the Health?’Episode Title: Alabama Court Rules Embryos Are Children. What Now?Episode Number: 335Published: Feb. 22,2024
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello, and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News, and I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, Feb. 22, at 10 a.m. As always, news happens fast, and things might have changed by the time you hear this, so here we go. We are joined today via video conference by Lauren Weber of The Washington Post.
Lauren Weber: Hello, hello.
Rovner: Victoria Knight of Axios.
Victoria Knight: Hello, everyone.
Rovner: And my KFF Health News colleague Rachana Pradhan.
Rachana Pradhan: Hi, there. Good to be back.
Rovner: Congress is out this week, but there is still tons of news, so we will get right to it. We’re going to start with abortion because there is lots of news there. The biggest is out of Alabama, where the state Supreme Court ruled last week that frozen embryos created for IVF [in vitro fertilization] are legally children and that those who destroy them can be held liable. In fact, the justices called the embryos “extrauterine children,” which, in covering this issue for 40 years, I never knew was a thing. There are lots of layers to this, but let’s start with the immediate, what it could mean to those seeking to get pregnant using IVF. We’ve already heard that the University of Alabama’s IVF clinic has ceased operations until they can figure out what this means.
Pradhan: I think that that is the immediate fallout right now. We’ve seen Alabama’s arguably flagship university saying that they are going to halt. And I believe some of the coverage that I saw, there was even a woman who was about to start a cycle or was literally about to have embryos implanted and had to encounter that extremely jarring development. Beyond the immediate, and of course, Julie, I’m sure we’ll talk about this, a bit about the personhood movement and fetal rights movement in general, but a lot of the country might say, “Oh, well, it’s Alabama. It’s only Alabama.” But as we know it, it really just takes one state, it seems like these days, to open the floodgates for things that might actually take hold much more broadly across the country. So that’s what I’m …
Rovner: It’s funny, the first big personhood push I covered was in 2011 in Mississippi, so next door to Alabama, very conservative state, where everybody assumed it was going to win. And one of the things that the opposition said is that this would ban most forms of birth control and IVF, and it got voted down in Mississippi. So here we are, what, 13 years later. But I mean, I think people don’t quite appreciate how IVF works is that doctors harvest as many eggs as they can and basically create embryos. Because for every embryo that results in a successful pregnancy, there are usually many that don’t.
And of course, couples who are trying to have babies using IVF tend to have more embryos than they might need, and, generally, those embryos are destroyed or donated to research, or, in some cases — I actually went back and looked this up — in the early 2000s there was a push, and it’s still there, there’s an adoption agency that will let you adopt out your unused embryos for someone else to carry to term. And apparently, all of this, I guess maybe not the adoption, but all the rest of this could theoretically become illegal under this Alabama Supreme Court ruling.
Pradhan: And one thing I just want to say, too, Julie, piggybacking on that point too is not just in each cycle that someone goes through with IVF — as you said, there are multiple embryos — but it often takes two people who want to start a family, it often takes multiple IVF cycles to have a successful pregnancy from that. It’s not like it’s a one-time shot, it usually takes a long time. And so you’re really talking about a lot of embryos, not just a one-and-done situation.
Rovner: And every cycle is really expensive. I know lots of people who have both successfully and unsuccessfully had babies using IVF and it’s traumatic. The drugs that are used to stimulate the extra eggs for the woman are basically rough, and it costs a lot of money, and it doesn’t always work. It seems odd to me that the pro-life movement has gotten to the point where they are stopping people who want to get pregnant and have children from getting pregnant and having children. But I guess that is the outflow of this. Lauren, you wanted to add something?
Weber: Yeah, I just wanted to chime in on that. I mean, I think we’re really going to see a lot of potential political ramifications from this. I mean, after this news came down, and just to put in context, the CDC [Centers for Disease Control and Prevention] reported in 2021 that there were 91,906 births via IVF. So that’s almost 92,000 families in 2021 alone. You have a political constituency of hundreds of thousands of parents across the U.S. that feel very strongly about this because they have received children that they paid a lot of money for and worked very hard to get. And it was interesting after this news came down — I will admit, I follow a lot of preppy Southern influencers who are very apolitical and if anything conservative, who all were very aggressively saying, “The only reason I could have my children is through this. We have to make a stand.”
I mean, these are not political people. These are people that are — you could even argue, veering into tradwife [traditional wife] territory in terms of social media. I think we’re really going to see some political ramifications from this that already are reflected in what Donald Trump has recently been reported as feeling about how abortion limits could cost him voters. I do wonder if IVF limits could really cause quite an uproar for conservative candidates. We’ll see.
Rovner: Yeah. Well, Nikki Haley’s already gotten caught up in this. She’s very pro-life. On the other hand, she had one of her children using IVF, which she’s been pretty frank about. She, of course, got asked about this yesterday and her eyes had the deer-in-the-headlights look, and she said, “Well, embryos are children,” and it’s like, “Well, then what about your extra embryos?” Which I guess nobody asked about. But yeah, I mean clearly you don’t have to be a liberal to use IVF to have babies, and I think you’re absolutely right. I want to expand this though, because the ruling was based on this 2018 constitutional amendment approved by voters in Alabama that made it state policy to, quote, “Recognize and support the sanctity of unborn life and the rights of unborn children.”
I should point out that this 2018 amendment did not directly try to create fetal personhood in the way that several states tried — and, as I mentioned, failed — in the 2010s, yet that’s how the Alabama Supreme Court interpreted it. Now, anti-abortion advocates in other states, Rachana, you mentioned this, are already trying to use this decision to apply to abortion bans and court cases there. What are the implications of declaring someone a person at the moment of fertilization? It obviously goes beyond just IVF, right?
Knight: Well, and I think you mentioned already, birth control is also the next step as well. Which basically they don’t want you to have a device that will stop a sperm from reaching an egg. And so I think that could have huge ramifications as well. So many young women across the U.S. use IUDs or other types of birth control. I know that’s one application that people are concerned about. I don’t know if there are others.
Rovner: Yeah, I’ve seen things like, if you’re pregnant, can you now drive in the HOV [high-occupancy vehicle] lane because you have another person?
Pradhan: I think that’s one of the more benign, maybe potential impacts of this. But I mean, if an embryo is a child, I mean it would affect everything from, I think, criminal laws affecting murder or any other … you could see there being criminal law impacts there. I think also, as far as child support, domestic laws, involving families, what would you — presumably maybe not everyone that I imagine who are turning to fertility treatments to start a family or to grow a family may not have a situation where there are two partners involved in that decision. I think it could affect everything, frankly. So much of our tax estate laws are impacted by whether people have children or not, and so …
Rovner: And whether those children have been born yet.
Pradhan: … tax deductions, can you claim an embryo as a dependent? I mean, it would affect everything. So I think they’re very wide, sweeping ramifications beyond the unfortunate consequences that some people might face, as Lauren said, which is that they’re just trying to start a family and now that’s being jeopardized.
Rovner: I think Georgia already has a law that you can take a tax deduction if you’re pregnant. I have been wondering, what happens to birthdays? Do they cease to mean anything? It completely turns on its head the way we think about people and humans, and I mean obviously they say, “Well, yeah, of course it is a separate being from the moment of fertilization, but that doesn’t make it a legal person.” And I think that’s what this debate is about. I did notice in Alabama — of course, what happened, what prompted this case was that some patient in a hospital got into the lab where the frozen embryos were kept and took some out and literally just dropped them on the floor and broke the vial that they were in. And the question is whether the families who belong to those embryos could sue for some kind of recourse, but it would not be considered murder because, under Alabama’s statutes, it has to be a child in utero.
And obviously frozen embryos are not yet in utero, they’re in a freezer somewhere. In that sense it might not be murder, but it could become — I mean, this is something that I think people have been thinking about and talking about obviously for many years, and you wonder if this is just the beginning of we’re going to see how far this can go, particularly in some of the more conservative states. Well, meanwhile, The New York Times reported last week that former President Trump, who’s literally been on just about every side of the abortion debate over the years, is leaning towards supporting a 16-week ban — in part, according to the story, because it’s a round number. Trump, of course, was a supporter of abortion rights until he started running for president as a Republican.
And, in winning the endorsement of skeptical anti-abortion groups in 2016, promised to appoint only anti-abortion judges and to reimpose government restrictions from previous Republican administrations. He did that and more, appointing the three Supreme Court justices who enabled the overturn of Roe v. Wade. But more recently, he’s seen the political backlash over that ruling and the number of states that have voted for abortion rights, including some fairly red states, and he’s been warning Republicans not to emphasize the issue. So why would he fail to follow his own advice now, particularly if it would animate voters in swing states? He keeps saying he’s not in the primaries anymore, that he’s basically running a general-election campaign.
Knight: I mean, I think to me, it seems like he’s clearly trying to thread the needle here. He knows some of the more social conservative of his supporters want him to do something about abortion. They want him to take a stand. And so he decided on allegedly 16 weeks, four months, which is less strict than some states. We saw Florida was 10 weeks. And then some other states …
Rovner: I think Florida is six weeks now.
Knight: Oh, sorry, six weeks. OK.
Rovner: Right. Pending a court decision.
Knight: Yeah. And then other states, in Tennessee, complete abortion ban with little room for exceptions. So 16 weeks is longer than some other states have enacted that are stricter. Roe v. Wade was about 24 weeks. So to me, it seems like he’s trying to find some middle ground to try to appease those social conservatives, but not be too strict.
Rovner: Although, I mean, one of the things that a 16-week ban would not do is protect all the women that we’ve been reading about who are with wanted pregnancies, who have things go wrong at 19 or 20 or 21 weeks, which are before viability but after 16 weeks. Well, unless they had — he does say he wants exceptions, and as we know, as we’ve talked about every week for the last six months, those exceptions, the devil is in the details and they have not been usable in a lot of states. But I’m interested in why Trump, after saying he didn’t want to wade into this, is now wading into this. Lauren, you wanted to add something?
Weber: Yeah, I wanted to echo your point because I think it’s important to note that 16 weeks is not based, it seems like, on any scientific reason. It sounds like to me, from what I understand from what’s out there, that 20 weeks is more when you can actually see if there’s heart abnormalities and other issues. So it sounds like from the reporting the Times did, was that he felt like 16 weeks was good as, quote, “It was a round number.” So this isn’t exactly, these weak timing of bans, as I’m sure we’ve discussed with this podcast, are not necessarily tied towards scientific development of where the fetus is. So I think that’s an important thing to note.
Rovner: Yes. Rachana.
Pradhan: I mean, I think, and we’ve talked about this, but it’s the perennial danger in weighing in on any limit, and certainly a national limit, but any limit at all, is that 16 weeks, of course as the anti-abortion movement and I think many more people know now, the CDC data shows that the vast majority of abortions annually occur before that point in pregnancy. And so there are, of course, some anti-abortion groups that are trying to thread the needle and back a more middle-ground approach such as this one, 15 weeks, 16 weeks, banning it after that point. But for many, it’s certainly not anywhere good enough. And I think if you’re going to try to motivate your conservative base, I still have a lot of questions about whether they would find that acceptable. And I think it depends on how they message it, honestly.
If they say, “This is the best we can do right now and we’re trying,” that might win over some voters. But on the flip side, it’s still enough for Democrats to be able to run with it and say any national ban obviously is unacceptable to them, but it gives them enough ammunition, I think, to still say that former President Trump wants to take your rights away. And I think, as Lauren noted, genetic testing and things these days of course can happen and does happen before 16 weeks. So there might be some sense of whether there might be, your child has a lethal chromosomal disorder or something like that, that might make the pregnancy not viable. But the big scan that happens about midway through pregnancy is around 20 weeks, and that’s often when you, unfortunately, some people find out that there are things that would make it very difficult for their baby to survive so …
Rovner: Well, it seems that no matter what Trump does or says he will do if he’s elected in November, it’s clear that people close to him, including former officials, are gearing up for a second term that could go way further than even his very anti-abortion first term. According to Politico, a plan is underway for Trump to govern as a, quote, “Christian nationalist nation,” which could mean not just banning abortion, but, as Victoria pointed out, contraception, too, or many forms of contraception. A separate planning group being run out of the Heritage Foundation is also developing far-reaching plans about women’s reproductive health, including enforcement of the long-dormant 19th century Comstock Act, which we have talked about here many times before. But someone please remind us what the Comstock Act is and what it could mean.
Weber: I feel like you’re the expert on this. I feel like you should explain it.
Rovner: Oh boy. I don’t want to be the expert on the Comstock Act, but I guess I’ve become it. It’s actually my favorite tidbit about the Comstock Act is that it is not named after a congressman. It is named after basically an anti-smut crusader named Anthony Comstock in the late 1800s. And it bans the mailing of, I believe the phrase is “lewd or obscene” information, which in the late 1880s included ways to prevent pregnancy, but certainly also abortion. When the Supreme Court basically ruled that contraception was legal, which did not happen until the late 1960s — and early 1970s, actually —, the Comstock Act sort of ceased to be. And obviously then Roe v. Wade, it ceased to be.
But it is still in the books. It’s never been officially repealed, and there’s been a lot of chatter in anti-abortion movements about starting to enforce it again, which could certainly stop if nothing else, the distribution of the abortion pill in its tracks. And also it’s anything using the mail. So it could not just be the abortion pill, but anything that doctors use to perform abortions or to make surgical equipment — it seems that using Comstock, you could implement a national ban without ever having to worry about Congress doing anything. And that seems to be the goal here, is to do as much as they can without even having to involve Congress. Yes.
Pradhan: Julie, I’m waiting for the phrase “anti-smut crusader” to end up on a campaign sign or bumper sticker, honestly. I feel like we might see it. I don’t think this election has gotten nearly weird enough yet. So we still have nine months to go.
Rovner: Yeah. I’m learning way more about the Comstock Act than I really ever wanted to know. But meanwhile, Rachana, it does not take state or federal action to restrict access to reproductive health care. You have a story this week about the continuing expansion of Catholic hospitals and what that means for reproductive health care. Tell us what you found.
Pradhan: Well, yes, I would love to talk about our story. So myself and my colleague Hannah Recht, we started reporting the story, just for background, before the Supreme Court’s Dobbs decision, obviously anticipating that that is what was going to happen. And our story really digs into, based on ample interviews with clinicians, other academic experts, reading lots of documents about what the ethical and religious directives for Catholic health care services, which is what all, any health facility, a hospital, a physician’s office, anything that deems itself Catholic, has to abide by these directives for care, and they follow church teaching. Which we were talking about fertility treatments and IVF earlier actually, so in vitro fertilization is also something that the Catholic Church teaches is immoral. And so that’s actually something that they oppose, which many people may not know that.
But other things that the ERDs [ethical and religious directives] so to speak, impact are access to contraception, access to surgeries that would permanently prevent pregnancy. So for women that would be removing or cinching your fallopian tubes, but also, for men, vasectomies. And then, of course, anything that constitutes what they would call a direct abortion. And that affects everything from care for ectopic pregnancies, how you can treat them, to managing miscarriages. The lead story or anecdote in our story is about a nurse midwife who I spoke with, who used to work at a Catholic hospital in Maryland and talked to me about, relayed this anecdote about, a patient who was about 19 or 20 weeks pregnant and had her water break prematurely.
At that point, her fetus was not viable and that patient did not want to continue her pregnancy, but the medical staff there, what they would’ve done is induce labor with the intent of terminating the pregnancy. And they were unable to do that because of ERDs. And so, we really wanted to look at it systemically, too. So we looked at that combined with state laws that protect, shield hospitals from liability when they oppose providing things like abortions or even sterilization procedures on religious grounds. And included fresh new data analysis on how many women around the country live either nearby to a Catholic hospital or only have Catholic hospitals nearby. So we thought it was important.
Rovner: That’s a little bit of the lead because there’s been so much takeover of hospitals by Catholic entities over the last, really, decade and a half or so, that women who often had a choice of Catholic hospital or not Catholic hospital don’t anymore. That Catholic hospital may be the only hospital anywhere around.
Pradhan: Right and if people criticize the story, which we’ve gotten some criticism over it, one of the refrains we’ll hear is, “Well, just go to a different hospital.” Well, we don’t live in a country where you can just pick any hospital you want to go to — even when you have a choice, insurance will dictate what’s in-network versus what’s not. And honestly, people just don’t know. They don’t know that a hospital has a religious affiliation at all, let alone that that religious affiliation could impact the care that you would receive. And so there’s been research done over the years showing the percentage of hospital beds that are controlled by Catholic systems, et cetera, but Hannah and I both felt strongly that that’s a useful metric to a point, but beds is not relatable to a human being. So we really wanted to boil it down to people and how many people we’re talking about who do not have other options nearby. How many births occur in Catholic hospitals so that you know those people do not have access to certain care if they deliver at these hospitals, that they would have in other places.
Rovner: It’s a continuing story. We’ll obviously post the link to it. Well, I also want to talk about age this week. Specifically the somewhat advanced age of our likely presidential candidates this year. President [Joe] Biden, currently age 81, and former President Trump, age 77. One thing voters of both parties seem to agree on is that both are generically too old, although voters in neither party seem to have alternative candidates in mind. My KFF Health News colleague Judy Graham has a really interesting piece on increasing ageism in U.S. society that the seniors we used to admire and honor we now scorn and ignore. Is this just the continuing irritation at the self-centeredness of the baby boomers or is there something else going on here that old people have become dispensable and not worth listening to? I keep thinking the “OK, boomer” refrain. It keeps ringing in my ears.
Weber: I mean, I think there’s a mix of things going on here. I mean, her piece was really fascinating because it also touched upon the fact — which all of us here reported on; Rachana and I wrote a story about this back in 2021 — on how nursing homes really have been abandoned to some extent. I mean, folks are not getting the covid vaccine. People are dying of covid, they die of the flu, and it’s considered a way of life. And there is almost an irritation that there would be any expectation that it would be any differently because it’s a “Don’t infringe upon my rights” thought. And I do think her piece was fascinating because it asks, “Are we really looking at the elderly?”
I mean, I think that’s very different when we talk about politicians. I mean, the Biden bit is a bit different. I mean, I think there is some frustration in the American populace with the age of politicians. I think that reached a bit of a boiling point with the Sen. [Dianne] Feinstein issue, that I think is continuing to boil over in the current presidential election. But that said, we’re hurtling towards an election with these two folks. I mean, that’s where we’re at. So I think they’re a bit different, but I do think there is a national conversation about age that is happening to some degree, but is not happening in consideration to others.
Well, I was going to say, I think the other aspect is that these people are in the public all the time, or they’re supposed to be. President Biden is giving speeches. Potential candidate President Trump, GOP main candidate, he’s in the spotlight all the time, too. And so you can actually see when they mess up sometimes. You can see potentially what people are saying is signs of aging. And so I think it’s different when they’re literally in front of your eyes and they’re supposed to be making decisions about the direction of this country, potentially. So I think it’s somewhat a valid conversation to have when the country is in their hands.
Rovner: Yeah, and obviously the presidency ages you. [Barack] Obama went in as this young, strong-looking guy and came out with very gray hair, and he was young when he went in. Bill Clinton, too, was young when he was elected and came out looking considerably older. And so Biden, if people have pointed out, looks a lot older now than he did when he was running back in 2020. But meanwhile, despite what voters and some special councils think — including the one who said that Biden was what a kindly old man with a bad memory — neuroscientists say that it’s actually bunk that age alone can determine how mentally fit somebody is, and that even if memory does start to decline, judgment and wisdom may improve as you age. Why is nobody in either party making this point? I mean, the people supporting Biden are just saying that he’s doing a good job and he deserves to continue doing a good job. I mean, talk about the elephant in the room and nobody’s talking about it at all with Trump.
Pradhan: Yeah, I mean, I think probably the short answer is that it’s not really as politically expedient to talk about those things. I thought it was really interesting. Yeah, I really appreciated Stat News had this really interesting Q&A article. And then also there was this opinion piece in The New York Times that, this line struck me so much about, again, both about Biden’s age and his memory. And this line I thought was so fascinating because it just is telling how people’s perceptions can change so much depending on the discourse. So it pointed out that Joe Biden is the same age as Harrison Ford, Paul McCartney, Martin Scorsese. He’s younger than Berkshire Hathaway CEO Warren Buffett, who is considered to be one of the shrewdest and smartest investors, I think, and CEOs of modern times. And no one is saying, “Well, they’re too old to be doing their jobs” or anything. I’m not trying to suggest that people who have concerns about both candidates’ age[s] are not valid, but I think we sometimes have to double-check why we might be being led to think that way, and when it’s not really the same standards are not applied across the board to people who are even older than they are.
Rovner: I do think that some of the frustration, I think, Lauren, you mentioned this, is that in recent years, the vast majority of leadership positions in the U.S. government have been held by people who are, shall we say, visibly old. I mean Nancy Pelosi is still in Congress, but she at least figured out that she needed to step down from being speaker because I think the three top leaders in the House were all in their either late 70s or early 80s. The Senate has long been the land of very old people because you get elected to a six-year term. I mean, Chuck Grassley is 90 now, is he not? Feinstein wasn’t even, I don’t think, the oldest member of the Senate. So I think it’s glaring and staring us in the face. Rachana, you wanted to add something before we moved on.
Pradhan: Well, I think probably, and a lot of that too is just I think probably a reflection of voters’ broader gripes or concerns about the fact that we have people who hold office for an eternity, to not exaggerate it. And so people want to see new leadership, new energy, and when you have public officeholders who hold these jobs for … they’re career politicians, and I think that that is frustrating to a lot of people. They want to see a new generation, even regardless of political party, of ideas and energy. And then when you have these octogenarians holding onto their seats and run over and over and over again, I think that that’s frustrating. And people don’t get energized about those candidates, especially when they’re running for president. They just don’t. So it’s a reflection of just, I think, broader concerns.
Knight: And I think one more thing too was, I mean, Sen. Feinstein died while she was in office. I mean, people also may be referencing Ruth Bader Ginsburg on the Supreme Court, and it’s the question of, should you be holding onto a position that you may die in it, and not setting the way for the new person to take over and making that path available for the next people? Is that the best way to lead in whatever position you’re in? I think, again, Rachana said that’s frustrating for a lot of people.
Rovner: And I think what both parties have been guilty of, although I think Democrats even more than Republicans, is preparing people, making sure that that next generation is ready, that you don’t want to go from these people with age and wisdom and experience to somebody who knows nothing. You need those people coming up through the ranks. And I think there’s been a dearth of people coming up through the ranks lately, and I think that’s probably the big frustration.
Pradhan: I’m not sure if this is still true now, but I certainly remember, I think when Paul Ryan was speaker of the House, I remember the average age of the House Republican conference was significantly younger than that of Democrats. And they would highlight that. They would say, “Look, we are electing a new generation of leaders and look at these aging Democrats over here.” And that might still be true, but I certainly remember that that was something that they tried to capitalize on, oh-so-long ago.
Rovner: As we talked about last week, there are now a lot of those not-so-young Republicans, but not really old, who are just getting out because it is no fun anymore to be in Congress. Which is a good segue because … oh, go ahead.
Knight: Oh, I was just saying one thing Republicans do do in the House, at least they do have term limits on the chairmanships to ensure people do not hold onto those leadership positions forever. And Democrats do not have that. That’s at least in the House.
Rovner: But then you get the expertise walking out the door. It’s a double-edged sword.
Knight: Which is, not all the ones that are leaving have reached their term limits, which is the interesting thing actually. But yes, that expertise can walk out the door.
Rovner: Well, speaking of Congress, here in Washington, as I mentioned at the top, Congress is in recess, but when they come back, they will have I believe it is three days before the first raft of temporary spending bills expire. Victoria, is this the time that the government’s going to actually shut down, or are we looking at yet another round of short-term continuing resolutions? And at some point automatic cuts kick in, right?
Knight: Yeah, the eternal question that we’ve had all of this Congress, I think both sides do not want to shut down. I saw some reporting this morning that was saying [Senate Majority Leader] Chuck Schumer is talking to [House Speaker] Mike Johnson, but he also, Schumer did not want to commit to a CR [continuing resolution] yet either. So it’s possible, but we said that every time and they’ve pulled it off. I think they just know a shutdown is so, not even maybe necessarily politically toxic, but potentially —because I don’t know how much the public understands what that means …
Rovner: Because they don’t understand who’s at fault.
Knight: Right. Who’s at fault …
Rovner: … when it does shut down. They just know that the Social Security office is closed.
Knight: Right, but I just know they know it’s dysfunctional or it just can make things messy when that happens; it’s harder for agencies and things like that. So we’ll see. So the deadline is next Friday for the first set of bills. It’s just four bills then, and then the next deadline is March 8 for the other eight bills. There’s some talk that we may see a package over the weekend, but it’s Mike Johnson’s deciding moment. Again, he’s getting pressure from the House Freedom Caucus to push for either spending cuts or policy riders that include anti-abortion riders, anti-gender-affirming care, a lot. There’s a whole list of things that they sent yesterday they want in bills, and so he’s going to have to …
Rovner: Culture wars is the shorthand for a lot of those.
Knight: Yes, exactly. And so House Freedom Caucus sent a letter yesterday, and so Mike Johnson’s going to have to decide does he want to acquiesce to any House Freedom Caucus demands or does he want to work? But if he doesn’t want to do that, then he’s going to have to pass any funding bills with Democratic votes because he does not have enough votes with the Republicans alone, if Freedom Caucus people and people aligned in that direction don’t vote for any funding bills. If he does that, if he works with Democrats, then there is talk that they might file a motion to vacate him out of the speakership. So it’s the same problem that Kevin McCarthy had. The one thing going for Johnson is that he doesn’t have the baggage that Kevin McCarthy had, a lot of political baggage. A lot of people had ill will towards him, just built up over the years. Johnson doesn’t seem to have that as much, and also Republicans, do they want to be leadership-less again?
Rovner: Because that worked so well the first two times.
Knight: Right, so he has got to decide again who he wants to work with. And it doesn’t seem like we know yet how that’s going to go, and that will determine whether the government shuts down or not.
Rovner: But somebody also reminded me that on April 1, if they haven’t done full-year funding, that automatic cuts kick in. I had forgotten that. So I mean, they can’t just keep rolling these deadlines indefinitely. This presumably is the last time they can roll a deadline without having other ramifications.
Knight: Absolutely. And Freedom Caucus, actually, I think that’s partly why they don’t want to agree to something, because they want the 1% cuts across the board. So that was part of the deal made last year under Kevin McCarthy was, if they don’t come up with full funding bills by April 1, there will be a 1% cut put into place. And so the more hard-liners [are] like, “Great, we’re going to cut funding, so we want to do that.” And then Democrats don’t want that to happen. And so yeah, it’s the last time that they can potentially do a CR before that.
Rovner: Yeah, just a reminder, for those who are not keeping track, that April 1 is six months, halfway through the fiscal year for them to have not finished the fiscal year spending bills.
Knight: And one more note is that usually they’re starting on this coming year spending bills by this point in Congress. So we’re still working on FY24 bills. We should be working on FY25 bills already. So they’re already behind. It’s dysfunctional.
Rovner: I think it’s fair to say the congressional budget process has completely broken down. Well, moving on to “This Week in Medical Misinformation,” we have a case of doing well by doing no good. Lauren, tell us about your story looking into the profits that accrued to anti-vaccine and anti-science groups during the pandemic.
Weber: So I took a look at a bunch of tax records, and what I found is that four major nonprofits that rose to prominence during the covid pandemic by capitalizing on the spread of misinformation collectively gained more than $118 billion from 2020 to 2022. And were able to deploy that money to gain influence in statehouses, courtrooms, and communities across the country. And it’s a pretty staggering figure to tabulate all together. And what was particularly interesting is there was four of these different groups that I was directed to look at by experts in the field, and one of them includes Children’s Health Defense, which was founded by Robert F. Kennedy Jr., and they received, in 2022, $23.5 million in contributions, grants, and other revenue. That was eight times what they got before the pandemic. And that kind of story was reflected in these other groups as well. And it just shows that the fair amount of money that they were able to collect during this time as they were promoting content and other things.
Rovner: Yeah, I mean literally misinformation pays. While we’re on this subject, I would also note that this week there’s a huge multinational study of 99 million people vaccinated against covid that confirmed previous studies showing an association between being vaccinated and developing some rare complications. But a number of stories, at least I thought, overstated the risks of the study that it actually identified. Most failed to include the context that almost every vaccine has the possibility of causing adverse reactions in some very small number of people. The question of course, when you’re evaluating vaccines, is if the benefit outweighs the benefit of protecting against whatever this disease or condition outweighs the risk of these rare side effects.
I would also point out that this is why the U.S. actually has something called the [National] Vaccine Injury Compensation Program, which helps provide for people, particularly children, who experience rare complications to otherwise mandatory vaccines. Anyway, that is the end of my rant. I was just frustrated by the idea that yes, yes, we know vaccines sometimes have side effects. That’s the nature of vaccines. That’s one of the reasons we study them.
All right, anyway, that is the news for this week. Now it is time for our extra-credit segment. That’s when we each recommend a story we read this week we think you should read, too. As always, don’t worry if you miss it. We will post the links on the podcast page at kffhealthnews.org and in our show notes on your phone or other mobile device. Victoria, why don’t you go first this week?
Knight: So my extra credit this week is a story in ProPublica called “The Year After a Denied Abortion.” It’s by [photographer] Stacy Kranitz and [reporter] Kavitha Surana. And it was a very moving photo essay and story about a woman who was denied an abortion in Tennessee literally weeks to a month after Roe v. Wade was overturned in June 2022, and this was in July 2022. She got pregnant and was denied an abortion. And so it followed her through the next year of her life after that happened. And in Tennessee, it’s one of the strictest abortion bans in the nation. Abortion is banned and there are very rare exceptions. And so this woman, Mayron Michelle Hollis, she already had some children that had been taken out of her care by the state, and so she was already fighting custody battles and then got pregnant. And Tennessee is also a state that doesn’t have a very robust safety-net system, so it follows her as she has a baby that’s born prematurely, has a lot of health issues, doesn’t have a lot of state programs to help her.
She was afraid to go through unemployment because she had had issues with that before. The paperwork situation’s really tough. There’s just so much stress involved also with the situation. She eventually ends up kind of relapsing, starting drinking too much alcohol, and she ends up in jail at the end of the story. And so it just talks about how if there is not a robust safety net in a state, if you’re kind of forced to have a pregnancy that you maybe are not able to take care of, it can be really tough financially and psychologically and tough for the mother and the child. So it was a really moving story and there were photos following her through that year.
Rovner: Lauren.
Weber: I wanted to shout out my colleague who I actually sit next to, David Ovalle, who is wonderful at The Washington Post. He wrote an article called “They Take Kratom to Ease Pain or Anxiety. Sometimes, Death Follows.” And, as our addiction reporter for the Post, he did a horribly depressing but wonderful job actually calculating how many kratom deaths or deaths associated with kratom have happened in recent years. And what he found through requests is that at least 4,100 deaths in 44 states and D.C. were linked to kratom between 2020 and 2022, which is public service journalism at its best. I mean, I think people are clear that there is more risks with this, but I think that it’s emerging actually how those risks are. And he catalogs through the hard numbers, which is often what it requires for folks to pay attention, that this is something that is interactive with other medications which is causing death, in some cases, on death certificates. So pretty moving story, he talked to a lot of the families of folks that have died and it really makes you wonder about the state of regulation around kratom.
Rovner: Yeah, and then, I mean, all food diet supplements that are basically unregulated by the FDA because Congress determined in the 1990s that they should be unregulated because the supplement industry lobbied them very heavily and we will talk about that at some other time. Rachana.
Pradhan: My extra credit is a story in Politico by Megan Messerly. It’s titled “Red States Hopeful for a 2nd Trump Term Prepare to Curtail Medicaid.” The short version is work requirements are in, again. There was an effort previously that Republicans wanted to impose employment as a condition of receiving Medicaid benefits, and then they were very quickly, a couple of states, were sued. Only one program really got off the ground, Arkansas. And what happened as a result is because of the paperwork burdens and other things, thousands of people lost coverage. So currently the Biden administration, of course, is not OK at all with tying any type of work, volunteer service, you name it, to Medicaid benefits. But I think Republicans would be — the story talks about how Republicans would be eager to go and pursue that policy push again and curtail enrollment as a result of that.
So I thought that was, it’s an interesting political story. One thing it did make me wonder though, just as an aside is, there’s also been discussion on the flip side, the states in the story, which focus on South Dakota and Louisiana, states that many of them have already expanded coverage to cover the ACA [Affordable Care Act] population, but there are also still states that have not expanded Medicaid under the ACA’s income thresholds. And those conservative states might find it slightly more palatable to do so if you allow them to impose these types of conditions on the program. And so I think we will see what happens.
Rovner: Although, as we talked about not too long ago, Georgia, one of the states that has not expanded Medicaid under the Affordable Care Act now has a work requirement for Medicaid. And they’ve gotten something in the neighborhood, I believe, of like 2,700 people who’ve signed up out of a potential 100,000 people who could be covered if they actually expanded Medicaid. So another space that we will watch.
Well, my extra credit this week is from Stat News and, warning, it’s super nerdy. It’s called “New CMS Rules Will Throttle Access Researchers Need to Medicare, Medicaid Data.” It’s by Rachel Werner, who’s a physician researcher at the University of Pennsylvania, and it’s about a change recently announced by the Centers for Medicare & Medicaid Services that will make it more difficult and more expensive for researchers to work with the program’s data, of which there is a lot. Since the new policy was announced earlier this month, according to CMS, in response to an increase in data breaches, I’ve heard from a lot of researchers who are worried that critical research won’t get done and that new researchers won’t get trained if these changes are implemented because only certain people will have access to the data because you’ll have to pay every time somebody else gets access to the data. Again, it’s an incredibly nerdy issue, but also really important. So the department is taking comment on this and we’ll see if they actually follow through.
OK, that is our show. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left us a review; that helps other people find us, too. Special thanks as always to our technical guru, Francis Ying, and our editor, Emmarie Huetteman. As always, you can email us your comments or questions. We’re at whatthehealth@kff.org, or you can still find me at X, @jrovner. Rachana, where are you?
Pradhan: Still on X, hanging on, @rachanadpradhan.
Rovner: Victoria.
Knight: I’m also on X @victoriaregisk.
Rovner: Lauren?
Weber: Still on X @LaurenWeberHP.
Rovner: I think people have come sort of slithering back. We will be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 8 months ago
Aging, Courts, Elections, Health Industry, Medicaid, Medicare, Multimedia, Public Health, States, Alabama, Biden Administration, Hospitals, KFF Health News' 'What The Health?', Legislation, Misinformation, Podcasts, Pregnancy, Tennessee, Trump Administration, Women's Health
KFF Health News' 'What the Health?': Biden Wins Early Court Test for Medicare Drug Negotiations
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
A federal judge in Texas has turned back the first challenge to the nascent Medicare prescription-drug negotiation program. But the case turned on a technicality, and drugmakers have many more lawsuits in the pipeline.
Meanwhile, Congress is approaching yet another funding deadline, and doctors hope the next funding bill will cancel the Medicare pay cut that took effect in January.
This week’s panelists are Julie Rovner of KFF Health News, Alice Miranda Ollstein of Politico, Rachel Cohrs of Stat, and Lauren Weber of The Washington Post.
Panelists
Alice Miranda Ollstein
Politico
Rachel Cohrs
Stat News
Lauren Weber
The Washington Post
Among the takeaways from this week’s episode:
- Rep. Cathy McMorris Rodgers (R-Wash.), chair of the powerful House Energy and Commerce Committee, announced she would retire at the end of the congressional session, setting off a scramble to chair a panel with significant oversight of Medicare, Medicaid, and the U.S. Public Health Service. McMorris Rodgers is one of several Republicans with significant health expertise to announce their departures.
- As Congress’ next spending bill deadline approaches, lobbyists for hospitals are feverishly trying to prevent a Medicare provision on “site-neutral” payments from being attached.
- In abortion news, anti-abortion groups are joining the call for states to better outline when life and health exceptions to abortion bans can be legally permissible.
- Senate Finance Chairman Ron Wyden (D-Ore.) is asking the Federal Trade Commission and the Securities and Exchange Commission to investigate a company that collected location data from patients at 600 Planned Parenthood sites and sold it to anti-abortion groups.
- And in “This Week in Health Misinformation”: Lawmakers in Wyoming and Montana float bills to let people avoid getting blood transfusions from donors who have been vaccinated against covid-19.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: Stateline’s “Government Can Erase Your Medical Debt for Pennies on the Dollar — And Some Are,” by Anna Claire Vollers.
Alice Miranda Ollstein: Politico’s “‘There Was a Lot of Anxiety’: Florida’s Immigration Crackdown Is Causing Patients to Skip Care,” by Arek Sarkissian.
Rachel Cohrs: Stat’s “FTC Doubles Down in Welsh Carson Anesthesia Case to Limit Private Equity’s Physician Buyouts,” by Bob Herman. And Modern Healthcare’s “Private Equity Medicare Advantage Investment Slumps: Report,” by Nona Tepper.
Lauren Weber: The Wall Street Journal’s “Climate Change Has Hit Home Insurance. Is Health Insurance Next?” by Yusuf Khan.
Also mentioned on this week’s podcast:
- The Washington Post’s “U.S. Investigates Alleged Medicare Fraud Scheme Estimated at $2 Billion,” by Dan Diamond, Lauren Weber, and Dan Keating.
- Super Bowl ads from Pfizer, Power to the Patients, and the American Values 2024 super PAC.
- KFF Health News’ “Rapper Fat Joe Says No One Is Making Sure Hospitals Post Their Prices,” by Julie Appleby.
click to open the transcript
Transcript: Biden Wins Early Court Test for Medicare Drug Negotiations
KFF Health News’ ‘What the Health?’Episode Title: Biden Wins Early Court Test for Medicare Drug NegotiationsEpisode Number: 334Published: Feb. 15, 2024
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello, and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News, and I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, Feb. 15, at 10 a.m. As always, news happens fast, and things might have changed by the time you hear this. So here we go.
We are joined today via video conference by Alice Miranda Ollstein of Politico.
Alice Miranda Ollstein: Good morning.
Rovner: Lauren Weber of The Washington Post.
Lauren Weber: Hello, hello.
Rovner: And Rachel Cohrs of Stat News.
Rachel Cohrs: Hi everyone.
Rovner: No interview this week, but we do have a special Valentine’s Day surprise. But first, the news. We’re going to start this week in federal district court, where the drug industry has lost its first legal challenge to the Biden administration’s Medicare drug price negotiation program, although on a technicality. Rachel, which case was this, and now what happens?
Cohrs: This was the capital “P” PhRMA trade association. And this case was a little bit of a stretch, anyways, because they were trying to find some way to get a judge in Texas to hear it. Because the broader strategy is for companies and trade groups to spread out across the country and try to get conflicting decisions from these lower courts.
Rovner: Which would force the Supreme Court to take it?
Cohrs: Exactly, yes. Or make it more likely. So PhRMA, in this case, they had recruited, there’s a national group that represents infusion centers and that was headquartered in Texas. The judge ultimately ended up ruling that this association didn’t follow the right procedure to qualify for judicial review and threw them off the case. And then they were like, well, if you throw them off the case, then there’s nobody in Texas, you can’t hear this here. So that was the ultimate decision there, but this could come back up. It was dismissed without prejudice. So this isn’t the end of the road for this lawsuit.
And it’s important to keep in mind that this wasn’t a ruling on any of the substance of the arguments. And trade groups generally are going to have less of an argument for standing, or it’s going to be a harder argument than the companies themselves that actually have drugs up for negotiation.
Rovner: And they’re suing too, the drug companies?
Cohrs: They are suing too. Yeah, just for everybody to keep on your calendars, there’s a judge in New Jersey who is hoping to have a quadruple oral argument on four of these cases, so stay tuned. That could be coming early next month. But these are very much moving. I think we are going to get insight on some of these arguments pretty soon, but this case is not quite that test case yet.
Rovner: All right, well, we’ll get to it eventually. Well, moving on to Capitol Hill. When we were taping last week, Sen. Bernie Sanders was holding his much-publicized hearing to grill drug company CEOs about their too-high prices. Rachel, you were there. Did anything significant happen?
Cohrs: I think it was kind of expected. I don’t think we were trying to find any innovative legislative solutions here. Honestly, it seemed, just from a candid take, that a lot of these lawmakers were not very well-prepared for questioning. There were a couple of notable exceptions, but we didn’t learn a whole lot new about why drug prices are high in the United States, how our system works differently from other countries.
I did find some useful nuggets in the CEO’s testimony about how low the net prices are for some of their medications, that they’re already offering a 70% discount, a 90% discount, which to me just kind of put into perspective some of the discounts we could be hearing in the Medicare negotiation program. That oh, even if it’s a 90% discount, that might not even be different from what they’re paying now. So just interesting to file a way for the future, but I think it was mostly a non-event for the CEOs who, for some reason, had to, under the threat of subpoena, come make these arguments. So it seemed like much ado about not a whole lot of substance.
Rovner: That was sort of my theory going in, but you always have to watch just in case. Well, also on Capitol Hill, the chairman of the powerful House Energy and Commerce Committee announced she will retire at the end of the Congress. Cathy McMorris Rodgers, who’s a Republican from Washington, was in her first term as chair of the committee that oversees parts of Medicare, all of Medicaid, as well as the entire U.S. Public Health Service.
I imagine this is going to set off a good bit of jockeying to take her place. And why would somebody step down early from such a powerful position? Do we have any idea?
Cohrs: Have you seen …? Oh, go ahead.
Ollstein: Facing Congress is what you say? Yes. This is part of a wave of retirements we’ve been seeing recently, including from some other committee chairs who could have theoretically continued to be powerful committee chairs for several years to come. People are taking this as part of the bad sign for Republicans. Either a sign that they don’t believe they’re going to hold the majority after this November’s election, or they’re just so fed up with the struggles they’ve had governing over the last few years and the inability to get anything done. And people are thinking, well, maybe I can get something done in a different role, not in Congress, because certainly, we’re not doing too much here to be proud of.
Rovner: Yeah, I feel like Cathy McMorris Rodgers is kind of this poster child for a very conservative Republican who’s not the far-right-wing MAGA type, who actually wants to do legislation. She just wants to do Republican legislation, and that seems to be getting harder in the House.
Ollstein: Right, right. And there’s a concern that, particularly on the right within Republicans, that we’re losing a health policy brain trust. We’re losing the people that have been really integral to a lot of the nitty-gritty policy work over the years, and they’re not being replaced with people who have that interest. They’re being replaced with people who are more focused on culture wars and other things. And so there’s concern in the future about the ability to cobble together things like Medicare reimbursement rates, or these technical things that aren’t really part of the culture wars.
Rovner: Yeah, I think we mentioned at some point that Mike Burgess is also retiring, also high up on the Energy and Commerce Committee. And he’s a doctor who’s really had his hands into some of this really nerdy stuff, like on Medicare physician reimbursement. And that will be obviously just a big loss of institutional memory there.
Cohrs: For the future of the committee, I know congressman Brett Guthrie has kind of thrown his hat in the ring to succeed her. Unclear who exactly is going to win this race, but he is the chairman of the health subcommittee, does bring some health expertise. So the E&C committee deals with a lot of different priorities, but if he were to succeed her, then I think we would see, at least at the top of the committee, some of the expertise remain.
Rovner: Well, meanwhile, in all of this jockeying, the next round of temporary government funding bills expires on March 1 and March 8, respectively, which is getting pretty close. And that brings back efforts to cancel the 3.4% pay cut that doctors got for Medicare patients in January. Where are we on funding, and are any of these health issues that people are out lobbying on going to make it into this next round? Is there going to be a next round?
Cohrs: Yeah, we don’t know if there’s going to be a next round, I don’t think. But at least the sources I’ve talked to have said that a full cancellation of the 3.4% cut for Medicare or payments to doctors is off the table at this point. They are hoping to do some sort of partial relief. They haven’t decided on percentages for that yet. And it’s unclear how much money will be available from pay-fors. It is still very much squishy, not finalized, two, three weeks out from the deadline, but I think …
Rovner: Two weeks.
Cohrs: There is some agreement on some relief, which has not been the case thus far for doctors. So I think that’s a positive sign.
Ollstein: Yeah. Overall, the chatter is about the need for yet another CR [continuing resolution] because the work is not getting done in time to meet these deadlines. That seems to be where we’re headed. Obviously, that will piss off a lot of members on the right who don’t want another CR, who didn’t want the last couple CRs. And so once again, we are staring down a possible shutdown.
Rovner: And I had forgotten, somebody reminded me, that even if they get another temporary funding bill, starting in April, there are automatic cuts if they’re not finished with this year’s funding bills. Which, I don’t know, is there any indication that they’re going to be finished with them by April either? I have not seen a lot of progress here. They’ve been fighting over other things, which is fine to fight over other things, but I’m not noticing a lot happening on the spending bills.
I’m seeing a lot of shaking heads. I guess nobody else is noticing either. Well, we will obviously keep watching that space because next week, we will only be one week away.
Well, another Medicare policy that supporters are hoping to get into one or another of these spending bills is creating something called more site-neutral payments in Medicare. Currently, Medicare pays hospitals and hospital outpatient departments, and sometimes even hospital-owned physician practices, more than it pays non-hospital affiliated providers for the exact same service.
The theory is that hospitals need higher payments because they have higher fixed costs, like keeping emergency rooms open 24/7. But it costs Medicare many billions of taxpayer dollars for this differential in payments. And this has become quite the lobbying frenzy for the hospital industry, yes?
Cohrs: Yes. I think it’s something that they can all get on board with hating, and I think they view it similarly to the drug pricing debate as a slippery slope. The policy Congress really is looking at now is a $3 billion, very small slice of all the services that could potentially be subjected to site-neutral payments. But the whole pie here is $150 billion potentially for Medicare.
We’re talking hundreds of billions of dollars for commercial payments. So I think they are really pushing to get to lawmakers, especially, from what I’ve talked to Senate Republicans, they are just not on board with it, they’re worried about the rural hospitals. And if they can connect to those things, which they have been successful in doing so far, they’re just not going to get very far.
I mean, if you look at the Senate Finance Committee, you have Mike Crapo from Idaho, Republican leadership. You have [John] Barrasso from Wyoming. There’s really just so many rural states that even Chuck Grassley, who is a moderate on a lot of health policy issues, talked about his rural hospitals in Iowa as soon as I asked him about this. So they’re not there yet right now, but I think hospitals are trying to keep it that way.
Rovner: And it was ever thus that the Senate is much more rural-focused than the House because pretty much every single senator has at least part of a rural area that they represent. Lauren, you wanted to add something?
Weber: Yeah, I just wanted to say, I always find it funny when rural hospitals come up as a cudgel by the big hospital associations, who don’t seem to look out for them the vast majority of the time when they’re closing. But as you pointed out, the Senate is much more rural-focused. So I do agree with all of you all, that I question whether or not this will have much ground to gain.
Rovner: Yeah. And the other thing that I keep wanting to point out is that there’s all this talk on Capitol Hill among Republicans of cutting the spending bills, the appropriations, and we’re going to balance the budget. Well, there’s just not enough money in the appropriation bills to do anything to the deficit. The money is in things like Medicare. I mean, that’s where, if you really want to make a dent in the deficit, you’re going to do it. And, as we’re seeing with this particular fight, every time they want to do something that’s going to save money, it’s going to hurt somebody. And I mean, there are obviously legitimate concerns about rural hospitals that are in trouble, particularly in states that haven’t expanded Medicaid, but that’s one of the reasons. It’s not so much the spending bills that make it hard to do anything about the deficit. It’s fights like these.
Meanwhile, for better or worse, another reason that Medicare costs so much is that it’s subject to a lot of fraud. Lauren, I have seen a lot of Medicare fraud stories over the years, but you’ve got one that was discovered in a pretty novel way. So tell us about it.
Weber: Yeah, my colleagues Dan Diamond, Dan Keating, and I found out early last week — we got a tip from the National Association of ACOs [Accountable Care Organizations] saying that they had seen this massive spike in catheter billing. When we did some digging into the companies they had identified — and to be clear, that spike of catheter billing was worth an alleged $2 billion in billings to Medicare. So when we talk about site-neutral payments, that’s almost what you would get for site-neutral payments: the $2 billion in Medicare fraud, but regardless.
So my colleagues and I dug in. So Dan, Dan, and I called around, and we found links between the seven companies that were charging Medicare for catheters that folks never received. I want to point out, I spoke to this lovely woman in Ponta Vedra Beach, Florida. She’s 74, Aileen Hatcher, who spotted this diligently going through her Medicare form, but as she said, she went to her — literally, these are her words — she’s like, “I went to my old lady luncheon and told them all this was on my Medicare statement.” And they said, “Oh, we don’t read those because we don’t pay Medicare the money. So we don’t read the explanation of benefits to see what we’ve been charged.”
And, unfortunately, I think that is what happens a lot of times with Medicare fraud. It goes unnoticed because folks aren’t the ones paying the dollars. But the bottom line is this was so large and so many people called into Medicare that Dan and I discovered that there is an ongoing federal investigation. Three of the companies, former owners that I called, confirmed to me that FBI had interviewed them or was talking to them about these folks that had taken over the companies and started charging Medicare this much money. And Dan also got some sources on that front as well.
So, I mean, it’s a pretty massive Medicare fraud scheme. I’ll give a call-out here. If anyone here has been affected by catheter and Medicare fraud, please give me an email. We’d love to hear more. I think it speaks to the fact that Medicare fraud — we all know this because we cover this — Medicare fraud is as old as time. It continues to happen, especially durable medical equipment Medicare fraud. But this is so much money. And it is wild that even though we talked to so many people that called Medicare over and over and over again, these folks were able to get away with billing for a very long time.
Rovner: What I found really fascinating about the story, though, is that it was the doctors in the ACOs that spotted it because — we’ve talked about these accountable care organizations — they’re accountable for how much it costs to take care of their patients.
The patients aren’t paying for it, as they point out, but these doctors, it’s coming right out of their bonuses and what they’re charged and how much they get for Medicare. So there’s finally somebody with a real incentive to spot this kind of fraud, because, basically, it was taking money from them. Right?
Weber: That’s exactly right. I think that’s why they were so hot to have some movement on this because, as they pointed out, they could lose millions of dollars in bonuses for better taking care of their patients.
It’s wild that it gets to this point. Like I said, we had all these people that called in to Medicare and many fraud lawyers we talked to said, “Look, why aren’t the NPIs [National Provider Identifiers] turned off?” Great question.
Rovner: Yeah. Anyway, I was fascinated by this story, and as I told Lauren earlier, I’m not a big fan of Medicare fraud stories just because there are so many of them. But this one is like, oh, maybe we finally have somebody … the ACOs can become bounty hunters for Medicare fraud, which would not be a bad thing.
All right, well, moving on to abortion this week, we have spent a lot of time talking about how doctors who perform abortions and patients who need them in emergencies have been trying to get state officials to spell out when the exceptions to state bans apply. Well, now it seems that it’s the other side looking for clarification.
Stat News reports that several anti-abortion groups have joined doctors and patients in urging the Texas Medical Board to spell out which conditions would qualify for the exception to the ban, and not subject doctors who guess wrong to potential prison terms and loss of their medical licenses.
Meanwhile, legislation moving through the House in South Dakota, endorsed by multiple anti-abortion groups, would require the state to make a video explaining how its ban works and under what circumstances. Alice, what’s going on here?
Ollstein: I think it’s this interesting confluence and it’s an interesting development because, at first, anti-abortion groups were insisting that the laws were perfectly clear. And that doctors were either willfully or mistakenly misinterpreting them. As more and more stories came forward of women being turned away while experiencing a medical emergency and suffering harm as a result, a lot of those women are part of lawsuits now.
They were saying the law is fine. In some cases, these anti-abortion groups wrote the laws themselves or advised on them saying, your interpretation is what’s wrong. The law is fine. But I think as so many of these stories are coming out, that’s not proving enough. And now they’re going back and saying, OK, well, maybe there do need to be some clarifications. They don’t want changes. There’s different camps because some people do want changes. Some people say, OK, we need more exceptions. We need more carve-outs to avoid these painful stories. Whereas other anti-abortion forces and elected officials say, no, we don’t need to change the law. We just need to clarify it and explain it. And so I think that’s going to be an ongoing tension.
Rovner: Yeah, I know one of the big themes earlier in this whole fight — I won’t say earlier this year, it was mostly last year — was redefining things as not abortions. That if you’re terminating an ectopic pregnancy, that’s not an abortion. Well, that is an abortion.
Ollstein: Medically, yes.
Rovner: So apparently, the … right. The renaming has not worked so far. So now I guess they’re trying to clarify things. Lauren, you wanted to add something?
Weber: Yeah, I just wanted to say, when you kick things to the medical board, I think people see that as an unbiased unpolitical organization. But medical boards are often appointed by the governor. So, in this case, Gov. [Greg] Abbott. And also take Ohio, for example: I believe that one of their medical board leaders is the head of the right-to-life movement.
I haven’t looked at Texas’. But kicking it to the medical board to make a decision — putting aside the fact that most medical boards are incredibly inadequate at their actual job, which is disciplining doctors, they’re not necessarily known for their competence — is that you also deal with some of the politics involved in this as well.
Rovner: So in South Dakota, it would kick this to the South Dakota Department of Health, which, of course, is controlled by the governor, who’s a Republican and pro-lifer. And so it’s hard to imagine what sort of doing a video explaining this is going to do to clarify things any further than they already think the law has gone. But at least … I’m fascinated by the effort here, that this is going on in multiple states. Speaking of state legislators, in Missouri, they’re working on a bill to create an abortion ban exception for children 12 and under — obviously thinking of the 10-year-old in Ohio in 2022 [who] had to go to Indiana to get a pregnancy terminated. But one Republican state senator complained that “a 1-year-old could get an abortion under this.” This is a serious question: Should legislators have to pass a basic biology test to make laws about reproductive health? As we know, 1-year-olds cannot get pregnant.
Ollstein: I mean, this was a more glaring example. We see this over and over in a lot more subtle ways, too, where doctors and medical societies are pointing out that these laws are drafted using language that is not medically accurate at all. And it can be small things in terms of when someone should qualify for a medical exemption to an abortion ban. Some states have language around if it would cause “irreversible damage.” That’s not a term doctors use in that circumstance, things like that. Or a major bodily function would be impaired if they don’t get an abortion. Well, what is a major bodily function? That’s not defined. And so, yes, this was an almost laughable example of this, but I think that it’s a sign of something more pervasive and maybe less obvious.
Rovner: Yeah, I mean, I have listened to a lot of state debates with a lot of legislators saying things that are, as I say, kind of laughably inaccurate. Sorry, Lauren.
Weber: Oh, I would just say as a Missourian and as someone who lived in Missouri until a year ago, this gentleman, in particular, it does seem like has a history of making somewhat inflammatory statements that he knows will be picked up by the media. I mean, I think he brought a flamethrower to an event. I mean, I think that’s part of the shtick. But welcome to Missouri politics. You never know what you’re going to get.
Ollstein: And of course, we have the famous assertion that people can’t get pregnant as a result of rape because the body knows how to shut it down, which is obviously not …
Rovner: Which happened in a Missouri Senate race.
Ollstein: Yes. Yep. Exactly. So Missouri, once again, covering itself in glory.
Rovner: All right, well, something we haven’t talked about a lot recently are crisis pregnancy centers, which are usually storefronts for anti-abortion organizations that often lure women seeking abortions by offering free pregnancy tests and ultrasounds so that they can then talk them into carrying their pregnancies to term. The centers are getting more and more public support from states. One estimate is that government support totaled some $344 million in fiscal 2022. So that was a couple of years back. And increasingly as abortion clinics close in states with bans, crisis pregnancy centers, which typically don’t have medical professionals on staff and aren’t technically medical facilities, may be the only resource available to pregnant women. It seems that could have some pretty serious ramifications. Yes?
Ollstein: I mean, I think people don’t realize just how vast the network of these centers are. They outnumber abortion clinics by a lot in a lot of states, including states that support abortion rights. They’re very, very pervasive. And this is becoming a huge focus for the anti-abortion movement. It was basically the theme of this year’s March for Life, was these sort of resources. In part, it is an attempt to show a kinder face of the movement and change public opinion. Obviously, like we discussed, there are all these painful stories coming out about people being denied care. And so promoting these stories of places that provide some form of something, some services, it’s not necessarily medical care, but …
Rovner: They provide diapers and strollers and car seats. I mean, they do actually … many of them actually provide services for babies once they’re born.
Ollstein: Right. Right, right, right. And so I think there is going to be a huge focus on this in the policy space, both in terms of directing more taxpayer funding to these centers, which progressives vehemently oppose.
And so I think this is going to be a big focus going forward. It already has in Texas. Texas has directed a lot of money towards what they call alternatives to abortion, which include these centers. And so I think it’s going to be a big focus going forward.
Rovner: Well, one other thing about crisis pregnancy centers, because they are not medical facilities, they are not subject to HIPAA medical privacy rules. And it turns out that is important. According to an investigation by Senate Finance Committee Chairman Ron Wyden, a company gathered and sold location data for people whose phones were in or around 600 separate Planned Parenthood locations, without the patients’ consent, to use an anti-abortion advertising.
Wyden is asking the SEC and the FTC to investigate the company, but this raises broader questions about information privacy, particularly in the reproductive health space. I remember right after Roe v. Wade was overturned, there were lots of warnings to women who were using period-tracking apps and other things about the concern about people who you may not want to know your private medical situation being able to find out your private medical situations. Is there any indication that there’s any way from the federal government point of view to crack down on this?
Ollstein: So I don’t know about that specifically, but there is a bigger effort on privacy and digital privacy and how it relates to abortion. We’re still waiting on the release of the final HIPAA rule from the Biden administration, which will extend more protections around abortion data, I think. But, because it’s HIPAA, it does only apply to certain entities and these centers are not among them. Another area I’ve been hearing concern about is research. A researcher at a university who is studying people who have abortions or don’t have abortions, their data is not protected. And so they are very stressed out about that, and that’s compromising medical research right now. So there’s a lot of these different areas of concern. And as we so often see, technology evolves a hell of a lot faster than government evolves to regulate it and address it. And that is just an ongoing concern.
Rovner: Yes, it is. And at some point, we’ll talk about artificial intelligence, but not today. Actually, right now, I want to turn to the Super Bowl. Yes, the Super Bowl. In between all the ads for blockbuster movies, beer, cars, and snack foods, and, right, a football game, there were three ads aimed directly at health policy issues.
In one, the nonprofit price transparency advocacy group Power to the Patients got musicians Jelly Roll, Lainey Wilson, and Valerie June to basically call hospitals and insurance companies greedy. It’s not clear to me if this was a free PSA or if this group paid for it, but I suspect the latter.
Does anybody know who this group is? They seem to have lots of access to big names for what seems to be a kind of obscure health issue. I mean, everybody’s for transparency, but I don’t think I’ve ever seen a Super Bowl ad about it.
Cohrs: This is not their first Super Bowl. It’s backed by Cynthia Fisher who is married to the CEO of Sam Adams, parent company. And he’s also a member of the Koch family. But she has been passionate about health care price transparency for years. I mean, was in President [Donald] Trump’s ear, has made the legal argument that the authority existed under the Affordable Care Act. Lobbied to get these regulations passed. And she has definitely employed unusual or unorthodox techniques, like Super Bowl ads, like painting murals, like hosting parties and concerts for health staff and health policy people in D.C. And I think she’s also lobbying for the codification of these transparency regulations.
And it is a little wonky, but I think her frustration is that she lobbied so hard to get these price transparency regulations and everyday people don’t even know that it should be available for them. And obviously academics disagree over how useful that information is for everyday people. But I think she has just taken it upon herself to do the PR campaign for these regulations that she believes could help people make more educated decisions about care that isn’t necessarily emergency care, like MRIs, that kind of thing. So she’s been around for years and has been very active.
I think Fat Joe is another celebrity that she’s brought onto the case. Jelly Roll — I hadn’t seen him do an event with her before or an ad. But I think there’s an ever-expanding cast of celebrities where this is just … it seems like a pretty noncontroversial issue. So I mean, Busta Rhymes, like French Montana, there’s been a lot of people involved in this campaign and I expect it to be ongoing.
Rovner: I feel like she’s kind of the Mark Cuban of price transparency, where Mark Cuban is all into drug prices. Alice, you want to add something?
Ollstein: Well, it’s just funny to me because, as we’ve discussed many, many times on this podcast, transparency goes not very far in helping actual patients. And so it’s funny that a group called Power to the Patients is going all in on this issue when, as we know, the vast majority of health care people need they cannot shop around for and, even when they can, it’s not something people are always able or willing to do.
And so transparency gets a lot of bipartisan support and sounds good in theory, but we’ve seen in terms of what’s been implemented so far in terms of hospital prices, et cetera, that it doesn’t do that much to bring down prices or empower people.
Rovner: Although, I don’t know, getting famous people to care about health policy can’t be a terrible thing. Lauren, did you want to add something too?
Weber: No, I just wanted to say, I mean, I will say as much as we’re all clear on price transparency, what this all means, the Super Bowl is a new audience. So, I mean, if you’re going to spend your money, at least you’re spending it — and that was the most watched TV program, I believe, of all time — so you’re spending it in a way that you’re getting some eyeballs on it.
Rovner: All right, well, that was not the only ad. Next, a company that clearly did pay for its ad was Pfizer, which used a soundtrack by Queen and talking paintings and statues to celebrate science and declare war on cancer. This is also one I don’t think I had seen before. I mean, what is Pfizer up to here? I mean, obviously, Pfizer can afford a Super Bowl ad. There’s no question about that, but why would they want to?
Cohrs: I mean, Pfizer has not been performing great financially lately. And I think they pulled out of the lobbying organization biome and chose to spend money on a Super Bowl ad, which I think is a really interesting choice. I mean, I don’t know what the dues are, but a Super Bowl ad is an expensive thing.
And I think there has been this attack on science, as a whole, and I think there’s an outstanding question of how to rebuild trust. And I think that this was Pfizer’s unorthodox tactic of trying to equate themselves with more credible, historical scientists who are less controversial. Yeah, my colleague did a good story on it.
Rovner: Yeah, like Einstein.
Cohrs: Right.
Rovner: Well, we’ll link to all of these ads. If you haven’t seen them there, they’re definitely worth watching. Well, finally, and in keeping with the occasional politics that does creep into Super Bowl ads, the super PAC supporting the presidential candidacy of independent anti-vaxxer Robert F. Kennedy Jr. paid $7 million for an ad that was basically a remake of the 1960 ad for his uncle John F. Kennedy, when he was running for president, which provoked an outcry from several of his Kennedy cousins who have repeatedly disavowed RFK Jr.’s candidacy and his causes.
For his part, the candidate apologized to his family members and said he didn’t have anything to do with the ad directly, because it was the super PAC. But then he pinned it to his Twitter profile, where he has more than 2½ followers. I can’t help but wonder if they’re going after football fans who actually believe the whole Taylor Swift-Travis Kelsey thing is a conspiracy.
No comment on Robert F. Kennedy Jr. and pissing off his entire family? We will move ahead then.
Speaking of conspiracy theories, in “This Week in Health Misinformation,” we have — drum roll — blood transfusions. Seems that there are a significant number of people who believe that getting blood from someone who has been vaccinated against covid, using the mRNA vaccines, will somehow change their DNA or otherwise harm them. And state legislators are listening.
In Wyoming, a state representative has introduced a bill that would require the labeling of blood from a covid-vaccinated donor. So prospective recipients could refuse it, at least in nonemergency situations. And in Montana, there’s a bill that would go even further, banning blood donations from the covid-vaccinated. That one appears to not be going anywhere, but this could have serious implications. It would create blood shortages, I imagine, even in rural areas where fewer people are vaccinated than in some of the urban areas. But I mean, this strikes me as not an insignificant kind of movement.
Ollstein: Well, it seems troubling on two fronts. One, we already have blood shortages and we already have dangerously low vaccination rates and not just covid vaccination rates. The hesitancy and anti-vax sentiment is spilling over into routine childhood vaccinations and all kinds of things.
And so I think anything that appears to give that sort of stigma and conspiracy a veneer of credibility, like state law for instance, threatens to further entrench those trends.
Rovner: All right, well, that is this week’s news. We will do our extra credits in a minute, but first, as promised, we have the winners of the KFF Health News “Health Policy Valentines” contest. This year’s winner, and we will post the link to the poem and its accompanying illustration, is from Jennifer Reck.
It goes, “Darling, this Valentine’s Day, let’s grab our passports and fly away to someplace where the same drugs cost a fraction of what they do in the States.” I have asked the panel to each choose a finalist of their own to read. So, Lauren, why don’t you start?
Weber: “The paperwork flirts with my affections, a dance of denials, full of rejections. My heart yearns for you, my sweet medication, but insurance insists on prior authorization.”
Rovner: And who’s that from?
Weber: That’s from Sally Nix. Excellent work, Sally.
Rovner: Alice.
Ollstein: OK, I have one from Kara Gavin. It’s “My love for you, darling, is blinding / Like a clinical trial pre-findings / But I fear we shall part / And I’ll lose my heart/ Because of Medicaid unwinding!” Very topical.
Rovner: Very. Rachel.
Cohrs: OK, this is from Andrea Ferguson. “Parental love is beautiful and guess what makes it stronger? A paid parental leave policy to stay with baby longer.”
Rovner: Very nice. Thank you all who entered. And we’ll do this again next year. All right, now it is time for our extra credit segment. That’s when we each recommend a story we read this week we think you should read, too. As always, don’t worry if you miss it. We will post the links on the podcast page at kffhealthnews.org and in our show notes on your phone or other mobile device. Alice, why don’t you go first this week?
Ollstein: I have a piece from my colleague Arek Sarkissian, down in Florida, and it is about how the state’s immigration law is deterring immigrants from seeking health care. And one of the areas they’re most concerned about is maternal health care. We already are in a maternal health crisis and the law requires hospitals that receive Medicaid funding to ask people about their immigration status when they come in for care. What a lot of people don’t know is that they don’t have to answer, but this fear of being asked and potentially being flagged for deportation enforcement, et cetera, is making people avoid care. And so there’s just a lot of concern about this and a lot of attempts to educate folks in the immigrant community. Obviously, Florida has a very large immigrant community. And it just reminded me of the fears that were happening early in the pandemic when the public charge rule under Trump was in effect and it was deterring immigrants from seeking care.
And in the middle of a pandemic, when we’re dealing with an infectious disease that doesn’t care if you have citizenship or not, having a large segment of the population avoid care is dangerous for everyone.
Rovner: Indeed. Lauren.
Weber: So I chose an article titled “Climate Change Has Hit Home Insurance. Is Health Insurance Next?” by Yusuf Khan in The Wall Street Journal. And, I mean, look, the insurers are — they’re looking out for their bottom line. And the bottom line is that climate change does have health impacts. So the question is, will that start to hit premiums? The sad answer, in part of this article, is that, unfortunately, the people often most affected by climate change don’t have health insurance. So that may not affect premiums as much as we expect, but I think this is a really fascinating test case of how when climate change comes for your money, you’ll start to see it validated more. So I’ll be curious to see how this plays out with the various health insurers.
Rovner: Yeah, obviously, we’re already seeing people not being able to get home insurance in places like Florida and California because of increasing fires and increasing hurricanes and increasing flooding in some places. Rachel?
Cohrs: So mine is a package deal. It’s two stories related to private equity investment in health care. The first is a piece in Modern Healthcare by Nona Tepper on a Medicare Advantage report by the Private Equity Stakeholder Project. And it just kind of highlighted the downturn in investment in Medicare Advantage, like marketing companies and brokers, consultants.
And I thought it was an interesting take because, I think so often, we see reporting about how private equity is expanding its investment in a certain sector. But this, I think, was an interesting indicator where, oh, it’s turning downward so dramatically. And I think that it’s interesting to track the tail end of more regulation or whatever rule comes out. How does that impact investment? And we talk a lot about that in the pharmaceutical space. But I thought this was a great interesting creative take on the Medicare Advantage side of things.
And also just highlighting some reporting from my colleague Bob Herman about the FTC doubling down on the Welsh Carson’s anesthesia case to limit private equity’s physician buyouts. So the FTC is taking on Welsh Carson, a powerful private equity firm, and other private equity firms asked for the case to be dismissed. And Bob does a great job breaking down these really complicated arguments by the FTC as to why they’re not backing down. They’re not going to cut a deal, they want this case to go forward.
So it will be interesting to watch as this develops, but I think Bob makes a great argument. There are applications for other cases as well and for the FTC and being able to attack these complex corporate arrangements where they’re using subsidiaries to drive prices up for physician services and other things. So definitely worth a read from Bob.
Rovner: Yes, another theme of the Federal Trade Commission getting more and more involved in health care in general and private equity in health care in particular. My extra credit this week is from Stateline by Anna Claire Vollers, and it’s called “Government Can Erase Your Medical Debt for Pennies on the Dollar — And Some Are.” It’s about how a growing number of states and cities are buying up and forgiving medical debt for their residents. Backers of the plans point out that medical debt is a societal problem that deserves a societal solution. And that relieving people’s debt burdens can actually add to economic growth. So it’s a good return on a small investment. It’s obviously not going to solve the medical debt problem, but it may well buy some government goodwill for some of the people of these states and cities.
All right, that is our show. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left us a review; that helps other people find us, too. Special thanks, as always, to our technical guru, Francis Ying, and to Stephanie Stapleton, filling in this week as our editor. As always, you can email us your comments or questions. We’re at whatthehealth@kff.org, or you can still find me at X, @jrovner, or @julierovner at Bluesky and @julie.rovner at Threads. Lauren, where are you these days?
Weber: Still just on Twitter @LaurenWeberHP, or X, I guess.
Rovner: Alice.
Ollstein: On X @AliceOllstein and on Bluesky @alicemiranda.
Rovner: Rachel.
Cohrs: I’m @rachelcohrs on X and also getting more engaged on LinkedIn lately. So feel free to follow me there.
Rovner: We will be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Stephanie Stapleton
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 8 months ago
Aging, Courts, COVID-19, Health Care Costs, Medicare, Multimedia, Pharmaceuticals, Public Health, States, Abortion, Biden Administration, KFF Health News' 'What The Health?', Podcasts, U.S. Congress, Women's Health
KFF Health News' 'What the Health?': To End School Shootings, Activists Consider a New Culprit: Parents
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
For the first time, a jury has convicted a parent on charges related to their child’s mass-shooting crime: A Michigan mother of a school shooter was found guilty of involuntary manslaughter. What remains unclear is whether this case succeeded because of compelling evidence of negligence by the shooter’s mother or if this could become a new avenue for gun control advocates to pursue.
Meanwhile, a prominent publisher of medical journals has retracted two articles that lower-court judges used in reaching decisions that the abortion pill mifepristone should be restricted. The case is before the Supreme Court, with oral arguments scheduled for March 26.
This week’s panelists are Julie Rovner of KFF Health News, Sarah Karlin-Smith of the Pink Sheet, Alice Miranda Ollstein of Politico, and Rachana Pradhan of KFF Health News.
Panelists
Sarah Karlin-Smith
Pink Sheet
Alice Miranda Ollstein
Politico
Rachana Pradhan
KFF Health News
Among the takeaways from this week’s episode:
- Sage Journals, a major medical publisher, has retracted two studies central to abortion opponents’ arguments in a federal court case over access to the abortion pill mifepristone. Although the retraction came before next month’s Supreme Court hearing on the case, the now-discredited studies have permeated the public debate over mifepristone.
- Florida’s Supreme Court has until April 1 to stop a measure about the availability of abortion from appearing on the November ballot. The decision could be pivotal in determining abortion access in the South, as Florida’s current 15-week ban (compared with near-total bans in surrounding states) has made it a regional destination for abortion care.
- In Medicaid news, the nation is about halfway through the “unwinding,” the redetermination process states are undergoing to strip ineligible beneficiaries from the program’s rolls. Although the process will amount to the biggest purge of the Medicaid and Children’s Health Insurance Program rolls in a one-year period, it is expected that, when all is said and done, overall enrollment will look much as it did before the pandemic — though how many people are left uninsured remains to be seen.
- In the states, Georgia is suing the Biden administration to extend its Medicaid work-requirement program. Meanwhile, some states are using Medicaid funding to address housing issues. Despite evidence that addressing housing insecurity can improve health, it is also clear that state budgets would need to be adjusted to meet those needs.
- And in “This Week in Health Misinformation,” PolitiFact awarded a “Pants on Fire!” rating to the claim — in a fundraising ad for Rep. Matt Rosendale (R-Mont.) — that Anthony Fauci, former director of the National Institute of Allergy and Infectious Diseases, “brought COVID to Montana” a year before it spread through the U.S., among other spurious claims.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: Alabama Daily News’ “Alabama Lawmakers Briefed on New ‘ALL Health’ Insurance Coverage Expansion Plan,” by Alexander Willis.
Alice Miranda Ollstein: Stat’s “FDA Urged to Move Faster to Fix Pulse Oximeters for Darker-Skinned Patients,” by Usha Lee McFarling.
Sarah Karlin-Smith: The Atlantic’s “GoFundMe Is a Health-Care Utility Now,” by Elisabeth Rosenthal.
Rachana Pradhan: North Carolina Health News’ “Atrium Health: A Unit of ‘Local Government’ Like No Other,” by Michelle Crouch and the Charlotte Ledger.
Also mentioned on this week’s podcast:
- Sage Journals’ “Retraction Notice.”
- KFF Health News’ “Halfway Through ‘Unwinding,’ Medicaid Enrollment Is Down About 10 Million,” by Phil Galewitz.
- KFF Health News’ “Congressman Off-Base in Ad Claiming Fauci Shipped Covid to Montana Before the Pandemic,” by Katheryn Houghton.
click to open the transcript
Transcript: To End School Shootings, Activists Consider a New Culprit: Parents
KFF Health News’ ‘What the Health?’Episode Title: To End School Shootings, Activists Consider a New Culprit: ParentsEpisode Number: 333Published: Feb. 8, 2024
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello, and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News, and I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, Feb. 8, at 10 a.m. As always, news happens fast, and things might have changed by the time you hear this, so here we go. Today, we are joined via video conference by Alice Miranda Ollstein of Politico.
Alice Miranda Ollstein: Hello.
Rovner: Sarah Karlin-Smith of the Pink Sheet.
Karlin-Smith: Hi, everybody.
Rovner: And my KFF Health News colleague Rachana Pradhan.
Rachana Pradhan: Hi, Julie.
Rovner: No interview today, so we will get straight to the news. We’re going to start in Michigan this week, where a jury convicted the mother of a teenager, who shot 10 of his high school classmates and killed four of them, of involuntary manslaughter. This is the first time the parent of an underage mass school shooter has been successfully prosecuted. The shooter’s father will be tried separately starting next month. Some gun control advocates say this could open the door to lots more cases like this, but others think this may have been a one-off because prosecutors had particularly strong evidence that both parents should have known that their son was both in mental distress and had easy access to their unlocked gun. Is this possibly a whole new avenue to pursue for the whole “What are we going to do about school shooters?” problem?
Ollstein: I mean, it seems like we’re just in an era where people are just trying various different things. I mean, there was ongoing efforts to try to hold gun manufacturers liable. There were efforts on a lot of different fronts. And the goal is to prevent more shootings in the future and prevent more deaths. And so, I think the goal here is to impress upon other parents to be more responsible in terms of weapon storage and also in terms of being aware of their child’s distress.
So, whether or not that happens, I think, remains to be seen, but these shootings have just gone on and on and on and not slowed down. And so, I think there’s just a desperation to try different solutions.
Rovner: Yeah. Apparently in other states they’re starting to look at this, but I guess we talk so much about the chilling effect. That’s actually what they’re going for here, right? As you say, to try and get parents to at least be more careful if they have guns in the house of how they’re storing them, and who has access to them.
Well, we will turn to abortion now. As we noted last week, the Supreme Court will hear the case challenging the FDA’s approval of the abortion drug mifepristone on March 26. We’ll get to some of the amicus briefs that are flooding in, in a minute. But I think the most surprising thing that happened this week is that two of the journal studies that the appeals court relied on in challenging the FDA’s actions were officially retracted this week by the journal’s publisher, Sage.
In a very pointed statement, Sage editors wrote that it had been unaware that the authors, and in one case one of the peer reviewers, were all affiliated with anti-abortion advocacy organizations and that the articles were found by a new set of peer reviewers to have, “fundamental problems with study design and methodology, unjustified or incorrect factual assumptions, material errors in the author’s analysis of the data.” And a lot more problems I won’t get into, but we will post the link to the entire statement in our show notes.
Now, close listeners to the podcast might remember that we talked about this last August, when a pharmacy professor in Georgia alerted the journals to some of the substantive and political problems, and Sage printed something at the time called an expression of concern. Alice, these articles were cited many times in both the lower-court and the appeals-court rulings. What does it mean that they’ve been formally disavowed by their publisher?
Ollstein: It’s really hard to tell what it’s going to mean because we’re in an era where facts don’t always matter in the courts. I mean, we had recently a whole Supreme Court case about a wedding website designer that was based on facts that did not turn out to be true about their standing. The football coach who prayed on the 50-yard line turned out to not be a true story.
And so, it’s really hard to tell. And pro-abortion rights groups have been arguing that evidence cited by the lower court was not scientifically sound. And so, it’s this “flood the zone with competing studies.” And the average person is just confused and throws up their hands. So, in terms of how much it’ll matter, I’m not sure. You already have the groups in question behind the retracted study accusing the publisher of bias. I think this back-and-forth and finger-pointing will continue, and it’s unclear what effect it’ll actually have in court.
Pradhan: I think the thing that I find troubling about it is it’s … and it’s happened with other issues too. It certainly happened during the covid-19 pandemic, where people would say that there would be research or science via press release instead of academic research really undergoing the controls that it is meant to undergo before it’s released and published in a journal. And I hope at the very least that it leads to this, if we’re going to get some amount of good change, it’s that it really does reinforce the need for really rigorous checks, regardless of what the subject of the study is, because clearly these things, it has real consequences.
And frankly, I mean, look at one of the best-known examples of a retracted study which links vaccines to autism. I mean, that happened. It was widely discredited after the fact, and it is still doing harm in society, even though it’s been retracted and the researcher discredited. So, I think it really underscores the importance. I hope that frankly some of these journals get their act together before they publish things that … because it’s too little too late by the time that the damage has been done already.
Rovner: Yeah, I feel like I would say the judicial version of the journalistic “he said, she said.”
Ollstein: I mean, that’s such a good point by Rachana about how the damage is already done in the public understanding of it. But I also am pretty cynical about the ramifications in court specifically, particularly given the fact that the same lower court that cited these studies also cited things that weren’t peer-reviewed or published in medical journals at all. Things that were just these online surveys of self-reported problems with abortion pills. And so, there doesn’t seem to be a clear bar for scientific rigor in the courts.
Karlin-Smith: I was going to say that gets to this fundamental issue in this case, which is: Are judges capable of really assessing the kinds of evidence you need to make these decisions or whether we should trust the FDA and the people we’ve charged with that to do that? Because they know how to look at research papers and the range of research papers out there and evaluate what science is credible, what’s been replicated, look for these problems.
Because if you want to make an argument, you probably can always find one scientific paper or two scientific paper that might seem like it was published in some journal somewhere that can help support your point, but it’s being able to really understand how science works and back it up with that breadth of evidence and the accurate and really reliable evidence.
Rovner: Yeah. I would note that one of the amicus briefs came from a bunch of former heads of the FDA who are very concerned that judges are taking on, basically, the kind of scientific questions that have been ceded to the expertise of the FDA over many, many generations. I don’t remember another amicus brief like this coming from former FDA commissioners banding together. Have you seen this before?
Karlin-Smith: Yeah. I mean, I certainly can’t think of something like it, but I haven’t necessarily scoured the history books to make sure of it, but it is pretty unusual. I did actually note that [former President Donald] Trump’s two FDA commissioners are not among the alive possible FDA commissioners who could have joined in, that didn’t join in on this one, which is interesting.
Ollstein: Oh, I just think that we’re seeing a lot of the medical community that has previously tried to stay above the fray now feeling like this is such a threat to the practice of medicine and regulatory scientific bodies that they feel like they have to get involved, where they didn’t before. And now you’ve reported a lot on how much the AMA [American Medical Association] has changed over time.
But I think seeing these folks in the medical community that aren’t exactly waving a flag at the front of the abortion rights parade really speaking out about this, and it’s a really interesting shift.
Pradhan: It’s certainly a case that challenges the administrative state, if you will, right? Like the one about mifepristone, about FDA’s expertise in science and scientific background in assessing whether a drug should be approved or not.
But as you all know, there’s another case going before the Supreme Court that challenges what’s known as the Chevron doctrine, which is how the agencies are relied upon to interpret federal laws and court rulings, and it’s their expertise that is deferred to, that also is now, I think being questioned and very well could be undermined potentially next year. So, who else? I guess it’s either judges or lawmakers that are supposed to be the ones that truly know how to implement various laws, instead of the folks that are working at these agencies.
Rovner: As you say, this is a lot broader than just the abortion pill. One of the briefs that I didn’t expect to see came from the former secretaries of the Army, Navy, and Air Force who argued that restricting medication abortion would threaten military readiness by hurting recruitment and retainment and the ability for active women service members in states that ban abortion to basically be able to serve. I did not have that particular amicus on my bingo card, but, Alice, this is becoming a bigger issue. Right?
Ollstein: Well, it’s just interesting because I think about the Biden administration policy supporting service members traveling across state lines for an abortion if they’re stationed in a state where it’s now banned. And the administration has been defending that policy from attacks from Capitol Hill, et cetera, and saying, “Look, we’re not backing this policy because it’s some high-minded abortion right priority. We’re backing this because they think it’s good for the military itself.”
And so, I think this amicus brief is making that same case and saying, having tens of thousands of service members lose access to decision-making ability would really hurt the military. So, I think that’s an interesting argument. Again, like these medical groups, you don’t see the military making this kind of case very often and you might not see it under a different administration.
Rovner: Yeah. It’s yet another piece of this that’s flowing out. Well, not everything on abortion is happening in Washington. The states are still skirmishing over whether abortion questions should even appear on ballots this fall. The latest happened in Florida this week, where the Supreme Court there heard arguments about a ballot question that would broadly guarantee abortion rights in the state. Alice, you were watching that, yes?
Ollstein: Yeah. It was an interesting mixed bag because most of the current state Supreme Court was appointed by [Republican Gov.] Ron DeSantis. These are very conservative people, a lot of them are very openly anti-abortion, and were making that clear during the oral arguments, and they were repeating anti-abortion talking points about what the amendment would do. But at the same time, they seemed really skeptical of the state’s argument that they should block it and kill it.
They were saying, “Look, it’s not our job to decide whether this amendment is good or not. It’s our job to decide whether the language is deceptive or not, whether voters who go to vote on it will understand what they’re voting for and against.” And so, they had this whole analogy of, “Is this a wolf in sheep’s clothing or is it just a wolf?” They seem to be leaning towards “it’s just a wolf” and voters can decide for themselves if they think it’s good or bad.
Rovner: Well, my favorite fun fact out of this case yesterday is that one of the five Republican members of the seven-member Florida Supreme Court is Charles Kennedy, who, when he was serving in the House in the 1990s, was the first member of Congress to introduce a bill to ban “partial-birth” abortion. So, he was at the very, very forefront of that very, very heated debate for many years. And now he is on the Florida Supreme Court, and we will see what they say.
Do we have any idea when we’re expecting a decision? Obviously, ballots are going to have to be printed in the not-too-distant future.
Ollstein: Yes. So, the court has to rule before April 1, otherwise the ballot measure will automatically go forward. And so, they can either rule to block it and kill it, they can rule to uphold it, or they can do nothing and then it’ll just go forward on its own.
Pradhan: The thing that — what I keep thinking about too is so, OK, they’ve indicated that they have to rule, right, by April 1. But then we also have this separate pending matter of what is the status of the six-week ban that is still blocked currently? And I just keep wondering, I’m like, how much could change over the course of 2024? We still don’t have a decision on that, even though that’s been pending for much longer. No?
Rovner: Yeah. Where is the Florida six-week ban? It’s not in effect, right?
Ollstein: Yes. There was the hearing on the 15-week ban, and if that gets upheld, the six-week ban automatically goes into effect after a certain period of time. So, we’re waiting on a ruling on the 15-week ban, which will determine the fate of the six-week ban, and then the ballot measure could wipe out both, potentially.
Pradhan: Right. So, it’s very topsy-turvy.
Ollstein: It’s very simple, very simple.
Pradhan: Right. Yeah. I mean, even just the 15-week ban and the six-week ban, to me, at first it was counterintuitive to think, “Oh, so either both of them stand or neither of them do.” So, it seems like we could be in for many, many changes in Florida this year, but I’m very curious about when that is going to happen because it’s been much longer since … rather than the abortion rights ballot measure for this year.
Rovner: And meanwhile, I mean, Florida is a really key state in this whole issue because it’s one of the only states in the South where abortion is still available, right?
Ollstein: Right. And we saw how important it’s become in the data where the number of abortions taking place plummeted in so many states, but in Florida, they’ve actually gone up since Dobbs, even with the 15-week ban in place. A lot of that is people coming from surrounding states. And so, it is really pivotal, and I think that’s why you’re seeing these big national groups like Planned Parenthood really prioritizing it, and there’s so many different ballot measure fights going on, but I think you’re seeing a lot of resources go to Florida, in part for that reason.
Rovner: We will keep an eye on it. Well, we have not talked about Medicaid in a while, and conveniently, my KFF Health News colleague Phil Galewitz has an interesting story this week that halfway through the largest eligibility redetermination in history, Medicaid rolls nationwide are down net about 10 million people or at roughly the number that they were before the pandemic. Rachana, you spend a lot of time looking at Medicaid. Does that surprise you, that the rolls ended up where they were before?
Pradhan: I think, no, not necessarily. Our esteemed KFF colleague Larry Levitt put it really well in the story Phil wrote, which is that the rapid clip at which this is happening is obviously notable, right? It is not normal for how fast enrollment is declining.
I do think the thing that I wish we had, and we only, I think maybe from a state or two know this, but we certainly don’t have nationwide data and won’t for several years, but how many of these people are becoming uninsured? I think at the end of the day, that’s really what big picture-wise matters. Right? But I think certainly, I mean, the unwinding is still occurring. We’re still probably going to have disenrollments that will, I think at least through basically the first half of this year, certain states are still going to take that long. And so, we really won’t know the full picture for obviously a little bit, but I thought that Phil’s piece was really interesting and on point, for sure.
Rovner: Yeah. We talked about how many more people joined the exchanges this year, on now ACA [Affordable Care Act] coverage. Anecdotally, we know that a lot of those came from being disenrolled from Medicaid, and obviously Medicaid is always full of churn. People get jobs and they get job insurance, and they go on, and then other people lose jobs and they lose their job insurance and they qualify for Medicaid. So, there’s always a lot of ups and downs.
But I’m just wondering, the rolls had gotten so swell during the pandemic when states were not allowed to take people off, that I think it will be interesting that when this is all said and done, Medicaid rolls end up where you would’ve expected them to be had there not been a pandemic, right?
Pradhan: Right. I think that what’ll be interesting to see is, I mean, we have some sense of ACA marketplace enrollment, the way it increased this past open enrollment, but again, we don’t know if some of those Medicaid enrollees, how many of them have shifted to job-based plans, if they have at all, or if they’ve just fallen off the rolls entirely.
One of the other things I think about also is the macro-level picture, of course, is important and good, but knowing who has lost their coverage is also … and so, children, I think have been impacted quite a lot by these disenrollments, and so that’s certainly something to keep in mind and keep an eye on. Right?
Rovner: Yeah. And I know, I mean, the federal government obviously has, I think, more data than they’re sharing about this because we know they’ve quietly or not so quietly told some states that they wish they were doing things differently and they should do things differently. But I think they’re trying very hard not to politicize this. And so, I think it’s frustrating for people who are trying to follow it because we know that they know more than we know, and we would like to know some of the things that they know, but I guess we’re not going to find out, at least not right away.
Well, so remember that work requirement that Georgia got permission to put in, as opposed to just expanding Medicaid? Georgia, remember, is one of the 10 states that have yet to expand Medicaid under the Affordable Care Act. Well, now Georgia is suing the Biden administration to try to keep their experiment going, which seems like a lot of trouble for a program that has enrolled only 2,300 of a potential pool of 100,000 people. Why does Georgia think that extending its program is going to increase enrollment substantially? Clearly, this is not going over in a very big way for the work requirements. Alice, you’ve been our work-requirement person. I’ll bet you’re not surprised.
Ollstein: So, the state’s argument is that all of the back-and-forth with the administration before they launched this partial, limited, whatever you want to call it, expansion, they say that that didn’t give them enough time to successfully implement it and that they shouldn’t be judged on the small amount of people they’ve enrolled so far. They should be given more time to really make it a success.
We don’t have a ton of data of what it looks like when states really go all in on these work requirements, but what we have shows that it really limits enrollment and a lot of people who should qualify are falling through the cracks. So, I don’t know if more time would help here, in Georgia and in some other states that haven’t expanded yet. There’s a real tussle right now between the people who just want to take the federal help and just do a real, full expansion like so many other states have done, and those who want to put more of a conservative stamp on the idea and feel like they’re not just wholeheartedly embracing something that they railed against for so many years.
Rovner: Yeah. Just a gentle reminder that the majority of people on Medicaid either are working or cannot work or are taking care of someone who cannot work. And that in the few states that tried to implement work requirements, the problem wasn’t so much that they weren’t working, it’s that they were having trouble reporting their work hours, that that turned out to be a bigger issue than actually whether or not they were … the perception that, I guess, from some of these state leaders that people on Medicaid are just sitting at home and collecting their Medicaid, turns out not to be the case, but that doesn’t mean that people don’t get kicked off the program likely when they shouldn’t.
I mean, that’s what we saw, Alice, you were in … it was Arkansas, right, that tried to do this and it all blew up?
Ollstein: That’s right. And there were other factors there that made it harder for folks to use the program. But I mean, everywhere that’s tried this, it shows that the administrative burdens of having to report hours trip people up and make it so that people who are working still struggle to prove they’re working or to prove they’re working in the right way in order to qualify for insurance that they theoretically should be entitled to.
Rovner: Well, before we leave Medicaid for this week, I want to talk about the newest state trend, which is using Medicaid money to help pay for housing for people who are homeless or at risk of eviction. California is doing it, so are Arizona and Oregon; even Arkansas is joining the club. All of them encouraged by the Biden administration.
The idea is to keep people from ending up in places that are even more expensive for taxpayers, in hospitals or jails or nursing homes, and that so very many health problems cannot be addressed unless patients have a stable place to live. But pouring money earmarked for health services into housing is a really slippery slope, isn’t it? I mean, we obviously have a housing crisis, but it’s hard to feel like Medicaid’s going to be able to plug that hole very effectively.
Karlin-Smith: I feel like that’s where some of the debate is moving next, which is there’s certainly lots of evidence that shows how much being unhoused impacts somebody’s health and their life span and so forth. But state Medicaid programs have to balance their budget and are usually not unlimited. And for me, in following drugs, that’s been a big issue with some of the really new expensive drugs coming on the market is it’s not that Medicaid doesn’t necessarily want to cover it, it’s that if they cover it, they might have to cut some other health service somewhere else, which they also don’t want to cut.
So, I think maybe this evidence of the ability to improve health through housing might have to lead to thinking about, OK, how do we change our budgets or our systems to ensure we’re actually tackling that? But I’m not sure that long-term, unless we really expand the funding of Medicaid, you can really continue doing that and serve all the traditional health needs Medicaid serves.
Pradhan: Yeah, I mean, if you think about Medicaid, I mean, just going back to the bread and butter of reimbursement of providers. I mean, everyone knows that it’s bad, right? It’s too low, it’s lower than Medicare, it’s lower than commercial insurance, and it affects even a Medicaid enrollee’s ability to see a primary care doctor, specialists. I mean, because there are clinicians that will not accept Medicaid as a form of insurance because they lose too much money on it.
And so, I think this is, it’s interesting, I think there’s this big philosophical debate of, is this Medicaid’s problem? Should it be paying for this type of need when there are so many other, you could argue, unmet needs in the program that you could be spending money on? But these states are not necessarily doing that. And so, I think, obviously, I think it would help to have housing stability, but it, for me, raises these broader questions of, but look at all these other things. Like Sarah said, being able to afford drugs that are expensive, but also are quite effective potentially and could really help people. But they’re already scrambling to do those basic things and now they’re moving on to, is it a new shiny toy? Or, something that’s obviously important, but then you’re ignoring some of the other challenges that have existed for a long time.
Rovner: And housing is only one of these social determinants of health that people are trying to address. And it’s absolutely true. I mean, nobody suggests that not having housing and nutrition and lots of other things very much affect your health, and if people have them, they’re very much likely to do better health-wise. But whether that should all fall to the Medicaid program is something that I think is going to have to be sorted out.
Well, back here in Washington, Congress is having some kind of week, mostly not on health care. So, if you’re interested in the gory details, you’re going to have to find them someplace else. But in the midst of the chaos, the House yesterday did manage to pass a bill called the Protecting [Health] Care for [All] Patients Act [of 2022], which certainly sounds benign enough. Its purpose is to ban the use of a measurement called quality-adjusted life years or QALYs, as they’re known. But Sarah, this is way more controversial than it seems, right? Particularly given the bill passed on a party-line vote.
Karlin-Smith: To back up a little bit, quality-adjusted life years, or QALYs, it’s basically a way to figure out cost-effectiveness or what’s a fair price of a product based on the dollar amount that they’re saying it costs per year of quality of your life extended. So, it’s not just taking into account if your life’s extended, but the quality of your life during that time.
And a lot of people have trouble with that metric because they feel like it unfairly penalizes people with disabilities or conditions where the quality of your life might not seem quite the same as somebody who a drug can make you almost perfectly healthy, if that makes sense? And so actually, Democrats are fairly in alignment with Republicans on not being huge fans of the QALY, that particular measure. It’s actually already banned in Medicare, but they are concerned that the way Republicans drafted this bill, it could make it pretty much hard to use any kind of metric that tries to help programs, state agencies, the VA, figure out what’s a fair price to pay for a drug. And then you get into really difficult problems figuring out what to cover, how to negotiate with a drug company for that.
So, Democrats have actually been pushing Republicans to take out some language that might basically narrow the bill or ensure you could use some other measures that are similar to QALYs, but they argue is a bit fairer for the entire populace. So, something that potentially down the road there could be some bipartisan agreement to ban this measure. I think the concern from people who work in the health economist space is that it does make people, I think, uncomfortable thinking about placing this dollar value on life.
But the flip side is, is that again, every drug that saves your life, we can’t spend a billion dollars on it. Right? And so, we have to come up with some way to effectively figure out how to bargain and deal with the drugmakers to figure out what is a fair price for the system. And these are tools to do it, and they’re really not meant to penalize people on an individual basis, because, again, if the drug is priced way too high, regardless of how beneficial it is, the system and you are not going to be able to afford it. It’s a way of figuring out, OK, what is a fair price based on what this does for you? And also then incentivize drug companies to develop drugs that at the price are really a good benefit for the price.
Rovner: It’s so infuriating because I mean, Congress and health policy experts and economists have been talking about cost-effectiveness measures for 30 years, and this was one of the few that there were, and obviously everybody agrees that it is far from perfect and there are a lot of issues. But on the other side, you don’t want to say, “Well, we’re just not going to measure cost-effectiveness in deciding what is allowed.” Which essentially is where we’ve been and what makes our system so expensive, right?
Karlin-Smith: Right. I mean, you can imagine, like, if you thought about other things that are crucial in your life, like I sometimes think about it, it makes it easier if I think about water, OK, everybody needs water to live. If we let the water utilities charge us $100,000 for every jug of water, we would get into problems.
So again, I think the people that use these metrics and try and think about it, they’re not trying to penalize people or put a price on life in the way I think the politicians use it to get out of this. They’re trying to figure out, how do we fairly allocate resources in society in an equitable way? But it can be easily politicized because it is so hard to talk about these issues when you’re thinking about your health care and what you have access to or not.
Rovner: We will watch this as it moves through what I’m calling the chaotic Congress. Turning to “This Week in Health Misinformation,” we have a story from KFF Health News’ Katheryn Houghton for PolitiFact that earned a rare “Pants on Fire!” rating. It seems that a fundraising ad for Republican congressman Matt Rosendale of Montana, who’s about to become Senate candidate Matt Rosendale of Montana, claims that former NIH [National Institutes of Health] official Tony Fauci brought covid to Montana a year before the pandemic. In other forums, Rosendale has charged that an NIH researcher at Rocky Mountain Laboratories infected bats with covid from China. It actually turns out that the laboratory was studying another coronavirus entirely, not the coronavirus that causes covid, the covid that we think of, and that the virus wasn’t actually shipped, but rather its molecular sequence was provided. To quote from this story, “Rosendale’s claim is wrong about when the scientists began their work, what they were studying, and where they got the materials.” But other than that, these kinds of scary claims keep getting used because they work in campaigns. Right?
Karlin-Smith: It taps into this theme that we’ve seen that Republicans on the Hill have certainly been tapping into over the past year or two of whether covid came from a lab and what funding from the U.S. to China contributed to that, and what do people in the U.S., particularly connected to Democrats, know that they’re not saying.
So, even though as you start to dig into this story and you see every level how it’s just not true, the surface of it, people have already been primed to believe that this is occurring, and it’s been how we do this sort of research in this country has already been politicized. So, if you just see a clip, people are easily persuaded.
Rovner: Yes. I think it was Alice, we started out by saying we’ve become a fact-free society. I think this is another example of it. All right, well that is this week’s news.
Now it is time for our extra-credit segment. That’s when we each recommend a story we read this week we think you should read, too. As always, don’t worry if you miss it. We will post the links on the podcast page at kffhealthnews.org and in our show notes on your phone or other mobile device. Rachana, you got the first one in this week. Why don’t you go first?
Pradhan: Oh, sure. The story I wanted to highlight was from North Carolina Health News. It is focusing on a very large health system known as Atrium Health, which is based in Charlotte, North Carolina. And basically, it’s really interesting, it talks about how Atrium actually operates under a public hospital authority. So, it enjoys certain benefits of being a public or government entity, including they avoid millions in state and federal taxes. They have the power of eminent domain, and they are not subject to antitrust regulations.
And again, this is one of the largest health systems in North Carolina, but it’s playing it both ways. Right? It tries to use the advantages of being a public entity like the ones I just named, but when it comes to other requirements to have checks and balances in government, as we do with various levels of government, like having open public meetings, being able to ask for public comment at these meetings and the like, Atrium does not behave like a government entity at all.
I would also note, as an aside, Atrium was, in the past, one of the most litigious hospital systems in North Carolina. They sued their patients for outstanding medical debt until they ended the practice last year. And so, it’s a really interesting story. So, I enjoyed it.
Rovner: It was a really interesting story. Sarah.
Karlin-Smith: I looked at a piece in the Atlantic from KFF [Health] News editor Elisabeth Rosenthal, “GoFundMe Is a Health-Care Utility Now,” and she tracks the rise of people in the U.S. using GoFundMe to help pay for medical bills, which I think, at first, maybe doesn’t seem so bad if people are having another way to help them pay for medical expenses. But she shows how it’s a band-aid for much bigger problems in an unfair and inequitable system. And, really, also documents how it tends to perpetuate the already existing socioeconomic disparities.
So, if you’re somebody who’s famous or has a lot of friends or just has a lot of friends with money, you’re more likely to actually have your crowdfunding campaign succeed than not. And talking about how health systems are actually directing patients there to fund their medical debt. So, it’s just one of those trends that highlights the state of where the U.S. health system is and that our health insurance system, which is in theory supposed to do what GoFundMe is now an extra band-aid for, which is, you pay money over time so that when you are sick, you’re not hit with these huge bills. But that obviously isn’t the case for many people.
Rovner: Indeed. Alice.
Ollstein: So, I have a piece from Stat’s Usha Lee McFarling, and it’s about the FDA coming under pressure to act more quickly now that they know that pulse oximeters, which were really key during the worst months of the covid pandemic for detecting who needed to be hospitalized, that they don’t work on people of color, they don’t work as well on detecting blood oxygen.
And so, it’s a really fascinating story about, now that we know this, how quickly are regulators going to act and how can they act? But also going forward, this is what happens when there’s not enough diversity in clinical trials. You don’t find out about really troubling racial disparities in efficacy until it’s too late and a lot of people have suffered. So, really curious about what reforms come out of this.
Rovner: Yeah, me too. Well, my extra credit this week is from the Alabama Daily News, and it comes with the very vanilla-sounding headline “Alabama Lawmakers Briefed on New ‘ALL Health’ Insurance Coverage Expansion Plan,” by Alexander Willis. Now, Alabama is also one of the 10 remaining states that have not expanded Medicaid under the Affordable Care Act, much to the chagrin of the state’s hospitals, which would likely have to provide much less free care if more low-income people actually had insurance, even Medicaid, which, as Rachana points out, doesn’t pay that well. The plan put forward by the state hospital association would create a public-private partnership where those who are in the current coverage gap, the ones who earn too much for Medicaid now, but not enough to qualify for Affordable Care Act subsidies, would get full Medicaid benefits delivered through a private insurer. Ironically, this is basically how neighboring Arkansas, another red state, initially expanded Medicaid back in 2013. I did go and look this up when this happened. And it wasn’t even new then. But still, the plan could provide a quarter of a million people in Alabama with insurance at apparently no additional cost to the state for at least the first five years and maybe the first 10. So, another place where we will watch that space.
All right, that is our show. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left us a review; that helps other people find us, too. Special thanks as always, to our technical guru, Francis Ying, and our editor, Emmarie Huetteman. As always, you can email us your comments or questions. We’re at whatthehealth@kff.org, or you can still find me at X, @jrovner, or @julierovner at Bluesky and @julie.rovner at Threads. Sarah, where are you these days?
Karlin-Smith: I’m on Twitter a little bit, @SarahKarlin. And Bluesky, I’m @sarahkarlin-smith, other platforms as well.
Rovner: Alice?
Ollstein: @AliceOllstein on X, and @alicemiranda on Bluesky.
Rovner: Rachana?
Pradhan: I’m @rachanadpradhan on X, although my presence lately has been a little lacking.
Rovner: Well, you can definitely find all of us. And we will be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 8 months ago
Aging, Courts, Medicaid, Multimedia, States, Abortion, CHIP, Florida, Georgia, Guns, KFF Health News' 'What The Health?', Misinformation, Podcasts, Women's Health
KFF Health News' 'What the Health?': The Struggle Over Who Gets the Last Word
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
The Supreme Court in March will hear oral arguments in two very different cases that boil down to the same question: How much power do “experts” in health and science deserve? At stake is the future accessibility of the abortion pill mifepristone, and the ability of government officials to advise social media companies about misinformation.
Meanwhile, abortion opponents are preparing action plans in case Donald Trump retakes the White House. While it’s unlikely Congress will have enough votes to pass a national abortion ban, a president can take steps to make abortion far less available, even in states where it remains legal.
This week’s panelists are Julie Rovner of KFF Health News, Sandhya Raman of CQ Roll Call, Joanne Kenen of Johns Hopkins University and Politico Magazine, and Sarah Karlin-Smith of the Pink Sheet.
Panelists
Joanne Kenen
Johns Hopkins Bloomberg School of Public Health and Politico
Sarah Karlin-Smith
Pink Sheet
Sandhya Raman
CQ Roll Call
Among the takeaways from this week’s episode:
- Abortion opponents are preparing for the possibility of a second Trump presidency. Among ways the former GOP president could influence policy without Congress is by installing an activist secretary of Health and Human Services, possibly allowing a political appointee to overrule decisions made by FDA employees.
- While President Joe Biden is embracing abortion rights, Donald Trump is highlighting two conflicting truths: that he appointed the Supreme Court justices who helped overturn the constitutional right to an abortion and that embracing abortion restrictions could drive away voters.
- The federal government is making its initial offers on 10 expensive pharmaceuticals targeted for Medicare price negotiations. But the process is private, so it is unknown what those offers are.
- Two pharmaceuticals that have been in the headlines — the controversial Alzheimer’s disease drug Aduhelm and the insulin Levemir — will soon be pulled from the market. The decisions to discontinue them play into an ongoing debate in drug development: When is innovation worth the price?
- “This Week in Health Misinformation” features an article by KFF Health News’ Amy Maxmen about how what once were fringe views questioning science are now becoming more mainstream.
Also this week, Rovner interviews Samantha Liss, who reported and wrote the latest KFF Health News-NPR “Bill of the Month” feature, about a husband and wife billed for preventive care that should have been fully covered. If you have an outrageous or confounding medical bill you’d like to share with us, you can do that here.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: ProPublica’s “Amid Recall Crisis, Philips Agrees to Stop Selling Sleep Apnea Machines in the United States,” by Debbie Cenziper, ProPublica, and Michael D. Sallah, Pittsburgh Post-Gazette.
Joanne Kenen: The New York Times’ “Elmo Asked an Innocuous Question,” by Callie Holtermann.
Sarah Karlin-Smith: The Texas Tribune’s “Texas Attorney General Requests Transgender Youths’ Patient Records From Georgia Clinic,” by Madaleine Rubin.
Sandhya Raman: The Associated Press’ “Community Health Centers Serve 1 in 11 Americans. They’re a Safety Net Under Stress,” by Devi Shastri.
Also mentioned on this week’s podcast:
- Politico’s “The Anti-Abortion Plan Ready for Trump on Day One,” by Alice Miranda Ollstein.
- The 19th’s “The Tools Trump Cold Use to Curb Abortion Access if He’s Elected,” by Shefali Luthra and Mel Leonor Barclay.
- The New York Times’ “How Trump Could Institute a Backdoor Federal Abortion Ban,” by Mary Ziegler.
- CQ Roll Call’s “GOP Pivots on Abortion Stance as 2024 Nears,” by Ariel Cohen and Sandhya Raman.
click to open the transcript
Transcript: The Struggle Over Who Gets the Last Word
KFF Health News’ ‘What the Health?’Episode Title: The Struggle Over Who Gets the Last WordEpisode Number: 332Published: Feb. 1, 2024
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello, and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News, and I’m joined by some of the best and smartest health reporters in Washington. We are taping this week on Thursday, Feb. 1, at 10 a.m. As always, news happens fast, and things might have changed by the time you hear this. So here we go.
We are joined today via video conference by Joanne Kenen of Johns Hopkins University and Politico Magazine.
Joanne Kenen: Good morning, everybody.
Rovner: Sandhya Raman of CQ Roll Call.
Sandhya Raman: Hello, everyone.
Rovner: And Sarah Karlin-Smith of the Pink Sheet.
Sarah Karlin-Smith: Morning.
Rovner: Later in this episode, we’ll have my interview with KFF Health News’ Samantha Liss, who reported and wrote the latest KFF Health News-NPR “Bill of the Month.” This month’s patient — actually, patients — got unexpected bills for care that should have been fully covered.
Before we get to this week’s news, it is February, so that means we want your health policy valentines. We will put a link to submit in our show notes. It’s on our web page at kffhealthnews.org. Show us, and your valentine, your affection for nerdy health policy topics. Winners will get read on the podcast and shared on our webpage and social media. The top poem will get its own illustration by our amazing in-house artist, Oona Tempest, so get those entries in.
OK, now the news. We will start this week in federal court where March is starting to look like “Health Policy Month.” At the 5th Circuit in New Orleans, judges will hear arguments in the case Braidwood v. Becerra, which challenges the very popular provision of the Affordable Care Act that requires insurers to cover a long list of preventive services at no out-of-pocket cost to patients. Fun fact: This is the provision in question in the latest “Bill of the Month,” which you will hear about in a few minutes. Another fun fact: The lower-court decision in this case came from Judge Reed O’Connor, whose name might sound familiar because he was the judge who tried to strike down the entire Affordable Care Act back in 2018. Somebody remind us why the plaintiffs here think the preventive services mandate is unlawful and should be stricken?
Raman: One of the issues that they have in this case is that certain types of this preventative care are in question — so, some of the things related to women’s health, vaccines, PrEP for preventing HIV, and just the moral issues that they have that those things do not necessarily need to be applied to under their plan. It’s some of those things in particular that come up.
Rovner: Yeah. I think in this case it seems to be mostly PrEP. It seems to be mostly about not wanting to encourage homosexual behavior, as the plaintiffs are saying, which is a rerun of what we had with the birth control cases, which went on, also for this provision of the ACA. No matter what happens in this case, Braidwood is sure to be appealed to the Supreme Court, which already has two health-related cases set for March oral arguments.
On March 18, the justices will hear Murthy v. Missouri, which challenges the government’s ability to coordinate with social media companies to downplay medical misinformation. The attorneys general of Louisiana and Missouri are arguing that the Biden administration essentially worked to censor conservative views. The Murthy in this case is Surgeon General Vivek Murthy, on whose behalf the Justice Department called the lower-court ruling seeking to bar communication between the White House and federal health agencies with social media companies, quote, “novel, unbounded, startling, radical, and ill-defined.” This could be a really important case for those trying to rein in medical misinformation, right? I mean, it’s obviously a really delicate thing. What serves as medical misinformation when the government gets to say, “Really, it should be at least de-algorithming,” if that’s a word, “this stuff because it’s not correct.”
Karlin-Smith: Right. I think one of the questions here is was the government collaborating and just sort of discussing and flagging these concerns to the companies, or did they exercise some sort of undue leverage here? Which is a big debate. Obviously, a private company has different ability to also regulate speech on its platform than the government does. So that’s another element to the case. I think sometimes people get confused about what your free speech rights are when you’re not directly dealing with the government in the U.S.
Rovner: Yes, there’s no guaranteed free speech in a private space like social media. I mean, they are not government-run. Although, I guess one of the arguments here is that they may be government-involved. I guess that’s what this case is supposed to try and create the guidelines for, but it’ll be … I’m looking forward to actually listening to these oral arguments.
Well, the following week, on March 26, the Supreme Court will hear the case FDA v. Alliance for Hippocratic Medicine, which is the one where conservative doctors challenged the original year 2000 approval of the abortion pill mifepristone. Technically, the justices are no longer considering canceling the original approval. They’re considering rolling back the FDA’s loosening of restrictions on the drug in 2016. But still, that alone could be a big deal, right? Sandhya, you’ve been following this, have you?
Raman: Yeah. Yeah. The Supreme Court decided at the end of last year that they would be taking up the case. So this week they set the actual oral arguments that we can look forward to. That’s going to be the first big abortion case that they’re going to hear since Dobbs. We have another abortion case coming up in April related to emergency health care. I think that it is interesting that it’s not over the full approval of the drug, it’s the regulations, but if you …
Rovner: Well, that’s because the 5th Circuit rolled back the original decision.
Raman: Yes. But I think that if you look at how much the regulations have changed since the original approval, there’s been a lot of expansion in just how it can be used, who can prescribe it, where it can be used, that kind of thing. So even if they were to rule to rescind some of those regulations and keep the original approval in place, that could have a huge effect in terms of who can get it. I mean, since the initial approval, we’ve been allowed to distribute it by mail, we’ve been allowed to do by telehealth to prescribe it. Just the length into pregnancy that it can be used, there’s been a lot of changes there. So we’ll have that to watch. The briefs have all started coming in, at least in favor of keeping the regulations as they are. We’ve had a huge lawmaker brief from a lot of Democrats. We had one from a lot of the pharmaceutical companies, including some big ones like Pfizer and Biogen.
Rovner: Yeah. I noticed in the PhRMA brief — or the pharmaceutical companies’ brief; I don’t believe it was from PhRMA the organization yet. But they did say that they were worried that if the court even were to uphold the 5th Circuit decision, which doesn’t cancel the approval but would cancel all of the changes since 2016, that that would basically freeze in place the use of drugs as we discover new uses for the same drugs. I mean, if you can’t relabel and put them out in a different way for different things, that would be a big hit to the drug industry, which, Sarah, spends a lot of time repurposing existing drugs, right? That’s a big part of drug development.
Karlin-Smith: Right. Improving upon a drug once it gets approved, expanding the label to treat different conditions is a big thing. The underlying tension for the pharmaceutical industry here is that there is a concern that this is the courts weighing in on sort of questioning the scientific judgment of the FDA in a way that would just make our whole drug approval regulatory system not function well for the industry, regardless of whether you’re talking about an abortion drug or a cancer drug or an arthritis drug. That’s really why there’s so much engagement from folks who are not necessarily here to argue about abortion politics. It’s just this concern that there’s certain scientific expertise and deference that we feel like the FDA should have, and that there’s concern that courts don’t really have that ability to accurately second-guess their judgments there.
Rovner: This really harkens back to what we’ve been talking about for the last couple of weeks with this big Supreme Court case on Chevron deference, which is basically the question of whether judges get to decide how to interpret federal laws or whether courts get to decide. This obviously would be a big deal because judges are not generally people with the expertise that doctors and scientists at the FDA have, right? Isn’t that sort of a big piece of this case too?
Kenen: Yes. We know that this particular court is anti-abortion. If they had just sort of a birthday cake wish, they would make the abortion pill go away. The question is where are they going to come down on who gets to decide? Is this an FDA decision or is this a legal decision elsewhere in the system? That’s the mystery. We really don’t know. In some ways, too, with the prior case we were just talking about, about preventive care, the USP has a lot of … the U.S. Preventive …
Rovner: Services Task Force.
Kenen: Who decides? What’s their authority? Which is part of the underlying legal battle in that case. So, are they anti-abortion? Yeah. Six, we know, are. Are they anti-FDA? Are they going to find some legal rationale for pulling this out of the FDA, with leaving other drugs in the FDA? That’s sort of part of what we’ll be watching for. Not just us. I mean, that’s what it comes down to.
Rovner: I was going to say, even the social media case, I mean, all of these cases are basically about scientific expertise and who gets to have the last say on questions of science and medicine. I mean, literally, all of these cases are about the same thing when you come right down to it.
So while we are on the subject of abortion, former South Carolina governor and, still, Republican presidential candidate Nikki Haley has been dodging questions about a federal abortion ban by pointing out that if neither party has 60 votes in the Senate, nothing can pass. Which is true as long as there’s still a filibuster. Well, it seems that the anti-abortion movement took that as a challenge. Two of our podcast colleagues, Shefali Luthra and Alice [Miranda] Ollstein, have eye-opening stories this week about all the things that President Donald Trump could do, if he’s elected again, without Congress. Some of those are things that he did in his first term that President Biden reversed, but some are new ones too. They’re already vetting people to carry out those policies. It looks like they want to be ready on day one. At least the anti-abortion forces want to be ready on day one, to do kind of a full-court press on anything that they consider to be abortion related.
Raman: Yeah, I think there have been, in the past, some of these policies that have gone back and forth between each administration. So something like Title X, the family planning program. Depending on if we have a Democrat or a Republican in office, they change what some of the regulations are there, but then …
Rovner: They basically kick Planned Parenthood in or out.
Raman: Yeah, things like that. Or like the Mexico City policy, which does something in a similar … but for overseas funding. And we’ve had also a ton of different new regulations since the Dobbs decision, in the Biden administration making it a little easier if you are, in certain cases, needing an abortion and are in the VA, in the Defense Department, things like that, that have been big issues for a lot of Republicans. So they would also have to — it’s more of a new territory to figure out how to roll back some of those compared to some of the things that they have a standard plan on.
But if you look at both of our podcast colleagues’ stories, one that stuck out to me was just kind of how they would have the FTC [Federal Trade Commission] try to crack down on abortion by mail, which comes back to the court case we were just discussing, abortion medication, abortion. And just how you could reinterpret some of the existing regulations that we do have regardless of what happens at the Supreme Court.
Karlin-Smith: I was going to say one thing that really stuck out to me in one of The New York Times pieces about this was how even the Trump administration could basically have their HHS [Department of Health and Human Services] secretary override FDA decisions, because we sort of forget that, actually, the way Congress has written a lot of the laws, actually, the HHS secretary has that ultimate authority around drug approvals. We just sort of take it for granted, I think, that for the most part they delegate that to FDA and the political appointees stay out of it. That’s another thing they raise is you could have sort of a more activist HHS secretary that could interfere with what does or doesn’t get approved by FDA. So there’s some pretty norm-ending ideas there for the government.
Rovner: I will say that I do remember Kathleen Sebelius came in and overrode an FDA … about contraception coverage decision. President [Barack] Obama made it clear that he asked Secretary Sebelius to override the FDA, but I think that was more to protect the FDA. Made it clear that this was a policy decision, not a medical decision. I know that they struggled with that a lot. For exactly the reason that you’re saying, that they didn’t want this to become normal, to have the secretary override the decision of the FDA.
Kenen: But that was a big controversy and someone at the FDA quit over it. I think it was the women’s health person. In that case, it was narrow. It was about, if I’m remembering correctly, Julie has a, sometimes, better memory, it was under-18 access to the morning-after pill, right? It was about 10 or 12 years ago.
Rovner: It was 2011 because it was the night my dog had her leg surgery and I had to come back to the office at 1 in the morning because we didn’t think that the secretary was going to override this decision.
Kenen: No, I said 10 to …
Rovner: I remember it really vividly.
Kenen: … 10 to 12 years ago. Yes, it was, then, 12 years ago. There hasn’t been a high-level repetition of that that I can think — of a HHS override. I mean, that’s one reason why the former FDA commissioners maybe … Julie, you and I were both at Aspen that year. It was maybe eight years ago or nine years ago where all the former FDA commissioners came together and called for the FDA to become an autonomous agency, sort of like the SEC [Securities and Exchange Commission], which was a proposal that then fell in a pond and was never heard from again. But that would prevent that kind of political interference. I mean, I actually spoke to a former FDA commissioner sort of recently and said, “Whatever happened to that?” And he said, “Wait.” So apparently they haven’t totally forgotten. We’re going to see reiterations of this fight over absolutely everything for the indefinite future: Who gets to decide?
Rovner: Yeah, I do think, like I was saying, that this is basically all about who gets to make medical and scientific decisions and whose, quote-unquote, “opinion” holds. Well, before we get off of this totally, both Alice’s and Shefali’s story, and an op-ed by University of California-Davis law professor Mary Ziegler, who’s also been on this podcast, talk about the revival of the Comstock Act. We have talked about this before and we surely will again, but somebody remind us what this 1873 law does and how it could be applied to abortion.
Karlin-Smith: In simple terms, it’s to prevent sending what are considered, quote-unquote, “obscene materials” through the mail. What that can refer to has been interpreted in different ways over the years. I mean, some of the … when it’s from the 1800s, it’s before we had medication abortion. It’s before we had the internet and telemedicine and all of these things. So there’s a lot of room that people have seen for just how it can be reinterpreted now with a lot of different things in place compared to over a 100-and-some years ago, and just how that can work in certain favors.
Rovner: I think I’ve said this before, now that we’re talking about the Comstock Act again, I realize that Anthony Comstock, who it is named after, was not a member of Congress. He was just an anti-smut crusader, basically. I believe the phrase, “You can’t send anything lewd or obscene through the mail.” This would be how they could sort of use it to say that anything abortion or possibly even contraception could be lewd or obscene. With all of this, that the Republicans are getting ready, or at least the anti-abortion groups are getting ready to do, Sandhya, you have a story out this week pointing out that abortion is not something Republicans are emphasizing on the campaign trail. Why not? There seems to be an awful lot of enthusiasm on that side.
Raman: It is pretty interesting. I mean, even if at this point it’s looking like we’re going to have the Round Two of the Trump-Biden matchup, if you look at how Trump, and then even Nikki Haley, have been messaging, all their ads, all that, they have not been as strong on anti-abortion issues as they have in the past. They’re both people that — both of them I’ve covered addressing annual Susan B. Anthony List events. I’ve covered March for Life where Trump has addressed them. They’ve both been very strong on this issue. And then, as you look at it now, neither of them have been really strong on committing to signing a national ban. Haley has really sidestepped the issue in a lot of the interviews that she’s done, just because, like you said, the Senate filibuster. I think even Trump has … they’ve been messaging on him being the most pro-life president that they’ve had. He’s just kind of sidestepped it as well, just kind of emphasizing other things. If you look at the advertising they’ve been doing, it’s not focused on this. It’s such a stark contrast to what the Biden campaign has done, which has really gone all in on abortion rights. They even had an all-reproductive-rights-themed rally a couple weeks ago.
Kenen: When Trump did the town hall on Fox, two, three weeks ago, whenever that was, he had it both ways, which meant that there’s a film clip to use whoever you’re advertising to. Within a minute and a half or two minutes or whatever it was, Trump took credit for knocking down Roe. He took credit for … “I accomplished that.” In other words, he appointed the justices or some of the justices that voted for that. So he took credit for finally being the one to get rid of abortion after 50 … get rid of Roe after 50 years. He was very …
Rovner: Which is true.
Kenen: It’s true. Well, both things he said were true because he took credit for that. So there’s your film clip one for that ad, or that message, or that social media, or whatever, direct mail. Whatever you want to use it for. It’s “I am the one.” And it’s true. And then, in the next breath, he said, “But we have to win elections.” He’s also said he’s for a … is it rape and incest or just rape? I think it was both. He’s for that exception. And then he talked about, “Face reality, we have to win.” Which is also a true statement if you’re running for president. You have to win or you don’t get to do these things that you’ve promised. So, I mean, he’s not the first politician or the last to try to have it both ways. It was interesting that he had it both ways, both accurately, in a two-minute conversation.
Rovner: Not that uncommon for him, though …
Kenen: No, but …
Rovner: To take both sides of an issue at the same time.
Kenen: He was so unabashed about it, it was sort of interesting that, “I did this, but maybe I won too much. Maybe it wasn’t …” I mean, at the polls, abortion has won.
Rovner: Yeah.
Kenen: Anytime there’s been a single-issue vote on abortion, the pro-choice people have won every ballot initiative since Dobbs.
Rovner: Yeah. And yet the other ironic thing, I mean, Sandhya, you already mentioned this, that the Biden administration is going all in on abortion because they know that Democratic women and independent women in most polls are supportive of abortion rights and not supportive of the Dobbs decision. On the other hand, Biden himself is an unlikely messenger for this. He’s a Catholic man of a certain age. He’s always been uncomfortable with this issue. He was pro-life early in his career. There was a joke that he didn’t even say “abortion,” I think, until a year into his presidency. There was an actual website that said, “Has Joe Biden said the word abortion yet?” So is he going to be able to bring along all of these people because they’re just going to, “If you support abortion rights, you’ll just vote for anybody not named Donald Trump”?
Raman: I mean, I think that we’ve already seen some of these different abortion-oriented groups really mobilize or kind of illustrate, commit how much money they’re going to spend, all the on-the-ground stuff they’re going to do to get him reelected. They have called out some of the things that he’s done, some of the regulations we’ve already talked about, that kind of thing. But I do get the sense that some of them are frustrated that we haven’t done enough. But I mean you could say the same for the other side. There’s always more that people want. Given the limitations of government when you don’t have the trifecta, and even when you do have the trifecta, if you don’t have enough of a majority to get some of your golden-ticket items done. So I think that it will be interesting to watch. I mean, we even, going forward, for the State of the Union coming up, they’ve already announced that they’re going to have … one of the guests is Kate Cox, the Texas woman who had to travel when she wasn’t able to get the court order to get the emergency abortion.
Rovner: Yeah.
Kenen: I mean, it’s a turnout issue. We know that voters are not enthusiastic about either candidate. We know that, right? I mean, will that change as the election gets closer? Who knows? But right now, many polls are finding that America’s not crazy about this particular rematch. So what are the issues that motivate people who are lukewarm to actually vote? This is going to be on both sides. This is going to be an issue, but the intensity in many ways is going to be on the Democratic side because they’re, just like it used to be, the one fighting for change. The one on the out is the one more likely to have that voter intensity. For 50 years, it was the Republicans. For the last 18 months, it’s been the Democrats. Vice President [Kamala] Harris has been talking about this. A lot of the other surrogates are talking about this. So this is a “Will this make you get out of whatever else you were going to do that Tuesday, or early vote, and actually vote?” It’s going to be one of the key issues in turnout.
Karlin-Smith: I think that’s a great point, that that is another reason why there’s so much Republican messaging on some of these other issues, on immigration, on crime and things like that. Because when it’s not a single-issue thing like the ballot — they’re still winning tons of races for governor and things like that. Maybe focusing on those issues might be good for them to boost some of the turnout.
Rovner: Well, another big issue that voters care about is drug prices. We actually have a lot of drug news this week. The federal government, just this morning, sent out its first set of proposed prices for the 10 drugs they have selected for Medicare price negotiation. Of course, they’re not telling us those prices because this is a private negotiation. But Sarah, did anything jump out at you from what they’ve said about kicking off this process?
Karlin-Smith: I think right now what the Biden administration is trying to do is just sort of publicize that this process is happening. Because again, this is a big political issue, an election thing that they’re hoping will motivate voters. But at the same time, it’s a little bit of a dud in some ways because the government can’t say what they’re offering and the companies don’t necessarily seem inclined to put out any information on this yet. So it’s going to be a pretty private process, potentially all the way up until this fall, in September, when we’ll get some public information. But I think the Biden administration just wants to keep ramming it into voters’ heads that, “Hey, we’re doing work to try and lower drug prices for people as much as we can.”
Rovner: Of course, the drug industry still hopes that some court will overrule and stop this whole thing, right?
Karlin-Smith: Right. There was actually oral arguments yesterday in one of the challenges from AstraZeneca to … that they’re hoping courts will intervene. I think some of the initial reporting from that was that the judge was fairly skeptical of some of AstraZeneca’s arguments, such as that there’s sort of a due process or taking of property that the government is not allowed to do here. The judge was basically saying, “Well, nobody is forcing you to participate in the Medicare program and sell your drugs there.” So some initial, at least, positive signs for the government in those oral arguments.
Rovner: Yeah. Although, as we know, they have a long way to go. In the individual-drug news category, remember when we were talking all about the controversial Alzheimer’s drug, Aduhelm, pretty much every week? Well, it is back and it’s sort of gone, or going, at least. Drug company Biogen is giving up ownership and prematurely ending a trial that was supposed to confirm the drug’s effectiveness in treating early Alzheimer’s. Sarah, you followed this from the very beginning. What do you take away from this whole saga? I mean, at one point, Aduhelm was going to be the answer, and then it was going to break Medicare because it costs so much. And then it was going to make people sick because it had side effects. And now it’s just going away.
Karlin-Smith: There’s so many layers to this story, but the quick version of it is, basically, FDA sort of controversially approved this drug over a lot of skepticism of whether it was actually going to be beneficial to patients. They use sort of a controversial measure that the drug reduced these amyloid plaques in the brain, but there were a lot of questions, including by outside scientists and so forth, as to whether this would actually improve the lives of patients with Alzheimer’s in terms of helping them function and memory. There’s a lot of side effects to the drug. Of course, the third layer of this is it was priced quite costly. What ended up happening was Medicare said, “We will only cover this drug at this point in time if it’s used in a clinical trial.” Part of what happened, I think in large part because of that, is there was no uptake of this product, no sales. That’s really why Biogen has pulled the plug here. The other element of this is that Biogen also has another Alzheimer’s drug that was approved fairly shortly thereafter that actually has better data to show there’s some benefit in actually improving people’s cognition. So again, they’re not necessarily invested in pushing forward a drug where they face all these payment challenges and have less solid data. The question now becomes, what does FDA do here? Do they officially go through the process and make sure … force Biogen to pull it off the market? What do they do about this clinical trial that they were supposed to be conducting to confirm the benefit? And what does science lose if that just gets stopped? I’m not sure if anyone will feel like there’s a need to complete that at this point. But it does raise interesting questions to me because I think about 1,500 or something patients were actually already enrolled in participating in that study.
Rovner: But I do think it’s important to emphasize that since Aduhelm was sort of all the rage, the big debate, we actually are finally seeing some drugs that do appear to have more benefit than cost for early Alzheimer’s. I mean, not a cure, but at least a slowing of the deterioration, right?
Karlin-Smith: I guess I think people are sort of cautiously optimistic about these drugs. They’re excited. Nobody thinks these are the holy grail yet of Alzheimer’s treatments. I think even some of the CEOs of the companies working on them have acknowledged that, but they do seem to offer some benefit. Again, there’s still a lot of these brain-swelling safety events that can be fairly devastating. So I think people are going to be watching really closely. Because usually what we know when a drug is initially approved is a fraction of what we end up knowing over time. So I think it’s still early days, but there is some hope that we finally sort of maybe cracked the code on some of the mechanisms of action of how to treat Alzheimer’s.
Kenen: Like with other drugs in cancer, elsewhere, sometimes you just need the first-draft drug. Hopefully, this isn’t the best we’re going to get. These new drugs that are showing some promise and some slowing down is sort of a proof of concept. Yes, you can make a drug that works. In other fields, too, you ended up … the first drug wasn’t a great drug, but it was a leap ahead in terms of understanding the science. So the fact that we have anything that does anything, scientists do consider that they don’t really understand Alzheimer’s, but it matters that there’s some effect. It’s not next week or next year, but there’s a goal that you can see. I think if you’re an Alzheimer’s researcher who’s spent their life not seeing a lot of tangible results, this is like a glimmer. Maybe more than a glimmer. I mean, this is like, “OK, we’re learning how to do this.”
Karlin-Smith: That was actually one of Biogen’s arguments, I think, for why Aduhelm should have been approved in the first place. Maybe even some folks at the FDA basically saying, “Look, we know this maybe isn’t the home run, but if you don’t approve these products, people are just going to leave this space and not invest in it and not keep trying to bring forth drugs.” I mean, there are people that vehemently disagree with that argument, that that’s the best way to encourage the right innovation for this country, but that wasn’t an argument you saw from industry and even some at the FDA, I think.
Kenen: But I wasn’t talking about Aduhelm specifically. I mean, the other ones that are in the pipeline that are coming out. I mean, it’s new and we don’t really know much about them yet. But the past Alzheimer’s drugs were basically useless or really limited use. These might be what we will later look back on as the first draft as opposed to another failure.
Rovner: I want to move on to another drug that’s being discontinued. European mega drugmaker Novo Nordisk has announced its ending production of a long-acting insulin, Levemir — I think that’s how you pronounce it — that, coincidentally, is one of the insulins that it slashed prices on last year under pressure from lawmakers. The announcement came the same week the company announced it would double the availability in the U.S. of its blockbuster weight loss drug, Wegovy, and the same week that the company hit $500 billion in market value. While there are substitutes for the insulin, for Levemir, many of its patients say this particular product is the best one for them, and there isn’t a one-to-one substitute. I guess this is a reminder that for drug companies, the prime goal is turning profits for their shareholders. I mean, they’re making a lot more money off of these weight loss drugs than they are off their diabetes drugs. We know that the weight loss drugs were in shortage because they couldn’t make enough of them. So you don’t have to be really good at math to kind of put two and two together here, right?
Raman: Right. I’m not sure they’re necessarily even hiding that fact, to some degree. They basically lowered the prices of a lot of these insulin products because of changes in the Medicaid rebate program, where because these products had their prices raised so much over the years, they were going to be subject to new inflation penalties, where they’d essentially owe Medicaid money if they didn’t lower the price. So now you have these older insulin products with lower prices that don’t make them as much money. And Novo Nordisk, in the insulin space, has innovated over the years and made some improvements. So they want to focus on selling their insulin products that they can sell at a higher price point. But again, you get patients who say, “Look, this older drug, actually, I personally, think works better.” And there’s a benefit to patients that it’s cheaper. This is, I think, an old story in the pharmaceutical space that sometimes is looked upon by lawmakers, which is, they innovate and they push patients onto newer products, but is the innovation really worth the price or should people have some way to choose the older product for the lower price if they think it works fine for them?
Rovner: Speaking of drug company profits, the CEOs of Merck and Johnson & Johnson have voluntarily agreed to testify before the Senate Health Committee — meaning that Chairman Bernie Sanders won’t have to subpoena them after all. The hearing is scheduled for Feb. 8. But it’s not about any specific legislation, this is just a chance for Sanders to lecture the CEOs about their high prices, Sandhya?
Raman: Essentially, yes. I think, also, it’s been such a big issue for him. Even if you look back when we had the various nominees, that they wanted to … that would go through his committee where he said that he really wanted more action on this. So I think it’ll be interesting what he brings up, and if there’s a clear pathway of something to move forward since this has been such a big issue for him for a while.
Rovner: Well, he successfully made me want to watch this hearing. We’ll see how it goes. All right. Well, let us turn to “This Week in Health Misinformation.” In addition to that case that the Supreme Court will hear, that we talked about at the top, we have a story from my new KFF Health News colleague, Amy Maxmen, about how what used to be fringe anti-science views are now mainstream among Republicans in general. Vaccine hesitancy has gone up. And that’s hesitancy even to long-proven childhood vaccines, not just the covid vaccine. While trust in science in general has dropped, according to numerous polls. In Florida, Gov. Ron DeSantis has made public health conspiracies part of his platform. And as a presidential candidate, he said he would’ve considered nominating noted conspiracy theoretician and anti-vaxxer Robert F. Kennedy Jr. to run the CDC [Centers for Disease Control and Prevention]. I’ve certainly seen more pushback in my reporting of things that people used to agree on. I assume you guys have too. I mean, it harkens right back to our original theme of who gets trusted when they talk about science and medicine.
Karlin-Smith: I think one of the interesting things that Amy’s story really points out very well, that people have been talking about a lot since the beginning of the covid era, is that this anti-science or anti-vaccine attitude has really become embedded in people’s personal identity and personal politics in a new way. Once it becomes part of your political identity, the experts are saying, it becomes much harder to change people’s views. That’s seen as one of the key problems right now, because, again, providing facts or just rebutting the information doesn’t seem to work when you’re basically sort of attacking somebody’s core identities and beliefs.
Rovner: Yeah, it’s an interesting subject, how we’re sort of freezing a lot of these things in place.
Kenen: Well, it’s also tied up with liberty and freedom in a way that has been part of the anti-vax movement for a long time, but it was a much smaller thread. Right now, this individual liberty or medical freedom, “You don’t have the right to mandate anything,” that “It’s my body.” Now, that’s fine if it’s really only your body, but when you’re talking about infectious diseases, it’s everybody’s bodies. Anti-vaxxing is across the … there are people on both the left and right who are against vaccination. That has changed in the intensity and the politicization on the right, during covid and since covid, and this medical freedom movement, which is sort of a subsection of libertarianism. We tend to talk about anti-vaxxers and anti-vaccination because that’s the most salient thing in the last few years, but there is a broader distrust of expertise, period. Scientific expertise, medical expertise, everything. I mean, some of you know I’m writing a book. We turned in the first draft this very morning. Misinformation is part of the book, and disinformation. This decline, when I was researching … it wasn’t that America was a really trusting society. I was surprised. Going back in history, we’ve always [had] pretty high distrust rates of many major institutions, but it’s much higher in health, medicine, science, public health right now.
Rovner: It’s not just the U.S. We’re seeing this around the world, basically, since the pandemic.
Kenen: It’s tied into the pandemic. It’s tied into the research of populism, a right-wing form of populism. It’s tied into a whole anxiety. The last few years have been really hard on people. Science didn’t have the answers and quick fixes that people wanted, because science is incremental, and people wanted instantaneous fixes. They didn’t understand the incremental changing nature of science, and scientists didn’t always explain it well enough. So it’s here to stay for the near future. It’s pretty insidious because it’s way beyond vaccines.
Rovner: I’m sure we will talk about it more. Well, that is this week’s news. Now we will play my “Bill of the Month” interview with Samantha Liss, and then we will come back with our extra credits.
I am pleased to welcome to the podcast my colleague Samantha Liss, who reported and wrote the latest KFF Health News-NPR “Bill of the Month” installment. Thanks for joining us, Sam.
Samantha Liss: Hi.
Rovner: So, this month’s patients, a husband and wife, got some mysterious bills for preventive care that they thought should have been free. Tell us who they are and what they got.
Liss: Yeah. So this month we bring you Chantal Panozzo and her husband. They live outside Chicago. And they underwent their first colonoscopies last year, after turning 45.
Rovner: Then, as we say, the bill came. Now, colonoscopies are very much on the list of preventive services that are supposed to be available at no out-of-pocket cost to patients. So there really shouldn’t even have been a bill. How much was the bill and what was it for?
Liss: Yeah. So their insurance company paid for the screening, but there was a separate $600 charge for something called “surgical trays.” Supplies you’d expect to be covered.
Rovner: Yeah. It’s like saying, “We’re going to charge you rent for lying on our table.”
Liss: Exactly.
Rovner: Chantal Panozzo knew that there shouldn’t be a charge. After getting no good explanation from her insurer or the gastroenterology practice, she went to complain. She went pretty much everywhere she could, right?
Liss: Yeah. Chantal is a savvy consumer, and she was furious. She lodged an appeal with her insurer, she filed a formal complaint with state regulators in Illinois, and she wrote to her elected officials.
Rovner: So what eventually happened?
Liss: She won, but she’ll tell you she did not feel victorious. Her insurer waived the bills for her and her husband, and they didn’t owe anything, but it was a months-long slog. I think seven months in total.
Rovner: Just to be clear, it was actually the insurer that she appealed to, and she won that appeal.
Liss: Yeah. I think part of what helped push that appeal along was her complaint to the Illinois Department of Insurance.
Rovner: So, doing all of those things apparently helped. It turns out that the couple uncovered quite the loophole in the preventive services mandate. What is that and how can others avoid falling into the same trap?
Liss: Yeah. Under the law, the insurer bears the legal burden to pay for preventative care. There’s no requirement on providers to bill a certain way. So I think as we tell all our folks who read and listen to our “Bill of the Month” series, never pay the first bill. Wait until you get your explanation of benefits, and if something doesn’t feel right, ask questions.
Rovner: So basically, people can go in and get care that they expect and should be free and get random charges, and they can complain about those, right?
Liss: Exactly. And I think Chantal’s example shows sometimes you have to fight so hard and for so long to get something waived that you shouldn’t have been charged for to begin with. It’s maddening and it ticks people off.
Rovner: And if all else fails, you can send your bill to us.
Liss: Yes, please do.
Rovner: Sam Liss, thank you very much.
Liss: Thanks.
Rovner: OK, we’re back. It’s time for our extra-credit segment. That’s when we each recommend a story we read this week we think you should read, too. As always, don’t worry if you miss it. We will post the links on the podcast page at kffhealthnews.org and in our show notes on your phone or other mobile device. Joanne, you have my favorite this week, why don’t you go first?
Kenen: I told Julie that Elmo didn’t want her to get sad if I was going to do this one, and she didn’t. I’m sure almost everybody saw the Elmo phenomenon this week. The particular story that I’m referring to is by Callie Holtermann in The New York Times, “Elmo Asked an Innocuous Question.” And then there’s this wonderful sub-headline, “Elmo was not expecting it to open a yawning chasm of despair.” Elmo tweeted or X’ed, whatever you call it … I mean, it wasn’t really Elmo, it was his human. Elmo is just checking in, “How is everybody doing?” There were tens of thousands of views. Last time I looked, there were more than 16,000 responses. I did not read all 16,000, but people really are not happy. And they told Elmo that. It just became this sort of mass confessional to Elmo of all the things that people were feeling despair about. And then Elmo ended up saying something like, “Wow, Elmo is glad he asked.” So I don’t know if Elmo has now become our national shrink, but to a certain extent this week, he was.
Rovner: Absolutely. Sarah?
Karlin-Smith: I looked at a piece from The Texas Tribune about not quite an amazing topic, maybe. The “Texas Attorney General Requests Transgender Youths’ Patient Records From Georgia Clinic,” by Madaleine Rubin. It basically looks at a trend where Texas seems to be trying to not only control what is happening to the care of transgender children within their state, but trying to maybe intimidate or prevent care from happening out of state by going after telehealth providers, but maybe even trying to request records related to people that have traveled outside of the state to get care because they can’t get it in the state. It reminds me a bit of some of what some of these states are also trying to do in the abortion space as well, but raises interesting questions about whether the state really has the authority to interfere here and so forth.
Rovner: Yeah, Texas is obviously fighting this border issue, too, with the federal government. So Texas is trying to basically see how far it can press its authority, in general. Sandhya?
Raman: My pick this week is called “Community Health Centers Serve 1 in 11 Americans. They’re a Safety Net Under Stress.” It’s from Devi Shastri at The AP. I just thought it was a great look at some of the challenges, some new, some evergreen for the 1,400 federal community health centers that provide medical care, social services, and so much for so many folks in the country. It just looks at some of the issues. In Congress, there’s always the periodic federal funding drama of just, “When will community health centers get funded?” And, “They can’t long-term plan on that.” That and just how the staffing concerns, whether it’s money or quality of life, or just how they can address new health equities and things like that.
Rovner: It was a really good story. My extra credit this week is from ProPublica. It’s a coda to a series of stories that they’ve been working on, and we’ve been talking about over the past several years, after reporters at our fellow nonprofit newsroom helped uncover serious defects in the CPAP breathing machines manufactured by Philips Respironics, and the company’s failure to report complaints about the foam in those machines crumbling and getting into patient’s lungs. The company finally issued a recall. Then, apparently, the replacement foam also started to deteriorate, which also became a subject of the series. Now the GAO is investigating the FDA’s oversight of medical devices, and a federal criminal probe is being sought for Philips. And now, at least, the company will stop selling the machines in the United States. So journalism works, particularly when reporters keep at it. And boy, did they keep at it on this story.
OK, that is our show. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left a review; that helps other people find us, too. Special thanks, as always, to our technical guru, Francis Ying, and our editor, Emmarie Huetteman. As always, you can email us your comments or questions. We’re at whatthehealth@kff.org, or you can still find me at X, @jrovner, or @julierovner at Bluesky and @julie.rovner at Threads. Joanne, where are you hanging out these days?
Kenen: I’m mostly on Threads @joannekenen1.
Rovner: Sarah?
Karlin-Smith: I am @SarahKarlin or @sarahkarlin-smith.
Rovner: Sandhya?
Raman: I’m still with X and on Bluesky, @Sandhya@Writes.
Rovner: We will be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 8 months ago
Courts, Health Care Costs, Medicare, Multimedia, Pharmaceuticals, States, Abortion, Drug Costs, KFF Health News' 'What The Health?', Misinformation, Podcasts, Prescription Drugs, Women's Health
Surge in Syphilis Cases Leads Some Providers to Ration Penicillin
When Stephen Miller left his primary care practice to work in public health a little under two years ago, he said, he was shocked by how many cases of syphilis the clinic was treating.
For decades, rates of the sexually transmitted infection were low. But the Hamilton County Health Department in Chattanooga — a midsize city surrounded by national forests and nestled into the Appalachian foothills of Tennessee — was seeing several syphilis patients a day, Miller said. A nurse who had worked at the clinic for decades told Miller the wave of patients was a radical change from the norm.
What Miller observed in Chattanooga is reflective of a trend that is raising alarm bells for health departments across the country.
Nationwide, syphilis rates are at a 70-year high. The Centers for Disease Control and Prevention said Jan. 30 that 207,255 cases were reported in 2022, continuing a steep increase over five years. Between 2018 and 2022, syphilis rates rose about 80%. The epidemic of sexually transmitted infections — especially syphilis — is “out of control,” said the National Coalition of STD Directors.
The surge has been even more pronounced in Tennessee, where infection rates for the first two stages of syphilis grew 86% between 2017 and 2021.
But this already difficult situation was complicated last spring by a shortage of a specific penicillin injection that is the go-to treatment for syphilis. The ongoing shortage is so severe that public health agencies have recommended that providers ration the drug — prioritizing pregnant patients, since it is the only syphilis treatment considered safe for them. Congenital syphilis, which happens when the mom spreads the disease to the fetus, can cause birth defects, miscarriages, and stillbirths.
Across the country, 3,755 cases of congenital syphilis were reported to the CDC in 2022 — that’s 10 times as high as the number a decade before, the recent data shows. Of those cases, 231 resulted in stillbirth and 51 led to infant death. The number of cases in babies swelled by 183% between 2018 and 2022.
“Lack of timely testing and adequate treatment during pregnancy contributed to 88% of cases of congenital syphilis,” said a report from the CDC released in November. “Testing and treatment gaps were present in the majority of cases across all races, ethnicities, and U.S. Census Bureau regions.”
Hamilton County’s syphilis rates have mirrored the national trend, with an increase in cases for all groups, including infants.
In November, the maternal and infant health advocacy organization March of Dimes released its annual report on states’ health outcomes. It found that, nationwide, about 15.5% of pregnant people received care beginning in the fifth month of pregnancy or later — or attended fewer than half the recommended prenatal visits. In Tennessee, the rate was even worse, 17.4%.
But Miller said even those who attend every recommended appointment can run into problems because providers are required to test for syphilis only at the beginning of a pregnancy. The idea is that if you test a few weeks before birth, there is time to treat the infection.
However, that recommendation hinges on whether the provider suspects the patient was exposed to the bacterium that causes syphilis, which may not be obvious for people who say their relationships are monogamous.
“What we found is, a lot of times their partner was not as monogamous, and they were bringing it into the relationship,” Miller said.
Even if the patient tested negative initially, they may have contracted syphilis later in pregnancy, when testing for the disease is not routine, he said.
Two antibiotics are used to treat syphilis, the injectable penicillin and an oral drug called doxycycline.
Patients allergic to penicillin are often prescribed the oral antibiotic. But the World Health Organization strongly advises pregnant patients to avoid doxycycline because it can cause severe bone and teeth deformities in the infant.
As a result, pregnant syphilis patients are often given penicillin, even when they’re allergic, using a technique called desensitization, said Mark Turrentine, a Houston OB-GYN. Patients are given low doses in a hospital setting to help their bodies get used to the drug and to check for a severe reaction. The penicillin shot is a one-and-done technique, unlike an antibiotic, which requires sticking to a two-week regimen.
“It’s tough to take a medication for a long period of time,” Turrentine said. The single injection can provide patients and their clinicians peace of mind. “If they don’t come back for whatever reason, you’re not worried about it,” he said.
The Metro Public Health Department in Nashville, Tennessee, began giving all nonpregnant adults with syphilis the oral antibiotic in July, said Laura Varnier, nursing and clinical director.
Turrentine said he started seeing advisories about the injectable penicillin shortage in April, around the time the antibiotic amoxicillin became difficult to find and physicians were using penicillin as a substitute, potentially precipitating the shortage, he said.
The rise in syphilis has created demand for the injection that manufacturer Pfizer can’t keep up with, according to the American Society of Health-System Pharmacists. “There is insufficient supply for usual ordering,” the ASHP said in a memo.
Even though penicillin has been around a long time, manufacturing it is difficult, largely because so many people are allergic, said Erin Fox, associate chief pharmacy officer for the University of Utah health system and an adjunct professor at the university, who studies drug shortages.
“That means you can’t make other drugs on that manufacturing line,” she said. Only major manufacturers like Pfizer have the resources to build and operate such a specialized, cordoned-off facility. “It’s not necessarily efficient — or necessarily profitable,” Fox said.
In a statement, Pfizer confirmed the amoxicillin shortage and surge in syphilis increased demand for injectable penicillin by about 70%. Representatives said the company invested $38 million in the facility that produces this form of penicillin, hiring more staff and expanding the production line.
“This ramp up will take some time to be felt in the market, as product cycle time is 3-6 months from when product is manufactured to when it is available to be released to customers,” the statement reads. The company estimated the shortage would be significantly alleviated by spring.
In the meantime, Miller said, his clinic in Chattanooga is continuing to strategize. Each dose of injectable penicillin can cost hundreds of dollars. Plus, it has to be placed in cold storage, and it expires after 48 months.
Even with the dramatic increase in cases, syphilis is still relatively rare. More than 7 million people live in Tennessee, and in 2019, providers statewide reported 683 cases of syphilis.
Health departments like Miller’s treat the bulk of syphilis patients. Many patients are sent by their provider to the health department, which works with contact tracers to identify and notify sexual partners who might be affected and tests patients for other sexually transmitted infections, including HIV.
“When you diagnose in the office, think of it as just seeing the tip of the iceberg,” Miller said. “You need a team of individuals to be able to explore and look at the rest of the iceberg.”
This story is part of a partnership that includes WPLN, NPR, and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 8 months ago
Pharmaceuticals, Public Health, Rural Health, States, CDC, Sexual Health, Tennessee
KFF Health News' 'What the Health?': Health Enters the Presidential Race
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
Based on the results of the first-in-the-nation primary in New Hampshire, it appears more likely than ever before that the 2024 presidential election will be a rerun of 2020: Joe Biden versus Donald Trump. And health is shaping up to be a key issue.
Trump is vowing — again — to repeal the Affordable Care Act, which is even more popular than it was when Republicans failed to muster the congressional votes to kill it in 2017. Biden is doubling down on support for contraception and abortion rights.
And both are expected to highlight efforts to rein in the cost of prescription drugs.
This week’s panelists are Julie Rovner of KFF Health News, Alice Miranda Ollstein of Politico, Anna Edney of Bloomberg News, and Jessie Hellmann of CQ Roll Call.
Panelists
Alice Miranda Ollstein
Politico
Anna Edney
Bloomberg
Jessie Hellmann
CQ Roll Call
Among the takeaways from this week’s episode:
- Trump had a strong showing in the New Hampshire GOP primary. But Biden may be gathering momentum himself from an unexpected source: Drug industry lawsuits challenging his administration’s Medicare price negotiation plan could draw attention to Biden’s efforts to combat rising prescription drug prices, a major pocketbook issue for many voters.
- Biden’s drug pricing efforts also include using the government’s so-called march-in rights on pharmaceuticals, which could allow the government to lower prices on certain drugs — it’s unclear which ones. Meanwhile, Sen. Bernie Sanders of Vermont is calling on his committee to subpoena the CEOS of two drugmakers in the latest example of lawmakers summoning Big Pharma executives to the Hill to answer for high prices.
- More than a year after the Supreme Court overturned the constitutional right to an abortion, abortion opponents gathered in Washington, D.C., for the March for Life rally, looking now to continue to advance their priorities under a future conservative presidency.
- One avenue that abortion opponents are eying is the 19th-century Comstock Act, which could not only prohibit the mailing of abortion pills to patients, but also prevent them from being mailed to clinics and medical facilities. Considering the abortion pill is now used in more than half of abortions nationwide, it would amount to a fairly sweeping ban.
- And state legislators continue to push more restrictive abortion laws, targeting care for minors and rape exceptions in particular. The ongoing quest to winnow access to the procedure amid public reservations reflected in polling and ballot initiatives highlights that, for at least some abortion opponents, fetuses are framed as an oppressed minority whose rights should not be subject to a majority vote.
Also this week, Rovner interviews Sarah Somers, legal director of the National Health Law Program, about the potential effects on federal health programs if the Supreme Court overturns a 40-year-old precedent established in the case Chevron USA v. Natural Resources Defense Council.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: Health Affairs’ “‘Housing First’ Increased Psychiatric Care Office Visits and Prescriptions While Reducing Emergency Visits,” by Devlin Hanson and Sarah Gillespie.
Alice Miranda Ollstein: Stat’s “The White House Has a Pharmacy — And It Was a Mess, a New Investigation Found,” by Brittany Trang.
Anna Edney: The New Yorker’s “What Would It Mean for Scientists to Listen to Patients?” by Rachael Bedard.
Jessie Hellmann: North Carolina Health News’ “Congenital Syphilis — An Ancient Scourge — Claimed the Lives of Eight NC Babies Last Year,” by Jennifer Fernandez.
Also mentioned on this week’s podcast:
Stat’s “Pharma’s Attack on Medicare Drug Price Negotiation Might Benefit Biden,” by John Wilkerson.
click to open the transcript
Transcript: Health Enters the Presidential Race
KFF Health News’ ‘What the Health?’Episode Title: Health Enters the Presidential RaceEpisode Number: 331Published: Jan. 25, 2024
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello, and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News, and I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, Jan. 25, at 10 a.m. As always, news happens fast, and things might’ve changed by the time you hear this. So here we go. We are joined today via video conference by Alice Miranda Ollstein of Politico.
Alice Miranda Ollstein: Good morning.
Rovner: Jessie Hellmann of CQ Roll Call.
Jessie Hellmann: Hi there.
Rovner: And Anna Edney of Bloomberg News.
Anna Edney: Hello.
Rovner: Later in this episode we’ll have my interview with Sarah Somers of the National Health Law Program. She’s going to explain what’s at risk for health care if the Supreme Court overturns the Chevron doctrine, and if you don’t know what that is, you will. But first, this week’s news. We’re going to start this week with politics. To absolutely no one’s surprise, Donald Trump won the first-in-the-nation New Hampshire primary, and even though he wasn’t even on the ballot, because Democrats no longer count New Hampshire as first, President [Joe] Biden handily won a write-in campaign.
Since it seems very likely at this point that the November ballot will pit Trump versus Biden once again, I thought we’d look, briefly at least, at both of their health agendas for now. Trump has once again vowed to try and repeal the Affordable Care Act, which not only didn’t go well in 2017, we learned this week that the federal marketplace enrolled a record 21.3 million people for this year. In 2017, that number was 12.2 million. Not to mention there are now a half a dozen more states that have expanded Medicaid to low-income childless adults.
So with so many more millions of Americans getting coverage via Obamacare, even if Trump wants to repeal and replace it, is there any chance Republicans would go along, even if he wins back majorities in the House and the Senate? They have seemed rather unwilling to reopen this box of worms.
Edney: I mean, certainly, I think that currently they’re unwilling. I don’t want to pretend that I know what the next several months will hold until November, but even before they’re willing or not, what would the plan be? We never saw one, and I don’t anticipate there would be any sort of real plan, particularly if it’s the Trump White House itself having to put the plan together to repeal Obamacare.
Rovner: Yes. How many times did he promise that “we’ll have a plan in two weeks” throughout most of his administration? Alice, you were saying?
Ollstein: Yes. I think what we should be thinking about, too, is this can happen not through Congress. There’s a lot of President Trump could do theoretically through the executive branch, not to repeal Obamacare, but to undermine it and make it work worse. They could slash outreach funding, they could let the enhanced tax credit subsidies expire — they’re set to expire next year. That would also be on Congress. But a president who is opposed to it could have a role in that; they could slash call center assistance. They could do a lot. So I think we should be thinking not only about could a bill get through Congress, but also what could happen at all of the federal agencies.
Rovner: And we should point out that we know that he could do some of these things because he did them in his first term.
Ollstein: He did them the first time, and they had an impact. The uninsured rate went up for the first time under Trump’s first term, for the first time since Obamacare went into effect. So it can really make a difference.
Rovner: And then it obviously went down again. But that was partly because Congress added these extra subsidies and even the Republican Congress required people to stay on Medicaid during the pandemic. Well, I know elsewhere, like on abortion, Trump has been all over the place, both since he was in office and then since he left office. And then now, Alice, do we have any idea where he is on this whole very sensitive abortion issue?
Ollstein: He has been doing something very interesting recently, which is he’s sort of running the primary message and the general message at the same time. So we’re used to politicians saying one thing to a primary audience. These are the hard-core conservatives who turn out in primaries and they want to hear abortion is going to be restricted. And then the general audience — look at how all of these states have been voting — they don’t want to hear that. They want to hear a more moderate message and so Trump has been sort of giving both at once. He’s both taking credit for appointing the Supreme Court justices, who overturned Roe v. Wade. He has said that he is pro-life, blah, blah, blah. But he has also criticized the anti-abortion movement for going too far in his view. He criticized Ron DeSantis’ six-week ban for going too far. He has said that any restrictions need to have exemptions for rape and incest, which not everyone in the movement agrees with. A lot of people disagree with that in the anti-abortion movement. And so it has been all over the place.
But his campaign is in close contact with a lot of these groups and the groups are confident that he would do what they want. So I think that you have this interesting tension right now where he is saying multiple mixed messages.
Rovner: Which he always does, and which he seems to somehow get away with. And again, just like with the ACA, we know that all of these things that he could do just from the executive branch about reproductive health, because he did them when he was president the first time. Meanwhile, President Biden, in addition to taking a victory lap on the Affordable Care Act enrollment, is doubling down on abortion and contraception, which is pretty hard because, first, as executive, he doesn’t have a ton of power to expand abortion rights the way Trump would actually have a lot of power to contract them.
And, also, because as we know, Biden is personally uncomfortable with this issue. So Alice, how well is this going to work for the Biden administration?
Ollstein: So what was announced is mostly sort of reiterating what is already the law, saying we’re going to do more to educate people about it and crack down on people who are not following it. So this falls into a few different buckets. Part of it is Obamacare’s contraception mandate. There have been lots of investigations showing that a lot of insurers are denying coverage for contraceptives they should be covering or making patients jump through hoops. And so it’s not reaching the people it should be reaching. And so they’re trying to do more on that front.
And then, on the abortion front, this is mostly in this realm of abortions in medical emergencies. They’re trying to educate patients on “you can file this complaint if you are turned away.” Of course, I’m thinking of somebody experiencing a medical emergency and needing abortion and being turned away, and I don’t think “I’m going to file an EMTALA [Emergency Medical Treatment and Active Labor Act] complaint with the federal government and hope that they do something” is maybe the first thing on their mind. But the new executive order also includes education for providers and hospitals on their obligations.
This is also something a Trump administration could completely change. They could come in and say, “Forget that guidance. Here’s our guidance, which is no abortions in these circumstances.” So this is a really sensitive issue, but I think that the Biden campaign has seen how people have been voting over the last two years and feels that this is a really good message for them to do something on.
Rovner: Meanwhile, one issue both Republicans and Democrats are trying to campaign on is bringing down the cost of prescription drugs. Stat News has a story this week suggesting that all the lawsuits against the Medicare drug negotiation program could actually help Biden with voters because it shows he’s going after Big Pharma. Frankly, it could also tell voters that the Biden administration actually did something to challenge Big Pharma. Polls show most people have no idea, but Trump can point to lots of lawsuits over things he tried to do to Big Pharma.
Does one or the other of them have an advantage here, Anna? I mean, I know they’re going in different directions, but when you sort of boil it into campaign-speak, it’s going to sound pretty similar, right?
Edney: I think that that’s true, but one of the differences is, at least currently, what Biden’s done and doing some price negotiation through Medicare so far for 10 drugs under his administration is going forward. And you can name the drugs, name the prices, talk about it a little bit more specifically. What Trump ran up against was the lawsuits not falling in his favor. So he wanted more transparency as far as the drug companies having to say the price of their drugs in TV ads, and that wasn’t able to happen. And also reference pricing, so that the prices would be benchmarked to other countries. And certainly that never went forward either. And Trump really used the going after pharma hard in the last campaign, I would say, in 2016. And it worked in the beginning, and you would see the stock of these companies start going down the second he said pharmaceutical companies are getting away with murder or whatever big comment he was making. But it eventually lost any real effect because there didn’t seem to be plans to do anything drastic.
He talked about potentially doing negotiation, like is happening currently, but then that never came to fruition once he was in office. So I don’t know if that will come across to voters, but certainly the pharma industry doesn’t seem to be as afraid of Trump as what Biden’s doing right now.
Rovner: Jessie, I know Congress is still working on this PBM [pharmacy benefit managers] transparency, big bill. Are we getting any closer to anything? I think members of Congress would also like to run on being able to say they’ve done something about prescription drug prices.
Hellmann: I was just talking to [Sen.] Chuck Grassley [R-Iowa] about this because he is the “OG PBM hater.” And he was like, “Why is nothing happening?” He was just very frustrated. There are several bills that have passed House and Senate committees, and so I think, at this point, it’s just a matter of cobbling them all together, finding ways to pay for things. And since there’s also so many other health care things that people want to get done, it’s a matter of “Do we have enough money to pay for everything? What’s going to save money? What’s going to cost money?”
There’s also these health care transparency measures that Congress is looking at. There’s this site-neutral hospital payments thing that could be a money saver. So I think there’s just a lot going on in trying to figure out how it all fits together. But PBMs, I could definitely see them doing something this year.
Rovner: Sometimes, I mean, often it’s like you can’t get things onto the agenda. In this case, it sounds like there’s lots of things on the agenda, but they’re going to need to pay for all of them and they’re going to fight over the few places where they could presumably get some savings.
Edney: I was going to say, I saw that Grassley and some other senators wrote the Federal Trade Commission because they are due for a report on PBMs they’ve been working on for about a year and a half. And I think that the senators who want to go after PBMs are kind of looking for that sort of backup and that deep dive into the industry to make those statements about cost savings and what this would do for pharmaceutical prices.
Rovner: Well, to ratchet this up one more step, the Biden administration has proposed a framework for when march-in rights might be used. Is this the real deal or a threat to get pharma to back down on complaints about the Medicare price negotiations? Anna, why don’t you explain what march-in rights are?
Edney: March-in rights, which have never been used on a pharmaceutical company, were something that were put into law — I think it was around 1980 with the Bayh-Dole Act — and what it allows the government to do is say we invested a ton of money, either through giving money to university research or in the company itself, to do the very basic science that got us to this breakthrough that then the company took across the finish line to get a drug on the market. But usually, I think the main reason you might use it is because then the company does nothing with it.
Say they bought it up and it could be a competitor to one of their drugs, so they don’t use it. But it seems like it could also be used if the price is prohibitive, that it’s something that’s really needed, but Americans aren’t getting access to it. And so the government would be able to take that patent back and lower the price on the drug. But I haven’t heard a specific drug that they want to use this on. So I don’t know if they’re serious about using the march-in rights.
There is a request for information to find out how people feel about this, how it might affect the industry. The argument being that it could hamper the innovation, but we hear that a lot from the pharmaceutical industry as well. So unclear if that’s a true defense to not using march-in rights.
Rovner: Although march-in rights are a pretty big gun. There’s a reason they’ve never been used. I’ve seen them … lawmakers sometimes trot it out kind of as a cudgel, but I’ve never … the only time I think I saw them come close was after the anthrax scare, right after 9/11, when there was potentially a shortage of the important antibiotic needed for that. There was muttering about this, but then I think the drug company decided on its own to lower the price, which got us over that.
Well, yet another tack is being pursued by Sen. Bernie Sanders, chairman of the Senate Health Committee. He’s going to make the committee vote next week on whether to subpoena the CEOs of Johnson & Johnson and Merck to require them to “provide testimony about why their companies charge substantially higher prices for medicine in the U.S. compared to other countries.” Well, we all know the answer to that. Other countries have price controls and the U.S. does not. So is this a stunt or not? And is he even going to get the rest of the committee to go along with the subpoena?
Edney: This wouldn’t be the first hearing on high drug prices pulling in CEOs. And it’s so opaque that you never get an answer. You never get something … I mean, certainly, they’ll blame PBMs and talk about that, and the finger-pointing will go somewhere else, but you never have some aha insight moment. So when the CEOs are coming in, it does feel a bit more like a show. And Bernie Sanders, the ones he wants to subpoena are from companies that are suing the Biden administration.
So there’s talk about whether that’s sort of a bit of a revenge him for that as well. I don’t know what exactly he would expect to hear from them that would change policy or what legislation they’re trying to work out by having this hearing.
Rovner: For an issue that everybody cares about, high drug prices. It sure has been hard to figure out a way into it for politicians.
Ollstein: We have seen public shaming, even without legislation behind it, can have a difference. I think we’ve seen that on the insulin front. And so I think it’s not completely a fool’s errand here, what Bernie’s trying to do. It will be interesting to see if the rest of the committee goes along with it. There’s been some tensions on the committee. There’s been bipartisan support for some of his efforts, and then others — less on the health front, I think more on the labor front — you’ve had a lot of pushback from the Republican members, and so it’ll be very telling.
Rovner: I was actually in the room when the tobacco industry CEOs came to testify at the House Energy and Commerce Committee, and that was pretty dramatic, but I feel like that was a very different kind of atmosphere than this is. I know everybody’s been trying to repeat that moment for — what is it? — 25, 30 years now. It was in the early 1990s, and I don’t think anybody really successfully has, but they’re going to keep at it.
All right, well, let us turn to abortion. Last Saturday would have been the 51st anniversary of Roe v. Wade, and the day before was the annual March for Life, the giant annual anti-abortion demonstration that used to be a march to the Supreme Court to urge the justices to overrule Roe. Well, that mission has been accomplished. So now what are their priorities, Alice?
Ollstein: Lots of things. And a lot of the effort right now is going towards laying the groundwork, making plans for a potential second Trump administration or a future conservative president. They see not that much hope on the federal level for their efforts currently, with the current president and Congress, but they are trying to do the prep work for the future. They want a future president to roll back everything Biden has done to expand abortion access. That includes the policies for veterans and military service members. That includes wider access to abortion pills through the mail and dispensing at retail pharmacies, all of that.
So they want to scrap all of that, but they also want to go a lot further and are exploring ways to use a lot of different agencies and rules and bureaucratic methods and funding mechanisms to do this, because they’re not confident in passing a bill through Congress. We’ve seen Congress not able to do that even under one-party rule in either direction. And so they’re really looking at the courts, which are a lot more conservative than they were several years ago.
Rovner: Largely thanks to Trump.
Ollstein: Exactly, exactly. So the courts, the executive branch, and then, of course, more efforts at the state level, which I know we’re going to get into.
Rovner: We are. Before that, though, one of the things that keeps coming up in discussions about the anti-abortion agenda is something called the Comstock Act. We have talked about this before, although it’s been a while, but this is an 1873 law, which is still on the books, although largely unenforced, that banned the mailing of anything that could be used to aid in an abortion, among other things. Could an anti-abortion administration really use Comstock to basically outlaw abortion nationwide?
I mean, even things that are used for surgical abortion tend to come through … it’s not just the mail, it’s the mail or FedEx or UPS, common carrier.
Ollstein: Yes. So this is getting a lot more attention now and it is something anti-abortion groups are absolutely calling for, and people should know that this wouldn’t only prohibit the mailing of abortion pills to individual patients’ homes, which is increasingly happening now. This would prevent it from being mailed to clinics and medical facilities. The mail is the mail. And so because abortion medication is used in more than half of all abortions nationwide, it could be a fairly sweeping ban.
And so the Biden administration put out a memo from the Justice Department saying, “Our interpretation of the Comstock Act is that it does not prohibit the mailing of abortion pills.” The Trump administration or whoever could come in and say, “We disagree. Our interpretation is that it does.” Now, how they would actually enforce it is a big question. Are you going to search everyone’s mail in the country? Are you going to choose a couple of people and make an example out of them?
That’s what happened under the original Comstock Act. Back in the day, they went after a few high-profile abortion rights activists and made an example out of them. I think nailing them down on how it would be enforced is key here. And of course there would be tons of legal challenges and battles no matter what.
Rovner: Absolutely. Well, let us turn to the states. It’s January, which is kind of “unveil your bills” time in state legislatures, and they are piling up. In Tennessee, there’s a bill that would create a Class C felony, calling for up to 15 years in prison, for an adult who “recruits, harbors or transports a pregnant minor out of state for an abortion.” There’s a similar bill in Oklahoma, although violators there would only be subject to five years in prison.
Meanwhile, in Iowa, Republican lawmakers who are writing guidelines for how to implement that state’s six-week ban, which is not currently in effect, pending a court ruling, said that the rape exception could only be used if the rape is “prosecutable,” without defining that word. Are these state lawmakers just failing to read the room or do they think they are representing what their voters want?
Edney: I don’t really know. I think clearly there are a lot of right-wing Republicans who are elected to office and feel that they have a higher calling that doesn’t necessarily reflect what their constituents may or may not want, but more is that they know better. And I think that that could be some of this, because certainly the anti-abortion bills or movements have been rejected by voters in places you might not exactly expect it.
Rovner: It feels like we’re getting more and more really “out there” ideas on the anti-abortion side at the same time that we’re getting more and more ballot measures of voters in both parties wanting to protect abortion rights, at least to some extent.
Ollstein: And I think going off what Anna said, I think that anti-abortion leaders, including lawmakers, are being more upfront now, saying that they don’t believe that this should be something that the democratic process has a voice in. The framing they use is that fetuses are an oppressed minority and their rights should not be subject to a majority vote. That’s their framing, and they’re being very upfront saying that these kinds of ballot referendums shouldn’t be allowed, and that states that do allow them should get rid of that. We’ll see if that happens. There are obviously lots of attempts to thwart specific state efforts to put abortion on the ballot. There are lawsuits pending in Nevada and Florida. There are attempts to raise the signature threshold, raise the vote threshold, just make it harder to do overall. But I found it very interesting and a pretty recent development that folks are coming out and saying the quiet part out loud. Saying, “We don’t believe The People should be able to decide this.”
Rovner: Well, obviously not an issue that is going away anytime soon. All right, well that is this week’s news. Now we will play my interview with Sarah Somers, and then we will come back and do our extra credits.
I am pleased to welcome to the podcast Sarah Somers, legal director of the National Health Law Program. She’s going to explain, in English hopefully, what’s at stake in the big case the Supreme Court heard earlier this month about herring fishing. Sarah, welcome to “What the Health?”
Sarah Somers: Thank you for having me, Julie. I’m glad to be here.
Rovner: So this case, and I know it’s actually two cases together, is really about much more than herring fishing, right? It seems to be about government regulation writ large.
Somers: That’s right. The particular issue in the case is about a national marine fisheries regulation that requires herring fishing companies to pay for observers who are on board — not exactly an issue that’s keeping everyone but herring fishermen up at night. And the fishing company challenged the rule, saying that it wasn’t a reasonable interpretation of the statute. But what they also asked the court to do was to overrule a Supreme Court case that requires courts to defer to reasonable agency interpretations of federal statutes. That’s what’s known as “Chevron deference.”
Rovner: And what is Chevron deference and why is it named after an oil company?
Somers: Why aren’t we talking about oil now? Yes, Chevron deference is the rule that says that courts have to defer to a reasonable agency interpretation of a federal statute. So, under Chevron, there’s supposed to be a two-step process when considering whether, say, a regulation is a reasonable interpretation. They say, “Does the statute speak directly to it?” So in this case, did the statute talk about whether you have to pay for observers on herring boats? It didn’t.
So the next question was, if it doesn’t speak directly to it or if it’s ambiguous or unclear, then the court should defer to a reasonable interpretation of that statute. And what’s reasonable depends on what the court determines are sort of the bounds of the statute, whether the agency had evidence before it that supported it, whether it showed the proper deliberation and expertise.
Rovner: One of the reasons that regulations are sometimes 200 pages long, right?
Somers: Exactly. And sometimes courts do say, “You know what? The statute spoke right to this. We don’t have to go any further. We know what Congress wanted.” Other times they take a step further. And the reason it’s called Chevron is it’s named after a case that was decided 40 years ago in 1984 during the Reagan administration, and it was Chevron Inc. USA v. the Natural Resources Defense Council. That case was about a regulation interpreting the Clean Air Act and about regulating air pollution.
Rovner: So, as you point out, you helped write one of the amicus briefs in the case about what overturning Chevron would mean for health care. It’s not just about herring fishing and Clean Air Act. Can you give us the CliffsNotes version of what it would mean for health care?
Somers: One of the purposes of our amicus brief was just to give another angle on this, because we were talking a lot about regulations in the context of air pollution, clean water, and the environment, but it touches so many other things, and this is just one aspect of it. So this brief, which we authored along with the American Cancer Society Action Network, and a Boston law firm called Anderson Kreiger, was signed by other health-oriented groups: the American Lung Association, American Heart Association, Campaign for Tobacco-Free [Kids], and then the American Academy of Pediatrics, American Academy of Public Health.
You get the picture. These are all groups that have a vested interest in programs of the Department and Health and Human Services. The brief talks about regulations promulgated by the Centers for Medicare & Medicaid Services. I’m going to call them CMS for short when we’re talking. And CMS is responsible for regulating the vast and complex Medicare and Medicaid programs. And, as you know, Medicare and Medicaid cover more than half of the population and touch the lives of almost everyone, regulating hospitals, some aspects of insurance, some aspects of practice of medicine.
You can’t escape the consequences of problems with these programs. And so that’s why the agency … Congress specifically gave HHS and CMS the power to regulate all of the issues in its purview. So that already have the power, and so the question is whether they use it wisely. We are arguing in this brief that for 40 years it’s worked just fine. That Congress has set the outer limits and been content to let the agency determine the specifics of these programs to fill in the gaps, as one Supreme Court case said. And this has implications for how hospitals operate, how insurance programs operate, and whether they operate smoothly.
And in our brief, we’re not really arguing for or against a particular interpretation or either for or against what the agency says. It’s just a matter of stability and certainty. The agency has the expertise, has the time, has the resources, and has the duty to figure out what these particular terms and statutes mean and how the programs should work. Just two examples we gave in the brief of the kind of issues that the agency should be determining are: What’s the definition of geographic area in the Medicaid Act for the purpose of setting hospital wages?
If your listeners are still listening, I hope, because that is boring, arcane, hyper-technical, and courts don’t have the expertise, much less the time, to do that. And CMS does. Or another question in a different area, whether feeding activities in a nursing home regulated by Medicaid: Are those nursing or nursing related services? The court’s not going to know. The courts doesn’t have expertise or time. And again, that’s what CMS is for.
So not only is this something that you need these interpretations in these rules to have the programs operate smoothly and consistently, and that’s the first part that’s important. But the second part is that you need consistency across the country. As you know well, there are hospital systems that operate across multi-states. There are Medicaid managed-care plans operating across multi-states. All aspects of health care is nationalized. If you have hundreds of district courts and courts of appeals coming up with different interpretations of these terms, you’re going to have a lot of problems. It’s not going to operate smoothly. So I heard some of the justices arguing, “Well, Congress just needs to do its job.”
Congress has obstacles to doing even the big, mega issues that are before them, these kinds of arcane specific issues. They don’t have the time or again, the expertise. That’s why they said, “CMS, you go do this.”
Rovner: When they were writing the Affordable Care Act, there were so many times in that legislation where it says, “The secretary shall” or “The secretary may.” It’s like, we’re going to punt all this technical stuff to HHS and let them do what they will.
Somers: Exactly. You figure out what the definition of a preventive service is, that’s not something that we are going to do. And there are also questions raised about is this … these unelected agency personnel, well, agencies — they are political appointees, and they also serve at the pleasure of the head of the agency. So they’re accountable to the executive branch and indirectly to the voters. The courts, at this point, once they’re on the court and the federal courts, they’re not accountable to the voters anymore. And so this would be a big shift of power towards the courts, and that is what we argued would be antithetical to the system working well.
Rovner: What would be an example of something that could get hung up in the absence of Chevron?
Somers: I thought that Justice [Ketanji Brown] Jackson, during the argument, gave a really good example. Under the Food and Drug Administration’s power to regulate new drugs and determining what is an adequate and well-controlled investigation. The idea of courts, every single drug that’s challenged in every single forum, having to delve into what that means without deference to the agency would be just a recipe for chaos, really.
Rovner: So some people have argued that Chevron is already basically gone, as far as the Supreme Court is concerned, that it’s been replaced by the major questions doctrine, which is kind of what it sounds like. If a judge thinks a question is major, and they will assume that the Congress has not delegated it to the agency to interpret. So what difference would it make if the court formally overturned Chevron or not here? I guess what you’re getting at is that we’re more worried about the lower courts at this point than the Supreme Court, right?
Somers: That’s right. The Supreme Court has not cited Chevron in something like 15 years. And they talked about that in the argument, but it’s for the lower courts. The lower courts still follow it. It is still very commonly cited and gives them a lot of guidance not to have to decide these issues in the first instance. It’s true that the major questions doctrine — and there are other threats to the power of the administrative agencies, and we should all be concerned about them. But this one is really the grease that keeps the machine going and keeps these systems going. And throwing all that up in the air would make a big difference. If only because the question in all of these Chevron cases, and so many of them was not the ultimate issue — about whether the regulation was a good policy — but the question was, was the statute ambiguous or not? And so that’s the part that would be up in the air and everyone can go back and re-litigate these, including the big interests that have a lot of time and resources to devote to litigation. And that would cause a great deal of uncertainty, a lot of disruption, and a lot of problem for the courts and for all the entities that function under these systems.
Rovner: And that’s a really important point. It’s not just going forward. People who are unhappy with what a regulation said could go back, right?
Somers: Oh yeah. They could go back. They could go to different courts. We’ve seen how litigants can forum-shop. They can find a judge that they think is going to be sympathetic to their argument and make a determination that affects the whole country.
Rovner: Well, we will be watching. Sarah Somers, thanks so much for joining us.
Somers: My pleasure. Thank you for having me.
Rovner: We are back, and it’s time for our extra-credit segment. That’s when we each recommend a story we read this week we think you should read, too. As always, don’t worry if you miss it. We will post the links on the podcast page at kffhealthnews.org and in our show notes on your phone or other mobile device. Jessie, you were the first to join in this week. Why don’t you tell us about your extra credit?
Hellmann: Yeah. Mine is from North Carolina Health News. They wrote about how congenital syphilis is killing babies in the state. They had eight cases of deaths last year — compared to a decade ago, they had one. So it’s something that’s been on the rise in North Carolina, but also nationwide, and it’s caused a lot of alarm among public health officials because it’s pretty preventable. It’s something that doesn’t need to happen, but the story is about what the state is doing to improve their outreach to pregnant people. They’re doing media campaigns, they’re trying to make sure that people are doing their prenatal care and just trying to stop this from happening. So I thought that was a good story. It’s definitely kind of an under-reported issue. It’s something that public health officials have been raising an alarm about for a while now, but there’s just not enough funding or attention on the issue.
Rovner: For all the arguing about abortion, there’s not been a lot of discussion about maternal and child health, which obviously appears to be the one place that both sides agree on. Anna.
Edney: Mine’s in The New Yorker by Rachael Bedard. It’s “What Would It Mean for Scientists to Listen to Patients?” And it’s interesting, it’s about two Yale researchers who are doing a long-covid study, but it’s unique in the sense that when the CDC or anyone else does a long-covid study, they typically are trying to say, “Here are the exact symptoms. We’re going to work with 12 of them.” Whereas we know long covid, it’s seemingly a much more expansive symptom list than that, but researchers really like to have kind of metrics to go by.
But what these Yale researchers are doing is letting all of that go and just letting anybody in this and talking to them. They’re holding monthly town halls with people who are in this, whoever wants to show up and come and just talk to them about what’s going on with them and trying to find out, obviously, what could help them. But they’re not giving medical advice during these, but just listening. And it just was so novel, and maybe it shouldn’t be, but I found it fascinating to read about and to get their reactions. And it’s not always easy for them. I mean, the patients get upset and want something to happen faster, but just that somebody is out there doing this research and including anybody who feels like they have long covid. It was really well-written too.
Rovner: It’s a really good story. Alice.
Ollstein: So I’m breaking my streak of extremely depressing, grim stories and sharing kind of a funny one, although it could have some serious implications. This is from Stat, and it’s from an inspector general report about how the White House pharmacy, which is run by basically the military, functioned under President Trump. And it functioned like sort of a frat house. There was no official medical personnel in charge of handing out the medications, and they were sort of handed out to whoever wanted them, including people who shouldn’t have been getting them. People were just rifling through bins of medications and taking what they wanted. These included pills like Ambien and Provigil, sort of uppers and downers in the common parlance. And so I think this kind of scrutiny on something that I didn’t even know existed. The White House pharmacy is pretty fascinating.
Rovner: It was a really, really interesting story. Well, I also have something relatively hopeful. My extra credit this week is a journal article from Health Affairs with the not-so-catchy headline “‘Housing First’ Increased Psychiatric Care Office Visits and Prescriptions While Reducing Emergency Visits,” by Devlin Hanson and Sarah Gillespie. And if they will forgive me, I would rename it, calling it maybe “Prioritizing Permanent Housing for Homeless People Provides Them a Better Quality of Life at Potentially Less Cost to the Public.”
It’s about a “Housing First” experiment in Denver, which found that the group that was given supportive housing was more likely to receive outpatient care and medications and less likely to end up in the emergency room. The results weren’t perfect. There was no difference in mortality between the groups that got supportive housing and the groups that didn’t. But it does add to the body of evidence about the use of so-called social determinants of health, and how medicine alone isn’t the answer to a lot of our social and public health ills.
OK. That is our show. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left us a review; that helps other people find us, too. Special thanks as always to our technical guru, Francis Ying, and our editor, Emmarie Huetteman. As always, you can email us your comments or questions. We’re at whatthehealth@kff.org, or you can still find me at X, @jrovner, or @julierovner at Bluesky or @julie.rovner at Threads. Anna, where are you these days?
Edney: Mostly just on Threads, so @anna_edneyreports.
Rovner: Alice?
Ollstein: @AliceOllstein.
Rovner: Jessie.
Hellmann: @jessiehellmann on Twitter.
Rovner: We will be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 9 months ago
Courts, Elections, Health Care Costs, Multimedia, Pharmaceuticals, Public Health, States, The Health Law, Abortion, Drug Costs, KFF Health News' 'What The Health?', New Hampshire, Podcasts, Women's Health
What the Health Care Sector Was Selling at the J.P. Morgan Confab
SAN FRANCISCO — Every year, thousands of bankers, venture capitalists, private equity investors, and other moneybags flock to San Francisco’s Union Square to pursue deals. Scores of security guards keep the homeless, the snoops, and the patent-stealers at bay, while the dealmakers pack into the cramped Westin St.
Francis hotel and its surrounds to meet with cash-hungry executives from biotech and other health care companies. After a few years of pandemic slack, the 2024 J.P. Morgan Healthcare Conference regained its full vigor, drawing 8,304 attendees in early January to talk science, medicine, and, especially, money.
1. Artificial Intelligence: Revolutionary or Not?
Of the 624 companies that pitched at the four-day conference, the biggest overflow crowd may have belonged to Nvidia, which unlike the others isn’t a health care company. Nvidia makes the silicon chips whose computing power, when paired with ginormous catalogs of genes, proteins, chemical sequences, and other data, will “revolutionize” drug-making, according to Kimberly Powell, the company’s vice president of health care. Soon, she said, computers will customize drugs as “health care becomes a technology industry.” One might think that such advances could save money, but Powell’s emphasis was on their potential for wealth creation. “The world’s first trillion-dollar drug company is out there somewhere,” she dreamily opined.
Some health care systems are also hyping AI. The Mayo Clinic, for example, highlighted AI’s capacity to improve the accuracy of patient diagnoses. The nonprofit hospital system presented an electrocardiogram algorithm that can predict atrial fibrillation three months before an official diagnosis; another Mayo AI model can detect pancreatic cancer on scans earlier than a provider could, said Matthew Callstrom, chair of radiology at the Mayo Clinic in Rochester, Minnesota.
No one really knows how far — or where — AI will take health care, but Nvidia’s recently announced $100 million deal with Amgen, which has access to 500 million human genomes, made some conference attendees uneasy. If Big Pharma can discover its own drugs, “biotech will disappear,” said Sherif Hanala of Seqens, a contract drug manufacturing company, during a lunch-table chat with KFF Health News and others. Others shrugged off that notion. The first AI algorithms beat clinicians at analyzing radiological scans in 2014. But since that year, “I haven’t seen a single AI company partner with pharma and complete a phase I human clinical trial,” said Alex Zhavoronkov, founder and CEO of Insilico Medicine — one of the companies using AI to do drug development. “Biology is hard.”
2. Weight Loss Pill Profits and Doubts
With predictions of a $100 billion annual market for GLP-1 agonists, the new class of weight loss drugs, many investors were asking their favorite biotech entrepreneurs whether they had a new Ozempic or Mounjaro in the wings this year, Zhavoronkov noted. In response, he opened his parlays with investors by saying, “I have a very cool product that helps you lose weight and gain muscle.” Then he would hand the person a pair of Insilico Medicine-embossed bicycle racing gloves.
More conventional discussions about the GLP-1s focused on how insurance will cover the current $13,000 annual cost for the estimated 40% of Americans who are obese and might want to go on the drugs. Sarah Emond, president of the Institute for Clinical and Economic Review, which calculates the cost and effectiveness of medical treatments, said that in the United Kingdom the National Health Service began paying in 2022 for obese patients to receive two years of semaglutide — something neither Medicare nor many insurers are covering in the U.S. even now.
But studies show people who go off the drugs typically regain two-thirds of what they lose, said Diana Thiara, medical director for the University of California-San Francisco weight management program. Recent research shows that the use of these drugs for three years reduces the risk of death, heart attack, and stroke in non-diabetic overweight patients. To do right by them, the U.S. health care system will have to reckon with the need for long-term use, she said. “I’ve never heard an insurer say, ‘After two years of treating this diabetes, I hope you’re finished,’” she said. “Is there a bias against those with obesity?”
3. Spotlight on Tax-Exempt Hospitals
Nonprofit hospitals showed off their investment appeal at the conference. Fifteen health systems representing major players across the country touted their value and the audience was intrigued: When headliners like the Mayo Clinic and the Cleveland Clinic took the stage, chairs were filled, and late arrivals crowded in the back of the room.
These hospitals, which are supposed to provide community benefits in exchange for not paying taxes, were eager to demonstrate financial stability and showcase money-making mechanisms besides patient care — they call it “revenue diversification.” PowerPoints skimmed through recent operating losses and lingered on the hospital systems’ vast cash reserves, expansion plans, and for-profit partnerships to commercialize research discoveries.
At Mass General Brigham, such research has led to the development of 36 drugs currently in clinical trials, according to the hospital’s presentation. The Boston-based health system, which has $4 billion in committed research funding, said its findings have led to the formation of more than 300 companies in the past decade.
Hospital executives thanked existing bondholders and welcomed new investors.
“For those of you who hold our debt, taxable and tax-exempt, thank you,” John Mordach, chief financial officer of Jefferson Health, a health system in Pennsylvania and New Jersey. “For those who don’t, I think we’re a great, undervalued investment, and we get a great return.”
Other nonprofit hospitals talked up institutes to draw new patients and expand into lucrative territories. Sutter Health, based in California, said it plans to add 30 facilities in attractive markets across Northern California in the next three years. It expanded to the Central Coast in October after acquiring the Sansum Clinic.
4. Money From New — And Old — Treatments for Autoimmune Disease
Autoimmunity drugs, which earn the industry $200 billion globally each year, were another hot theme, with various companies talking up development programs aimed at using current cancer drug platforms to create remedies for conditions like lupus and rheumatoid arthritis. AbbVie, which has led the sector with its $200 billion Humira, the world’s best-selling drug, had pride of place at the conference with a presentation in the hotel’s 10,000-square-foot Grand Ballroom.
President Robert Michael crowed about the company’s newer autoimmune drugs, Skyrizi and Rinvoq, and bragged that sales of two-decades-old Humira were going “better than anticipated.” Although nine biosimilar — essentially, generic — versions of the drug, adalimumab, entered the market last year, AbbVie expects to earn more than $7 billion on Humira this year since the “vast majority” of patients will remain on the market leader.
In its own presentation, biosimilar-maker Coherus BioSciences conceded that sales of Yusimry, its Humira knockoff listed at one-seventh the price of the original, would be flat until 2025, when Medicare changes take effect that could push health plans toward using cheaper drugs.
Biosimilars could save the U.S. health care system $100 billion a year, said Stefan Glombitza, CEO of Munich-based Formycon, another biosimilar-maker, but there are challenges since each biosimilar costs $150 million to $250 million to develop. Seeing nine companies enter the market to challenge Humira “was shocking,” he said. “I don’t think this will happen again.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 9 months ago
california, Health Industry, Pharmaceuticals, States, Health IT, Hospitals, Prescription Drugs