KFF Health News' 'What the Health?': Federal Health Work in Flux
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
Two months into the new administration, federal workers and contractors remain off-balance as the Trump administration ramps up its efforts to cancel jobs and programs — even as federal judges declare many of those efforts illegal and/or unconstitutional.
As it eliminates programs deemed duplicative or unnecessary, however, President Donald Trump’s Department of Government Efficiency is also cutting programs and workers aligned with Health and Human Services Secretary Robert F. Kennedy Jr.’s “Make America Healthy Again” agenda.
This week’s panelists are Julie Rovner of KFF Health News, Jessie Hellmann of CQ Roll Call, Sarah Karlin-Smith of the Pink Sheet, and Rachel Roubein of The Washington Post.
Panelists
Jessie Hellmann
CQ Roll Call
Sarah Karlin-Smith
Pink Sheet
Rachel Roubein
The Washington Post
Among the takeaways from this week’s episode:
- Kennedy’s comments this week about allowing bird flu to spread unchecked through farms provided another example of the new secretary of health and human services making claims that lack scientific support and could instead undermine public health.
- The Trump administration is experiencing more pushback from the federal courts over its efforts to reduce and dismantle federal agencies, and federal workers who have been rehired under court orders report returning to uncertainty and instability within government agencies.
- The second Trump administration is signaling it plans to dismantle HIV prevention programs in the United States, including efforts that the first Trump administration started. A Texas midwife is accused of performing illegal abortions. And a Trump appointee resigns after being targeted by a Republican senator.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: The Washington Post’s “The Free-Living Bureaucrat,” by Michael Lewis.
Rachel Roubein: The Washington Post’s “Her Research Grant Mentioned ‘Hesitancy.’ Now Her Funding Is Gone.” by Carolyn Y. Johnson.
Sarah Karlin-Smith: KFF Health News’ “Scientists Say NIH Officials Told Them To Scrub mRNA References on Grants,” by Arthur Allen.
Jessie Hellmann: Stat’s “NIH Cancels Funding for a Landmark Diabetes Study at a Time of Focus on Chronic Disease,” by Elaine Chen.
Also mentioned in this week’s podcast:
- The Wall Street Journal’s “Trump Administration Weighing Major Cuts to Funding for Domestic HIV Prevention,” by Liz Essley White, Dominique Mosbergen, and Jonathan D. Rockoff.
- The Washington Post’s “Disabled Americans Fear Losing Protections if States’ Lawsuit Succeeds,” by Amanda Morris.
click to open the transcript
Transcript: Federal Health Work in Flux
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello, and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News, and I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, March 20, at 10 a.m. As always, news happens fast and things might have changed by the time you hear this. So, here we go.
Today we are joined via videoconference by Rachel Roubein of The Washington Post.
Rachel Roubein: Hi.
Rovner: Sarah Karlin-Smith of the Pink Sheet.
Sarah Karlin-Smith: Hi, everybody.
Rovner: And Jessie Hellmann of CQ Roll Call.
Jessie Hellmann: Hello.
Rovner: No interview today, but, as usual, way more news than we can get to, so let us jump right in. In case you missed it, there’s a bonus podcast episode in your feed. After last week’s Senate Finance Committee confirmation hearing for Dr. Mehmet Oz to head the Centers for Medicare & Medicaid Services, my KFF Health News colleagues Stephanie Armour and Rachana Pradhan and I summarized the hearing and caught up on all the HHS [Department of Health and Human Services] nomination actions. It will be the episode in your feed right before this one.
So even without Senate-confirmed heads at — checks notes — all of the major agencies at HHS, the department does continue to make news. First, Robert F. Kennedy Jr., the new HHS secretary, speaks. Last week it was measles. This week it was bird flu, which he says should be allowed to spread unchecked in chicken flocks to see which birds are resistant or immune. This feels kind of like what some people recommended during covid. Sarah, is there any science to suggest this might be a good idea?
Karlin-Smith: No, it seems like the science actually suggests the opposite, because doctors and veterinary specialists are saying basically every time you let the infection continue to infect birds, you’re giving the virus more and more chances to mutate, which can lead to more problems down the road. The other thing is they were talking about the way we raise animals, and for food these days, there isn’t going to be a lot of genetic variation for the chickens, so it’s not like you’re going to be able to find a huge subset of them that are going to survive bird flu.
And then the other thing I thought is really interesting is just it doesn’t seem economically to make the most sense either as well, both for the individual farmers but then for U.S. industry as a whole, because it seems like other countries will be particularly unhappy with us and even maybe put prohibitions on trading with us or those products due to the spread of bird flu.
Rovner: Yeah, it was eyebrow-raising, let us say. Well, HHS this week also announced its first big policy effort, called Operation Stork Speed. It will press infant formula makers for more complete lists of ingredients, increase testing for heavy metals in formula, make it easier to import formula from other countries, and order more research into the health outcomes of feeding infant formula. This feels like maybe one of those things that’s not totally controversial, except for the part that the FDA [Food and Drug Administration] workers who have been monitoring the infant formula shortage were part of the big DOGE [Department of Government Efficiency] layoffs.
Roubein: I talked to some experts about this idea, and, like you said, they thought it kind of sounded good, but they basically needed more details. Like, what does it mean? Who’s going to review these ingredients? To your point, some people did say that the agency would need to staff up, and there was a neonatologist who is heading up infant formula that was hired after the 2022 shortage who was part of the probationary worker terminations. However, when the FDA rescinded the terminations of some workers, so, that doctor has been hired back. So I think that’s worth noting.
Rovner: Yes. This is also, I guess, where we get to note that Calley Means, one of RFK Jr.’s, I guess, brain trusts in the MAHA movement, has been hired as, I guess, in an Elon Musk-like position in the White House as an adviser. But this is certainly an area where he would expect to weigh in.
Hellmann: Yeah, I saw he’s really excited about this on Twitter, or X. There’s just been concerns in the MAHA movement, “Make America Healthy Again,” about the ingredients that are in baby formula. And the only thing is I saw that he also retweeted somebody who said that “breast is best,” and I’m just hoping that we’re not going back down that road again, because I feel like public health did a lot of work in pushing the message that formula and breast milk is good for the child, and so that’s just another angle that I’ve been thinking about on this.
Rovner: Yes, I think this is one of those things that everybody agrees we should look at and has the potential to get really controversial at some point. While we are on the subject of the federal workforce and layoffs, federal judges and DOGE continue to play cat-and-mouse, with lots of real people’s lives and careers at stake. Various judges have ordered the reinstatement, as you mentioned, Rachel, of probationary and other workers. Although in many cases workers have been reinstated to an administrative leave status, meaning they get put back on the payroll and they get their benefits back, but they still can’t do their jobs. At least one judge has said that does not satisfy his order, and this is all changing so fast it’s basically impossible to keep up. But is it fair to say that it’s not a very stable time to be a federal worker?
Karlin-Smith: That’s probably the nicest possible way to put it. When you talk to federal workers, everybody seems stressed and just unsure of their status. And if they do have a job, it’s often from their perspective tougher to do their job lately, and then they’re just not sure how stable it is. And many people are considering what options they have outside the federal government at this point.
Rovner: So for those lucky federal workers who do still have jobs, the Trump administration has also ordered everyone back to offices, even if those offices aren’t equipped to accommodate them. FDA headquarters here in Maryland’s kind of been the poster child for this this week.
Karlin-Smith: Yeah, FDA is an interesting one because well before covid normalized working from home and transitioned a lot of people to working from home, FDA’s headquarters couldn’t accommodate a lot of the new growth in the agency over the years, like the tobacco part of the FDA. So it was typical that people at least worked part of their workweek at home, and FDA really found once covid gave them additional work-from-home flexibilities, they were able to recruit staff they really, really needed with specialized degrees and training who don’t live near here, and it actually turned out to be quite a benefit from them.
And now they’re saying everybody needs to be in an office five days a week, and you have people basically cramped into conference rooms. There’s not enough parking. People are trying to review technical scientific data, and you kind of can’t hear yourself think. Or you’re a lawyer — I heard of a situation where people are basically being told, Well, if you need to do a private phone call because of the confidentiality around what you’re doing, go take the call in your car. So I think in addition to all of the concerns people have around the stability of their jobs, there’s now this element of, on a personal level, I think for many of them it’s just made their lives more challenging. And then they just feel like they’re not actually able to do, have the same level of efficiency at their work as they normally would.
Rovner: And for those who don’t know, the FDA campus is on a former military installation in the Maryland suburbs. It’s not really near any public transportation. So you pretty much have to drive to get there. And I think that the parking lots are not that big, because, as you pointed out, Sarah, the workforce is now bigger than the headquarters was created to accommodate it. And we’re seeing this across the government. This week it happened to be FDA. You have to ask the question: Is this really just an effort to make the government not work, to make federal workers, if they can’t fire them, to make them quit?
Hellmann: I definitely think that’s part of the underlying goal. If you see some of the stuff that Elon Musk says about the federal workforce, it’s very dismissive. He doesn’t seem to have a lot of respect for the civil servants. And they’ve been running into a lot of pushback from federal judges over many lawsuits targeting these terminations. And so I think just making conditions as frustrating as possible for some of these workers until they quit is definitely part of the strategy.
Roubein: And I think this is overlaid with the additional buyout offers, the additional early retirement offers. There’s also the reduction-in-force plans that federal workers have been unnerved about, bracing for future layoffs. So it’s very clear that they want to shrink the size of the federal workforce.
Rovner: Yeah, we’ve seen a lot of these people, I’ve seen interviews with them, who are being reinstated, but they’re still worried that now they’re going to be RIF-ed. They’re back on the payroll, they’re off the payroll. I mean there’s nothing — this does not feel like a very efficient way to run the federal government.
Karlin-Smith: Right. I think that’s what a lot of people are talking about is, again, going back to offices, for many of these people, is not leading to productivity. I talked to one person who said: I’m just leaving my laptop at the office now. I’m not going to take it home and do the extra hours of work that they might’ve normally gotten from me. And that includes losing time to commute. FDA is paying for parking-garage spaces in downtown Silver Spring [Maryland] near the Metro so that they can then shuttle people to the FDA headquarters. I’ve taken buses from that Metro to FDA headquarters. In traffic, that’s a 30-minute drive. They’re spending money on things that, again, I think are not going to in the long run create any government efficiency.
And in fact, I’ve been talking to people who are worried it’s going to do the opposite, that drug review, device review, medical product review times and things like that are going to slow. We talked about food safety. I think The New York Times had a really good story this week about concerns about losing the people. We need to make sure that baby formula is actually safe. So there’s a lot of contradictions in the messaging of what they’re trying to accomplish and how the actions actually are playing out.
Rovner: Well, and finally, I’m going to lay one more layer on this. There’s the question of whether you can even put the toothpaste back in the tube if you wanted to. After weeks of back-and-forth, the federal judge ruled on Tuesday that the dissolution of USAID [the U.S. Agency for International Development] was illegal and probably unconstitutional, and ordered email and computer access restored for the remaining workers while blocking further cuts. But with nearly everybody fired, called back from overseas, and contracts canceled, USAID couldn’t possibly come close to doing what it did before DOGE basically took it apart, right?.
Karlin-Smith: You hear stories of if someone already takes a new job, they’re lucky enough to find a new job, why are they going to come back? Again, even if you’re brought back, my expectation is a lot of people who have been brought back are probably looking for new jobs regardless because you don’t have that stability. And I think the USAID thing is interesting, too, because again, you have people that were working in all corners of the world and you have partnerships with other countries and contractors that have to be able to trust you moving forward. And the question is, do those countries and those organizations want to continue working with the U.S. if they can’t have that sort of trust? And as people said, the U.S. government was known as, they could pay contractors less because they always paid you. And when you take that away, that creates a lot of problems for negotiating deals to work with them moving forward.
Rovner: And I think that’s true for federal workers, too. There’s always been the idea that you probably could earn more in the private sector than you can working for the federal government, but it’s always been a pretty stable job. And I think right now it’s anything but, so comes the question of: Are we deterring people from wanting to work for the federal government? Eventually one would assume there’s still going to be a federal government to work for, and there may not be anybody who wants to do it.
Roubein: Yeah, you saw various hiring authorities given to try and recruit scientists and other researchers who make a lot, lot more in the public health sector, and some of those were a part of the probationary workforce because they had been hired recently under those authorities.
Rovner: Yeah, and now this is all sort of coming apart. Well, meanwhile, the cuts are continuing even faster than federal judges can rule against them. Last week, the administration said it would reduce the number of HHS regional offices from 10 to four. Considering these are where the department’s major fraud-fighting efforts take place, that doesn’t seem a very effective way of going after fraud and abuse in programs like Medicare and Medicaid. Those regional offices are also where lots of beneficiary protections come from, like inspections of nursing homes and Head Start facilities. How does this serve RFK Jr.’s Make America Healthy Again agenda?
Karlin-Smith: I think it’s not clear that it does, right? You’re talking about, again, the Department of Government Efficiency has focused on efficiency, cost savings, and Medicare and Medicaid does a pretty good job of fighting fraud and making HHS OIG [Office of Inspector General], all those organizations, they collect a lot of money back. So when you lose people—
Rovner: And of course the inspector general has also been laid off in all of this.
Karlin-Smith: Right. It’s not clear to me, I think one of the things with that whole reorganization of their chief counsel is people are suggesting, again, this is sort of a power move of HHS wanting to get a little bit more control of the legal operations at the lower agencies, whether it’s NIH [the National Institutes of Health] or FDA and so forth. But, right, it’s reducing head count without really thinking about what people’s roles actually were and what you lose when you let them go.
Rovner: Well, the Trump administration is also continuing to cut grants and contracts that seem like they’d be the kind of things that directly relate to Make America Healthy Again. Jessie, you’ve chosen one of those as your extra credit this week. Tell us about it.
Hellmann: Yeah. So my story is from Stat [“NIH Cancels Funding for a Landmark Diabetes Study at a Time of Focus on Chronic Disease”], and it’s about a nationwide study that tracks patients with prediabetes and diabetes. And it was housed at Columbia University, which as we know has been the subject of some criticism from the Trump administration. They had lost about $400 million in grants because the administration didn’t like Columbia’s response to some of the protests that were on campus last year. But that has an effect on some research that really doesn’t have much to do with that, including a study that looked at diabetes over a really long period of time.
So it was able to over decades result in 200 publications about prediabetes and diabetes, and led to some of the knowledge that we have now about the interventions for that. And the latest stage was going to focus on dementia and cognitive impairment, since some of the people that they’ve been following for years are now in their older ages. And now they have to put a stop to that. They don’t even have funding to analyze blood samples that they’ve done and the brain scans that they’ve collected. So it’s just another example of how what’s being done at the administration level is contradicting some of the goals that they say that they have.
Rovner: Yeah, and it’s important to remember that Columbia’s funding is being cut not because they deemed this particular project to be not helpful but because they are, as you said, angry at Columbia for not cracking down more on pro-Palestinian protesters after Oct. 7.
Well, meanwhile, people are bracing for still more cuts. The Wall Street Journal is reporting the administration plans to cut domestic AIDS-HIV programming on top of the cuts to the international PEPFAR [President’s Emergency Plan for AIDS Relief] program that was hammered as part of the USAID cancellation. Is fighting AIDS and HIV just way too George W. Bush for this administration?
Hellmann: It’s interesting because President [Donald] Trump unveiled the Ending the HIV Epidemic initiative in his first term, and the goal was to end the epidemic in the United States. And so if they were talking about reducing some of that funding, or I know there were reports that maybe they would move the funding from CDC [the Centers for Disease Control and Prevention] to HRSA [the Health Resources and Services Administration], it’s very unclear at this point. Then it raises questions about whether it would undermine that effort. And there’s already actions that the Trump administration has done to undermine the initiative, like the attacks on trans people. They’ve canceled grants to researchers studying HIV. They have done a whole host of things. They canceled funding to HIV services organizations because they have “trans” in their programming or on their websites. So it’s already caused a lot of anxiety in this community. And yeah, it’s just a total turnaround from the first administration.
Rovner: I know the Whitman-Walker clinic here in Washington, which has long been one of the premier AIDS-HIV clinics, had just huge layoffs. This is already happening, and as you point out, this was something that President Trump in his first term vowed to end AIDS-HIV in the U.S. So this is not one would think how one would go about that.
Well, it’s not just the administration that’s working to constrict rights and services. A group of 17 states, led by Texas, of course, are suing to have Biden-era regulations concerning discrimination against trans people struck down, except as part of that suit, the states are asking that the entirety of Section 504 of the Rehabilitation Act be declared unconstitutional. Now, you may never have heard of Section 504, but it is a very big deal. It was the forerunner of the Americans With Disabilities Act, and it prevents discrimination on the basis of disability in all federally funded activities. It is literally a lifeline for millions of disabled people that enables them to live in the community rather than in institutions. Are we looking at an actual attempt to roll back basically all civil rights as part of this war on “woke” and DEI [diversity, equity, and inclusion] and trans people?
Hellmann: The story is interesting, because it seems like some of the attorneys general are saying, That’s not our intent. But if you look at the court filings, it definitely seems like it is. And yeah, like you said, this is something that would just have a tremendous impact. And Medicaid coverage of home- and community-based services is one of those things that states are constantly struggling to pay for. You’re just continuing to see more and more people need these services. Some states have waiting lists, so—
Rovner: I think most states have waiting lists.
Hellmann: Yeah. It’s something, you have to really question what the intent is here. Even if people are saying, This isn’t our intent, it’s pretty black-and-white on paper in the court records, so—
Rovner: Yeah, just to be clear, this was a Biden administration regulation, updating the rules for Section 504, that included reference to trans people. But in the process of trying to get that struck down, the court filings do, as you say, call for the entirety of Section 504 to be declared unconstitutional. This is obviously one of those court cases that’s still before the district court, so it’s a long way to go. But the entire disability community, certainly it has their attention.
Well, we haven’t had any big abortion news the past couple of weeks, but that is changing. In Texas, a midwife and her associate have become the first people arrested under the state’s 2022 abortion ban. The details of the case are still pretty fuzzy, but if convicted, the midwife who reportedly worked as an OB-GYN doctor in her native Peru and served a mostly Spanish-speaking clientele, could be sentenced to up to 20 years in prison. So, obviously, be watching that one. Meanwhile, here in Washington, Hilary Perkins, a career lawyer chosen by FDA commissioner nominee Marty Makary to serve as the agency’s general counsel, resigned less than two days into her new position after complaints from Missouri Sen. Josh Hawley that she defended the Biden administration’s position on the abortion pill mifepristone.
Now, Hilary Perkins is no liberal trying to hide out in the bureaucracy. She’s a self-described pro-life Christian conservative hired in the first Trump administration, but she was apparently forced out for the high crime of doing her job as a career lawyer. Is this administration really going to try to evict anyone who ever supported a Biden position? Will that leave anybody left?
Roubein: I think what’s notable is Sen. Josh Hawley here, who expressed concerns and I had heard expressed concerns to the White House, and the post on X from the FDA came an hour before the hearing. There were concerns that he was not going to make it out of committee and—
Rovner: Before the Marty Makary hearing.
Roubein: Yes, sorry, before the vote in the HELP [Health, Education, Labor and Pensions] Committee on Marty Makary. And Hawley said because of that, he would vote to support him. What was interesting is two Democrats actually ended up supporting him, so he could have passed without Hawley’s vote. But I think in general it poses a test for Marty Makary when he’s an FDA commissioner, and how and whether he’s going to get his people in and how he’ll respond to different pressure points in Congress and with HHS and with the White House.
Rovner: And of course, Hawley’s not a disinterested bystander here, right?
Karlin-Smith: So his wife was one of the key attorneys in the recent big Supreme Court case that was pushed down to the lower courts for a lack of standing, but she was trying to essentially get tighter controls on the abortion pill mifepristone. But it seems like almost maybe Hawley jumped too soon before doing all of his research or fully understanding the role of people at Justice. Because even before this whole controversy erupted, I had talked to people the day before about this and asked them, “Should we read into this, her being involved in this?” And everybody I talked to, including, I think, a lot of people that have different views than Perkins does on the case, that they were saying she was in a role as a career attorney. You do what your boss, what the administration, wants.
If you really, really had a big moral problem with that, you can quit your job. But it’s perfectly normal for an attorney in that kind of position to defend a client’s interest and then have another client and maybe have to defend them wrongly. So it seems like if they had just maybe even picked up the phone and had a conversation with her, the whole crisis could have been averted. And she was on CNN yesterday trying to plead her case and, again, emphasize her positions because perhaps she’s worried about her future career prospects, I guess, over this debacle.
Rovner: Yeah, now she’s going to be blackballed by both sides for having done her job, basically. Anyway, all right, well, one big Biden initiative that looks like it will continue is the Medicare Drug Price Negotiation program. And we think we know this because CMS announced last week that the makers of all of the 15 drugs selected for the second round of negotiations have agreed to, well, negotiate. Sarah, this is news, right? Because we were wondering whether this was really going to go forward.
Karlin-Smith: Yeah, they’ve made some other signals since taking over that they were going to keep going with this, including last week at his confirmation hearing, Dr. Oz, for CMS, also indicated he seemed like he would uphold that law and they were looking for ways to lower drug costs. So I think what people are going to be watching for is whether they yield around the edges in terms of tweaks the industry wants to the law, or is there something about the prices they actually negotiate that signal they’re not really trying to get them as low as they can go? But this seems to be one populist issue for Trump that he wants to keep leaning into and keep the same consistency, I think, from his first administration, where he always took a pretty hard line on the drug industry and drug pricing.
Rovner: And I know Ozempic is on that list of 15 drugs, but the administration hasn’t said yet. I assume that’s Ozempic for its original purpose in treating diabetes. This administration hasn’t said yet whether they’ll continue the Biden declaration that these drugs could be available for people for weight loss, right?
Karlin-Smith: Correct. And I think that’s going to be more complicated because that’s so costly. So negotiating the price of drugs saves money. So yes, basically because Ozempic and Wegovy are the same drug, that price should be available regardless of the indication. But I’m more skeptical that they continue that policy, because of the cost and also just because, again, HHS Secretary Robert F. Kennedy seems to be particularly skeptical of the drugs, or at least using that as a first line of defense, widespread use, reliance on that. He tends to, in general, I think, support other ways of medical, I guess, treatment or health treatments before turning to pharmaceuticals.
Rovner: Eating better and exercising.
Karlin-Smith: Correct, right. So I think that’s going to be a hard sell for them because it’s just so costly.
Rovner: We will see. All right, that is as much news as we have time for this week. Now, it is time for our extra-credit segment, that’s where we each recognize the story we read this week we think you should read, too. Don’t worry if you miss it. We will put the links in our show notes on your phone or other mobile device. Jessie, you’ve done yours already this week. Rachel, why don’t you go next?
Roubein: My extra credit, the headline is “Her Research Grant Mentioned ‘Hesitancy.’ Now Her Funding Is Gone.” In The Washington Post by my colleague Carolyn Y. Johnson. And I thought the story was particularly interesting because it really dove into the personal level. You hear about all these cuts from a high level, but you don’t always really know what it means and how it came about. So the backstory is the National Institutes of Health terminated dozens of research grants that focused on why some people are hesitant to accept vaccines.
And Carolyn profiled one researcher, Nisha Acharya, but there was a twist, and the twist was she doesn’t actually study how to combat vaccine hesitancy or ways to increase vaccine uptake. Instead, she studies how well the shingles vaccine works to prevent the infection, with a focus on whether the shot also prevents the virus from affecting people’s eyes. But in the summary of her project, she had used the word “hesitancy” once and used the word “uptake” once. And so this highlights the sweeping approach to halting some of these vaccine hesitancy research grants.
Rovner: Yeah that was like the DOD [Department of Defense] getting rid of the picture of the Enola Gay, the plane that dropped the atomic bomb, because it had the word “Gay” in it. This is the downside, I guess, of using AI for these sorts of things. Sarah.
Karlin-Smith: I took a look at a KFF story by Arthur Allen, “Scientists Say NIH Officials Told Them to Scrub mRNA References on Grants,” and it’s about NIH officials urging people to remove any reference to mRNA vaccine technology from their grants. And the story indicates it’s not yet clear if that is going to translate to defunding of such research, but the implications are quite vast. I think most people probably remember the mRNA vaccine technology is really what helped many of us survive the covid pandemic and is credited with saving millions of lives, but the technology promise seems vast even beyond infectious diseases, and there’s a lot of hope for it in cancer.
And so this has a lot of people worried. It’s not particularly surprising, I guess, because again, the anti-vaccine movement, which Kennedy has been a leader of, has been particularly skeptical of the mRNA technology. But it is problematic, I think, for research. And we spent a lot of time on this call talking about the decimation of the federal workforce that may happen here, and I think this story and some of the other things we talked about today also show how we may just decimate our entire scientific research infrastructure and workforce in the U.S. outside of just the federal government, because so much of it is funded by NIH, and the decisions they’re making are going to make it impossible for a lot of scientists to do their job.
Rovner: Yeah, we’re also seeing scientists going to other countries, but that’s for another time. Well, my extra credit this week, probably along the same lines, also from The Washington Post. It’s part of a series called “Who Is Government?” This particular piece [“The Free-Living Bureaucrat”] is by bestselling author Michael Lewis, and it’s a sprawling — and I mean sprawling — story of how a mid-level FDA employee who wanted to help find new treatments for rare diseases ended up not only figuring out a cure for a child who was dying of a rare brain amoeba but managed to obtain the drug for the family in time to save her. It’s a really good piece, and it’s a really excellent series that tells the stories of mostly faceless bureaucrats who actually are working to try to make the country a better place.
OK, that’s this week’s show. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left us a review. That helps other people find us, too. Thanks as always to our producer, Francis Ying, and our editor, Emmarie Huetteman. As always, you can email us your comments or questions. We’re at whatthehealth@kff.org, or you can still find me at X, @jrovner, and at Bluesky, @julierovner. Where are you guys these days? Sarah?
Karlin-Smith: A little bit everywhere. X, Bluesky, LinkedIn — @SarahKarlin or @sarahkarlin-smith.
Rovner: Jessie.
Hellmann: I’m @jessiehellmann on X and Bluesky, and I’m also on LinkedIn more these days.
Rovner: Great. Rachel.
Roubein: @rachelroubein at Bluesky, @rachel_roubein on X, and also on LinkedIn.
Rovner: We will be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
7 months 1 week ago
Courts, Health Care Costs, Medicare, Multimedia, Pharmaceuticals, Public Health, States, Abortion, Children's Health, CMS, Disabilities, Drug Costs, FDA, Food Safety, HHS, HIV/AIDS, KFF Health News' 'What The Health?', Podcasts, Prescription Drugs, texas, Trump Administration, vaccines
Drinking is cheaper than it’s been in decades. Lobbyists are fighting to keep it that way
For years, it has been a reliable way to cut back on the consumption of cigarettes and sugary drinks: raise taxes on them. So it might seem an obvious tactic to apply to alcohol, which contributes to untold injuries, diseases and deaths in the United States each year.
That’s the thinking of advocates and state legislators across the country, who also see it as a way to pull in more revenue. But at virtually every turn — including in Nebraska, Colorado, Oregon and New Mexico — efforts to raise taxes on alcoholic beverages have been thwarted by the alcohol industry, a vast and powerful coalition of corporate conglomerates, mom-and-pop producers, retail stores, hospitality workers, trade associations and their lobbyists. The result is a population with mounting alcohol-related woes and an ever-cheaper, more accessible supply of drink.
1 year 2 days ago
Health, addiction, finance, Public Health, States
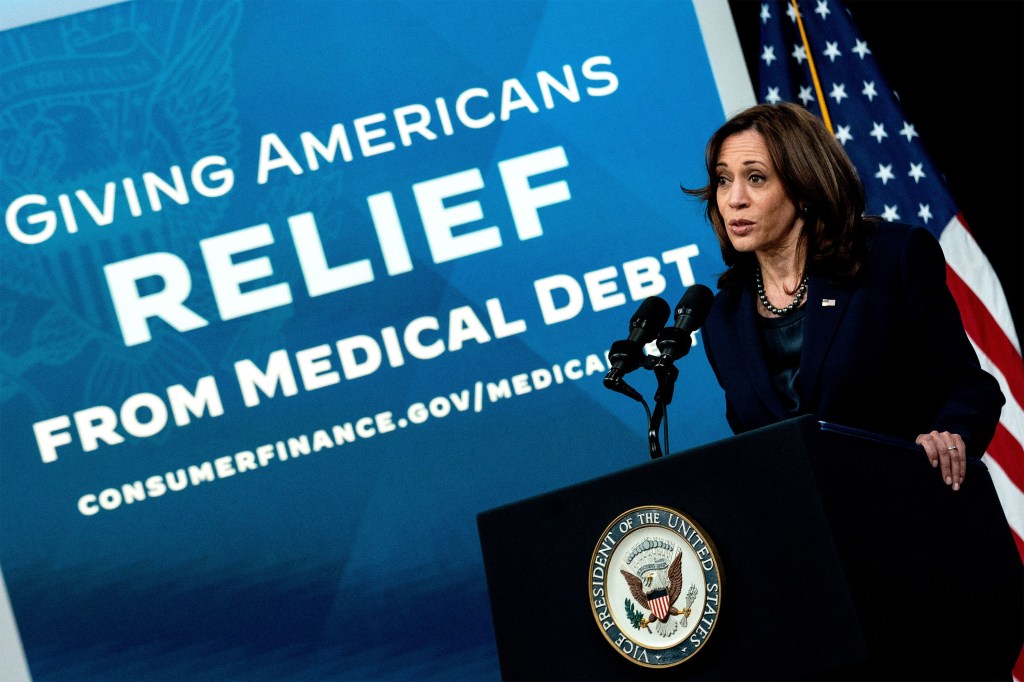
Harris apoya la reducción de la deuda médica. Los “conceptos” de Trump preocupan a defensores.
Defensores de pacientes y consumidores confían en que Kamala Harris acelere los esfuerzos federales para ayudar a las personas que luchan con deudas médicas, si gana en las elecciones presidenciales del próximo mes.
Y ven a la vicepresidenta y candidata demócrata como la mejor esperanza para preservar el acceso de los estadounidenses a seguros de salud. La cobertura integral que limita los costos directos de los pacientes es la mejor defensa contra el endeudamiento, dicen los expertos.
La administración Biden ha ampliado las protecciones financieras para los pacientes, incluyendo una propuesta histórica de la Oficina de Protección Financiera del Consumidor (CFPB) para eliminar la deuda médica de los informes de crédito de los consumidores.
En 2022, el presidente Joe Biden también firmó la Ley de Reducción de la Inflación, que limita cuánto deben pagar los afiliados de Medicare por medicamentos recetados, incluyendo un tope de $35 al mes para la insulina. Y en legislaturas de todo el país, demócratas y republicanos han trabajado juntos de manera discreta para promulgar leyes que frenen a los cobradores de deudas.
Sin embargo, defensores dicen que el gobierno federal podría hacer más para abordar un problema que afecta a 100 millones de estadounidenses, obligando a muchos a trabajar más, perder sus hogares y reducir el gasto en alimentos y otros artículos esenciales.
“Biden y Harris han hecho más para abordar la crisis de deuda médica en este país que cualquier otra administración”, dijo Mona Shah, directora senior de política y estrategia en Community Catalyst, una organización sin fines de lucro que ha liderado los esfuerzos nacionales para fortalecer las protecciones contra la deuda médica. “Pero hay más por hacer y debe ser una prioridad para el próximo Congreso y administración”.
Al mismo tiempo, los defensores de los pacientes temen que si el ex presidente Donald Trump gana un segundo mandato, debilitará las protecciones de los seguros permitiendo que los estados recorten sus programas de Medicaid o reduciendo la ayuda federal para que los estadounidenses compren cobertura médica. Eso pondría a millones de personas en mayor riesgo de endeudarse si enferman.
En su primer mandato, Trump y los republicanos del Congreso intentaron en 2017 derogar la Ley de Cuidado de Salud a Bajo Precio (ACA), un movimiento que, según analistas independientes, habría despojado de cobertura médica a millones de estadounidenses y habría aumentado los costos para las personas con afecciones preexistentes, como diabetes y cáncer.
Trump y sus aliados del Partido Republicano continúan atacando a ACA, y el ex presidente ha dicho que quiere revertir la Ley de Reducción de la Inflación, que también incluye ayuda para que los estadounidenses de bajos y medianos ingresos compren seguros de salud.
“Las personas enfrentarán una ola de deuda médica por pagar primas y precios de medicamentos recetados”, dijo Anthony Wright, director ejecutivo de Families USA, un grupo de consumidores que ha apoyado las protecciones federales de salud. “Los pacientes y el público deberían estar preocupados”.
La campaña de Trump no respondió a consultas sobre su agenda de salud. Y el ex presidente no suele hablar de atención médica o deuda médica en la campaña, aunque dijo en el debate del mes pasado que tenía “conceptos de un plan” para mejorar la ACA. Trump no ha ofrecido detalles.
Harris ha prometido repetidamente proteger ACA y renovar los subsidios ampliados para las primas mensuales del seguro creados por la Ley de Reducción de la Inflación. Esa ayuda está programada para expirar el próximo año.
La vicepresidenta también ha expresado su apoyo a un mayor gasto gubernamental para comprar y cancelar deudas médicas antiguas de los pacientes. En los últimos años, varios estados y ciudades han comprado deuda médica en nombre de sus residentes.
Estos esfuerzos han aliviado la deuda de cientos de miles de personas, aunque muchos defensores dicen que cancelar deudas antiguas es, en el mejor de los casos, una solución a corto plazo, ya que los pacientes seguirán acumulando facturas que no pueden pagar sin una acción más sustantiva.
“Es un bote con un agujero”, dijo Katie Berge, una cabildera de la Sociedad de Leucemia y Linfoma. Este grupo de pacientes fue una de más de 50 organizaciones que el año pasado enviaron cartas a la administración Biden instando a las agencias federales a tomar medidas más agresivas para proteger a los estadounidenses de la deuda médica.
“La deuda médica ya no es un problema de nicho”, dijo Kirsten Sloan, quien trabaja en política federal para la Red de Acción contra el Cáncer de la Sociedad Americana de Cáncer. “Es clave para el bienestar económico de millones de estadounidenses”.
La Oficina de Protección Financiera del Consumidor está desarrollando regulaciones que prohibirían que las facturas médicas aparezcan en los informes de crédito de los consumidores, lo que mejoraría los puntajes crediticios y facilitaría que millones de estadounidenses alquilen una vivienda, consigan un trabajo o consigan un préstamo para un automóvil.
Harris, quien ha calificado la deuda médica como “crítica para la salud financiera y el bienestar de millones de estadounidenses”, apoyó con entusiasmo la propuesta de regulación. “No se debería privar a nadie del acceso a oportunidades económicas simplemente porque experimentó una emergencia médica”, dijo en junio.
El compañero de fórmula de Harris, el gobernador de Minnesota, Tim Walz, quien ha dicho que su propia familia luchó con la deuda médica cuando era joven, firmó en junio una ley estatal que reprime el cobro de deudas.
Los funcionarios de la CFPB dijeron que las regulaciones se finalizarán a principios del próximo año. Trump no ha indicado si seguiría adelante con las protecciones contra la deuda médica. En su primer mandato, la CFPB hizo poco para abordarla, y los republicanos en el Congreso han criticado durante mucho tiempo a la agencia reguladora.
Si Harris gana, muchos grupos de consumidores quieren que la CFPB refuerce aún más las medidas, incluyendo una mayor supervisión de las tarjetas de crédito médicas y otros productos financieros que los hospitales y otros proveedores médicos han comenzado a ofrecer a los pacientes. Por estos préstamos, las personas están obligadas a pagar intereses adicionales sobre su deuda médica.
“Estamos viendo una variedad de nuevos productos financieros médicos”, dijo April Kuehnhoff, abogada senior del Centro Nacional de Derecho del Consumidor. “Estos pueden generar nuevas preocupaciones sobre las protecciones al consumidor, y es fundamental que la CFPB y otros reguladores supervisen a estas empresas”.
Algunos defensores quieren que otras agencias federales también se involucren.
Esto incluye al enorme Departamento de Salud y Servicios Humanos (HHS), que controla cientos de miles de millones de dólares a través de los programas de Medicare y Medicaid. Ese dinero otorga al gobierno federal una enorme influencia sobre los hospitales y otros proveedores médicos.
Hasta ahora, la administración Biden no ha utilizado esa influencia para abordar la deuda médica.
Pero en un posible anticipo de futuras acciones, los líderes estatales en Carolina del Norte recientemente obtuvieron la aprobación federal para una iniciativa de deuda médica que obligará a los hospitales a tomar medidas para aliviar las deudas de los pacientes a cambio de ayuda gubernamental. Harris elogió la iniciativa.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 1 week ago
Elections, Health Care Costs, Health Industry, Insurance, Noticias En Español, States, Biden Administration, Diagnosis: Debt, Investigation, Obamacare Plans, Trump Administration
Happening in Springfield: New Immigrants Offer Economic Promise, Health System Challenges
When Republican vice presidential candidate JD Vance claimed Haitian immigrants had caused infectious-disease rates to “skyrocket” in Springfield, Ohio, local health commissioner Chris Cook checked the records.
They showed that in 2023, for example, there were four active tuberculosis cases in Clark County, which includes Springfield, up from three in 2022. HIV cases had risen, but sexually transmitted illnesses overall were decreasing.
“I wouldn’t call it skyrocketing,” said Cook, noting that there were 190 active cases in 2023 in all of Ohio. “You hear the rhetoric. But as a whole, reportable infectious diseases to the health department are decreasing.”
Tensions are running high in this industrial town of about 58,000 people. Bomb threats closed schools and public buildings after GOP presidential nominee Donald Trump falsely claimed that Haitian immigrants — who he alleged were there illegally — were stealing and eating household pets. City and county officials disputed the claims the former president levied during his Sept. 10 debate with Vice President Kamala Harris, his Democratic opponent.
Trump was amplifying comments made by Vance that — along with his claims about the immigration status of this population — were broadly panned as false. When asked during a CNN interview about the debunked pet-eating rumor, Vance, a U.S. senator from Ohio, acknowledged that the image he created was based not on facts but on “firsthand accounts from my constituents.” He said he was willing “to create” stories to focus attention on how immigration can overrun communities.
But Ohio Gov. Mike DeWine, also a Republican, has said immigrants have been an economic boon to Springfield. Many began arriving because businesses in the town, which had seen its population decrease, needed labor.
Largely lost in the political rancor is the way Springfield and the surrounding area responded to the influx of Haitian immigrants. Local health institutions tried to address the needs of this new population, which had lacked basic public health care such as immunization and often didn’t understand the U.S. health system.
The town is a microcosm of how immigration is reshaping communities throughout the United States. In the Springfield area, Catholic charities, other philanthropies, volunteers, and county agencies have banded together over the past three to four years to tackle the challenge and connect immigrants who have critical health needs with providers and care.
For instance, a community health center added Haitian Creole interpreters. The county health department opened a refugee health testing clinic to provide immunizations and basic health screenings, operating on such a shoestring budget that it’s open only two days a week.
And a coalition of groups to aid the Haitian community was created about two years ago to identify and respond to immigrant community needs. The group meets once a month with about 55 or 60 participants. On Sept. 18, about a week after Trump ramped up the furor at the debate, a record 138 participants joined in.
“We have all learned the necessity of collaboration,” said Casey Rollins, director of Springfield’s St. Vincent de Paul, a nonprofit Catholic social services organization that has become a lifeline for many of the town’s Haitian immigrants. “There’s a lot of medical need. Many of the people have high blood pressure, or they frequently have diabetes.”
Several factors have led Haitians to leave their Caribbean country for the United States, including a devastating earthquake in 2010, political unrest after the 2021 assassination of Haiti’s president, and ongoing gang violence. Even when health facilities in the country are open, it can be too treacherous for Haitians to travel for treatment.
“The gangs typically leave us alone, but it’s not a guarantee,” said Paul Glover, who helps oversee the St. Vincent’s Center for children with disabilities in Haiti. “We had a 3,000-square-foot clinic. It was destroyed. So was the X-ray machine. People have been putting off health care.”
An estimated 12,000 to 15,000 Haitian immigrants live in Clark County, officials said. About 700,000 Haitian immigrants lived in the United States in 2022, according to U.S. Census data.
Those who have settled in the Springfield area are generally in the country legally under a federal program that lets noncitizens temporarily enter and stay in the United States under certain circumstances, such as for urgent humanitarian reasons, according to city officials.
The influx of immigrants created a learning curve for hospitals and primary care providers in Springfield, as well as for the newcomers themselves. In Haiti, people often go directly to a hospital to receive care for all sorts of maladies, and county officials and advocacy groups said many of the immigrants were unfamiliar with the U.S. system of seeing primary care doctors first or making appointments for treatment.
Many sought care at Rocking Horse Community Health Center, a nonprofit, federally qualified health center that provides mental health, primary, and preventive care to people regardless of their insurance status or ability to pay. Federally qualified health centers serve medically underserved areas and populations.
The center treated 410 patients from Haiti in 2022, up more than 250% from 115 in 2021, according to Nettie Carter-Smith, the center’s director of community relations. Because the patients required interpreters, visits often stretched twice as long.
Rocking Horse hired patient navigators fluent in Haitian Creole, one of the two official languages of Haiti. Its roving purple bus provides on-site health screenings, vaccinations, and management of chronic conditions. And this school year, it’s operating a $2 million health clinic at Springfield High.
Many Haitians in Springfield have reported threats since Trump and Vance made their town a focus of the campaign. Community organizations were unable to identify any immigrants willing to be interviewed for this story.
Hospitals have also felt the impact. Mercy Health’s Springfield Regional Medical Center also saw a rapid influx of patients, spokesperson Jennifer Robinson said, with high utilization of emergency, primary care, and women’s health services.
This year, hospitals also have seen several readmissions for newborns struggling to thrive as some new mothers have trouble breastfeeding or getting supplemental formula, county officials said. One reason: New Haitian immigrants must wait six to eight weeks to get into a program that provides supplemental food for low-income pregnant, breastfeeding, or non-breastfeeding postpartum women, as well as for children and infants.
At Kettering Health Springfield, Haitian immigrants come to the emergency department for nonemergency care. Nurses are working on two related projects, one focusing on cultural awareness for staff and another exploring ways to improve communication with Haitian immigrants during discharge and in scheduling follow-up appointments.
Many of the immigrants are able to get health insurance. Haitian entrants generally qualify for Medicaid, the state-federal program for the low-income and disabled. For hospitals, that means lower reimbursement rates than with traditional insurance.
During 2023, 60,494 people in Clark County were enrolled in Medicaid, about 25% of whom were Black, according to state data. That’s up from 50,112 in 2017, when 17% of the enrollees were Black. That increase coincides with the rise of the Haitian population.
In September, DeWine pledged $2.5 million to help health centers and the county health department meet the Haitian and broader community’s needs. The Republican governor has pushed back on the recent national focus on the town, saying the spread of false rumors has been hurtful for the community.
Ken Gordon, a spokesperson for the Ohio Department of Health, acknowledged the difficulties Springfield’s health systems have faced and said the department is monitoring to avert potential outbreaks of measles, whooping cough, and even polio.
People diagnosed with HIV in the county increased from 142 residents in 2018 to 178 to 2022, according to state health department data. Cook, the Clark County health commissioner, said the data lags by about 1.5 years.
But Cook said, “as a whole, all reportable infections to the health department are not increasing.” Last year, he said, no one died of tuberculosis. “But 42 people died of covid.”
Healthbeat is a nonprofit newsroom covering public health published by Civic News Company and KFF Health News. Sign up for its newsletters here.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 2 weeks ago
Elections, Health Industry, Public Health, Race and Health, States, Healthbeat, Immigrants, Ohio
Watch: ‘Breaking the Silence Is a Step’ — Beyond the Lens of ‘Silence in Sikeston’
KFF Health News Midwest correspondent Cara Anthony took a reporting trip to the small southeastern Missouri city of Sikeston and heard a mention of its hidden past. That led her on a multiyear reporting journey to explore the connections between a 1942 lynching and a 2020 police killing there — and what they say about the nation’s silencing of racial trauma.
Along the way, she learned about her own family’s history with such trauma.
This formed the multimedia “Silence in Sikeston” project from KFF Health News, Retro Report, and WORLD as told through a documentary film, educational videos, digital articles, and a limited-series podcast. Hear about Anthony’s journey and join this conversation about the toll of racialized violence on our health and our communities.
Explore more of the “Silence in Sikeston”project:
LISTEN: The limited-series podcast is available on PRX, Apple Podcasts, Spotify, iHeart, or wherever you get your podcasts.
- Episode 1: “Racism Can Make You Sick”
- Episode 2: “Hush, Fix Your Face”
- Episode 3: “Trauma Lives in the Body”
- Episode 4: “Is There a Cure for Racism”
WATCH: The documentary film “Silence in Sikeston,” a co-production of KFF Health News and Retro Report, is now available to stream on WORLD’s YouTube channel, WORLDchannel.org, and the PBS app.
READ: KFF Health News Midwest correspondent Cara Anthony wrote an essay about what her reporting for this project helped her learn about her own family’s hidden past.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 2 weeks ago
Mental Health, Public Health, Race and Health, Rural Health, States, Missouri, Silence in Sikeston
Calif. Ballot Measure Targets Drug Discount Program Spending
Californians in November will weigh in on a ballot initiative to increase scrutiny over the use of health-care dollars — particularly money from a federal drug discount program — meant to support patient care largely for low-income or indigent people.
Californians in November will weigh in on a ballot initiative to increase scrutiny over the use of health-care dollars — particularly money from a federal drug discount program — meant to support patient care largely for low-income or indigent people. The revenue is sometimes used to address housing instability and homelessness among vulnerable patient populations.
Voters are being asked whether California should increase accountability in the 340B drug discount program, which provides money for community clinics, safety net hospitals and other nonprofit health-care providers.
The program requires pharmaceutical companies to give drug discounts to these clinics and nonprofit entities, which can bank revenue by charging higher reimbursement rates.
Advocates pushing the measure, Proposition 34, say some entities are using the drug discount program as a slush fund, plowing money into housing and homelessness initiatives that don’t meet basic patient safety standards. Researchers and advocates have called for greater oversight.
“There are 340B entities that are misusing these public dollars,” said Nathan Click, a spokesperson for the pro-Proposition 34 campaign. “The whole point of this program is to use this money to get more low-income people health-care services.”
The initiative wouldn’t bar 340B providers from using health-care funds for housing or homelessness programs. Instead, it targets providers that spend more than $100 million on purposes other than direct patient care over 10 years. It would mandate that 98 percentof 340B revenues go to direct patient care. It also targets 340B providers with health insurer contracts and pharmacy licenses and those serving low-income Medicaid or Medicare patients that have been dinged with at least 500 high-severity housing violations for substandard or unsafe conditions.
That has placed a bull’s eye on the Los Angeles-based AIDS Healthcare Foundation, a nonprofit that provides direct patient care via clinics and pharmacies in California and other states, including Illinois, Texas and New York. It also owns housing for low-income and homeless people.
A Los Angeles Times investigation found that many residents of AIDS Healthcare Foundation properties are living in deplorable, unhealthy conditions.
Michael Weinstein, the foundation’s president, disputes those claims and argues that Proposition 34 proponents, including real estate interests, are going after him for another ballot initiative that seeks to implement rent control in more communities across California.
“It’s a revenge initiative,” Weinstein said, arguing that the deep-pocketed California Apartment Association is targeting his foundation — and its health and housing operations — because it has backed ballot measures pushing rent control across California. “This is a two-pronged attack against us to defeat rent control.”
Weinstein is locked in a feud with the apartment association, the chief sponsor of the initiative, which has contributed handsomely to pass Proposition 34. Opponents argue that the initiative is “a wolf in sheep’s clothing.”
Weinstein acknowledged to KFF Health News that his nonprofit uses money from 340B drug discounts to support its housing initiatives but argued they are helping treat and house some of the most vulnerable people, who would otherwise be homeless.
The apartment association declined several requests for comment. But Proposition 34 backers say they aren’t going after rent control — or Weinstein and his nonprofit.
Supporters argue that “rising health care costs are squeezing millions of Californians” and say that the initiative would “give California patients and taxpayers much needed relief, and lowers state drug costs, while saving California taxpayers billions.”
If the initiative passes and 340B providers do not spend 98 percent of the revenue on direct patient care, they could lose their license to practice health care and their nonprofit status.
This article is not available for syndication due to republishing restrictions. If you have questions about the availability of this or other content for republication, please contact NewsWeb@kff.org.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 2 weeks ago
california, Elections, Health Care Costs, Health Industry, Pharmaceuticals, States, Drug Costs, Health Brief
Silence in Sikeston: Is There a Cure for Racism?
SIKESTON, Mo. — In the summer of 2021, Sikeston residents organized the biggest Juneteenth party in the city’s history. Sikeston police officers came too, both to provide security for the event and to try to build bridges with the community. But after decades of mistrust, some residents questioned their motives.
In the series finale of the podcast, a confident, outspoken Sikeston teenager shares her feelings in an uncommonly frank conversation with Chief James McMillen, head of Sikeston’s Department of Public Safety, which includes Sikeston police.
Host Cara Anthony asks what kind of systemic change is possible to reduce the burden of racism on the health of Black Americans. Health equity expert Gail Christopher says it starts with institutional leaders who recognize the problem, measure it, and take concrete steps to change things.
“It is a process, and it’s not enough to march and get a victory,” Christopher said. “We have to transform the systems of inequity in this country.”
Host
Cara Anthony
Midwest correspondent, KFF Health News
Cara is an Edward R. Murrow and National Association of Black Journalists award-winning reporter from East St. Louis, Illinois. Her work has appeared in The New York Times, Time magazine, NPR, and other outlets nationwide. Her reporting trip to the Missouri Bootheel in August 2020 launched the “Silence in Sikeston” project. She is a producer on the documentary and the podcast’s host.
In Conversation With …
Gail Christopher
Public health leader and health equity expert
click to open the transcript
Transcript: Is There a Cure for Racism?
Editor’s note: If you are able, we encourage you to listen to the audio of “Silence in Sikeston,” which includes emotion and emphasis not found in the transcript. This transcript, generated using transcription software, has been edited for style and clarity. Please use the transcript as a tool but check the corresponding audio before quoting the podcast.
[Ambient sounds from Sikeston, Missouri’s 2021 Juneteenth celebration — a DJ making an announcement over funky music, people chatting — begin playing.]
Cara Anthony: It’s 2021. It’s hot and humid. We’re at a park in the heart of Sunset — Sikeston, Missouri’s historically Black neighborhood.
Emory: Today is Juneteenth, baby.
Cara Anthony: The basketball courts are jumping. And old-school funk is blaring from the speakers. Kids are playing.
Cara Anthony: [Laughter] Are you enjoying the water?
Cara Anthony: People are lining up for barbecue.
I’ve been here reporting on the toll racism and violence can take on a community’s health. But today, I’m hoping to capture a little bit of Sikeston’s joy.
Taneshia Pulley: When I look out to the crowd of my people, I see strength. I see power. I just see all magic.
Cara Anthony: I drift over to a tent where people are getting their blood pressure, weight, and height checked … health screenings for free.
Cara Anthony: I’m a journalist.
Community Health Worker: Ooooh! Hi! Hi!
Cara Anthony: The ladies working the booth are excited I’m there to report on the event.
Cara Anthony: OK, and I’m a health journalist.
Community health worker: Baby, that’s what I told them. Yeah, she healthy. [Laughter]
[Dramatic instrumental music plays.]
Cara Anthony: This Juneteenth gathering is happening a little over a year after Sikeston police officers shot and killed 23-year-old Denzel Taylor.
We made a documentary about Denzel’s death and the death of another young Black man — also killed in Sikeston.
Denzel was shot by police. Nearly 80 years earlier, Cleo Wright was lynched by a white mob.
Both were killed before they got their day in court.
In these years of reporting, what I’ve found is that many Black families worry that their kids don’t have an equal chance of growing up healthy and safe in Sikeston.
[Dramatic instrumental ends.]
Rosemary Owens: Being Black in the Bootheel can get you killed at any age.
Cara Anthony: That’s Rosemary Owens. She raised her children here in Southeast Missouri.
Cara Anthony: About 10 Sikeston police officers showed up to Juneteenth — for security and to connect with the community. Some are in uniform; some are in plain clothes.
Rosemary has her doubts about why they came today.
Cara Anthony: You see the police chief talking to people. What’s going through your mind as you see them milling about?
Rosemary Owens: I hope they are real and wanting to close the gap between the African Americans and the white people.
Anybody can come out and shake hands. But at the end of the day, did you mean what you said? Because things are still going on here in Sikeston, Missouri.
Cara Anthony: For Rosemary, this brings to mind an encounter with the police from years ago.
[Slow, minor, instrumental music plays softly.]
When her son was maybe 16 years old, she says, she and her sister gave their boys the keys to their new cars — told them they could hang out in them.
Rosemary had gotten her new car for Mother’s Day.
Rosemary Owens: A brand-new red Dodge Caravan. We, we knew the boys were just going from the van to the car. You know, just showing out — they were boys. They weren’t driving.
Cara Anthony: Someone nearby saw the boys …
Rosemary Owens: … called and told the police that two Black men were robbing cars.
When the boys saw the police come up, there was three police cars. So they were like, something’s going on. So their intention, they were like, they were trying to run to us. And my brother said, stop. When they looked back, when the police got out of the car, they already had their guns drawn on my son and my nephew. Cara Anthony: That’s what Rosemary thinks about when she sees Sikeston police at Juneteenth.
[Slow, minor, instrumental music ends.]
[“Silence in Sikeston” theme song plays.] Cara Anthony: In this podcast series, we’ve talked about some of the ways racism makes Black people sick. But Juneteenth has me thinking about how we get free — how we STOP racism from making us sick.
The public health experts say it’s going to take systemwide, institutional change.
In this episode, we’re going to examine what that community-level change looks like — or at least what it looks like to make a start.
From WORLD Channel and KFF Health News, distributed by PRX, this is “Silence in Sikeston.”
Episode 4 is our final episode: “Is There a Cure for Racism?”
[“Silence in Sikeston” theme song ends.]
James McMillen: How you doing?
Juneteenth celebration attendee: Good. Good.
James McMillen: Good to see you, man.
Juneteenth celebration attendee: What’s up? How are you?
Cara Anthony: When I spot Sikeston’s director of public safety in his cowboy hat, sipping soda from a can, I head over to talk. James McMillen: Well, you know, I just, I, I’m glad to be … on the inside of this.
Cara Anthony: James McMillen leads the police department. He says he made it a point to come to Juneteenth. And he encouraged his officers to come, too.
James McMillen: I remember as being a young officer coming to work here, not knowing anybody, driving by a park and seeing several Black people out there. And I remember feeling, you know, somewhat intimidated by that. And I don’t really know why.
I hadn’t always been, um, that active in the community. And, um, I, I have been the last several years and I’m just wanting to teach officers to do the same thing.
Cara Anthony: The chief told me showing up was part of his department’s efforts to repair relations with Sikeston’s Black residents.
James McMillen: What’s important about this is, being out here and actually knowing people, I think it builds that trust that we need to have to prevent and solve crimes.
Cara Anthony: A few minutes into our conversation, I notice a teenager and her friend nearby, listening.
Cara Anthony: Yeah, we have two people who are watching us pretty closely. Come over here. Come over here. Tell us your names.
Lauren: My name is Lauren.
Michaiahes: My name is Michaiahes.
Cara Anthony: Yeah. And what are you all … ?
James McMillen: I saw you over there.
Cara Anthony: So, what do you think about all of this?
Michaiahes: Personally, I don’t even know who this is because I don’t mess with police because, because of what’s happened in the past with the police. But, um …
Cara Anthony: As she starts to trail off, I encourage her to keep going.
Cara Anthony: He’s right here. He’s in charge of all of those people.
Michaiahes: Well, in my opinion, y’all should start caring about the community more.
Cara Anthony: What are you hearing? She’s speaking from the heart here, Chief. What are you hearing?
James McMillen: Well, you know what? I agree with everything she said there.
Cara Anthony: She’s confident now, looking the chief in the eye.
Michaiahes: And let’s just be honest: Some of these police officers don’t even want to be here today. They’re just here to think they’re doing something for the community.
James McMillen: Let’s be honest. Some of these are assumptions that y’all are making about police that y’all don’t really know.
[Subtle propulsive music begins playing.]
Michaiahes: If we seen you protecting community, if we seen you doing what you supposed to do, then we wouldn’t have these assumptions about you.
James McMillen: I just want to say that people are individuals. We have supervisors that try to keep them to hold a standard. And you shouldn’t judge the whole department, but, but just don’t judge the whole department off of a few. No more than I should judge the whole community off of a few.
Cara Anthony: But here’s the thing … in our conversations over the years, Chief McMillen has been candid with me about how, as a rookie cop, he had judged Sikeston’s Black residents based on interactions with just a few.
James McMillen: Some of, um, my first calls in the Black community were dealing with, obviously, criminals, you know? So if first impressions mean anything, that one set a bad one. I had, um, really unfairly judging the whole community based on the few interactions that I had, again, with majority of criminals.
Cara Anthony: The chief says he’s moved past that way of thinking and he’s trying to help his officers move past their assumptions.
And he told me about other things he wants to do …
Hire more Black officers. Invest in racial-bias awareness education for the department. And open up more lines of communication with the community.
James McMillen: I know that we are not going to see progress or we’re not going to see success without a little bit of pain and discomfort on our part.
Cara Anthony: I don’t think I’ve ever heard the chief use the term institutional change, but the promises and the plans he’s making sound like steps in that direction.
Except … here’s something else the chief says he wants …
[Subtle propulsive music ends with a flourish.]
James McMillen: As a police officer, I would like to hear more people talk about, um, just complying with the officer.
Cara Anthony: That phrase is chilling to me.
[Quiet, dark music starts playing.]
When I hear “just comply” … a litany of names cross my mind.
Philando Castile.
Sonya Massey.
Tyre Nichols.
Cara Anthony: After Denzel Taylor was killed, people felt unsafe. I talked to a lot of residents on the record about them feeling like they didn’t know if they could be next.
One thing that you told me was, like, well, one thing that people can do is comply with the officers, you know, if they find themselves having an interaction with law enforcement.
James McMillen: Well, I mean, I think that’s, that’s a good idea to do.
And if the person is not complying, that officer has got to be thinking, is this person trying to hurt me? So, asking people to comply with the officer’s command — that’s a reasonable statement.
Cara Anthony: But, it’s well documented: Black Americans are more likely than our white peers to be perceived as dangerous by police.
That perception increases the chances we’ll be the victim of deadly force. Whether we comply — or not.
[Quiet, dark music ends.]
That’s all to say … even with the promise of more Black officers in Sikeston and all the chief’s other plans, I’m not sure institutional change in policing is coming soon to Sikeston.
[Sparse electronic music starts playing.]
Cara Anthony: I took that worry to Gail Christopher. She has spent her long career trying to address the causes of institutional racism.
Cara Anthony: We’ve been calling most of our guests by their first name, but what’s your preference? I don’t want to get in trouble with my mom on this, you know? [Cara laughs.]
Gail Christopher: If you don’t mind, Dr. Christopher is good.
Cara Anthony: OK. All right. That sounds good. I’m glad I asked.
Cara Anthony: Dr. Christopher thinks a lot about the connections between race and health. And she’s executive director of the National Collaborative for Health Equity. Her nonprofit designs strategies for social change.
She says the way to think about starting to fix structural racism … is to think about the future.
Gail Christopher: What do you want for your daughter? What do I want for my children? I want them not to have interactions with the police, No. 1, right?
Uh, so I want them to have safe places to be, to play, to be educated … equal access to the opportunity to be healthy.
Cara Anthony: But I wonder if that future is even possible.
[Sparse electronic music ends.]
Cara Anthony: Is there a cure for racism? And I know it’s not that simple, but is there a cure?
Gail Christopher: I love the question, right? And my answer to you would be yes. It is a process, and it’s not enough to march and get a victory. We have to transform the systems of inequity in this country.
Cara Anthony: And Dr. Christopher says it is possible. Because racism is a belief system.
[Hopeful instrumental music plays.]
Gail Christopher: There is a methodology that’s grounded in psychological research and social science for altering our beliefs and subsequently altering our behaviors that are driven by those beliefs.
Cara Anthony: To get there, she says, institutions need a rigorous commitment to look closely at what they are doing — and the outcomes they’re creating.
Gail Christopher: Data tracking and monitoring and being accountable for what’s going on.
We can’t solve a problem if we don’t admit that it exists.
Cara Anthony: One of her favorite examples of what it looks like to make a start toward systemic change comes from the health care world.
I know we’ve been talking about policing so far, but — bear with me here — we’re going to pivot to another way institutional bias kills people.
A few years ago, a team of researchers at the Brigham and Women’s Hospital in Boston reviewed admission records for patients with heart failure. They found that Black and Latinx people were less likely than white patients to be admitted to specialized cardiology units.
Gail Christopher: Without calling people racist, they saw the absolute data that showed that, wait a minute, we’re sending the white people to get the specialty care and we’re not sending the people of color.
Cara Anthony: So, Brigham and Women’s launched a pilot program.
When a doctor requests a bed for a Black or Latinx patient with heart failure, the computer system notifies them that, historically, Black and Latinx patients haven’t had equal access to specialty care.
The computer system then recommends the patient be admitted to the cardiology unit. It’s still up to the doctor to actually do that.
The hard data’s not published yet, but we checked in with the hospital, and they say the program seems to be making a difference.
Gail Christopher: It starts with leadership. Someone in that system has the authority and makes the decision to hold themselves accountable for new results.
[Hopeful instrumental music ends.]
Cara Anthony: OK, so it could be working at a hospital. Let’s shift back to policing now.
Gail Christopher: There should be an accountability board in that community, a citizens’ accountability board, where they are setting measurable and achievable goals and they are holding that police department accountable for achieving those goals.
Cara Anthony: But, like, do Black people have to participate in this? Because we’re tired.
Gail Christopher: Listen, do I know that we’re tired! Am I tired? After 50 years? Uh, I think that there is work that all people have to do. This business of learning to see ourselves in one another, to be fully human — it’s all of our work.
[Warm, optimistic instrumental music plays.]
Now, does that preclude checking out at times and taking care of yourself? I can’t tell you how many people my age who are no longer alive today, who were my colleagues and friends in the movement. But they died prematurely because of this lack of permission to take care of ourselves.
Cara Anthony: Rest when you need to, she says, but keep going.
Gail Christopher: We have to do that because it is our injury. It is our pain. And I think we have the stamina and the desire to see it change.
Cara Anthony: Yep. Heard. It’s all of our work.
Dr. Christopher has me thinking about all the Black people in Sikeston who aren’t sitting around waiting for someone else to change the institutions that are hurting them.
People protested when Denzel Taylor was killed even with all the pressure to stay quiet about it.
Protesters: Justice for Denzel on 3. 1, 2, 3 … Justice for Denzel! Again! 1, 2, 3 … Justice for Denzel!
Cara Anthony: And I’m thinking about the people who were living in the Sunset neighborhood of Sikeston in 1942 when Cleo Wright was lynched.
Harry Howard: They picked up rocks and bricks and crowbars and just anything to protect our community.
Cara Anthony: And Sunset did not burn.
[Warm, optimistic instrumental music begins fading out.]
[Piano starts warming up.]
Cara Anthony: After nearly 80 years of mostly staying quiet about Cleo’s lynching, Sikeston residents organized a service to mark what happened to him — and their community.
Reverend: We are so honored and humbled to be the host church this evening for the remembrance and reconciliation service of Mr. Cleo Wright.
[Piano plays along with Pershard singing.]
Pershard Owens: [Singing] It’s been a long, long time coming, but I know a change gonna come, oh yes it will. It’s been too hard a-livin but I’m afraid to die and I don’t know what’s up next, beyond the sky …
[Pershard singing and piano accompaniment fade out.]
Cara Anthony: I want to introduce you to that guy who was just singing then. His name is Pershard Owens.
Remember Rosemary Owens? The woman who told us about someone calling the police on her son and nephew when they were playing with their parents’ new cars? Pershard is Rosemary’s younger son.
Pershard Owens: Yeah, I definitely remember that.
Cara Anthony: Even after all this time, other people didn’t want to talk to us about it. We couldn’t find news coverage of the incident. But Pershard remembers. He was in his weekly karate practice when it happened. He was 10 or 11 years old.
Pershard Owens: My brother and cousin were, like, they were teens. So what do you think people are going to feel about the police when they do that, no questions asked, just guns drawn?
Cara Anthony: Pershard’s dad works as a police officer on a different police force in the Bootheel. Pershard knows police. But that didn’t make it any less scary for him.
Pershard Owens: You know, my parents still had to sit us down and talk and be like, “Hey, this is, that’s not OK, but you can’t, you can’t be a victim. You can’t be upset.” That’s how I was taught. So we acknowledge the past. But we don’t, we don’t stay down.
Cara Anthony: So years later, when Chief James McMillen started a program as a more formal way for people in Sikeston and the police to build better relationships, Pershard signed up. They started meeting in 2020.
The group is called Police and Community Together, or PACT for short.
[Sparse, tentative music begins playing.]
Pershard Owens: It was a little tense that first couple of meetings because nobody knew what it was going to be.
Cara Anthony: This was only five months after Sikeston police killed Denzel Taylor.
PACT is not a citizens’ accountability board. The police don’t have to answer to it.
The committee met every month. For a while. But they haven’t met in over a year now.
Pershard Owens: We would have steps forward and then we would have three steps back.
Cara Anthony: People have different accounts for why that is. Busy schedules. Mutual suspicion. Other things police officers have done that shook the trust of Black residents in Sikeston.
Pershard Owens: And people were like, bro, like, how can you work with these people?
The community is like, I can’t fully get behind it because I know what you did to my little cousin and them. Like, I know what the department did back in, you know, 15 years ago, and it’s hard to get past that.
So, I mean, I’m getting both sides, like, constantly, and listen, that is, that is tough.
[Sparse, tentative music ends.]
Cara Anthony: But Pershard says something important changed because he started working with PACT.
Pershard Owens: Chief did not like me at first [Pershard laughs]. He did not.
Chief didn’t … me and Chief did not see eye to eye. Because he had heard things about me and he — people had told him that I was, I was anti-police and hated police officers, and he came in with a defense up.
So, it took a minute for me and him to, like, start seeing each other in a different way. But it all happened when we sat down and had a conversation.
[Slow instrumental music begins playing.]
Cara Anthony: Just have a conversation. It sounds so simple; you’re probably rolling your eyes right now hearing it.
But Pershard says … it could be meaningful.
Pershard Owens: I truly want and believe that we can be together and we can work together and we can have a positive relationship where you see police and y’all dap each other up and y’all legit mean it. I think that can happen, but a lot of people have to change their mindsets.
Cara Anthony: That’s a challenge Pershard is offering to police AND community members: Have a conversation with someone different from you. See if that changes the way you think about the person you’re talking to. See if it changes your beliefs.
The more people do that, the more systems can change.
Pershard Owens: We got to look in the mirror and say, “Am I doing what I can to try and change the dynamic of Sikeston, even if it does hurt?”
Cara Anthony: Pershard says he’s going to keep putting himself out there. He ran for City Council in 2021. And even though he lost, he says he doesn’t regret it.
Pershard Owens: When you’re dealing with a place like Sikeston, it’s not going to change overnight.
Cara Anthony: And he’s glad he worked with PACT. Even if the community dialogue has fizzled for now, he’s pleased with the new relationship he built with Chief McMillen. And all of this has broadened his view of what kind of change is possible.
[Slow instrumental music ends.]
Pershard Owens: If you want something that has never been done, you have to go places that you’ve never been.
[“Silence in Sikeston” theme music plays.]
Cara Anthony: Places that you’ve never been … stories that you’ve never told out loud … maybe all of that helps build a Sikeston where Black residents can feel safer. Where Black people can live healthier lives.
A world you might not be able to imagine yet, but one that could exist for the next generation.
[“Silence in Sikeston” theme music ends.]
[Upbeat instrumental music plays.]
Cara Anthony: Thanks for listening to “Silence in Sikeston.”
Next, go watch the documentary — it’s a joint production from Retro Report and KFF Health News, presented in partnership with WORLD.
Subscribe to WORLD Channel on YouTube. That’s where you can find the film “Silence in Sikeston,” a Local, USA special.
If you made it this far, thank you. Let me know how you’re feeling.
I’d love to hear more about the conversations this podcast has sparked in your life. Leave us a voicemail at (202) 654-1366.
And thanks to everyone in Sikeston for sharing your stories with us.
This podcast is a co-production of WORLD Channel and KFF Health News and distributed by PRX.
It was produced with support from PRX and made possible in part by a grant from the John S. and James L. Knight Foundation.
This audio series was reported and hosted by me, Cara Anthony.
Audio production by me, Zach Dyer. And me, Taylor Cook.
Editing by me, Simone Popperl.
And me, managing editor Taunya English.
Sound design, mixing, and original music by me, Lonnie Ro.
Podcast art design by Colin Mahoney and Tania Castro-Daunais.
Tarena Lofton and Hannah Norman are engagement and social media producers for the show.
Oona Zenda and Lydia Zuraw are the landing page designers.
Lynne Shallcross is the photo editor, with photography from Michael B. Thomas.
Thank you to vocal coach Viki Merrick.
And thank you to my parents for all their support over the four years of this project.
Music in this episode is from Epidemic Sound and Blue Dot Sessions.
Some of the audio you heard across the podcast is also in the film.
For that, special thanks to Adam Zletz, Matt Gettemeier, Roger Herr, and Philip Geyelin.
Kyra Darnton is executive producer at Retro Report.
I was a producer on the film.
Jill Rosenbaum directed the documentary.
Kytja Weir is national editor at KFF Health News.
WORLD Channel’s editor-in-chief and executive producer is Chris Hastings.
Help us get the word out about “Silence in Sikeston.” Write a review or give us a quick rating wherever you listen to this podcast.
Thank you! It makes a difference.
Oh yeah! And tell your friends in real life too!
[Upbeat instrumental music ends.]
Credits
Taunya English
Managing editor
Taunya is deputy managing editor for broadcast at KFF Health News, where she leads enterprise audio projects.
Simone Popperl
Line editor
Simone is broadcast editor at KFF Health News, where she shapes stories that air on Marketplace, NPR, and CBS News Radio, and she co-manages a national reporting collaborative.
Zach Dyer
Senior producer
Zach is senior producer for audio with KFF Health News, where he supervises all levels of podcast production.
Taylor Cook
Associate producer
Taylor is an independent producer who does research, books guests, contributes writing, and fact-checks episodes for several KFF Health News podcasts.
Lonnie Ro
Sound designer
Lonnie Ro is an audio engineer and a composer who brings audio stories to life through original music and expert sound design for platforms like Spotify, Audible, and KFF Health News.
Additional Newsroom Support
Lynne Shallcross, photo editorOona Zenda, illustrator and web producerLydia Zuraw, web producerTarena Lofton, audience engagement producer Hannah Norman, video producer and visual reporter Chaseedaw Giles, audience engagement editor and digital strategistKytja Weir, national editor Mary Agnes Carey, managing editor Alex Wayne, executive editorDavid Rousseau, publisher Terry Byrne, copy chief Gabe Brison-Trezise, deputy copy chief Tammie Smith, communications officer
The “Silence in Sikeston” podcast is a production of KFF Health News and WORLD. Distributed by PRX. Subscribe and listen on Apple Podcasts, Spotify, Amazon Music, iHeart, or wherever you get your podcasts.
Watch the accompanying documentary from WORLD, Retro Report, and KFF here.
To hear other KFF Health News podcasts, click here.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 2 weeks ago
Mental Health, Multimedia, Race and Health, Rural Health, States, Missouri, Podcasts, Silence in Sikeston
Vance-Walz Debate Highlighted Clear Health Policy Differences
Ohio Republican Sen. JD Vance and Minnesota Democratic Gov. Tim Walz met in an Oct. 1 vice presidential debate hosted by CBS News that was cordial and heavy on policy discussion — a striking change from the Sept. 10 debate between Vice President Kamala Harris and former President Donald Trump.
Ohio Republican Sen. JD Vance and Minnesota Democratic Gov. Tim Walz met in an Oct. 1 vice presidential debate hosted by CBS News that was cordial and heavy on policy discussion — a striking change from the Sept. 10 debate between Vice President Kamala Harris and former President Donald Trump.
Vance and Walz acknowledged occasional agreement on policy points and respectfully addressed each other throughout the debate. But they were more pointed in their attacks on their rival’s running mate for challenges facing the country, including immigration and inflation.
The moderators, “CBS Evening News” anchor Norah O’Donnell and “Face the Nation” host Margaret Brennan, had said they planned to encourage candidates to fact-check each other, but sometimes clarified statements from the candidates.
After Vance made assertions about Springfield, Ohio, being overrun by “illegal immigrants,” Brennan pointed out that a large number of Haitian immigrants in Springfield, Ohio, are in the country legally. Vance objected and, eventually, CBS exercised the debate ground rule that allowed the network to cut off the candidates’ microphones.
Most points were not fact-checked in real time by the moderators. Vance resurfaced a recent health care theme — that as president, Donald Trump sought to save the Affordable Care Act — and acknowledged that he would support a national abortion ban.
Walz described how health care looked before the ACA compared with today. Vance offered details about Trump’s health care “concepts of a plan” — a reference to comments Trump made during the presidential debate that drew jeers and criticism for the former president, who for years said he had a plan to replace the ACA that never surfaced. Vance pointed to regulatory changes advanced during the Trump administration, used weedy phrases like “reinsurance regulations,” and floated the idea of allowing states “to experiment a little bit on how to cover both the chronically ill but the non-chronically ill.”
Walz responded with a quick quip: “Here’s where being an old guy gives you some history. I was there at the creation of the ACA.” He said that before then insurers had more power to kick people off their plans. Then he detailed Trump’s efforts to undo the ACA as well as why the law’s preexisting condition protections were important.
“What Sen. Vance just explained might be worse than a concept, because what he explained is pre-Obamacare,” Walz said.
The candidates sparred on numerous topics. Our PolitiFact partners fact-checked the debate here and on their live blog.
The health-related excerpts follow.
The Affordable Care Act:
Vance: “Donald Trump could have destroyed the [Affordable Care Act]. Instead, he worked in a bipartisan way to ensure that Americans had access to affordable care.”
As president, Trump worked to undermine and repeal the Affordable Care Act. He cut millions of dollars in federal funding for ACA outreach and navigators who help people sign up for health coverage. He enabled the sale of short-term health plans that don’t comply with the ACA consumer protections and allowed them to be sold for longer durations, which siphoned people away from the health law’s marketplaces.
Trump’s administration also backed state Medicaid waivers that imposed first-ever work requirements, reducing enrollment. He also ended insurance company subsidies that helped offset costs for low-income enrollees. He backed an unsuccessful repeal of the landmark 2010 health law and he backed the demise of a penalty imposed for failing to purchase health insurance.
Affordable Care Act enrollment declined by more than 2 million people during Trump’s presidency, and the number of uninsured Americans rose by 2.3 million, including 726,000 children, from 2016 to 2019, the U.S. Census Bureau reported; that includes three years of Trump’s presidency. The number of insured Americans rose again during the Biden administration.
Abortion and Reproductive Health:
Vance: “As I read the Minnesota law that [Walz] signed into law … it says that a doctor who presides over an abortion where the baby survives, the doctor is under no obligation to provide lifesaving care to a baby who survives a botched late-term abortion.”
Experts said cases in which a baby is born following an attempted abortion are rare. Less than 1% of abortions nationwide occur in the third trimester. And infanticide, the crime of killing a child within a year of its birth, is illegal in every state.
In May 2023, Walz, as Minnesota governor, signed legislation updating a state law for “infants who are born alive.” It said babies are “fully recognized” as human people and therefore protected under state law. The change did not alter regulations that already required doctors to provide patients with appropriate care.
Previously, state law said, “All reasonable measures consistent with good medical practice, including the compilation of appropriate medical records, shall be taken by the responsible medical personnel to preserve the life and health of the born alive infant.” The law was updated to instead say medical personnel must “care for the infant who is born alive.”
When there are fetal anomalies that make it likely the fetus will die before or soon after birth, some parents decide to terminate the pregnancy by inducing childbirth so that they can hold their dying baby, Democratic Minnesota state Sen. Erin Maye Quade told PolitiFact in September.
This update to the law means infants who are “born alive” receive appropriate medical care dependent on the pregnancy’s circumstances, Maye Quade said.
Vance supported a national abortion ban before becoming Trump’s running mate.
CBS News moderator Margaret Brennan told Vance, “You have supported a federal ban on abortion after 15 weeks. In fact, you said if someone can’t support legislation like that, quote, ‘you are making the United States the most barbaric pro-abortion regime anywhere in the entire world.’ My question is, why have you changed your position?”
Vance said that he “never supported a national ban” and, instead, previously supported setting “some minimum national standard.”
But in a January 2022 podcast interview, Vance said, “I certainly would like abortion to be illegal nationally.” In November, he told reporters that “we can’t give in to the idea that the federal Congress has no role in this matter.”
Since joining the Trump ticket, Vance has aligned his abortion rhetoric to match Trump’s and has said that abortion legislation should be left up to the states.
— Samantha Putterman of PolitiFact, on the live blog
A woman’s 2022 death in Georgia following the state passing its six-week abortion ban was deemed “preventable.”
Walz talked about the death of 28-year-old Amber Thurman, a Georgia woman who died after her care was delayed because of the state’s six-week abortion law. A judge called the law unconstitutional this week.
A Sept. 16 ProPublica report found that Thurman had taken abortion pills and encountered a rare complication. She sought care at Piedmont Henry Hospital in Atlanta to clear excess fetal tissue from her uterus, called a dilation and curettage, or D&C. The procedure is commonly used in abortions, and any doctor who violated Georgia’s law could be prosecuted and face up to a decade in prison.
Doctors waited 20 hours to finally operate, when Thurman’s organs were already failing, ProPublica reported. A panel of health experts tasked with examining pregnancy-related deaths to improve maternal health deemed Thurman’s death “preventable,” according to the report, and said the hospital’s delay in performing the procedure had a “large” impact.
— Samantha Putterman of PolitiFact, on the live blog
What Project 2025 Says About Some Forms of Contraception, Fertility Treatments
Walz said that Project 2025 would “make it more difficult, if not impossible, to get contraception and limit access, if not eliminate access, to fertility treatments.”
Mostly False. The Project 2025 document doesn’t call for restricting standard contraceptive methods, such as birth control pills, but it defines emergency contraceptives as “abortifacients” and says they should be eliminated from the Affordable Care Act’s covered preventive services. Emergency contraception, such as Plan B and ella, are not considered abortifacients, according to medical experts.
PolitiFact did not find any mention of in vitro fertilization throughout the document, or specific recommendations to curtail the practice in the U.S., but it contains language that supports legal rights for fetuses and embryos. Experts say this language can threaten family planning methods, including IVF and some forms of contraception.
— Samantha Putterman of PolitiFact, on the live blog
Walz: “Their Project 2025 is gonna have a registry of pregnancies.”
Project 2025 recommends that states submit more detailed abortion reporting to the federal government. It calls for more information about how and when abortions took place, as well as other statistics for miscarriages and stillbirths.
The manual does not mention, nor call for, a new federal agency tasked with registering pregnant women.
Fentanyl and Opioids:
Vance: “Kamala Harris let in fentanyl into our communities at record levels.”
Mostly False.
Illicit fentanyl seizures have been rising for years and reached record highs under Biden’s administration. In fiscal year 2015, for example, U.S. Customs and Border Protection seized 70 pounds of fentanyl. As of August 2024, agents have seized more than 19,000 pounds of fentanyl in fiscal year 2024, which ended in September.
But these are fentanyl seizures — not the amount of the narcotic being “let” into the United States.
Vance made this claim while criticizing Harris’ immigration policies. But fentanyl enters the U.S. through the southern border mainly at official ports of entry. It’s mostly smuggled in by U.S. citizens, according to the U.S. Sentencing Commission. Most illicit fentanyl in the U.S. comes from Mexico made with chemicals from Chinese labs.
Drug policy experts have said that the illicit fentanyl crisis began years before Biden’s administration and that Biden’s border policies are not to blame for overdose deaths.
Experts have also said Congress plays a role in reducing illicit fentanyl. Congressional funding for more vehicle scanners would help law enforcement seize more of the fentanyl that comes into the U.S. Harris has called for increased enforcement against illicit fentanyl use.
Walz: “And the good news on this is, is the last 12 months saw the largest decrease in opioid deaths in our nation’s history.”
Mostly True.
Overdose deaths involving opioids decreased from an estimated 84,181 in 2022 to 81,083 in 2023, based on the most recent provisional data from the Centers for Disease Control and Prevention. This decrease, which took place in the second half of 2023, followed a 67% increase in opioid-related deaths between 2017 and 2023.
The U.S. had an estimated 107,543 drug overdose deaths in 2023 — a 3% decrease from the 111,029 deaths estimated in 2022. This is the first annual decrease in overall drug overdose deaths since 2018. Nevertheless, the opioid death toll remains much higher than just a few years ago, according to KFF.
More Health-Related Comments:
Vance Said ‘Hospitals Are Overwhelmed.’ Local Officials Disagree.
We asked health officials ahead of the debate what they thought about Vance’s claims about Springfield’s emergency rooms being overwhelmed.
“This claim is not accurate,” said Chris Cook, health commissioner for Springfield’s Clark County.
Comparison data from the Centers for Medicare & Medicaid Services tracks how many patients are “left without being seen” as part of its effort to characterize whether ERs are able to handle their patient loads. High percentages usually signal that the facility doesn’t have the staff or resources to provide timely and effective emergency care.
Cook said that the full-service hospital, Mercy Health Springfield Regional Medical Center, reports its emergency department is at or better than industry standard when it comes to this metric.
In July 2024, 3% of Mercy Health’s patients were counted in the “left-without-being-seen” category — the same level as both the state and national average for high-volume hospitals. In July 2019, Mercy Health tallied 2% of patients who “left without being seen.” That year, the state and national averages were 1% and 2%, respectively. Another CMS 2024 data point shows Mercy Health patients spent less time in the ER per visit on average — 152 minutes — compared with state and national figures: 183 minutes and 211 minutes, respectively. Even so, Springfield Regional Medical Center’s Jennifer Robinson noted that Mercy Health has seen high utilization of women’s health, emergency, and primary care services.
— Stephanie Armour, Holly Hacker, and Stephanie Stapleton of KFF Health News, on the live blog
Minnesota’s Paid Leave Takes Effect in 2026
Walz signed paid family leave into law in 2023 and it will take effect in 2026.
The law will provide employees up to 12 weeks of paid medical leave and up to 12 weeks of paid family leave, which includes bonding with a child, caring for a family member, supporting survivors of domestic violence or sexual assault, and supporting active-duty deployments. A maximum 20 weeks are available in a benefit year if someone takes both medical and family leave.
Minnesota used a projected budget surplus to jump-start the program; funding will then shift to a payroll tax split between employers and workers.
— Amy Sherman of PolitiFact, on the live blog
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 3 weeks ago
Elections, Health Care Costs, Insurance, States, Abortion, Children's Health, Contraception, Guns, Hospitals, Immigrants, KFF Health News & PolitiFact HealthCheck, Minnesota, Obamacare Plans, Ohio, Opioids, Substance Misuse, Women's Health
KFF Health News' 'What the Health?': Congress Punts to a Looming Lame-Duck Session
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
Congress has left Washington for the campaign trail, but after the Nov. 5 general election lawmakers will have to complete work on the annual spending bills for the fiscal year that starts Oct. 1. While the GOP had hoped to push spending decisions into 2025, Democrats forced a short-term spending patch that’s set to expire before Christmas.
Meanwhile, on the campaign trail, abortion continues to be among the hottest issues. Democrats are pressing their advantage with women voters while Republicans struggle — with apparently mixed effects — to neutralize it.
This week’s panelists are Julie Rovner of KFF Health News, Joanne Kenen of Politico and the Johns Hopkins schools of nursing and public health, Alice Miranda Ollstein of Politico, and Lauren Weber of The Washington Post.
Panelists
Joanne Kenen
Johns Hopkins University and Politico
Alice Miranda Ollstein
Politico
Lauren Weber
The Washington Post
Among the takeaways from this week’s episode:
- When Congress returns after the election, there’s a chance lawmakers could then make progress on government spending and more consensus health priorities, like expanding telehealth access. After all, after the midterm elections in 2022, Congress passed federal patient protections against surprise medical billing.
- As Election Day approaches, Democrats are banging the drum on health care — which polls show is a winning issue for the party with voters. This week, Democrats made a last push to extend Affordable Care Act subsidies expanded during the pandemic — an issue that will likely drag into next year in the face of Republican opposition.
- The outcry over the first reported deaths tied to state abortion bans seems to be resonating on the campaign trail. With some states offering the chance to weigh in on abortion access via ballot measures, advocates are telling voters: These tragedies are examples of what happens when you leave abortion access to the states.
- And Sen. Bernie Sanders of Vermont summoned the chief executive of Novo Nordisk before the health committee he chairs this week to demand accountability for high drug prices. Despite centering on a campaign issue, the hearing — like other examples of pharmaceutical executives being thrust into the congressional hot seat — yielded no concessions.
Plus, for “extra credit” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: KFF Health News’ “How North Carolina Made Its Hospitals Do Something About Medical Debt,” by Noam N. Levey and Ames Alexander, The Charlotte Observer.
Lauren Weber: Stat’s “How the Next President Should Reform Medicare,” by Paul Ginsburg and Steve Lieberman.
Joanne Kenen: The Atlantic’s “The Woo-Woo Caucus Meets,” by Elaine Godfrey.
Alice Miranda Ollstein: Stat’s “How Special Olympics Kickstarted the Push for Better Disability Data,” by Timmy Broderick.
Also mentioned on this week’s podcast:
- KFF Health News’ “Florida’s New Covid Booster Guidance Is Straight-Up Misinformation,” by Arthur Allen, Daniel Chang, and Sam Whitehead.
- KFF Health News’ “Feds Killed Plan To Curb Medicare Advantage Overbilling After Industry Opposition,” by Fred Schulte.
- KFF Health News’ “Audits — Hidden Until Now — Reveal Millions in Medicare Advantage Overcharges,” by Fred Schulte and Holly K. Hacker.
- KFF Health News’ “ACA Plans Are Being Switched Without Enrollees’ OK,” by Julie Appleby.
- KFF Health News’ “Biden Administration Tightens Broker Access to Healthcare.gov To Thwart Rogue Sign-Ups,” by Julie Appleby.
click to open the transcript
Transcript: Congress Punts to a Looming Lame-Duck Session
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello, and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News, and I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, September 26th, at 10 a.m. As always, news happens fast, and things might have changed by the time you hear this. So, here we go.
Today we are joined via teleconference by Lauren Weber of The Washington Post.
Lauren Weber: Hello hello.
Rovner: Alice Ollstein of Politico.
Alice Miranda Ollstein: Good morning.
Rovner: And Joanne Kenen of the Johns Hopkins Schools of Public Health and Nursing, and Politico.
Joanne Kenen: Hi, everybody.
Rovner: Big props to Emmarie for hosting last week while I was in Ann Arbor at the Michigan Daily reunion. I had a great time, but I brought back an unwelcome souvenir in the form of my first confirmed case of covid. So apologies in advance for the state of my voice. Now, let us get to the news.
To steal a headline from Politico earlier this week, Congress lined up in punt formation, passing a continuing resolution that will require them to come back after the election for what could be a busy lame-duck session. Somebody remind us who wanted this outcome — the Let’s only do the CR through December — and who wanted it to go into next year? Come on, easy question.
Ollstein: Well, the kicking it to right before Christmas, which sets up the stage for what we’ve seen so many times before where it just gets jammed through and people who have objections, generally conservatives who want to slash spending and add on a bunch of policy riders, which they tried and failed to do this time, will have a weaker base to operate from, given that everybody wants to go home for the holidays.
And so once again, we’re seeing people mad at Speaker Mike Johnson, who, again and again, even though he is fully from the hard right of the party, is not catering to their priorities as much as they would like. And so obviously his speakership depends on which party wins control of the House in November. But I think even if Republicans win control, I’m already starting to hear rumblings of throwing him overboard and replacing with someone who they think will cater to them more.
Rovner: It was so déjà vu all over again, which is, last year, as we approached October 1st and the Republican House could not pass any kind of a continuing resolution with just Republican votes, that eventually Kevin McCarthy had to turn to Democrats, and that’s how he lost his job.
And yet that’s exactly what happened here, which is the Republicans wanted to go until March, I guess on the theory that they were betting that they would be in full power in March and would have a chance to do a lot more of what they wanted in terms of spending bills than if they just wait and do it in the lame duck. And yet the speaker doesn’t seem to be paying the same price that Kevin McCarthy did. Is that just acknowledgment on the part of the right wing that they can’t do anything with their teeny tiny majority?
Kenen: I mean, yes, it’s pretty stalemate-y up there right now, and nobody is certain who’s going to control the House, and at this point it is likely to still be a narrow majority, whoever wins it. I mean, they’re six weeks out. Things can change. This has been an insane year. Nobody’s making predictions, but it looks like pretty divided.
Rovner: Whoever wins isn’t going to win by much.
Kenen: We have a pretty divided country, and the likelihood is we’re going to have a pretty divided House. So the dynamic will change depending on who’s in charge, but the Republicans are more fractious and divided right now than the Democrats, although that’s really easy to change, and even the Democrats have gone through their rambunctious divided phases, too.
Everybody just doesn’t know what’s next, because the top of the ticket is going to change things. So the more months you push out, the less money you’re spending. If you control the CR, if you make the CR, the continuing resolution, meaning current spending levels for six months, it’s a win for the Republicans in many ways because they’re keeping — they’re preventing increases. But in terms of policy, both sides get some of the things they want extended.
I don’t know if you can call it a productive stalemate. That’s sort of a contradiction in terms. But I mean, for the Republicans, longer, it would’ve been better.
Rovner: So now that we know that Congress has to come back after the election, there’s obviously things that they are able to do other than just the spending bills. And I’m thinking of a lot of unfinished health legislation like the telehealth extensions and the constant, Are we going to do something about pharmacy benefit managers? which has been this bipartisan issue that they never seem to solve.
I would remind the listeners that in 2022 after the election, that’s when they finally did the surprise-bills legislation. So doing big things in the lame duck is not unheard of. Is there anything any of you are particularly looking toward this time that might actually happen?
Kenen: It’s something like telehealth because it’s not that controversial. I mean, it’s easiest to get something through in — in lame duck, you want to get some things off the plate that are either overdue and need to be taken care of or that you don’t want hanging over you next year. So telehealth, which is, there are questions about does it save money, et cetera, and what form it should take and how some of it should be regulated, so forth, but the basic idea, telehealth is popular. Something like that, yes.
PBMs [pharmacy benefit managers] is a lot harder, where there is some agreement on the need to do something but there’s less agreement about what that something should look like. So although I’m not personally covering that day-to-day basis, in any sense, that’s harder. The more consensus there is and the fewer moving parts, the easier it is to do, as a rule. I mean, sometimes they do get something big done in lame duck, but a lot of it gets kicked.
And also there’s a huge, huge, huge tax fight next year, and it’s going to require a lot of wheeling and dealing no matter what shape it takes, because it’s expiring and things have to be either renewed or allowed to die. So that’s just going to be mega-enormous, and a lot of this stuff become bargaining chips in that larger debate, and that becomes the dominant domestic policy vehicle next year.
Rovner: Well, even before we get to the lame duck, we have to finish the campaign, which is only a month and a half away. And we are still talking about the Affordable Care Act in an election where it was not going to be a campaign issue, everybody said.
I know that you talked last week about all the specifics of the ways former President [Donald] Trump actually tried to sabotage rather than save the ACA and all the ways what [Sen.] JD Vance was talking about on “Meet the Press,” dividing up risk pools once again so sicker people would no longer be subsidized by the less sick, would turn the clock back to the individual insurance market as it existed before 2014.
Now the Democrats in the Senate are taking one last shot at the ACA with a bill — that will fail — to renew the expanded marketplace subsidies, so it will expire unless Congress acts by the end of next year. Might this last effort have some impact in the swing states, or is it just a lot more campaign noise?
Weber: I think this is a lot of campaign noise, to some extent. I mean, I think Democrats are clear in polling shows that the average American voter does trust Democrats more than Republicans on ACA and health issues and health insurance. So I do think this is a messaging push in part by the Dems to speak to voters. As we all know, this is a turnout election, so I think anything that they feel like voters care about, which often has to do with their pocketbook, I think they’re going to lead the drum on.
I do think it’s interesting again that JD Vance really is reiterating a talking point that Donald Trump used in the debate, which is that he said he had improved the ACA and many experts would say it was very much the opposite. Again, I think I did this on the last podcast, but let me reread this because I think it’s important as a fact check. Most of the Trump administration’s ACA-related actions included cutting the program.
So they reduced millions of dollars of funding for marketing and enrollment, and he repeatedly tried to overturn the law. So I think some of the messaging around this is getting convoluted, in part because it’s an election year, to your point.
Rovner: And because it’s popular. Because Nancy Pelosi was right. When people found out what was in it, it got popular.
Kenen: I think there are two things. I mean, I agree with what Lauren just said, but the Democrats came out in favor of extending the subsidies yesterday, which not only changed the eligibility criteria — more people, more higher up the middle-income chain could get subsidized — but also everybody in it had extra benefits for it, including people who were already covered. But it’s better for them.
The idea that Republicans are going to try to take that benefit away from people six weeks before an election — they were probably not. How they handle it next year? I was really surprised by the silence yesterday. The Democrats rolled out their plans for renewing this, and I didn’t see a lot of Republican pushback. So they were really quiet about it.
The other thing that struck me is that JD Vance went on on this risk pool thing last week on “Meet the Press” and in Raleigh, in North Carolina, and then there was pushback. And on that particular point, there’s been silence for the last week. I don’t think he stuck his neck out on that one again. Who knows what next week will bring, but it didn’t continue, and nor did I hear other Republicans saying, “Yeah, let’s go do that.”
So if that was a trial balloon, it was somewhat leaden. So I think that we really don’t know how the subsidy fight is going to play —how or when the subsidy fight will play out. It’s really, you know, we’ve all said many times before, once you give people the benefit, it’s really hard to take it away. And—
Rovner: Although we did that with the Child Tax Credit. We gave everybody the Child Tax Credit and then took it away.
Kenen: We did, and other things that were temporary during the pandemic, and we’ll just see how many of those temporary things do in fact go away. I mean, does it come back next year? I mean, now SALT [state and local taxes], right? I mean, Trump backed backing what’s called SALT. It’s a limit based on mortgage and state taxes. And now he’s talking about he’s going to rescue that like it wasn’t him who … So it all comes around again.
Ollstein: Yeah, and I think what you’re seeing is both sides drawing the battle lines for next year and signaling what the core arguments are going to be. And so you had Democrats come out with their bill this year, and you are hearing a lot of Republicans in hearings and speeches sprinkled around talking about claiming that there is a huge amount of fraud in the ACA marketplaces and linking that to the subsidies and saying, Why would we continue to subsidize something where there’s all this fraud?
I think that is going to be a big argument on that side next year for not extending the subsidies. So I would urge people to keep listening for that.
Kenen: And that came from a conservative think tank consulting firm in which they blame — I actually happened to read it this week, so it’s fresh in my mind. They’re blaming the fraud actually on brokers rather than individuals. They’re saying that people are—
Rovner: That was an investigation uncovered by my colleague Julie Appleby here at KFF Health News.
Kenen: Right. And they ran with that, and they were talking about the low end of the income bracket. And I’m waiting for the sequel in which the people at the upper end of the income bracket, which is the law that’s expiring that we’re talking about, it’s pretty — I’m waiting for the sequel Paragon paper saying, See, it’s even worse at the upper end, and that’s easy to get rid of because it’ll expire. That’s the argument of the day, but there’s so many flavors of anti-ACA arguments that we’ve just scratched the beginning of this round.
Rovner: Exactly. It’ll come back. All right, well, let us move on to abortion. Vice President [Kamala] Harris said in an interview this week that she would support ending the filibuster in the Senate in order to restore abortion rights with 51 rather than 60 votes, which has apparently cost her the endorsement of retiring West Virginia Democratic senator Joe Manchin. Was Manchin’s endorsement even that valuable to her? It’s not like West Virginia was going to vote Democratic anytime soon.
Ollstein: The Harris campaign has really leaned into emphasizing endorsements she’s been getting from across the ideological spectrum, from as far right as Dick Cheney to more centrist types and economists and national security people. And so she’s clearly trying to brandish her centrist credentials. So I guess in that sense. But like you said, Democrats are not going to win West Virginia, and so I think also he was getting upset about something, a position she’s been voicing for years now. This is not new, this question of the filibuster. So I doubt it’ll have much of an impact.
Kenen: It’s a real careful-what-you-wish for, because if the Senate goes Republican, which at the moment looks like it’s going to be a narrow Republican majority. We don’t know until November. There’s always a surprise. There’s always a surprise.
Rovner: You’re right. It’s more likely that it’ll be 51-49 Republican than it’ll be 51-49 Democrat.
Kenen: Right. So if the filibuster is going to be abolished, it would be to advance Republican conservative goals. So it’s sort of dangerous territory to walk into right now. The Democrats have played with abolishing the filibuster. They wanted to do it for voting rights issues, and they decided not to go there on legislation. They did modify it a number of years ago on judicial appointments and other Cabinet appointments and so forth.
But legislative, the filibuster still exists. It’s very, very, very heavily used, much more than historically, by both parties, whoever is in power. So changing it would be a really radical change in how things move or don’t move. So it could have a long tail, that remark.
Rovner: Meanwhile, Senate Democrats, who don’t have the votes now, as we know, to abolish the filibuster, because Manchin is among their one-vote margin, are continuing to press Republicans on reproductive rights issues that they think work in their favor. Earlier this week, the Senate Finance Committee had a hearing on EMTALA, the Emergency Medical Treatment and Labor Act.
It’s a federal law that’s supposed to guarantee women access to abortion in medical emergencies. But in practice, it has not. Last week we talked about the ProPublica stories on women whose pregnancy complications actually did lead to their death. Is this something that’s breaking through as a campaign issue? I do feel like we’ve seen so much more on pregnancy complications and the health impacts of those rather than just, straight, women who want to end pregnancies.
Ollstein: I just got back from Michigan, and I would say it is having a big impact. I was really interested in how Democrats were trying to campaign on abortion in Michigan, even now that the state does have protections. And I heard over and over from voters and candidates that Trump’s leave-it-to-the-states stance, they really are still energized by that.
They’re not mollified by that, because they are pointing to stories like the ones that just came out in Georgia and saying: See? That’s what happens when you leave it to the states. We may be fine, but we care about more than just ourselves. We’re going to vote based on our concern for women in other states as well. I found that really interesting to be hearing out in the field.
Rovner: Lauren, you want to add something?
Weber: Yeah, I just was going to add, I mean, Harris obviously highlighted this effectively in the debate, and I think that has helped bring it to more of a crescendo, but there’s obviously been a lot of reporting for months on this. I mean, the AP has talked about — I think they did a count. It’s over 100 women, at least, have been denied emergency care due to laws like this.
I’d be curious — and it sounds like Alice has this, for voters that are in swing states, that it’s breaking through to — I’d be curious how much this has siloed to people that are outraged by this, and so we’re hearing it and how much it’s skidding down to those that — the Republican talking points have been that these are rare, they don’t really happen, it’s a liberal push to get against this. I’d be curious how much it’s breaking through to folks of all stripes.
Rovner: I watched a big chunk of the Finance Committee hearing, and the anti-abortion witnesses were saying this is not how it worked, that ectopic pregnancies, pregnancy complications do not qualify as abortions, and basically just denying that it happened. They’re sitting here. They’re sitting at the witness table with the woman to whom this happened and saying that this does not happen. So it was a little bit difficult, shall we say. Go ahead.
Ollstein: Well, and the pushback I’ve been hearing from the anti-abortion side is less that it’s not happening and more that it’s not the fault of the laws, it’s the fault of the doctors. They are claiming that doctors are either intentionally withholding care or are wrong in their interpretation of the law and are withholding care for that reason. They’re pointing to the letter of the law and saying, Oh no, it doesn’t say let women bleed out and die, so clearly it’s fine. They’re not really grappling with the chilling effect it’s having.
Rovner: Although we do know that in Texas when, I think it was Amanda Zurawski, there was — no, it was Kate Cox who actually got a judge to say she should be allowed to have an abortion. Ken Paxton, the Texas attorney general, then threatened the hospital, said, If you do this, I will come after you. On the one hand, they say, Well, that’s not what the law says. On the other hand, there are people saying, Yeah, that’s what the law says.
Turning to the Republicans, Donald Trump had some more things to say about abortion this week, including that he is women’s protector and that women will, and I quote, “be happy, healthy, confident, and free. You will no longer be thinking about abortion.”
If that wasn’t enough, in Ohio, Bernie Moreno, who’s the Republican running against Senator Sherrod Brown in the otherwise very red state, said the other night that he doesn’t understand why women over 50 would even care about abortion, since, he suggested, they can no longer get pregnant, which isn’t correct, by the way. But who exactly are the voters that Trump and Moreno are going after here?
Kenen: Moreno is already lagging in the polls. Sherrod Brown is a pretty liberal Democrat in an increasingly conservative state, and he’s also very popular. And it looks like he’s on a glide path to win, and this probably made it easier for him to win. And there are men who support abortion rights, and there are women who oppose.
I mean, this country’s divided on abortion, but it’s not age-related. It’s not like if you’re under 50 and female, you care about abortion and nobody else does. I mean, that’s really not the way it works. Fifty-year-old and older women, some of whom had abortions when they were younger, would want that right for younger women, including their daughters. It’s not a quadrant. It’s not like, oh, only this segment cares.
Ollstein: It’s interesting that it comes amid Democrats really working to broaden who they consider an abortion voter, like I said, trying to encourage people in states where abortion is protected to vote for people in states where abortion is not protected and doing more outreach to men and saying this is a family issue, not just a women’s issue, and this affects everybody.
So as you see Democrats trying to broaden their outreach and get more people to care, you have Bernie Moreno saying the opposite, saying, I don’t understand why people care when it doesn’t affect their own particular life and situation.
Rovner: Although I will say, having listened to a bunch of interviews with undecided voters in the last couple of weeks, I do hear more and more voters saying: Well, such and such candidate, and this is on both sides, is not speaking to me. It’s almost like this election is about them individually and not about society writ large.
And I do hear that on both sides, and it’s kind of a surprise. And I don’t know, is that maybe where Moreno is coming from? Maybe that’s what he’s hearing, too, from his pollsters? It’s only that people are most interested in their own self-interest and not about others? Lauren, you wanted to add to that?
Weber: I mean, I would just say I think that’s a kind interpretation, Julie. I think that more likely than not, he was just speaking out of turn. And in some prior reporting I did this year on misinformation around birth control and contraception, I spoke to a bunch of women legislators, I believe it was in Idaho, who found that in speaking with their male legislator friends, that a lot of them were uncomfortable talking about abortion, birth control, et cetera, which led to a lot of these misconceptions. And I wonder if we’re seeing that here.
Ollstein: Just quickly, I think it’s also reflective of a particular conservative mind-set. I mean, it reminds me of when I was covering the Obamacare fight in Congress and you had Republican lawmakers making jokes about, Oh, well, wouldn’t want to lose coverage for my mammograms. And just what we were just talking about, about the separate risk pools and saying, Oh, I’m healthy. Why should I subsidize a sick person? when that’s literally how insurance works.
But I think just the very individualistic go-it-alone, rugged-individual mind-set is coming out here in different ways. And so it seems like he did not want this particular comment to be scrutinized as it is getting now, but I think we hear versions of this from conservative lawmakers all the time in terms of, Why should I have to care about, pay for, subsidize, et cetera, other people in society?
Rovner: Yeah, there’s a lot of that. Well, finally this week in reproductive health issues that never seem to go away, a federal judge in North Dakota this week slapped an injunction on the Equal Employment Opportunity Commission’s enforcement of some provisions of the 2022 Pregnant Workers Fairness Act, ruling that Catholic employers, including for-profit Catholic-owned entities, don’t have to provide workers with time off for abortions or fertility treatments that violate the church’s teachings.
Now, lest you think this only applies to North Dakota, it does not. There’s a long way to go before this ruling is made permanent, but it’s kind of awkward timing for Republicans when they’re trying to convince voters of their strong support of IVF [in vitro fertilization], and yet here we have a large Catholic entity saying, We don’t even want to give our workers time off for IVF.
Ollstein: Yeah, I think you’ve been hearing a lot of Republicans scoffing at the idea that anyone would oppose IVF, when there are many, many conservatives who do either oppose it in its entirety or oppose certain ways that it is currently commonly practiced. You had the Southern Baptist Convention vote earlier this year in opposition to IVF. You have these Catholic groups who are suing over it.
And so I think there needs to be a real reckoning with the level of opposition there is on the right, and I think that’s why you’re seeing an interesting response to Trump’s promise for free IVF for all and whether or not that is feasible. I think this shows that it would get a lot of pushback from groups on the right if they were ever to pursue that.
Rovner: Yeah, I will also note that this was a Trump-appointed judge, which is pretty … The EEOC, when they were doing these final regulations, acknowledged that there will be cases of religious employers and that they will look at those on a case-by-case basis. But this is a pretty sweeping ruling that basically says, we’re back to the Hobby Lobby Supreme Court case: If you don’t believe in something, you don’t have to do it.
I mean, that’s essentially where we are with this, and we will see as this moves forward. Well, moving on to another big election issue, drug prices, the CEO of Novo Nordisk, makers of the blockbuster obesity and diabetes drugs Ozempic and Wegovy, appeared at the Senate Health, Education, Labor and Pensions Committee on Tuesday in front of Senator Bernie Sanders, who has been one of their top critics.
And maybe it’s just my covid-addled brain, but I watched this hearing and I couldn’t make heads or tails of how Lars Jørgensen, the CEO, tried to explain why either the differences between prices in the U.S. and other countries for these drugs weren’t really that big, or how the prices here are actually the fault of PBMs, not his company. Was anybody able to follow this? It was super confusing, I will say, that he tried to …
First he says that, well, 80% of the people with insurance coverage can get these drugs for $25 a month or less, which I’m pretty sure only applies to people who are using it for diabetes, not for obesity, because I think most insurers aren’t covering it for obesity. And there was much backing and forthing about how much it costs and how much we pay and how much it would cost the country to actually allow people, everybody who’s eligible for these drugs, to use them. And no real response. I mean, this is a big-deal campaign issue, and yet I feel like this hearing was something of a bust.
Weber: I mean, do we really expect a CEO of a highly profitable drug to promise to reduce it immediately on the spot? I mean, I guess I’m not surprised that the hearing was a back-and-forth. From what I understand of what happened, I mean, most hearings with folks that have highly lucrative drugs, they’re not looking to give away pieces of the lucrative drugs. So I think to some extent we come back to that.
But I did think what was interesting about the hearing itself was that Sanders did confront him with promises from PBMs that they would be able to offer these drugs and not short the American consumer, which was actually a fascinating tactic on Sanders part. But again, what did we really walk away with? I’m not sure that we know.
Rovner: Yeah, I mean, even if you were interested in this issue — and I’m interested in this issue and I know this issue better than the average person, as I said —I literally could not follow it. I found it super frustrating. I mean, I know what Sanders was going for here. I just don’t feel like he got what he was hoping to. I don’t know. Maybe he was hoping to get the CEO to say, “We’ve been awful, and so many people need this drug, and we’re going to cut the price tomorrow.” And yes, you point out, Lauren, that did not happen. But we shall see.
Well, speaking of PBMs, the Federal Trade Commission late last week filed an administrative complaint against the nation’s three largest PBMs, accusing them of inflating insulin prices and steering patients toward higher-cost products so they, the PBMs, can make more money, which is, of course, the big problem with PBMs, which is that they get a piece of the action. So the more expensive the drug, the bigger the piece of the action that they get.
I was most interested in the fact that the FTC’s three Democratic appointees voted in favor of the legal action. Its two Republican appointees didn’t vote but actually recused themselves. This whole PBM issue is kind of awkward for Republicans who say they want to fight high drug prices, isn’t it? I feel like the whole PBM issue, which, as we said, is something that Congress in theory wants to get to during the lame-duck session, is tricky.
I mean, it’s less tricky for Democrats who can just demagogue it and a little bit more tricky for Republicans who tend to have more support from both the drug industry and the insurance industry and the PBM industry. How much can they say they want to fight high drug prices without irritating the people with whom they are allied?
Kenen: And the PBMs themselves are owned by insurers. The pharmaceutical drug pricing, it’s really, really, really confusing, right?
Rovner: Nobody understands it.
Kenen: The four of us, none of us cover pharma full time, but the four of us are all pretty sophisticated health care reporters. And if we had to take a final exam on the drug industry, none of us would probably get an A-plus. So I’d be surprised if they figure this out in lame duck. I mean, they could —there’s always the possibility that when they look at the outcome of things, they decide: We do need to cut a deal and get this off the plate. This is the best we’re going to get. We’re going to be in a worse position next month. And they do it.
But it just seems really sticky and complicated, and it doesn’t feel like it’s totally jelled yet to the point that they can move it. I would expect this to spill into next year. If a deal comes through, if a big budget deal comes through at the end of the year, it does have a lot of trade-offs and moving parts, and this could, in fact, get wrapped into it.
If I had to guess, I would say it’s more likely to spill into the following year, but maybe they’ve decided they’ve had enough and want to tie the bow on it and move on. And then it’ll go to court and we’ll spend the next year talking about the court fight against the PBM law. So it’s not going to be gone one way or another, and nor are high drug prices going to be gone one way or another.
Rovner: The issue that keeps on giving. Well, finally this week, a new entry in out This Week in Health Misinformation segment from, surprise, Florida. This is a story from my KFF Health News colleagues Arthur Allen, Daniel Chang, and Sam Whitehead. And the headline kind of says it all: “Florida’s New Covid Booster Guidance Is Straight-Up Misinformation.”
This is the continuing saga involving the state surgeon general, Joseph Ladapo, who’s been talking down the mRNA covid vaccine for several years now and is recommending that people at high risk from covid not get the latest booster. What surprised me about this story, though, was how reluctant other health leaders in Florida, including the Florida Medical Association, have been to call the surgeon general out on this.
I guess to avoid angering his boss, Republican governor Ron DeSantis, who’s known to respond to criticism with retribution. Anybody else surprised by the lack of pushback to this there in Florida? Lauren?
Weber: No, I’m not really surprised. I mean, we’ve seen the same thing over and over and over again. I mean, this is the man who really didn’t make a push to vaccinate against measles when there was an outbreak. He has previously stated that seniors over 65 should not get an mRNA vaccine, with misinformation about DNA fragments. We’ve seen this pattern over and over again.
He is a bit of a rogue state public health officer in a crew that usually everyone else is on pretty much the same page, whether or not they’re red- or blue-state public health officers. And I think what’s interesting about this story and what continues to be interesting is as we see RFK [Robert F. Kennedy Jr.] gaining influence, obviously, in Trump’s potential health picks, you do wonder if this is a bit of a tryout. Although Ladapo is tied to DeSantis, who Trump obviously has feelings about. So who knows there. But it very clearly is the politicization of public health writ large.
Kenen: And DeSantis, during the beginning of the pandemic, he disagreed with the CDC [Centers for Disease Control and Prevention] guidelines about who should get vaccinated, but he did push them for older people. And I think that was his cutoff. If you’re 15 up, you should have them. He was quite negative from the start on under. Florida’s vaccination rates for the older population back when they rolled out in late 2020, early 2021, were not — they were fairly high. And there’s been a change of tone. As the political base became more anti-vax, so did the Florida state government.
Rovner: And obviously, Florida, full of older people who vote. So, I mean, super-important constituency there. Well, we will watch that space. All right, that is this week’s news. Now it is time for our extra credits. That’s when we each recommend a story we read this week we think you should read, too. Don’t worry if you miss the details. We will include links to all these stories in our show notes on your phone or other device. Joanne, why don’t you go first this week?
Kenen: Elaine Godfrey in the Atlantic has a story called “The Woo-Woo Caucus Meets,” and it’s about a four-hour summit on the Hill with RFK Jr., moderated by Senator Ron Johnson of Wisconsin, who also has some unconventional ideas about vaccination and public health. The writer called it the “crunch-ificiation of conservatism.”
It was the merging of the anti-vax pharma-skeptic left and the Trump right and RFK Jr. talking about MAHA, Making America Healthy Again, and his priorities for what he expects to be a leading figure in some capacity in a Trump administration fixing our health. It was a really fun — just a little bit of sarcasm in that story, but it was a good read.
Rovner: Yeah, and I would point out that this goes, I mean, back more than two decades, which is that the anti-vax movement has always been this combination of the far left and the far right.
Kenen: But it’s changed now. I mean, the medical liberty movement, medical freedom movement and the libertarian streak has changed. It started changing before covid, but it’s not the same as it was a few years ago. It’s much more conservative-dominated, or conservative-slash-libertarian-dominated.
Rovner: Alice.
Ollstein: I have an interesting story from Stat. It’s called “How Special Olympics Kickstarted the Push for Better Disability Data.” It’s about how the Special Olympics, which just happened, over the years have helped shine a light on just how many people with developmental and intellectual disabilities just aren’t getting the health care that they need and aren’t even getting recognized as having those disabilities.
And the data we’re using today comes from the Clinton administration still. It’s way out of date. So there have been improvements because of these programs like Healthy Athletes that have been launched around this, but it’s still nowhere near good enough. And so this was a really fascinating story on that front and on a population that’s really falling through the cracks.
Rovner: It really was. Lauren.
Weber: I actually picked an opinion piece in Stat that’s called, quote, “How the Next President Should Reform Medicare,” by Paul Ginsburg and Steve Lieberman. And I want to give a shoutout to my former colleague Fred Schulte, who basically has single-handedly revealed — and now, obviously, there’s been a lot of fall-on coverage — but he was really beating this drum first, how much Medicare Advantage is overbilling the government.
And Fred, through a lot of FOIAs [Freedom of Information Act requests] — and KFF has sued to get access to these documents — has shown that, through government audits, the government’s being charged billions and billions of dollars more than it should be to pay for Medicare Advantage, which was billed as better than Medicare and a free-market solution and so on. But the reality is …
Rovner: It was billed as cheaper than Medicare.
Weber: And billed as cheaper.
Rovner: Which it’s not.
Weber: It’s not. And this opinion piece is really fascinating because it says, look, no presidential candidate wants to talk about changing Medicare, because all the folks that want to vote usually have Medicare. But something that you really could do to reduce Medicare costs is getting a handle around these Medicare Advantage astronomical sums. And I just want to shout out Fred, because I really think this kind of opinion piece is possible due to his tireless coverage to really dig into what’s some really wonky stuff that reveals a lot of money.
Rovner: Yes, I feel like we don’t talk about Medicare Advantage enough, and we will change that at some point in the not-too-distant future. All right, well, my story is from KFF Health News from my colleague Noam Levey, along with Ames Alexander of the Charlotte Observer. It’s called “How North Carolina Made Its Hospitals Do Something About Medical Debt.”
Those of you who are regular listeners may remember back in August when we talked about the federal government approving North Carolina’s unique new program to have hospitals forgive medical debt in exchange for higher Medicaid payments. It turns out that getting that deal with the state hospitals was a lot harder than it looked, and this piece tells the story in pretty vivid detail about how it all eventually got done. It is quite the tale and well worth your time.
OK, that is our show for this week. As always, if you enjoy the podcast, you can subscribe wherever you get your podcast. We’d appreciate it if you left us a review. That helps other people find us, too. Special thanks as always to our technical guru, Francis Ying, and our editor, Emmarie Huetteman. Also, as always, you can email us your comments or questions. We’re at whatthehealth@kff.org, or you can still find me at X. I’m @jrovner. Lauren, where are you?
Weber: I’m still on X @LaurenWeberHP.
Rovner: Alice?
Ollstein: On X at @AliceOllstein.
Rovner: Joanne?
Kenen: X @JoanneKenen and Threads @JoanneKenen1.
Rovner: We will be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 1 month ago
Elections, Health Care Costs, Multimedia, Pharmaceuticals, States, Abortion, Drug Costs, KFF Health News' 'What The Health?', Obamacare Plans, Podcasts, reproductive health, U.S. Congress, Women's Health
In Montana Senate Race, Democrat Jon Tester Misleads on Republican Tim Sheehy’s Abortion Stance
Tim Sheehy “would let politicians like him ban abortion, with no exceptions for rape or to save a woman’s life, and criminalize women.”
A Facebook ad from the campaign of Sen. Jon Tester (D-Mont.), launched on Sept. 6, 2024
Tim Sheehy “would let politicians like him ban abortion, with no exceptions for rape or to save a woman’s life, and criminalize women.”
A Facebook ad from the campaign of Sen. Jon Tester (D-Mont.), launched on Sept. 6, 2024
In a race that could decide control of the U.S. Senate, Sen. Jon Tester (D-Mont.) is attacking his challenger, Republican Tim Sheehy, for his stance on abortion.
Montana’s Senate race is one of a half-dozen tight contests around the country in which Democrats are defending seats needed to keep their one-seat majority. If Republicans flip Tester’s seat, they could take over the chamber even if they fail to oust Democrats in any other key races.
In a series of Facebook ads launched in early September, Tester’s campaign said Sheehy supports banning abortion with no exceptions.
An ad launched on Sept. 6 said, “Tim Sheehy wants to take away the freedom to choose what happens with your own body, and give that power to politicians. Sheehy would let politicians like him ban abortion, with no exceptions for rape or to save a woman’s life, and criminalize women. We can’t let Tim Sheehy take our freedom away.”
Sheehy’s Anti-Abortion Stance Allows for Rape, Health Exceptions
Sheehy’s website calls him “proudly pro-life,” and he’s campaigning against abortion. He opposes a measure on Montana’s November ballot that would amend the Montana Constitution to provide the right to “make and carry out decisions about one’s own pregnancy, including the right to abortion.”
In July, we rated False Sheehy’s statement that Tester and other Democrats have voted for “elective abortions up to and including the moment of birth. Healthy, 9-month-year-old baby killed at the moment of birth.”
But contrary to the new ad’s message, Sheehy has voiced support for exceptions.
In a Montana Public Radio interview in May, Sheehy was asked, “Yes or no, do you support a federal ban on abortion?”
Sheehy said, “I am proudly pro-life and support commonsense protections for when a baby can feel pain, as well as exceptions for rape, incest, and the life of the mother, and I believe any further limits must be left to each state.”
And in a June debate with Tester, Sheehy said, “I’ll always protect the three rights for women: rape, incest, life of the mother.”
The issues section of Sheehy’s campaign website does not say that he has a no-exceptions stance, nor does it say he would “criminalize women” who have abortions.
In a statement, the Sheehy campaign told PolitiFact that the ad mischaracterizes Sheehy’s abortion position. Allowing no exceptions “has never been Tim’s position,” the campaign said.
Our Ruling
The Tester campaign’s ad says Sheehy “would let politicians like him ban abortion, with no exceptions for rape or to save a woman’s life, and criminalize women.”
Sheehy has said he supports abortion ban exceptions for rape or to save a pregnant woman’s life. We found no instances of him saying he would be OK with states criminalizing women who receive abortions in violation of state laws.
What gives the ad a kernel of truth is that Sheehy has voiced support for letting states decide abortion parameters within their borders. The Tester campaign argues that this means Sheehy would effectively enable legislators to pass abortion restrictions that don’t include exceptions or that criminalize women.
The Tester campaign’s argument relies on hypotheticals and ignores Sheehy’s stated support for exceptions, giving a misleading impression of Sheehy’s position.
We rate it Mostly False.
Our Sources
Jon Tester, Facebook ad, Sept. 6, 2024
Tim Sheehy, campaign issues page, accessed Sept. 12, 2024
KFF, “Policy Tracker: Exceptions to State Abortion Bans and Early Gestational Limits,” last updated July 29, 2024
Montana Public Radio, “Q&A: Tim Sheehy, Republican Candidate for U.S. Senate,” May 15, 2024
Montana Senate debate (excerpt), June 9, 2024
Last Best Place PAC, “choice” web page, accessed Sept. 12, 2024
Montana Republican Party, 2024 platform, accessed Sept. 12. 2024
Daily Montanan, “Sheehy criticizes ballot measures, including initiative to protect abortion,” Aug. 22, 2024
Sabato’s Crystal Ball, “Where Abortion Rights Will (or Could) Be on the Ballot,” July 9, 2024
Heartland Signal, “Unearthed audio shows Tim Sheehy calling abortion ‘sinful,’ wanting it to ‘end tomorrow,’” Aug. 30, 2024
Montana Independent, “Jon Tester accuses Tim Sheehy of lying about abortion during first Senate campaign debate,” June 11, 2024
Statement to PolitiFact from the Sheehy campaign
Statement to PolitiFact from the Tester campaign
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 1 month ago
States, Abortion, KFF Health News & PolitiFact HealthCheck, Montana, U.S. Congress, Women's Health